Abstract
Due to global climate change, the world will, on average, experience a higher number of heat waves, and the intensity and length of these heat waves is projected to increase. Knowledge about the implications of heat exposure to human health is growing, with excess mortality and illness occurring during hot weather in diverse regions. Certain groups, including the elderly, the urban poor, and those with chronic health conditions, are at higher risk. Preventive actions include: establishing heat wave warning systems; making cool environments available (through air conditioning or other means); public education; planting trees and other vegetation; and modifying the built environment to provide proper ventilation and use materials and colors that reduce heat build-up and optimize thermal comfort. However, to inspire local prevention activities, easily understood information about the strategies' benefits needs to be incorporated into decision tools. Integrating heat health information into a comprehensive adaptation planning process can alert local decision-makers to extreme heat risks and provide information necessary to choose strategies that yield the largest health improvements and cost savings. Tools to enable this include web-based programs that illustrate effective methods for including heat health in comprehensive local-level adaptation planning; calculate costs and benefits of several activities; maps showing zones of high potential heat exposure and vulnerable populations in a local area; and public awareness materials and training for implementing preventive activities. A new computer-based decision tool will enable local estimates of heat-related health effects and potential savings from implementing a range of prevention strategies.
Keywords: Global climate, health effects, temperature, vulnerability, adaptation
1. Introduction
Heat related mortality and morbidity occurs across industrialized and less developed nations. Heat related mortality disproportionately affects lower socioeconomic status individuals, those without access to indoor air conditioning and the elderly.[1] With climate change, concern about increasing duration, intensity and frequency of heat waves[2] has added to the urgency of preparing properly to protect health during hot weather. This paper briefly reviews epidemiologic evidence on links between heat exposure and adverse health outcomes, discusses options for prevention of such outcomes, and describes the role of local authorities in implementing preventive activities. Next, we present an approach for developing a computer-based decision tool to enable local authorities to estimate how heat might impact the health of residents and to choose a range of potential strategies for mitigating these effects.
2. The epidemiology of heat and health
Excess mortality during hot weather has been reported in several epidemiological studies, and recent reviews assess that literature and the less extensive body of work on other health outcomes.[1, 3, 4] Other reports show associations between heat exposure and cause-specific hospital admissions,[5–7] but these can be inconsistent with the mortality associations in the same communities. [8, 9] The heat-related epidemiology literature has utilized case-control, case-crossover, case-control and time series approaches to estimate the health burden associated with relative and absolute measures of temperature variation.
The conclusions of these studies vary across geographical and political boundaries, but in general, excess temperature-associated mortality, including from extreme heat events, is expected to become more widespread geographically with increased climactic variation.[10] Several multi-city studies from around the world [11–19] show variations in heat-mortality associations. Community-specific models consistently illustrate different, typically non-linear, dose-response associations with U, J or V shapes that vary by location, e.g. [11].
Clearly, local characteristics of communities and populations affect differences in health vulnerability to heat. Often, acclimatization, whereby individuals living in higher temperature climates have different physiological responses to heat as well as cultural and social adaptive behaviors, plays a significant role in terms of who suffers and to what degree from heat-related illness. The predictors of vulnerability to heat-related mortality vary across the globe. [11, 13, 20, 21] European studies have shown increased risk for elderly women and, by contrast to the United States (U.S.), no difference by socio-economic position. Europeans have a much lower proportion of residential air conditioning [1], and the decreasing trend in heat-related mortality in the U.S. may be due to increased access to indoor air conditioning [16]. In general, morbidity and mortality associated with heat depends on age, race, sex, class, home characteristics, access to air conditioning, general health and living in an urban area versus a rural area.[6, 17, 22–25] Vulnerability has been noted particularly among children, pregnant women, older adults, impoverished populations, people with chronic health conditions, including diabetes, mobility and cognitive constraints, and outdoor workers.[26] Several strategies to prevent heat-related illness are informed by this knowledge base.
3. Preventive strategies
3.1 Heat health warning systems
The differences between communities in terms of climate, geography, and demographics illustrate the need for locally-tailored, short- and long-term intervention strategies. After the heat-waves in Chicago during the 1990’s and France during 2003 and 2006, improved access to cooling centers, increased air-conditioning prevalence, and heat health warning systems have been implemented. A heat health warning system is a ‘system that uses meteorological forecasts to initiate acute public health interventions designed to reduce heat-related impacts on human health during atypically hot weather’,[27] and interventions include media announcements, opening of cooling centers, home visits or telephone calls to vulnerable people, and website bulletins. Such interventions have been shown to reduce excess mortality [28], but true efficacy of these tools in reducing mortality and at which point they should be implemented requires further study.[1] Many cities are now implementing reverse 911 calls, where, for example, every home with a school child gets an automated call when school is delayed for snow or other reasons. Such a system could easily be extended to target vulnerable people during a heat warning.
3.2 Air conditioning
One proposed solution to reduce heat-related mortality and illness is to increase the use of air conditioning by individuals.[29] Cities in the U.S. with higher air conditioning prevalence have lower or no heat-related mortality [14, 18, 30]. During the 1995 Chicago heat wave, the odds of dying during the heat wave were 70% lower among individuals with working air conditioners than among individuals without working air conditioners [20]. Air conditioners may also offer the added benefit of reducing air-pollution-related mortality by filtering air [31]. However, air conditioners are not a viable heat adaptation strategy during power outages. Air conditioners also emit heat during use, raising the ambient temperature, and often use electricity generated by fossil fuel burning power plants. These plants release air pollutants and greenhouse gasses. The former may result in a net increase in mortality [37], respiratory, and cardiovascular disease [38]; the latter may exacerbate the need for adaptation measures. Cooling centers may provide air conditioning more efficiently and reach a larger number of people unable to afford air conditioning in their own homes. However, cooling centers as a heat mitigation strategy require that individuals have transportation to and recognize when they need to go to the centers. Other heat mitigation strategies have focused on the design of urban areas, as described next.
3.3 Increasing albedo and planting trees
Studies of the urban heat island effect (whereby air temperatures in an urban area are 1–5° C, higher than in a nearby rural area) have shown that the albedo, or reflectivity, of an urban area is one of the most important determinants of the magnitude of the heat island. [32, 33] Simulation studies of reductions in city-wide albedo produced modest, though significant, reductions in air temperature of 1–3.5° C. [34–37]
Increasing the canopy cover may also reduce air temperature by 1–3° C. [38, 39] Green roofs, or plantings on roofs, may also decrease the urban heat island effect and decrease storm water runoff and building energy use.[40] Increasing albedo and vegetation may also reduce ground-level ozone and lower energy costs associated with air conditioning use. [37, 38]
Some simpler models of these effects, for use by planners and policy makers, have been developed. A preliminary resource is the Urban Heat Island Mitigation Impact Screening Tool (MIST).[41] This simplified tool allows the user to select from 170 U.S. cities and enter changes in albedo and vegetation to estimate effects on air temperature, ozone and energy use. Other simple models estimating the change in heat island intensity associated with changes in urban features include an energy balance model [42] and a modified version of an air pollution model (TAPM).[34] These models do not estimate economic or health benefits, and little research exists comparing costs and benefits of these mitigation strategies in terms of health care savings and potential decreases in mortality.
3.4 The role of local action
Given that extreme heat events and their impacts on health and well-being generally take place at the local level, the involvement of local decision-makers is critical in recognizing the risk to their communities and effectively deploying preventive measures during hot weather. Local governments may underestimate the risk of extreme heat events because they may be more subtle and insidious than more dramatic events such as hurricanes or floods; but given the high degree of certainty that temperatures will rise overall and lead to more intense and frequent extreme heat events, and the high likelihood that this will lead to more heat-related illnesses and death, this recognition is vital. Unlike other climate impacts that may require costly long-term adaptation measures, such as building sea walls or moving infrastructure to cope with anticipated sea level rise, multiple effective and relatively low-cost preventive measures can be taken by local governments to reduce risk during hot weather. These preventive measures can be classified as short-term education and public health response systems, such as education campaigns regarding heat stress symptoms and heat health warning systems. Additionally, long-term program infrastructure improvements that lower heat in communities (such as urban heat island mitigation and tree planting) can be implemented.
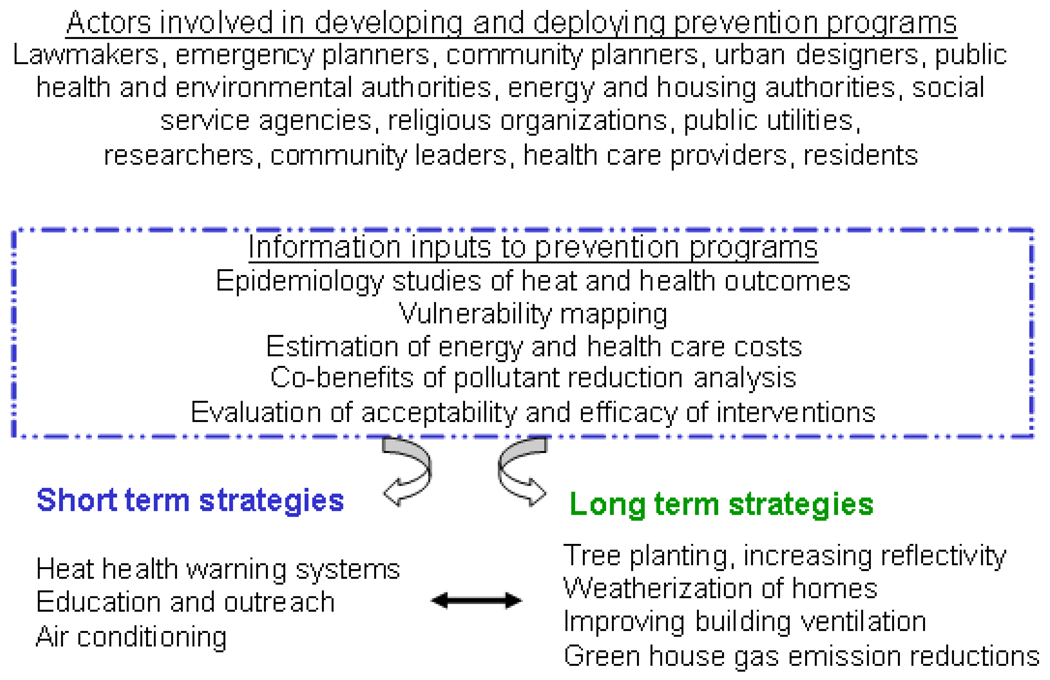
Using dynamic, evidence-based tools in planning for extreme heat events can provide helpful information for short term and long term strategies to reduce morbidity and mortality related to heat. These tools can be used on a national as well as local level by community leaders, public health officers, emergency planners and urban planners. Information such as epidemiologic analyses and qualitative studies can inform short-term strategies for a given area. Data that can inform these short-term strategies also includes vulnerability mapping, and the costs and benefits of using air conditioning given its influence on both energy use and air pollution. Long-term measures can complement the short-term measures where they share similar goals.
Figure 1 provides a diagram of the variety of actors and information needed to inform development of these prevention programs. We next discuss decision tools available to inform these local preventive programs
Figure 1.
Local prevention of heat related morbidity and mortality
4. Decision tools
Decision-tools can help communities better understand location-specific heat-health associations and vulnerabilities, and the available infrastructure for implementing prevention programs. Such tools ideally allow for use of community-specific information on heat-health associations, population characteristics, settlement patterns, transportation, energy use, climate and other factors.
4. 1 Quantifying health benefits of specific actions
An adaptable framework for evaluating short- and long-term intervention strategies to reduce heat-related illness exists in the Climate and Air Pollution Planning Assistant (CAPPA) decision tool.[43] This tool, developed for use by local government agencies, produces estimates of cost-savings and air pollutant reductions related to “green” infrastructure improvements in communities. Recent work has shown that sustainability initiatives aimed at reducing energy consumption in communities may have a positive benefit on human health by reducing heat-related, air pollution, and infectious disease. [44]. Currently, the CAPPA tool lacks a human health component. The U.S. Environmental Protection Agency has, however, developed a tool for evaluating health benefits of pollution reductions, and an extension to health benefits related to heat exposure reduction is conceivable.[45]
4.2 Vulnerability mapping
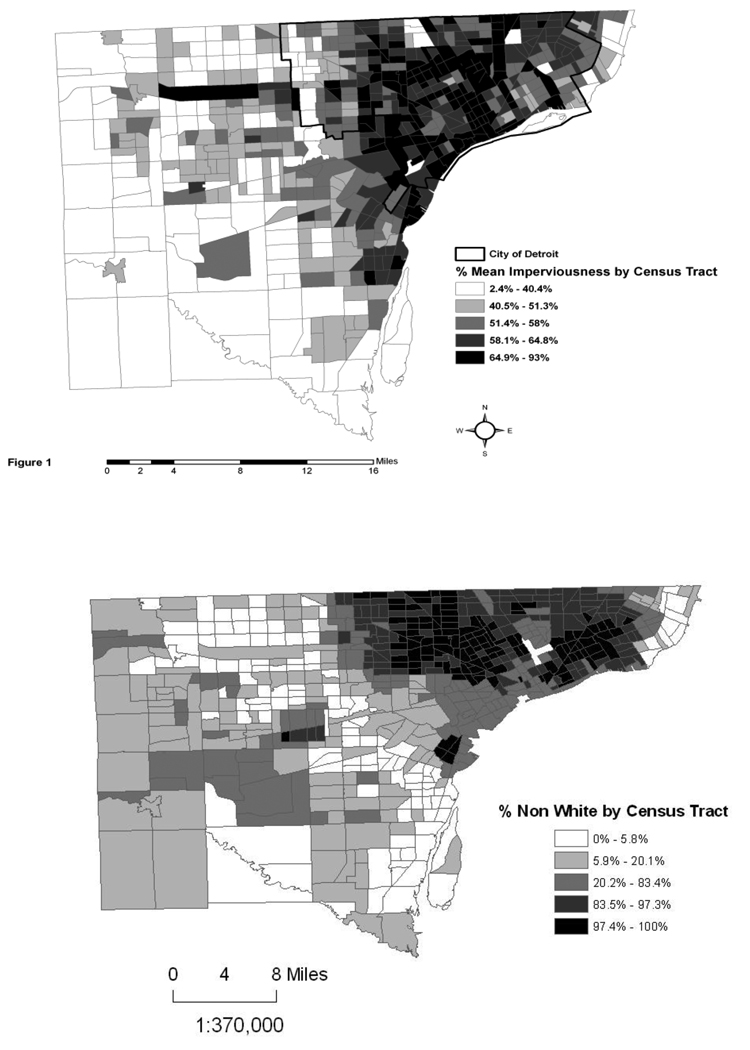
Vulnerability mapping can be used to help visualize risk to certain populations within a community. Vulnerability is defined in one instance as the summation of all risk and protective factors that ultimately determine whether an individual or subpopulation experiences adverse health outcomes.[26] In the case of heat, both potential exposure to heat, as indicated by land cover and air conditioning availability, and potential individual susceptibilities, as indicated by age and chronic health conditions, can be inputs into a vulnerability map.[46] Targeting the most vulnerable in a population can help direct implementation of prevention programs and decisions about what strategies are most beneficial. For example, the social vulnerability in the city of Chicago from 2004 to 2007 was examined by mapping census tract demographic variables, crime incident data and heat related dispatches to determine which variables, if any, were correlated with heat related illness.[25] Most cities are inadequately informed on where the most vulnerable people live and which areas of a city are most at risk for an extreme heat event.[47] Geographic and geospatial technologies can help identify who is most at risk.
A simple example of data inputs for vulnerability mapping is shown in the Figure 2 for Wayne County, Michigan, U.S. Overlaying maps with various information, such as land cover data (% imperviousness), with various census tract variables that relate to vulnerable populations (below the poverty line, non-white), gives an idea where social vulnerability may intersect with higher heat exposure potential. Vulnerability mapping can include socioeconomic variables, thermal remote sensing resources, numbers of heat-related dispatch calls, and surveillance programs that record chronic disease prevalence from a certain area.
Figure 2.
Potential vulnerability mapping inputs: Quintiles of percentage mean impervious surface by census tract from the 2001 National Land Cover Data (satellite images), and quintiles of percent non-white population (a variable highly correlated with socioeconomic disadvantage in the U.S.) from the 2000 U.S. Census, Wayne County, Michigan USA
4.3 Other web-based tools
Fourteen universities in the United Kingdom are participating in a multi-institutional research program to produce a decision based tool about extreme weather events.[48] The Crew, or Community Resilience to Extreme Weather, is developing a tool kit to support decision making and improve community capacity to adapt to extreme weather. A set of web-based tools will enable mapping of potential future weather events, assessing their impacts under various scenarios and evaluating a range of coping measures, as described at www.extreme-weather-impacts.net. This is just one example of an effort to gather information from multiple disciplines and apply it to tools to support local programming.
5. A new decision tool for developing local heat illness prevention programs
As part of a similar multi-disciplinary collaboration between researchers and local governments, we propose to integrate information about heat health vulnerability, risk and adaptation options into a new computer-based interactive tool designed to guide local governments through a comprehensive adaptation planning and implementation process. This new tool, being developed by International Council for Local Environmental Initiatives (ICLEI)-Local Governments for Sustainability USA and tentatively titled the Resiliency Planning Workbook Series, will guide local government decision makers and emergency planning agencies through an adaptation planning process known as the Five Milestones for Climate Adaptation. (Table 1) Heat health will be featured as a detailed example throughout the Five Milestone process, to insure that local governments consider this issue as they work towards developing and implementing a robust climate adaptation plan.
Table 1.
ICLEI USA's Five Milestones for Adaptation as described in Preparing for Climate Change: A Guidebook for Local, Regional and State Governments*
| MILESTONE 1: Initiate your climate resiliency effort |
| •Scope the climate change impacts expected in your region |
| •Pass a resolution or administrative order directing your government to prepare for climate change |
| •Build and maintain support to prepare for climate change |
| •Build your climate change preparedness team |
| •Identify your planning areas relevant to climate change impacts |
| MILESTONE 2: Conduct a climate resiliency study |
| •Analyze the change climate impacts to your major sectors |
| •Conduct a climate change vulnerability assessment |
| •Conduct a climate change risk assessment |
| •Prioritize planning areas for action |
| MILESTONE 3: Prioritize adaptation actions and develop implementation plan |
| •Develop, select and prioritize your preparedness actions |
| •Create a plan to fund and carry out actions |
| MILESTONE 4: Implement your preparedness plan |
| •Ensure that you have the right implementation tools |
| MILESTONE 5: Measure your progress and update your plan |
| •Track progress toward meeting implementation goals |
| •Update your plan to reflect experience and new information |
The Guidebook was produced by ICLEI USA in collaboration with the Climate Impacts Group at the University of Washington and staff of King County, Washington, with funding from the National Oceanic and Atmospheric Association (NOAA) http://www.icleiusa.org/library/documents/action-center/Adaptation_Guidebook.pdf
In Milestone 1, when local governments form an adaptation planning and implementation team, they are prompted to recognize that public health impacts will be an important aspect of effective climate change adaptation, and to include public health officials on their adaptation planning team.
In Milestone 2, local governments assess which impacts they are vulnerable to and which groups and locations within their communities are most at risk, and prioritize the impacts they will focus on in the near-, mid-, and long-terms. Excessive heat will be included as a detailed example to illustrate how local governments can include this impact in their assessment.
The example will involve compiling data from published epidemiologic studies estimating the percent increase in mortality and morbidity (hospital admissions and emergency room admissions) for each degree increase in temperature. We will divide U.S. localities into five climate regions using the mean annual temperature as a criterion, since prevailing climate in an area is a determinant of how sensitive a population's health is to given absolute or relative temperatures and weather conditions. Then we will average the health effect estimates from localities belonging to each region using meta-analysis techniques to provide an overall estimate of percent excess deaths and hospital admissions associated with hotter temperatures for each region. By obtaining the baseline mortality and morbidity rates (events per day) for a large number of communities in the U.S., and multiplying this baseline by the percent excess corresponding to the each community's climate region, we can quantify the estimated excess deaths and illnesses related to heat.
Then, in Milestone 3, local governments will assess their options for adapting to the impacts they have identified as priorities. Options for preventing or reducing heat-related illness and death, and guidance in choosing the right options will be provided, with a detailed example of how to include such measures in their climate resiliency plan. Heat health will also be featured as a detailed example in the workbooks for Milestone 4, implementing the plan, and Milestone 5, monitoring and evaluating.
Once the heat health example and supporting information are developed and integrated into the workbooks, we intend to convene meetings, in person and using virtual technology, to introduce this tool to potential users and provide guidance on implementing both the short-term prevention programs and urban infrastructure interventions. In the long-term, the goal is to have the tool accessible on the web so that it could be used by communities around the world; currently, the focus is on U.S. communities.
Further results of this study will be integrated into the guidance provided in the workbook as follows: We will roughly estimate how particular measures might reduce these health impacts according to the amount by which each particular strategy is able to lower temperature. The workbook user will then select his/her region of the country, quantify the benefits of measures that reduce ambient air temperature and compare these benefits to the costs of implementing such measures, for which estimates will be provided. Table 2 is a prototype of the kind of information that a user might be able to view after putting in their locale-specific information.
Table 2.
Example of decision-tool fields with example estimates that might be calculated by or made available to a local decision-maker for evaluating the costs and benefits of mitigation activities
| Mitigation activities |
||||||
|---|---|---|---|---|---|---|
| Costs and benefits | Tree Planting |
Cooling Centers |
Reflective Paving |
Reflective Roofing |
Increased air conditioning |
Heat health warning system |
| Heat exposure reduction (°C) | −3 | −5 | −4 | −3 | −5 | −3 |
| Air pollution (e.g., PM10, in µg/m3) | −5 | +5 | −1 | −1 | +7 | +1 |
| Mortality reduction (% drop per °C) | −3 | −5 | −4 | −3 | −5 | −3 |
| Health cost savings in dollars | 4 | 5 | 3 | 2 | 6 | 7 |
| Energy cost or savings in dollars | 5 | −2 | 2 | 2 | −5 | −1 |
| Net cost or benefit* | ||||||
This would be calculated by combining the above variables and other information for each activity based on local conditions. Numbers shown are just for the purpose of illustrating potential estimates.
6. Discussion and conclusions
Ample evidence exists that exposure to high temperatures can result in a variety of adverse health effects, including death, and preventing such effects requires a range of intervention types. With climate change increasing the frequency of hot weather, among other effects, multiple collaborations worldwide are attempting to apply research results to prevention efforts that are both sustainable and effective at the local level.
Some of the challenges inherent in this type of work, and specifically to developing decision tools of the sort we have described, include:
quantifying the temperature exposure reductions from certain interventions; this is much less straightforward than quantifying air pollution exposure reductions, which is in itself challenging
weighing the benefits of air conditioning in reducing heat exposure with its energy, health and environmental costs
properly communicating uncertainty about estimates of these benefits to local decision-makers
projecting how societies will adapt to climate change
assigning a value to health care cost savings and lives saved
These challenges are discussed in more detail in recent publications.[49, 50], and further research in these areas will assist in moving the field forward. In spite of such challenges, the proliferation of multidisciplinary collaborations and public programs to prepare for climate change is testament to the need for all sectors to work together to improve health and environmental sustainability, both related to heat exposure and other conditions.
Acknowledgments
Competing interests and funding information
All authors have seen and approved the final version and none of the authors have conflicts of interest to declare. Funding was provided by U.S. Environmental Protection Agency Science to Achieve Results (STAR) Program grant R832752010 and grant R01ES016932 from the National Institute of Environmental Health Sciences.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions
All authors participated in the paper with contributions detailed next. Marie O’Neill, Jonathan Kish, Carina Gronlund and Jalonne White-Newsome made the first draft of the manuscript and prepared the figures. Rebecca Carter developed Table 1. Xico Manarolla, Rebecca Carter, Joel Schwartz and Antonella Zanobetti participated with the rest of the team in structuring the paper and developing the ideas described in the manuscript. All authors provided comments and suggestions and assisted with editing the manuscript.
References
- 1.Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health. 2008;29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. [DOI] [PubMed] [Google Scholar]
- 2.Meehl GA, Tebaldi C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science. 2004;305:994–997. doi: 10.1126/science.1098704. [DOI] [PubMed] [Google Scholar]
- 3.Gosling S, Lowe J, McGregor G, Pelling M, Malamud B. Associations between elevated atmospheric temperature and human mortality: a critical review of the literature. Climate Change. 2009;92(3):299–341. [Google Scholar]
- 4.O'Neill M, Ebi K. Temperature extremes and health: impacts of climate variability and change in the United States. J Occup Environ Med. 2009 Jan;51(1):13–25. doi: 10.1097/JOM.0b013e318173e122. [DOI] [PubMed] [Google Scholar]
- 5.Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, et al. The 2006 California heat wave: Impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117:61–67. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michelozzi P, Accetta G, De Sario M, D'Ippoliti D, Marino C, Baccini M, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Resp Crit Care Med. 2009 Mar 1;179(5):383–389. doi: 10.1164/rccm.200802-217OC. [DOI] [PubMed] [Google Scholar]
- 7.Hansen AL. The effect of heat waves on hospital admissions for renal disease in a temperate city of Australia. Int J Epidemiol. 2008 doi: 10.1093/ije/dyn165. [DOI] [PubMed] [Google Scholar]
- 8.Nitschke M, Tucker GR, Bi P. Morbidity and mortality during heatwaves in metropolitan Adelaide. Med J Australia. 2007;187(11–12):662–665. doi: 10.5694/j.1326-5377.2007.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 9.Kovats RS, Hajat S, Wilkinson P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup Environ Med. 2004;61(11):893–898. doi: 10.1136/oem.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frumkin H, Hess J, Luber G, Malilay J, McGeehin M. Climate Change: The Public Health Response. Am J Public Health. 2008 March 1;98(3):435–445. doi: 10.2105/AJPH.2007.119362. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McMichael AJ. International study of temperature, heat and urban mortality: the 'ISOTHURM' project. Int J Epidemiol. 2008;37(5):1121–1131. doi: 10.1093/ije/dyn086. [DOI] [PubMed] [Google Scholar]
- 12.Michelozzi P, De Sario M, Accetta G, de'Donato F, Kirchmayer U, D'Ovidio M, et al. Temperature and summer mortality: geographical and temporal variations in four Italian cities. J Epidemiol Comm Health. 2006 May;60(5):417–423. doi: 10.1136/jech.2005.040857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell ML. Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol. 2008;37(4):796–804. doi: 10.1093/ije/dyn094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson GB, Bell ML. Weather-related mortality: A study of how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20(2):205–213. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baccini M, Biggeri A, Accetta G, Kosatsky T, Katsouyanni K, Analitis A, et al. Heat effects on mortality in 15 European cities. Epidemiology. 2008 Sep;19(5):711–719. doi: 10.1097/EDE.0b013e318176bfcd. [DOI] [PubMed] [Google Scholar]
- 16.Barnett AG. Temperature and cardiovascular deaths in the US elderly. Epidemiology. 2007;18:369–372. doi: 10.1097/01.ede.0000257515.34445.a0. [DOI] [PubMed] [Google Scholar]
- 17.Medina-Ramon M, Zanobetti A, Cavanagh DP, Schwartz J. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect. 2006;114(9):1331–1336. doi: 10.1289/ehp.9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect. 2002;110:859–863. doi: 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hajat S, Armstrong BG, Gouvia N, et al. Mortality displacement of heat-related deaths: a comparison of Delhi, Sao Paulo and London. Epidemiology. 2005;16:613–620. doi: 10.1097/01.ede.0000164559.41092.2a. [DOI] [PubMed] [Google Scholar]
- 20.Semenza JC, Rubin CH, Falter KH, et al. Heat-related deaths during the July 1995 heat wave in Chicago. New Engl J Med. 1996;335:84–90. doi: 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- 21.Canouï-Poitrine F, Cadot E, Spira A. Excess deaths during the August 2003 heat wave in Paris, France. Rev Epidemiol Sante Publique. 2006;54(2):127–135. doi: 10.1016/s0398-7620(06)76706-2. [DOI] [PubMed] [Google Scholar]
- 22.Harlan SL, Brazel AJ, Prashad L, Stefanov WL, Larsen L. Neighborhood microclimates and vulnerability to heat stress. Soc Sci Med. 2006;63(11):2847. doi: 10.1016/j.socscimed.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 23.O'Neill MS, Zanobetti A, Schwartz J. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol. 2003;157(12):1074–1082. doi: 10.1093/aje/kwg096. [DOI] [PubMed] [Google Scholar]
- 24.O'Neill MS, Zanobetti A, Schwartz J. Disparities by race in heat-related mortality in four U.S. cities: The role of air conditioning prevalence. J Urban Health. 2005;82:191–197. doi: 10.1093/jurban/jti043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sister C, Golden J, Chuang W-C, Hartz D. Mapping Social Vulnerability to heat wave in Chicago. The 89th American Meteorological Society Annual Meeting; Phoenix, AZ. 2009. [Google Scholar]
- 26.Balbus JM. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med. 2009;51(1):33–37. doi: 10.1097/JOM.0b013e318193e12e. [DOI] [PubMed] [Google Scholar]
- 27.Kovats RS, Ebi KL. Heatwaves and public health in Europe. Eur J Public Health. 2006;16(6):592–599. doi: 10.1093/eurpub/ckl049. [DOI] [PubMed] [Google Scholar]
- 28.Fouillet A, Rey G, Wagner V, Laaidi K, Empereur-Bissonnet P, Le Tertre A, et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int J Epidemiol. 2008 Apr;37(2):309–317. doi: 10.1093/ije/dym253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Keatinge WR. Death in heat waves: simple preventive measures may help reduce mortality. BMJ. 2003;327:512–513. doi: 10.1136/bmj.327.7414.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chestnut L, Breffle WS, Smith JB, Kalkstein LS. Analysis of the differences in hot-weather-related mortality across 44 U.S. metropolitan areas. Environ Sci & Policy. 1998;1(1):59–70. [Google Scholar]
- 31.Janssen N, Schwartz J, Zanobetti A, Suh H. Air conditioning and source-specific particles as modifiers of the effect of PM(10) on hospital admissions for heart and lung disease. Environ Health Perspect. 2002;110(1):43–49. doi: 10.1289/ehp.0211043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kolokotroni M, Giridharan R. Urban heat island intensity in London: An investigation of the impact of physical characteristics on changes in outdoor air temperature during summer. Solar Energy. 2008;82(11):986–998. [Google Scholar]
- 33.Lynn BH, Carlson TN, Rosenzweig C, Goldberg R, Druyan L, Cox J, et al. A Modification to the NOAH LSM to Simulate Heat Mitigation Strategies in the New York City Metropolitan Area. J Appl Meteorol Climatol. 2009 Feb;48(2):199–216. [Google Scholar]
- 34.Coutts AM, Beringer J, Tapper NJ. Investigating the climatic impact of urban planning strategies through the use of regional climate modelling: a case study for Melbourne, Australia. Int J Climatol. 2008 Nov;28(14):1943–1957. [Google Scholar]
- 35.Rizwan AM, Dennis LYC, Liu C. A review on the generation, determination and mitigation of Urban Heat Island. J Environ Sciences. 2008;20(1):120–128. doi: 10.1016/s1001-0742(08)60019-4. [DOI] [PubMed] [Google Scholar]
- 36.Synnefa A, Dandou A, Santamouris M, Tombrou M, Soulakellis N. On the Use of Cool Materials as a Heat Island Mitigation Strategy. J Appl Meteorol Climatol. 2008 Nov;47(11):2846–2856. [Google Scholar]
- 37.Taha H. Meso-urban meteorological and photochemical modeling of heat island mitigation. Atmos Environ. 2008 Dec;42(38):8795–8809. [Google Scholar]
- 38.Akbari H. Shade trees reduce building energy use and CO2 emissions from power plants. Environmental Pollution. 2002;116 Supp 1:S119–S126. doi: 10.1016/s0269-7491(01)00264-0. [DOI] [PubMed] [Google Scholar]
- 39.Taha H. Modeling impacts of increased urban vegetation on ozone air quality in the South Coast air basin. Atmos Environ. 1996;30(20):3423–3430. [Google Scholar]
- 40.Rosenzweig C, Gaffin S, Parshall LE. Green Roofs in the New York Metropolitan Region: Research Report. New York: Columbia University Center for Climate Systems Research and NASA Goddard Institute for Space Studies; 2006. [Google Scholar]
- 41.Sailor DJ, Dietsch N. The urban heat island Mitigation Impact Screening Tool (MIST) Environmental Modelling & Software. 2007;22(10):1529–1541. [Google Scholar]
- 42.Silva HR, Bhardwaj R, Phelan PE, Golden JS, Grossman-Clarke S. Development of a Zero-Dimensional Mesoscale Thermal Model for Urban Climate. J Appl Meteorol Climatol. 2009 Mar;48(3):657–668. [Google Scholar]
- 43.ICLEI. [Accessed July 27, 2009];Climate and Air Pollution Planning Assistant. 2009 http://wwwicleiusaorg/action-center/tools/decision-support-tool.
- 44.Frumkin H, McMichael AJ, Hess JJ. Climate Change and the Health of the Public. Am J Prev Med. 2008;35(5):401–402. doi: 10.1016/j.amepre.2008.08.031. [DOI] [PubMed] [Google Scholar]
- 45.EPA. Environmental Benefits Mapping and Analysis Program (BenMAP) 2009 doi: 10.1080/15287390600884982. http://wwwepagov/air/benmap/ [DOI] [PubMed]
- 46.Reid C, O'Neill M, Gronlund C, Brines S, Brown D, Diez-Roux A, et al. Mapping Community Determinants of Heat Vulnerability Environ Health Perspect. 2009 doi: 10.1289/ehp.0900683. doi:10.1289/ehp.0900683( http://ehp.niehs.nih.gov/docs/2009/0900683/abstract.html). [DOI] [PMC free article] [PubMed]
- 47.Costello A. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373(9676):1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 48.Goodier CI, Wood GA, Shao L. Briefing: Community Resilence to Extreme Weather. Institution of Civil Engineers; 2008. pp. 97–99. [Google Scholar]
- 49.Kinney PL, O’Neill MS, Bell ML, Schwartz J. Approaches for estimating effects of climate change on heat-related deaths: Challenges and opportunities. Environ Sci Policy. 2008;11(1):87–96. [Google Scholar]
- 50.Bell ML. Ancillary human health benefits of improved air quality resulting from climate change mitigation. Environ Health. 2008;7:41. doi: 10.1186/1476-069X-7-41. [DOI] [PMC free article] [PubMed] [Google Scholar]