A 68-year-old woman presented with an episode of painless hematemesis that later progressed to retrosternal pain radiating to the epigastric area. She was taking acetylsalicylic acid as prophylaxis for cerebrovascular disease. The patient was hemodynamically stable, but her hemoglobin concentration was 81 (normal 120–150) g/L. After myocardial ischemia was excluded, an esophagogastroduodenoscopy showed multiple, sharply demarcated red lesions of varying sizes in the distal esophagus and large amounts of blood in the stomach (Figure 1A).
Figure 1.
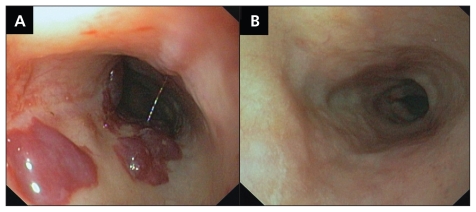
A) Endoscopy of the distal esophagus of a 68-year-old woman with hematemesis who was taking prophylactic acetylsalicylic acid. The image shows sharply demarcated lesions without evidence of bleeding. B) A repeat endoscopy performed 8 days later shows complete resolution of the esophageal lesions.
A repeat esophagogastroduodenoscopy performed the next day showed a small ulcer in the gastric body that had been missed during the first examination. Although some of the esophageal lesions remained unchanged, others had become areas of sloughed mucosa, consistent with spontaneous luminal rupture. The patient was given high-dose acid suppression therapy by continuous intravenous administration of pantoprazole 8 mg/h and transfused two units of packed red blood cells. The patient recovered uneventfully and her chest pain gradually subsided. A repeat endoscopy performed eight days later showed complete resolution of the esophageal lesions (Figure 1B).
Esophageal submucosal hematoma is an uncommon condition in the spectrum of esophageal injury ranging from mucosal tears (Mallory-Weiss syndrome) to transmural perforation (Boerhaave syndrome). Elderly patients who have intrinsic coagulopathies or are taking anticoagulant or antiplatelet medication are at higher risk for the condition. Patients may present with chest pain, dysphagia or hematemesis. Esophageal hematomas are usually secondary to traumatic injury caused by vigorous vomiting, ingestion of a toxic substance or foreign body, or complications of esophageal instrumentation.1 Our patient’s hematemesis was not due to esophageal hematoma, but rather to a bleeding ulcer. Acetylsalicylic acid therapy and changes in pressure in the esophageal wall related to vomiting likely contributed to formation of the hematoma.
Although unusual, esophageal hematoma is a potential cause of acute chest pain that may become more common given the increasing use of multiple antithrombotic agents. Early diagnosis can be challenging and relies on adequate imaging studies, such as computed tomography, unless additional symptoms prompt endoscopic evaluation.2 If endoscopy shows a large isolated hematoma, radiological exclusion of aortoesophageal fistula is warranted.3 Once the diagnosis is established, a conservative approach is usually appropriate because spontaneous luminal rupture followed by uncomplicated mucosal healing commonly occurs.4
Footnotes
Competing interests: None declared.
Previously published at www.cmaj.ca
This article has been peer reviewed.
REFERENCES
- 1.Ouatu-Lascar R, Bharadhwaj G, Triadafilopoulos G. Endoscopic appearance of esophageal hematomas. World J Gastroenterol. 2000;6:307–9. doi: 10.3748/wjg.v6.i2.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Restrepo CS, Lemos DF, Ocazionez D, et al. Intramural hematoma of the esophagus: a pictorial essay. Emerg Radiol. 2008;15:13–22. doi: 10.1007/s10140-007-0675-0. [DOI] [PubMed] [Google Scholar]
- 3.Maher MM, Murphy J, Dervan P, et al. Aortooesophageal fistula presenting as a submucosal oesophageal haematoma. Br J Radiol. 1998;71:972–4. doi: 10.1259/bjr.71.849.10195014. [DOI] [PubMed] [Google Scholar]
- 4.Nagai T, Torishima R, Nakashima H, et al. Spontaneous esophageal submucosal hematoma in which the course could be observed endoscopically. Intern Med. 2004;43:461–7. doi: 10.2169/internalmedicine.43.461. [DOI] [PubMed] [Google Scholar]