Abstract
Background
Rates of cardiac arrhythmias increase with age and may be associated with clinically significant morbidity. We studied the association between sleep-disordered breathing (SDB) with nocturnal atrial fibrillation or flutter (AF) and complex ventricular ectopy (CVE) in older men.
Methods
A total of 2911 participants in the Outcomes of Sleep Disorders in Older Men Study underwent unattended polysomnography. Nocturnal AF and CVE were ascertained by electrocardiogram-specific analysis of the polysomnographic data. Exposures were (1) SDB defined by respiratory disturbance index (RDI) quartile (a major index including all apneas and hypopneas), and ancillary definitions incorporating (2) obstructive events, obstructive sleep apnea (OSA; Obstructive Apnea Hypopnea Index quartile), or (3) central events, central sleep apnea (CSA; Central Apnea Index category), and (4) hypoxia (percentage of sleep time with <90% arterial oxygen percent saturation). Multivariable logistic regression analyses were performed.
Results
An increasing RDI quartile was associated with increased odds of AF and CVE (P values for trend, .01 and <.001, respectively). The highest RDI quartile was associated with increased odds of AF (odds ratio [OR], 2.15; 95% confidence interval [CI], 1.19–3.89) and CVE (OR, 1.43; 95% CI, 1.12–1.82) compared with the lowest quartile. An increasing OSA quartile was significantly associated with increasing CVE (P value for trend, .01) but not AF. Central sleep apnea was more strongly associated with AF (OR, 2.69; 95%CI, 1.61–4.47) than CVE (OR, 1.27; 95% CI, 0.97–1.66). Hypoxia level was associated with CVE (P value for trend, <.001); those in the highest hypoxia category had an increased odds of CVE (OR, 1.62; 95% CI, 1.23–2.14) compared with the lowest quartile.
Conclusions
In this large cohort of older men, increasing severity of SDB was associated with a progressive increase in odds of AF and CVE. When SDB was characterized according to central or obstructive subtypes, CVE was associated most strongly with OSA and hypoxia, whereas AF was most strongly associated with CSA, suggesting that different sleep-related stresses may contribute to atrial and ventricular arrhythmogenesis in older men.
Sleep-Disordered Breathing (SDB) is a common disorder that causes a number of physiologic stressors, including overnight hypoxia and sympathetic nervous system activation, 1,2 which may cause adverse cardiovascular responses. Increasing data have demonstrated an association between SDB and cardiac arrhythmias and cardiovascular disease (CVD).3–18 Furthermore, recent longitudinal data underscore the importance of moderate to severe SDB as a risk factor for overall as well as cardiovascular-specific mortality.13,14,18 Sleep-disordered breathing may also specifically contribute to cardiac arrhythmias, through abnormal automaticity, triggered automaticity, and reentrant mechanisms elicited by intermittent hypoxia, overshoot hyperoxia, acidosis, mechanical effects of intrathoracic pressure swings, and sympathetic nervous system surges.19,20 Given data that SDB is associated with atrial fibrillation or flutter (AF)12,21 and is also related to stroke17,22 it is plausible that SDB may be a salient risk factor in the development of AF and AF-related morbidity, particularly because the etiologic underpinnings of AF are not completely understood.
Support for an association between SDB and cardiac arrhythmias comes from a number of relatively small studies of patients either referred for evaluation or treatment of heart disease or for sleep disorders,5,9–11 including a small randomized controlled trial that demonstrated improvement in ventricular arrhythmias in patients with heart failure (HF) treated with continuous positive airway pressure.23 However, it is unclear whether the results from these studies are generalizable to individuals in the community who are less symptomatic or have fewer underlying comorbidities than the typical patients referred to either sleep laboratories or heart disease centers. We therefore investigated the cross-sectional association of SDB and nocturnal cardiac arrhythmias based on only a subset of data collected from the Sleep Heart Health Study.15 This study limited its focus to a comparison of individuals with severe SDB vs those without SDB, precluding an assessment of dose response relationships.
Given uncertainty over the extent to which SDB increases the arrhythmia risk level in older individuals, who overall have higher rates of AF and are at increased risk for AF-related complications than younger individuals, we evaluated the relationship between SDB and nocturnal arrhythmia in a large cohort designed to study sleep-related outcomes in older men, who have been reported to have an increased risk of SDB-related mortality compared with women.14,15,18 We analyzed data from the Outcomes of Sleep Disorders in Older Men Study (MrOS Sleep Study), accessing data across the entire range of SDB severity, unlike previously published findings, in which only extremes of SDB were considered.15 The analysis was designed to overcome limitations of prior research by examining both the dose-response relationships between indices of SDB severity and arrhythmia occurrence, as well as whether indices of obstructive apnea, central apnea, and overnight hypoxia vary in the strength of their associations with arrhythmia outcomes. We hypothesize that SDB is associated with nocturnal AF and complex ventricular ectopy (CVE), and such associations persist after adjusting for CVD. We also postulate that there is a stronger association between central sleep apnea (CSA) and Cheyne-Stokes respirations–CSA (CSR-CSA) with nocturnal AF and CVE compared with obstructive sleep apnea (OSA) owing to the association of CSA and CSR-CSA with underlying CVD.
METHODS
SUBJECTS AND STUDY DESIGN
Data from the current study were derived from participants of the MrOS Sleep Study, an ancillary cohort of the Osteoporotic Fractures in Men Study (MrOS Study); the latter enrolled 5995 community-dwelling men 65 years or older who were able to walk without assistance and without history of bilateral hip replacements from 6 clinical centers (Birmingham, Alabama; Minneapolis, Minnesota; Palo Alto, California; the Monongahela Valley near Pittsburgh, Pennsylvania; Portland, Oregon; and San Diego, California). The study is coordinated by the San Francisco Coordinating Center. The study design and methods of recruitment and demographics of this cohort have been previously published.24,25 The MrOS Sleep Study (December 2003–March 2005) visit took place an average of 3.4 years after the baseline visit. Of the initial 5995 MrOS participants, 3135 participated in the MrOS Sleep Study. Of the 3135 men at the sleep visit, 179 did not participate in sleep studies owing either to refusal or because they were receiving treatment for SDB. Of the 2956 men who participated in sleep studies, 45 had a failed study (1.5%), resulting in 2911 participants comprising the final analytic sample. Ethics approval was obtained from the institutional review board of each site and coordinating center. Written informed consent for participation in the MrOS Sleep Study was obtained for all participants.
OUTCOME DATA
Electrocardiography (EKG)-specific software was used to analyze the EKG data collected during polysomnography (Somté; CompuMedics Ltd, Abbotsford, Victoria, Australia). The EKG data were scored as supraventricular, ventricular ectopic, or normal sinus beats. The EKG data from the 2911 sleep studies were manually reviewed by a single observer (R.S.) while blinded to respiratory events, with arbitration by a board-certified critical care physician for any uncertainty in event categorization. The single reviewer (R.S.) of the EKG data is a polysomnologist with EKG training. We have previously published findings that the estimated intraclass correlation coefficients for this reviewer and the physician for coding arrhythmia in a random sample of 20 sleep studies were 0.98 to 0.99.15 In the current study, all studies demonstrating nocturnal AF and CVE were confirmed by the physician (R.M.). Any questionable categorization of arrhythmias were referred to a cardiologist for arbitration. The primary outcomes considered include the occurrence of nocturnal AF (paroxysmal, or occurring only intermittently on the overnight polysomnogram record, continuous AF, and atrial flutter) and nocturnal CVE, the latter defined as bigeminy, trigeminy, quadrigeminy, or nonsustained ventricular tachycardia. It is worth noting that only 8 EKG tracings from polysomnogram records demonstrated paroxysmal AF. In addition, other outcomes included the occurrence of any atrial arrhythmias (supraventricular tachycardia; premature atrial contractions occurring ≥5 times per hour), other ventricular arrhythmias (nonsustained ventricular tachycardia defined as ≥3 consecutive ventricular ectopic beats with a mean rate of ≥100 beats/min; premature ventricular contractions occurring ≥5 times per hour) and conduction delay arrhythmias (sinus pause with a duration of ≥3 seconds, atrioventricular block).When analyzing premature atrial contractions, the data for studies with AF and supraventricular tachycardia were excluded from the analyses.
POLYSOMNOGRAPHY DATA COLLECTION
In-home sleep studies using a portable polysomnography unit (Safiro; CompuMedics Ltd) were performed. The recording montage consisted of C3/A2 and C4/A1 electroencephalograms, bilateral electrooculograms, a bipolar submental electromyogram, thoracic and abdominal respiratory inductance plethysmography, airflow (by nasal-oral thermocouple) and nasal pressure (via cannula), oximetry (Nonin Medical Inc, Plymouth, Minnesota; sampling frequency of 25 Hz), lead I EKG (sampled at 250 Hz), body position (mercury switch sensor), and bilateral leg movements (piezoelectric sensors). Participants were examined for 1 night in their own homes to minimize the burden of travel. Trained, certified staff members performed home visits for setup of the sleep study units.
Polysomnographic data quality for the MrOS Sleep Study was excellent; there was less than a 4% failure rate, and more than 70% of the studies were graded as excellent or outstanding in quality. Quality codes for signals and studies in the MrOS Sleep Study were graded using previously described approaches, 26 which included coding the duration of artifact-free data per channel and overall study quality (reflecting the combination of grades for each channel).
The CSR-CSA was characterized by a minimum consecutive 5-minute period of crescendo-decrescendo respiratory pattern culminating in a nadir of central apneas with typical cycle length. Apneas were identified as episodes of absent or nearly absent airflow, and were categorized as obstructive if effort persisted on thoraco-abdominal inductance channels or as central if there was no effort detected. Hypopneas were scored if amplitude changes on respiratory effort or airflow signals did not meet the threshold for apneas but were clearly discernible as defined by an approximate reduction of more than 30%. For the purposes of this study, we included only hypopneas associated with a 3% or more oxygen desaturation. Using similar approaches, between- and within-scorer reliability for various derivations of the respiratory disturbance index (RDI) in the same scoring group has been excellent, with intraclass correlation coefficients ranging from 0.76 to 0.99.27
The severity of SDB was determined by the RDI, which is the number of all apneas (both obstructive and central) and hypopneas that occurred per hour of sleep. Similar to SDB, OSA was defined by the Obstructive Apnea-Hypopnea Index (OAHI), the number of obstructive apneas and hypopneas per hour of sleep, and was also categorized by quartile. Owing to the right-skewed nature of the Central Apnea Index (CAI, the number of central apneas per hour of sleep) and the recognized lack of uniform criteria to define clinically significant CSA,28 we selected categories that were reasonable based on our data distribution (CAI = 0: 40.5% of patients; CAI > 0 to 1: 34.8%; CAI > 1 to 3: 12.5%; and CAI > 3: 12.2%). Given the right-skewed distribution of total sleep time (TST) with arterial oxygen percent saturation less than 90% used to define hypoxia, this was defined as follows: less than 1.0%, 1.0% to less than 3.5%, 3.5% to less than 10.0%, and 10% or greater.
COVARIATE DATA COLLECTION
All of the covariate data were collected at the time of the sleep study visit except cholesterol levels, which had been collected during the baseline MrOS visit an average of 3.4 years earlier. Information regarding medical history was ascertained from questionnaire data. Race was based on self-report and categorized as white, African American, Asian, and Hispanic or other. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared, and obesity was defined as a BMI of at least 30.29,30 During the visits, body weight was measured with a standard balance beam or digital scale that was calibrated with standard weights, height with a wall-mounted Harpenden stadiometer (Holtain Ltd, Crymych, Dyfed, Wales). Waist circumference was also measured using standard methods. 31 Cholesterol was measured using total cholesterol (milligrams per deciliter), calculated as high-density lipoprotein (HDL) cholesterol (milligrams per deciliter) + low-density cholesterol (LDL) cholesterol (milligrams per deciliter) + 0.5 × (triglycerides [milligrams per deciliter]). An automated analyzer (calibrated daily) was used (COBAS Integra 800; Roche Diagnostics Corp, Indianapolis, Indiana).
STATISTICAL ANALYSIS
Participant characteristics were summarized by quartile of RDI. Differences among quartiles were examined using analysis of variance for normally distributed continuous variables, Kruskal-Wallis tests for skewed continuous data, and χ2 tests for homogeneity for categorical data.
The primary predictor in this analysis was SDB categorized by RDI quartile. For all analyses involving SDB defined by RDI, analyses were also performed to assess the association between each arrhythmia and clinically defined RDI categories (<5.0, 5.0 to <15.0, 15.0 to <30.0, and ≥30.0)32 using logistic regression models. Because results yielded findings similar to those found in models using the quartiles of RDI, the latter results are presented. Proportions of all outcomes by SDB category were calculated, and a Cochran-Armitage test for trend was performed to examine a linear trend across the categories.
Logistic models were used to examine the association of SDB indices and arrhythmia outcomes. Odds ratios (ORs) with 95% confidence intervals (CIs) and P values are presented. The SDB predictors were used categorically in these models with the lowest category acting as a reference. We also examined evidence of a linear trend across the categories by using the categorical predictor as a linear (continuous) variable in the logistic models. Unadjusted relationships were explored as well as models adjusted for age, race, BMI, study site, hypertension, diabetes mellitus (DM), cardiac disease (defined by history of coronary heart disease, coronary artery bypass graft surgery, percutaneous coronary intervention, cardiomyopathy, congestive HF, myocardial infarction, and angina), pacemaker placement, and total cholesterol levels.
Secondary analyses were performed by restricting to those without history of HF to additionally minimize potential confounding by HF. A cutoff of CAI greater than 3 was used for these analyses for ease of interpretation and for consistency with the upper CAI category cutoff in the primary analyses. Also, analyses restricted to those without history of DM were performed given prior literature demonstrating associations of DM with central apnea and periodic breathing.33 Sensitivity analyses were performed excluding those participants with a CAI of at least 3 when considering OSA as the outcome and similarly excluding those with an Obstructive Apnea Index (OAI) of 5 or higher when considering CSA as the outcome to ascertain OSA- vs CSA-specific effects. Analyses were performed using SAS statistical software (version 9.1; SAS Institute Inc, Cary, North Carolina).
RESULTS
OVERALL
The 2860 individuals who did not participate in the sleep visit were similar in age (mean [SD] age, 73.1 [5.6] years vs 74.1 [6.1] years; P < .001) compared with the 3135 MrOS Sleep Study participants and similar in mean (SD) BMI: 27.4 (3.7) vs 27.4 (3.9) (P > .99). There were 138 participants with AF (4.7%) and 1048 with CVE (36.0%). Table 1 shows the subject characteristics for the analytic sample stratified by RDI category. Increasing severity of SDB category was associated with increasing age, BMI, and comorbid factors such as DM, hypertension, and CVD (Table 1).
Table 1.
Demographics and Risk Factors by Sleep-Disordered Breathing Quartilea
| Quartile | ||||||
|---|---|---|---|---|---|---|
| Patient Characteristic | Overall (N = 2911) |
1 (n = 727) |
2 (n = 728) |
3 (n = 728) |
4 (n = 728) |
P Valueb |
| Age, mean (SD), y | 76.4 (5.5) | 76.3 (5.7) | 76.1 (5.6) | 76.1 (5.4) | 77.1 (5.5) | <.001 |
| Race or ethnicity | ||||||
| White | 90.7 | 90.9 | 90.0 | 91.8 | 90.3 | .70 |
| African American | 3.4 | 3.2 | 3.7 | 3.6 | 3.2 | |
| Asian | 2.9 | 3.3 | 3.2 | 1.7 | 3.4 | |
| Other | 3.0 | 2.6 | 3.2 | 3.0 | 3.2 | |
| BMI, mean (SD) | 27.2 (3.8) | 25.7 (3.3) | 27.0 (3.6) | 27.4 (3.7) | 28.5 (4.1) | <.001 |
| BMI ≥30 | 20.3 | 9.1 | 19.0 | 21.0 | 32.1 | <.001 |
| Waist circumference, mean (SD), cm | 99.6 (10.9) | 96.0 (10.4) | 99.2 (10.4) | 100.0 (10.4) | 103.2 (11.2) | <.001 |
| Medical history | ||||||
| DM | 13.3 | 9.5 | 12.1 | 14.6 | 17.1 | <.001 |
| Hypertension | 49.9 | 44.4 | 48.6 | 50.4 | 56.3 | <.001 |
| CVD | 32.2 | 29.9 | 30.8 | 32.2 | 35.8 | .08 |
| HF | 6.0 | 3.6 | 5.9 | 5.0 | 9.5 | <.001 |
| MI | 17.5 | 16.5 | 17.0 | 17.3 | 19.0 | .63 |
| Stroke | 3.8 | 4.3 | 3.9 | 4.0 | 3.2 | .73 |
| Total cholesterol, mean (SD), mg/dL | 193.1 (34.0) | 191.1 (33.7) | 194.1 (34.1) | 194.2 (34.0) | 193.2 (34.3) | .29 |
| Pacemaker placement | 4.1 | 4.0 | 3.2 | 4.5 | 4.5 | .50 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CVD, cardiovascular disease; DM, diabetes mellitus; HF, heart failure; MI, myocardial infarction; RDI, Respiratory Disturbance Index (defined as numbers of obstructive apneas and hypopneas that occur per hour of sleep).
SI conversion factor: To convert total cholesterol to millimoles per liter, multiply by 0.0259.
Quartiles of RDI (numbers of obstructive apneas and hypopneas that occur per hour of sleep) are defined as follows: 1, RDI <5.9; 2, 5.9 ≤ RDI <12.6; 3, 12.6 ≤ RDI < 23.9; 4, RDI ≥ 23.9. Continuous variables are presented as means (SDs) and categorical variables as percentages.
P values for normally distributed continuous variables are from analysis of variance, for skewed variables, a Kruskal-Wallis test. P values for categorical data are from a χ2 test for homogeneity.
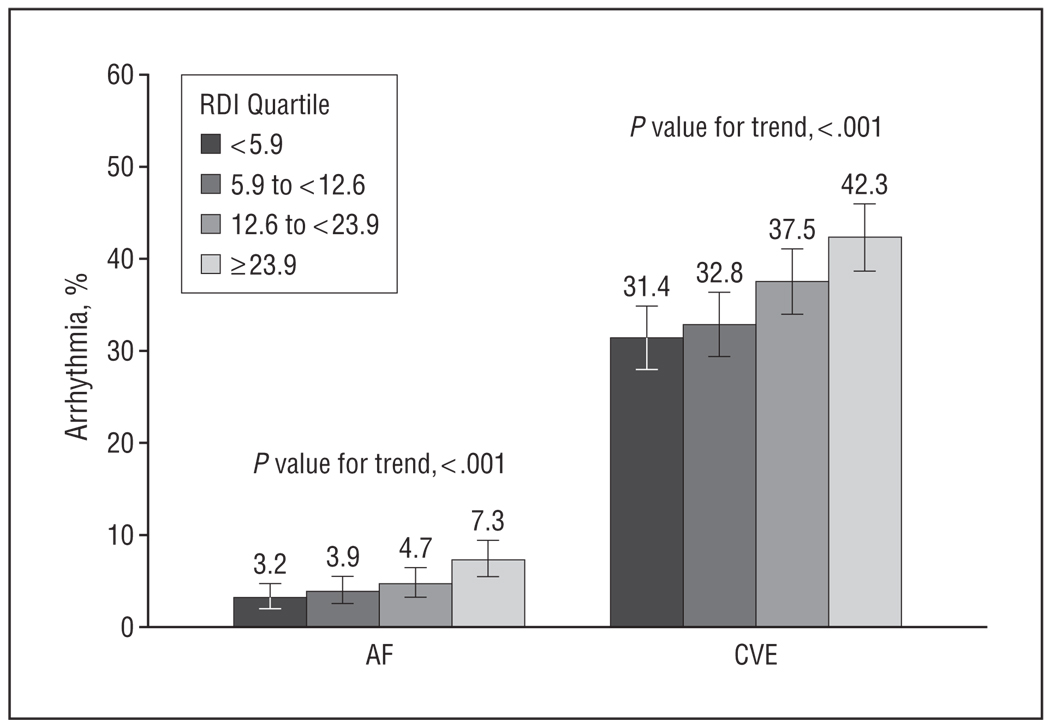
SDB INDICES AND NOCTURNAL AF
Overall, when examining increasing SDB severity defined by RDI quartile in unadjusted analyses, an increasing percentage of AF was noted (P value for trend, <.001) (Table 2, and Figure 1). Unadjusted and adjusted logistic regression analyses both showed a significant dose-response relationship between increasing RDI quartile and the occurrence of AF, with ORs ranging from 1.38 for quartile 2 (5.9 ≤ RDI < 12.6) to 2.15 for quartile 4 (RDI ≥ 23.9) in adjusted analyses (P value for trend, .01) (Table 3).
Table 2.
Distribution of Arrhythmias According to Sleep-Disordered Breathing Quartilea
| Quartile | |||||
|---|---|---|---|---|---|
| Type of Arrhythmia | 1 (n = 727) | 2 (n = 728) | 3 (n = 728) | 4 (n = 728) |
P Valueb |
| Ventricular arrhythmias | |||||
| Premature ventricular contraction, ≥5/h c | 266 (38.1) | 262 (37.4) | 296 (42.7) | 334 (47.9) | <.001 |
| Bigeminy | 167 (23.0) | 166 (22.8) | 208 (28.6) | 223 (30.6) | <.001 |
| Trigeminy | 166 (22.8) | 176 (24.2) | 181 (24.9) | 223 (30.6) | .001 |
| Quadrigeminy | 152 (20.9) | 148 (20.3) | 165 (22.7) | 199 (27.3) | .002 |
| Nonsustained ventricular tachycardia | 24 (3.3) | 11 (1.5) | 24 (3.3) | 30 (4.1) | .14 |
| Complex ventricular ectopyd | 228 (31.4) | 239 (32.8) | 273 (37.5) | 308 (42.3) | <.001 |
| Atrial arrhythmias | |||||
| Premature atrial contraction, ≥5/he | 258 (49.1) | 237 (45.2) | 240 (48.3) | 242 (52.5) | .20 |
| Atrial fibrillation | 23 (3.2) | 28 (3.8) | 34 (4.7) | 53 (7.3) | .001 |
| Supraventricular tachycardia | 150 (20.6) | 150 (20.6) | 162 (22.3) | 185 (25.4) | .02 |
| Conduction delay arrhythmias | |||||
| Sinus pause, ≥3 s | 3 (0.4) | 1 (0.1) | 2 (0.3) | 3 (0.4) | .88 |
| First-degree atrioventricular block | 303 (41.7) | 267 (36.7) | 289 (39.7) | 263 (36.1) | .09 |
| Second-degree atrioventricular block type 1 | 8 (1.1) | 20 (2.8) | 14 (1.9) | 13 (1.8) | .59 |
| Second-degree atrioventricular block type 2 | 2 (0.3) | 2 (0.3) | 1 (0.1) | 1 (0.1) | .46 |
| Intraventricular conduction delay | 29 (4.0) | 31 (4.3) | 39 (5.4) | 38 (5.2) | .17 |
Abbreviation: RDI, Respiratory Disturbance Index (defined as numbers of obstructive apneas and hypopneas that occur per hour of sleep).
Quartiles of RDI are defined as follows: 1, RDI < 5.9; 2, 5.9 ≤ RDI < 12.6; 3, 12.6 ≤ RDI < 23.9; 4, RDI ≥ 23.9. Data are given as number (percentage) except where indicated.
P value for trend.
For premature ventricular contraction (PVC) ≥5/h, only 2790 had data for total PVC beats (121 missing data) resulting in the following 4 quartiles: Q1, n = 698; Q2, n = 701; Q3, n = 693; Q4, n = 698.
Complex ventricular ectopy represents a composite of bigeminy, trigeminy, quadrigeminy, and nonsustained ventricular tachycardia.
Premature atrial contraction (≥5/h) excludes data from those individuals with atrial fibrillation/flutter and supraventricular tachycardia resulting in the following 4 quartiles: Q1, n = 526; Q2, n = 524; Q3, n = 497; Q4, n = 461.
Figure 1.
Arrhythmia by increasing Respiratory Disturbance Index (RDI) quartile relative to atrial fibrillation or flutter (AF) and complex ventricular ectopy (CVE). The error bars indicate standard errors.
Table 3.
Adjusted and Unadjusted Odds Ratios (ORs) Relating Sleep Apnea Indices and EKG-Identified Arrhythmias as Dichotomous Outcomesa
| Atrial Fibrillation/Atrial Flutter | Complex Ventricular Ectopy | |||
|---|---|---|---|---|
| Quartile or Category | Unadjusted | Adjustedb | Unadjusted | Adjustedb |
| RDI quartile | ||||
| RDI < 5.9 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 5.9 ≤ RDI < 12.6 | 1.22 (0.70–2.15) | 1.38 (0.74–2.57) | 1.07 (0.86–1.33) | 1.00 (0.79–1.27) |
| 12.6 ≤ RDI < 23.9 | 1.50 (0.87–2.57) | 1.58 (0.85–2.91) | 1.31 (1.06–1.63) | 1.31 (1.04–1.66) |
| RDI ≥ 23.9 | 2.40 (1.46–3.97)c | 2.15 (1.19–3.89)c | 1.61 (1.30–1.99)c | 1.43 (1.12–1.82)c |
| OAHI quartile | ||||
| OAHI < 2.9 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2.9 ≤ OAHI <6.5 | 1.32 (0.78–2.22) | 1.49 (0.83–2.67) | 1.10 (0.88–1.37) | 1.12 (0.88–1.41) |
| 6.5 ≤ OAHI < 12.7 | 1.24 (0.73–2.10) | 1.21 (0.66–2.21) | 1.20 (0.96–1.49) | 1.18 (0.93–1.50) |
| OAHI ≥ 12.7 | 1.82 (1.11–2.97)c | 1.49 (0.83–2.68) | 1.58 (1.28–1.96)c | 1.37 (1.08–1.75)c |
| CAI category | ||||
| CAI = 0 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 0 < CAI ≤1 | 0.77 (0.47–1.25) | 0.81 (0.49–1.36) | 0.83 (0.69–0.99) | 0.84 (0.69–1.02) |
| 1 < CAI ≤ 3 | 1.58 (0.91–2.73) | 1.05 (0.53–2.05) | 0.98 (0.76–1.26) | 1.03 (0.79–1.35) |
| CAI > 3 | 3.17 (2.00–5.03)c | 2.69 (1.61–4.47)c | 1.32 (1.03–1.70) | 1.27 (0.97–1.66) |
| CSR-CSA | 5.20 (3.58–7.58) | 4.54 (2.96–6.96)c | 1.62 (1.28–2.05) | 1.55 (1.20–2.00) |
| TST < 90 category | ||||
| (TST < 90) <1 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1 ≤ (TST < 90) <3.5 | 1.14 (0.75–1.74) | 1.33 (0.84–2.12) | 1.33 (1.11–1.61) | 1.31 (1.07–1.60) |
| 3.5 ≤ (TST < 90) < 10 | 1.14 (0.66–1.95) | 1.11 (0.59–2.07) | 1.27 (1.01–1.62) | 1.27 (0.97–1.66) |
| (TST < 90) ≥ 10 | 1.54 (0.94–2.52) | 1.30 (0.71–2.40) | 1.89 (1.49–2.39)c | 1.62 (1.23–2.14)c |
Abbreviations: CAI, Central Apnea Index; CS-CSA, Cheyne-Stokes respirations–central sleep apnea; EKG, electrocardiogram; OAHI, Obstructive Apnea-Hypopnea Index; RDI, Respiratory Disturbance Index (defined as numbers of obstructive apneas and hypopneas that occur per hour of sleep); TST <90, total sleep time with less than 90% oxygen saturation.
Data are presented as ORs (95% confidence intervals).
Adjusted for age, race, study site, body mass index, diabetes mellitus, hypertension, cardiovascular disease, hypercholesterolemia, and pacemaker placement.
P value for trend, <.05.
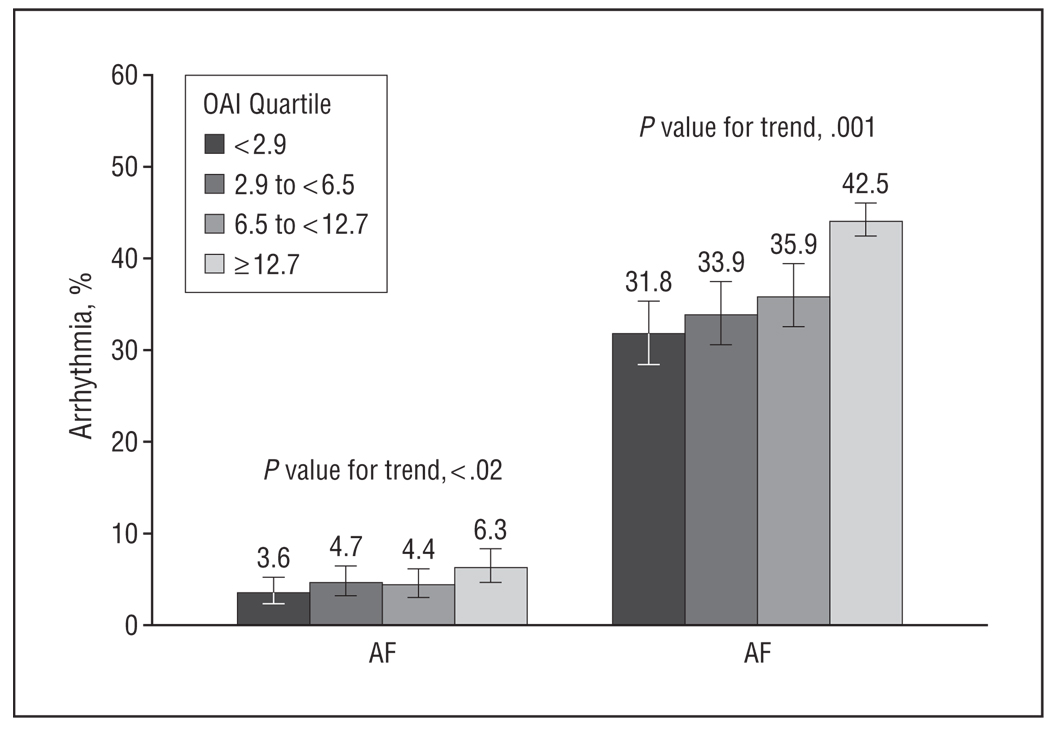
When assessing OSA-specific relationships, in unadjusted analyses, there was a significant association with increasing OAHI quartile and AF (P value for trend, .02) (Figure 2). Although unadjusted analyses demonstrated a significant association with the highest quartile of OSA and AF (with quartile 1 as the reference category; OR, 1.82; 95% CI, 1.11–2.97), this association did not persist after taking into account confounding factors.
Figure 2.
Arrhythmia by increasing Obstructive Apnea Index (OAI) quartile relative to atrial fibrillation or flutter (AF) and complex ventricular ectopy (CVE). The error bars indicate standard errors.
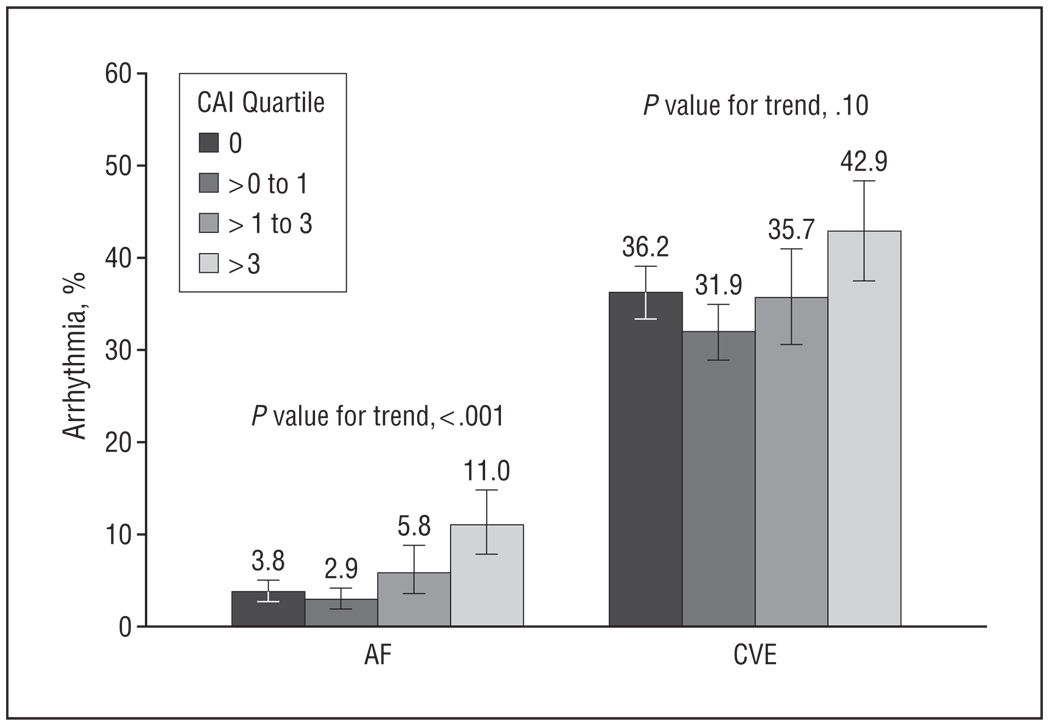
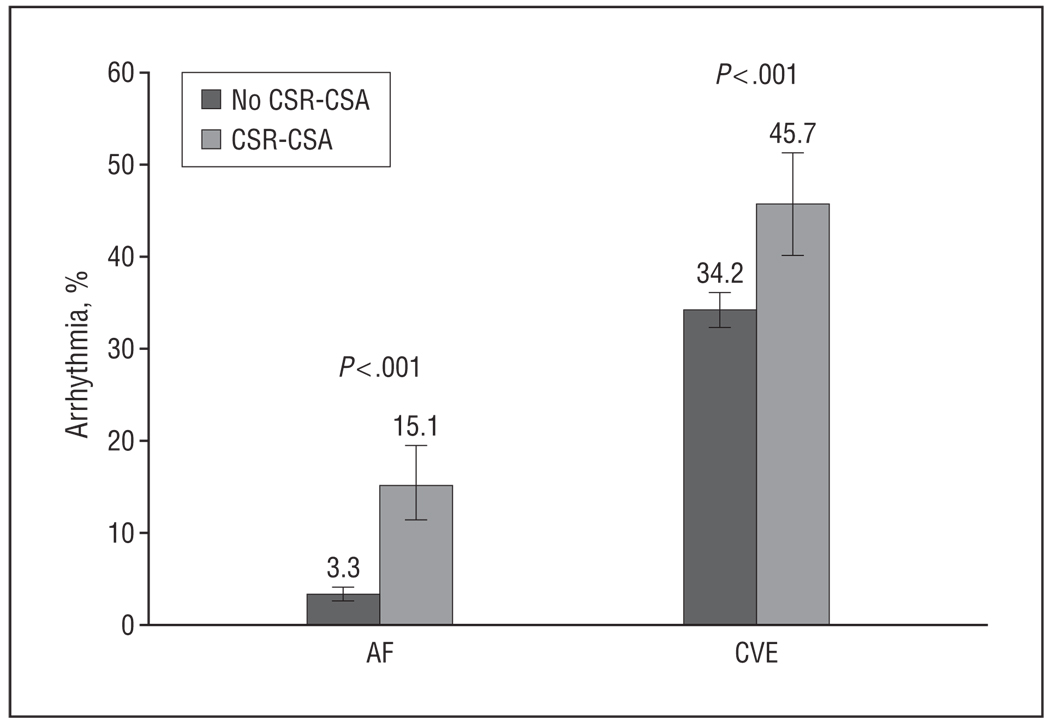
Alternatively, when assessing CSA-specific relationships, in unadjusted analyses there was a significant association with increasing CSA category with AF (P value for trend, <.001) (Figure 3). Unadjusted analyses demonstrated a significant association with the highest CAI category (reference category=0; OR, 3.17; 95% CI, 2.00–5.03), which persisted after taking into account confounding factors (reference category=0; OR, 2.69; 95% CI, 1.61–4.47) (Table 3). Similarly, in unadjusted analyses, there was a significant association with CSR-CSA and AF (P<.001) (Figure 4). In analyses adjusted for potential confounders, including HF, a significant association was demonstrated between CSR-CSA and AF (OR,4.54; 95% CI, 2.96–6.96) (Table 3). To examine which physiologic effects of SDB may contribute to arrhythmogenicity, we assessed the relationships of hypoxia with arrhythmias, which demonstrated no significant association of TST with less than 90% oxygen saturation and AF (see Table 3 for ORs and 95% CIs).
Figure 3.
Arrhythmia by increasing Central Apnea Index (CAI) category relative to atrial fibrillation or flutter (AF) and complex ventricular ectopy (CVE). The error bars indicate standard errors.
Figure 4.
Arrhythmia by increasing Cheyne-Stokes respirations–central sleep apnea (CSR-CSA) category relative to atrial fibrillation or flutter (AF) and complex ventricular ectopy (CVE). The error bars indicate standard errors.
SDB INDICES AND NOCTURNAL CVE
There was a significant relationship between increasing SDB severity with CVE (P value for trend, <.001) (Figure 1). Both unadjusted and adjusted logistic regression analyses showed significantly increased OR estimates associated per increasing RDI quartile and CVE: adjusted OR, 1.00 (quartile 2); 1.31 (quartile 3); and 1.43 (quartile 4), respectively (P value for trend, <.001) (Table 3).
When assessing OSA-specific relationships, in unadjusted analyses, there was an association with increasing OAHI quartile and CVE (P value for trend, <.001) (Figure 2). Unadjusted analyses demonstrated a significant association with CVE and the highest OAHI quartile relative to the reference category (OR, 1.58; 95% CI, 1.28–1.96), which persisted after taking into account potential confounders (fully adjusted OR, 1.37, 95% CI, 1.08–1.75) (Table 3).
When assessing CSA-specific relationships, in unadjusted analyses, there was not a significant association with increasing CSA category and CVE (P=.10) (Figure 3). A significant association was observed between the highest quartile of CSA and CVE; however, although this association was no longer significant in the fully adjusted model (reference category = 0; OR, 1.27, 95% CI, 0.97–1.66), the effect size was very similar. A significant association was observed between CSR-CSA and CVE in unadjusted analyses (Figure 4), even after adjusting for confounders such as CVD including HF (OR, 1.55; 95% CI, 1.20–2.00) (Table 3).
Contrary to AF analyses, a significant association was observed between TST with less than 90% oxygen saturation and CVE with fully adjusted analyses showing the following trend per increasing category of sleep time in oxygen desaturation: OR, 1.31; 95% CI, 1.07 to 1.60 (TST with < 90% oxygen saturation: 1 to <3.5%); OR, 1.27; 95% CI, 0.97 to 1.66 (TST with < 90% oxygen saturation: 3.5 to <10%); OR, 1.62; 95% CI, 1.23 to 2.14 (TST with < 90% oxygen saturation ≥ 10%) (Table 3).
SDB INDICES AND OTHER NOCTURNAL ARRHYTHMIAS
In the fully adjusted model, there was a significant association between the highest RDI quartile and supraventricular tachycardia compared with the reference category, but no association with premature atrial contractions occurring 5 or more times per hour. There was not a significant relationship between increasing SDB severity with nonsustained ventricular tachycardia (P value for trend, .14). Also, in the fully adjusted model, there was a significant association between the highest RDI quartile and premature ventricular contractions occurring at least 5 times per hour compared with the reference category. When considering conduction delay arrhythmias such as sinus pauses, atrioventricular block patterns (first, second, and third degree), and intraventricular conduction delay, no significant associations were noted with these arrhythmias and SDB severity defined by RDI quartile. (See Table 2 for ORs and 95% CIs.)
SECONDARY ANALYSES
Because HF may be a risk factor for CSA, additional analyses were restricted to those without HF and also tested for an interaction between each of the sleep apnea indices (RDI, OAHI, and CAI) and HF. There were 174 participants (6.0%) with a self-reported history of HF. In those without HF, a significantly higher percentage of those with a CAI higher than 3 had AF (P < .001) and CVE (P = .01) compared with those with a CAI of 3 or less. Also, in those without HF, a significantly higher percentage of those with CSR-CSA had AF (P < .001) and CVE (P < .001) compared with those without CSR-CSA. In fully adjusted stratified analyses, in those without HF, a significant association was observed between AF and CSA defined as a CAI greater than 3 (reference CAI = 0; OR, 2.84; 95% CI, 1.65–4.91) and between AF and CSR-CSA (OR, 4.99; 95% CI, 3.11–8.01). However, in combined analyses, the interaction term between sleep apnea indices and HF was not statistically significant (P > .05). Similarly, in the sample restricted to those without DM (n = 2524), compared with the reference group, AF was significantly associated with a CAI higher than 3 (OR, 2.57; 95% CI, 1.48–4.48) and with CSR-CSA (OR, 4.31; 95% CI, 2.70–6.89).
Sensitivity analyses were performed excluding those with a CAI of 3 or higher when considering OSA (336 excluded) and similarly excluding those with an OAI of 5 or higher when considering CSA (880 excluded). On the one hand, when excluding those with a CAI of 3 or higher, there was no association between OSA defined by OAHI quartile and AF. On the other hand, when excluding those with an OAI of 5 or higher, the association between CSA and AF slightly increased in magnitude (fully adjusted for reference CAI = 0; CAI > 3, OR, 3.65; 95% CI, 1.75–7.62) as did the association of AF and CSR-CSA (fully adjusted OR, 5.19; 95% CI, 2.81–9.60).
When excluding those with a CAI of 3 or higher, the association between the highest OAHI quartile relative to the reference quartile and CVE persisted; however, it was slightly attenuated (fully adjusted OR, 1.31; 95% CI, 1.01–1.70).When excluding those with an OAI of at least 5, the association between CSA and CVE was not significant, but the association with CSR-CSA and CVE increased in magnitude (fully adjusted OR, 1.84; 95% CI, 1.25–2.72).
COMMENT
In a large, community-dwelling group of older men, an extensive series of analyses demonstrated a progressive increase in odds of nocturnal AF or of CVE with increasing severity of SDB. In addition, significantly increased risks of nocturnal AF and CVE were observed at a threshold RDI of 24 and 13, respectively (corresponding to the upper and middle quartiles of RDI for nocturnal AF and CVE, respectively; n = 728). In addition, a detailed series of analyses investigating the relative contribution of obstructive and CSA to these associations indicated that the relationship between SDB and nocturnal AF was largely associated with CSA but not purely by OSA. In contrast, nocturnal CVE was associated with OSA, but not CSA, and was also associated with overnight hypoxia.
Epidemiological studies of SDB commonly describe the occurrence of obstructive and central events. In clinical settings, these apnea subtypes are often characterized by distinct clinical features such as obesity, sleepiness, snoring, and witnessed apneas resulting from complete or partial airway collapse of a narrowed pharynx in OSA and sleep disruption and paroxysmal nocturnal dyspnea related to central apneas occurring as a result of reductions in central respiratory drive in CSA. In the current study, we identified important differences in the associations of each apnea type in relation to specific arrhythmias in older men.
The stronger association between CSA with AF compared with OSA and AF could reflect common risk factors for each condition, such as HF, that may not have been completely accounted for in these models. It is well known that HF may precipitate CSR-CSA via mechanisms of increased respiratory chemoreceptor drive, pulmonary congestion and/or hyperventilation, and prolonged circulation time. Therefore, we performed analyses in which we adjusted for self-reported HF and also restricted analyses to individuals without reported HF. The latter analyses still showed an approximately 3-fold increased odds of AF in association with CSA and 5-fold increased odds of AF with CSR-CSA. It is possible that these relationships could be the result of unrecognized HF, or be related to underlying structural heart disease not measured in this study, such as ventricular hypertrophy, atrial enlargement, and so forth. In fact, CSA may be a sensitive marker of cardiac dysfunction or autonomic function that is etiologically linked to the development of AF. Our findings are consistent with previously published data demonstrating, even in the absence of HF, that AF is more strongly associated with idiopathic CSA compared with OSA.34 Because of the cross-sectional design and limited data on cardiac function, this study cannot more precisely address the causal pathways that may link CSA and AF. Nonetheless, the strong association between the 2 conditions emphasizes the potential usefulness in screening patients with AF for CSA. Aggressive evaluation of such patients may be warranted given data supporting an increased mortality in patients with HF and with nocturnal CSR-CSA compared with those without CSR-CSA despite a similar degree of left ventricular dysfunction. 35,36
In contrast to the association between AF and CSA, a relatively weak association was demonstrated between AF and OSA. In the Sleep Heart Health Study,15 a cohort with a mean age of 69 years, an overall 4-fold increased odds of AF was demonstrated in those with severe SDB compared with the 2-fold increased odds in the current study. However, this finding is consistent with results reported in the Sleep Heart Health Study15 showing an attenuation of this association with advancing age. This observation may be the result of survivorship bias or competing risk factors. Further studies comparing age-related modification of SDB-associated CVD are needed to better understand potential age-related differences in SDB morbidity and to determine whether OSA confers the same increased risk for AF in older vs younger individuals.
In contrast to the analyses that modeled CSA, OSA was associated with CVE but not with AF. Furthermore, the strength of these associations increased after excluding those with CSA from analyses. Complex ventricular ectopy also was strongly associated with overnight hypoxia, a cardinal characteristic of OSA. Thus, unlike AF occurring in elderly individuals, CVE seems to be more common in those who experience intermittent hypoxia and intermittent collapse of the upper airway—triggers for intrathoracic pressure changes, blood pressure surges, and sympathetic nervous system activation that are likely to precipitate ventricular arrhythmogenicity. These findings are consistent with observations describing reduction in ventricular irritability in those patients with SDB who effectively responded to SDB treatment as gauged by a reduction in RDI and dramatic improvement in hypoxia. 37 To date, the aggregate data suggest the need to more systematically assess whether treatment of OSA reduces the risk of CVE, particularly in light of increased sudden nocturnal cardiac death (typically characterized by cardiac electrophysiologic malfunction as a result of ventricular arrhythmias) noted during the usual sleeping hours of midnight to 6 am in those with sleep OSA compared with those without OSA.38
In adjusted analyses, a significant association was observed between the highest category of RDI and supraventricular tachycardia and 5 or more premature ventricular contractions per hour. We did not, however, observe associations of SDB with conduction delay arrhythmias in adjusted analyses, which is consistent with previously reported findings in the Sleep Heart Health Study.15 This differs from the reports of several small studies39,40 that have suggested that SDB is associated with bradyarrythmias and heart block, and which have given rise to a widely held notion that SDB is associated with heightened vagal tone. It is possible that the disparate findings are the result of differences in underlying comorbidities in clinic referrals compared with community-dwelling adults or differences in autonomic function in older individuals compared with the generally middle-aged patients reported in the literature.
The strengths of the current study include analysis of data from a large, community-based sample of older men, allowing inferences to be generalized to other community-dwelling male geriatric populations; rigorous, standardized data collection; scoring of arrhythmia outcome data blinded to respiratory disturbance data and status; and the ability to examine the full spectrum of SDB severity. Limitations of the study include the cross-sectional nature of the analyses, which precludes inference of causality, and assessment of nocturnal EKG data only, which does not allow us to assess the daytime occurrence of arrhythmias relative to SDB status. Another potential limitation is single-lead EKG examination, which did not allow us to effectively assess regional ST segment T-wave changes; however, this was not the focus of the current study. Self-report of key comorbid factors, such as HF and lack of objective data on cardiac function from measurements (eg, echocardiograms), may have contributed to misclassification of confounding conditions. Selection bias is a concern given that the MrOS Sleep Study is an ancillary cohort of a parent cohort; however, no difference in subject characteristics were noted in participants compared with nonparticipants; therefore, this is unlikely to represent a substantive limitation.
In summary, although there seems to be a monotonic increase in the prevalence of AF and CVE with increasing severity of SDB, there also seems to be a threshold effect such that moderate-to-severe SDB confers the greatest increased odds of clinically significant arrhythmia independent of self-reported HF and CVD. This line of investigation also identified hypoxia as the possible culprit pathophysiologic characteristic of SDB that may serve as the trigger of ventricular cardiac arrhythmia development in older men. The strong associations between CSA and AF suggest that CSA may be a sensitive marker of underlying abnormalities in autonomic or cardiac dysfunction associated with AF. Further prospective and intervention studies are needed to better determine causality and the impact of aggressive SDB interventions on cardiac outcomes.
Acknowledgments
Funding/Support: The following institutes provide support for the Osteoporotic Fractures in Men (MrOS) Study: the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the National Institute on Aging, the National Center for Research Resources, and National Institutes of Health Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140. The National Heart, Lung, and Blood Institute (NHLBI) provides funding for the MrOS Sleep ancillary study, Outcomes of Sleep Disorders in Older Men, under grant numbers R01 HL071194, R01 HL070848, R01 HL070847, R01 HL070842, R01 HL070841, R01 HL070837, R01 HL070838, and R01 HL070839. This work was also supported by NHLBI grant K23 HL079114, American Heart Association Scientific Development grant 0530188N, an American College of Chest Physicians–Associated Subspecialties T. Franklin Williams Geriatrics Development Award, and a Research Career Development Award (RCD 04-115-2) from the VA Office of Health Services Research and Development.
Footnotes
Author Contributions: All of the authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Mehra, Stone, Varosy, and Redline. Acquisition of data: Mehra, Stone, Varosy, Hoffman, Marcus, and Redline. Analysis and interpretation of data: Mehra, Stone, Varosy, Hoffman, Blackwell, Ibrahim, Salem, and Redline. Drafting of the manuscript: Mehra, Marcus, and Salem. Critical revision of the manuscript for important intellectual content: Stone, Varosy, Hoffman, Marcus, Blackwell, Ibrahim, and Redline. Statistical analysis: Stone, Varosy, and Blackwell. Obtained funding: Mehra, Stone, and Redline. Administrative, technical, and material support: Varosy and Redline. Study supervision: Stone, Hoffman, Marcus, Ibrahim, and Salem.
Financial Disclosure: Dr Varosy has performed research consulting for Atricure, Cierra, and BioNova, and has received honoraria from Sanofi-Aventis and Boston Scientific.
Additional Contributions: Liezl Concepcion and the Case Western Reserve University Reading Center staff, Susan Surovec, BA, Nancy Scott, BS, Jean Arnold, RPSGT, Joanna Romaniuk, MS, and Sinziana Seicean, MD, provided administrative assistance.
REFERENCES
- 1.Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96(4):1897–1904. doi: 10.1172/JCI118235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Somers VK, Dyken ME, Skinner JL. Autonomic and hemodynamic responses and interactions during the Mueller maneuver in humans. J Auton Nerv Syst. 1993;44(2–3):253–259. doi: 10.1016/0165-1838(93)90038-v. [DOI] [PubMed] [Google Scholar]
- 3.Arias MA, Alonso-Fernandez A, Garcia-Rio F, Sanchez A, Lopez JM, Pagola C. Obstructive sleep apnea in atrial fibrillation patients. Int J Cardiol. 2006;110(3):426. doi: 10.1016/j.ijcard.2005.09.039. [DOI] [PubMed] [Google Scholar]
- 4.Arias MA, Sanchez AM. Obstructive sleep apnea and its relationship to cardiac arrhythmias. J Cardiovasc Electrophysiol. 2007;18(9):1006–1014. doi: 10.1111/j.1540-8167.2007.00891.x. [DOI] [PubMed] [Google Scholar]
- 5.Flemons WW, Remmers JE, Gillis AM. Sleep apnea and cardiac arrhythmias: is there a relationship? Am Rev Respir Dis. 1993;148(3):618–621. doi: 10.1164/ajrccm/148.3.618. [DOI] [PubMed] [Google Scholar]
- 6.Gami AS, Friedman PA, Chung MK, Caples SM, Somers VK. Therapy insight: interactions between atrial fibrillation and obstructive sleep apnea. Nat Clin Pract Cardiovasc Med. 2005;2(3):145–149. doi: 10.1038/ncpcardio0130. [DOI] [PubMed] [Google Scholar]
- 7.Gami AS, Hodge DO, Herges RM, et al. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol. 2007;49(5):565–571. doi: 10.1016/j.jacc.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 8.Goldin JM, Naughton MT. Obstructive sleep apnoea induced atrial fibrillation. Intern Med J. 2006;36(2):136–137. doi: 10.1111/j.1445-5994.2006.01000.x. [DOI] [PubMed] [Google Scholar]
- 9.Guilleminault C, Connolly SJ, Winkle RA. Cardiac arrhythmia and conduction disturbances during sleep in 400 patients with sleep apnea syndrome. Am J Cardiol. 1983;52(5):490–494. doi: 10.1016/0002-9149(83)90013-9. [DOI] [PubMed] [Google Scholar]
- 10.Harbison J, O’Reilly P, McNicholas WT. Cardiac rhythm disturbances in the obstructive sleep apnea syndrome: effects of nasal continuous positive airway pressure therapy. Chest. 2000;118(3):591–595. doi: 10.1378/chest.118.3.591. [DOI] [PubMed] [Google Scholar]
- 11.Hoffstein V, Mateika S. Cardiac arrhythmias, snoring, and sleep apnea. Chest. 1994;106(2):466–471. doi: 10.1378/chest.106.2.466. [DOI] [PubMed] [Google Scholar]
- 12.Kanagala R, Murali NS, Friedman PA, et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589–2594. doi: 10.1161/01.CIR.0000068337.25994.21. [DOI] [PubMed] [Google Scholar]
- 13.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 14.Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31(8):1079–1085. [PMC free article] [PubMed] [Google Scholar]
- 15.Mehra R, Benjamin EJ, Shahar E, et al. Sleep Heart Health Study. Association of nocturnal arrhythmias with sleep-disordered breathing: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2006;173(8):910–916. doi: 10.1164/rccm.200509-1442OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163(1):19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 17.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034–2041. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 18.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–1078. [PMC free article] [PubMed] [Google Scholar]
- 19.Adamantidis MM, Caron JF, Dupuis BA. Triggered activity induced by combined mild hypoxia and acidosis in guinea-pig Purkinje fibers. J Mol Cell Cardiol. 1986;18(12):1287–1299. doi: 10.1016/s0022-2828(86)80432-1. [DOI] [PubMed] [Google Scholar]
- 20.Wang TM, Luk HN, Sheu JR, Wu HP, Chiang CE. Inducibility of abnormal automaticity and triggered activity in myocardial sleeves of canine pulmonary veins. Int J Cardiol. 2005;104(1):59–66. doi: 10.1016/j.ijcard.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 21.Gami AS, Pressman G, Caples SM, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110(4):364–367. doi: 10.1161/01.CIR.0000136587.68725.8E. [DOI] [PubMed] [Google Scholar]
- 22.Valham F, Mooe T, Rabben T, Stenlund H, Wiklund U, Franklin KA. Increased risk of stroke in patients with coronary artery disease and sleep apnea: a 10-year follow-up. Circulation. 2008;118(9):955–960. doi: 10.1161/CIRCULATIONAHA.108.783290. [DOI] [PubMed] [Google Scholar]
- 23.Ryan CM, Usui K, Floras JS, Bradley TD. Effect of continuous positive airway pressure on ventricular ectopy in heart failure patients with obstructive sleep apnoea. Thorax. 2005;60(9):781–785. doi: 10.1136/thx.2005.040972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS) Contemp Clin Trials. 2005;26(5):557–568. doi: 10.1016/j.cct.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study: a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26(5):569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Redline S, Sanders MH, Lind BK, et al. Sleep Heart Health Research Group. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep. 1998;21(7):759–767. [PubMed] [Google Scholar]
- 27.Whitney CW, Gottlieb DJ, Redline S, et al. Reliability of scoring respiratory disturbance indices and sleep staging. Sleep. 1998;21(7):749–757. doi: 10.1093/sleep/21.7.749. [DOI] [PubMed] [Google Scholar]
- 28.Yumino D, Bradley TD. Central sleep apnea and Cheyne-Stokes respiration. Proc Am Thorac Soc. 2008;5(2):226–236. doi: 10.1513/pats.200708-129MG. [DOI] [PubMed] [Google Scholar]
- 29.Javaheri S, Corbett WS. Association of low PaCO2 with central sleep apnea and ventricular arrhythmias in ambulatory patients with stable heart failure. Ann Intern Med. 1998;128(3):204–207. doi: 10.7326/0003-4819-128-3-199802010-00006. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. Geneva, Switzerland: World Health Organization; Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity. 2000 [PubMed]
- 31.Callaway CW, Chumlea WC, Bouchard C, et al. Circumferences. In: Lohman TG, Roche AF, Martorell R, editors. Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics Books; 1988. pp. 41–45. [Google Scholar]
- 32.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research: the Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22(5):667–689. [PubMed] [Google Scholar]
- 33.Resnick HE, Redline S, Shahar E, et al. Sleep Heart Health Study. Diabetes and sleep disturbances: findings from the Sleep Heart Health Study. Diabetes Care. 2003;26(3):702–709. doi: 10.2337/diacare.26.3.702. [DOI] [PubMed] [Google Scholar]
- 34.Leung RS, Huber MA, Rogge T, Maimon N, Chiu KL, Bradley TD. Association between atrial fibrillation and central sleep apnea. Sleep. 2005;28(12):1543–1546. doi: 10.1093/sleep/28.12.1543. [DOI] [PubMed] [Google Scholar]
- 35.Hanly PJ, Zuberi-Khokhar NS. Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure. Am J Respir Crit Care Med. 1996;153(1):272–276. doi: 10.1164/ajrccm.153.1.8542128. [DOI] [PubMed] [Google Scholar]
- 36.Lanfranchi PA, Braghiroli A, Bosimini E, et al. Prognostic value of nocturnal Cheyne-Stokes respiration in chronic heart failure. Circulation. 1999;99(11):1435–1440. doi: 10.1161/01.cir.99.11.1435. [DOI] [PubMed] [Google Scholar]
- 37.Javaheri S. Effects of continuous positive airway pressure on sleep apnea and ventricular irritability in patients with heart failure. Circulation. 2000;101(4):392–397. doi: 10.1161/01.cir.101.4.392. [DOI] [PubMed] [Google Scholar]
- 38.Gami AS, Howard DE, Olson EJ, Somers VK. Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med. 2005;352(12):1206–1214. doi: 10.1056/NEJMoa041832. [DOI] [PubMed] [Google Scholar]
- 39.Daccarett M, Segerson NM, Hamdan AL, Hill B, Hamdan MH. Relation of daytime bradyarrhythmias with high risk features of sleep apnea. Am J Cardiol. 2008;101(8):1147–1150. doi: 10.1016/j.amjcard.2007.11.068. [DOI] [PubMed] [Google Scholar]
- 40.Efremidis M, Sideris A, Kardaras F. Excessive sinus pauses and their elimination in a patient with sleep apnea syndrome. Int J Cardiol. 1998;67(3):265–266. doi: 10.1016/s0167-5273(98)00255-1. [DOI] [PubMed] [Google Scholar]