Abstract
AIMS
Despite the widespread use of self-medication among the child population and the potential harm it can do, up-to-date epidemiological data on self-medication are sparse worldwide. The aim was to investigate the prevalence and correlates of self-medication use among non-institutionalized children in Germany, focusing on the paediatric self-medications that are most frequently used.
METHODS
All cases of last-week medicine use were recorded among 17 450 children aged 0–17 years who participated in the 2003-2006 German Health Interview and Examination Survey for Children and Adolescents. Self-medication was defined as the use of medicines that had either been bought over the counter or obtained from other sources (OS). The complex sample method was used to estimate the prevalence of, and factors associated with self-medication use.
RESULTS
During the previous week 25.2% of participants had used self-medication (17.0% used over-the-counter drugs and 9.9% other-sources drugs). Self-medication accounted for 38.5% of total medicine use and included all medication classes. These clustered among drugs acting on the respiratory system (32.1%), alimentary tract and metabolism (21.6%), skin (14.2%) and nervous system (11.3%), as well as homoeopathic preparations (8.6%). Vitamin preparations were most frequently used with a weighted user prevalence of 4.7% (5.2% vs. 4.1%, P < 0.001, boys vs. girls), followed by cough and cold medicines (CCMs) 4.4% (4.3 vs. 4.5, P > 0.05) and analgesics 3.7% (3.0% vs. 4.4%, P < 0.001, both boys vs. girls). Overall use of aspirin among children <12 years old was 0.3%; use of CCMs was substantial (4.4%), particularly among children <6 years old. Use of self-medication was closely related to older adolescent ages of between 14 and 17 years (odds ratio 1.16; 95% confidence interval 1.00, 1.33), children with a poor health status (1.29; 1.10, 1.52), with no immigration background (1.55; 1.33, 1.80), from families with a higher household income (1.23; 1.06, 1.42) and with mothers with a higher educational level (1.37; 1.19, 1.57).
CONCLUSIONS
Self-medication use is highly prevalent in Germany, particularly among children and adolescents from families with a higher socioeconomic status. Self-medication in younger children using such drugs as CCMs and aspirin suggested inappropriate drug use and potential risks. This should be closely monitored and warrants an education programme for parents in Germany.
Keywords: children and adolescents, Germany, KiGGS, paediatric, self-medication
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Common paediatric over-the-counter medications, such as cough and cold medicines (CCM) and antipyretic analgesics, can lead even to serious adverse drug effects among self-medicating children and adolescents.
The U.S. Food and Drug Administration and the UK Medicines and Healthcare Products Regulatory Agency recently again reviewed the safety of CCM use in children.
Despite the widespread use of self-medication among the child population and the potential harm it can do, up-to-date epidemiological data on self-medication are sparse worldwide.
WHAT THIS STUDY ADDS
One quarter of non-institutionalized children and adolescents in Germany had used self-medication during the previous week.
Self-medication accounted for nearly 40% of total medicine use and included all medication classes, particularly drugs acting on the respiratory system (32.1%), the alimentary tract and metabolism (21.6%), the skin (14.2%) and the nervous system (11.3%), as well as homoeopathic preparations (8.6%).
Vitamin preparations were most frequently used with a weighted prevalence of 4.7%, followed by CCMs with 4.4% and analgesics 3.7%.
Overall use of aspirin among children under 12 years of age was 0.3%; use of CCMs was substantial among children under the age of 6 years.
Our results suggest that self-medication use is highly prevalent in Germany, particularly among children and adolescents from families with a higher socioeconomic status.
Introduction
The term self-medication refers to patients who use nonprescription medicines, usually over-the-counter (OTC) drugs, to treat certain ‘minor’ ailments themselves without consulting a medical practitioner and without any medical supervision. Younger children are often given medications by their parents, whereas older adolescents may self-medicate. Paediatric OTC drugs cover a wide range of medications including cough and cold medicines (CCMs), antipyretic analgesics (e.g. paracetamol and ibuprofen), vitamin supplements and dermatological products, etc. These account for the vast majority of all paediatric OTC drugs [1–3].
Most paediatric OTC drugs, such as vitamin supplements and dermatological preparations, are safe when used properly, i.e. according to the package insert. Nevertheless, parents and adolescents may have insufficient knowledge about the medicines they use, which can lead to inappropriate drug use – even to serious, adverse drug effects among self-medicating children and adolescents [4]. For example, Reye syndrome is a life-threatening adverse reaction to aspirin in young children. Many parents are unaware that aspirin should not be given to children <12 years old [4] and that it should be used very carefully or not at all in adolescents aged 12–16 years to avoid such serious adverse drug reactions [5]. Furthermore, very few paediatric OTC drugs have been adequately tested for safety and efficacy among child populations; the dosages of most paediatric OTC drugs have been extrapolated from adult clinical and pharmacological data. Use of OTC drugs in children has been linked to serious adverse cardiovascular events due to the inadvertent overdosing of CCMs [6], for example. These events have included several infant deaths [7, 8]. In view of the severe potential risks involved, the US Food and Drug Administration and the UK Medicines and Healthcare products Regulatory Agency recently again reviewed the safety of CCM use in children [9, 10].
In spite of the risks and potential harm that can be caused by self-medication, previous epidemiological studies have revealed that self-medication among children and adolescents is common. An earlier study conducted in the USA involving 8145 young children found that 54% had been given OTC medication in the 30 days preceding the study [2]. A cross-sectional study in Australia found that 73% of children in day care had received OTC medications at some time [11], and a survey of 8500 pupils aged 11–12 and 14–15 years in the UK also indicated high rates of OTC medication use: about 20% of them had used OTC painkillers, CCMs or cold-sore treatments in any one week [12]. These studies were conducted >10 years ago, however; up-to-date population-representative surveys are sparse worldwide. Our own latest paediatric drug-use data (published in 2007) suggest that medications against upper respiratory symptoms, alimentary tract and metabolism agents (mostly various kinds of vitamin supplements) and dermatologicals are the most frequently used medication classes among children in Germany [13]. Although we noted that a substantial proportion of these medications belong to the category of paediatric OTC drugs, the author did not conduct a stratified intensive analysis because of the publication's general descriptive character [13].
According to German Federal Health Reporting (Gesundheitsberichterstattung des Bundes, http://www.gbe-bund.de), self-medication sales in Germany were worth over €5.4 billion in 2006, accounting for 15.5% of all drug consumption. There are scant data on the prevalence and correlates of OTC drugs among children in Germany, although it has been investigated in the adult population [14]. Against this background, using the data from the latest German Health Interview and Examination Survey for Children and Adolescents (KiGGS), we present the prevalence and correlates of self-medication use among the non-institutionalized child population in Germany, focusing on the most frequently used paediatric self-medications.
Methods
German Health Interview and Examination Survey for Children and Adolescents
The KiGGS was formally conducted by the Robert Koch Institute between May 2003 and May 2006, following a 1-year pre-test [15]. The survey's target population were all non-institutionalized children and adolescents aged 0–17 years living in Germany. The design, sampling strategy and study protocol have been described in detail elsewhere [15]. Briefly, two-stage sampling procedures were applied. In the first stage, a sample of 167 German municipalities was drawn that was representative of municipality sizes and structures in Germany. Stratified by sex and age, random samples of children and adolescents aged 0–17 years were then drawn from local population registries in proportion to the age and gender structure of Germany's child population. The final sample included 17 641 children and adolescents (8985 boys, 8656 girls); the response rate was 66.6% [15]. Nonresponse analysis showed little variation between the age groups and sexes, but marked variations between residence regions in east and west Germany, rural areas and cities, etc. [16], yet no difference when it came to health-related variables [15]. The survey was approved by federal data-protection officials. Written, informed consent was obtained prior to each interview and examination from children's parents and the children themselves who were aged ≥14 years.
Data collection
As described elsewhere in detail [15], standard, age-specified (0–2, 3–6, 7–10, 11–13 and 14–17 years) self-administered questionnaires completed by parents, and a parallel questionnaire filled in by children >11 years old were used to collect data on sociodemographic characteristics, family economic background, the children's medical history and health status, as well as health-related behaviour patterns such as smoking, alcohol consumption and physical leisure-time activities. The information collected on immigration background included nationality, country of birth and the year of immigration of both parents. Children with immigration background are defined as those who themselves have no German nationality or whose mother/father has no German nationality or was not born in Germany [17]. In addition, a standardized face-to-face, computer-assisted health interview was conducted with children's parents and the children themselves by trained physicians to obtain a detailed medical history of pre-existing, physician-diagnosed health problems and any medication used during the last 7 days prior to the interview. The drug-use history covered both prescribed and OTC drugs. Parents were asked in advance to bring prescriptions or original containers to the examination sites for the purpose of verification. Drug use was measured according to the following question: ‘Has your child taken any medications in the last seven days? Please also mention the use of any ointments, liniments, contraceptive pills, vitamin and mineral supplements, medicinal teas, herbal medicines or homoeopathic medicines’. Details of medication use were documented, such as brand name, condition(s) treated, daily dosage, route of application and duration of use. Specific Anatomical Therapeutic Chemical (ATC) codes were assigned to all reported medications, and World Health Organization International Classification of Diseases-10 codes to the conditions for which the medications were taken. The present analysis is based on 17 450 children and adolescents (8880 or 50.9% boys, 8570 or 49.1% girls) who provided full data on medicine use during the survey [13]. We asked about the origin of all medicines recorded, i.e. whether they were (i) prescribed by a medical doctor, (ii) prescribed by a Heilpraktiker (non-medical practitioner), (iii) OTC drugs, or (iv) from other sources (e.g. family medicine cabinet, relatives or friends, etc.). Self-medications used were defined in the present study as drugs that were either bought OTC or obtained from other sources (OS). Use of OTC and OS drugs was presented separately where deemed necessary.
Statistical analysis
Because of the differences between survey respondents and nonrespondents [16], a weighting factor was computed to adjust for deviations in demographic characteristics (age, sex, residence in west or east Germany and level of urbanicity) between the survey population and official population statistics to ensure that the survey population was representative of the national child population [15]. Descriptive statistics were used to analyse characteristics of the study population. A complex sample method was used to estimate the prevalence of, and factors associated with, self-medication use. Odds ratios (ORs) and 95% confidence intervals (CIs) were obtained from multivariate logistic regression models. All statistical analyses were performed using SPSS statistical software (release 15.0; SPSS Inc., Chicago, IL, USA). A probability level of P < 0.05 based on two-sided tests was considered statistically significant.
Results
Characteristics of the study population
The gender-specific main characteristics of the study population are described in Table 1. In this study sample, the vast majority of children (>90%) reported a good/excellent health status; about 17% of boys and girls came from families with an immigration background. Similar percentages were also observed for children residing in the former East Germany and in villages. There was no significant difference between boys and girls with regard to these selected sociodemographic and health-related characteristics except for parent-rated health status (P= 0.005).
Table 1.
Sociodemographic and health-related characteristics of survey participants by gender; German Health Interview and Examination Survey for Children and Adolescents (KiGGS), 2003–2006
| Boys | Girls | |||
|---|---|---|---|---|
| n | % (weighted) | n | % (weighted) | |
| Total | 8880 | 100 | 8570 | 100 |
| Age group, years | ||||
| 0–2 | 1397 | 13.6 | 1373 | 13.6 |
| 3–6 | 1925 | 21.0 | 1907 | 21.1 |
| 7–10 | 2103 | 21.7 | 2004 | 21.8 |
| 11–13 | 1572 | 17.3 | 1468 | 17.3 |
| 14–17 | 1883 | 26.4 | 1818 | 26.3 |
| Region | ||||
| East | 2889 | 16.5 | 2847 | 16.5 |
| West | 5991 | 83.5 | 5723 | 83.5 |
| Urbanicity | ||||
| Village | 1958 | 17.9 | 1939 | 17.9 |
| Small city | 2337 | 27.6 | 2229 | 27.2 |
| Medium-sized city | 2498 | 29.0 | 2475 | 29.3 |
| Large city | 2087 | 25.5 | 1927 | 25.6 |
| Migrant background | ||||
| Yes | 1350 | 17.4 | 1230 | 16.9 |
| No | 7498 | 82.6 | 7292 | 83.1 |
| Parent-rated health status | ||||
| Excellent | 3407 | 38.2 | 3466 | 40.1 |
| Good | 4759 | 54.7 | 4491 | 53.6 |
| Satisfactory/poor | 593 | 7.2 | 509 | 6.3 |
| Household income (€) | ||||
| <1500 | 1826 | 18.9 | 1732 | 19.2 |
| 1500–2250 | 2277 | 26.9 | 2192 | 26.3 |
| 2250–3000 | 2202 | 27.1 | 2152 | 27.3 |
| ≥3000 | 1997 | 27.1 | 1989 | 27.3 |
| Maternal educational level | ||||
| Primary | 2002 | 25.7 | 1847 | 25.2 |
| Middle | 3934 | 39.6 | 3902 | 41.1 |
| Higher | 2485 | 29.1 | 2353 | 28.0 |
| Others | 459 | 5.7 | 468 | 5.7 |
| Paternal educational level | ||||
| Primary | 2477 | 31.7 | 2355 | 31.7 |
| Middle | 3052 | 28.4 | 2881 | 27.7 |
| Higher | 2559 | 31.2 | 2541 | 31.3 |
| Others | 792 | 8.7 | 793 | 9.3 |
The sum in each category may not be equal to the total due to missing data. All percentages are weighted according to the German national child population aged 0–17 years.
Overview of self-medication use
A total of 14 588 medicines was recorded in the study sample. Of these, 5621 (38.5%) belonged to the self-medication category according to our definition, i.e. they were either bought as OTC drugs (3759, 24.5%) or obtained from other sources (2042, 14.0%). Drugs acting on the respiratory system (R00, 32.1%) were most frequently used, accounting for one-third of all self-medications. They were followed by drugs affecting the alimentary tract and metabolism (A00, 21.6%), skin (D00, 14.2%), nervous system (N00, 11.3%) and the musculoskeletal system (M00, 6.5%), as well as homoeopathic preparations (Z00, 8.6%). In contrast, all the other medication classes except for V00 (various, 2.3%) were used much less frequently with a percentage of <1% (Figure 1). Stratified analysis showed that OTC drugs differed from OS drugs. A00 drugs were more likely to be bought as OTC drugs, whereas N00 and M00 drugs were more frequently obtained from other sources (Figure 1). The most frequently mentioned indication for all self-medications was prophylactic measures (17.1%), followed by acute rhinopharyngitis (16.7%) and other common-cold symptoms such as cough (12.7%), sore throat (3.3%) and fever (2.9%) (data not shown in Figure 1). Headache was also one of the most frequently mentioned indications (7.2%). In addition, most self-medications were used for a short period within 1 week, particularly OS drugs (OS drugs 88.5% vs. OTC drugs 71.4%, P < 0.001, overall 77.6%, data not shown).
Figure 1.
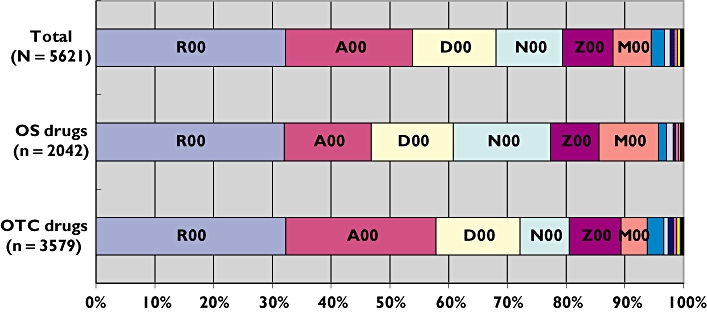
Vitamin preparations (A00) were more likely to be bought as over-the-counter (OTC) drugs, whereas medicines acting on the nervous system (N00) and musculoskeletal system (M00) (most of them are antipyretic analgesics) were more frequently obtained from other sources. R00 ( ); A00 (
); A00 ( ); D00 (
); D00 ( ); N00 (
); N00 ( ); Z00 (
); Z00 ( ); M00 (
); M00 ( ); V00 (
); V00 ( ); S00 (
); S00 ( ); L00 (
); L00 ( ); C00 (
); C00 ( ); B00 (
); B00 ( ); H00 (
); H00 ( ); G00 (
); G00 ( ); J00 (
); J00 ( ); P00 (
); P00 ( )
)
Prevalence of self-medication use by medication class and the most frequently used drugs
Table 2 lists the prevalence of last-week use of each therapeutic medication class, as well as the most frequently used medicines within specific medication classes. Five thousand six hundred and twenty-one self-medications were taken by 4294 children (weighted prevalence 25.2%; 17.0% for OTC drugs and 9.9% for OS drugs). The prevalence for the most frequently used medication classes was 8.1% for R00, 6.8% for A00, 4.4% for D00, 3.9% for N00 and 2.6% for Z00. The most frequently used subclasses were various vitamin preparations (A11) with a weighted prevalence of 4.7%, followed by CCMs (R05) with 4.4%, analgesics (N02) 3.7% (aspirin 1.3% and paracetamol 2.2%) and nasal preparations (R01) 2.8% (Table 2).
Table 2.
Last-week use of self-medications among 17 450 children in Germany; German Health Interview and Examination Survey for Children and Adolescents (KiGGS) 2003–2006
| ATC code | Medication/class | No. of drugs | No. of users | Prevalence % | 95% CI |
|---|---|---|---|---|---|
| A00 | Alimentary tract and metabolism | 1214 | 1120 | 6.8 | 6.2, 7.4 |
| A11 | Vitamin supplements | 804 | 773 | 4.7 | 4.2, 5.2 |
| A12 | Mineral supplements | 182 | 174 | 1.1 | 1.0, 1.3 |
| B00 | Blood and blood-forming organs | 28 | 27 | 0.2 | 0.1, 0.2 |
| C00 | Cardiovascular system | 32 | 32 | 0.2 | 0.1, 0.3 |
| D00 | Dermatologicals | 796 | 764 | 4.4 | 3.9, 4.9 |
| D03 | Preparations for treating wounds and ulcers | 280 | 276 | 1.6 | 1.3, 1.8 |
| D04 | Antipruritics, incl. antihistamines, anaesthetics, etc. | 140 | 139 | 0.8 | 0.6, 1.1 |
| G00 | Genitourinary system and sex hormones | 7 | 8 | 0.0 | 0.0, 0.1 |
| H00 | Systemic hormonal preparations, excluding sex hormones and insulins | 10 | 10 | 0.1 | 0.0, 0.1 |
| J00 | Anti-infectives for systemic use | 7 | 6 | 0.0 | 0.0, 0.1 |
| L00 | Antineoplastic and immunomodulating agents | 38 | 38 | 0.2 | 0.1, 0.3 |
| M00 | Musculoskeletal system | 365 | 358 | 2.2 | 1.9, 2.6 |
| M02 | Topical products for joint and muscular pain | 234 | 230 | 1.5 | 1.2, 1.7 |
| M01 | Anti-inflammatory and antirheumatic products | 120 | 120 | 0.7 | 0.6, 0.9 |
| N00 | Nervous system | 635 | 621 | 3.9 | 3.5, 4.3 |
| N02 | Analgesics | 602 | 590 | 3.7 | 3.3, 4.1 |
| N02BA01/51 | Aspirin | 189 | 188 | 1.3 | 1.1, 1.5 |
| N02BE01/51 | Paracetamol | 371 | 369 | 2.2 | 1.9, 2.5 |
| P00 | Antiparasitic products, insecticides and repellents | 7 | 7 | 0.0 | 0.0, 0.1 |
| R00 | Respiratory system | 1807 | 1440 | 8.1 | 7.3, 8.9 |
| R05 | Cough and cold medications | 838 | 775 | 4.4 | 3.9, 5.0 |
| R01 | Nasal preparations | 500 | 484 | 2.8 | 2.4, 3.2 |
| R04 | Breast ointments | 290 | 286 | 1.4 | 1.2, 1.6 |
| S00 | Sensory organs | 52 | 52 | 0.3 | 0.2, 0.4 |
| V00 | Various | 128 | 126 | 0.7 | 0.6, 0.8 |
| Z00 | Homoeopathics | 483 | 409 | 2.6 | 2.2, 3.0 |
| Unclassified | 12 | ||||
| Drugs bought over the counter | 3579 | 2891 | 17.0 | 16.0, 18.0 | |
| Drugs obtained from other sources | 2042 | 1679 | 9.9 | 8.6, 11.4 | |
| Overall self-medication | 5621 | 4294 | 25.2 | 23.8, 26.7 | |
All percentages are weighted according to the German national child population aged 0–17 years.
Multiple medicine use
Of the 4294 children on self-medication, 1309 (30.4%) used prescription medicines concomitantly, 1001 (23.6%) used two or more self-medications simultaneously (ranging from two to seven medicines) (Figure 2). The prevalence of multiple medicine use was 5.9% (95% CI 5.3, 6.6) for two or more self-medications, 7.4% (6.8, 8.1) for one self-medication plus at least one prescription medicine and 11.5% (10.6, 12.5) for overall (Figure 2). Use of two or more self-medications was associated with children residing in the former West Germany (OR 1.35, 95% CI 1.07, 1.71), children with no immigration background (3.05; 2.16, 4.29), with a poor health status (1.98; 1.53, 2.57) and whose mothers had a middle to higher educational level (1.58; 1.21, 2.06). The same was true when use of prescription medicine was considered (data not shown).
Figure 2.
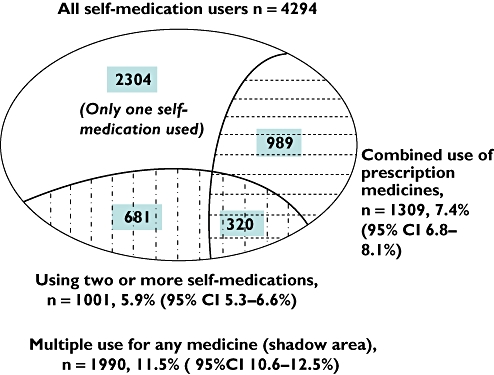
Multiple medicine use among children and adolescents on self-medication in Germany, KiGGS 2003–2006
Table 3 lists the prevalence rates of the five most frequently used medication classes and the top 10 subclasses stratified by age and gender. Together with homoeopathic preparations, the top five medication classes and the top 10 subclasses accounted for 94.3% and 80.0% of all self-medications, respectively. Overall, girls showed a significantly higher level of self-medication use (26.0% vs. 24.4%, P < 0.05), particularly in medication classes N00 (mainly N02 analgesics) and D00 (mainly D03 preparations for treating wounds and ulcers, and D04 antipruritics), but used less A00 than boys. Among adolescents aged 11–17 years, boys used significantly more vitamin (A11) and mineral supplements (A12) than girls, whereas girls used significantly more analgesics (N02, both aspirin and paracetamol) than boys. Girls aged 3–13 years used significantly more skin products (D00) before puberty than boys, and girls aged 14–17 years used significantly more musculoskeletal system drugs (M00, mainly M01) during puberty than boys. Overall use of aspirin in children <12 years old was 0.3%, with no difference between boys and girls (data not shown in Table 3). Girls appeared more likely to obtain medicines from other sources than boys (10.4% vs. 9.4%, P < 0.05). Overall, CCM use was substantial, particularly among boys and girls aged <6 years (4.3% and 4.5% for the age group 0–2 years, 7.4% and 7.2% for the age group 3–6 years, respectively; Table 3).
Table 3.
Prevalence of the most frequently used self-medications among children in Germany, stratified by gender and age; German Health Interview and Examination Survey for Children and Adolescents (KiGGS) 2003–2006
| Total | 0–2 | 3–6 | 7–10 | 11–13 | 14–17 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | ||
| Rank | n= 8880 | n= 8570 | n= 1397 | n= 1373 | n= 1925 | n= 1907 | n= 2103 | n= 2004 | n= 1572 | n= 1468 | n= 1883 | n= 1818 | |
| Most frequently used medication classes | |||||||||||||
| 1 | R00 Respiratory system | 7.8 | 8.4 | 10.0 | 8.7 | 11.7 | 11.9 | 7.4 | 7.8 | 5.5** | 7.9 | 5.4 | 6.2 |
| 2 | A00 Alimentary tract and metabolism | 7.8*** | 5.7 | 4.6 | 4.1 | 7.4 | 5.4 | 7.6 | 6.5 | 8.8** | 5.8 | 9.2*** | 6.1 |
| 3 | D00 Dermatologicals | 3.7*** | 5.0 | 5.3 | 5.5 | 3.7** | 5.4 | 4.1** | 6.3 | 3.1* | 4.6 | 3.0 | 3.7 |
| 4 | N00 Nervous system | 3.2*** | 4.6 | 2.2 | 2.8 | 1.5 | 1.3 | 2.5 | 1.6 | 3.5** | 5.6 | 5.6*** | 9.9 |
| 5 | M00 Musculoskeletal system | 2.0 | 2.4 | 0.7 | 0.3 | 1.1 | 0.9 | 2.0 | 1.7 | 3.2 | 2.7 | 2.7*** | 5.1 |
| 6 | Z00 Homoeopathics | 2.5 | 2.7 | 3.1 | 3.5 | 3.6 | 3.7 | 3.1 | 2.9 | 1.6 | 2.0 | 1.3 | 1.7 |
| Most frequently used subclasses | |||||||||||||
| 1 | A11 Vitamin supplements | 5.2*** | 4.1 | 1.5 | 2.0 | 5.8 | 4.5 | 5.6 | 4.9 | 6.4** | 4.2 | 5.7* | 4.2 |
| 2 | R05 Cough and cold medications | 4.3 | 4.5 | 4.3 | 4.5 | 7.4 | 7.2 | 4.1 | 4.5 | 3.3 | 3.9 | 2.5 | 2.9 |
| 3 | N02 Analgesics | 3.0*** | 4.4 | 2.0 | 2.6 | 1.4 | 1.2 | 2.1 | 1.5 | 3.3* | 5.1 | 5.4*** | 9.8 |
| -N02BA01/51, aspirin | 1.0*** | 1.6 | 0.0 | 0.2 | 0.0 | 0.1 | 0.6 | 0.3 | 1.2 | 1.6 | 2.4*** | 4.6 | |
| -N02BE01/51, paracetamol | 1.9*** | 2.5 | 2.0 | 2.3 | 1.4 | 1.0 | 1.4 | 1.2 | 1.9* | 3.4 | 2.6** | 4.4 | |
| 4 | R01 Nasal preparations | 2.5* | 3.1 | 4.2 | 3.7 | 3.4 | 4.4 | 2.4 | 2.7 | 1.7 | 2.2 | 1.5** | 2.6 |
| 5 | R04 Breast ointments | 1.4 | 1.3 | 2.9 | 2.2 | 2.4 | 2.3 | 1.1 | 1.1 | 0.8 | 0.8 | 0.5 | 0.7 |
| 6 | D03 Preparations for treating wounds and ulcers | 1.3** | 1.8 | 2.5 | 2.8 | 1.4 | 2.1 | 1.3* | 2.2 | 0.9 | 1.4 | 0.9 | 1.2 |
| 7 | M02 Topical products for joint and muscular pain | 1.5 | 1.4 | 0.2 | 0.1 | 0.5 | 0.7 | 1.8 | 1.1 | 2.3 | 2.0 | 2.3 | 2.4 |
| 8 | A12 Mineral supplements | 1.5*** | 0.7 | 0.1 | 0.1 | 0.6 | 0.4 | 0.9 | 0.8 | 2.3*** | 0.6 | 3.0*** | 1.4 |
| 9 | D04 Antipruritics, incl. antihistamines, anaesthetics, etc. | 0.7* | 0.9 | 0.3 | 0.1 | 0.9 | 1.2 | 0.9** | 2.0 | 0.6 | 0.8 | 0.5 | 0.4 |
| 10 | M01 Anti-inflammatory and antirheumatic products | 0.5*** | 1.0 | 0.6 | 0.3 | 0.6 | 0.2 | 0.2 | 0.5 | 0.8 | 0.7 | 0.4*** | 2.6 |
| OTC drugs | 16.5 | 17.5 | 17.5 | 17.6 | 17.0 | 16.2 | 16.0 | 16.1 | 15.8 | 16.0 | 16.7*** | 20.5 | |
| OS drugs | 9.4* | 10.4 | 7.9 | 7.3 | 11.1 | 10.9 | 9.5 | 9.5 | 8.7* | 11.6 | 9.1** | 11.7 | |
| Total self-medications | 24.4* | 26.0 | 24.1 | 22.9 | 26.0 | 25.2 | 24.1 | 24.4 | 23.2*** | 26.1 | 24.4*** | 29.6 | |
Data presented in % are weighted according to the German national child population aged 0–17 years.
P < 0.05,
P < 0.01,
P < 0.001 for comparison between boys and girls within the same age group (χ2 test).
Factors associated with self-medication use
Multivariable regression analysis shows that overall use of self-medication was positively associated with the 14–17 years age group, children with no immigration background, with a poor health status, from families with higher household income, and whose mothers had a middle to higher educational level (Table 4). The same factors (except for the 14–17 years age group) were also found for the use of OTC drugs. Children aged 0–2 years were found to be significantly less likely to be associated with the use of OS drugs, whereas children from families with a higher household income and whose mothers had a middle to higher educational level were significantly more likely to be associated with the use of OS drugs (Table 4).
Table 4.
Factors associated with use of self-medications among children in Germany; German Health Interview and Examination Survey for Children and Adolescents (KiGGS) 2003–2006
| Self-medication overall | OTC drugs | OS drugs | |
|---|---|---|---|
| Sex | |||
| Boys | Reference | Reference | Reference |
| Girls | 1.07 (0.99, 1.16) | 1.06 (0.97, 1.16) | 1.10 (0.98, 1.23) |
| Age group, years | |||
| 0–2 | Reference | Reference | Reference |
| 3–6 | 1.08 (0.95, 1.24) | 0.92 (0.79, 1.07) | 1.38 (1.14, 1.67) |
| 7–10 | 1.00 (0.87, 1.14) | 0.87 (0.74, 1.02) | 1.20 (0.97, 1.49) |
| 11–13 | 1.06 (0.92, 1.22) | 0.90 (0.77, 1.06) | 1.29 (1.04, 1.61) |
| 14–17 | 1.16 (1.00, 1.34) | 1.09 (0.93, 1.28) | 1.28 (1.02, 1.62) |
| Region | |||
| East | Reference | Reference | Reference |
| West | 1.16 (0.97, 1.38) | 1.15 (0.96, 1.38) | 1.18 (0.81, 1.71) |
| Urbanicity | |||
| Village | Reference | Reference | Reference |
| Small city | 1.11 (0.87, 1.41) | 1.11 (0.86, 1.45) | 1.09 (0.72, 1.66) |
| Medium-sized city | 1.34 (0.91, 1.42) | 1.28 (1.00, 1.65) | 0.89 (0.59, 1.33) |
| Large city | 1.18 (0.93, 1.50) | 1.14 (0.86, 1.51) | 1.15 (0.76, 1.74) |
| Migrant background | |||
| Yes | Reference | Reference | Reference |
| No | 1.55 (1.33, 1.80) | 1.88 (1.56, 2.27) | 1.16 (0.96, 1.40) |
| Health status | |||
| Excellent | Reference | Reference | Reference |
| Good | 1.16 (1.05, 1.27) | 1.18 (1.06, 1.31) | 1.08 (0.94, 1.25) |
| Satisfactory/poor | 1.29 (1.10, 1.52) | 1.34 (1.11, 1.62) | 1.15 (0.89, 1.48) |
| Household income (€) | |||
| <1500 | Reference | Reference | Reference |
| 1500–2250 | 1.14 (0.91, 1.17) | 1.07 (0.92, 1.25) | 0.95 (0.79, 1.16) |
| 2250–3000 | 1.13 (0.99, 1.29) | 1.19 (1.02, 1.39) | 0.99 (0.80, 1.21) |
| ≥3000 | 1.23 (1.06, 1.42) | 1.20 (1.00, 1.43) | 1.27 (1.04, 1.56) |
| Maternal educational level | |||
| Primary | Reference | Reference | Reference |
| Middle | 1.20 (1.06, 1.36) | 1.26 (1.08, 1.48) | 1.19 (0.91, 1.37) |
| Higher | 1.37 (1.19, 1.57) | 1.40 (1.17, 1.67) | 1.30 (1.06, 1.58) |
| Others | 1.01 (0.80, 1.27) | 1.10 (0.84, 1.44) | 0.85 (0.60, 1.21) |
| Paternal educational level | |||
| Primary | Reference | Reference | Reference |
| Middle | 1.13 (1.00, 1.26) | 1.13 (0.99, 1.29) | 1.01 (0.85, 1.20) |
| Higher | 1.09 (0.96, 1.25) | 1.15 (0.99, 1.33) | 0.96 (0.79, 1.15) |
| Others | 0.93 (0.76, 1.15) | 0.82 (0.64, 1.04) | 1.08 (0.81, 1.45) |
Data are presented as an odds ratio (95% confidence interval), Odds ratios and 95% confidence intervals were obtained from multivariate regression models with self-medication use, overall and in subgroup OTC and OS drugs, as dependent variable and all other variables shown in the table as independent variables. Figures in body text mean statistically significant.
Discussion
In the present study we found that 25.2% of children aged 0–17 years had used self-medication in the previous week (17.0% used OTC drugs and 9.9% OS drugs). Self-medication by children accounted for 38.5% of total drug use. These drugs included all medication classes, but clustered among drugs acting on the respiratory system (R00, 32.1%), alimentary tract and metabolism (A00, 21.6%), skin (D00, 14.2%) and nervous system (N00, 11.3%), as well as homoeopathic preparations (Z00, 8.6%). Vitamin preparations were most frequently used with a weighted prevalence of 4.7%, followed by CCMs with 4.4% and analgesics 3.7%. The most frequently mentioned indications for self-medication were prophylactic measures (17.1%), followed by acute rhinopharyngitis (16.7%) and other common-cold symptoms such as cough (12.7%) and sore throat (3.3%). Use of self-medication was closely related to older adolescents, children with a poor health status, with no immigration background, from families with a higher household income, and children's mothers who had a middle to higher educational level.
These findings confirmed that the use of self-medications was widespread among children and consistent with results of previous studies [1–3]. The majority of self-medications were vitamin and mineral supplements or CCMs, which were mostly used either for prophylactic purposes or for treating rhinopharyngitis and various other symptoms of the common cold. Furthermore, use of self-medication was positively associated with socioeconomic status and the educational level of the children's mothers [1, 2].
Medicines use among children varied greatly in terms of type of medicines and extent of use. Furthermore, epidemiological data on self-medication use by children are sparse worldwide, making it difficult to compare studies. Differences in study design, sample selection and the measurement timeframe in particular can influence study results. An earlier survey investigated medicines use among approximately 8500 pupils in the UK and found that approximately 20% of boys and girls aged between 11 and 15 years had used a nonprescribed painkiller in any one week [12]. Among girls aged 14–15 years, the proportion was as high as two-fifths [12]. These prevalence rates are much higher than the results on analgesics use among children aged 11–17 years in our study (Table 3). This study also reported a much higher use of nonprescription CCMs and cold-sore treatments (both approximately 20%) [12] than our results. The high level of use of these drugs in this study may be attributed to differences in methodology. Medicine use in the UK study [12] was ticked on questionnaires by the pupils themselves. It therefore seems unavoidable that pupils influenced each other, misclassified drugs due to a lack of knowledge of medicines, and perhaps entered multiple ticks for the same medicine. For example, a pain killer might also be ticked as a cold-sore treatment. It may also be difficult for pupils to distinguish a CCM from a cold-sore treatment. Furthermore, prescription drugs did not look very different from nonprescription drugs [12]. All these factors may result in much higher use-prevalence rates than our findings. In a more recently published US study among 4267 children aged <18 years, Vernacchio et al. reported that approximately 10% of children had used CCMs in a given week during the period from 1999 to 2006 [18]– also higher than the figure found in our study (Table 3). The differences between the two studies may be due to the definition of CCM. In our study CCMs were exclusively drugs of the ATC class R05, whereas in the US study CCMs included drugs from other medication classes such as decongestants and antihistamines [18], which belong to drugs with the ATC codes R01 and R06, respectively. Bearing in mind that the vast majority of medications in R00 are used for treating cold and coughs in our study, the overall prevalence of R00 in our study (8.1%) is roughly comparable to that of the US study [18].
Despite the differences, CCM use in the present study is substantial, particularly among boys and girls <6 years old (Table 3). This raises several concerns. First, the use of CCMs by young children does not have any clinical benefit. This has been evidenced by randomized clinical trials, which show that the clinical effects of CCMs in children <12 years old are no greater than placebo [9, 19]. Second, the use of CCMs by young children can have serious adverse effects. In the USA, the most common age group involved in emergencies caused by adverse drug events involving CCMs was children between the ages of 2 and 5 years [6]. Several baby deaths associated with CCM use have been reported [7–9]. No clinical benefits, but potential risks: this is why experts and health authorities consistently warn against the use of CCMs in young children [9, 10, 20]. CCM use declined in the USA between 1999 and 2006 [18]. Future developments in Germany should be further monitored. The high level of CCM use in young children suggests the need for an education programme for parents in Germany.
Self-medication use of vitamin and mineral tablets seems quite constant in Germany. A previous investigation of 3-day dietary records conducted among 931 German children aged 2–18 years and including the use of nonprescription vitamin and mineral supplements found that 4.5 and 2.4%, respectively, of the study subjects had used vitamins and minerals [21]. Our finding for last-week use of the two substances was 4.7% and 1.1% of children aged 0–17 years, respectively. In the UK study [12], last-week use of vitamins was also largely consistent with our findings. Yet, in a US investigation of vitamin and mineral supplement use among >10 000 children aged 2–17 years, Shaikh et al. reported that one-third (34%) of children had taken a vitamin/mineral supplement in the previous month [22], much higher than the figures found in Germany. Interestingly, contrary to previous studies indicating no gender differences [21], our results showed that boys used significantly more vitamin preparations and mineral supplements than girls during puberty. In the US study [22], it was found that those children who in fact do not need supplements of vitamins and minerals were more likely to take them [22], raising concerns of the rational use of vitamins among children [23]. Whereas hydrosoluble vitamins can be metabolized quickly, fat-soluble vitamins can accumulate in the body, causing adverse effects [24]. Recent clinical trials on the use of vitamin supplements for disease prevention in adults have shown no positive results [25–28]. The effects of vitamin supplements on the development and health of children and adolescents have rarely been reported up to now.
Chronic pain among children has become an important public health problem in recent years. In a Danish study of pupils aged 11, 13 and 15 years, 40.7% and 13.9% of children, respectively, reported using medicines for headache and stomach ache during the previous month, particularly 13- and 15-year-old girls [29, 30]. In a regional study conducted in Germany among 749 children and adolescents, 622 (83%) had experienced pain during the preceding 3 months [31]. This finding was confirmed by KiGGS results of 64.5% and 77.6%, respectively, for children aged 3–10 and 11–17 years [32]. The high prevalence of chronic pain among children in Germany suggests a high potential use of analgesics. An international survey of self-reported medicine use among adolescents in 28 countries including Germany revealed that, overall, 24.5% of German boys and 33.3% of German girls reported having used medicines for headache in the previous month (internationally the figures ranged from 21.1% to 49.9% for boys and from 28.3% to 65.9% for girls) [33]. The numbers for stomach ache were 11.9% and 14.5%, respectively, for German boys and girls (internationally it ranged from 5.1% to 26.9% for boys and from 10.3% to 43.0% for girls) [33]. Yet our results showed that only 3.7% reported last-week use of self-medicated analgesics. This is because prescribed analgesics were not considered. Higher use of analgesics by girls than boys >10 years old, whether self-medication only or overall, was consistently observed both in our study and in many others [12, 31, 33–35]. Menstruation-related disorders are regarded as one of reasons for this difference.
Like previous studies, we found that self-medication use was associated with socioeconomic factors, such as the mothers' educational level, household income and immigration background. The higher the socioeconomic status of the children's family, or the higher the educational level of the children's mother, the more OTC medications the children were likely to receive [1, 2, 36]. Mothers usually spend more time looking after their children than fathers, and well-educated mothers often believe they have enough medical knowledge to give their children medications. Even though the costs of all drugs, both prescription and OTC, are covered by health insurance in Germany for children <12 years old, age-specified prevalence rates did not show a higher prevalence rate in this age group (data not shown). Self-medications bought from pharmacy stores or supermarkets are paid for by parents, and families with an immigration background in Germany are often associated with a lower educational level, a lower household income and hence a lower socioeconomic status. It is no surprise therefore that families with a higher household income and no immigration background were associated with self-medication use. Furthermore, various vitamin preparations, mineral supplements and homoeopathic preparations accounted for a substantial proportion of all self-medications in the present study. The high proportion of such drugs may reflect an underlying desire among parents with a higher socioeconomic status for greater self-care and a need for opportunities to address the concerns of their children themselves. Our previous study indicated that the use of such medicines was closely associated with a higher socioeconomic status and higher educational levels among mothers [37]. It is no wonder that use of two or more self-medications was also largely associated with children from families with a higher socioeconomic status.
The main strength of our study is that we used a large, nationally representative sample of non-institutionalized children. The weighted results can be generalized to the entire German child population. Actual drug use was verified by asking the children's parents to bring the medication containers or product labels to the study sites. Recall bias was also minimized by measuring drug use over the previous week. However, use of self-medication does not reflect disease prevalence or therapy, since prescription drug use was not included in the present study. For example, last-week analgesic use in our study was about 4.0%, much lower than the overall use of analgesics found in other studies [29, 30, 33]. Furthermore, our study did not separate self-medications taken by teenagers themselves from those given to them by their parents and did not collect information concerning teenagers sharing medicines with each other, making it impossible for us to explore the possible motives of self-medication.
In summary, self-medication use is highly prevalent among children and adolescents in Germany and associated with children from families with a higher socioeconomic status. Self-medications cover drugs of all therapeutic classes, but cluster among vitamin and mineral supplements, CCMs and non-addictive analgesics, most of which are used for a short period, either for disease prevention or to treat acute rhinopharyngitis and other common-cold symptoms. The use of CCMs and aspirin in younger children suggests inappropriate drug use and potential risks. These should be further monitored and warrant an education programme targeting parents in Germany.
Competing interests
None declared.
The German Health Interview and Examination Survey for Children and Adolescents (KiGGS) was funded by the German Federal Ministry of Health, the Ministry of Education and Research, and the Robert Koch Institute.
REFERENCES
- 1.Bi P, Tong S, Parton KA. Family self-medication and antibiotics abuse for children and juveniles in a Chinese city. Soc Sci Med. 2000;50:1445–50. doi: 10.1016/s0277-9536(99)00304-4. [DOI] [PubMed] [Google Scholar]
- 2.Kogan MD, Pappas G, Yu SM, Kotelchuck M. Over-the-counter medication use among US preschool-age children. JAMA. 1994;272:1025–30. [PubMed] [Google Scholar]
- 3.Rylance GW, Woods CG, Cullen RE, Rylance ME. Use of drugs by children. BMJ. 1988;297:445–7. doi: 10.1136/bmj.297.6646.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Costello I, Wong IC, Nunn AJ. A literature review to identify interventions to improve the use of medicines in children. Child Care Health Dev. 2004;30:647–65. doi: 10.1111/j.1365-2214.2004.00478.x. [DOI] [PubMed] [Google Scholar]
- 5.Macdonald S. Aspirin use to be banned in under 16 year olds. BMJ. 2002;325:988. doi: 10.1136/bmj.325.7371.988/c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaefer MK, Shehab N, Cohen AL, Budnitz DS. Adverse events from cough and cold medications in children. Pediatrics. 2008;121:783–7. doi: 10.1542/peds.2007-3638. [DOI] [PubMed] [Google Scholar]
- 7.Rimsza ME, Newberry S. Unexpected infant deaths associated with use of cough and cold medications. Pediatrics. 2008;122:e318–22. doi: 10.1542/peds.2007-3813. [DOI] [PubMed] [Google Scholar]
- 8.Wingert WE, Mundy LA, Collins GL, Chmara ES. Possible role of pseudoephedrine and other over-the-counter cold medications in the deaths of very young children. J Forensic Sci. 2007;52:487–90. doi: 10.1111/j.1556-4029.2007.00391.x. [DOI] [PubMed] [Google Scholar]
- 9.Sharfstein JM, North M, Serwint JR. Over the counter but no longer under the radar – pediatric cough and cold medications. N Engl J Med. 2007;357:2321–4. doi: 10.1056/NEJMp0707400. [DOI] [PubMed] [Google Scholar]
- 10.Press release of Medicines and Healthcare products Regulatory Agency (MHRA): Better medicines for children's coughs and colds. Available at http://wwwmhragovuk/NewsCentre/Pressreleases/CON038902 (last accessed 6 May 2009.
- 11.Slack-Smith LM, Read AW, Stanley FJ. The use of medication in children attending childcare in Western Australia. J Paediatr Child Health. 1998;34:183–7. doi: 10.1046/j.1440-1754.1998.00196.x. [DOI] [PubMed] [Google Scholar]
- 12.Dengler R, Roberts H. Adolescents' use of prescribed drugs and over-the-counter preparations. J Public Health Med. 1996;18:437–42. doi: 10.1093/oxfordjournals.pubmed.a024542. [DOI] [PubMed] [Google Scholar]
- 13.Knopf H. Arzneimittelanwendung bei Kindern und Jugendlichen. Erfassung und erste Ergebnisse beim Kinder- und Jugendgesundheitssurvey (KiGGS) [Medicine use in children and adolescents. Data collection and first results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50:863–70. doi: 10.1007/s00103-007-0249-z. [DOI] [PubMed] [Google Scholar]
- 14.Beitz R, Doren M, Knopf H, Melchert HU. Self-medication with over-the-counter (OTC) preparations in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2004;47:1043–50. doi: 10.1007/s00103-004-0923-3. [DOI] [PubMed] [Google Scholar]
- 15.Kurth BM, Kamtsiuris P, Hölling H, Schlaud M, Dölle R, Ellert U, Kahl H, Knopf H, Lange M, Mensink GB, Neuhauser H, Rosario AS, Scheidt-Nave C, Schenk L, Schlack R, Stolzenberg H, Thamm M, Thierfelder W, Wolf U. The challenge of comprehensively mapping children's health in a nation-wide health survey: design of the German KiGGS-Study. BMC Public Health. 2008;8:196. doi: 10.1186/1471-2458-8-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamtsiuris P, Lange M, Schaffrath RA. The German Health Interview and Examination Survey for Children and Adolescents (KiGGS): sample design, response and nonresponse analysis. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50:547–56. doi: 10.1007/s00103-007-0215-9. [DOI] [PubMed] [Google Scholar]
- 17.Schenk L, Ellert U, Neuhauser H. Children and adolescents in Germany with a migration background. Methodical aspects in the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50:590–9. doi: 10.1007/s00103-007-0220-z. [DOI] [PubMed] [Google Scholar]
- 18.Vernacchio L, Kelly JP, Kaufman DW, Mitchell AA. Cough and cold medication use by US children, 1999–2006: results from the Slone survey. Pediatrics. 2008;122:e323–9. doi: 10.1542/peds.2008-0498. [DOI] [PubMed] [Google Scholar]
- 19.Schroeder K, Fahey T. Systematic review of randomised controlled trials of over the counter cough medicines for acute cough in adults. BMJ. 2002;324:329. doi: 10.1136/bmj.324.7333.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abell S, Ey JL. Ask Dr. Sue: no more cough and cold medications for children. Clin Pediatr. 2008;47:316–8. doi: 10.1177/0009922807303549. [DOI] [PubMed] [Google Scholar]
- 21.Sichert-Hellert W, Kersting M. Vitamin and mineral supplements use in German children and adolescents between 1986 and 2003: results of the DONALD Study. Ann Nutr Metab. 2004;48:414–9. doi: 10.1159/000083574. [DOI] [PubMed] [Google Scholar]
- 22.Shaikh U, Byrd RS, Auinger P. Vitamin and mineral supplement use by children and adolescents in the 1999–2004 national health and nutrition examination survey: relationship with nutrition, food security, physical activity, and health care access. Arch Pediatr Adolesc Med. 2009;163:150–7. doi: 10.1001/archpediatrics.2008.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moreno MA, Furtner F, Rivara FP. Vitamin and mineral supplementation in children. Arch Pediatr Adolesc Med. 2009;163:192. doi: 10.1001/archpediatrics.2008.548. [DOI] [PubMed] [Google Scholar]
- 24.Krinsky NI. Human requirements for fat-soluble vitamins, and other things concerning these nutrients. Mol Aspects Med. 2003;24:317–24. doi: 10.1016/s0098-2997(03)00027-x. [DOI] [PubMed] [Google Scholar]
- 25.Lin J, Cook NR, Albert C, Zaharris E, Gaziano JM, Van Denburgh M, Buring JE, Manson JE. Vitamins C and E and beta carotene supplementation and cancer risk: a randomized controlled trial. J Natl Cancer Inst. 2009;101:14–23. doi: 10.1093/jnci/djn438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sesso HD, Buring JE, Christen WG, Kurth T, Belanger C, MacFadyen J, Bubes V, Manson JE, Glynn RJ, Gaziano JM. Vitamins E and C in the prevention of cardiovascular disease in men: the Physicians' Health Study II Randomized Controlled Trial. JAMA. 2008;300:2123–33. doi: 10.1001/jama.2008.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bjelakovic G, Nikolova D, Gluud LL, Simonetti RG, Gluud C. Mortality in randomized trials of antioxidant supplements for primary and secondary prevention: systematic review and meta-analysis. JAMA. 2007;297:842–57. doi: 10.1001/jama.297.8.842. [DOI] [PubMed] [Google Scholar]
- 28.Huang HY, Caballero B, Chang S, Alberg AJ, Semba RD, Schneyer CR, Wilson RF, Cheng TY, Vassy J, Prokopowicz G, Barnes GJ, II, Bass EB. The efficacy and safety of multivitamin and mineral supplement use to prevent cancer and chronic disease in adults: a systematic review for a National Institutes of Health State-of-the-Science Conference. Ann Intern Med. 2006;145:372–85. doi: 10.7326/0003-4819-145-5-200609050-00135. [DOI] [PubMed] [Google Scholar]
- 29.Holstein BE, Hansen EH, Due P. Social class variation in medicine use among adolescents. Eur J Public Health. 2004;14:49–52. doi: 10.1093/eurpub/14.1.49. [DOI] [PubMed] [Google Scholar]
- 30.Andersen A, Holstein BE, Hansen EH. Is medicine use in adolescence risk behavior? Cross-sectional survey of school-aged children from 11 to 15. J Adolesc Health. 2006;39:362–6. doi: 10.1016/j.jadohealth.2005.12.023. [DOI] [PubMed] [Google Scholar]
- 31.Roth-Isigkeit A, Thyen U, Stoven H, Schwarzenberger J, Schmucker P. Pain among children and adolescents: restrictions in daily living and triggering factors. Pediatrics. 2005;115:e152–62. doi: 10.1542/peds.2004-0682. [DOI] [PubMed] [Google Scholar]
- 32.Ellert U, Neuhauser H, Roth-Isigkeit A. Pain in children and adolescents in Germany: the prevalence and usage of medical services. Results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50:711–7. doi: 10.1007/s00103-007-0232-8. [DOI] [PubMed] [Google Scholar]
- 33.Hansen EH, Holstein BE, Due P, Currie CE. International survey of self-reported medicine use among adolescents. Ann Pharmacother. 2003;37:361–6. doi: 10.1345/aph.1C111. [DOI] [PubMed] [Google Scholar]
- 34.Holstein BE, Hansen EH, Due P, Almarsdottir AB. Self-reported medicine use among 11- to 15-year-old girls and boys in Denmark 1988–1998. Scand J Public Health. 2003;31:334–41. doi: 10.1080/14034940210165082. [DOI] [PubMed] [Google Scholar]
- 35.Holstein BE, Andersen A, Krolner R, Due P, Hansen EH. Young adolescents' use of medicine for headache: sources of supply, availability and accessibility at home. Pharmacoepidemiol Drug Saf. 2008;17:406–10. doi: 10.1002/pds.1563. [DOI] [PubMed] [Google Scholar]
- 36.Tobi H, Meijer WM, Tuinstra J, de Jong-van den Berg LT. Socio-economic differences in prescription and OTC drug use in Dutch adolescents. Pharm World Sci. 2003;25:203–6. doi: 10.1023/a:1025836704150. [DOI] [PubMed] [Google Scholar]
- 37.Du Y, Knopf H. Pediatric homoeopathy in Germany: results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Pharmacoepidemiol Drug Saf. 2009;18:370–9. doi: 10.1002/pds.1720. [DOI] [PubMed] [Google Scholar]


