Abstract
Objectives
To assess the effects of taking an intercalated degree (BSc) on the study habits and learning styles of medical students and on their interest in a career in medical research.
Design
Longitudinal questionnaire study of medical students at application to medical school and in their final year.
Setting
All UK medical schools.
Participants
6901 medical school applicants for admission in 1991 were studied in the autumn of 1990. 3333 entered medical school in 1991 or 1992, and 2695 who were due to qualify in 1996 or 1997 were studied 3 months before the end of their clinical course. Response rates were 92% for applicants and 56% for final year students.
Main outcome measures
Study habits (surface, deep, and strategic learning style) and interest in different medical careers, including medical research. Identical questions were used at time of application and in final year.
Results
Students who had taken an intercalated degree had higher deep and strategic learning scores than at application to medical school. Those with highest degree classes had higher strategic and deep learning scores and lower surface learning scores. Students taking intercalated degrees showed greater interest in careers in medical research and laboratory medicine and less interest in general practice than their peers. The effects of the course on interest in medical research and learning styles were independent. The effect of the intercalated degree was greatest in schools where relatively few students took intercalated degrees.
Conclusions
Intercalated degrees result in a greater interest in research careers and higher deep and strategic learning scores. However, the effects are much reduced in schools where most students intercalate a degree. Introduction of intercalated degrees for all medical students without sufficient resources may not therefore achieve its expected effects.
Key messages
Although intercalated degrees are well established, little is known about their effect on medical students
In this longitudinal study final year students who had taken intercalated degree were more interested in medical research, and had higher deep and strategic learning style scores than other students
The effects of the intercalated degree were dose dependent, being greatest in those gaining a first class degree
The effects of the intercalated degree were greatest in medical schools where a relatively small proportion of medical students took the degree.
Differences between medical schools are most easily explained by resource dilution
Introduction
About one third of medical students in the United Kingdom add an additional year to the basic five year undergraduate course and intercalate a degree in a medical science (generically a BSc). In some schools intercalated degrees are an integral part of a six year course. Intercalated degrees are controversial. Most recently, the Medical Research Council, in a “senseless sacrifice,”1 withdrew its funding for students2,3 despite a 1986 statement that: “most members of Council considered that intercalated awards were of the highest value in introducing future clinicians to research, and providing a cadre of graduates who were likely to become attracted to, and excel in, a career in academic medicine.”4
Although many medical teachers believe that intercalated degrees are beneficial, genuine doubt remains about its effect on attitudes and careers. Previous studies have found that medical academics tend to have intercalated a degree,5,6 and intercalating students may7 or may not4 perform better in final examinations. The problem of interpretation was emphasised by the Committee of Vice-Chancellors and Principals’ report into clinical academic careers: “the data ... do not (cannot) demonstrate that intercalated degrees cause students to take up academic careers ... it may be that those that are interested in academic research are those that seek to do the intercalated degree.”8
Although the literature has emphasised a research career as a principal outcome,5 intercalated degrees may have broader effects. Modern medicine emphasises self directed learning and critical evaluation, skills which may be acquired during an intercalated degree and are relevant to all doctors. Learning styles may therefore also be a useful outcome measure, emphasising not what has been learned but how and why learning is taking place.9–11 This study assesses the effect of an intercalated degree on learning styles and career preferences in a large prospective cohort of UK medical students and examines the effect of the degree in different medical schools.
Participants and methods
In a prospective, longitudinal study of medical student selection and training we studied 6901 applicants in 1990 for admission in 1991 to five UK medical schools.12 These applicants represented 71% of all applicants to UK medical schools in that year. We sent questionnaires to applicants with European addresses and received replies from 92% (5361/5845). Applicants were informed that participation was not compulsory and was independent of the selection process.
Of the cohort, 3333were admitted toany of the UK medical schools to which they had applied (that is, not only the five schools in the selection survey), 2961 in 1991 and 372 in 1992. In 1995 and 1996 all UK medical schools provided information on the progress of the 3333 entrants. A total of 3048 students had entered clinical courses, and 2695 were due to qualify in 1996 or 1997 and formed the subjects for the present study. The students were sent questionnaires about 3 months before final examinations (in 1996 or 1997). Response rate was 56% (1495/2695).
Learning styles (study habits) were assessed by an 18 item version of Biggs’s study process questionnaire,11,13–15 which has surface, deep, and strategic scales (box).10 Reliability coefficients (α) were 0.534, 0.721, and 0.637 in applicants and 0.591, 0.734, and 0.727 in final year students.
Summary of differences in motivation and study process of surface, deep, and strategic approaches to study
| Style | Motivation | Process |
| Surface | Completion of the course | Rote learning of facts and ideas |
| Fear of failure | Focusing on task components in isolation | |
| Deep | Little real interest in content | |
| Interest in the subject | Relate ideas to evidence | |
| Strategic | Vocational relevance | Integration of material across courses |
| Personal understanding | Identifying general principles | |
| Achieving high grades | Use techniques that achieve highest grades | |
| Competing with others | Level of understanding patchy and variable | |
| To be successful | ||
Career preferences were assessed by a questionnaire rating 27 specialty areas on a five point scale from “definite intention to go into this” through to “definite intention not to go into this,” scored 5 to 1.16 Previous factor analyses suggested seven factors (see table 2), for which mean scores were calculated. The item on medical research was also analysed separately. Academic achievement was coded as average A level grade (A=5; B=4; C=3; D=2; E=1; O/F=0) and number of A levels.
Table 2.
Mean (SD) scores for career preferences at time of application to medical school and in final year for students who did and did not take intercalated degree. Score of 5 indicates definite intention to go into specialty and 1 definite intention not to go into specialty
| Scale (component specialties) | Application
|
Final year
|
|||||
|---|---|---|---|---|---|---|---|
| BSc (n=739) | No BSc (n=1401) | Significance | BSc (n=429) | No BSc (n=1004) | Significance | ||
| Continuing hospital care (medicine in hospital (cardiology, neurology, etc); infectious diseases; obstetrics and gynaecology; genitourinary medicine; geriatrics) | 2.89 (0.52) | 2.91 (0.52) | t=−0.56, 2138 df, P=0.576 | 2.53 (0.57) | 2.52 (0.58) | t=0.33, 1431 df, P=0.744 | |
| Non-continuing hospital care (anaesthetics; ophthalmology; dermatology; radiology/radiotherapy) | 2.43 (0.48) | 2.42 (0.49) | 0.55, 2138 df, P=0.586 | 2.22 (0.57) | 2.22 (0.56) | t=−0.72, 1431 df, P=0.942 | |
| Surgery (neurosurgery, thoracic surgery, etc; traumatic and orthopaedic surgery; ear, nose, and throat) | 3.20 (0.67) | 3.17 (0.72) | t=1.25, 2138 df, P=0.213 | 2.31 (1.00) | 2.30 (1.01) | t=0.18, 1431 df, P=0.858 | |
| Laboratory medicine (microbiology, chemical pathology, haematology; pathology; medical research; basic medical sciences; pharmaceutical industry*) | 2.49 (0.69) | 2.41 (0.68) | t=2.58, 2138 df, P=0.010 | 1.77 (0.61) | 1.52 (0.49) | t=8.25, 1431 df, P<0.001 | |
| Administrative medicine (medical administration; public health*; pharmaceutical industry*; armed forces; forensic medicine; industrial medicine) | 2.07 (0.57) | 2.10 (0.55) | t=−1.48, 2138 df, P=0.139 | 1.57 (0.48) | 1.55 (0.46) | t=0.78, 1431 df, P=0.435 | |
| General practice (single handed; small partnership; large group or health centre; public health*) | 2.65 (0.83) | 2.78 (0.85) | t=−3.52, 2138 df, P<0.001 | 2.27 (0.83) | 2.46 (0.88) | t=−3.83, 1431 df, P<0.001 | |
| Psychiatry | 2.88 (1.05) | 2.89 (1.02) | t=−0.23, 2138 df, P=0.815 | 2.31 (1.12) | 2.32 (1.12) | t=−0.14, 1431 df, P=0.887 | |
| Medical research | 2.73 (1.08) | 2.60 (1.05) | t=2.67, 2138 df, P=0.008 | 2.18 (1.10) | 1.71 (0.88) | t=8.65, 1431 df, P<0.001 | |
Item included in two scales and therefore weighted by a half.
The proportion of students taking intercalated degrees differs between medical schools (a “compositional variable”17). We used multilevel modelling to assess the effect of this factor using final year strategic learning score as the response variable, allowing random variation at student and medical school level, and fixed effects of strategic learning at application, A level attainment, the taking of a BSc, the proportion of students at a school taking a BSc, and the interaction of the last two measures.
We used spss for windows version 8.0 for conventional statistical analysis and MLn for multilevel modelling.17,18 Missing values, which represented about 1% of the questionnaire responses, were replaced by means when appropriate. Denominators are not always equal because of missing values. Significance tests from multiple regression and multilevel modelling are reported as z statistics (estimate/standard error).
Results
Intercalated degrees were taken by 904/2695 (33.5%) of the students. Degree classes were known for 795 students: 166 (20.9%) gained a first, 532 (66.9%) a 2.1, 86 (10.8%) a 2.2, and 11 (1.4%) a third, pass degree, or fail.
Learning styles
Students who subsequently took intercalated degrees had significantly lower surface learning scores at application to medical school and significantly higher A level grades and number of A levels than those who did not (table 1). Final year students who had taken intercalated degrees had higher deep and strategic learning scores (table 1). After scores at application were partialled out, final year students who had taken an intercalated degree had higher deep (z=3.73, P<0.001) and strategic (z=4.56; P<0.001) scores (but not lower surface scores (z=0.546, P=0.585)) than those who had not taken an intercalated degree. Significance remained similar after A level results were taken into account.
Table 1.
Study habits at time of application and in final year and A level results for students taking or not taking an intercalated degree
| BSc
|
No BSc
|
Significance (BSc v No BSc)* | ||||
|---|---|---|---|---|---|---|
| No of students | Mean (SD) | No of students | Mean (SD) | |||
| Surface learning score: | ||||||
| Application | 839 | 12.84 (3.49) | 1603 | 13.33 (3.88) | t=−3.04, 2440 df, P=0.0002 | |
| Final year | 434 | 13.78 (3.69) | 1012 | 14.07 (3.81) | t=−1.32 1444 df, P=0.187 | |
| Deep learning score: | ||||||
| Application | 839 | 21.29 (4.16) | 1603 | 21.10 (4.29) | t=1.02, 2440 df, P=0.307 | |
| Final year | 434 | 19.17 (4.32) | 1012 | 18.17 (4.40) | t=4.00, 1444 df, P<0.001 | |
| Strategic learning score: | ||||||
| Application | 839 | 23.10 (4.12) | 1603 | 22.75 (4.21) | t=1.93, 2440 df, P=0.053 | |
| Final year | 434 | 16.26 (5.11) | 1012 | 14.81 (4.93) | t=5.10, 1444 df, P<0.001 | |
| Mean A level grade | 890 | 4.36 (0.641) | 1716 | 4.07 (0.705) | t=9.51, 2604 df, P<0.001 | |
| No of A levels | 904 | 3.43 (0.948) | 1789 | 3.34 (1.15) | t=2.05, 2691 df, P=0.041 | |
Unpaired t tests.
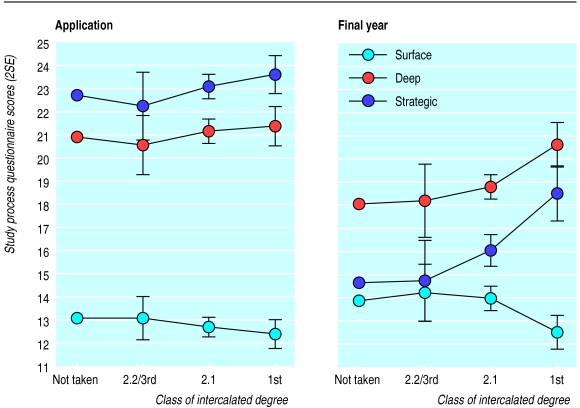
Surface, deep, and strategic learning showed linear trends on class of intercalated degree attained (z=−2.67, 2.21, and 4.51; P=0.008, 0.027, and <0.001 respectively) after scores at application were partialled out (figure 1).
Figure 1.
Surface, deep, and strategic learning scores at application and in final year in students who did and did not take intercalated degree and according to degree class. Note: absolute differences in separate scores should be considered arbitrary
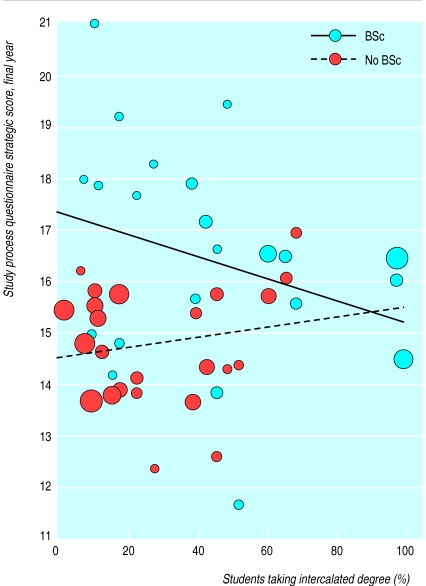
The average proportion of students taking an intercalated degree at a medical school was 36% (n=28; SD 29%; median 26%; interquartile range 12-51%; range 2-100%). The interaction between the effect of taking a BSc on strategic learning and the proportion of students taking a BSc was significant (z=2.47, P=0.014; fig 2), the effect of the BSc being greater in schools where fewer students took it. Regression on proportion of students intercalating a degree was significantly negative in those taking a BSc (z=2.57, P=0.010) but not significant in those not taking a BSc (z=0.79, NS).
Figure 2.
Average final year strategic learning score for medical students who did and did not take an intercalated in relation to percentage of students in each school taking degree. Average number of students at a school who were in our study and taking a BSc was 16.4 (SD 17.6; median 9; interquartile range 6-24; range 1-70), and number not taking a BSc was 35.6 (SD 21.2; median 36; interquartile range 18-49; range 1-79). Regression lines were calculated with all data points, but points are plotted only for schools with at least four students in that category. Size of points is proportional to number of students at school
Career preferences
At application to medical school, students who subsequently took an intercalated degree had a higher preference for laboratory medicine and a lower preference for general practice (table 2) and were more interested in medical research (tables 2 and 3). Final year medical students who had taken an intercalated degree had higher preferences for laboratory medicine and medical research and lower preferences for general practice, the effect remaining significant after scores at entry and A levels were partialled out. Students gaining higher degree classes had a greater interest in medical research (z=7.98, P<0.001) and laboratory medicine (z=7.31, P<0.001) and a decreased interest in general practice (z=−3.32, P=0.001) after scores at application were partialled out.
Table 3.
Attitude towards medical research as a career at time of application to medical school and in final year in relation to intercalated degree being taken or not. Values are numbers (percentages) of students
| Application*
|
Final year†
|
||||
|---|---|---|---|---|---|
| BSc (n=807) | No BSc (n=1531) | BSc (n=426) | No BSc (n=1000) | ||
| Definite intention to go into | 28 (4) | 47 (3) | 12 (3) | 5 (1) | |
| Very attractive | 198 (25) | 292 (19) | 44 (10) | 37 (4) | |
| Moderately attractive | 230 (29) | 478 (31) | 100 (23) | 140 (14) | |
| Not very attractive | 243 (30) | 478 (31) | 125 (29) | 299 (30) | |
| Definite intention not to go into | 108 (13) | 236 (15) | 145 (34) | 519 (52) | |
U=581 024, z=−2.45, P=0.014 for difference between BSc and no BSc (Mann-Whitney U test).
U=1 753 770, z=−7.81, P<0.001 for difference between BSc and no BSc (Mann-Whitney U test).
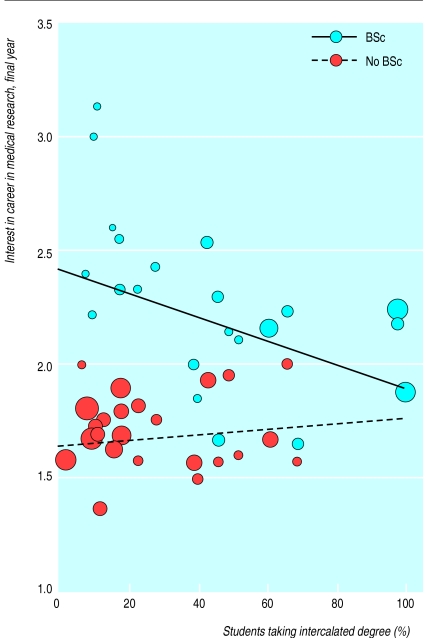
Analysis of difference between medical schools was restricted to interest in medical research. Multilevel modelling showed that after research career at application to medical school, mean A level grade, and number of A levels were partialled out there was a significant interaction between the effect of taking an intercalated degree and the proportion of students in each medical school taking an intercalated degree (fig 3; z=2.60, P=0.010); a significant negative association was seen in those taking an intercalated degree (z=−3.65, P<0.001) and no association in those not taking a degree (z=0.27, NS).
Figure 3.
Average final year score for interest in a career in medical research for students who did and did not take an intercalated degree in relation to percentage of students in each school taking degree. Regression lines were calculated with all data points, but points are plotted only for schools with at least four students in that category. Size of points is proportional to number of students at school
Relation between study habits and career preferences
Since taking an intercalated BSc affects both study habits and career preferences, it is important to ask if the effects are independent or mediated.19 For individual students, regression of strategic learning on taking an intercalated degree was significant after strategic learning at application and interest in medical research at application and final year were partialled out (z=3.95, P<0.001); similarly, an intercalated degree was significantly related to interest in medical research, after interest in medical research at application and strategic learning at application and final year were partialled out (z=7.20, P<0.001). At medical school level, the proportion of students taking a BSc remained significant after covarying the other variable (effect on strategic learning, z=2.12, P=0.034; effect on career in medical research, z=3.34, P<0.0001). Intercalated degrees therefore have independent effects on study habits and career preferences at student and medical school level.
Discussion
This study provides evidence that students taking an intercalated degree are more interested in medical research and also favour deep and strategic learning. The effect on learning has broad implications for medical education since these learning techniques could benefit all doctors. The benefits of the intercalated degree were present 3 years after it had been taken and might be expected to last much longer. Because our study is longitudinal, the hypothesis that the effects of an intercalated degree are due to self selection8 can largely be discounted. Although detailed results cannot be presented here, there was no evidence that final year respondents were substantively different from non-respondents based on scores at application. This was also found in our previous studies.20
Differences between medical schools
A simple reading of our overall data might suggest that all medical students should take an intercalated degree. This is already the case at Oxford, Cambridge, and Nottingham and is being implemented at Imperial College School of Medicine and Royal Free and University College Medical School. Our large sample size, coupled with multilevel modelling, allowed comparison of medical schools. As more students in a medical school take an intercalated degree the benefit decreases. The mechanism of this effect cannot be elucidated from our data, but a possible explanation is dilution of resources: as proportionately more students take an intercalated degree there are fewer resources for each student, each member of staff supervising more students. If this hypothesis is correct, proper resourcing of intercalated degrees is necessary for them to be effective.
Direction of effects
It might be argued that our study does not show positive effects of the intercalated degree, but rather that the degree mitigates the negative effects of the rest of the course, preventing a fall in deep and strategic learning and decreased interest in research. That is possible. The effects of the other five years of the course are, however, more difficult to study, since all students take all components of it, and the effects are heavily confounded by maturational and age related changes.21
Most of the students in our study were taking a traditional curriculum, but many medical schools are now introducing curriculums containing problem based learning.22 These may themselves increase deep and strategic learning.23–26 Nevertheless, the intercalated degree remains an option in most new curriculums. Our study provides a baseline from which to determine whether new curriculums will increase deep and strategic learning in their own right.
Evidence based medical education
Although intercalated degrees have been encouraged and funded for many decades, this is the first prospective study assessing their impact. If medical education is to be based on evidence rather than mere custom, funding must be found for similar systematic studies of new curriculums.
Acknowledgments
We thank Ms Agni Keeling for data entry, the deans and academic registrars of UK medical schools for help in following up students, and the students for completing the lengthy questionnaires.
Footnotes
Funding: The Department of Health funded the study of final year students, and the Leverhulme Trust, the Nuffield Foundation, and the Department of Health funded the study of student selection.
Competing interests: None declared.
References
- 1.Smith R. A senseless sacrifice: the fate of intercalated degrees. BMJ. 1986;292:1619–1620. doi: 10.1136/bmj.292.6536.1619-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tamber PS. MRC withdraws intercalated degree funds. BMJ. 1996;312:1117–1118. [Google Scholar]
- 3.Attwell D, Boyd R. Withdrawal of medical research council funding for intercalated BSc students. Lancet. 1996;348:198. doi: 10.1016/s0140-6736(05)66145-4. [DOI] [PubMed] [Google Scholar]
- 4.Tait N, Marshall T. Is an intercalated BSc degree associated with higher marks in examinations during the clinical years? Med Educ. 1995;29:216–219. doi: 10.1111/j.1365-2923.1995.tb02833.x. [DOI] [PubMed] [Google Scholar]
- 5.Evered DC, Anderson J, Griggs P, Wakeford R. The correlates of research success. BMJ. 1987;295:241–246. doi: 10.1136/bmj.295.6592.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eaton DG, Thong YH. The bachelor of medical science research degree as a start for clinician-scientists. Med Educ. 1985;19:445–451. doi: 10.1111/j.1365-2923.1985.tb01352.x. [DOI] [PubMed] [Google Scholar]
- 7.Wyllie AH, Currie AR. The Edinburgh intercalated honours BSc in pathology: evaluation of selection methods, undergraduate performance, and postgraduate career. BMJ. 1986;292:1646–1648. doi: 10.1136/bmj.292.6536.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Committee of Vice-Chancellors and Principals. Clinical academic careers: report of an independent task force. London: CVCP; 1997. [Google Scholar]
- 9.Entwistle N. Styles of learning and teaching. Chichester: John Wiley; 1981. [Google Scholar]
- 10.Newble DI, Entwistle NJ. Learning styles and approaches: implications for medical education. Med Educ. 1986;20:162–175. doi: 10.1111/j.1365-2923.1986.tb01163.x. [DOI] [PubMed] [Google Scholar]
- 11.Biggs JB. Student approaches to learning and studying. Melbourne: Australian Council for Educational Research; 1987. [Google Scholar]
- 12.McManus IC, Richards P, Winder BC, Sproston KA, Styles V. Medical school applicants from ethnic minorities: identifying if and when they are disadvantaged. BMJ. 1995;310:496–500. doi: 10.1136/bmj.310.6978.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Biggs JB. Study process questionnaire: manual. Melbourne: Australian Council for Educational Research; 1987. [Google Scholar]
- 14.O’Neil MJ, Child D. Biggs’ SPQ: a British study of its internal structure. Br J Educ Psychol. 1984;54:228–234. [Google Scholar]
- 15.Biggs JB. What do inventories of students’ learning processes really measure? A theoretical review and clarification. Br J Educ Psychol. 1993;63:3–19. doi: 10.1111/j.2044-8279.1993.tb01038.x. [DOI] [PubMed] [Google Scholar]
- 16.Crimlisk H, McManus IC. The effect of personal illness experience on career preference in medical students. Med Educ. 1987;21:464–467. doi: 10.1111/j.1365-2923.1987.tb01403.x. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein H. Multilevel statistical models. London: Arnold; 1995. [Google Scholar]
- 18.Woodhouse G. Multilevel modelling applications: a guide for users of MLn. London: Multilevel Models Project, Institute of Education; 1996. [Google Scholar]
- 19.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. J Personality Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 20.McManus IC, Richards P, Winder BC, Sproston KA. Clinical experience, performance in final examinations, and learning style in medical students: prospective study. BMJ. 1998;316:345–350. doi: 10.1136/bmj.316.7128.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McManus IC. Medical students: origins, selection, attitudes and culture [ MD thesis]. London: University of London; 1985. [Google Scholar]
- 22.General Medical Council. Tomorrow’s doctors: recommendations on undergraduate medical education. London: GMC; 1993. pp. 1–28. [Google Scholar]
- 23.Coles CR. Differences between conventional and problem-based curricula in their students’ approaches to studying. Med Educ. 1985;19:308–309. doi: 10.1111/j.1365-2923.1985.tb01327.x. [DOI] [PubMed] [Google Scholar]
- 24.Vernon DTA, Blake RL. Does problem-based learning work? A meta-analysis of evaluative research. Acad Med. 1993;68:550–563. doi: 10.1097/00001888-199307000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Albanese MA, Mitchell S. Problem-based learning: a review of literature on its outcomes and implementation issues. Acad Med. 1993;68:52–81. doi: 10.1097/00001888-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Mårtenson DF. Students’ approaches to studying in four medical schools. Med Educ. 1986;20:532–534. doi: 10.1111/j.1365-2923.1986.tb01395.x. [DOI] [PubMed] [Google Scholar]