The rate of progression to new AIDS defining events has been reduced considerably since the introduction of potent antiretroviral combination therapy.1,2 It is unclear, however, whether the reduction has been the same for all opportunistic infections and malignancies, or whether the effect has been greater for some conditions than for others. We examined this question in the Swiss HIV Cohort Study, a large community cohort of adults with HIV infection.
Participants, methods, and results
The study methods are described in detail elsewhere.1,3 The cohort includes the majority of people with advanced HIV infection in Switzerland. Potent antiretroviral combination therapy (triple combinations including at least one protease inhibitor) was gradually introduced from 1995 onwards. By mid-1997, 70% of patients with a history of CD4 cell counts below 200 × 106/l were receiving this treatment.
The incidence of all new AIDS conditions fell from 157 events (95% confidence interval 148 to 166) per 1000 person-years in 1992 to 1994 (before combination therapy) to 35 events (26 to 45) in the year from July 1997 to June 1998. We analysed AIDS defining opportunistic and malignant events in separate Cox regression models, treating calendar periods as time dependent covariates and adjusting hazard ratios for transmission group, age, and CD4 cell count at baseline. Analyses were based on 6636 participants and 18 498 person-years of follow up.
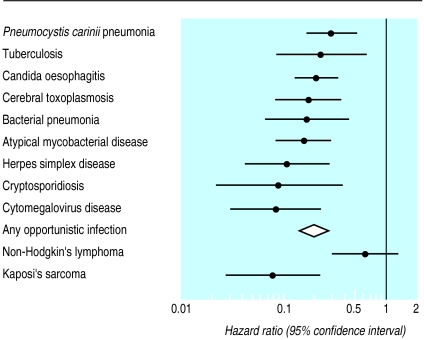
We found substantial reductions in rates of opportunistic events after the introduction of combination therapy. The figure shows hazard ratios for the common AIDS defining opportunistic infections (50 diagnoses or more), any AIDS defining opportunistic infection (1734 diagnoses), Kaposi’s sarcoma (258 diagnoses), and systemic non-Hodgkin’s lymphoma (110 diagnoses). The relative hazard for progression to any AIDS defining opportunistic infection was 0.20 (0.15 to 0.27), with little heterogeneity between infections. A substantial reduction was also observed for Kaposi’s sarcoma (0.08; 0.03 to 0.22). However, no significant trend was evident for non-Hodgkin’s lymphoma (0.61; 0.30 to 1.29), with the difference observed between the two malignancies unlikely to be the product of chance (P=0.002). Most non-Hodgkin’s lymphomas had intermediate or high grade histology and affected extranodal sites. Results for primary lymphoma of the brain were similar to those for non-Hodgkin’s lymphoma, but the number of cases was small (n=27) and confidence intervals were wide.
Comment
The incidence of both Kaposi’s sarcoma and non-Hodgkin’s lymphoma is increased over 100-fold among patients with AIDS,4 and these conditions are also more common among patients with other acquired or congenital immune defects. In addition to immunosuppression, other factors including Epstein-Barr virus infection, chronic antigen stimulation, and proto-oncogenes, have been implicated in the pathogenesis of the different clinical and histopathological manifestations of AIDS related non-Hodgkin’s lymphoma, whereas human herpes virus type 8 may be an infectious cofactor which is required for all forms of Kaposi’s sarcoma.5
Our data indicate that patients cease to be at risk of Kaposi’s sarcoma once immune function has been improved by combination therapy. Conversely, patients with a history of severe immunodeficiency continue to be at risk of non-Hodgkin’s lymphoma, despite antiretroviral combination therapy. Although the initiation of carcinogenesis requires an immunodeficient state, the factors promoting the development of non-Hodgkin’s lymphoma further along the causal chain do not seem to be related to immune function or are related to aspects not affected by antiretroviral combination therapy. Because of the large number of susceptible patients with a history of severe immunodeficiency, the fall in the incidence of non-Hodgkin’s lymphoma will probably lag behind that observed for other opportunistic diseases. Non-Hodgkin’s lymphoma will thus remain a relatively common complication among patients treated with antiretroviral combination therapy.
Supplementary Material
Figure.
Relative risk (hazard ratio) of AIDS defining opportunistic infections and malignancies, comparing 1992-4 (before introduction of potent antiretroviral combination therapy) with July 1997 to June 1998 (after introduction). Results from Cox regression models adjusted for transmission group, age, and CD4 cell count at baseline
Acknowledgments
We thank the patients for participating.
Footnotes
Funding: Swiss Federal Office of Public Health (Grant No 3600.010.1).
Competing interests: None declared.
website extra: Members of the Swiss HIV Cohort Study are listed on the BMJ’s website www.bmj.com
References
- 1.Egger M, Hirschel B, Francioli P, Sudre P, Wirz M, Flepp M, et al. for the Swiss HIV Cohort Study. Impact of new antiretroviral combination therapies in HIV infected patients in Switzerland: prospective multicentre study BMJ 19973151194–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mocroft A, Vella S, Benfield TL, Chiesi A, Miller V, Gargalianos P, et al. for the EuroSIDA Study Group. Changing patterns of mortality across Europe in patients infected with HIV-1 Lancet 19983521725–1730. [DOI] [PubMed] [Google Scholar]
- 3.Ledergerber B, von Overbeck J, Egger M, Lüthy R. The Swiss HIV cohort study: rationale, organization and selected baseline characteristics. Soz Praeventivmed. 1994;39:387–394. doi: 10.1007/BF01299670. [DOI] [PubMed] [Google Scholar]
- 4.Goedert JJ, Coté TR, Virgo P, Scoppa SM, Kingma DW, Gail MH, et al. Spectrum of AIDS-associated malignant disorders. Lancet. 1998;351:1833–1839. doi: 10.1016/s0140-6736(97)09028-4. [DOI] [PubMed] [Google Scholar]
- 5.Chang Y, Cesarman E, Pessin MS, Lee F, Culpepper J, Knowles DM, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi’s sarcoma. Science. 1994;266:1865–1869. doi: 10.1126/science.7997879. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.