Abstract
OBJECTIVE
A1C ≥6.5% has been recently proposed as the defining criterion for diabetes. However, performance characteristics of this definition have not been described.
RESEARCH DESIGN AND METHODS
In the Insulin Resistance Atherosclerosis Study, we compared new to previous definitions of diabetes: 1999 World Health Organization (DM1999WHO) and 2003 American Diabetes Association based on fasting glucose alone (DMFPG126).
RESULTS
Participants with A1C ≥6.5%, DM1999WHO, and DMFPG126 were 44 (5.2%), 132 (15.4%), and 61 (7.1%), respectively. In individuals with DM1999WHO, mean, median, and interquartile range of A1C were 6.3, 5.9, and 5.5–6.6%, respectively; in individuals with DMFPG126, mean, median, and interquartile range of A1C were 7.0, 6.6, and 6.0–7.1%.
CONCLUSIONS
A1C ≥6.5% identifies fewer individuals than DM1999WHO or DMFPG126. Studies are needed to determine that A1C ≥6.5% compromises neither blood pressure and lipid management in early diabetes nor the implementation of lifestyle interventions for diabetes prevention.
An expert committee recently recommended using A1C as the preferred marker for diagnosing diabetes (≥6.5%) and detecting individuals at the highest risk for developing diabetes (6.0–6.4%) (1). Early definition attempts were based on a perceived bimodal glucose distribution in some populations (2) and later on the relationship between glucose levels and the presence of long-term complications, particularly retinopathy (3). A1C is now recommended, because A1C correlates well with retinopathy (4) and has superior technical attributes (less biological variability and more convenience by requiring no fasting or timed samples) (1). However, clinical consequences of A1C testing are not known.
In this study, we compared performance characteristics of the new definition relative to the 1999 World Health Organization (WHO) (DM1999WHO) (5) and 2003 American Diabetes Association (ADA) (DMFPG126) (6) definitions in the Insulin Resistance Atherosclerosis Study (IRAS) (5).
RESEARCH DESIGN AND METHODS
The design and methods of the IRAS have been previously described (7). The IRAS protocol was approved by local institutional review committees, and all participants provided written informed consent.
We used follow-up data (n = 855), because A1C was not measured at baseline. DMFPG126 was defined as fasting plasma glucose concentration ≥126 mg/dl (6) and DM1999WHO as fasting plasma glucose concentration ≥126 mg/dl and/or 2-h plasma glucose concentration ≥200 mg/dl (5). Individuals treated with antidiabetic medications were excluded. Indication for treatment with antihypertensive and LDL-lowering medications was examined using the Seventh Report of the Joint Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) and the National Cholesterol Education Program–Adult Treatment Panel III (NCEP-ATPIII) guidelines, respectively.
Logistic regression model was used to study the diagnostic performance of A1C using receiver operating characteristic (ROC) curves (SAS statistical software, version 9.1; SAS, Cary, NC).
RESULTS
The number of participants with A1C <6.0, 6.0–6.4, and ≥6.5% was 766 (89.5%), 45 (5.3%), and 44 (5.2%), respectively. A1C 6.0–6.4% and ≥6.5% categories had comparable insulin sensitivity index (0.45 ± 0.10 vs. 0.46 ± 0.76 × 10−4 min−1 · μU−1 · ml−1, P = 0.994) and metabolic syndrome prevalence (71.3% [56.0–82.9] vs. 80.5% [66.1–89.7], P = 0.519) (see supplementary Table 1 in the online appendix, available at http://care.diabetesjournals.org/cgi/content/full/dc09-1357/DC1). How- ever, acute insulin response was higher in the A1C 6.0–6.4% category (51.4 ± 6.3 vs. 27.2 ± 3.4 μU/ml, P < 0.001).
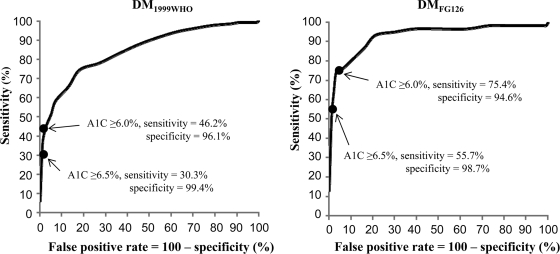
There were 132 (15.4%) individuals with DM1999WHO and 61 (7.1%) with DMFPG126. In individuals with DM1999WHO, mean, median, and interquartile range of A1C levels were 6.3, 5.9, and 5.5–6.6%, respectively; in individuals with DMFPG126, mean, median, and interquartile range of A1C levels were 7.0, 6.6, and 6.0–7.1%. The area under the ROC curve of A1C for identifying participants with DM1999WHO and DMFPG126 was 0.843 and 0.931, respectively (Fig. 1). Because of the low sensitivity and high specificity, A1C ≥6.5% was a strong indicator of the presence of DM1999WHO and DMFPG126; however, absence of A1C ≥6.5% could exclude neither. To a certain degree, results were similar for the 6.0% A1C threshold.
Figure 1.
ROC curves for detecting subjects with DM1999WHO or DMFPG126 for A1C. In subjects with A1C ≥6.5%, 40 had DM1999WHO and 4 did not; in subjects with A1C <6.5%, 92 had DM1999WHO and 719 did not. DMFPG126 was present and absent in 34 and 10 individuals with A1C ≥6.5%, respectively; corresponding numbers of individuals in the A1C <6.5% category were 27 and 784, respectively. DM1999WHO and DMFPG126 indicate type 2 diabetes by 1999 WHO and 2003 ADA criteria, respectively.
Among the 92 individuals with DM1999WHO and A1C <6.5, 75.8, and 82.6% met the criteria for antihypertensive (≥130/80 mmHg) and LDL-lowering treatment (LDL cholesterol ≥100 mg/dl), respectively. Because these individuals were considered nondiabetic by the new definition, only 56.0 and 59.1% fulfilled the requirements for treatment by JNC-7 (≥140/90 mmHg) and NCEP-ATPIII (based on global risk score) guidelines, respectively; consequently, 19.8 and 23.5% could potentially miss treatment.
CONCLUSIONS
The number of individuals identified by A1C ≥6.5% is one-third the number of individuals identified with the 1999 WHO criteria and 70% the number of individuals identified with the 2003 ADA criteria. Individuals with A1C 6.0–6.4% differ little from those with A1C ≥6.5% in terms of insulin resistance and metabolic syndrome, but have less β-cell dysfunction.
The question whether the new definition of diabetes (A1C ≥6.5%) improves previous attempts falls outside the scope of this study. Outcome data are needed. A1C correlates well with retinopathy (4), but 2-h glucose concentration better predicts mortality and/or cardiovascular disease than A1C and fasting glucose concentration in most studies (8–11) but not all (12). Our results indicate that A1C ≥6.5% is insensitive; therefore, this threshold could jeopardize treatment benefits of blood pressure and lipids in early diabetes.
Insulin resistance is, for the most part, fully developed, and β-cell function is largely compromised in individuals with impaired glucose tolerance (13). Because more than half of the individuals with DM1999WHO have A1C levels <6.0%, this A1C threshold has the potential of deemphasizing the implementation of lifestyle interventions with proven efficacy for preventing diabetes (14).
A significant limitation of our study is the use of single determinations of plasma glucose levels to diagnose diabetes. Concordance for obtaining fasting glucose concentration ≥126 mg/dl (or 2-h glucose concentration ≥140 mg/dl) in two different days is 70% (15). However, imprecision in measurement cannot explain much of the disparity between the new and 1999 WHO definitions.
In summary, the new definition identifies fewer individuals than the 1999 WHO definition. Studies are needed to demonstrate that the 6.5 and 6.0% A1C cut-points compromise neither the management of blood pressure and lipids in early diabetes nor the implementation of lifestyle interventions to delay the disease process. New and old definitions should be tested in studies with outcome data.
Supplementary Material
Acknowledgments
This study was supported by National Heart, Lung, and Blood Institute Grants HL-47887, HL-47889, HL-47890, HL-47892, and HL-47902 and the General Clinical Research Centers Program (NCRR GCRC, M01 RR431, M01 RR01346).
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009; 32: 1327– 1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vistisen D, Colagiuri S, Borch-Johnsen KDETECT-2 Collaboration. Bimodal distribution of glucose is not universally useful for diagnosing diabetes. Diabetes Care 2009; 32: 397– 403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997; 20: 1183– 1197 [DOI] [PubMed] [Google Scholar]
- 4.Tapp RJ, Tikellis G, Wong TY, Harper CA, Zimmet PZ, Shaw JEAustralian Diabetes Obesity and Lifestyle Study Group. Longitudinal association of glucose metabolism with retinopathy. Diabetes Care 2008; 31: 1349– 1354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization Department of Noncommunicable Disease Surveillance. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications: Report of a WHO Consultation Geneva, World Health Org., 1999 [Google Scholar]
- 6.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2003; 26 ( Suppl. 1): S5– S20 [DOI] [PubMed] [Google Scholar]
- 7.Wagenknecht LE, Mayer EJ, Rewers M, Haffner S, Selby J, Borok GM, Henkin L, Howard G, Savage PJ, Saad MF, Bergman RN, Hamman R. The Insulin Resistance Atherosclerosis Study: design, objectives and recruitment results. Ann Epidemiol 1995; 5: 464– 472 [DOI] [PubMed] [Google Scholar]
- 8.Barr EL, Boyko EJ, Zimmet PZ, Wolfe R, Tonkin AM, Shaw JE. Continuous relationships between non-diabetic hyperglycaemia and both cardiovascular disease and all-cause mortality: the Australian Diabetes, Obesity, and Lifestyle (AusDiab) study. Diabetologia 2009; 52: 415– 424 [DOI] [PubMed] [Google Scholar]
- 9.de Vegt F, Dekker JM, Ruhé HG, Stehouwer CD, Nijpels G, Bouter LM, Heine RJ. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia 1999; 42: 926– 931 [DOI] [PubMed] [Google Scholar]
- 10.Meigs JB, Nathan DM, D'Agostino RB, Sr, Wilson PWFramingham Offspring Study. Fasting and postchallenge glycemia and cardiovascular disease risk: the Framingham Offspring Study. Diabetes Care 2002; 25: 1845– 1850 [DOI] [PubMed] [Google Scholar]
- 11.Qiao Q, Dekker JM, de Vegt F, Nijpels G, Nissinen A, Stehouwer CD, Bouter LM, Heine RJ, Tuomilehto J. Two prospective studies found that elevated 2-hr glucose predicted male mortality independent of fasting glucose and HbA1c. J Clin Epidemiol 2004; 57: 590– 596 [DOI] [PubMed] [Google Scholar]
- 12.Park S, Barrett-Connor E, Wingard DL, Shan J, Edelstein S. GHb is a better predictor of cardiovascular disease than fasting or postchallenge plasma glucose in women without diabetes: The Rancho Bernardo Study. Diabetes Care 1996; 19: 450– 456 [DOI] [PubMed] [Google Scholar]
- 13.Defronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009; 58: 773– 795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DMDiabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393– 403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Selvin E, Crainiceanu CM, Brancati FL, Coresh J. Short-term variability in measures of glycemia and implications for the classification of diabetes. Arch Intern Med 2007; 167: 1545– 1551 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.