Abstract
Cardiac myocytes have been shown to express constitutively endothelial nitric oxide synthase (eNOS) (nitric oxide synthase 3), the activation of which has been implicated in the regulation of myocyte L-type voltage-sensitive calcium channel current (ICa-L) and myocyte contractile responsiveness to parasympathetic nervous system signaling, although this implication remains controversial. Therefore, we examined the effect of the muscarinic cholinergic agonist carbachol (CCh) on ICa-L and contractile amplitude in isoproterenol (ISO)-prestimulated ventricular myocytes isolated from adult mice, designated eNOSnull mice, with targeted disruption of the eNOS gene. Although both eNOSnull and wild-type (WT) ventricular myocytes exhibited similar increases in ICa-L in response to ISO, there was no measurable suppression of ICa-L by CCh in cells from eNOSnull mice, in contrast to cells from WT mice. These results were reflected in the absence of an effect of CCh on the positive inotropic effect of ISO in eNOSnull myocytes. Also, unlike myocytes from WT animals, eNOSnull myocytes failed to exhibit an increase in cGMP content in response to CCh. Nevertheless, the pharmacologic nitric oxide donors 3-morpholino-sydnonimine and S-nitroso-acetyl-cystein increased cGMP generation and suppressed ISO-augmented ICa-L in eNOSnull cells, suggesting that the signal transduction pathway(s) downstream of eNOS remained intact. Of importance, activation of the acetylcholine-activated K+ channel by CCh was unaffected in atrial and ventricular eNOSnull myocytes. These results confirm the obligatory role of eNOS in coupling muscarinic receptor activation to cGMP-dependent control of ICa-L in cardiac myocytes.
The regulation of the beating rate and force of contraction of the heart by the autonomic nervous system has been one of the most intensively studied aspects of cardiovascular pharmacology. Recently, a number of studies have implicated an important role for nitric oxide (NO) generation in mediating some aspects of muscarinic cholinergic and adrenergic signaling, both in intact hearts and in isolated myocytes (1–12). NO, whether released by pharmacologic NO donors or generated by activation of endogenous NO synthases (NOS), has been shown to suppress the activation of voltage-sensitive Ca2+ current (ICa-L) by β-adrenergic agonists (7–12). Conversely, inhibition of NO generation within cardiac myocytes, including specialized pacemaker and conduction system cells, has been shown to blunt the negative inotropic and chronotropic effects of parasympathetic nerve stimulation in the mammalian heart in situ when infused with a β-adrenergic agonist (3–6).
The enzyme responsible for the generation of NO within cardiac myocytes is the NOS originally described in endothelial cells (i.e., eNOS or NOS3). eNOS is a Ca2+–calmodulin-activated enzyme that is localized in both myocytes and endothelial cells to specialized plasmalemmal microdomains termed caveolae (15, 16). A principal target of eNOS-generated NO is the soluble guanylyl cyclase (17–21). Indeed, agents that prevent cGMP generation have been shown to attenuate significantly the inhibitory effect of NO on ICa-L (8–10, 17).
Nevertheless, the importance of endogenous NO generation in the regulation of cardiac ICa-L, particularly in response to muscarinic cholinergic agonists, remains controversial (see refs. 16, 21, and 22 for reviews). In frog ventricular myocytes, for example, NOS inhibitors failed to modify cholinergic inhibition of ICa-L (23). Inhibition of a cAMP-stimulated chloride current by cholinergic agonists in guinea pig ventricular myocytes also was unaffected by NOS inhibitors (24). This controversy prompted us to examine the control of ICa-L by muscarinic cholinergic signaling in atrial and ventricular myocytes of mice with targeted disruption of eNOS (eNOSnull). We found that muscarinic cholinergic agonists significantly increased intracellular cGMP levels in wild-type (WT) but not eNOSnull myocytes and that cholinergic inhibition of β-adrenergic agonist-stimulated ICa-L and myocyte contractile amplitude both were impaired in myocytes lacking functional eNOS.
METHODS
Cell Isolation.
Calcium-tolerant ventricular and atrial myocytes were isolated from mice as described (25). eNOSnull founder mice were backcrossed into their C57B/6 and 129SvEv backgrounds from which both eNOSnull and WT animals were obtained. In brief, hearts obtained from mice with targeted disruption of eNOS (eNOSnull) (26) or from age-matched WT animals were excised under ether anesthesia and retrogradely perfused with Hepes-buffered Tyrode’s solution for 5 min, followed by perfusion with a nominally Ca2+-free Hepes-buffered Tyrode’s solution for 5–10 min and an additional 10 min with the Ca2+-free Hepes-buffered Tyrode’s solution containing 0.05% collagenase (Worthington). The great vessels, atria, and valvular tissues were removed, and ventricular muscle was gently minced in the same enzyme-containing solution plus trypsin (0.02 mg/ml; Sigma). Myocytes then were dissociated and sedimented in 2% BSA. Cells were plated onto laminin-coated glass coverslips and were transferred to perfusion chambers mounted on the stage of an inverted microscope for measurements of whole-cell current and single-cell shortening.
Electrophysiological Experiments.
Whole-cell ICa-L was measured by using the membrane-ruptured patch configuration (27). To facilitate ICa-L measurement, K+ was replaced by Cs+ on either side of the membrane. The pipette solution contained 90 mM aspartic acid, 30 mM CsCl, 110 mM CsOH, 10 mM EGTA, 3 mM ATP–Mg2+, 3 mM Na2–phosphocreatine, 5 mM Hepes, and 1 mM CaCl2 (pH 7.2) when it was titrated with CsOH. pCa2+ was calculated to be in the range of 7.4–7.5 (28). When measuring acetylcholine-sensitive K+ current, the pipette solution contained 110 mM potassium aspartate, 30 mM KCl, 10 mM EGTA, 1 mM CaCl2, 3 mM ATP–K, 2 mM ATP–Mg, 3 mM Na2–phosphocreatine, and 5 mM Hepes (pH 7.2) when it was titrated with KOH. Cells were perfused with Hepes-buffered solution containing 145 mM NaCl, 5.4 mM CsCl, 1.0 mM MgCl2, 1.0 mM Na2HPO4, 5.0 mM Hepes, 1 mM CaCl2, and 10 mM glucose; pH was adjusted to 7.4 with CsOH. A liquid junction potential of −10 mV was measured and was corrected electronically. The electrode direct current resistance was between 1 and 3 MΩ. Experiments were performed at 32.5°C. The temperature of the perfusion chamber was controlled by a Biowarmer MT-1 (Narishige, Japan). Holding potential was −80 mV. To inactivate the fast inward Na+ current and the T-type Ca2+ current, a prepulse of 200-ms duration to −40 mV was applied first, and ICa-L was activated by a further depolarization to 0 mV for 200 ms. ICa-L was measured as the difference between the steady-state current level and the peak inward current at 0 mV. Data acquisition and storage were performed by using [smcap]pclamp software (version 5.51, Axon Instruments, Foster City, CA) interfaced with a computer and analyzed off-line. Membrane currents were digitized at 2.5 kHz. The recording chamber volume was 0.5 ml, and a constant flow rate of 1.5 ml/min was used to superfuse the cells. A solenoid, driver-controlled, fast perfusion apparatus was used to change among solutions containing various test agents.
Measurement of Myocyte Contractility.
Myocyte contractile amplitude was measured as described (12) by using a video motion detector (Crescent Electronics, Sandy, UT). Cells were field-stimulated at 1.5× the threshold at 1–3 Hz with a stimulator (Grass Instruments, Quincy, MA) that generates rectangular waves of 3-ms duration.
cGMP Assay.
Basal and carbachol (CCh)-stimulated, intracellular cGMP production were determined by cGMP enzyme immunoassay. In brief, murine ventricular myocytes were used 2–3 h after plating. After removing the medium, cells were washed twice with Locke’s buffer (154 mM NaCl/5.6 mM KCl/2.0 mM CaCl2/1.0 mM MgCl2/3.6 mM NaHCO3/5.6 mM glucose/10 mM Hepes, pH 7.4). Cells then were equilibrated at 37°C for 30 min in Locke’s buffer containing 1 mM 3-isobutyl-1-methylxanthine and 1 mM L-arginine or L-nitroarginine. Superoxide dismutase (100 units/ml) was added after 25 min of equilibration. Myocytes were treated with 5 μM CCh or 10 μM 3-morpholino-sydnonimine (SIN-1) for 3 min at 37°C. The medium was removed rapidly, and the reaction was terminated with ice-cold 0.1 M HCl. After 20 min of incubation on ice, the cells were scraped, and the extracts were collected, were neutralized by NaOH, and were buffered with 2.5 M sodium acetate to pH 5.8. After centrifugation for 5 min at 14,000 × g, cGMP levels in the supernatant were determined by using a kit according to the manufacturer’s instructions (Cayman Chemicals, Ann Arbor, MI). Each experiment was performed in triplicate, and the results were calibrated against standard curves and were expressed as picomole per mg protein.
Reagents.
Collagenase and DNase were purchased from Worthington. Trypsin, hyaluronidase, isoproterenol (ISO), carbamylcholine chloride, phenylmethanesulfonyl fluoride, and pepstatin were purchased from Sigma. NG-monomoethyl-L-arginine monoacetate was purchased from Alexis Biochemicals (San Diego).
Statistics.
Statistical analyses were done by using Student’s t test or ANOVA followed by the Bonferroni modification where appropriate.
RESULTS
To determine whether eNOS-dependent signaling pathways played a role in muscarinic cholinergic regulation of cardiac function, we first compared the inotropic response of ventricular myocytes isolated from either WT or eNOSnull mice to the β-adrenergic agonist ISO alone and in combination with the cholinergic agonist CCh. The absence of a Ca2+–calmodulin-regulated NOS was verified by the lack of detectable eNOS in ventricular muscle and isolated murine myocytes from eNOSnull animals by Western blot analysis, as has been reported (26); no neuronel NOS protein could be detected by immunoprecipitation in either WT or eNOSnull myocytes (data not shown).
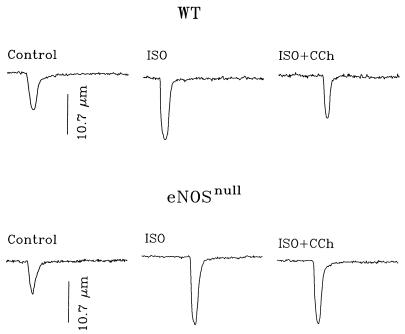
Representative examples of WT and eNOSnull myocyte contractile amplitude in response to ISO and CCh are shown in Fig. 1. As expected, in WT cells, myocyte contractility was enhanced significantly by ISO (10 nM) and could be inhibited by CCh (10 μM), a phenomenon termed “accentuated antagonism.” ISO increased contractile amplitude to about the same extent in an eNOSnull cell, but subsequent application of CCh resulted in only minimal diminution of the effect of ISO. Data for a number of myocytes obtained from WT and eNOSnull animals are shown in Table 1, in which contractile amplitude is expressed as percentage changes in cell length. In 10 cells from four WT mice, myocyte shortening was increased by ISO from 9.2 to 17.5% of resting cell length, a response that could be diminished to 12.8% by CCh (P < 0.01). ISO-stimulated myocyte shortening was not significantly different in eNOSnull myocytes (n = 10) isolated from four age-matched animals from the appropriate (C57B/6 × 129 SvEv) background strains. However, unlike in WT cells, subsequent application of CCh did not result in a significant reduction in the amplitude of myocyte shortening (P > 0.1; Table 1).
Figure 1.
Absence of muscarinic agonist suppression of β-adrenergic, agonist-mediated, increased contractile amplitude in myocytes from eNOSnull mice. The effects of ISO (10 nM) and CCh (10 μM) on amplitude of shortening of single ventricular myocytes from WT and eNOSnull mice are illustrated. Myocyte contraction was elicited by field stimulation (1.5× the threshold). Unlike CCh-suppressed myocyte contractile responsiveness to ISO in WT cells (“accentuated antagonism”), CCh had little effect on ISO-stimulated contraction in the eNOSnull myocyte.
Table 1.
Percent shortening of murine ventricular myocytes in response to ISO (10 nM) and CCh (10 μM)
| Cell # | WT
|
eNOSnull
|
||||
|---|---|---|---|---|---|---|
| Baseline | ISO | ISO + CCh | Baseline | ISO | ISO + CCh | |
| 1 | 8.40 | 15.98 | 9.90 | 7.98 | 14.65 | 14.38 |
| 2 | 9.77 | 13.29 | 10.56 | 10.73 | 16.46 | 16.84 |
| 3 | 9.32 | 13.26 | 10.77 | 9.28 | 18.46 | 16.92 |
| 4 | 10.11 | 17.52 | 12.64 | 8.61 | 17.07 | 16.46 |
| 5 | 8.48 | 18.29 | 13.00 | 7.69 | 17.46 | 15.82 |
| 6 | 5.91 | 20.00 | 14.21 | 13.09 | 20.20 | 20.20 |
| 7 | 9.16 | 18.27 | 12.79 | 7.43 | 15.70 | 11.11 |
| 8 | 10.91 | 19.13 | 13.20 | 6.25 | 24.28 | 16.97 |
| 9 | 12.32 | 21.80 | 16.71 | 10.14 | 23.92 | 21.39 |
| 10 | 7.49 | 17.20 | 14.10 | 10.69 | 15.43 | 14.78 |
| Mean | 9.19 | 17.47* | 12.79** | 9.19 | 18.36* | 16.49 |
| ± SEM | ± 0.57 | ± 0.86 | ± 0.64 | ± 0.64 | ± 1.08 | ± 0.91 |
*Significantly different from Baseline.
**Significantly different from ISO-treated group.
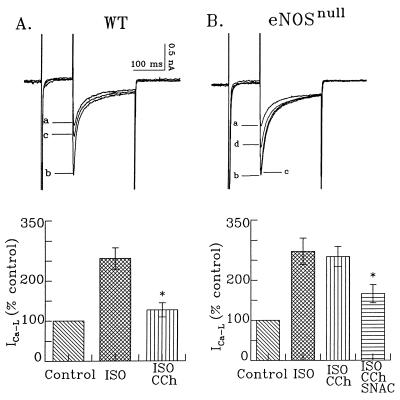
Because transmembrane influx of Ca2+ is a major determinant of myocyte contractility, we next examined the responsiveness of transmembrane Ca2+ current, ICa-L, to adrenergic and cholinergic agonists. In all myocytes (n = 21) from WT mice, CCh (1 μM) resulted in marked, accentuated antagonism of ISO (1 μM)-stimulated ICa-L (Fig. 2A). As with myocyte amplitude of shortening, increases in ICa-L in response to ISO were not affected in eNOSnull myocytes. However, as shown in Fig. 2B, CCh inhibition of ISO-stimulated ICa-L was abolished in the majority of cells studied (n = 17 cells for eNOSnull mice). Of interest, subsequent application of the NO donor S-nitroso-acetyl-cysteine (100 μM) resulted in suppression of ISO-stimulated ICa-L.
Figure 2.
Muscarinic cholinergic suppression of ISO-stimulated ICa-L is absent in eNOSnull ventricular myocytes. The effects of ISO and CCh on L-type calcium current (ICa-L) in ventricular myocytes from both WT and eNOSnull mice are shown. (A) CCh significantly inhibited ISO-stimulated ICa-L in WT myocytes. Current traces labeled a, b, and c were recorded under control conditions (a), during ISO infusion (10 nM) (b), and during CCh infusions (10 μM) in the continuous presence of ISO (c). Averaged data for 21 cells is illustrated in the bar graphs. (B) CCh had no significant effect on ISO-stimulated ICa-L in ventricular myocytes from eNOSnull mice. Current traces were recorded under control conditions (a), during ISO infusion (b), during CCh infusion in the continuous presence of ISO (c), and during infusion of the NO donor S-nitroso-acetyl-cysteine (SNAC) (100 μM) in the presence of ISO and CCh. Note that direct application of NO caused a significant inhibition in ISO-stimulated ICa-L (d).
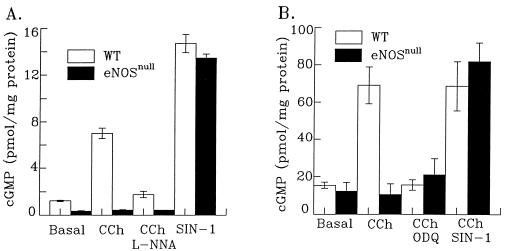
Because the signal transduction cascade linking M2 muscarinic cholinergic receptor activation, eNOS, and control of ICa-L is presumed to act via cGMP, we next examined cGMP levels in isolated myocytes and whole hearts removed from eNOSnull and WT animals. As shown in Fig. 3 A and B, CCh significantly increased myocyte cGMP levels in WT myocytes and whole ventricular muscle slices, respectively, an effect that could be blocked by the NOS inhibitor L-nitroarginine. In contrast, CCh had no effect on cellular cGMP levels in eNOSnull animals. To demonstrate that cGMP levels in myocytes from eNOSnull animals could be elevated by NO, the pharmacologic NO donor SIN-1 was employed. As shown in Fig. 3, SIN-1 markedly increased cGMP levels in both WT and eNOSnull myocytes both in isolated myocytes (A) and in whole tissue slices (B). As expected, the muscarinic agonist-induced elevation of cGMP in WT myocytes could be suppressed by the guanylyl cyclase inhibitor 1H-[1,2,4])Oxadiazole-[4,3-a] quinoxalin-1-one (1 μM).
Figure 3.
CCh does not activate guanylyl cyclase in eNOSnull myocytes. (A) CCh significantly increased cGMP levels in ventricular myocyte primary isolates from WT but not in myocytes from eNOSnull mice. The increase in cGMP production induced by CCh in WT myocytes could be prevented by the NOS inhibitor L-nitroarginine (L-NNA) (100 μM). The NO donor SIN-1 (100 μM), increased cGMP levels to a similar extent in both WT and eNOSnull myocytes. (B) The CCh-stimulated increase in cGMP production in ventricular muscle slices was caused by the activation of a NO-dependent guanylyl cyclase. The guanylyl cyclase inhibitor 1H-[1,2,4]Oxadiazole-[4,3-a] quinoxalin-1-one (1 μM) blocked CCh-induced cGMP elevation in ventricular muscle from WT mice. The NO donor SIN-1 (100 μM) again increased cGMP levels in both WT and eNOSnull ventricular slices.
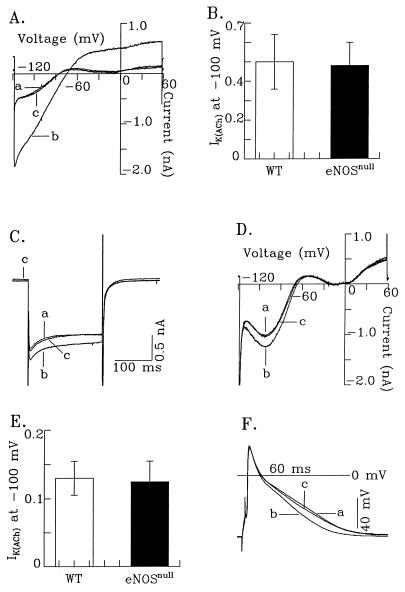
In atrial muscle, muscarinic cholinergic stimulation is known to activate an acetylcholine-sensitive K+ current (IK(ACh)), which hyperpolarizes the membrane and abbreviates action potential duration, an important regulatory mechanism for suppressing the chronotropic and inotropic responsiveness of the heart. To verify that activation of IK(ACh) by muscarinic agonists, which is not known to be linked to NOS activation, remained unaffected in eNOSnull myocytes, we examined IK(ACh) in atrial and ventricular myocytes. Fig. 4A shows the current–voltage relationship of IK(ACh) generated by using a ramp protocol in an atrial myocyte isolated from an eNOSnull mouse. In seven cells from two eNOSnull mice, CCh (1 μM) markedly and reversibly activated IK(ACh). The amplitude of IK(ACh) measured at −100 mV was not significantly different from the current seen in WT atrial myocytes (Fig. 4B). IK(ACh) also could be detected in ventricular myocytes from both WT and eNOSnull hearts. Fig. 4C shows the activation of IK(ACh) in an eNOSnull ventricular myocyte. Hyperpolarization from a holding potential of −40 mV to −100 mV activated the inwardly rectifying background K+ current. Exposure to CCh (1 μM) significantly increased this current, which returned to control levels on removal of CCh. The current–voltage relationship of ventricular IK(ACh) is shown in Fig. 4D. The muscarinic cholinergic antagonist atropine (1 μM) completely reversed the effect of CCh. When measured at a test potential of −100 mV, the magnitude of ventricular IK(ACh) did not differ between WT and eNOSnull mice (Fig. 4E). Because activation of IK(ACh) is known to shorten action potential duration, we verified that this could be demonstrated in eNOSnull ventricular myocytes, as shown in Fig. 4F. This CCh-induced abbreviation in action potential duration was caused by the activation of muscarinic receptors because the action potential shortening could be reversed by atropine.
Figure 4.
Targeted disruption of eNOS does not affect muscarinic activation of acetylcholine-sensitive K+ current (IK(ACh)). (A) The activation of IK(ACh) in an eNOSnull atrial myocyte is illustrated at a holding potential of −40 mV and after a ramp pulse from −150 to +60 mV, applied to the cell at 0.1V/s. ICa-L was blocked by 0.4 mM Cd2+. The fast inward sodium current also was blocked largely by Cd2+. (B) A comparison of IK(ACh) from eNOSnull (n = 5) and WT (n = 7) atrial myocytes. The amplitude of IK(ACh) was determined as the difference current level at −100 mV. (C) The activation of IK(ACh) in an eNOSnull ventricular myocyte. A hyperpolarization pulse from a holding potential of −40 mV to −100 mV was applied to the cell, and traces a, b, and c were recorded under control conditions, with CCh (1 μM) application, and after washout of CCh, respectively. (D) The current–voltage relationship of IK(ACh) in an eNOSnull ventricular myocyte. The ramp pulse was identical to that described in A. ICa-L and sodium current were blocked by Cd2+ (0.4 mM). Traces a, b, and c were recorded under control conditions, with CCh (1 μM), and with atropine (1 μM) in the continuous presence of CCh. (E) A comparison of IK(ACh) (at −100 mV) from both eNOSnull (n = 8) and WT (n = 7) ventricular myocytes. (F) Activation of IK(ACh) in an eNOSnull ventricular myocyte abbreviates action potential duration. Traces a, b, and c were recorded under control conditions (a), during CCh (1 μM) application (b), and with atropine (1 μM) in the continuous presence of CCh (c).
DISCUSSION
Three areas of controversy have been resolved in this study using the eNOSnull mice. The first is the unequivocal demonstration that eNOS activation is essential for muscarinic cholinergic control of ventricular ICa-L but not for the activation of IK(ACh). Secondly, we have demonstrated that the stimulation of myocyte guanylyl cyclase and the increase in intracellular cGMP by muscarinic cholinergic agonists are dependent on the activation of myocyte eNOS. Although the effects of increased intracellular cGMP on ICa-L in myocytes have been reported to range from stimulatory to neutral to inhibitory, depending on the specific species, myocyte phenotype, and level of intracellular cAMP, the data reported here support a growing consensus that cGMP suppresses the magnitude of Ca2+ influx via ICa-L in cells that have elevated cAMP levels (19, 29–32). A similar NO/cGMP-dependent signal transduction pathway also has been demonstrated in cardiac pacemaker cells (33, 34) and basophilic cells (35) after exposure to adenosine. Finally, we have demonstrated that IK(ACh) is present within murine ventricular as well as atrial myocytes. Although the IK(ACh) current density was relatively low in ventricular myocytes, activation of IK(ACh) was able to shorten action potential duration in these cells.
The presence of IK(ACh) channels in ventricular cells may account in part for the demonstration of some NO-independent effects of muscarinic cholinergic agonists on myocyte contractile function (36–42). Expression of IK(ACh) in ventricular muscle may explain why there was a trend for CCh to inhibit myocyte contractile responsiveness to ISO in eNOSnull mice. Indeed, in two eNOSnull myocytes (cells 7 and 8 in Table 1), the extent of CCh-induced inhibition of contractile responsiveness was comparable to that seen in myocytes from WT mice. These differences in responsiveness to CCh in eNOSnull myocytes may be in part caused by the known heterogeneity in expression levels of IK(ACh) in different regions of ventricular muscle (40, 43). It also is possible that eNOSnull ventricular myocytes might exhibit an increase in expression of IK(ACh) because increased expression of K+ channels has been reported recently in response to hypertrophic stimuli in vitro (44). The hearts of eNOSnull animals typically are hypertrophied moderately compared with WT hearts, presumably because of the sustained hypertension characteristic of this animal model (26).
Regardless of the effects of limited expression of IK(ACh) in ventricular myocytes from eNOSnull animals, the absence in eNOSnull cells of an intact signal transduction cascade linking muscarinic cholinergic receptor activation to myocyte contractile responsiveness could be verified by measurement of intracellular cGMP levels and by whole-cell patch clamp measurements of ICa-L. Of interest, data from our laboratory on isolated adult rat ventricular myocytes and by others on intact heart preparations have noted that NOS inhibition accentuates the contractile response to ISO even in the absence of a muscarinic agonist (2). Although there was a trend toward an (≈10%) increase in contractile amplitude in WT compared with eNOSnull cells, this increase did not reach statistical significance in the number of cells studied here. This likely is caused in part by the fact that the previous report (2) used submaximal concentrations of ISO (e.g., 2 nM ISO in isolated adult rat ventricular myocytes), unlike the near maximal response elicited by 10 nM ISO in the experiments reported here.
Direct effects of pharmacologic NO donors on myocyte ion channel function also have been reported. Campbell et al. (45) and Hu et al. (46) noted that NO donors, and particularly S-nitrosothiols, can directly affect ICa-L in ferret ventricular myocytes and in L-type Ca2+ channel subunits transiently transfected into HEK293 cells, respectively. In neither report were these effects attributable to activation of guanylyl cyclase in these cells. Musialek et al. (47) also reported that the NO donors SIN-1 and sodium nitroprusside both had a concentration-dependent, biphasic effect on the hyperpolarization-activated inward current If in guinea pig sinoatrial node cells, an effect that was at least in part caused by activation of guanylyl cyclase. These and other reports (reviewed in refs. 16, 21, and 22) show that NO donors can have both cGMP-dependent and cGMP-independent effects on ICa-L, If, and other ion channel components in cardiac myocytes and suggest additional mechanisms through which both endogenous and exogenous sources of NO could affect myocardial contractile function.
However, pharmacologic NO donors cannot mimic the spatial and temporal constraints on NO generated endogenously within cells, such as the targeting of eNOS in cardiac myocytes to sarcolemmal caveolae. The data presented here in eNOSnull cardiac myocytes nevertheless support previous work using pharmacologic NOS inhibitors and/or NO donors that implicate an important role for eNOS in mediating parasympathetic nervous system signaling in the heart (1–12). These data also support the contention that the effects of endogenously generated NO within cardiac myocytes are mediated by activation of guanylyl cyclase. Of importance, although the data presented here imply that regulation of ICa-L is a major intracellular target of CCh-mediated eNOS activation, other mechanisms may be involved (e.g., an alteration in myofilament Ca2+ sensitivity by regulation of cAMP-dependent or cGMP-dependent phosphorylation of, for example, troponin I). Finally, the detection of IK(ACh) in ventricular myocytes provides one explanation for the observation of some NO-independent effects of muscarinic cholinergic agonists on the contractile function of ventricular myocytes.
Acknowledgments
This work was supported by National Institutes of Health Grant HL52320.
ABBREVIATIONS
- NO
nitric oxide
- NOS
NO synthase
- eNOS
endothelial NOS
- ICa-L
voltage-sensitive L-type Ca2+ channels
- IK(ACh)
acetylcholine-activated K+ channel
- WT
wild-type
- ISO
isoproterenol
- CCh
carbachol
- SIN-1
3-morpholino-sydnonimine
References
- 1.Sterin-Borda L, Echague A V, Leiros C P, Genaro A, Borda E. Br J Pharmacol. 1995;115:1525–1531. doi: 10.1111/j.1476-5381.1995.tb16646.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balligand J-L, Kelly R A, Marsden P A, Smith T W, Michel T. Proc Natl Acad Sci USA. 1993;90:347–351. doi: 10.1073/pnas.90.1.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hare J M, Keaney J F, Balligand J L, Loscalzo J, Smith T W, Colucci W S. J Clin Invest. 1995;95:360–366. doi: 10.1172/JCI117664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keaney J F, Hare J M, Balligand J-L, Loscalzo J, Smith T W, Colucci W S. Am J Physiol. 1996;271:H2646–H2652. doi: 10.1152/ajpheart.1996.271.6.H2646. [DOI] [PubMed] [Google Scholar]
- 5.Hare J M, Loh E, Creager M A, Colucci W S. Circulation. 1995;92:2198–2203. doi: 10.1161/01.cir.92.8.2198. [DOI] [PubMed] [Google Scholar]
- 6.Elvan A, Rubart M, Zipes D P. Am J Physiol. 1997;272:H263–H271. doi: 10.1152/ajpheart.1997.272.1.H263. [DOI] [PubMed] [Google Scholar]
- 7.Han X, Shimoni Y, Giles W R. J Physiol (London) 1994;476:309–314. doi: 10.1113/jphysiol.1994.sp020132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han X, Shimoni Y, Giles W R. J Gen Physiol. 1995;106:45–65. doi: 10.1085/jgp.106.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Han X, Kobzik L, Balligand J-L, Kelly R A, Smith T W. Circ Res. 1996;78:998–1008. doi: 10.1161/01.res.78.6.998. [DOI] [PubMed] [Google Scholar]
- 10.Levi R C, Alloatti G, Penna C, Gallo MP. Pflügers Arch. 1994;426:419–426. doi: 10.1007/BF00388305. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y G, Lipsius S L. Circ Res. 1995;76:634–644. doi: 10.1161/01.res.76.4.634. [DOI] [PubMed] [Google Scholar]
- 12.Balligand J-L, Kobzik L, Han X, Kaye D M, Belhassen L, O’Hara D S, Kelly R A, Smith T W, Michel T. J Biol Chem. 1995;270:14582–14586. doi: 10.1074/jbc.270.24.14582. [DOI] [PubMed] [Google Scholar]
- 13.Seki T, Hagiwara H, Naruse K, Kadowaki M, Kashiwagi M, Demura H, Hirose S, Naruse M. Biochem Biophys Res Commun. 1996;218:601–605. doi: 10.1006/bbrc.1996.0106. [DOI] [PubMed] [Google Scholar]
- 14.Mery P-F, Pavoine C, Belhassen L, Pecker F, Fischmeister A. J Biol Chem. 1993;268:26286–26295. [PubMed] [Google Scholar]
- 15.Michel T, Feron O. J Clin Invest. 1997;100:2146–2152. doi: 10.1172/JCI119750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly R A, Balligand J-L, Smith T W. Circ Res. 1996;79:363–380. doi: 10.1161/01.res.79.3.363. [DOI] [PubMed] [Google Scholar]
- 17.Wahler G M, Dollinger S J. Am J Physiol. 1995;268:C45–C54. doi: 10.1152/ajpcell.1995.268.1.C45. [DOI] [PubMed] [Google Scholar]
- 18.Moncada S, Palmer R M J, Higgs E A. Pharmacol Rev. 1991;433:109–142. [PubMed] [Google Scholar]
- 19.McDonald T F, Pelzer P, Trautwein W, Pelzer D J. Physiol Rev. 1994;74:365–507. doi: 10.1152/physrev.1994.74.2.365. [DOI] [PubMed] [Google Scholar]
- 20.Ignarro L, Murad F. Adv Pharmacol. 1995;34:1–516. [Google Scholar]
- 21.Kelly R A, Han X. Circulation. 1997;96:2493–2495. [PubMed] [Google Scholar]
- 22.Mery P-F, Abi-Gerges N, Vandecasteele G, Jurevicius J, Eschenhagen T, Fischmeister R. Life Sci. 1997;60:1113–1120. doi: 10.1016/s0024-3205(97)00055-6. [DOI] [PubMed] [Google Scholar]
- 23.Mery P-F, Hove-Madsen L, Chesnais J M, Hartzell H C, Fischmeister R. Am J Physiol. 1996;270:H1178–H1188. doi: 10.1152/ajpheart.1996.270.4.H1178. [DOI] [PubMed] [Google Scholar]
- 24.Zakharov S I, Pieramici S, Kumar G K, Prabhakar N R, Harvey R D. Circ Res. 1996;78:925–935. doi: 10.1161/01.res.78.5.925. [DOI] [PubMed] [Google Scholar]
- 25.Valenzuela D, Han X, Mende U, Fankhouser C, Mashimo H, Huang P, Pfeffer J, Neer E J, Fishman M C. Proc Natl Acad Sci USA. 1997;94:1727–1732. doi: 10.1073/pnas.94.5.1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang P L, Huang Z, Moshimo H, Bloch K D, Moskowitz M A, Bevan J S, Fishman M C. Nature (London) 1995;377:239–242. doi: 10.1038/377239a0. [DOI] [PubMed] [Google Scholar]
- 27.Hamill O P, Marty A, Neher E, Sakmann B, Sigworth F J. Pflügers Arch. 1981;391:85–10. doi: 10.1007/BF00656997. [DOI] [PubMed] [Google Scholar]
- 28.Fabiato A, Fabiato F. J Physiol (Paris) 1979;75:463–505. [PubMed] [Google Scholar]
- 29.Hartzell H C. Prog Biophys Mol Biol. 1988;52:165–247. doi: 10.1016/0079-6107(88)90014-4. [DOI] [PubMed] [Google Scholar]
- 30.Ono K, Trautwein W. J Physiol (London) 1991;443:387–404. doi: 10.1113/jphysiol.1991.sp018839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shirayama T, Pappano A J. J Pharmacol Exp Ther. 1996;279:1274–1281. [PubMed] [Google Scholar]
- 32.Sumii K, Sperelakis N. Circ Res. 1995;77:803–812. doi: 10.1161/01.res.77.4.803. [DOI] [PubMed] [Google Scholar]
- 33.Martynyuk A E, Kane K A, Cobbe S M, Rankin A C. Pflügers Arch. 1996;431:452–457. doi: 10.1007/BF02207285. [DOI] [PubMed] [Google Scholar]
- 34.Shimoni Y, Han X, Giles W R. Br J Pharmacol. 1996;119:1463–1469. doi: 10.1111/j.1476-5381.1996.tb16059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller K J, Hoffman B J. J Biol Chem. 1994;269:27351–27356. [PubMed] [Google Scholar]
- 36.McMorn S O, Harrison S M, Zang W J, Yu X J, Boyett M R. Am J Physiol. 1993;265:H1393–H1400. doi: 10.1152/ajpheart.1993.265.4.H1393. [DOI] [PubMed] [Google Scholar]
- 37.Koumi S-I, Wasserstrom J A. Am J Physiol. 1994;266:H1812–1821. doi: 10.1152/ajpheart.1994.266.5.H1812. [DOI] [PubMed] [Google Scholar]
- 38.Koumi S-I, Sato R, Hayakawa H. J Membr Biol. 1995;145:143–150. doi: 10.1007/BF00237372. [DOI] [PubMed] [Google Scholar]
- 39.Gadbut A P, Riccardi D, Wu L, Hebert S C, Galper J B. J Biol Chem. 1996;271:6398–6402. doi: 10.1074/jbc.271.11.6398. [DOI] [PubMed] [Google Scholar]
- 40.Yang Z K, Boyett M R, Janvier N C, McMorn S O, Shui Z, Karim F. J Physiol (London) 1996;492:789–806. doi: 10.1113/jphysiol.1996.sp021346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xie L-H, Takano M, Noma A. Am J Physiol. 1997;272:H1741–1750. doi: 10.1152/ajpheart.1997.272.4.H1741. [DOI] [PubMed] [Google Scholar]
- 42.Koumi S-I, Sato R, Nagasawa K, Hayakawa H. J Membr Biol. 1997;157:71–81. doi: 10.1007/s002329900217. [DOI] [PubMed] [Google Scholar]
- 43.Litovsky S H, Antzelevitch C. Circ Res. 1990;67:615– 627. doi: 10.1161/01.res.67.3.615. [DOI] [PubMed] [Google Scholar]
- 44.Guo W, Kada K, Kamiya K, Toyama J. Am J Physiol. 1997;272:H2599–H2606. doi: 10.1152/ajpheart.1997.272.6.H2599. [DOI] [PubMed] [Google Scholar]
- 45.Campbell D L, Stamler J S, Strauss H C. J Gen Physiol. 1996;108:277–293. doi: 10.1085/jgp.108.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hu H, Chiamvimonvat N, Yamagishi T, Marban E. Circ Res. 1997;81:742–752. doi: 10.1161/01.res.81.5.742. [DOI] [PubMed] [Google Scholar]
- 47.Musialek P, Lei M, Brown H F, Paterson D J, Casadei B. Circulation. 1997;81:60–68. doi: 10.1161/01.res.81.1.60. [DOI] [PubMed] [Google Scholar]