Abstract
Background
Clinician-assigned New York Heart Association (NYHA) class is an established predictor of outcomes in heart failure. This study aims to test whether patients' self-assessment of functional status by NYHA class predicts hospital admissions, quality of life, and mortality.
Methods and Results
This was an observational study within a randomized controlled trial. A total of 293 adult patients diagnosed with heart failure were recruited after an emergency admission at 3 acute hospitals in Norfolk, UK. Outcome measures included number of emergency admissions over 6 months, self-assessed quality of life measured with the Minnesota Living with Heart Failure questionnaire (MLHFQ) and EQ-5D at 6 months, and deaths up to 20 months' follow-up. Patients were grouped into 3 NYHA groups (I/II, III, and IV) based on patients' self-assigned NYHA class (SA-NYHA). A Poisson model indicated an increased readmission rate associated with higher SA-NYHA class (adjusted rate ratio 1.21; 95% CI 1.04–1.41; P = .02). Higher SA-NYHA class at baseline predicted worse quality of life at 6 months' follow-up (P = .002 for MLHFQ; P = .047 for EQ-5D), and was associated with higher mortality rate (adjusted hazard ratio 1.84; 95% CI 1.10–3.06; P = .02).
Conclusions
SA-NYHA class is predictive of hospitalization, quality of life, and mortality among patients with heart failure.
Key Words: Heart failure, self-assessment, functional status, survival
The New York Heart Association (NYHA) classification is the most commonly used system to describe the impact of heart failure on a patient's daily activities.1 The classification was originally developed in 1928 and subsequently revised.2 It classifies patients with heart failure into 4 categories (I, II, III, IV), with higher class indicating more severe symptoms, limitation in physical activity, and worse health. Clinicians assign NYHA class on the basis of their indirect interpretation of reported patients' symptoms, medical history, and results from clinical tests on cardiac structure and function.3 Physician-assigned NYHA class has been shown to be predictive of outcomes in heart failure including hospitalization and mortality.4,5 However, because the NYHA classification involves doctors' subjective judgment of symptoms and clinical data, wide interobserver variability has been reported.6 Furthermore, disparities between clinician-assigned NYHA class and patient-reported limitation in function have been observed in a number of studies.7
The prognostic value of patients' own reports of their symptoms has received less attention in heart failure.8 One approach has been to derive NYHA class through responses to other brief patient-completed questionnaires. An early example is the Specific Activity Scale,6 a 5-item questionnaire assessing maximum physical activity. This scale has been shown to predict mortality. Nevertheless, a recent study demonstrated that patient assessed Specific Activity Scale levels did not appear to correlate with clinician assigned NYHA class.6 Similarly, a study deriving NYHA class from patient responses to the Kansas City Cardiomyopathy Questionnaire9 found only “slight agreement” with clinician-assigned NYHA class.10
Our recently completed trial11 asked patients to assign themselves an NYHA class using standard NYHA class descriptors, as opposed to other similar questions (eg, Specific Activity Scale, Kansas City Cardiomyopathy Questionnaire). This study sets out to examine whether patient-assigned NYHA class can predict patient outcomes in terms of mortality, hospital admission, and quality of life.
Methods
Study Design and Participants
This report is based on an observational (cohort) analysis within a randomized controlled trial. The methods of the HeartMed randomized controlled trial have been described in detail elsewhere.11 Briefly, a total of 293 adult patients, ages 42 to 95 years (mean 77 years, standard deviation 9.3), in whom heart failure was an important ongoing clinical condition, were recruited from 3 large district general hospitals in Norfolk after an emergency admission, and followed over 6 months. The intervention tested was 2 home visits by community pharmacists who reviewed medication and gave symptom self-management and lifestyle advice. The intervention did not lead to significant differences in the outcome measures (hospital admissions, survival, and quality of life) between the intervention and the control group. The objective of this additional observational analysis was to test whether the patients' self-assigned NYHA class (SA-NYHA) at baseline predicted outcomes.
Baseline Measures
Baseline measures included demographic and socioeconomic characteristics, medicines at recruitment, abbreviated mental test,12 clinical information (such as blood pressure), quality of life measures (EQ-5D13 and Minnesota Living with Heart Failure Questionnaire [MLHFQ ]14), and self-assigned NYHA classification (SA-NYHA). Wherever possible, patients were encouraged to classify themselves into 1 of the 4 SA-NYHA classes. However, where patients considered themselves unable (generally because of their poor health state or cognitive function) to classify themselves into an SA-NYHA class, this was recorded, and the researcher or the carer/relative then helped the patient complete this. The questionnaire used by patients is presented in Box 1 with SA-NYHA Class I at the top and Class IV at the bottom.15
Box 1. Self-completed Questionnaire on SA-NYHA Class of Heart Failure.
| Please tick one box containing the description which best summarizes your ability to do physical activity before coming into hospital: | |
| □ | I can perform all physical activity without getting short of breath or tired, or having palpitations. |
| □ | I get short of breath or tired, or have palpitations when performing more strenuous activities. For example, walking on steep inclines or walking up several flights of steps. |
| □ | I get short of breath or tired, or have palpitations when performing day to day activities. For example, walking on the flat. |
| □ | I feel breathless at rest, and am mostly housebound. I am unable to carry out any physical activity without getting short of breath or tired, or having palpitations. |
SA-NYHA, self-assigned New York Heart Association.
Outcome Measures
The outcome measures included number of emergency admissions to hospital over 6 months from randomization, quality of life (measured by a generic instrument [EQ-5D] and a disease-specific instrument [MLHFQ ]14), and mortality. Data on emergency admissions were obtained from Hospital Episode Statistics. The EQ-5D consists of 5 questions covering the domains mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.13 The EQ-5D is scored from −0.594 to +1, where +1 represents perfect health, 0 represents a state equivalent to death, and −0.594 the worst imaginable health state.13 The MLHFQ consists of 21 questions each scored from 0 to 5, and total scores vary from 0 to 105.14 For MLHFQ, higher scores imply worse quality of life, and a change of 5 points is considered to be clinically significant.16 In addition, the MLHFQ can provide a physical dimension score (calculated from 8 of the questions) and an emotional dimension score (calculated from 5 of the questions). To maximize response, the quality of life questionnaires were mailed up to 3 times to participants at both the 3- and the 6-month follow-up. Mortality data were collected from the Office for National Statistics from the study start up to September 30, 2005. This provided a minimum of 6 months of data for the last recruited subject, and up to 20 months of follow-up for those recruited at the start of the study.
Analysis
We examined differences among SA-NYHA groups. Few patients classified themselves as Class I (no limitation), and therefore this class was merged with Class II (mild limitation). Where there appeared to be no significant difference among the 3 groups, we merged Class III (moderate limitation) with Class IV (severe limitation) and tested the difference between SA-NYHA groups (I/II) and (III/IV). We used Poisson regression to compare the number of readmissions between the SA-NYHA groups (Poisson regression is a standard approach used for analyzing count data). We compared quality of life scores (EQ-5D and MLHFQ) at 6 months between SA-NYHA groups by using analysis of covariance adjusting for differences in baseline characteristics, and quality of life scores at baseline and 3 months. As an additional analysis, we investigated the association between SA-NYHA groups and both physical and emotional dimension scores of the MLHFQ. It should be noted that when analyzing EQ-5D scores, those who die are allocated a score of 0, which represents a state equivalent to death.13
Mortality data were analyzed using survival analysis comparing the SA-NYHA groups with the Cox proportional hazard ratio. The proportional hazards assumption was checked by inspection of “log-log” plots, Schoenfeld residual plots, and a chi-squared test using the Schoenfeld residuals.
For each analysis we first conducted an unadjusted analysis of the effect of SA-NYHA class on a given outcome (eg, admission). Then, for all multivariable analyses, we entered all the variables found to be significantly different between the SA-NYHA classes at baseline. Final models were obtained by stepwise removal of nonstatistically significant (P > .05) variables from the multivariable model, having started with all variables found to be at least of borderline statistical significance (P < .1) in our univariable analysis. The importance of trial group (ie, intervention or control) as a potential confounder of the effect of SA-NYHA class on each outcome was tested in all final models but was never found to be statistically significant. Stata version 9.0 was used.
Results
Baseline Characteristics
A total of 293 patients completed the SA-NYHA class questionnaire at baseline, and approximately equal numbers of patients fell into the 3 categories (I/II, III, IV). The baseline characteristics of these 3 SA-NYHA groups are presented in Table 1. Higher SA-NYHA class was associated with a larger proportion of patients living alone, greater number of medications taken daily, significantly higher number of patients treated with spironolactone, antiarrhythmic drugs, digoxin and higher dose of furosemide, or needing help with their medications. Patients from higher SA-NYHA groups also had longer length of stay in hospital and worse quality of life, measured by total MLHFQ score, both its physical and emotional dimensions, and by EQ-5D at baseline.
Table 1.
Baseline Comparison of SA-NYHA Groups of all Patients: Demographic and Clinical Variables
| Variable | SA-NYHA I/II (n = 97) Number (%) or Mean (SD) | SA-NYHA III (n = 99) Number (%) or Mean (SD) | SA-NYHA IV (n = 97) Number (%) or Mean (SD) | P Value (Chi-squared Test, Except where Indicated) |
|---|---|---|---|---|
| Female sex | 27 (27.8%) | 42 (42.4%) | 38 (39.2%) | P = .085 |
| Mean (SD) age (y) | 78.8 (8.2) | 76.8 (9.99) | 75.6 (9.2) | P = .052∗ |
| Living alone | 31 (32.0%) | 47 (47.5%) | 32 (33.0%) | P = .043 |
| Social class† | ||||
| High (I, II, IIINM)∗∗∗ | 53 (55.8%) | 50 (52.1%) | 36 (39.6%) | P = .069 |
| Abbreviated Mental Test | 9.32 (0.93) | 9.18 (1.34) | 9.18 (1.07) | P = .7208∗ |
| No. of prescribed drugs taken daily | 7.15 (2.15) | 7.52 (2.13) | 8.70 (2.78) | P < .001∗ |
| Help with medication‡ | 36 (38.7%) | 63 (64.3%) | 65 (68.4%) | P < .001 |
| Medication adherence aid§ | 13 (13.7%) | 22 (22.5%) | 26 (27.1%) | P = .070 |
| Medication at discharge includes: | ||||
| ACE inhibitor/angiotensin-2 receptor antagonist | 77 (79.4%) | 79 (79.8%) | 71 (73.2%) | P = .466 |
| Loop diuretic | 91 (93.8%) | 98 (99.0%) | 95 (97.9%) | P = .086 |
| Spironolactone | 28 (28.9%) | 40 (40.4%) | 46 (47.4%) | P = .028 |
| β-blocker | 45 (46.4%) | 38 (38.4%) | 31 (32.0%) | P = .118 |
| Antiarrhythmic drug | 9 (9.3%) | 8 (8.1%) | 18 (18.6%) | P = .048 |
| Warfarin | 36 (37.1%) | 33 (33.3%) | 31 (32.0%) | P = .735 |
| Antiplatelet drug | 53 (54.6%) | 51 (51.5%) | 50 (51.6%) | P = .882 |
| Digoxin | 22 (22.7%) | 40 (40.4%) | 34 (35.1%) | P = .026 |
| Furosemide dose (mg)‖ | 71.5 (38.0) | 84.5 (42.1) | 107.9 (72.5) | P < .001∗ |
| Systolic BP | 140.1 (28.6) | 133.5 (27.9) | 128.9 (23.7) | P = .02¶ |
| Diastolic BP | 79.1 (17.8) | 77.0 (15.2) | 73.8 (15.0) | P = .068¶ |
| Heart rate | 89.4 (27.1) | 92.2 (21.8) | 91.2 (20.1) | P = .70¶ |
| Sodium | 138.9 (3.8) | 137.7 (4.1) | 137.1 (4.7) | P = .008∗ |
| Creatinine | 132.8 (56.8) | 141.0 (65.9) | 139.0 (63.2) | P = .70∗ |
| Hemoglobin | 13.0 (2.2) | 12.5 (2.1) | 12.3 (2.1) | P = .04∗ |
| Body mass index | 25.9 (4.8) | 27.2 (5.4) | 28.3 (6.1) | P = .02∗ |
| Acute hospital length of stay at baseline (days) | 8.9 (7.1) | 12.7 (14.1) | 12.9 (10.9) | P = .004∗ |
| CCU/ICU/HDU admissions | 13 (13.4%) | 3 (3.03%) | 8 (8.3%) | P = .030 |
| MLHFQ total∗∗ | 31.5 (20.98) | 49.1 (21.3) | 57.1 (22.9) | P < .0001¶ |
| MLHFQ physical dimension | 14.9 (10.6) | 24.5 (9.3) | 28.1 (9.5) | P = .0001∗ |
| MLHFQ emotional dimension | 5.6 (5.8) | 9.1 (7.4) | 10.8 (7.6) | P = .0001∗ |
| EQ-5D | 0.72 (0.25) | 0.53 (0.32) | 0.47 (0.35) | P < .0001¶ |
SA-NYHA, self-assigned New York Heart Association; ACE, angiotensin-converting enzyme; BP, blood pressure; CCU, care unit; ICU, intensive care unit; HDU, high dependency unit; MLHFQ, Minnesota Living with Heart Failure questionnaire; EQ-5D.
Kruskal-Wallis test.
Social class data recorded for 281 patients.
Data recorded for 285 patients.
Data recorded for 288 patients.
Calculated for 248 patients.
Analysis of variance.
Calculated for 274 patients.
UK Registrar General's classification: I = professional, II = semi-professional, IIINM = skilled non-manual.
Participants could either complete our SA-NYHA questionnaire independently or with help from a trial researcher or a carer. In total, 157 (54%) completed it independently (SELF subgroup) and 135 (46%) needed help from the researcher or carer/relative to choose the statement which best described their functional status (HELP subgroup). For 1 patient, it was not recorded who completed the questionnaire. The baseline characteristics of these 2 subgroups are presented in Table 2. Those in the HELP group appeared to be of higher SA-NYHA class, though this was not statistically significant. However, the HELP subgroup were significantly more likely to be female, older, living alone, to have worse abbreviated mental test scores, to use a medication adherence aid, and to need help with their medication. The HELP group also reported a significantly lower (better) quality of life on the MLHFQ, but no difference was detected on the EQ-5D measure.
Table 2.
Baseline Comparison of SELF and HELP Groups of Patients: Demographic and Clinical Variables
| Variable | SELF (n = 157) Number (%) or Mean (SD) | HELP (n = 135) Number (%) or Mean (SD) | P Value (Chi-squared Test, except where Indicated∗) |
|---|---|---|---|
| SA-NYHA class | |||
| I/II | 54 (34.4%) | {43 (31.9%)} | P = .510 |
| III | 56 (35.7%) | {43 (31.9%)} | |
| IV | 47 (29.9%) | {49 (36.3%)} | |
| Female | 44 (28.0%) | 63 (46.7%) | P = .001 |
| Age | 75.67 (9.4) | 78.64 (8.9) | P = .0042∗ |
| Living alone | 51 (32.5%) | 59 (43.7%) | P = .049 |
| Social class - High (I, II, IIINM)† | 76 (49.7%) | 62 (48.4%) | P = .837 |
| Abbreviated Mental Test | 9.46 (0.76) | 8.95 (1.40) | P = .0011∗ |
| No. of prescribed drugs taken daily | 7.72 (2.3) | 7.87 (2.6) | P = .8438∗ |
| Help with medication‡ | 74 (49.0%) | 90 (67.2%) | P = .002 |
| Medication adherence aid§ | 26 (16.8%) | 35 (26.3%) | P = .048 |
| MLHFQ‖ | 52.7 (23.6) | 38.1 (22.4) | P < .001∗ |
| EQ-5D | 0.57 (0.31) | 0.57 (0.35) | P = .60 |
SA-NYHA, self-assigned New York Heart Association; MLHFQ, Minnesota Living with Heart Failure questionnaire; EQ-5D, quality of life questionnaire.
Mann-Whitney nonparametric test.
Social class data recorded for 281 patients (153 SELF and 128 HELP).
Data recorded for 285 patients (151 SELF and 134 HELP).
Data recorded for 288 patients (153 SELF and 133 HELP).
Calculated for 274 patients (147 SELF and 127 HELP).
Number of Hospital Readmissions
Two patients (0.7%) had incomplete Hospital Episode Statistics data as they moved outside the study area during follow-up. A total of 149 of the remaining 291 patients were readmitted to hospital at least once during the follow-up period with a total of 246 admissions (a mean of 0.85 admissions per patient). The distribution of admissions among the SA-NYHA groups is presented in Table 3. The unadjusted rate ratio for increasing SA-NYHA class was 1.21, and adjusted this was 1.26 (95% confidence interval [CI] 1.06–1.51, P = .01) when SA-NYHA class was considered as a continuous variable (I/II to III to IV). Table 3 presents the results with SA-NYHA considered categorically with SA-NYHA I/II compared against Class III and Class IV. In the final model, the following variables were also significantly associated with admission: number of drugs taken daily (increasing drugs associated with increased admission [rate ratio = 1.08]), antiarrhythmic drugs (use associated with fewer admissions [rate ratio = 0.56]), dose of furosemide (higher dose reducing admissions [rate ratio = 0.997]), diastolic blood pressure (higher blood pressure reducing admissions [rate ratio = 0.991]), and whether the patient had been admitted to intensive or coronary care units (admission increasing admission [rate ratio = 1.61]).
Table 3.
Number of Emergency Readmissions by SA-NYHA Group during 6 Months' Follow-up
| n | No. Admissions | Mean Rate | Unadjusted Rate Ratio vs SA-NYHA I/II (95% CI)∗ | Adjusted Rate Ratio vs. SA-NYHA 1/II (95% CI)† | |
|---|---|---|---|---|---|
| SA-NYHA I/II | 97 | 59 | 0.61 | 1.0 | 1.0 |
| SA-NYHA III | 98 | 98 | 1.0 | 1.64 (1.19–2.27, P = .003) | 1.56 (1.08–2.24, P = .02) |
| SA-NYHA IV | 96 | 89 | 0.93 | 1.52 (1.10–2.12, P = .012) | 1.64 (1.13–2.37, P = .008) |
SA-NYHA, self-assigned New York Heart Association.
†Poisson model after adjustment for differences in baseline characteristics among the SA-NYHA groups.
Assuming a linear effect, the overall rate ratio across the 3 groups is 1.21 (unadjusted) and 1.26 (adjusted).
Poisson model after adjustment for differences in baseline characteristics among the SA-NYHA groups
Separate analysis of re-admissions among the subgroup of patients who classified their SA-NYHA status themselves (SELF group) also identified that SA-NYHA I/II patients had the lowest rate of admissions. However, in this subgroup analysis only the difference between SA-NYHA III patients and SA-NYHA I/II patients was statistically significant after adjustment for baseline characteristics.
Quality of Life
SA-NYHA class was a significant predictor of quality of life of patients at 6 months of follow-up (Table 4) with higher (worse) SA-NYHA scores predicting worse quality of life at follow-up as measured by both the MLHFQ and the EQ-5D. It should be noted that MLHFQ was completed by 158 patients (66% of the participants who survived 6 months) and compared with patients who did not complete the MLHFQ at 6 months; those who did were slightly younger, had higher (better) abbreviated mental test scores, and were more likely to live alone (data available from the authors). In contrast, EQ-5D scores were completed by 214 patients at 6 months' follow-up with 54 additional patients included who died (given score of 0). Thus, EQ-5D scores were available on 91% of participants at 6 months (Table 4). Completers of EQ-5D were similar at baseline to noncompleters.
Table 4.
Mean MLHFQ Scores and EQ-5D Scores for SA-NYHA Groups (ALL Patients and SELF-assessed Patients) at Baseline and at 6 Months' Follow-up
| SA-NYHA I/II |
SA-NYHA III |
SA-NYHA IV |
|||||
|---|---|---|---|---|---|---|---|
| Mean Score (SD) | No. of Respondents | Mean Score (SD) | No. of Respondents | Mean Score (SD) | No. of Respondents | P Value | |
| ALL patients | |||||||
| MLHFQ at 6 months∗ | 29.1 (19.5) | 56 | 50.9 (28.4) | 51 | 60.0 (23.0) | 51 | P = .002† |
| EQ-5D at 6 months‡ | 0.60 (0.32) | 91 | 0.38 (0.36) | 90 | 0.34 (0.35) | 87 | P = .047† |
| SELF patients | |||||||
| MLHFQ at 6 months∗ | 28.9 (20.7) | 32 | 49.8 (28.4) | 32 | 62.2 (22.5) | 25 | P < .0001† |
| EQ-5D at 6 months‡ | 0.61 (0.33) | 51 | 0.37 (0.35) | 50 | 0.35 (0.35) | 42 | P = .11† |
MLHFQ, Minnesota Living with Heart Failure Questionnaire; EQ-5D; SA-NYHA: self-assigned New York Heart Association.
Low scores imply better health.
Analysis of variance adjusted for baseline differences.
High scores imply better health.
In both the univariable and the multivariable analysis adjusting for baseline differences among the 3 NYHA class groups, the mean MLHFQ scores at 6 months follow-up differed significantly among the 3 groups (unadjusted P < .0001, adjusted P = .002). In the final model, other significant predictors of 6-month MLHFQ score were 3-month MLHFQ scores, use of an antiarrhythmic (associated with better quality of life), and body mass index (higher body mass index was associated with worse quality of life). In the adjusted analysis, SA-NYHA Class I/II had MLHFQ scores a mean of 17.1 points lower (better) than SA-NYHA Class IV, and SA-NYHA Class III patients' scores were on average 7.3 points lower (better) than SA-NYHA Class IV. The adjusted R-squared for the final model was 0.75, whereas the model solely containing SA-NYHA class had an adjusted R-squared of 0.23; implying almost a quarter of the variance of the final MLHFQ results was explained by baseline SA-NYHA class. Similar results were found when the analysis was limited to those patients who self-classified their SA-NYHA class, though in this case our final model explained almost 90% of the variance, and both SA-NYHA III and SA-NYHA IV differed significantly from SA-NYHA I/II. It should be noted that due to missing values, both the adjusted models were calculated on approximately 30% of the participants. Finally, baseline SA-NYHA class was also found to predict both physical and emotional dimension scores of the MLHFQ at 6 months.
In both the univariable analysis and multivariable analysis of EQ-5D, results were significantly different among the 3 groups with mean scores of EQ-5D at 6 months higher (better) in those with lower SA-NYHA classes (unadjusted P < .0001, adjusted P = .047). When results were limited to self-completers, SA-NYHA class was no longer significantly associated with final EQ-5D score (adjusted P = .11).
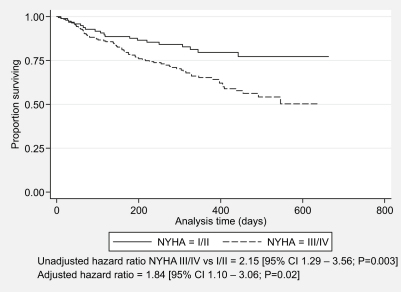
Mortality
Mortality data were available for all 293 patients. A total of 91 deaths (31.1%) from all causes occurred during follow-up. Lower self-assigned NYHA class was associated with lower mortality rate: 19.6% among SA-NYHA I/II group, 34.3% among SA-NYHA III, and 39.2% among SA-NYHA IV. Survival plots for the 3 groups showed similar survival between those classified as SA-NYHA III and IV and analysis demonstrated no statistically difference between these 2 groups, so these groups were merged. Survival analysis did demonstrate marked difference in survival between SA-NYHA I/II patients and those classified as III/IV (unadjusted hazard ratio = 2.15; 95% confidence interval 1.29 to 3.56, P = .002) (Fig. 1). Similar results were obtained after adjusting for baseline differences (hazard ratio = 2.03, 95% CI 1.22–3.39, P = .007) and when limited to those self-classifying their SA-NYHA class with unadjusted hazard ratio = 2.36 (adjusted hazard ratio = 2.69, 95% CI 1.33–5.45, P = .006). Inspection of Schoenfeld residual and “log-log” plots and a chi-squared test using the Schoenfeld residuals, suggested that the proportional hazards assumption was not violated.
Fig. 1.
Kaplan-Meier graph showing time to death in self-assigned New York Heart Association (SA-NYHA) Class I/II vs SA-NYHA III/IV groups (all patients).
Discussion
Clinician-assigned NYHA class is an established predictor of outcomes in heart failure.4,17,18 Our study has demonstrated that heart failure patients' own assessment of their NYHA class is also predictive of future outcomes. Higher (worse) self-assigned NYHA class was associated with increased hospitalization rates, worse quality of life, and decreased survival. Interestingly, the SA-NYHA classification in this study also predicted not only the physical dimension of the MLHFQ measure, but also the emotional dimension.
Usually the NYHA class is assigned by physicians or nurses based on their subjective interpretation of patients' cardiac symptoms, their interpretation of impact on daily activities, and the results of objective clinical investigations.1,2 There is no agreed-on method of assigning NYHA class. A limitation of the NYHA classification is its poor interobserver and intraobserver reproducibility. In a recent study, providers used a considerable variety of different questions and criteria to determine the NYHA classification.19 Furthermore, the interobserver concordance was little better than chance: for a series of 50 patients, 2 independent cardiologists assessors agreed on the NYHA class in only 54% of cases.19
It has been suggested that a way to improve its reliability may be to use the criteria as a patient self-report instrument.1 The NYHA classification is based on the main symptoms of heart failure (breathlessness, fatigue, and palpitations) as experienced by patients and the limitation in their physical activity resulting from their condition.3 Being subjective experiences, symptoms should in principle be most reliably elicited by asking patients directly. It has been argued that functional status may be appropriate for self-report because it is affected by a variety of psychological, social, and environmental influences experienced by the patient.1 Our study provides evidence that self-reported functional status has predictive validity.
An advantage of our study is that it explicitly describes the method used for assigning the SA-NYHA class. In contrast, a recent review showed that 99% of the reviewed papers did not reference the methods they used to distinguish between different classes of patients.19 An additional strength of our study is that the questionnaire is very brief and was derived directly from the NYHA criteria.
Our study was limited by there being no clinician assessment to compare with patients' own assessment. Furthermore, follow-up was reasonably brief (limited to 6 months) and only 54% of the patients could complete our SA-NYHA questionnaire themselves. Patients who needed help selecting their SA-NYHA class were more likely to be older, had worse abbreviated mental test scores, and needed help with their medication, indicating that further refinement of the questions is needed to make them clearer and easier to use by older or sicker patients. Equally on a positive side, researchers were generic health researchers or research nurses, none of whom had a background in cardiology implying that no specialist expertise was used to assign SA-NYHA class where help was given. A further weakness of our study was that in general we only identified differences between mild (SA-NYHA I/II) heart failure and moderate/severe (SA-NYHA III/IV) heart failure. We found little difference between SA-NYHA Class III and IV except for 1 quality of life measure. This finding is in line with previous research, which has often failed to find prognostic differences between NYHA Classes II and III or between NYHA Classes III and IV.20 Finally, our study measure was not validated against objective measures of functional capacity.
We are not aware of other published studies in which NYHA was assigned by directly asking patients to choose the NYHA class that best describes their condition. Our study supports earlier findings that patients' self-reported symptoms have predictive significance for outcomes in heart failure. NYHA functional class is a well known and simple risk stratification tool. We have demonstrated that it has a clinically significant predictive value when used directly by patients. Further research is necessary to refine the instrument for self-determining NYHA class and to validate it against objective measures of functional capacity in heart failure and clinician assessment. In conclusion, this study suggests that self-assigned NYHA class appears to predict patient outcome. It could be used by researchers who need a quick tool to stratify patients with heart failure, or by nonspecialist clinical staff needing a simple estimate of disease severity.
Acknowledgments
We thank Liz Lenaghan and Kate Ashton for coordinating the trial; Annie Blyth, Vivienne Maskrey, Bett Barrett, Julia Hill, Jane Trippett-Jones, Jeanette Blacklock, and Lisa Regan for their hard work recruiting patients and collecting data; our trial management group which included Lee Shepstone, Richard Smith, Alistair Lipp, Laura Hay, Amanda Howe and Clare Daly, and the study participants. We are also very grateful to British Heart Foundation for funding the HeartMed trial which provided the data for this study.
Footnotes
Research costs were funded by a project grant from the British Heart Foundation (Grant number: PG/02/171). Excess treatment costs were funded by Great Yarmouth and Southern Norfolk Primary Care Trusts. The HeartMed trial received support for the educational training events from Pfizer UK. All researchers are independent from the British Heart Foundation who funded this study and from Pfizer UK who funded the educational events for the trial intervention.
R.H. and B.R. designed this secondary analysis of the HeartMed trial data, K.S. wrote the first draft of the introduction for this paper, B.R. used that and produced the first full draft of the paper which was modified by R.H. I.B. and I.H. contributed to design and delivery of the original trial on which this subsequent analysis was based and all authors contributed to the final draft of this paper. R.H. is the guarantor for the data and this article.
Ethical approval: Norwich District, King's Lynn, and Great Yarmouth and Waveney local research ethics committees.
Conflict of interests: None.
References
- 1.Bennett J.A., Riegel B., Bittner V., Nichols J. Validity and reliability of the NYHA classes for measuring research outcomes in patients with cardiac disease. Heart Lung. 2002;31:262–270. doi: 10.1067/mhl.2002.124554. [DOI] [PubMed] [Google Scholar]
- 2.The Criteria Committee of the New York Heart Association . Functional capacity and objective assessment. In: Dolgin M., editor. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th ed. Little, Brown and Company; Boston, MA: 1994. pp. 253–255. [Google Scholar]
- 3.Ekman I., Cleland J.G., Andersson B., Swedberg K. Exploring symptoms in chronic heart failure. Eur J Heart Fail. 2005;7:699–703. doi: 10.1016/j.ejheart.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Madsen B.K., Hansen J.F., Stokholm K.H., Brons J., Husum D., Mortensen L.S. Chronic congestive heart failure. Description and survival of 190 consecutive patients with a diagnosis of chronic congestive heart failure based on clinical signs and symptoms. Eur Heart J. 1994;15:303–310. doi: 10.1093/oxfordjournals.eurheartj.a060495. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed A., Aronow W.S., Fleg J.L. Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J. 2006;151:444–450. doi: 10.1016/j.ahj.2005.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldman L., Hashimoto B., Cook E.F., Loscalzo A. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: advantages of a new specific activity scale. Circulation. 1981;64:1227–1234. doi: 10.1161/01.cir.64.6.1227. [DOI] [PubMed] [Google Scholar]
- 7.Ekman I., Cleland J.G., Swedberg K., Charlesworth A., Metra M., Poole-Wilson P.A. Symptoms in patients with heart failure are prognostic predictors: insights from COMET. J Card Fail. 2005;11:288–292. doi: 10.1016/j.cardfail.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Ekman I., Kjork E., Andersson B. Self-assessed symptoms in chronic heart failure—important information for clinical management. Eur J Heart Fail. 2007;9:424–428. doi: 10.1016/j.ejheart.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 9.Green C.P., Porter C.B., Bresnahan D.R., Spertus J.A. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35:1245–1255. doi: 10.1016/s0735-1097(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 10.Subramanian U., Weiner M., Gradus-Pizlo I., Wu J., Tu W., Murray M.D. Patient perception and provider assessment of severity of heart failure as predictors of hospitalization. Heart Lung. 2005;34:89–98. doi: 10.1016/j.hrtlng.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Holland R., Brooksby I., Lenaghan E., Ashton K., Hay L., Smith R. Effectiveness of visits from community pharmacists for patients with heart failure: HeartMed randomized controlled trial. BMJ. 2007;334:1098–1101. doi: 10.1136/bmj.39164.568183.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jitapunkul S., Pillay I., Ebrahim S. The abbreviated mental test: its use and validity. Age Ageing. 1991;20:332–336. doi: 10.1093/ageing/20.5.332. [DOI] [PubMed] [Google Scholar]
- 13.Rabin R., de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 14.Rector T.S., Cohn J.N. Assessment of patient outcome with the Minnesota Living with Heart Failure questionnaire: reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Pimobendan Multicenter Research Group. Am Heart J. 1992;124:1017–1025. doi: 10.1016/0002-8703(92)90986-6. [DOI] [PubMed] [Google Scholar]
- 15.Watson R., Gibbs C., Lip G. ABC of heart failure: clinical features and complications. BMJ. 2000;320:236–239. doi: 10.1136/bmj.320.7229.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rector T.S., Tschumperlin L.K., Kubo S.H., Bank A.J., Francis G.S., McDonald K.M. Use of the Living With Heart Failure questionnaire to ascertain patients' perspectives on improvement in quality of life versus risk of drug-induced death. J Card Fail. 1995;1:201–206. doi: 10.1016/1071-9164(95)90025-x. [DOI] [PubMed] [Google Scholar]
- 17.van den Broek S.A., van Veldhuisen D.J., de Graeff P.A., Landsman M.L., Hillege H., Lie K.I. Comparison between New York Heart Association classification and peak oxygen consumption in the assessment of functional status and prognosis in patients with mild to moderate chronic congestive heart failure secondary to either ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1992;70:359–363. doi: 10.1016/0002-9149(92)90619-a. [DOI] [PubMed] [Google Scholar]
- 18.Muntwyler J., Abetel G., Gruner C., Follath F. One-year mortality among unselected outpatients with heart failure. Eur Heart J. 2002;23:1861–1866. doi: 10.1053/euhj.2002.3282. [DOI] [PubMed] [Google Scholar]
- 19.Raphael C., Briscoe C., Davies J., Ian Whinnett Z., Manisty C., Sutton R. Limitations of the New York Heart Association functional classification system and self-reported walking distances in chronic heart failure. Heart. 2007;93:476–482. doi: 10.1136/hrt.2006.089656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bettencourt P., Ferreira A., Dias P., Pimenta J., Frioes F., Martins L. Predictors of prognosis in patients with stable mild to moderate heart failure. J Card Fail. 2000;6:306–313. doi: 10.1054/jcaf.2000.20558. [DOI] [PubMed] [Google Scholar]