Summary
Restoration of a harmonious and pleasant appearance is a crucial aspect of surgical treatment for many congenital and acquired deformities of the face. A 38-year-old female patient with residual scarring on the right hemiface following evacuation of a odontogenic phlegmon underwent microsurgical reconstruction with a free adipofascial anterolateral thigh free flap. A stable result was achieved 7 years later. Thanks to adipofascial anterolateral thigh free flap fixation onto the periosteum a very good long-lasting aesthetic and dynamic result was obtained; this approach can be used in patients both with severe and mild abnormalities. Whereas many methods of facial contour restoration are described in the literature, in Authors’ opinion, microsurgical techniques are the gold standard unless contraindications; fasciocutaneous flaps, in particular, have shown the best aesthetic results since they can be sculptured to match the defect and stable anchoring is possible thanks to the thick fascia of the anterolateral thigh free flap.
Keywords: Hemifacial atrophy, Free flap, Anterolateral thigh free flap, Muscular fascia, Facial periosteum
Riassunto
Ristabilire un aspetto piacevole e armonioso è un aspetto cruciale nel trattamento chirurgico di molte deformità congenite ed acquisite della faccia. Una paziente di 38 anni con esiti cicatriziali a livello dell’emivolto destro in seguito a drenaggio di un flemmone odontogeno, è stata sottoposta ad intervento microchirurgico utilizzando il lembo anterolaterale di coscia. Viene mostrato il risultato stabile dopo sette anni. Grazie all’ancoraggio del lembo adipofasciale a livello del periostio è stato ottenuto un ottimo risultato estetico statico e dinamico duraturo nel tempo. Questo approccio chirurgico è applicabile in tutti i casi di atrofie facciali di grado medio-severo. Anche se in letteratura sono descritti diversi metodi per la correzione dei profili facciali, secondo gli Autori l’utilizzo delle tecniche microchirurgiche rappresenta il gold standard a meno di controindicazioni anestesiologiche; specialmente i lembi fasciocutanei hanno mostrato un risultato estetico superiore in quanto il sottocute può essere modellato in base al difetto da riempire e la fascia muscolare può essere ancorata in modo stabile al periostio, specialmente la fascia del lembo anterolaterale di coscia.
Introduction
The face presents man’s identity to others and functions, such as speech, mastication, deglutition and respiration, are strongly influenced by midface morbidity. Therefore, the aim in midface reconstruction is to minimize functional and aesthetic defects. Since a three-dimensional reconstruction of the skin, bone and mucosa complex may be necessary, technical difficulties may interfere with adequate midface reconstruction 1 2.
Several surgical procedures have been described for correction of soft tissue defects of the face, from lipofilling 3, to local flaps. Currently, thanks to a rapid development in functional refinements in microsurgical reconstructions 4 5 8, many free flaps have become popular in facial contouring such as the omental flap 6 7, the scapular and parascapular flap 9–11, the groin flap 12 and the deep inferior epigastric artery perforator flap 5. A consensus on the best method has not yet been reached and investigations to discover the ideal surgical procedure continue.
The reconstructed skin should have good tissue texture, colour match and sufficient subcutaneous tissue 1–4 8. To this end, it is advisable to use the pre-existing skin when possible. To improve mobility, free flaps have been used but these are too thick and colour match is very poor. The adipofascial anterolateral thigh free flap can be thinned in order to fit the mid face defect with no risk. The fascia is thick and resistant, allowing stable anchoring to the periosteum of the face with low donor site morbidity 4. Furthermore, a perfect colour match is obtained since the flap is covered by the facial skin.
Materials and methods
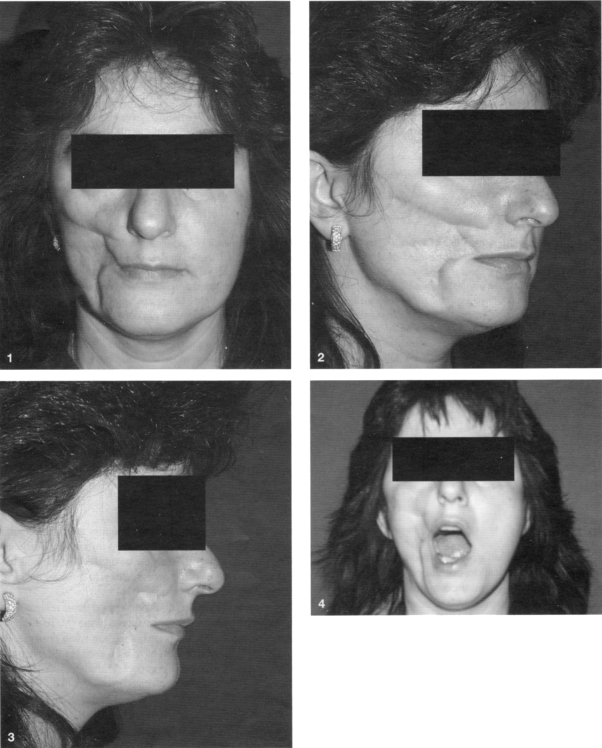
A 38-year-old female affected by a right Romberg’s Syndrome like lesion came to our attention, in March 1999. The hemiface deformity was the outcome of an odontogenic phlegmon occurring during an immunodepression state following a spinal marrow transplant on account of a B lymphoblastic lymphoma (Figs. 1–4). The residual scarring on the right hemiface involved primarily the buccal subunit of the cheek. Pre-operative electromyography confirmed facial nerve vitality. First of all, two lipofillings according to Coleman’s technique were performed, at intervals of six months, but the result was very unsatisfactory on account of complete re-absorption, in both cases, probably due to the scarred tissue. A 10 x 7 cm adipofascial anterolateral thigh free flap was harvested. More fascia was dissected to obtain a more stable and easier anchoring to the facial periosteum key points, planned pre-operatively. Before cutting the vascular pedicle of the flap, de-epithelialization, followed by trimming of excess fat tissue and a careful haemostasis, are recommended. The amount of soft tissue necessary to fit the facial defect was calculated pre-operatively by a virtual three-dimensional magnetic resonance. An artificial template was sculptured and sterilized in order to have a precise bench mark. The residual scarring from drainage of the phlegmon, on the outer cheek was chosen to fit the flap into the defect.
Fig. 1-4.
Pre-operative frontal, lateral, oblique and dynamic views.
The vascular anastomosis were harvested with facial artery and vein. The muscular fascia was sutured using non-absorbable material to the periosteum of the malar, orbitozygomatic, pyriform and mandibular periosteum to contrast against gravity. A small part of the flap, along the residual scarring, wasn’t de-epithelialized in order to have a sentinel for clinical monitoring together with ecocolordoppler in the post-operative. The post-operative was uneventful. Five days after surgery the patient was discharged. Liposuction of the cheek, with scar revision, were necessary to achieve good symmetry and very good results were obtained one year later (Figs. 5–8). The post-operative results are stable seven years later.
Fig. 5-8.
Frontal, lateral, oblique and dynamic results 7 years after surgery.
Discussion
The cheek is the largest aesthetic and functional unit of the face. Outlines differ, in each person, due to age, skeleton and quantity of adipose and muscular tissue. The characteristics of laxity and low rigidity of the cheek make it possible to adopt a wide variety of flaps but its close proximity to the lower eyelid, lips and nose represents a challenge since any alterations resulting from reconstruction may affect the function and symmetry of the entire hemiface 1–14.
Plastic surgeons can now correct the deformity thanks to various surgical techniques, from lipofilling, to local flaps and free tissue transfer.
Numerous cervical flaps have been reported with random flaps and platysmal flaps but with unpredictable results and poor mobility. Recently, Tan et al. 2 used the de-epithelialized submental flap: it is a skin-muscle flap successfully used to restore lower and midface defects but, in Authors’ opinion, the contour defect on the lower face deriving from rotation of the flap is too evident in the frontal and oblique view, and, therefore, not aesthetically acceptable in young patients; nevertheless, the pedicled submental flap remains a very good alternative in patients not candidate for microsurgery. Several microsurgery procedures are described: the omental flap offers good consistency, ideal for facial contour restoration when considering its pliability, but the most important disadvantage, in addition to the intra-abdominal harvest, is the lack of a muscular fascia thus lacking an ideal structure to be anchored to the facial periosteum obtaining a stable and long-lasting result 6 7. In most cases, re-operations and revisions of excess omentum are necessary since this flap is immediately well vascularized. The scapular or parascapular flaps are a good alternative but the muscular fascia is less thick, thus making flap positioning more difficult and often the scar at the donor site remains anti-aesthetic 9–11. The groin flap is the source of a large amount of skin and subcutaneous tissue; donor site morbidity is minimal but the vascular pedicle is rather short and the vascular anatomy can be complex 12.
Since the first description by Song et al., the anterolateral thigh free flap has become one of the ideal donor sites for soft tissue regeneration; the flap can be converted into an adipofascial flap, the skin excised and the fat trimmed to fit the facial defect 4. An extended approach to the vascular pedicle, when its maximum length was required, has been described 15. The muscular fascia, the thickest in the body, can be folded into variable thicknesses to correct contour defects of the medial and lateral canthus, eyelids and angle of the mouth to the inferior border of the mandible. Placing the flap on the periosteum avoids the shape being visible as well as possible displacement due to gravity thus improving patient satisfaction, as compared to subcutaneous positioning.
Furthermore, the placement over periosteum allows the upper muscular and fatty tissues natural mimic movements 1 that, together with the minimal atrophic tendency of this flap, increases post-operative aesthetic and functional results as well as surgeon’s satisfaction. Liposuction may be necessary to obtain a thinner flap and a more pleasant appearance, without risks.
As far as access is concerned, a pre-auricular rhytidectomy-like incision was excluded due to the risk of facial nerve injury 7–11 and since a greater dissection was necessary. A trans-buccal access, as described by Masaki 1, was not performed in order to avoid possible infection and the difficulty in fixing the flap to the periosteum in the malar and orbitozygomatic areas.
Conclusions
Coverage of facial defects is a challenge, because this area must match both skin colour and tissue texture. Minimal donor site morbidity, good mobility and a reliable flap are also recommended.
In Authors’ opinion, adipofascial anterolateral thigh free flap can be safely used for all restorations of the lower and midface, thus achieving a stable and long-lasting anchoring of the flap to the facial periosteum. Furthermore, the flap can be thinned and shaped as necessary to meet the needs of the facial defect. Donor site morbidity is minimal.
References
- 1.Masaki F. Correction of hemifacial atrophy using a free flap placed on the periosteum. Plast Reconstr Surg 2003;111:818-20. [DOI] [PubMed] [Google Scholar]
- 2.Tan O, Atik B, Parmaksizoglu D. Soft tissue augmentation of the middle and lower face using the de-epithelialized submental flap. Plast Reconstr Surg 2007;119:873-9. [DOI] [PubMed] [Google Scholar]
- 3.Mori A, Lo Russo G, Agostini T, Pattarino J, Vichi F, Dini M. Treatment of human immunodeficiency virus-associated facial lipoatrophy with lipofilling and submalar silicon implants. Plast Reconstr Surg 2006;59:1209-16. [DOI] [PubMed] [Google Scholar]
- 4.Agostini V, Dini M, Mori A, Franchi A, Agostini T. Adipofascial anterolateral thigh free flap for tongue repair. Br J Plast Surg 2003;56:614-8. [DOI] [PubMed] [Google Scholar]
- 5.Wang XC, Qiao Q, Liu ZF, Feng R, Zhang HL, Yan YJ, et al. Microsurgical tissue transfer for the reconstruction of hemifacial atrophy (Parry-Romberg syndrome). Zhonghua Zheng Xing Wai Ke Za Zhi 2006;22:433-5. [PubMed] [Google Scholar]
- 6.Wang X, Qiao Q, Liu Z, Zhao R, Zhang H, Yang Y, et al. Free anterolateral thigh adipofascial flap for hemifacial atrophy. Ann Plast Surg 2005;55:617-22. [DOI] [PubMed] [Google Scholar]
- 7.Asai S, Kamei Y, Nishibori K, Katoh T, Torii S. Reconstruction of Romberg disease defects by omental flap. Ann Plast Surg 2006;57:154-8. [DOI] [PubMed] [Google Scholar]
- 8.Losken A, Carlson GW, Culbertson JH, Scott Hultman C, Kumar AV, Jones GE, et al. Omental free flap reconstruction in complex head and neck deformities. Head Neck 2002;24:326-31. [DOI] [PubMed] [Google Scholar]
- 9.Vaienti L, Soresina M, Menozzi A. Parascapular free flap and fat grafts: combined surgical methods in morphological restoration of hemifacial progressive atrophy. Plast Reconstr Surg 2005;116:699-711. [DOI] [PubMed] [Google Scholar]
- 10.Ugurlu K, Ozcelik D, Hacikerim S, Karasoy A, Bas L. The combined use of flaps based on subscapular vascular system for unilateral facial deformities. Plast Reconstr Surg 2000;106:1079-89. [DOI] [PubMed] [Google Scholar]
- 11.Upton J, Albin RE, Mulliken JB, Murray JE. The use of scapular and parascapular flaps for cheek reconstruction. Plast Reconstr Surg 1992;90:959-71. [DOI] [PubMed] [Google Scholar]
- 12.Cooper TM, Lewis N, Baldwin MA. Free groin flap revisited. Plast Reconstr Surg 1999;103:918-24. [DOI] [PubMed] [Google Scholar]
- 13.Longaker MT, Siebert JW. Microvascular free-flap correction of severe hemifacial atrophy. Plast Reconstr Surg 1995;96:800-9. [DOI] [PubMed] [Google Scholar]
- 14.Stamatopoulos C, Panayotou P, Tsirigotou S, Ioannovich JD. Use of free flaps in the aesthetic reconstruction of face and neck deformities. Microsurgery 1992;13:188-91. [DOI] [PubMed] [Google Scholar]
- 15.Spyriounis PK. The extended approach to the vascular pedicle of the anterolateral thigh perforator flap: anatomical and clinical study. Plast Reconstr Surg 2006;117:997-1001. [DOI] [PubMed] [Google Scholar]