Abstract
Purpose
Cancer survivors exposed to anthracyclines experience an increased risk of cardiovascular (CV) events. We hypothesized that anthracycline use may increase aortic stiffness, a known predictor of CV events.
Patients and Methods
We performed a prospective, case-control study involving 53 patients: 40 individuals who received an anthracycline for the treatment of breast cancer, lymphoma, or leukemia (cases), and 13 age- and sex-matched controls. Each participant underwent phase-contrast cardiovascular magnetic resonance measures of pulse wave velocity (PWV) and aortic distensibility (AoD) in the thoracic aorta at baseline, and 4 months after initiation of chemotherapy. Four one-way analyses of covariance models were fit in which factors known to influence thoracic aortic stiffness were included as covariates in the models.
Results
At the 4-month follow-up visit, aortic stiffness remained similar to baseline in the control participants. However, in the participants receiving anthracyclines, aortic stiffness increased markedly (relative to baseline), as evidenced by a decrease in AoD (P < .0001) and an increase in PWV (P < .0001). These changes in aortic stiffness persisted after accounting for age, sex, cardiac output, administered cardioactive medications, and underlying clinical conditions known to influence aortic stiffness, such as hypertension or diabetes (P < .0001).
Conclusion
A significant increase in aortic stiffness occurs within 4 months of exposure to an anthracycline which was not seen in an untreated control group. These results indicate that previously regarded cardiotoxic cancer therapy adversely increases thoracic aortic stiffness, a known independent predictor of adverse cardiovascular events.
INTRODUCTION
Injury to the left ventricular (LV) myocardium, reduction of LV ejection fraction (LVEF), and precipitation of congestive heart failure (CHF)1–5 can occur in the weeks to months after receipt of anthracycline therapy. In addition, latent cardiovascular disease (including myocardial infarction [MI], cardiac death, stroke, and CHF)6 is emerging (5 to 10 years after receipt of anthracyclines) in patients surviving breast cancer or a hematologic malignancy (leukemia or lymphoma). These late adverse cardiovascular outcomes are increasing in prevalence as patients attain higher cancer cure rates.
In other patient populations, such as those with hypertension, diabetes, or advanced age,7–9 abnormally increased stiffness of the thoracic aorta has been implicated in the pathophysiology of MI, stroke, and late-onset CHF.7–9 Stiffening of the aorta increases LV afterload and serves as a potent stimulus for LV hypertrophy. In fact, increased aortic stiffness is an independent predictor of adverse cardiovascular events even after accounting for the Framingham risk score.7–9
Because cancer survivors receiving regimens containing anthracyclines experience an increased risk of MI, stroke, and CHF, we hypothesized that the administration of cancer treatment regimens containing anthracyclines could increase stiffness within the thoracic aorta. To test this hypothesis, we performed a case-control study in individuals receiving anthracycline treatment for breast cancer, leukemia, or lymphoma (cases), and in relatively healthy age- and sex-matched individuals without cancer treatments (controls). In both groups, we measured thoracic aortic stiffness at two time points separated by 4 months.
PATIENTS AND METHODS
Study Population and Design
This study was approved by the institutional review board of the Wake Forest University School of Medicine; all participants provided informed consent. The study population consisted of 53 participants; 40 (age 24 to 65 years with 50% ≥ 50 years of age) were recruited from the hematology and oncology clinic and inpatient hospital and were scheduled to receive anthracyclines. Other potentially cardiotoxic therapy could be coadministered including trastuzumab or cyclophosphamide.1–5 The control group (n = 13; 62% ≥ 50 years of age; range, 24 to 65 years of age) included community-dwelling adult volunteers recruited by mail, age-matched to the participants, and without clinical or documented evidence of cardiovascular or cardio-respiratory diseases. Participants were ineligible for enrollment into either group if they had a contraindication to cardiovascular magnetic resonance (CMR) imaging (implanted metal or electronic devices) or had received prior treatment for cancer.
All participants underwent CMR examinations twice, each session separated by 3.6 ± 0.8 months. In patients receiving cancer therapy, the first CMR examination was performed before receipt of any cancer treatment, and the subsequent examination was performed 4 months after initiation of treatment. Acquired images were transferred to workstations for determination of aortic stiffness, cardiac output, LV volumes (LVV), and LVEF. All studies were analyzed by individuals blinded to participant identifiers, study group, and the date or results of the other CMR examination (a blinded, unpaired read).
CMR Technique and Measurements
Phase-contrast cardiovascular magnetic resonance (PC-CMR)10–12 studies were performed according to previously published techniques at 1.5 tesla using either a Magnetom Avanto Scanner (Siemens, Munich, Germany) or a Signa Twinspeed Scanner (General Electric Medical Systems, Waukesha, WI). Images of the proximal thoracic aorta were obtained in an axial cross-sectional plane placed at the pinnacle of the main pulmonary artery (identified with a sagittal localizer). PC-CMR imaging parameters included a 34- to 36-cm field of view, a 256 × 192 matrix, a 10-ms repetition time, a 3- to 5-ms echo time, a 15- to 20-degree flip angle, an 8-mm thick slice, and a through-plane velocity encoding of 150 cm/sec.10–12 A nonferromagnetic brachial blood pressure (BP) cuff was applied to record BP during the PC-CMR image acquisition.10,11 In addition to measurements of aortic stiffness, we also acquired measurements of LVV and LVEF, according to previously published techniques.10,13 These sequences incorporated steady-state free-precession cine white blood imaging techniques in which a series of short axis slices were positioned across the LV apical four-chamber view beginning at the LV base and terminating at the LV apex. Imaging parameters included a 34-cm field of view, a 10-ms repetition time, a 4-ms echo time, a 20-degree flip angle, an 8-mm thick slice with a 2-mm interslice gap, a 256 × 160 matrix, and a 32-kHz bandwidth.
Arterial Stiffness Analysis
All images were analyzed according to previously published techniques10–12 and were transferred to a processing work station where the boundary of the aortic lumen was defined on the magnitude image of the reference scan by manually tracing a region of interest. To precisely trace the boundary of the flow lumen, each image was magnified by 400% to 800%. Thoracic aortic distensibility (AoD) and pulse wave velocity (PWV) were determined according to the previously used formulas displayed in Figure 1.10–12 In addition to determination of aortic stiffness, cardiac output was measured according to previously published techniques.13,14
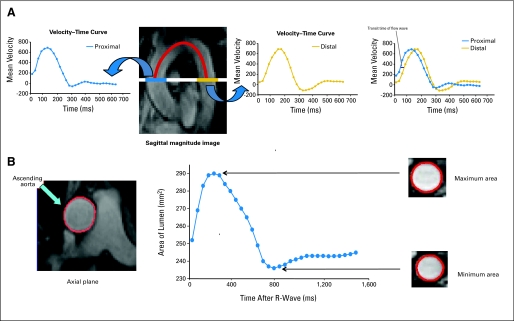
Fig 1.
(A) Sagittal magnitude image of the thoracic aorta was used to select the axial plane at the level of pulmonary artery and perpendicular to aortic flow (solid white line). The distance between ascending and descending thoracic aorta was obtained by tracing the centerline of the aortic lumen (red line). The two velocity–time curves are shown across the thoracic aorta. The sagittal magnitude image demonstrates the velocity–time curves for the ascending and descending thoracic aorta. Transit time of the flow wave was computed on the basis of the upstroke time difference of the velocity–time curve at two different regions (blue line). The location of the best cross-correlation of two partial upstroke velocity curves was used to estimate the time delay. Pulse wave velocity (PWV) was calculated by dividing the distance between the ascending and descending thoracic aorta by the transit time of the flow wave. (B) After slice selection from the initial sagittal images, axial phase-contrast cardiovascular magnetic resonance of the ascending and proximal descending thoracic aorta was obtained. From these images, maximum and minimum aortic areas over the cardiac cycle were determined by manually tracing the region of interest (red boundaries). Distensibility was then calculated by dividing relative change in aortic area by pulse pressure multiplied by the resting area at end-diastole.
Determination of LVVs and LVEF
LVVs and LVEF were measured according to previously published techniques.10,15 To determine LVV, the endocardial border of the LV cavity was traced at end-diastole and end-systole for each short-axis slice and then calculated by summation using Simpson's rule. The LVEF was calculated from the ratio of the difference between the LV end-diastolic volume (LVEDV) and LV end-systolic volume (LVESV) divided by LVEDV. Volume indices were calculated by dividing the LVEDV, LVESV, or LV stroke volume by the body surface area.
Statistical Analysis
The baseline population characteristics of the participants in the control and case groups were compared using t tests (for continuous variables) or χ2 tests (for categoric variables). To examine differences between groups on the primary outcome measures of AoD and PWV, a series of analysis of covariance (ANCOVA) models were fit. Initially, a simple ANCOVA model was fit for each outcome where the baseline value of that outcome (PWV or AoD) was the covariate in the model, and the group indicator (Cancer, yes/no) was the factor of interest. Next, adjusted models were fit that included the following additional covariates that have previously been associated with aortic stiffness: age, sex, body mass index, systolic BP, serum hemoglobin, medication use, and the presence of hypertension, diabetes, or hyperlipidemia. Finally, an overall model was fit with all baseline covariates (mentioned above), the cardiac output during the PC-CMR acquisition, and the baseline CMR outcomes included to ensure that the baseline differences would not influence potential differences in follow-up CMR outcomes. Correlation analyses were performed to determine whether the type or cumulative dose of cancer therapy medications was associated with any of the CMR outcomes. In addition, to examining the potential effect of sex, we refit our models for PWV and AoD stratified by sex. To compare the two groups (cases and controls) in regard to the hemodynamic data and the outcome measurements of LVV, t tests were used. Unless noted otherwise, all data are reported as mean ± standard deviation. All tests were two-tailed, and P values less than .05 were considered statistically significant with 80% power to detect a difference between cases and controls equivalent to 0.91 standard deviations of the measure of variations, assuming a two-sided test and alpha = .05. Analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC).
RESULTS
CMR procedures were accomplished in less than 30 minutes in all participants; demographic data are displayed in Table 1. The time between the first and second examinations for participants receiving (cases) versus not receiving (controls) cancer therapy were similar (3.5 ± 1 months and 4 ± 1 months, respectively; P = .12). Our study population included eight African American participants (representing 15% of the study population), among whom seven received cancer treatment and one was a control participant; the remaining participants were white. All control and cancer participants had normal renal function (Table 1). As shown in Table 1, participants treated for cancer exhibited trends toward having more hypertension, hyperlipidemia, diabetes, and anemia than participants in the control group. Participants receiving cancer treatments were diagnosed with breast cancer (n = 19), lymphoma (n = 11), or leukemia (n = 10). Therapies received by participants for treatment of their malignancy included doxorubicin (n = 30), daunorubicin (n = 10), cyclophosphamide (n = 35), and trastuzumab (n = 2), according to established protocols.16–24 Five participants received one of these agents, 33 received two of these agents, and two received three of these agents during the follow-up period. The median cumulative doses of cancer therapy at 3 to 4 months (roughly at the midpoint of the standard prescribed regimens) included doxorubicin 215.3 mg/m2 (range, 60 to 320 mg/m2), daunorubicin 265 mg/m2 (range, 100 to 600 mg/m2), trastuzumab 919.8 mg (range, 820 to 1,020 mg), and cyclophosphamide 54.6 mg/kg and 4,585.7 mg (range 1,080 to 9,980 mg). Additional chemotherapeutic agents administered to the patients included the antimetabolites fluorouracil, cytarabine, and methotrexate; the alkylating agent cisplatin; and plant alkaloids including vincristine and vinblastine. None of the participants received biologicals such as bevacizumab or rituximab or radiation therapy.
Table 1.
Demographic Data for Control Group and Cancer Therapy Recipients (mean ± standard error of the estimate)
| Characteristic | Control Group(n = 13) |
Cancer Therapy Group(n = 40) |
P | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Age, years | 53 ± 10 | 52 ± 11 | .67 | ||
| Male | 8 | 62 | 12 | 30 | .06 |
| White:African American | 12:1 | 33:7 | .38 | ||
| Weight, kg | 82 ± 17 | 83 ± 21 | .36 | ||
| Height, cm | 173 ± 10 | 168 ± 9 | .58 | ||
| BMI, kg/m2 | 27.6 ± 5.1 | 28 ± 6.3 | .44 | ||
| Historical information | |||||
| Diabetes | 1 | 8 | 6 | 13 | .58 |
| Hypertension | 2 | 15 | 13 | 33 | .21 |
| Hyperlipidemia | 3 | 23 | 9 | 23 | 1.0 |
| Smoking | 0 | 0 | 0 | 0 | 1.0 |
| Cancer therapy | |||||
| Doxorubicin | 29 | 72 | |||
| Daunorubicin | 11 | 28 | |||
| Cyclophosphamide | 28 | 70 | |||
| Trastuzumab or herceptin | 2 | 5 | |||
| Others medications | |||||
| Beta blocker | 1 | 8 | 5 | 13 | .49 |
| ACE inhibitor | 1 | 8 | 7 | 18 | .39 |
| ARB | 1 | 8 | 2 | 5 | .88 |
| Calcium channel blocker | 2 | 15 | 3 | 8 | .66 |
| Hydralazine | 0 | 0 | 1 | 3 | .59 |
| Nitrate | 0 | 0 | 1 | 3 | .59 |
| Diuretic | 0 | 0 | 6 | 15 | .09 |
| Statin | 2 | 15 | 8 | 20 | .43 |
| Hormone replacement therapy | 0 | 0 | 2 | 5 | .45 |
| Blood parameters | |||||
| Hemoglobin, g/dL | 13.2 ± 5.8 | 11.1 ± 2.7 | .08 | ||
| Hematocrit, % | 39.8 ± 14.3 | 33.1 ± 9.3 | .07 | ||
| Serum creatinine, mg/dL | 0.81 ± 0.1 | 0.77 ± 0.2 | .59 | ||
| Unadjusted baseline measurements of stiffness | |||||
| Pulse wave velocity, ms | 4.5 ± 0.9 | 6.9 ± 2.3 | < .0001* | ||
| Ascending aorta distensibility, 10−3 × mmHg−1 | 4.9 ± 1.6 | 4.1 ± 1.6 | .06 | ||
| Descending aorta distensibility, 10−3 × mmHg−1 | 4.8 ± 1.5 | 4.0 ± 1.6 | .06 | ||
NOTE. Conditions that could influence stiffness are age, sex, weight, height, body mass index (BMI), systolic blood pressure, pulse pressure, heart rate, historical diseases (hypertension, diabetes, hyperlipidemia), medications (beta blockers, angiotensin-converting enzyme inhibitor, calcium channel blocker, statin).
Abbreviations: ACE, angiotensin converting enzyme; ARB, angiotensin II receptor blocker.
P value < .05; mean follow-up time ± standard error of the estimate, 3.6 ± 0.8 months.
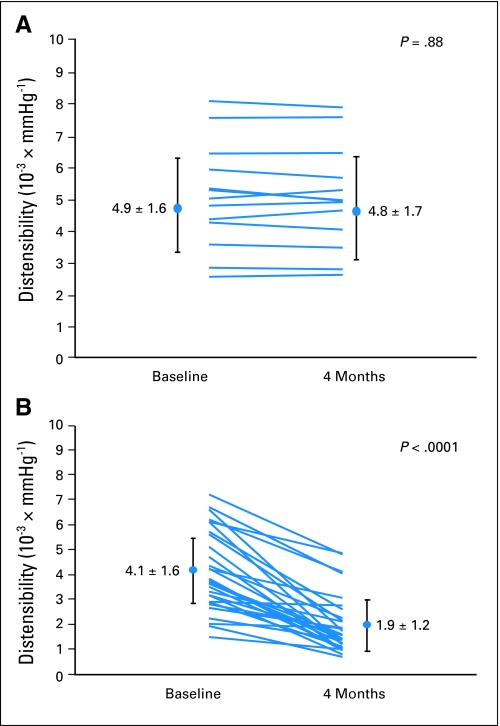
Findings regarding AoD and PWV are shown in Figures 2 and 3, as well as in Table 1. Participants receiving cancer therapy demonstrated a higher baseline PWV (P < .0001), and tended toward a lower baseline AoD (P = .06) compared with control participants. At the follow-up visit, arterial stiffness (AoD and PWV) remained similar to the baseline value in the control participants; however, in those receiving cancer therapy, aortic stiffness notably increased (as evidenced by a decrease in AoD and an increase in PWV) relative to baseline when compared with that of the control group participants (Figs 2 and 3).
Fig 2.
Results of ascending aortic distensibility for the control participants (A) and the participants receiving cancer therapy (B). As shown, the aortic distensibility decreased in participants receiving cancer therapy.
Fig 3.
Pulse wave velocity (PWV) results for the control participants (A) and the participants receiving cancer therapy (B). PWV increased in participants receiving cancer therapy.
After adjusting for baseline measures of aortic stiffness, AoD and PWV remained different between the two groups at the follow-up sample point in the study (P < .0001 for both). We also performed analyses to assess the effects on our results of age, sex, body mass index, systolic BP (baseline), heart rate (baseline), pulse pressure (PP; baseline), serum hemoglobin (baseline), medical comorbidities (hypertension, diabetes, hyperlipidemia), resting cardiac output, and cardioactive medications. Importantly, after adjusting for all of these conditions, the differences in AoD and PWV between cancer therapy and control participants persisted at the 4-month follow-up visit (P < .0001 for both AoD and PWV).
There were no significant associations between cancer diagnoses (breast cancer versus hematologic malignancies) and baseline PWV and AoD (P = .86 and P = .78, respectively). Four months after receiving anthracyclines, both breast cancer and hematologic malignancy participants experienced an increase in PWV (P < .0001 for both) and a decrease in AoD (P = .0004 for those treated for breast cancer, and P < .0001 for those treated for a hematologic malignancy).
White (n = 33) and African American (n = 7) cancer participants had similar baseline measures of PWV and AoD (P = .36 and P = .35, respectively). Four months after receipt of anthracyclines, both whites and African Americans experienced an increase in PWV (P = .29 for comparison of differences in increased PWV, and a decrease in AoD; P = .11 for comparison of differences in decrease of AoD).
For cancer participants, both men (n = 12) and women (n = 28) had similar baseline measures of PWV and AoD (P = .62 and P = .42, respectively). Four months after receipt of anthracyclines, both men and women experienced an increase in PWV (P < .0001 for men and P = .004 for women compared with control participants), and a decrease in AoD (P = .0002 for men and P = .0003 for women compared with control participants).
The cumulative doses of anthracyclines administered in this study correlated with higher reduction of ascending thoracic AoD (Pearson correlation coefficient r = 0.34; P = .02). The addition of trastuzumab or cyclophosphamide to anthracyclines was not associated with a greater increase in aortic stiffness, relative to receipt of anthracyclines alone (P = .76).
The baseline hemodynamic data, LVV, and LVEF were not different between the two groups (Table 2). However, at the follow-up CMR, there was a decrease in diastolic BP, an increase in PP, a decrease in LVEF, and an increase in LVESV (and LVESV index) in participants receiving cancer therapy compared with the control group (P = .04, P = .02, P = .0003, P = .002, and P = .008, respectively). The cardiac output for both cases and controls remained similar between the baseline and follow-up exams (P = .86 and P = .95, respectively). The LVESV was not correlated with AoD or PWV (r = 0.09, P = .51; and r = 0.18, P = .24, respectively).
Table 2.
Hemodynamic Data and Left Ventricular Volume (mean ± standard error of the estimate)
| Variable | Control Group(n = 13) | Cancer Therapy Group(n = 40) | P |
|---|---|---|---|
| Baseline | |||
| Systolic blood pressure, mmHg | 120.2 ± 5.8 | 120.8 ± 14.8 | .89 |
| Diastolic blood pressure, mmHg | 79.7 ± 4.2 | 76.6 ± 12.3 | .38 |
| Pulse pressure, mmHg | 40.5 ± 2.3 | 43.8 ± 8.9 | .19 |
| Heart rate, beats/min | 78.1 ± 7.7 | 79.5 ± 12.8 | .69 |
| LVEDV, mL | 102.5 ± 18.4 | 113.1 ± 29.5 | .21 |
| LVESV, mL | 41.9 ± 11.3 | 49.7 ± 18.2 | .15 |
| LVSV, mL | 60.9 ± 13.6 | 65.2 ± 20.5 | .49 |
| LVEDVi, mL/m2 | 53.5 ± 11.2 | 57.9 ± 12.9 | .27 |
| LVESVi, mL/m2 | 21.1 ± 5.8 | 25.2 ± 7.9 | .09 |
| LVSVi, mL/m2 | 32.2 ± 6.2 | 33.0 ± 8.0 | .75 |
| LVEF, % | 60.9 ± 5.2 | 58.6 ± 6.3 | .24 |
| Cardiac output, L/min | 4.7 ± 0.7 | 4.8 ± 1.5 | .86 |
| Follow-up* | |||
| Systolic blood pressure, mmHg | 120.6 ± 6.4 | 123.0 ± 22.8 | .59 |
| Diastolic blood pressure, mmHg | 80.2 ± 5.2 | 74.4 ± 15.9 | .04† |
| Pulse pressure, mmHg | 40.4 ± 2.2 | 49.6 ± 13.5 | .02† |
| Heart rate, beats/min | 76.2 ± 5.6 | 76.4 ± 15.0 | .95 |
| LVEDV, mL | 98.8 ± 15.2 | 118.6 ± 39.7 | .08 |
| LVESV, mL | 41.3 ± 9.7 | 54.9 ± 12.5 | .002† |
| LVSV, mL | 57.4 ± 10.6 | 62.7 ± 20.0 | .36 |
| LVEDVi, mL/m2 | 51.6 ± 9.9 | 60.3 ± 15.3 | .06 |
| LVESVi, mL/m2 | 20.7 ± 5.2 | 27.9 ± 8.9 | .008† |
| LVSVi, mL/m2 | 30.9 ± 5.3 | 32.0 ± 8.4 | .65 |
| LVEF, % | 59.9 ± 4.1 | 53.9 ± 6.4 | .0003† |
| Cardiac output, L/min | 4.5 ± 0.8 | 4.5 ± 1.4 | .95 |
Abbreviations: LVEDV, left ventricular end-diastolic volume; LVESV, left ventricular end-systolic volume; LVSV, left ventricular stroke volume; LVEDVi, left ventricular end-diastolic volume index; LVESVi, left ventricular end-systolic volume index; LVSVi, left ventricular stroke volume index; LVEF, left ventricular ejection fraction.
Mean follow-up time ± standard error of the estimate, 3.6 ± 0.8 months.
P value < .05.
DISCUSSION
There are three important new findings in this study. First, cancer patients who receive anthracyclines exhibit an increase in aortic stiffness compared with age matched individuals who do not receive therapy for cancer. Second, the increase in aortic stiffness occurs relatively soon (3.6 ± 0.8 months) after initiation of anthracycline therapy. The increase in stiffness manifests by an increase in PWV and a reduction in AoD within the thoracic aorta. Third, this increase in aortic stiffness occurs after accounting for other factors, such as age, sex, diabetes, hypertension, or hyperlipidemia, that can influence aortic stiffness.
The emergence of cardiovascular events is becoming increasingly relevant in cancer survivors.25–29 Five years after treatment for breast cancer, CHF occurs in 1% to 5% of individuals.25 In 10-year survivors of breast cancer, data from 1970 through 1986 indicate that women who received adjuvant chemotherapy or radiation therapy experience an increase in MI (hazard ratio, 2.55; 95% CI, 1.55 to 4.19; P < .001) and stroke (hazard ratio, 1.85; 95% CI, 1.25 to 2.73; P = .002).26 Cardiovascular disease is the most important cause of excess mortality, after secondary malignancy, in long-term survivors of Hodgkin's and non-Hodgkin's lymphoma.27–29
To the best of our knowledge, this is the first study to examine aortic stiffness in patients receiving cancer therapy. Heightened aortic stiffness serves as a stimulus to LV hypertrophy30 and can reduce coronary artery perfusion (promoting subendocardial ischemia).31 In patients not receiving cancer treatment, aortic stiffness is also associated with a future risk of adverse cardiovascular events even after accounting for the Framingham risk score.7–9 As shown in Figures 2 and 3, administration of cancer therapy adversely affected aortic stiffness, a known risk factor of cardiac events.
The magnitude of the increase in PWV observed 3.6 months after receipt of chemotherapy in this study was clinically relevant compared with that in prior studies of PWV in other study populations. At the follow-up visit, the PWV in the participants treated for cancer increased 6.6 ms to an average of 13.5 ± 4.7 ms whereas the mean increase in PWV in the control group was 0.1 ms. Previous studies have shown that a 5-ms change in PWV is relatively large and is associated with cardiovascular mortality in patients with essential hypertension.32 In a study by Laurent et al32 of 1,980 hypertensive patients age 50 ± 13 years (one of three women), 56 cardiovascular events occurred during an average follow-up of 122 ± 53 months. They found that a PWV value of 11.5 ± 3.4 ms was associated with an odds ratio of 1.51 for cardiovascular mortality. In this same study, a 5-ms increase in PWV was equivalent to an increase in cardiovascular risk associated with aging 10 years (odds ratio = 2.14).
Anthracyclines may influence aortic stiffness through one of several mechanisms. Anthracyclines increase oxygen free radicals and induce oxidative stress,1–5 thereby increasing arterial stiffness by causing structural changes within the vascular matrix and interfering with endothelial regulation of vascular smooth muscle tone. Vascular endothelial damage diminishes nitric oxide synthesis and promotes endothelial cell dysfunction that increases vascular stiffness.33 Anthracyclines promote overexpression of inflammatory cytokines that can cause endothelial injury.33–37
The average baseline PWV of the cancer participants was slightly increased relative to previously published values for age-equivalent healthy individuals38 as well as the values present in our control participants. The relatively higher incidence of underlying medical conditions such as hypertension and diabetes known to influence aortic stiffness in our cancer participants may account for this higher baseline value of PWV relative to these other populations. After accounting for baseline differences in aortic stiffness in our populations, the effect of cancer treatment remained associated with an increase in aortic stiffness (P < .0001).
We found that higher cumulative doses of anthracyclines correlated with aortic stiffness. Because we have no data on the longitudinal follow-up of our participants, we are uncertain whether the increase in aortic stiffness observed 4 months after treatment is reversible. Further longitudinal studies regarding the relationship of aortic stiffness to chemotherapy dosing could better address the time-dependent nature of our findings.
Those treated for breast cancer and those treated for a hematologic malignancy experienced similar increases in aortic stiffness after receipt of anthracyclines. In addition, those receiving doxorubicin and daunorubicin experienced increases in aortic stiffness at the relatively low median cumulative doses of doxorubicin 215.3 mg/m2 and daunorubicin 265 mg/m2. Both whites and African Americans experienced an increase in aortic stiffness.
Our study also demonstrated a decrease in LVEF that was related to an increase in LVESV after receipt of anthracyclines. The increase in LVESV occurred without an increase in systolic BP indicating a rightward shift of LVESV relationship due to reduced LV contractility.39,40 We found no differences in LVEDV in our study, which suggests that changes in LV preload did not influence the changes noted in LVEF in this study. Importantly, even though LVEF was somewhat diminished in the cancer participants, cardiac output was maintained in cancer participants at their 4-month visit relative to baseline. Thus, we do not believe changes in cardiac output were responsible in the observed changes in aortic stiffness in the cancer participants.
Our study has potential limitations. First, our case-control study design may lead to underestimating or overestimating the association between treatment exposure and adverse events because of potential differences in the number of confounding factors that may exist between our case and control groups. Importantly, however, after accounting for those potential confounding factors, the differences in AoD and PWV between cancer and control participants persist (P < .0001). Second, the calculation of AoD relies on a brachial assessment of PP as a surrogate for PP in the ascending aorta. Although this approach is used widely and correlates with invasive measures (r = 0.95; P < .001),10–12,41 brachial BP may not be entirely representative of central aortic pressure. In this study, PWV, calculated by dividing the distance between ascending and descending thoracic aorta by transit time of flow wave, was also analyzed. PWV measures are relatively load-independent and thus negate the necessity for BP measurements. Our PWV measures markedly increased after chemotherapy and paralleled the increases in aortic stiffness observed with our AoD results.
Patients who receive anthracycline chemotherapy experience marked reductions in measures of thoracic AoD and increases in thoracic aortic PWV. The results of this study indicate that previously regarded cardiotoxic chemotherapy adversely increases aortic stiffness, a known independent predictor of cardiovascular events.
Footnotes
Supported in part by Grants No. R33CA12196, R01HL076438, M01RR07122, and P30CA012197 from the National Institutes of Health and Grant No. BCTR0707769 from the Susan B. Komen Foundation.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Narumol Chaosuwannakit, Ralph D'Agostino Jr, Frank M. Torti, William C. Little, W. Gregory Hundley
Financial support: W. Gregory Hundley
Administrative support: Kimberly S. Lane, William C. Little, W. Gregory Hundley
Provision of study materials or patients: Julia Lawrence, Susan A. Melin, W. Gregory Hundley
Collection and assembly of data: Narumol Chaosuwannakit, William O. Ntim, W. Gregory Hundley
Data analysis and interpretation: Narumol Chaosuwannakit, Ralph D'Agostino Jr, Craig A. Hamilton, Kimberly S. Lane, William O. Ntim, Julia Lawrence, Frank M. Torti, William C. Little, W. Gregory Hundley
Manuscript writing: Narumol Chaosuwannakit, Ralph D'Agostino Jr, Kimberly S. Lane, William O. Ntim, Julia Lawrence, Leslie R. Ellis, William C. Little, W. Gregory Hundley
Final approval of manuscript: Narumol Chaosuwannakit, Ralph D'Agostino Jr, Craig A. Hamilton, Frank M. Torti, William C. Little, W. Gregory Hundley
REFERENCES
- 1.Floyd JD, Nguyen DE, Lobins RL, et al. Cardiotoxicity of cancer therapy. J Clin Oncol. 2005;23:7685–7696. doi: 10.1200/JCO.2005.08.789. [DOI] [PubMed] [Google Scholar]
- 2.Yeh ET, Tong AT, Lenihan DJ, et al. Cardiovascular complications of cancer therapy: Diagnosis, pathogenesis, and management. Circulation. 2004;109:3122–3131. doi: 10.1161/01.CIR.0000133187.74800.B9. [DOI] [PubMed] [Google Scholar]
- 3.Gianni L, Herman EH, Lipshultz SE, et al. Anthracycline cardiotoxicity: From bench to bedside. J Clin Oncol. 2008;26:3777–3784. doi: 10.1200/JCO.2007.14.9401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singal PK, Iliskovic N. Doxorubicin-induced cardiomyopathy. N Engl J Med. 1998;339:900–905. doi: 10.1056/NEJM199809243391307. [DOI] [PubMed] [Google Scholar]
- 5.Chen MH, Kerkela R, Force T. Mechanisms of cardiac dysfunction associated with tyrosine kinase inhibitor cancer therapy. Circulation. 2008;118:84–95. doi: 10.1161/CIRCULATIONAHA.108.776831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carver JR, Shapiro CL, Ng A, et al. American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: Cardiac and pulmonary late effects. J Clin Oncol. 2007;25:3991–4008. doi: 10.1200/JCO.2007.10.9777. [DOI] [PubMed] [Google Scholar]
- 7.Boutouyrie P, Tropeano AI, Asmar R, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: A longitudinal study. Hypertension. 2002;39:10–15. doi: 10.1161/hy0102.099031. [DOI] [PubMed] [Google Scholar]
- 8.Cruickshank K, Riste L, Anderson SG, et al. Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose tolerance: An integrated index of vascular function? Circulation. 2002;106:2085–2090. doi: 10.1161/01.cir.0000033824.02722.f7. [DOI] [PubMed] [Google Scholar]
- 9.Sutton-Tyrrell K, Najar SS, Boudreau RM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005;111:3384–3390. doi: 10.1161/CIRCULATIONAHA.104.483628. [DOI] [PubMed] [Google Scholar]
- 10.Hundley WG, Kitzman DW, Morgan TM, et al. Cardiac cycle-dependent changes in aortic area and distensibility are reduced in older patients with isolated diastolic heart failure and correlate with exercise intolerance. J Am Coll Cardiol. 2001;38:796–802. doi: 10.1016/s0735-1097(01)01447-4. [DOI] [PubMed] [Google Scholar]
- 11.Groenink M, de Roos A, Mulder BJ, et al. Changes in aortic distensibility and pulse wave velocity with magnetic resonance imaging following beta-blocker therapy in the Marfan syndrome. Am J Cardiol. 1998;82:203–208. doi: 10.1016/s0002-9149(98)00315-4. [DOI] [PubMed] [Google Scholar]
- 12.Malayeri AA, Natori S, Bahrami H, et al. Relation of aortic wall thickness and distensibility to cardiovascular risk factors (from the Multi-Ethnic Study of Atherosclerosis [MESA]) Am J Cardiol. 2008;102:491–496. doi: 10.1016/j.amjcard.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hundley WG, Li HF, Hillis D, et al. Quantitation of cardiac output with velocity-encoding, phase-difference magnetic resonance imaging. Am J Cardiol. 1995;75:1250–1255. doi: 10.1016/s0002-9149(99)80772-3. [DOI] [PubMed] [Google Scholar]
- 14.Hundley WG, Li HF, Lange RA, et al. Assessment of left-to-right intracardiac shunting by velocity-encoded, phase-difference magnetic resonance imaging: A comparison with oximetric and indicator dilution techniques. Circulation. 1995;91:2955–2960. doi: 10.1161/01.cir.91.12.2955. [DOI] [PubMed] [Google Scholar]
- 15.Thiele H, Paetsch I, Schnackenburg B, et al. Improved accuracy of quantitative assessment of left ventricular volume and ejection fraction by geometric models with steady-state free precession. J Cardiovasc Magn Reson. 2002;4:327–339. doi: 10.1081/jcmr-120013298. [DOI] [PubMed] [Google Scholar]
- 16.Fisher B, Brown AM, Dimitrov NV, et al. Two months of doxorubicin-cyclophosphamide with and without interval reinduction therapy compared with 6 months of cyclophosphamide, methotrexate, and fluorouracil in positive-node breast cancer patients with tamoxifen-nonresponsive tumors: Results from the National Surgical Adjuvant Breast and Bowel Project B-15. J Clin Oncol. 1990;8:1483–1496. doi: 10.1200/JCO.1990.8.9.1483. [DOI] [PubMed] [Google Scholar]
- 17.Citron ML, Berry DA, Cirrincione C, et al. Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: First report of Intergroup Trial C9741/Cancer and Leukemia Group B Trial 9741. J Clin Oncol. 2003;21:1431–1439. doi: 10.1200/JCO.2003.09.081. [DOI] [PubMed] [Google Scholar]
- 18.Larson RA, Dodge RK, Bloomfield CD, et al. Treatment of biologically determined subsets of acute lymphoblastic leukemia in adults: Cancer and Leukemia Group B studies. In: Buchner T, editor. Acute Leukemias: VI. Prognostic Factors and Treatment Strategies. Berlin, Germany: Springer-Verlag; 1997. pp. 677–680. [Google Scholar]
- 19.Larson RA, Dodge RK, Burns CP, et al. A five-drug remission induction regimen with intensive consolidation for adults with acute lymphoblastic leukemia: Cancer and Leukemia Group B study 8811. Blood. 1995;85:2025–2037. [PubMed] [Google Scholar]
- 20.Fenaux P, Chastang C, Chevret S, et al. A randomized comparison of all trans retinoic acid (ATRA) followed by chemotherapy and ATRA plus chemotherapy and the role of maintenance therapy in newly diagnosed acute promyelocytic leukemia. Blood. 1999;94:1192–1200. [PubMed] [Google Scholar]
- 21.Engert A, Franklin J, Eich HT, et al. Two cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine plus extended-field radiotherapy is superior to radiotherapy alone in early favorable Hodgkin's lymphoma: Final results of the GHSG HD7 Trial. J Clin Oncol. 2007;25:3495–3502. doi: 10.1200/JCO.2006.07.0482. [DOI] [PubMed] [Google Scholar]
- 22.Straus DJ, Portlock CS, Qin J, et al. Results of a prospective randomized clinical trial of doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) followed by radiation therapy (RT) versus ABVD alone for stages I, II, and IIIA nonbulky Hodgkin disease. Blood. 2004;104:3483–3489. doi: 10.1182/blood-2004-04-1311. [DOI] [PubMed] [Google Scholar]
- 23.Thomas DA, Faderl S, O'Brien S, et al. Chemoimmunotherapy with hyper-CVAD plus rituximab for the treatment of adult Burkitt and Burkitt-type lymphoma or acute lymphoblastic leukemia. Cancer. 2006;106:1569–1580. doi: 10.1002/cncr.21776. [DOI] [PubMed] [Google Scholar]
- 24.Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large B-cell lymphoma. N Engl J Med. 2002;346:235–242. doi: 10.1056/NEJMoa011795. [DOI] [PubMed] [Google Scholar]
- 25.Jensen BV. Cardiotoxic consequences of anthracycline-containing treatment in patients with breast cancer. Semin Oncol. 2006;33(suppl 8):S15–S21. doi: 10.1053/j.seminoncol.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 26.Hooning MJ, Botma A, Aleman BM, et al. Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst. 2007;99:365–375. doi: 10.1093/jnci/djk064. [DOI] [PubMed] [Google Scholar]
- 27.Aleman BMP, van den Belt-Dusebout AW, Klokman WJ, et al. Long-term cause-specific mortality of patients treated for Hodgkin's disease. J Clin Oncol. 2003;21:3431–3439. doi: 10.1200/JCO.2003.07.131. [DOI] [PubMed] [Google Scholar]
- 28.Swerdlow AJ, Higgins CD, Smith P, et al. Myocardial infarction mortality risk after treatment for Hodgkin disease: A collaborative British cohort study. J Natl Cancer Inst. 2007;99:206–214. doi: 10.1093/jnci/djk029. [DOI] [PubMed] [Google Scholar]
- 29.Moser EC, Noordijk EM, van Leeuwen FE, et al. Long-term risk of cardiovascular disease after treatment for aggressive non-Hodgkin lymphoma. Blood. 2006;107:2912–2919. doi: 10.1182/blood-2005-08-3392. [DOI] [PubMed] [Google Scholar]
- 30.Girerd X, Laurent S, Pannier B, et al. Arterial distensibility and left ventricular hypertrophy in patients with sustained essential hypertension. Am Heart J. 1991;122:1210–1214. doi: 10.1016/0002-8703(91)90941-a. [DOI] [PubMed] [Google Scholar]
- 31.Vinereanu D, Nicolaides E, Boden L. Conduit arterial stiffness is associated with impaired left ventricular subendocardial function. Heart. 2003;89:449–450. doi: 10.1136/heart.89.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37:1236–1241. doi: 10.1161/01.hyp.37.5.1236. [DOI] [PubMed] [Google Scholar]
- 33.Lakatta EG, Levy D. Arterial and cardiac aging: Major shareholders in cardiovascular disease enterprises: Part I. Aging arteries: A “set up” for vascular disease. Circulation. 2003;107:139–146. doi: 10.1161/01.cir.0000048892.83521.58. [DOI] [PubMed] [Google Scholar]
- 34.Duquaine D, Hirsch GA, Chakrabarti A, et al. Rapid-onset endothelial dysfunction with adriamycin : Evidence for a dysfunctional nitric oxide synthase. Vasc Med. 2003;8:101–107. doi: 10.1191/1358863x03vm476oa. [DOI] [PubMed] [Google Scholar]
- 35.Drímal J, Zúrová-Nedelcevová J, Knezl V, et al. Cardiovascular toxicity of first line chemotherapy agents: Doxorubicin, cyclophosphamide, streptozotocin and bevacizumab. Neuro Endocrinol Lett. 2006;27(suppl 2):176–179. [PubMed] [Google Scholar]
- 36.Wenzel DG, Cosma GN. A model system for measuring comparative toxicities of cardiotoxic drugs for cultured rat heart myocytes, endothelial cells and fibroblasts: II. Doxorubicin, 5-fluorouracil and cyclophosphamide. Toxicology. 1984;33:117–128. doi: 10.1016/0300-483x(84)90067-2. [DOI] [PubMed] [Google Scholar]
- 37.Ross R. Atherosclerosis: An inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 38.O'Rourke FM, Staessen JA, Viachopoulos C, et al. Clinical application of arterial stiffness: Definitions and reference values. Am J Hypertens. 2002;15:426–444. doi: 10.1016/s0895-7061(01)02319-6. [DOI] [PubMed] [Google Scholar]
- 39.Carabello BA, Spann JF. The uses and limitations of end-systolic indexes of left ventricular function. Circulation. 1984;69:1058–1064. doi: 10.1161/01.cir.69.5.1058. [DOI] [PubMed] [Google Scholar]
- 40.Grossman W, Braunwald E, Mann T, et al. Contractile state of the left ventricle in man as evaluated from end-systolic pressure-volume relation. Circulation. 1977;56:845–852. doi: 10.1161/01.cir.56.5.845. [DOI] [PubMed] [Google Scholar]
- 41.Stefanadis C, Stratos C, Boudoulas H, et al. Distensibility of the ascending aorta: Comparison of invasive and non-invasive techniques in healthy men and in men with coronary artery disease. Eur Heart J. 1990;11:990–996. doi: 10.1093/oxfordjournals.eurheartj.a059639. [DOI] [PubMed] [Google Scholar]