Abstract
Objectives/Hypothesis
The present study proposed to estimate phonation threshold pressure (PTP) non-invasively using airflow redirection into a pneumatic capacitance system.
Study Design
Prospective study.
Methods
Subjects phonated into the device, which interrupts airflow mechanically and redirects the flow into a pneumatic capacitor. Five interruptions were effected per trial. PTP was estimated as the difference between subglottal pressure (SGP) and transglottal pressure at phonation offset. The novel method was tested for consistency in 20 normal human subjects at low (75 dB) and high (85 dB) sound pressure levels. The device was tested for validity on a tracheotomy patient.
Results
Mean SGP was 9.02 ± 3.27 cm H2O and mean PTP was 3.68 ± 1.41 cm H2O. Intrasubject coefficient of variation, a measure of intrasubject consistency, was 0.33 ± 0.23. Statistically significant differences existed between the means of SGP but not PTP at 75 dB and 85 dB. The correlation coefficient between accepted and experimental SGP in a tracheotomy patient was 0.947 (p<0.001).
Conclusions
Measurements corresponded well to previously reported values, and intrasubject variability was low, indicating the device was consistent. Testing on a tracheotomy patient demonstrated validity. More research is needed to determine the sensitivity and specificity of the device in differentiating between normal and pathological voices. This device may have clinical application as a non-invasive and reliable method of estimating PTP and indicating that laryngeal health is likely abnormal.
Keywords: phonation threshold pressure, subglottal pressure, laryngeal aerodynamics, EGG, mechanical interruption
INTRODUCTION
The efficacy of the larynx as an energy transducer can be described, in part, by quantifying the aerodynamic input. One parameter describing this input is phonation threshold pressure (PTP), the minimum subglottal pressure required to initiate phonation. PTP is dependent upon the biomechanical properties of the larynx, including the vocal fold thickness, tissue damping coefficient, prephonatory glottal width, and mucosal wave velocity.1,2 These variables reflect the physiological state of the larynx. The degree of vocal fold hydration, for example, is inversely related to the vocal fold tissue viscosity and stiffness. Both viscosity and stiffness affect the dampening coefficient and mucosal wave velocity which in turn directly influence PTP; therefore, hydration is expected to inversely affect PTP. Studies have shown that PTP is also altered by abnormal states of the larynx, including disease,3 vocal scarring,4 wound healing,5 vocal fatigue,6 and abnormal hydration levels.6,7 Because PTP is dependent on the biomechanical properties of the larynx, it may be a useful parameter for suggesting that laryngeal function is abnormal. Moreover, a low PTP indicates a low required respiratory effort, and thus a greater ease of phonation. Minimizing PTP should increase phonatory efficiency and decrease respiratory demand.8
Several invasive methods have been used to measure PTP directly. Subglottal pressure (SGP) measurements can be directly recorded during phonation using a small pressure transducer inserted into a tracheotomy tube;9 using this procedure at phonation onset or offset provides a measure of PTP.10,11 Another direct method of SGP detection uses a miniature pressure transducer which is inserted transnasally into the subglottal region.12 This method has also been used to measure PTP. However, these techniques are too invasive to employ in a routine clinical assessment of laryngeal health.
Intraoral pressure measurements during labial interruption of phonation can be used to estimate PTP in a non-invasive, clinically feasible fashion. SGP is closely estimated by intraoral pressure when the airway is interrupted during the repetition of a combination of voiceless stop consonants and vowels,13 and this technique has also been applied to estimate PTP.14 Kitajima et al. calculated SGP by measuring the intraoral pressure during the consonant /p/ and the peak intraoral pressure by measuring the intraoral pressure during the consonant /b/: they predicted that the difference of these two points was equal to PTP.15 Another labial interruption method describes using a repetition of voiceless stop consonant-vowel combinations at a suprathreshold effort level, subthreshold effort level (whisper), and then near-threshold effort level to estimate PTP.7 The first supra- and subthreshold tasks were designed to help provide a target intensity range for the subject. Subjects must be trained to maintain consistent glottal configuration and lung pressure at an abnormally low subglottal pressure for the measurement to be accurate, which may contribute to inconsistent results, especially in subjects with neuromuscular disorders. Fluctuations in the way subjects accomplish lip closure and inadvertent modification of glottal configuration or phonatory effort at the time of labial occlusion may introduce additional variability into the measurement. These confounding variables decrease the reliability of this measurement method. Mechanical interruption of phonation has become a method of interest in estimating PTP through intraoral pressure measurements, showing promising results in recent literature.
Mechanical interruption using a balloon valve was first introduced by Bard et al. in 1992 to measure SGP; these measurements were validated by direct SGP measurements in a tracheotomy patient.16 This technique was applied to measure PTP by Jiang et al. using a 500 ms complete mechanical interruption.10 PTP was estimated by subtracting from SGP the intraoral pressure at the time that phonation ceased after interruption of airflow. This technique was shown to have high sensitivity and specificity using receiver operating characteristic curves in normal subjects and subjects with Parkinsonism.17 While these measurements were validated against simultaneous direct SGP measurements in a tracheotomy patient, the long interruption time sometimes caused confounding artifacts in the flow and pressure that may have been the result of a laryngeal reflex. Baggott et al. calculated the interruption time to maximize airway occlusion while avoiding laryngeal adductor reflexes to be 135 ms, and used a series of three balloon interruptions to redirect airflow into a one-way valve gated tank that was pre-pressurized below SGP.18 This novel method of estimating SGP used a tank as a pneumatic capacitor, with each interruption redirecting oral airflow into the capacitor until the pressure inside the tank was equal to SGP.
This study proposed to estimate PTP by redirecting airflow during mechanical interruptions of phonation into a pneumatic capacitor. Phonation offset was determined by electroglottography, a robust and relatively noise-free indicator of vocal fold vibration. The difference between SGP and intraoral pressure using this method at phonation offset was interpreted to be the PTP. To our knowledge, PTP has never before been measured using a pneumatic capacitance-model system. This method was tested for consistency in 20 normal human subjects, and validated in a tracheotomy patient.
MATERIALS AND METHODS
Apparatus
The apparatus (Figure 1) is a novel system for determining PTP, based on the work of Baggott et al.18 Subjects phonate into a mouthpiece (Series 9063; Hans Rudolph) connected to the tank via 1.905 cm CPVC tubing, which is open to the environment by default. During the mechanical interruption, a balloon valve (9340 Series 2-way Shutoff Valve, Inflatable-Balloon Type; Hans Rudolph) occludes the opening to the environment, redirecting airflow into the 5 L tank, constructed of 10.16 cm diameter PVC pipe capped at both ends. The tank contains two ports: one is an input from the mouthpiece and is gated by a low-flow one-way valve (1810 Series; Hans Rudolph), and the other is an exhaust which is capped with a rubber stopper. The input-only one-way valves provide the pneumatic capacitance characteristics of the tank. Two separate Pneumotach Amplifier 1 model pressure transducers (Series 1110; Hans Rudolph) measure the pressures both inside the tank and in the mouthpiece. These output voltage to the data acquisition system, through a Baby-N Connector Block (BNC-2110; National Instruments, Austin, TX), a DAQ PCMCIA card (PCI-6036E, National Instruments), and LabVIEW 8.0 Software (custom-programmed Acquisition and Control program, National Instruments). Phonation is monitored by a digital sound pressure level meter (33 2055; Radioshack, Fort Worth, TX) and an electroglottograph (EG2; Glottal Enterprises, Syracuse, New York) attached to the subject’s neck by a Velcro strap. Both acoustic and EGG systems output voltage to the data acquisition system for digital recording.
Figure 1.
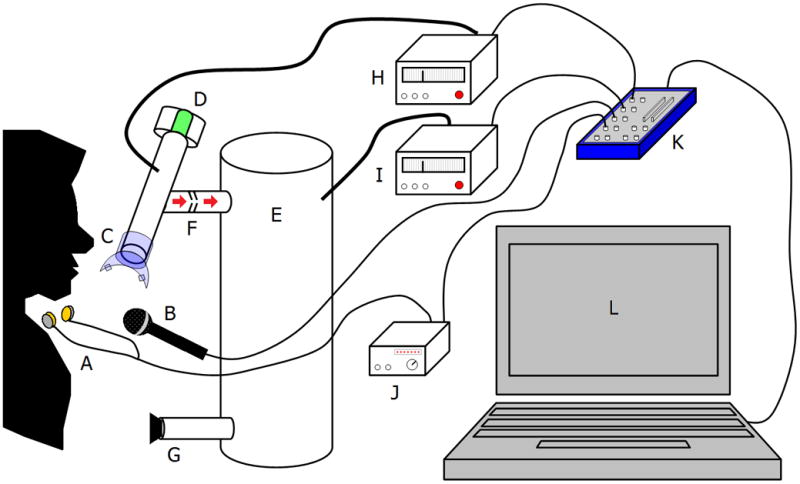
Diagram of the PTP interruption-redirection system. The central components are as follows: (A) EGG electrodes; (B) microphone for SPL meter; (C) mouthpiece; (D) inflatable balloon valve; (E) air tank (pneumatic capacitor); (F) one-way air valve; (G) plugged air escape gate; (H) intraoral pressure transducer; (I) tank pressure transducer; (J) EGG; (K) digital data acquisition board; (L) laptop computer. Pneumatic cables are thick and electrical cables are thin.
In each trial, subjects were instructed to phonate the phoneme /a/ for approximately 10 seconds, maintaining consistent vocal effort throughout. The decibel meter provided feedback of the sound pressure level to the subjects to assist them in maintaining a consistent level. A series of mechanical interruptions approximately 200 ms in duration interrupted phonation, redirecting airflow into the tank. At least five mechanical interruptions of phonation were effected per trial. PTP values for each interruption were calculated retrospectively and averaged over the trial. The coefficient of variation (defined as the ratio of standard deviation to the mean) in PTP was calculated for each subject to quantify intrasubject consistency.
PTP was estimated using the expression reported by Jiang et al.; the subglottal pressure minus the transglottal pressure at the point of phonation cessation.10 Phonation offset was determined by the EGG signal. For each trial, there was a single SGP measurement and as many transglottal pressure measurements as there were interruptions in which phonation ceased. The peak tank pressure was interpreted to be the estimated SGP. The intraoral pressures at the moments phonation ceased during each interruption were reported as the transglottal pressures. In accordance with the expression reported by Jiang et al., the difference between these pressures was the estimated PTP.
Testing on normal subjects
Approval for this study was obtained from the University of Wisconsin-Madison Health Sciences Institutional Review Board. The apparatus was tested for consistency on a sample population of 20 volunteer human subjects ages 18–25 from the area around the University of Wisconsin-Madison. Exclusion criteria included (1) history of vocal, respiratory, or neurological disorders, (2) recent history of upper respiratory infections, and (3) inability to sustain a vowel sound for ten seconds. The subjects were each tested five times at sound pressure levels (SPL) of approximately 75 dB (“low”) and 85 dB (“high”), for a total of ten trials. SGP, PTP, and coefficient of variation in PTP were averaged in each sound pressure level condition of each subject, and means and standard deviations were calculated.
Testing on a patient with a tracheotomy
The apparatus was tested for validity by applying the method to a patient with a tracheotomy. Direct subglottal pressure measurements were taken by inserting a pressure transducer into the tracheostomy tube and sealing the area around the transducer. The experimental measurements were compared to actual SGP measurements as measured through the subglottal tracheotomy. The correlation coefficient was reported and a paired t-test was conducted to determine if statistically significant differences existed between the means of the experimental SGP data and the actual SGP data.
RESULTS
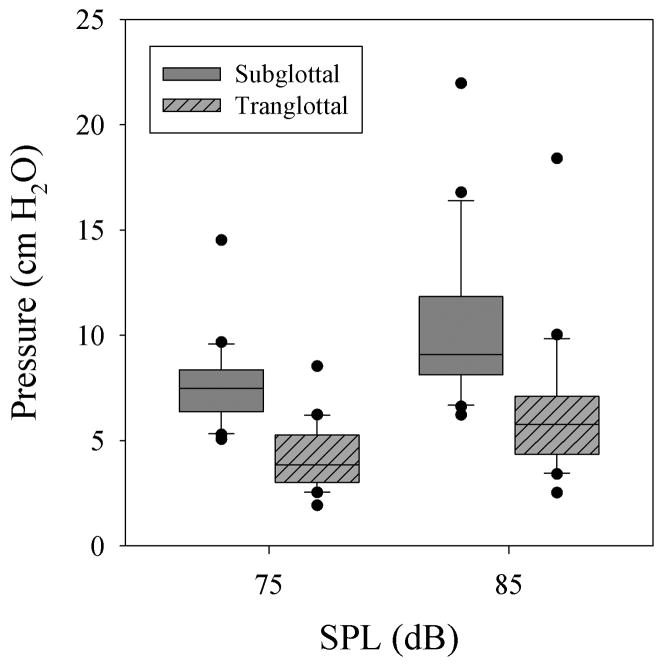
Phonation threshold pressure data collected from 20 subjects, each performing five trials at low and high SPLs, can be seen in Figure 2. There were no statistically significant differences between the means of PTP at both SPL(p=0.191, t19=−1.355, paired two-tailed t-test). The mean PTP at low and high SPL were 3.45 ± 1.18 cm H2O and 3.91 ± 1.62 cm H2O. The overall mean PTP was 3.68 ± 1.41 cm H2O. A sample interruption using the device is shown in Figure 3.
Figure 2.
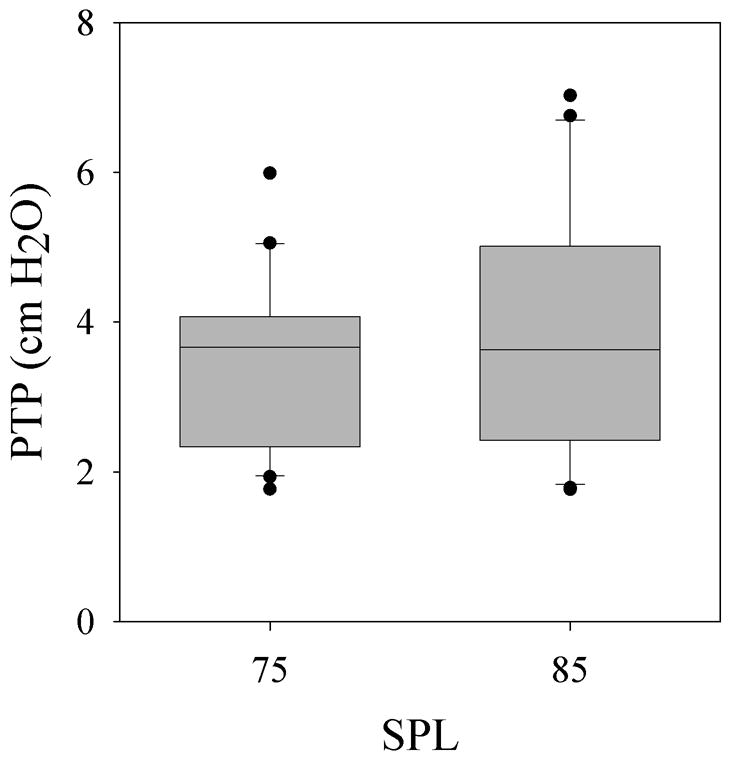
Phonation threshold pressures from 20 normal subjects at low and high SPLs. There were no statistically significant differences between the means of both groups (p=0.191, t19=−1.355, paired two-tailed t-test). The upper and lower edges of the box represent the 75th and 25th percentile, respectively, and a line within each box marks the median PTP for the given elongation level. Whiskers above and below each box represent the 90th and 10th percentiles, respectively. Statistical outliers are graphed as points.
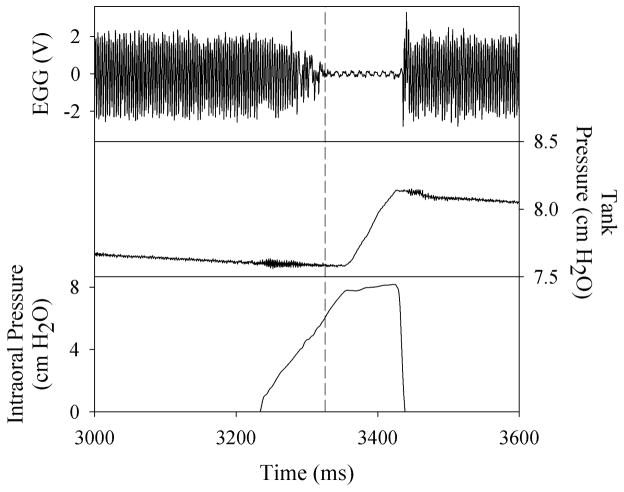
Figure 3.
A sample interruption from the middle of a trial using the airflow interruption-redirection system. The intraoral pressure at the time of phonation offset (dashed line) is interpreted to be the transglottal pressure, and the peak tank pressure is interpreted to be the SGP. For each trial, as many transglottal pressure measurements as there were interruptions and a single SGP measurement were recorded. The differential pressure at each instance of phonation offset is the estimated PTP. The delayed rise in tank pressure during the interruption illustrates the capacitance characteristics. A minimum of five interruptions occurred within each ten second trial.
The coefficient of variation (Cv) was calculated for each subject as a measure of intrasubject variability normalized to the mean. Figure 4 shows boxplots of the Cv of PTP at both SPL, and a paired t-test suggested that there were no statistically significant differences between the means of Cv (p=0.845, t19=−0.199). The overall mean Cv was 0.33 ± 0.23.
Figure 4.
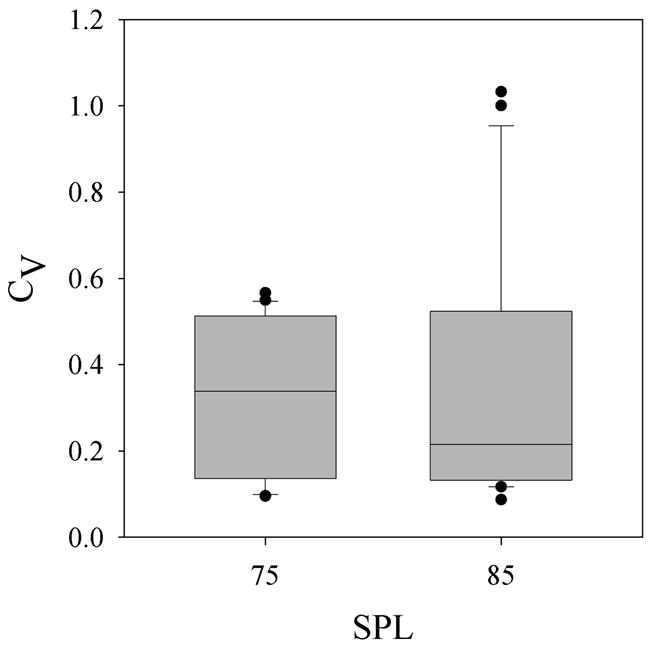
Coefficient of variation (Cv) in PTP from 20 normal subjects at low and high SPLs. There were no statistically significant differences between the means of both groups (p=0.845, t19=−0.199, paired two-tailed t-test). The upper and lower edges of the box represent the 75th and 25th percentile, respectively, and a line within each box marks the median PTP for the given elongation level. Whiskers above and below each box represent the 90th and 10th percentiles, respectively. Statistical outliers are graphed as points.
Figure 5 shows boxplots of SGP and transglottal pressure during the phoneme task in both SPL groups. The differences between the means of SGP in both SPL conditions (p<0.001, t19=−4.803, paired two-tailed t-test) and between the means of transglottal pressure in both SGP conditions (p<0.001, t19=−4.477, paired two-tailed t-test) are statistically significant. The overall mean SGP was 9.02 ± 3.27 cm H2O.
Figure 5.
Subglottal and transglottal pressure during speech task in 20 normal subjects at low and high SPLs. The differences between the means of SGP (p<0.001, t19=−4.803, paired two-tailed t-test) and transglottal pressure (p<0.001, t19=−4.477, paired two-tailed t-test) in both SGP groups were statistically significant.
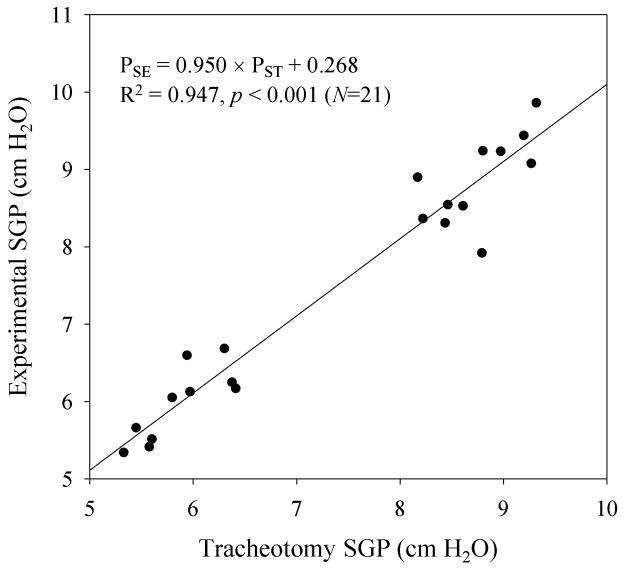
Figure 6 shows validation of the device on a tracheotomy patient. The correlation coefficient of experimentally measured SGP as a function of directly measured SGP was 0.947 (p<0.001). A paired t-test suggested that there were no statistically significant differences between the means of the two data groups (p=0.185, t20=−1.372).
Figure 6.
Experimentally measured SGP using the incomplete airflow redirection device (PSE) as a function of directly measured SGP in a tracheotomy patient (PST).
DISCUSSION
The novelty of this system lies in the measures taken to increase the reliability of PTP estimations, including (1) using an EGG to determine phonation offset precisely, and (2) maximizing the utility of mechanical interruptions while avoiding laryngeal reflexes.
The electroglottograph measures the impedance across the larynx as an estimate of the degree of contact between the vocal folds. The time-varying impedance signal, called an electroglottogram (EGG), describes the movements of the vocal folds with the amplitude variations representative of abduction variations; it is an indicator of the lateral contact area between the contralateral folds. An EGG provides a robust and relatively noise-free indicator of vocal fold oscillation, making it a useful tool for phonation offset determination, which is characterized by the cessation of small-amplitude vocal fold oscillations.
Previous mechanical interruption techniques to estimate PTP used a single, large interruption to measure the SGP and transglottal pressure. This technique sometimes yielded unreliable results, as pressure artifacts were seen which may have corresponded to the elicitation of laryngeal reflexes. A series of smaller duration interruptions coupled with airflow redirection into a pneumatic capacitor may circumvent laryngeal reflexes.18 Kearney et al. observed that a minimum 80 ms latency was required to elicit a laryngeal reflex using air puff stimuli, and Baggott et al. showed that the minimum interruption time to maximize airflow redirection yet avoid laryngeal reflexes was 135 ms.18,19 This was determined by adding the time required to occlude the vocal tract completely using a balloon valve (55 ms) and the minimum latency to laryngeal reflex elicitation by air puff stimulation (80 ms). Unpublished data from our laboratory suggested that this may have been an overly conservative estimate, particularly because of the differences between the direct air puff stimulation used in the study by Kearney et al. and the air pressure sensation that is characteristic of a mechanical interruption of phonation. During mechanical interruption, the oral air pressure gradually rises from the time that the vocal tract is occluded. Eventually, the air pressure increases enough to potentially stimulate the laryngeal adductor reflex. Because this is not comparable to direct air puff stimulation, which has an immediate stimulatory onset, the expected stimulation of possible laryngeal reflexes would be later than the immediate onset of a mechanical interruption. An interruption time of 200 ms was used in this study, and a minimum of five interruptions were effected in each trial.
In a few subjects, the number of interruptions during the trial was increased to accommodate for large SGP. Given the capacitance of the tank C = 4.995 mL / cm H2O and the relationship between added volume and pressure in a capacitor , the maximum detectable SGP of the apparatus can then be written as a function of the tank capacitance (C), interruption time (t), minimum oral airflow (Uo), and number of interruptions (N):
| (1) |
According to Baken et al., the minimum oral airflow is about 61 mL/s.20 The maximum SGP detectable by the device then would be a function of N and t:
| (2) |
Baken et al. surveyed 11 different sources of SGP data and found the maximum SGP was 7.6 cm H2O for “soft” vocal intensity, 13.7 cm H2O for “normal” vocal intensity, and 27.7 cm H2O for “loud” vocal intensity 20. Using an interruption time of 0.200 s, these maximum SGP could be detected using a minimum of 4, 6, and 11 interruptions, respectively. In our study, the maximum SGP was 21.97 cm H2O at a loud vocal intensity. The increased number of interruptions in some subjects is not problematic, because the researcher can observe the pressure trace of the pneumatic capacitor and determine if it has reached a horizontal asymptote. Because the tank pressure trace will have the characteristics of the trace of a charging capacitor, the researcher can determine if the capacitor has reached its maximum pneumatic charge, indicating SGP, or if additional interruptions are needed until each interruption no longer increases the pressure significantly within the capacitor.
The variability in measurement, quantified by the coefficient of variation (Cv), suggests that the device is consistent. PTP measurements are expected to vary within and between utterances due to their sensitivity to subtle changes in glottal variables. The proposed device measures the subglottal pressure at one time point and assumes it remains constant during the phoneme task, but phonation is a dynamic process and subjects are not likely able to consciously maintain a static glottal configuration. Because of this, high variability in PTP measurement does not entail imprecision or invalidity; it may simply reflect the heterogeneity of glottal configurations within subjects.
The PTP of the sample population corresponds well with previously reported values. Verdolini et al. measured the PTP of normal subjects at varying pitches using an intraoral pressure transducer and found the mean PTP to be 3.19 ± 0.86 cm H2O, 3.23 ± 0.67 cm H2O, and 8.52 ± 3.69 cm H2O at low, conversational, and high pitches.7 The Cv in PTP for these pitches were 0.270, 0.207, and 0.433, respectively. Using a similar mechanical interruption device, Jiang et al. found the mean PTP of normal subjects to be 2.38 ± 1.27 cm H2O, 2.67 ± 1.87 cm H2O, and 2.98 ± 2.23 cm H2O at 75, 80, and 85 dB.10 The Cv in PTP at these SPL were 0.534, 0.700, and 0.748. Plant measured the PTP directly using percutaneous puncture of the cricothyroid membrane in five subjects, but no means or standard deviations were reported.11 Our estimates of PTP are slightly higher than those reported by Jiang et al., and this may be due to the fact that the apparatus measures the maximum SGP during a trial using pneumatic capacitance and subtracts the intraoral pressure during each interruption. Because subjects do not maintain perfectly consistent respiratory effort throughout the trial, SGP will vary as a function of time. The pneumatic capacitor measures the maximum SGP in the time-varying SGP series of the trial. While there is a single SGP measurement per trial, there are several phonation interruptions and accordingly several intraoral pressure measurements per trial. Thus, the differences between SGP and transglottal pressure may include a small systematic error making them slightly larger than actuality. However, this is only true if the SGP at the time of phonation interruption is significantly different from the measured SGP. Variation in SGP was minimized by frequently reminding subjects to maintain consistent respiratory effort and providing visual feedback of their current SPL throughout the trials. In addition, there were no statistically significant differences between the SGP measurements using the device and those measured directly in a tracheotomy patient (Figure 6). The Cv data suggest that our method is about as consistent as the intraoral pressure transducer method, and more consistent than the complete interruption technique pioneered by Jiang et al.10
The reliability of this method requires that the cessation of phonation be due to a decrease in transglottal pressure, rather than the active adduction of the vocal folds to close the glottis. It is important that subjects do not initiate interruption of phonation actively; in our study, this was easily avoided by randomizing the occurrence of interruptions within the trial. However, attention must be paid to ensure that adequate rest time exists between interruptions.
The current study presents a new method of PTP estimation with low intrasubject variability and wider application than previously published non-invasive estimation methods.10 Future research should investigate the reliability of this device in differentiating between PTP of normal and pathological voices. Recently, researchers have investigated a new parameter to quantify the aerodynamic input at phonation threshold: phonation threshold flow;21 however, no comparison of this new parameter to PTP in human subjects has been made. Studies should compare these two parameters in normal and pathological voices to contrast the sensitivities and specificities and determine if one parameter may be more clinically useful for detecting potentially abnormal laryngeal function. In addition, more research is needed to determine the latency times for laryngeal adductor reflexes elicited by mechanical interruption. While the air flow data from this study suggested that no such reflexes occurred using 0.200 s interruptions, studies quantifying these latency times would be valuable in determining the ideal phonation interruption time for maximizing airflow redirection while minimizing the probability of reflexes.
CONCLUSION
This study proposed a novel method for estimating PTP measurements in a non-invasive and clinically feasible way, using EGG to detect phonation cessation and airflow interruption-redirection into a pneumatic capacitor to determine SGP. The device was tested on 20 normal human subjects and testing on a tracheotomy patient suggested that this method was valid. Measurements using this device correspond well to previously reported values. Intrasubject variability, as measured by the coefficient of correlation, suggested that this method is reliable, and testing on a tracheotomy patient suggested this method is valid. Because PTP is a function of laryngeal biomechanical properties, this device may have clinical applications in indicating that laryngeal function is likely abnormal. However, more research is needed to establish the specificity and sensitivity of the device in differentiating between normal and pathological laryngeal states.
Acknowledgments
This research was supported by NIH grant number R01 DC008153 from the National Institute on Deafness and Other Communication Disorders.
References
- 1.Titze IR. The physics of small-amplitude oscillation of the vocal folds. J Acoust Soc Am. 1988;83:1536–1552. doi: 10.1121/1.395910. [DOI] [PubMed] [Google Scholar]
- 2.Titze IR, Schmidt SS, Titze MR. Phonation threshold pressure in a physical model of the vocal fold mucosa. J Acoust Soc Am. 1995;97:3080–3084. doi: 10.1121/1.411870. [DOI] [PubMed] [Google Scholar]
- 3.Jiang J, O’Mara T, Chen HJ, Stern JI, Vlagos D, Hanson D. Aerodynamic measurements of patients with Parkinson’s disease. J Voice. 1999;13:583–591. doi: 10.1016/s0892-1997(99)80012-5. [DOI] [PubMed] [Google Scholar]
- 4.Hirano S, Bless DM, Rousseau B, et al. Prevention of vocal fold scarring by topical injection of hepatocyte growth factor in a rabbit model. Laryngoscope. 2004;114:548–556. doi: 10.1097/00005537-200403000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Rousseau B, Tateya I, Lim X, Munoz-del-Rio A, Bless DM. Investigation of anti-hyaluronidase treatment on vocal fold wound healing. J Voice. 2006;20:443–451. doi: 10.1016/j.jvoice.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Solomon NP, DiMattia MS. Effects of a vocally fatiguing task and systemic hydration on phonation threshold pressure. J Voice. 2000;14:341–362. doi: 10.1016/s0892-1997(00)80080-6. [DOI] [PubMed] [Google Scholar]
- 7.Verdolini K, Titze IR, Fennell A. Dependence of phonatory effort on hydration level. J Speech Hear Res. 1994;37:1001–1007. doi: 10.1044/jshr.3705.1001. [DOI] [PubMed] [Google Scholar]
- 8.Scherer RC. Physiology of phonation: A review of basic mechanics. In: Ford CN, Bless DM, editors. Phonosurgery: Approaches to assessment and treatment. New York: Raven Press; 1991. pp. 77–93. [Google Scholar]
- 9.Isshiki N. Regulatory Mechanism of Voice Intensity Variation. J Speech Hear Res. 1964;128:17–29. doi: 10.1044/jshr.0701.17. [DOI] [PubMed] [Google Scholar]
- 10.Jiang J, O’Mara T, Conley D, Hanson D. Phonation threshold pressure measurements during phonation by airflow interruption. Laryngoscope. 1999;109:425–432. doi: 10.1097/00005537-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Plant RL, Freed GL, Plant RE. Direct measurement of onset and offset phonation threshold pressure in normal subjects. J Acoust Soc Am. 2004;116:3640–3646. doi: 10.1121/1.1812309. [DOI] [PubMed] [Google Scholar]
- 12.Kitzing P, Lofqvist A. Subglottal and oral air pressures during phonation-preliminary investigation using a miniature transducer system. Med Biol Eng. 1975;13:644–648. doi: 10.1007/BF02477320. [DOI] [PubMed] [Google Scholar]
- 13.Lofqvist A, Carlborg B, Kitzing P. Initial validation of an indirect measure of subglottal pressure during vowels. J Acoust Soc Am. 1982;72:633–635. doi: 10.1121/1.388046. [DOI] [PubMed] [Google Scholar]
- 14.McAllister A, Sundberg J. Data on subglottal pressure and SPL at varied vocal loudness and pitch in 8- to 11-year-old children. J Voice. 1998;12:166–174. doi: 10.1016/s0892-1997(98)80036-2. [DOI] [PubMed] [Google Scholar]
- 15.Kitajima K, Tanaka K. Intraoral pressure in the evaluation of laryngeal function. Acta Otolaryngol. 1993;113:553–559. doi: 10.3109/00016489309135862. [DOI] [PubMed] [Google Scholar]
- 16.Bard MC, Slavit DH, McCaffrey TV, Lipton RJ. Noninvasive technique for estimating subglottic pressure and laryngeal efficiency. Ann Otol Rhinol Laryngol. 1992;101:578–582. doi: 10.1177/000348949210100706. [DOI] [PubMed] [Google Scholar]
- 17.Jiang J, Stern J. Receiver operating characteristic analysis of aerodynamic parameters obtained by airflow interruption: a preliminary report. Ann Otol Rhinol Laryngol. 2004;113:961–966. doi: 10.1177/000348940411301205. [DOI] [PubMed] [Google Scholar]
- 18.Baggott CD, Yuen AK, Hoffman MR, Zhou L, Jiang JJ. Estimating subglottal pressure via airflow redirection. Laryngoscope. 2007;117:1491–1495. doi: 10.1097/mlg.0b013e318063e89e. [DOI] [PubMed] [Google Scholar]
- 19.Kearney PR, Poletto CJ, Mann EA, Ludlow CL. Suppression of thyroarytenoid muscle responses during repeated air pressure stimulation of the laryngeal mucosa in awake humans. Ann Otol Rhinol Laryngol. 2005;114:264–270. doi: 10.1177/000348940511400403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baken RJ, Orlikoff RF. Clinical Measurement of Speech and Voice. San Diego, CA: Singular Publishing Group; 2000. [Google Scholar]
- 21.Jiang JJ, Regner MF, Tao C, Pauls S. Phonation threshold flow in elongated excised larynges. Ann Otol Rhinol Laryngol. 2008;117:548–553. doi: 10.1177/000348940811700714. [DOI] [PMC free article] [PubMed] [Google Scholar]