The increase in high technology medicine, complex surgical techniques, and use of immunosuppressive agents means that more patients are managed with broad spectrum antibiotics. Such regimens may contribute to the emergence of multidrug resistant micro-organisms,1 and many authorities are now rationalising use of antibiotics in hospital to try to limit the spread of antibiotic resistant organisms. For this strategy to be successful, however, it should be combined with attempts to limit the requirement for antibiotic treatment in patients in hospital.1
Recent studies indicate that many inpatients may be predisposed to infectious complications because of altered host defences. A subgroup of adults in intensive care with severe sepsis has been shown to express low amounts of HLA-DR on circulating monocytes; this was associated with a relatively immunodeficient state termed monocyte deactivation2 or immunoparalysis. These patients improved after being given the cytokine interferon gamma. These observations suggest that focusing on host defences may provide an additional strategy for reducing antimicrobial resistance in hospitals.
Subjects, methods, and results
We undertook a prospective study of admissions to the paediatric intensive care unit to determine whether monocyte deactivation also occurred in critically ill children. Monocyte HLA-DR expression was determined by flow cytometric analysis of 50 μl of blood after staining with fluorochrome labelled monoclonal antibodies against HLA-DR and CD14. A minimum of 2000 monocyte events was collected and the results expressed as median fluorescence intensity.
We studied five groups: 23 consecutive admissions to the paediatric intensive care unit for single system failure (isolated head injury, bronchiolitis due to infection with respiratory syncitial virus, and viral laryngotracheobronchitis); 18 consecutive admissions for severe sepsis and multiple organ system failure3 with three or more systems failing, nine patients being studied further in follow up outpatient visits 14-28 days after admission; 11 children undergoing routine outpatient investigations; and five healthy adult laboratory staff. Analysis was performed within 18 hours of admission and repeated roughly 48 hourly for patients with multiorgan system failure.
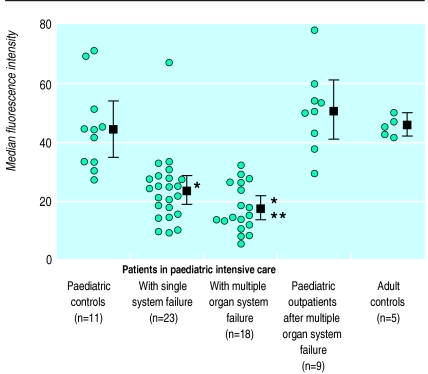
Monocyte HLA-DR expression was similar among the healthy adults (mean 45.7 (95% confidence interval 41.8 to 49.6)), children undergoing routine outpatient investigation (44.4 (35.0 to 53.8)), and children reviewed after recovery from multiple organ system failure (50.5 (40.2 to 60.7)). However, children with multiple organ system failure (17.5 (13.5 to 21.4)) and those with single system failure (26.9 (18.5 to 35.2)) had significantly reduced HLA-DR expression (P<0.05, one way analysis of variance with least significant difference after correction for multiple comparisons) (figure). HLA-DR expression was significantly lower among children with multiple organ system failure than among those with single system failure (P=0.045, two sample t test). Expression remained low throughout their stay in the paediatric intensive care unit (data not shown).
Comment
This study shows that all children requiring intensive care may be at increased risk of nosocomial infections because of acquired immunoparalysis. Monocyte HLA-DR expression fell in children with single or multiple organ system failure, although more so in the more severely ill children. Adults show similar falls in HLA-DR expression after systemic insults (neurosurgery, burns, trauma, and sepsis).2,4,5 Previous studies have indicated that patients with monocyte deactivation are at an increased risk of infectious complications.4,5 When those studies are taken together with ours severely ill patients of all ages seem to be predisposed to infections as a result of these alterations in host defences.
Future strategies to decrease nosocomial infection and the emergence of multiresistant micro-organisms should address the capacity of the host to resist infection in hospital environments.
Figure 1.
Median fluorescence intensity of monocyte HLA-DR expression in control paediatric outpatients, cases in paediatric intensive care unit because of single or multiple organ system failure, paediatric patients receiving outpatient follow up after multiple system failure, and healthy adults. Individual values and means with 95% confidence intervals (bars) are shown for each group (*P<0.05, analysis of variance v control groups). HLA-DR expression was also significantly lower in children with multiple organ system failure than those with single system failure (**P<0.05)
Footnotes
Funding: MP was supported by the Dunhill Medical Trust, GD by the Royal College of Physicians, and DI by SIMS-Portex.
Competing interests: None declared.
References
- 1.Wise R, Hart T, Cars O, Streulens M, Helmuth R, Huovinen P, et al. Antimicrobial resistance. BMJ. 1998;317:609–610. doi: 10.1136/bmj.317.7159.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Docke WD, Randow F, Syrbe U, Krausch D, Asadullah K, Reinke P, et al. Monocyte deactivation in septic patients: restoration by IFN-gamma treatment. Nat Med. 1997;3:678–681. doi: 10.1038/nm0697-678. [DOI] [PubMed] [Google Scholar]
- 3.Wilkinson JD, Pollack MM, Ruttimann UE, Glass NL, Yeh TS. Outcome of pediatric patients with multiple organ system failure. Crit Care Med. 1986;14:271–274. doi: 10.1097/00003246-198604000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Asadullah K, Woiciechowsky C, Docke WD, Liebenthal C, Wauer H, Kox W, et al. Immunodepression following neurosurgical procedures. Crit Care Med. 1995;23:1976–1983. doi: 10.1097/00003246-199512000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Schinkel C, Sendtner R, Zimmer S, Faist E. Functional analysis of monocyte subsets in surgical sepsis. J Trauma. 1998;44:743–748. doi: 10.1097/00005373-199805000-00001. [DOI] [PubMed] [Google Scholar]