Abstract
The neurotropic JHM strain of mouse hepatitis virus (JHMV) replicates primarily within glial cells following intracranial inoculation of susceptible mice, with relative sparing of neurons. This study demonstrates that glial cells derived from neural progenitor cells are susceptible to JHMV infection and that treatment of infected cells with IFN-γ inhibits viral replication in a dose-dependent manner. Although type I IFN production is muted in JHMV-infected glial cultures, IFN-β is produced following IFN-γ-treatment of JHMV-infected cells. Also, direct treatment of infected glial cultures with recombinant mouse IFN-α or IFN-β inhibits viral replication. IFN-γ-mediated control of JHMV replication is dampened in glial cultures derived from the neural progenitor cells of type I receptor knock-out mice. These data indicate that JHMV is capable of infecting glial cells generated from neural progenitor cells and that IFN-γ-mediated control of viral replication is dependent, in part, on type I IFN secretion.
Keywords: Virus, Neural progenitor cells, Central nervous system, Interferons
Introduction
Inoculation of the neurotropic JHMV strain of mouse hepatitis virus (a positive-strand RNA virus and a member of the Coronaviridae family) into the CNS of susceptible strains of mice results in an acute encephalomyelitis. The resulting infection is characterized by wide-spread viral replication in astrocytes, microglia, and oligodendrocytes with relatively few infected neurons (Buchmeier and Lane, 1999, Knobler et al., 1981, Parra et al., 1999, Perlman et al., 1999). JHMV infection of the CNS induces localized expression of pro-inflammatory factors that precedes and accompanies the activation and recruitment of immune cells into the CNS. During the acute disease phase, infiltrating virus-specific CD8+ T cells control viral replication by two different effector mechanisms: IFN-γ secretion controls viral replication in oligodendrocytes, while a perforin-dependent mechanism promotes viral clearance from astrocytes and microglia (Lin et al., 1997, Parra et al., 1999). While a robust and effective cell-mediated immune response is generated in response to JHMV infection, virus persists within the CNS and is associated with the development of an immune-mediated demyelinating disease similar to the human demyelinating disease MS. During this stage, both T cells and macrophages are important in amplifying disease severity by contributing to myelin damage (Cheever et al., 1949, Perlman et al., 1999).
Stem cells and neural precursors represent attractive sources for the generation of remyelination-competent cells since they can readily amplify and differentiate into oligodendrocyte committed cells (Ben-Hur et al., 1998, Brustle et al., 1999). Stem cell-derived glial precursors have been shown to myelinate following transplantation into the myelin-deficient rat (Brustle et al., 1999), and neural precursor-derived glial-committed progenitors (Ben-Hur et al., 1998, Keirstead et al., 1999) have been shown to remyelinate following transplantation into regions of acute experimental demyelination (Keirstead et al., 1999). More recently, intracerebroventricular or intrathecal implantation of neural precursors into rodents with EAE, an autoimmune model of demyelination, resulted in the migration of transplanted cells into white matter and improved clinical outcome (Ben-Hur et al., 2003, Pluchino et al., 2003).
While implantation of myelin-competent cells has shown to be effective in promoting remyelination in animal models of demyelination initiated by either infiltration of autoreactive lymphocytes or injury, there is limited information available with regards to the ability of these cells to enhance demyelination resulting from viral infection. We believe this is an important and clinically relevant question as the etiology of MS remains enigmatic although viruses have long been considered potential triggering agents for initiating disease (Gilden, 2005, Olson et al., 2005). Therefore, evaluating potential cell-replacement strategies for inducing remyelination in viral models of neurologic disease may yield insight into whether this method of treatment is effective within the CNS in which a persistent virus is present. With this in mind, we recently demonstrated that surgical engraftment of glial committed progenitor cells derived from neural precursors into JHMV-infected mice with established demyelination resulted in extensive migration accompanied by remyelination and axonal sparing (Totoiu et al., 2004). Moreover, remyelination was not associated with dampened T cell infiltration into the CNS as has recently been reported following NSC transplantation in mice with EAE (Aharonowiz et al., 2008, Einstein et al., 2006, Hardison et al., 2006). Having demonstrated that engraftment of glial cells promotes remyelination following JHMV-induced demyelination, we next were interested in addressing several interrelated issues including i) if glial cells derived from neural precursor cells were susceptible to infection and ii) how infection may be controlled within this population of cells. We believe these are relevant questions within the context of studying animal models of viral-induced demyelination as cells are being transplanted into the CNS in which a persistent virus is present. Therefore, analyzing the susceptibility of cellular progeny derived from neural precursor cells to viral infection is important in that these cells may represent important viral reservoirs in the face of persistent infection. Understanding consequences of infection and how replication may be controlled within these cells will provide insight into understanding host defense mechanisms of implanted cells as well as potential relevance to disease outcome. The relevance of this is further highlighted by the fact that while previous studies have demonstrated that JHMV is able to infect and replicate within glial cells (Dubois-Dalcq et al., 1982, Lavi et al., 1987, Rempel et al., 2005), the fate of neural progenitor cells as well as cells derived from this population to viral infection is not well characterized.
In the present study, we demonstrate that primary cultures of glia derived from neural progenitor cells are susceptible to JHMV infection and support viral replication. Additionally, while IFN-β production is dampened in response to viral infection, treatment with recombinant mouse IFN-γ inhibits JHMV replication. The IFN-γ-mediated antiviral effect is dampened in experiments using cells derived from type I IFN receptor-deficient mice (IFNAR−/−) indicating a role for type I IFN signaling in limiting JHMV replication in glia-committed progenitor cells. Therefore, these findings provide, to our knowledge, the first demonstration that glia-committed cells derived from neural precursors are susceptible to JHMV infection as well as identify a potential mechanism responsible for controlling viral replication.
Results
Neural progenitor cell cultures
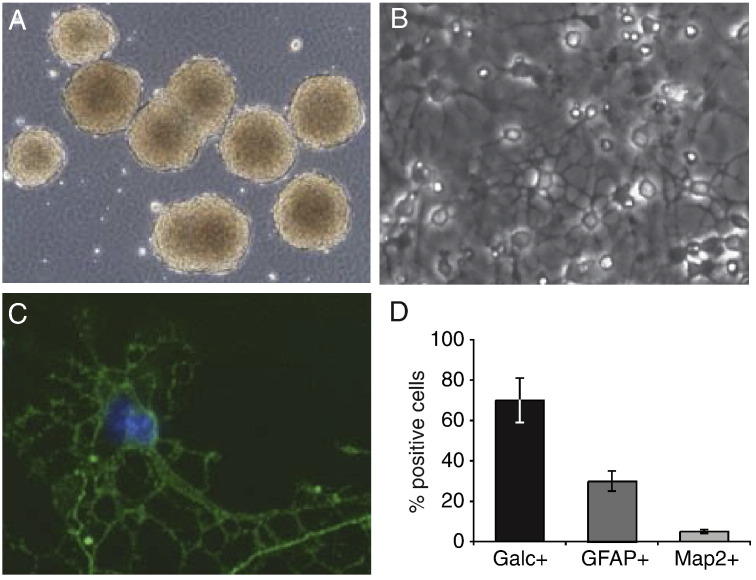
The in vitro culture of neural progenitor cells dissected from the striatal region of the brains of day 1 postnatal C57BL/6 mice resulted in the generation of numerous neurospheres (Fig. 1 A) (Hardison et al., 2006, Totoiu et al., 2004). After the mature neurospheres were plated on an adherent matrix and incubated in growth medium, the majority of the cells exhibited oligodendrocyte morphology characterized by extensive arborization (Fig. 1B). Immunocytochemical staining confirmed the morphology results indicating that ∼ 70% of the cells differentiated into oligodendrocytes (determined by GalC staining) (Fig. 1C). The remaining cells had differentiated into either astrocytes (∼ 25%, GFAP-expression) or neurons (< 5%, Map2 staining) (Fig. 1D). These differentiated neural progenitor cultures were used for the subsequent studies examining JHMV susceptibility to infection.
Fig. 1.
Differentiation of neural progenitor cells. The differentiation potential of striatal neural precursors can be restricted by culture conditions. (A) Cell cluster after 5 days of growth in non-adherent growth factor containing media, viewed in phase contrast. Cells were grown as free-floating clusters, reaching approximately 200 mm in diameter. (B) Cells spread out from clusters within 6 h of plating, and by 2 days, possess complex morphologies. (C) Multipolar GalC-positive (green) oligodendrocytes were abundant after 7 days of growth on adherent substrate in the absence of growth factors (Hoechst-positive nuclei is blue). (D) Quantification of cell types after 7 days of growth on adherent substrate in the absence of growth factors indicated that the differentiation protocol yielded ∼ 70% Galc+ oligodendrocytes, ∼ 25% GFAP+ astrocytes, and ∼ 5% Map2+ neurons as determined by immunocytochemistry. Data are presented as average ± SEM and are representative of results of four independent cultures. 40× magnification for (A), 200× magnification for (B), and 400× for magnification for (C).
JHMV infects and replicates in differentiated neural progenitor cell cultures
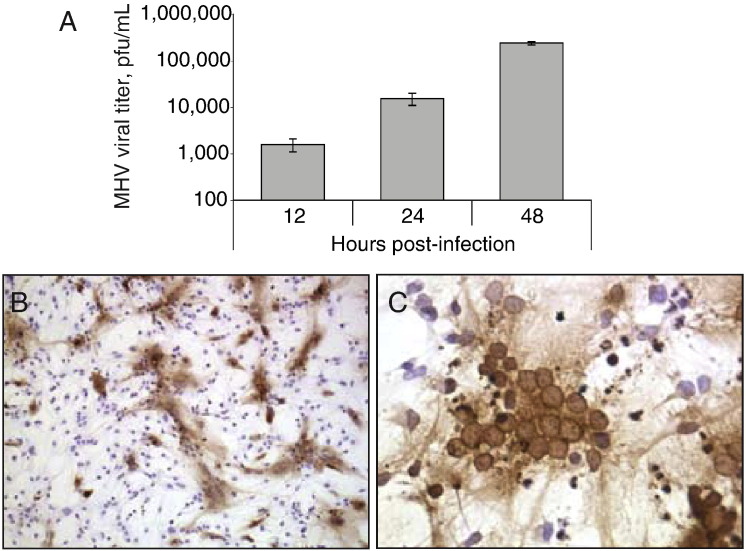
JHMV is able to infect and replicate in differentiated neural progenitor cultures as demonstrated by increasing viral titers measured at 12, 24, and 48 h p.i. (Fig. 2 A). Immunocytochemistry revealed viral antigen distributed extensively throughout the monolayer (Fig. 2B). In addition, JHMV infection resulted in cytopathic effects by 24 h p.i. characterized by wide-spread syncytia formation (Fig. 2C). These findings indicate that differentiated cells derived from neural progenitors are susceptible to JHMV infection and are capable of supporting replicating virus which results in extensive cytopathology.
Fig. 2.
JHMV replicates in glial-derived cell cultures. (A) Differentiated progenitor cultures were infected with JHMV and viral titers in supernatants determined at 12, 24, and 48 h post-infection (p.i.) by plaque assay. Data are presented as average ± SEM and represent two independent experiments. Immunocytochemical staining for viral antigen at 2 SEM and represent two independent experiments. Immunocytochemical staining for viral antigen at 2. 4 h p.i. revealed wide-spread distribution of virus throughout the cell culture (B, 100× magnification) with extensive cytopathology as characterized by large areas of syncytia formation (C, 400× magnification). Expression of viral antigen was determined using mAb-specific for the N protein of JHMV and visualized by immunoperoxidase staining.
IFN-γ suppresses JHMV replication in cultured OPC
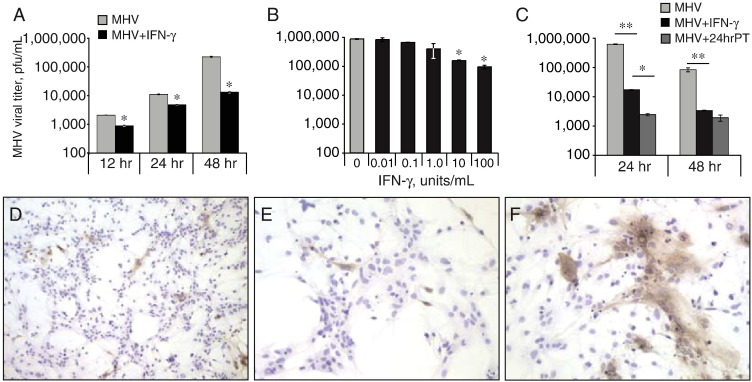
Previous studies by Parra et al. (1999) demonstrated that IFN-γ has an important role in controlling JHMV replication within oligodendrocytes of persistently infected mice. Therefore, we next determined whether IFN-γ was capable of inhibiting JHMV replication following infection of differentiated neural progenitor cells. As shown in Fig. 3 A, treatment of JHMV-infected cells with recombinant mouse IFN-γ inhibited viral replication at 12 (57% reduction, p < 0.05), 24 (56% reduction, p < 0.05), and 48 h p.i. (94% reduction, p < 0.05) compared to media-treated controls. Moreover, the IFN-γ-mediated inhibition of JHMV-replication was concentration-dependent; titration of IFN-γ resulted in diminished antiviral effects (Fig. 3B). The pretreatment of cultures with IFN-γ (100 U/ml) resulted in a significant (p < 0.05) reduction in viral titers at 24 h p.i. when compared to cultures incubated with IFN-γ following infection (Fig. 3C). Immunocytochemistry revealed that IFN-γ treatment of differentiated neural progenitor cultures limited the extensive cytopathic effects (Figs. 3D and E) observed in untreated cells (Fig. 3F) as characterized by diminished syncytium formation. Together these data indicate that IFN-γ activates differentiated neural progenitors to inhibit JHMV replication, which correlates with muted cytopathology.
Fig. 3.
IFN-γ inhibits viral replication in glial-derived cultures. (A) Differentiated progenitor cultures were infected with JHMV and subsequently treated with recombinant mouse IFN-g (10 (100 U/ml). Viral titers were determined in culture supernatants at 12, 24, and 48 h p.i. IFN-γ-treated cultures had significantly (p ≤ 0.05) reduced viral titers at all time points examined. (B) Titration of IFN-γ revealed a concentration-dependent anti-viral effect with significant (p ≤ 0.05) inhibition in viral replication occurring with IFN-γ treatment of 100 or 10 U/ml. Viral titers were determined at 24 h p.i. (C) Pre-treatment of cultures with IFN-γ (100 U/ml, 24 h) enhanced anti-viral effect as demonstrated by significant reduction in viral titers at 24 h p.i. compared to cultures treated with IFN-γ at the time of infection. (D–F) Staining for viral antigen in IFN-γ-treated cultures at 24 h p.i. revealed limited syncytia formation (D, 100× magnification) and viral antigen detected in single cells (E, 200× magnification). In contrast, media controls exhibited extensive viral replication and syncytium (F, 200× magnification). ⁎p ≤ 0.05, ⁎⁎p ≤ 0.001.
IFN-γ-mediated suppression of JHMV replication is not dependent on expression of non-ELR chemokines
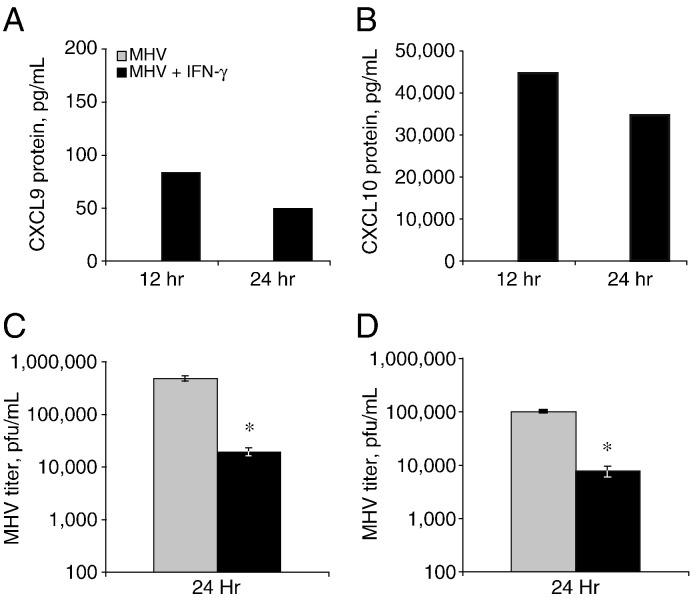
It is known that IFN-γ is capable of inducing expression of the non-ELR chemokines CXCL9 and CXCL10 in numerous cell types including resident cells of the CNS such as astrocytes and microglia (Bhowmick et al., 2007, Majumder et al., 1998, Vanguri and Farber, 1994). Moreover, in vivo astrocytes have been shown to express CXCL9 and CXCL10 mRNA transcripts during the acute response to JHMV infection and in vitro cultured astrocytes are capable of expressing CXCL10 mRNA transcripts (Lane et al., 1998, Liu et al., 2000, Liu et al., 2001). Neither CXCL9 nor CXCL10 are detectable in differentiated neural progenitor cultures in response to JHMV infection at 12 or 24 h p.i. (Figs. 4 A and B). In contrast, IFN-γ treatment of infected cultures resulted in measurable levels of both CXCL9 and CXCL10 at 12 and 24 h p.i. (Figs. 4A and B). Levels of CXCL10 were dramatically higher (∼ 45,000 pg/ml at 12 h) compared to CXCL9 levels (∼ 75 pg/ml at 12 h) suggesting differential promoter sensitivities to IFN-γ treatment or altered stability at either RNA or protein levels. To assess the importance of IFN-γ-mediated production of CXCL9 and CXCL10 in the inhibition of JHMV replication, neural progenitor cells were isolated from CXCL10−/− mice and mice deficient in the signaling receptor for CXCL9 and CXCL10, CXCR3 (CXCR3−/− mice). The neural progenitor cells from deficient mice were differentiated in vitro, infected with JHMV and treated with IFN-γ. As we observed in wildtype mice, such treatment resulted in a significant reduction in viral titers at 24 h p.i. compared to infected cells incubated with medium alone (Figs. 4C and D). Therefore, the IFN-γ-mediated anti-viral effect observed occurs independently of either production of CXCL9, and CXCL10 or CXCR3 signaling.
Fig. 4.
The IFN-γ-mediated antiviral effect is not dependent upon expression of CXCL9 or CXCL10. Expression of the non-ELR CXC chemokines CXCL9 (A) and CXCL10 (B) was determined by ELISA at 12 and 24 h following either infection with JHMV alone or IFN-g-treatment of infected cultures. JHMV infection did not result in detectable protein levels for either CXCL9 or CXCL10. Treatment of infected cultures with IFN--treatment of infected cultures. JHMV infection did not result in detectable protein levels for either CXCL9 or CXCL10. Treatment of infected cultures with IFN-γ (100 U/ml) did result in elevated levels of both CXCL9 and CXCL10. IFN-γ treatment of JHMV-infected cells derived from either CXCL10−/− mice (C) or CXCR3−/− mice (D) resulted in significant (⁎p < 0.05) reduction in viral replication at 24 h p.i. Results shown in (A) and (B) are representative of two independent experiments. Results in (C) and (D) are presented as average ± SEM and represent two independent experiments.
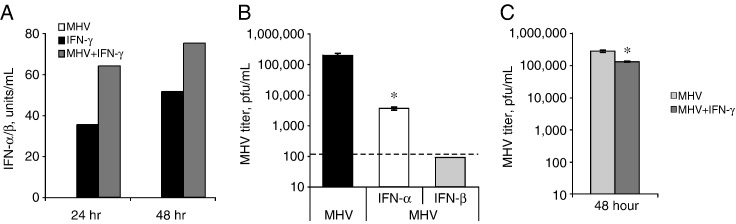
IFN-α/β production following IFN-γ-treatment
Type I IFN (IFN α and β) exhibit potent antiviral activity and have recently been shown to be important in controlling JHMV replication in vivo (Ireland et al., 2008). Therefore, we next evaluated production of type I IFN from differentiated progenitor cultures following JHMV infection. As shown in Fig. 5 A, JHMV infection did not result in detectable levels of IFN-α/β at either 24 or 48 h p.i. However, IFN-γ treatment of JHMV-infected cultures resulted in expression of IFN-α/β that was elevated compared to treatment with IFN-γ alone (Fig. 5A). Further, direct treatment with either recombinant mouse IFN-α or IFN-β of JHMV-infected cultures resulted in a dramatic reduction in viral replication compared to media treatment (Fig. 5B). IFN-β exhibited ∼ 90% greater reduction in viral replication compared to IFN-α treatment indicating a more potent antiviral activity associated with IFN-β signaling (Fig. 5B). Next, progenitor derived glial cultures were generated from type I IFN receptor-deficient mice (IFN-R−/−) mice and treated with IFN-γ following JHMV infection. As shown in Fig. 5C, such treatment did result in a reduction in viral replication (p < 0.05) compared to media-treated controls by 48 h p.i. However, viral replication was reduced, on average, by only 53% in IFN-R−/− cells compared to > 90% reduction in wildtype cells (Figs. 3A and C). Therefore, these data indicate that the IFN-γ-mediated antiviral effect is diminished in the absence of type I IFN signaling indicating that one mechanism by which IFN-γ promotes control of JHMV replication within glial-derived progenitors is through induction of type I IFN.
Fig. 5.
Type I IFN inhibits JHMV replication in differentiated glial cultures. (A) Type I IFN was measured in supernatants from cell cultures infected with JHMV and/or treated with IFN-γ (100 U/ml) at 24 and 48 h p.i. No detectable IFN-α/β was present in cultures infected with virus alone yet IFN-γ treatment resulted in IFN-α/β production at 24 h that increased by 48 h post-treatment. IFN-γ treatment of JHMV-infected cultures resulted in increased IFN-α/β production compared to IFN-γ treatment alone at both 24 and 48 h time points. (B) Treatment of JHMV-infected cultures with either 100 U/ml of recombinant IFN-α or IFN-β diminished viral replication compared to untreated cultures with a greater anti-viral effect observed with IFN-β (value below limit of detection, < 150 pfu/ml) compared to IFN-α (⁎p < 0.05). (C) Glial cultures were derived from progenitor cells obtained from type I IFNR−/− mice, infected with virus and treated with IFN-γ (100 U/ml) and viral titers determined at 48 h p.i. IFN-γ treatment resulted in a reduction (⁎p < 0.05) in viral titers when compared to media control cultures at either time point. Data are presented as average ± SEM and are representative of two independent experiments.
Discussion
The findings put forth in this paper provide, to our knowledge, the first demonstration that JHMV is capable of infecting and replicating within primary cultures of glia derived from neural progenitor cells. These findings are distinct from earlier studies (Dubois-Dalcq et al., 1982, Lavi et al., 1987, Rempel et al., 2005) showing that primary neural cultures are susceptible to viral infection, as we have allowed for differentiation of glial cells from neural progenitor cells into defined glia populations. In addition, we have demonstrated that IFN-γ treatment of JHMV-infected cultures suppresses JHMV replication and this is dependent, in part, on secretion of IFN-I. The importance of IFN-I in defense following viral infection of the CNS has been documented in several animal models. Infection of mice in which IFN-I is genetically silenced or signaling blocked results in uncontrolled proliferation of West Nile virus (Samuel and Diamond, 2005), Sindbis virus (Burdeinick-Kerr et al., 2007, Byrnes et al., 2000), and Semliki forest virus (Fragkoudis et al., 2007). The cellular source of IFN-I production is controlled by viral tropism and the model system employed. For example, neurons are a primary source of IFN-I in response to West Nile virus infection and these cells also represent a prominent cellular target for viral infection and replication (Samuel and Diamond, 2005). Similarly, robust cytokine production, including IFN-β, is observed following infection of astrocyte cultures with Theiler's murine encephalomyelitis virus (TMEV) (Palma et al., 2003). In the case of JHMV infection, emerging evidence highlights the importance of IFN-I in protection of the CNS in response to infection. Bergmann and colleagues (Ireland et al., 2008) recently demonstrated increased mortality correlating with wide-spread JHMV dissemination throughout the parenchyma including expanded cell tropism with neurons infected in mice deficient in IFN-I receptor (IFNR−/−). Additional support for an important role for IFN-I in host defense in response to infection with mouse coronaviruses are derived from studies that demonstrate increased disease severity following anti-IFN antibody treatment (Lavi and Wang, 1995) and enhanced resistance following treatment with recombinant IFN-β (Matsuyama et al., 2000, Smith et al., 1987).
Further support for mouse coronaviruses in initiating IFN-I production following experimental infection of mice are provided by studies from Cervantes-Barragan et al. (2007) indicating that peripheral infection with a hepatotropic strain of MHV (MHV-A59) results in increased IFN-I production by plasmacytoid dendritic cells. While it is clear that IFN-I is produced in vivo in response to mouse coronavirus infection and participates in effective host defense, the molecular signals regulating expression on a cellular basis are less well characterized. Indeed, IFN-β is not produced in response to JHMV infection of fibroblasts but this is not dependent on the absence of intracellular double-stranded RNA or deficiencies in IFN-β signaling (Roth-Cross et al., 2007). Impaired IFN-β production within JHMV-infected cultures correlated with impaired translocation of transcription factors IRF-3 and IRF-7 into the nucleus of infection cells (Versteeg et al., 2007, Zhou and Perlman, 2007). In addition, it may be possible that double-stranded RNA generated during the course of JHMV infection is not accessible to cellular pattern recognition receptors (PPR) such as RIG-I, Mda-5, and TLR-3 (Zhou and Perlman, 2007). While the molecular mechanisms associated with inhibited IFN-β production have not been completely defined, the MHV nucleocapsid protein has been suggested to be an IFN-I antagonist (Ye et al., 2007).
Data provided in the current study demonstrate that JHMV infection of differentiated progenitor cells resulted in muted expression of IFN-I and virus was able to replicate in an unrestricted manner. In addition, secretion of CXCL9 and CXCL10 was also impaired following JHMV infection of differentiated progenitor cultures and this is in contrast to previous findings indicating robust chemokine expression following infection of primary cultures of astrocytes. These results support the earlier hypothesis that within certain host cell populations, double-stranded RNA generated during the course of JHMV replication may not be accessible to PPR and this impacts secretion of IFN-I and non-ELR chemokines CXCL9 and CXCL10. Moreover, since the majority of progenitor cells (∼ 70–80%) differentiate into oligodendrocyte progenitor cells (OPC), it is possible that oligodendrocytes are unable to synthesize either CXCL9 or CXCL10 in response to JHMV infection.
Treatment of progenitor cultures with IFN-γ resulted in reduced JHMV replication and this highlights the importance of this cytokine in host defense following JHMV infection. Additionally, these data support and extend studies by Stohlman and colleagues (Gonzalez et al., 2005 Gonzalez et al., 2006, Parra et al., 1999) that have demonstrated IFN-γ is critical in controlling JHMV replication in oligodendrocytes in vivo. Infection of IFN-γ−/− mice with JHMV highlighted a critical role for this cytokine in controlling viral replication within oligodendrocytes (Parra et al., 1999). Additionally, transgenic mice expressing a dominant-negative IFN-γ-receptor specifically on oligodendroglia demonstrated that IFN-γ is required for inhibiting viral replication (Gonzalez et al., 2005 , 2006). The findings put forth in the present study clearly indicate that IFN-γ suppresses JHMV replication in glial-committed progenitor cells derived from neural precursors. Moreover, the IFN-γ-mediated antiviral effect is not dependent on secretion of CXCR3-binding chemokines. Although the in vivo mechanism(s) by which IFN-γ evokes an antiviral response have not yet been defined, our data suggest that production of IFN-I by IFN-γ-treated glia may contribute to viral control. Further support for type I IFN in controlling JHMV replication within oligodendrocyte-enriched cultures is provided by the demonstration that treatment of JHMV-infected oligodendrocytes with either recombinant IFN-α or IFN-β resulted in > 1 log decrease in viral titers with IFN-β having a much greater anti-viral effect compared to IFN-α in controlling replication.
Neurotropic viruses are capable of infecting and replicating within OPC (Dietrich et al., 2004, Levine et al., 1998, Mock et al., 2006). For example, human herpesvirus 6 (HHV6) is capable of infecting and replicating within the human oligodendrocytes and suggested to be involved in the pathogenesis of both acute and chronic inflammatory demyelinating diseases (Dietrich et al., 2004, Mock et al., 2006). HHV6 infection of human OPC cultures results in formation of multinucleated syncytia and elevated expression of GalC (Dietrich et al., 2004). OPC proliferation was also impaired in HHV6-infected cultures and infected cells and suggests that infection in vivo may have long-lasting effects on precursor cell properties. These findings are interesting in that remyelination is relatively slow in JHMV-infected mice yet OPC are present within and surrounding areas of on-going demyelination. This suggests that the ability of OPC to successfully remyelinate axons is impaired and/or an environment that is conducive for promoting remyelination is not available. Having demonstrated that JHMV is capable of infecting and replicating within primary cultures of OPC indicates that these cells are susceptible to infection in vivo. Therefore, it is interesting to speculate that early infection of neural progenitor cells impacts either generation of OPC and/or the ability of OPC to successfully remyelinate demyelinated axons at later stages of infection. We are currently addressing these possibilities.
Materials and methods
Virus and mice
The neurotropic strain JHMV (2.2V-1) of mouse hepatitis virus (MHV) was used for all experiments described here (Fleming et al., 1986). Wild type mice for progenitor cell isolation, C57BL/6 mice (on the H-2b background), were purchased from the National Cancer Institute (Frederick, MD). Additional mouse strains used for progenitor cultures, CXCL10−/−, CXCR3−/−, and IFN-I receptor deficient (IFNAR−/−) (C57BL/6 H-2b background), were bred in the University of California, Irvine animal facility. The animal protocols and procedures used for these studies were reviewed and approved by the Institutional Animal Care and Use Committee of the University of California, Irvine.
Neural progenitor cultures
Neural progenitor cells were cultured as previously described (Totoiu et al., 2004). In brief, striata from 5 to 6 postnatal day 1 mice were dissected, triturated and dissociated in 0.05% Trypsin-EDTA. The resulting single cell suspension was cultured for 6–7 days in 25 ml serum free media (DMEM:F12 supplemented with B27 supplement, 1× Insulin–Transferrin–Selenium-X Supplement, 1× Penicillin–Streptomycin and T3) with 20 ng/ml human recombinant epidermal growth factor (EGF; Sigma-Aldrich) (Ben-Hur et al., 1998). Media was replaced on days 1, 3, and 5; culture supernatant and floating clusters were removed, centrifuged at 300 ×g for 5 min and resuspended in fresh media with EGF. After one week, cells had proliferated into numerous free-floating spheres.
Adhesion and differentiation of cell spheres
After one week, cell spheres were transferred to matrigel (BD Bioscience, Bedford, MA) coated flasks (use thin coat method, 1:30 dilution) at a low density. Individual cells spread out from the attached spheres and formed a monolayer with 1 to 2 days. Once the monolayer formed, cells were trypsinized, counted and plated into four chamber imaging slides (Nalgene-Nunc International, Rochester, NY), 6-well plates or T25 flask (Costar, Corning, NY) previously coated with matrigel (BD Biosciences). Cells were allowed to equilibrate for an additional 1–2 days before viral infection or staining procedures were done.
Viral infection and viral titer assay
For all experiments shown, JHMV was added to cultures at a multiplicity of infection (MOI) of 0.1 pfu/cell. Virus was allowed to adsorb for 1 h, cultures were washed with PBS and replaced with 4 ml of fresh medium. Recombinant mouse IFN-γ, IFN-α, and IFN-β cytokines were purchased from Cell Sciences (Canton, MA). Viral titers in supernatants of infected cultures were determined on DBT astrocytoma cells at defined time points post-infection (p.i.) (Hirano et al., 1978, Lane et al., 2000).
Immunofluorescence
To assess differentiation potential, cells were grown on matrigel coated imaging slides for a total of 4 days, fixed in 4% paraformaldehyde (Fisher Scientific, Fair Lawn, NJ) for 20 min and immunofluorescence staining was performed using standard protocols. Imaging chambers were blocked with 10% normal goat serum (NGS) (Vector Laboratories, Burlingame, CA) for 1 h at room temperature. Primary antibodies (polyclonal rabbit anti-GalC, Chemicon, 1:100 dilution in 10% NGS; monoclonal mouse anti-Map2, Sigma, 1:750 dilution in 10% NGS; polyclonal rabbit anti-GFAP, Invitrogen, 1:500 dilution in 10% NGS) or blocking solution (negative control, 10% NGS in PBS) were applied to chambers overnight at 4 °C on rocker. Slides were rinsed three times with PBS and fluorescent-conjugated secondary antibody (Alexa 594, goat anti-rabbit or goat anti-mouse IgG H + L, 1:400 dilution in 10% NGS; Invitrogen) was applied and incubated for 30 min at room temperature. Slides were rinsed three times in PBS, and nuclear staining was with Hoechst 33342 (1 μg/ml in PBS, Molecular Probes, Eugene, OR) for 10 min. Cell quantification was conducted using an Olympus BX-60 microscope, 200× magnification. The percentage of immunopositive cells was determined by dividing the total number of immunopositive cells by the total number of Hoechst-positive cells in five images from each chamber, and averaging the results from three different chambers per marker. Each 4-chamber imaging slide had one no-primary control chamber and three stained chambers for each of the markers mentioned above. Only immunopositive cells with a Hoechst-positive nucleus were counted.
Immunocytochemistry
Distribution of viral antigen in cultures was determined by immunoperoxidase staining, as specified by the manufacturer (Vectastain-ABC kit and DAB peroxidase substrate kit; Vector Laboratories). Imaging chambers were blocked with triton containing blocking buffer (BB), (0.3% Triton X-100 and 10% NGS normal goat serum in PBS), for 1 h at room temperature. The anti-JHMV mAb J.3.3 (1:20 dilution in BB) specific for the carboxyl terminus of the viral nucleocapsid (N) protein was applied and incubated overnight at 4ϒC. Slides were rinsed three times in PBS and secondary antibody (biotinylated goat-anti-mouse IgG H + L, Vector Laboratories, 1:750 dilution in BB) was applied and incubated for 1.5 h at room temperature. Slides were rinsed three times in PBS and counterstained with hematoxylin (Bergmann et al., 2003, Fleming et al., 1983, Walsh et al., 2007).
Interferon bioassay
Differentiated neural progenitor cells were infected with MHV, and levels of IFN were measured using a bioassay based on inhibition of VSV growth in L929 cells. Supernatants were harvested and exposed to UV light to inactivate infectious virus. L929 cells infected with 1000 pfu VSV were treated with dilutions of supernatants or recombinant murine IFN-β (PBL Biomedical Laboratories, Piscataway, NJ) at 30 min post-infection (p.i.). Titers of VSV were determined on Vero cells. IFN levels were calculated based on standard curves generated with recombinant IFN-β.
ELISA
OPC culture supernatants were used to measure chemokines CXCL9 and CXCL10. ELISAs were performed using the Duoset Mouse CXCL9 and CXCL10 ELISA kit (R & D Systems, Minneapolis, MN), as specified by the manufacturer.
Statistical analysis
Statistically significant differences between groups of mice were determined by Student's t test and p values of < 0.05 were considered significant.
Acknowledgments
This work was supported by the National Multiple Sclerosis Society grants 3847 (T.E.L.) and 2864 (S.P.) and the National Institutes of Health grant NS41249 to T.E.L.
References
- Aharonowiz M., Einstein O., Fainstein N., Lassmann H., Reubinoff B., Ben-Hur T. Neuroprotective effect of transplanted human embryonic stem cell-derived neural precursors in an animal model of multiple sclerosis. PLoS ONE. 2008;3(9):e3145. doi: 10.1371/journal.pone.0003145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Hur T., Rogister B., Murray K., Rougon G., Dubois-Dalcq M. Growth and fate of PSA-NCAM+ precursors of the postnatal brain. J. Neurosci. 1998;18(15):5777–5788. doi: 10.1523/JNEUROSCI.18-15-05777.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Hur T., Einstein O., Mizrachi-Kol R., Ben-Menachem O., Reinhartz E., Karussis D., Abramsky O. Transplanted multipotential neural precursor cells migrate into the inflamed white matter in response to experimental autoimmune encephalomyelitis. Glia. 2003;41(1):73–80. doi: 10.1002/glia.10159. [DOI] [PubMed] [Google Scholar]
- Bergmann C.C., Parra B., Hinton D.R., Chandran R., Morrison M., Stohlman S.A. Perforin-mediated effector function within the central nervous system requires IFN-gamma-mediated MHC up-regulation. J. Immunol. 2003;170(6):3204–3213. doi: 10.4049/jimmunol.170.6.3204. [DOI] [PubMed] [Google Scholar]
- Bhowmick S., Duseja R., Das S., Appaiahgiri M.B., Vrati S., Basu A. Induction of IP-10 (CXCL10) in astrocytes following Japanese encephalitis. Neurosci. Lett. 2007;414(1):45–50. doi: 10.1016/j.neulet.2006.11.070. [DOI] [PubMed] [Google Scholar]
- Brustle O., Jones K.N., Learish R.D., Karram K., Choudhary K., Wiestler O.D., Duncan I.D., McKay R.D. Embryonic stem cell-derived glial precursors: a source of myelinating transplants. Science. 1999;285(5428):754–756. doi: 10.1126/science.285.5428.754. [DOI] [PubMed] [Google Scholar]
- Buchmeier M.J., Lane T.E. Viral-induced neurodegenerative disease. Curr. Opin. Microbiol. 1999;2(4):398–402. doi: 10.1016/S1369-5274(99)80070-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdeinick-Kerr R., Wind J., Griffin D.E. Synergistic roles of antibody and interferon in noncytolytic clearance of Sindbis virus from different regions of the central nervous system. J. Virol. 2007;81(11):5628–5636. doi: 10.1128/JVI.01152-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrnes A.P., Durbin J.E., Griffin D.E. Control of Sindbis virus infection by antibody in interferon-deficient mice. J. Virol. 2000;74(8):3905–3908. doi: 10.1128/jvi.74.8.3905-3908.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervantes-Barragan L., Zust R., Weber F., Spiegel M., Lang K.S., Akira S., Thiel V., Ludewig B. Control of coronavirus infection through plasmacytoid dendritic cell-derived type I interferon. Blood. 2007;109(3):1131–1137. doi: 10.1182/blood-2006-05-023770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheever F.S., Daniels J.B., Pappenheimer A.M., Bailey O.T. A murine virus (JHM) causing disseminated encephalomyelitis with extensive destruction of myelin. J. Exp. Med. 1949;90(3):181–210. doi: 10.1084/jem.90.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietrich J., Blumberg B.M., Roshal M., Baker J.V., Hurley S.D., Mayer-Proschel M., Mock D.J. Infection with an endemic human herpesvirus disrupts critical glial precursor cell properties. J. Neurosci. 2004;24(20):4875–4883. doi: 10.1523/JNEUROSCI.5584-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois-Dalcq M.E., Doller E.W., Haspel M.V., Holmes K.V. Cell tropism and expression of mouse hepatitis viruses (MHV) in mouse spinal cord cultures. Virology. 1982;119(2):317–331. doi: 10.1016/0042-6822(82)90092-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einstein O., Grigoriadis N., Mizrachi-Kol R., Reinhartz E., Polyzoidou E., Lavon I., Milonas I., Karussis D., Abramsky O., Ben-Hur T. Transplanted neural precursor cells reduce brain inflammation to attenuate chronic experimental autoimmune encephalomyelitis. Exp. Neurol. 2006;198(2):275–284. doi: 10.1016/j.expneurol.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Fleming J.O., Stohlman S.A., Harmon R.C., Lai M.M., Frelinger J.A., Weiner L.P. Antigenic relationships of murine coronaviruses: analysis using monoclonal antibodies to JHM (MHV-4) virus. Virology. 1983;131(2):296–307. doi: 10.1016/0042-6822(83)90498-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming J.O., Trousdale M.D., el-Zaatari F.A., Stohlman S.A., Weiner L.P. Pathogenicity of antigenic variants of murine coronavirus JHM selected with monoclonal antibodies. J. Virol. 1986;58(3):869–875. doi: 10.1128/jvi.58.3.869-875.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fragkoudis R., Breakwell L., McKimmie C., Boyd A., Barry G., Kohl A., Merits A., Fazakerley J.K. The type I interferon system protects mice from Semliki Forest virus by preventing widespread virus dissemination in extraneural tissues, but does not mediate the restricted replication of avirulent virus in central nervous system neurons. J. Gen. Virol. 2007;88(Pt 12):3373–3384. doi: 10.1099/vir.0.83191-0. [DOI] [PubMed] [Google Scholar]
- Gilden D.H. Infectious causes of multiple sclerosis. Lancet Neurol. 2005;4(3):195–202. doi: 10.1016/S1474-4422(05)01017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez J.M., Bergmann C.C., Fuss B., Hinton D.R., Kangas C., Macklin W.B., Stohlman S.A. Expression of a dominant negative IFN-gammareceptor on mouse oligodendrocytes. Glia. 2005;51(1):22–34. doi: 10.1002/glia.20182. [DOI] [PubMed] [Google Scholar]
- Gonzalez J.M., Bergmann C.C., Ramakrishna C., Hinton D.R., Atkinson R., Hoskin J., Macklin W.B., Stohlman S.A. Inhibition of interferon-gamma signaling in oligodendroglia delays coronavirus clearance without altering demyelination. Am. J. Pathol. 2006;168(3):796–804. doi: 10.2353/ajpath.2006.050496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardison J.L., Nistor G., Gonzalez R., Keirstead H.S., Lane T.E. Transplantation of glial-committed progenitor cells into a viral model of multiple sclerosis induces remyelination in the absence of an attenuated inflammatory response. Exp. Neurol. 2006;197(2):420–429. doi: 10.1016/j.expneurol.2005.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirano N., Murakami T., Fujiwara K., Matsumoto M. Utility of mouse cell line DBT for propagation and assay of mouse hepatitis virus. Jpn. J. Exp. Med. 1978;48(1):71–75. [PubMed] [Google Scholar]
- Ireland D.D., Stohlman S.A., Hinton D.R., Atkinson R., Bergmann C.C. Type I interferons are essential in controlling neurotropic coronavirus infection irrespective of functional CD8 T cells. J. Virol. 2008;82(1):300–310. doi: 10.1128/JVI.01794-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keirstead H.S., Ben-Hur T., Rogister B., O'Leary M.T., Dubois-Dalcq M., Blakemore W.F. Polysialylated neural cell adhesion molecule-positive CNS precursors generate both oligodendrocytes and Schwann cells to remyelinate the CNS after transplantation. J. Neurosci. 1999;19(17):7529–7536. doi: 10.1523/JNEUROSCI.19-17-07529.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knobler R.L., Dubois-Dalcq M., Haspel M.V., Claysmith A.P., Lampert P.W., Oldstone M.B. Selective localization of wild type and mutant mouse hepatitis virus (JHM strain) antigens in CNS tissue by fluorescence, light and electron microscopy. J. Neuroimmunol. 1981;1(1):81–92. doi: 10.1016/0165-5728(81)90010-2. [DOI] [PubMed] [Google Scholar]
- Lane T.E., Asensio V.C., Yu N., Paoletti A.D., Campbell I.L., Buchmeier M.J. Dynamic regulation of alpha- and beta-chemokine expression in the central nervous system during mouse hepatitis virus-induced demyelinating disease. J. Immunol. 1998;160(2):970–978. [PubMed] [Google Scholar]
- Lane T.E., Liu M.T., Chen B.P., Asensio V.C., Samawi R.M., Paoletti A.D., Campbell I.L., Kunkel S.L., Fox H.S., Buchmeier M.J. A central role for CD4(+) T cells and RANTES in virus-induced central nervous system inflammation and demyelination. J. Virol. 2000;74(3):1415–1424. doi: 10.1128/jvi.74.3.1415-1424.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavi E., Wang Q. The protective role of cytotoxic T cells and interferon against coronavirus invasion of the brain. Adv. Exp. Med. Biol. 1995;380:145–149. doi: 10.1007/978-1-4615-1899-0_24. [DOI] [PubMed] [Google Scholar]
- Lavi E., Suzumura A., Hirayama M., Highkin M.K., Dambach D.M., Silberberg D.H., Weiss S.R. Coronavirus mouse hepatitis virus (MHV)-A59 causes a persistent, productive infection in primary glial cell cultures. Microb. Pathog. 1987;3(2):79–86. doi: 10.1016/0882-4010(87)90066-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine J.M., Enquist L.W., Card J.P. Reactions of oligodendrocyte precursor cells to alpha herpesvirus infection of the central nervous system. Glia. 1998;23(4):316–328. [PubMed] [Google Scholar]
- Lin M.T., Stohlman S.A., Hinton D.R. Mouse hepatitis virus is cleared from the central nervous systems of mice lacking perforin-mediated cytolysis. J. Virol. 1997;71(1):383–391. doi: 10.1128/jvi.71.1.383-391.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M.T., Chen B.P., Oertel P., Buchmeier M.J., Armstrong D., Hamilton T.A., Lane T.E. The T cell chemoattractant IFN-inducible protein 10 is essential in host defense against viral-induced neurologic disease. J. Immunol. 2000;165(5):2327–2330. doi: 10.4049/jimmunol.165.5.2327. [DOI] [PubMed] [Google Scholar]
- Liu M.T., Armstrong D., Hamilton T.A., Lane T.E. Expression of Mig (monokine induced by interferon-gamma) is important in T lymphocyte recruitment and host defense following viral infection of the central nervous system. J. Immunol. 2001;166(3):1790–1795. doi: 10.4049/jimmunol.166.3.1790. [DOI] [PubMed] [Google Scholar]
- Majumder S., Zhou L.Z., Chaturvedi P., Babcock G., Aras S., Ransohoff R.M. Regulation of human IP-10 gene expression in astrocytoma cells by inflammatory cytokines. J. Neurosci. Res. 1998;54(2):169–180. doi: 10.1002/(SICI)1097-4547(19981015)54:2<169::AID-JNR5>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- Matsuyama S., Henmi S., Ichihara N., Sone S., Kikuchi T., Ariga T., Taguchi F. Protective effects of murine recombinant interferon-beta administered by intravenous, intramuscular or subcutaneous route on mouse hepatitis virus infection. Antivir. Res. 2000;47(2):131–137. doi: 10.1016/s0166-3542(00)00097-8. [DOI] [PubMed] [Google Scholar]
- Mock D.J., Strathmann F., Blumberg B.M., Mayer-Proschel M. Infection of murine oligodendroglial precursor cells with Human Herpesvirus 6 (HHV-6) — establishment of a murine in vitro model. J. Clin. Virol. 2006;37(Suppl 1):S17–S23. doi: 10.1016/S1386-6532(06)70006-3. [DOI] [PubMed] [Google Scholar]
- Olson J.K., Ercolini A.M., Miller S.D. A virus-induced molecular mimicry model of multiple sclerosis. Curr. Top. Microbiol. Immunol. 2005;296:39–53. doi: 10.1007/3-540-30791-5_3. [DOI] [PubMed] [Google Scholar]
- Palma J.P., Kwon D., Clipstone N.A., Kim B.S. Infection with Theiler's murine encephalomyelitis virus directly induces proinflammatory cytokines in primary astrocytes via NF-kappaB activation: potential role for the initiation of demyelinating disease. J. Virol. 2003;77(11):6322–6331. doi: 10.1128/JVI.77.11.6322-6331.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra B., Hinton D.R., Marten N.W., Bergmann C.C., Lin M.T., Yang C.S., Stohlman S.A. IFN-gamma is required for viral clearance from central nervous system oligodendroglia. J. Immunol. 1999;162(3):1641–1647. [PubMed] [Google Scholar]
- Perlman S.R., Lane T.E., Buchmeier M.J. Coronaviruses: hepatitis, peritonitis, and central nervous system disease. In: Cunningham M.W., Fujinami R.S., editors. Vol. 1. Lippincott Williams & Wilkins; Philadelphia: 1999. pp. 331–348. (Effects of Microbes on the Immune System). [Google Scholar]
- Pluchino S., Quattrini A., Brambilla E., Gritti A., Salani G., Dina G., Galli R., Del Carro U., Amadio S., Bergami A., Furlan R., Comi G., Vescovi A.L., Martino G. Injection of adult neurospheres induces recovery in a chronic model of multiple sclerosis. Nature. 2003;422(6933):688–694. doi: 10.1038/nature01552. [DOI] [PubMed] [Google Scholar]
- Rempel J.D., Quina L.A., Blakely-Gonzales P.K., Buchmeier M.J., Gruol D.L. Viral induction of central nervous system innate immune responses. J. Virol. 2005;79(7):4369–4381. doi: 10.1128/JVI.79.7.4369-4381.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth-Cross J.K., Martinez-Sobrido L., Scott E.P., Garcia-Sastre A., Weiss S.R. Inhibition of the alpha/beta interferon response by mouse hepatitis virus at multiple levels. J. Virol. 2007;81(13):7189–7199. doi: 10.1128/JVI.00013-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel M.A., Diamond M.S. Alpha/beta interferon protects against lethal West Nile virus infection by restricting cellular tropism and enhancing neuronal survival. J. Virol. 2005;79(21):13350–13361. doi: 10.1128/JVI.79.21.13350-13361.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A.L., Barthold S.W., Beck D.S. Intranasally administered alpha/beta interferon prevents extension of mouse hepatitis virus, strain JHM, into the brains of BALB/cByJ mice. Antivir. Res. 1987;8(5–6):239–245. doi: 10.1016/S0166-3542(87)80002-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Totoiu M.O., Nistor G.I., Lane T.E., Keirstead H.S. Remyelination, axonal sparing, and locomotor recovery following transplantation of glial-committed progenitor cells into the MHV model of multiple sclerosis. Exp. Neurol. 2004;187(2):254–265. doi: 10.1016/j.expneurol.2004.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanguri P., Farber J.M. IFN and virus-inducible expression of an immediate early gene, crg-2/IP-10, and a delayed gene, I-A alpha in astrocytes and microglia. J. Immunol. 1994;152(3):1411–1418. [PubMed] [Google Scholar]
- Versteeg G.A., Bredenbeek P.J., van den Worm S.H., Spaan W.J. Group 2 coronaviruses prevent immediate early interferon induction by protection of viral RNA from host cell recognition. Virology. 2007;361(1):18–26. doi: 10.1016/j.virol.2007.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K.B., Edwards R.A., Romero K.M., Kotlajich M.V., Stohlman S.A., Lane T.E. Expression of CXC chemokine ligand 10 from the mouse hepatitis virus genome results in protection from viral-induced neurological and liver disease. J. Immunol. 2007;179(2):1155–1165. doi: 10.4049/jimmunol.179.2.1155. [DOI] [PubMed] [Google Scholar]
- Ye Y., Hauns K., Langland J.O., Jacobs B.L., Hogue B.G. Mouse hepatitis coronavirus A59 nucleocapsid protein is a type I interferon antagonist. J. Virol. 2007;81(6):2554–2563. doi: 10.1128/JVI.01634-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou H., Perlman S. Mouse hepatitis virus does not induce Beta interferon synthesis and does not inhibit its induction by double-stranded RNA. J. Virol. 2007;81(2):568–574. doi: 10.1128/JVI.01512-06. [DOI] [PMC free article] [PubMed] [Google Scholar]