Abstract
Objective To assess the evidence for prophylactic treatment with systemic antibiotics in burns patients.
Design Systematic review and meta-analysis of randomised or quasi-randomised controlled trials recruiting burns inpatients that compared antibiotic prophylaxis (systemic, non-absorbable, or topical) with placebo or no treatment.
Data sources PubMed, Cochrane Library, LILACS, Embase, conference proceedings, and bibliographies. No language, date, or publication status restrictions were imposed.
Review methods Two reviewers independently extracted data. The primary outcome was all cause mortality. Risk or rate ratios with 95% confidence intervals were pooled with a fixed effect model if no heterogeneity was present.
Results 17 trials were included. Trials that assessed systemic antibiotic prophylaxis given for 4-14 days after admission showed a significant reduction in all cause mortality (risk ratio 0.54, 95% confidence interval 0.34 to 0.87, five trials). The corresponding number needed to treat was 8 (5 to 33), with a control event rate of 26%. Perioperative non-absorbable or topical antibiotics alone did not significantly affect mortality. There was a reduction in pneumonia with systemic prophylaxis and a reduction in wound infections with perioperative prophylaxis. Staphylococcus aureus infection or colonisation was reduced with anti-staphylococcal antibiotics. In three trials, resistance to the antibiotic used for prophylaxis significantly increased (rate ratio 2.84, 1.38 to 5.83). The overall methodological quality of the trials was poor.
Conclusions Prophylaxis with systemic antibiotics has a beneficial effect in burns patients, but the methodological quality of the data is weak. As such prophylaxis is currently not recommended for patients with severe burns other than perioperatively, there is a need for randomised controlled trials to assess its use.
Introduction
Severe burns are an important health burden worldwide and affect young healthy adults and children.1 2 Infections among burns patients are a major problem; the reported incidence of nosocomial infections varies at 63-240 per 100 patients and 53-93 per 1000 patient days, depending mainly on the definitions used.3 4 Infections are independently associated with adverse outcomes and mortality.3 4 In a series of 175 patients with severe burns, infections preceded multiorgan dysfunction in 83% of patients and were considered as the direct cause of death in 36% of patients who died.5
In burns patients infections arise from multiple sources. Burn wounds become rapidly infected with Gram positive bacteria, mainly staphylococci, that are normal deep inhabitants of the sweat glands and hair follicles exposed by the burn.6 The moist, vascular burn eschar further fosters microbial growth. Gram negative bacterial infections result from translocation from the colon because of reduced mesenteric blood flow at the time of burn and subsequent insults.7 Furthermore, several immune deficits have been described among burns patients, including impaired cytotoxic T lymphocyte response, myeloid maturation arrest causing neutropenia, impaired neutrophil function, and decreased macrophage production.6 8 9 10 Finally, burns patients can incur hospital acquired infections common to other patients in intensive care units, including intravascular catheter related infections and ventilator associated pneumonia, with an overall incidence of infection higher than that of other patients in intensive care units.3 4
Antibiotic prophylaxis reduces mortality, bacteraemia, and ventilator associated pneumonia among patients in intensive care units.11 12 Similarities between intensive care and burns patients suggest possibly similar benefit of prophylaxis. Both populations are critically ill, and bacterial translocation from the colon is an important source of infection, as are foreign bodies and invasive procedures. In burns patients the skin is an additional source of infection, and they have a higher degree of immunosuppression. Nevertheless, there is a broad and uniform consensus in the current literature that prophylaxis with systemic antibiotics should not be given to patients with severe burns. Recommendations for management do not address systemic antibiotic prophylaxis1 13 or explicitly state that prophylactic antibiotics are not recommended.14 15 16 17 18 The rationale given is lack of evidence, no benefit, or risk for adverse events, mainly colitis associated with Clostridium difficile and induction of antibiotic resistance. Indeed, most episodes of bloodstream infection after the first week are caused by hospital-type multidrug resistant bacteria.4 19 Recommendations regarding perioperative prophylaxis vary and most sources recommend limited perioperative prophylaxis only for those with severe burns (>40% total body surface area).14 16 17
We performed a systematic review and meta-analysis of randomised and quasi-randomised controlled trials assessing antibiotic prophylaxis for burns patients, both in the perioperative and general setting. We primarily examined the effect of prophylaxis on all cause mortality.
Methods
Selection criteria
We included randomised controlled trials or quasi-randomised trials (with inadequate allocation generation methods), recruiting inpatients with burns injuries (any total body surface area or burn degree, with or without inhalation injury), regardless of publication status or language. The intervention assessed was antibiotic prophylaxis versus placebo or no treatment. Prophylaxis was defined as antibiotics administered to patients without documented infection regardless of systemic inflammatory signs, including systemic antibiotics given intravenously, orally, or intramuscularly; non-absorbable oral antibiotics; or topical (wound dressing or inhalation) antibiotics. Regimens including both systemic and non-absorbable or topical antibiotics were included in the systemic category. Antibiotics could be administered at any time after admission (“general”) or specifically targeted at a surgical procedure (“perioperative”). We excluded topical non-antibiotic antimicrobial ointments or dressings (silver with or without sulpha, iodine, or mafenide) and antifungals, unless applied identically to intervention and control arms. We excluded dose or schedule comparisons of the same antibiotics.
Outcomes
The protocol defined primary outcome was all cause mortality 100 days after randomisation. None of the studies reported 100 day data or similar, nor at another fixed point in time, and so we extracted in hospital mortality from all the studies, per protocol. Secondary outcomes included bacteraemia, pneumonia (including ventilator associated pneumonia), infection of the burn wound, length of stay in hospital, infections caused by Pseudomonas aeruginosa, Staphylococcus aureus, and meticillin resistant S aureus (MRSA), resistance induction, fungal infections (fungaemia or other clinical fungal infection), and adverse events. Resistance induction was defined per protocol as clinical infection (not colonisation) caused by bacteria resistant to one or more of the antibiotics included in the prophylactic regimen. Studies, however, reported only on selected “resistant isolates” (including both clinical and colonising bacteria); these data and their definitions were extracted. Similarly, we accepted and documented other outcomes definitions used in individual studies.
Search methods
We searched PubMed (1966 to February 2009), Cochrane Library (issue 4, 2008), LILACS (1982 to February 2009), Embase (1974 to October 2009), and conference proceedings (Interscience Conference on Antimicrobial Agents and Chemotherapy 1995-2008; European Congress of Clinical Microbiology and Infectious Diseases 2000-8; Annual Meeting of the American Burn Association 2001-9; Congress of the International Society for Burn Injuries 2007; and the Annual Southern Region Burn Conference 2008-9). We crossed the words “burn” or “total body surface area or TBSA” and their MESH terms with the terms “antibiotic,” “infection”, “sepsis”, or “bacteremia”. For PubMed, this was combined with the Cochrane highly sensitive filter for randomised controlled trials.20 We scanned the references of all included articles for additional studies. Authors were contacted to complement data on mortality and trial methods (one author21 supplied additional data on methods).
Data collection
Two reviewers (TA and AL) independently inspected each reference identified by the search, scanned full texts of relevant studies, applied the inclusion criteria, and extracted the data. Disagreements on data extraction were resolved by discussion with a third reviewer (MP). We assessed risk of bias in duplicate using domain based evaluation, classifying studies primarily according to the risk of non-random allocation of patients to the intervention arm (sequence generation) and concealment of this process (allocation concealment). These were graded as adequate, unclear, or not described and inadequate (for example, alternation, allocation by day of admission, hospital room), as recommended in the Cochrane Handbook.20 We also assessed blinding and intention to treat analysis. The effect of allocation concealment on results was assessed through sensitivity analysis, with restriction of the analysis to studies with adequate allocation concealment.
Data analysis
Dichotomous outcomes (mortality, resistance development, and adverse events) are expressed per patient and count data (infections, bacteraemia) are given per patient day. Individual study results are expressed as risk ratios or rate ratios, respectively, with 95% confidence intervals. Rate ratios were calculated as the ratio of events per patient day. Results were pooled with the Mantel-Haenszel fixed effect model (Review Manager (RevMan), version 5 for Windows, Cochrane Collaboration, Oxford). We used χ2 test to determine heterogeneity (P<0.1) or an I2 measure for inconsistency (>50%).20 Outcomes with significant heterogeneity were not pooled. We anticipated heterogeneity related to total body surface area and degree of burn but did not perform subgroup analyses because of paucity of trials. Analyses were stratified by antibiotic mode and intervention: systemic antibiotics (which could be administered in the general or perioperative setting), non-absorbable antibiotics, and topical antibiotics. Because of paucity of trials in each analysis, we did not use any formal method to investigate publication bias.
Results
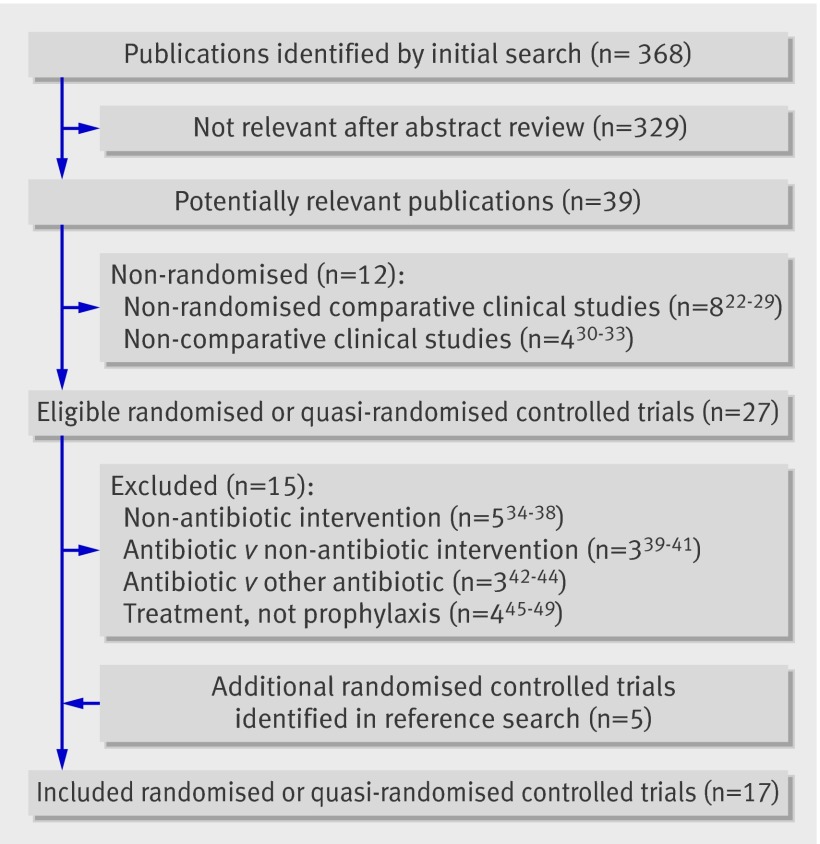
The search yielded 368 different publications, of which 39 were potentially relevant. Twenty seven studies were excluded (fig 1). We identified five trials through reference searching and altogether included 17 studies (37 trial arms), one of which was published as an abstract.21 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 The trials were published from 1968 to 2008 and recruited 1113 patients (median 51, range 15-149). Four trials recruited children51 52 54 62 and the others young adults (tables 1 and 2 ). The mean total body surface area affected was >20% in 12 trials (>30% in nine). Most trials did not report the number of patients with full thickness burns. Twelve administered systemic antibiotic prophylaxis; six trial arms assessed general53 55 56 57 59 64 and six perioperative prophylaxis.50 59 60 61 62 63 Systemic antibiotics usually targeted Gram positive bacteria and were given for a median of 8.5 days (range 4-14) in the general setting. Two trials assessing systemic general prophylaxis and none of the trials in the perioperative setting included a non-absorbable component. One trial assessed only non-absorbable prophylaxis,52 three trials topical antibiotic treatment,21 54 58 and one trial inhalation antibiotics,65 targeting mainly Gram negative bacteria.
Fig 1 Identification of studies for inclusion
Table 1.
Study characteristics of trials examining prophylactic antibiotics for burns patients in general settings. Figures are means (SD or SE) or median (range) unless stated otherwise
| Study and intervention details | Intervention duration (days) | No of patients randomised | Age (years) | TBSA (%) | 3rd degree burns (%) | Inhalation injury (%) |
|---|---|---|---|---|---|---|
| Barret 200152 | ||||||
| Non-absorbable per nasogastric tube polymyxin E, tobramycin, amphotericin B | Until open burn area <10% TBSA | 11 | 8 (1) | 67 (6) | 100 | 75 |
| Placebo | 12 | 9.4 (2) | 58 (6) | 100 | 63.6 | |
| De la Cal 200553 | ||||||
| Systemic intravenous cefotaxime + oropharyngeal paste and non-absorbable digestive administration of polymyxin E, tobramycin, amphotericin B | 4 | 58 | 41.4 (17.1) | 34 (21.4) | 19.3 (15.3) | 64.2 |
| Placebo | 59 | 48.2 (28.5) | 37.7 (21.1) | 19.0 (18.8) | 68.5 | |
| Desai 199154 | ||||||
| Topical gentamicin 1% cream | Until wound healing | 7 | 11.4 (1.2) | 35 (7) | 20 (9) | NS |
| No treatment | 8 | 9.5 (1.6) | 50 (6) | 32 (7) | ||
| Deutsch 199055 | ||||||
| Systemic and non-absorbable oral/nasogastric tube erythromycin, neomycin, nystatin | 10 | 15 | 44.7 (15-79) | 49.9 (22-91) | 26.3 (0-75) | 26.7 |
| No treatment | 12 | 35 (18-75) | 44.9 (20-75) | 26.3 (0-50) | 41.7 | |
| Durtschi 198256 | ||||||
| Systemic intravenous or oral penicillin | 5 | 25 | 31.1 (18-77) | 14.9 (1-70) | NS | NS |
| Placebo | 26 | 36.8 (18-66) | 20 (1-91) | |||
| Kimura 199857 | ||||||
| Systemic per nasogastric tube sulfamethoxazole-trimethoprim | 10 | 21 | 44 (10-91) | 49 (22-87) | NS | 52 |
| Placebo | 19 | 48 (12-85) | 43 (20-80) | 63 | ||
| Levine 197865 | ||||||
| Inhalation gentamicin | 10 | 12 | 28.1 | 53.8 | NS | 100 |
| Placebo | 18 | 34.3 | 57.6 | 100 | ||
| Livingston 199021 | ||||||
| Topical neomycin and bacitracin | Until graft healing | 18 | <20% TBSA 46 (22); 20-40% 27 (5); >40% 49 (10) | <20% TBSA 14 (5); 20-40% 29 (7); >40% 47 (6) |
NS | 22.2 |
| Normal saline | 15 | <20% TBSA 43 (27); 20-40% 34 (20); >40% 43 (19) | <20% TBSA 11 (3); 20-40%28 (6); >40% 53 (16) | NS | 33.3 | |
| Lowbury 196858 | ||||||
| Topical silver nitrate + gentamicin | Until burns had healed or were grafted | 21 | NS | <30 | NS | NS |
| Topical silver nitrate | 20 | |||||
| Munster 198959 | ||||||
| Systemic intravenous polymyxin B* | 7 | 22 | 34.4 | 29.3 | NS | NS |
| No treatment | 23 | 38.8 | 32.8 | |||
| Ugburo 200464 | ||||||
| Systemic oral ampicillin + oxacillin | 14 | 21 | 22.9 (4.1) | 41.5 (5.8) | NS | 0 |
| Systemic intravenous gentamicin+ oral erythromycin | 20 | 24.9 (3.3) | 46 (5.6) | |||
| None | 20 | 23.3 (3) | 44.3 (6.3) | |||
TBSA=total body surface area; MRSA=meticillin resistant S aureus.
**Two sequential parts randomising patients to general systemic prophylaxis (first part) and perioperative systemic prophylaxis (second part), kept separate in our analyses.
Table 2.
Study characteristics of trials examining systemic prophylactic antibiotics for burns patients in perioperative settings. Figures are means (SD or SE) or median (range) unless stated otherwise
| Study and intervention details | Intervention duration (days) | No of patients randomised | Age (years) | TBSA (%) | Third degree burns (%) | Inhalation injury (%) |
|---|---|---|---|---|---|---|
| Alexander 198251 | ||||||
| Systemic intravenous cephalothin | 1 | 127 | 10.5 (0.4) | NS | NS | NS |
| Placebo | 122 | 10.8 (0.4) | ||||
| Alexander 198450 | ||||||
| Systemic antibiotics tailored to wound cultures | 1 | 35 | NS | 45.7% >30% | NS | NS |
| No treatment | 34 | 38.2% >30% | ||||
| Munster 198959 | ||||||
| Systemic intravenous polymyxin B* | 5 | 6 | 47.7 | 54.8 | NS | NS |
| No treatment | 11 | 40.6 | 38.4 | |||
| Piel 198560 | ||||||
| Systemic intravenous cephalosporin | 1 | 25 | 33.6 | 42.6 | NS | NS |
| Placebo | 26 | 39.2 | 37 | |||
| Ramos 200861 | ||||||
| Systemic intravenous cephalothin or antibiotics tailored to surveillance cultures | 2 | 46 | 39 (21.7) | 21.6 (21) | NS | NS |
| No treatment | 44 | 35 (22) | 27.7 (22.3) | |||
| Rodgers 199762 | ||||||
| Systemic intravenous cefazolin | 1 | 10 | 1.5 | 10 | NS | NS |
| Placebo | 10 | 1.9 | 11 | |||
| Steer 199763† | ||||||
| Systemic intravenous teicoplanin | 1 | 67 (110 episodes) | 38 (23-54) | 8.5 (4-18) | 44 | NS |
| Placebo | 67 (110 episodes) | 42.5 (26-56) | 8.0 (4-16) | 45 | ||
TBSA=total body surface area; NS=not stated; MRSA=meticillin resistant S aureus.
*Two sequential parts randomising patients to general systemic prophylaxis (first part) and perioperative systemic prophylaxis (second part), kept separate in our analyses.
†Trial included patients before surgery (46% of episodes) or change of dressing.
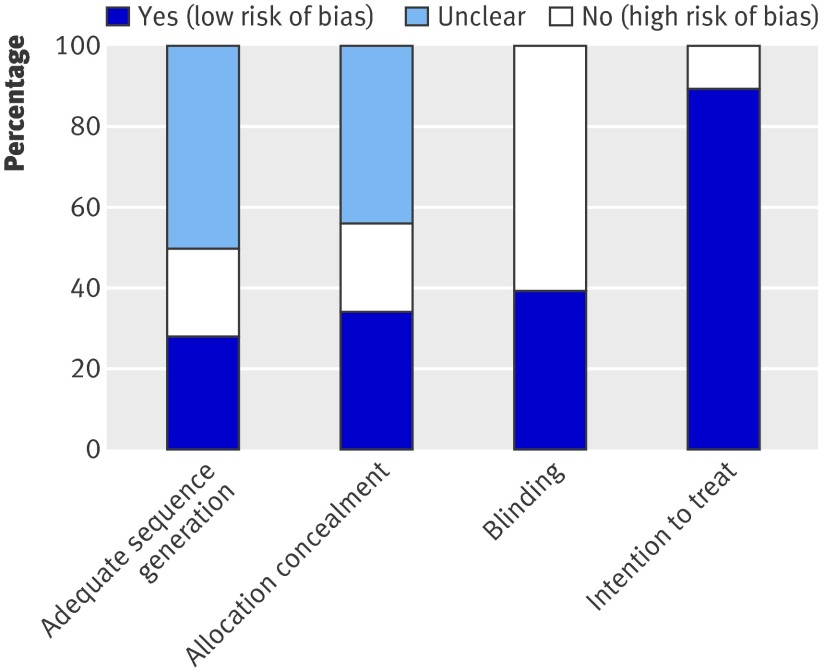
Five and six trials, respectively, described adequate sequence generation and allocation concealment. Both were inadequate in three quasi-randomised trials that used alternation or hospital number for sequence generation55 58 59 and were not described in all other trials (table 3 and fig 2). Patients and carers were blinded in seven trials (six assessing systemic prophylaxis). Results by intention to treat were reported in all but two trials.
Table 3.
Methods and outcome definitions used in individual trials
| Study | Allocation generation | Allocation concealment | Blinding* | Intention to treat analysis | Secondary outcomes evaluated and definitions | Resistance development/surveillance cultures† |
|---|---|---|---|---|---|---|
| Alexander 198251 | Adequate (random choice of envelopes) | Adequate (central pharmacist) | DB (placebo used, only pharmacist aware of treatment assignment) | Yes | Wound infection (discharge of pus from graft associated with graft loss); P aeruginosa and S aureus infections; hospital stay | NA. No surveillance |
| Alexander 198450 | Unclear (not stated) | Unclear (not stated) | Open (treatment and control patients placed in different wards) | Yes | Bacteraemia; wound infection | NA. Wound and blood surveillance |
| Barret 200152 | Adequate (random number chart) | Adequate (central pharmacy) | DB (placebo used, only pharmacist aware of treatment assignment) | Yes | Pneumonia (by CDC criteria or similar66); systemic fungal infection; hospital stay | NA. Wound, sputum, urine, blood, gastric aspirates, and stool surveillance |
| De la Cal 200553 | Unclear (not stated) | Adequate (central, pharmacy and kept in sealed envelopes) | DB (placebo used, only pharmacist aware of treatment assignment) + evaluator blinded | No | Pneumonia and bacteraemia (CDC criteria66); wound infection (according to previously proposed criteria67); candidaemia; P aeruginosa and S aureus infections; hospital stay | Unrelated; ventilator associated pneumonia or bacteraemia caused by MRSA. Wound, throat, rectal surveillance |
| Desai 199154 | Unclear (not stated) | Unclear (not stated) | Open | Yes | Wound infection (chondritis, defined); hospital stay | Related; chondritis caused by gentamicin-resistant bacteria. Wound surveillance |
| Deutch 199055 | Inadequate (chronological alternation) | Inadequate (chronological alternation) | Open | Yes for mortality; no for secondary outcomes | Wound and fungal infection (positive wound cultures); bacteraemia; P aeruginosa and S aureus infections; hospital stay | NA. Wound surveillance |
| Durtschi 198256 | Unclear (not stated) | Unclear (not stated) | DB (placebo used) | Yes | Wound infection (sepsis and warm, spreading, painful cutaneous erythema); bacteraemia; P aeruginosa, S aureus, and fungal infections; hospital stay | Unrelated; infections caused by gentamicin-resistant bacteria. Wound, rectal surveillance |
| Kimura 199857 | Unclear (not stated) | Adequate (central pharmacy) | DB | Yes | Pneumonia (by CDC criteria66); P aeruginosa and S aureus infections | Unrelated; MRSA infections. No surveillance |
| Levine 197865 | Unclear (not stated) | Unclear (not stated) | Single or DB (placebo inhalations used) | Yes | Pneumonia (pulmonary infiltrate); bacteraemia; P aeruginosa infections | NA. Blood surveillance |
| Livingston 199021 | Adequate (cards shuffled at assignment) | Adequate (cards placed in sealed envelopes) | Open | Yes | Wound infection (>10% graft loss and >105 organisms/g tissue, both in non-adherent graft and recipient site; candida wound infections; hospital stay | Unrelated; MRSA infections. Wound surveillance |
| Lowbury 196858 | Inadequate (alternation) | Inadequate (alternation) | Open (no placebo, no blinding described) | Yes | P aeruginosa and S aureus infections | Related; infections caused by gentamicin-resistant bacteria. Wound surveillance |
| Munster 198959 | Inadequate (randomised by hospital number) | Inadequate (randomised by hospital number) | Open (no placebo, no blinding described) | Yes | No secondary outcome | NA. No surveillance |
| Piel 198560 | Unclear (not stated) | Unclear (not stated) | Open (intervention listed on bedside flow chart) | Yes | Bacteraemia | NA. Wound and blood surveillance |
| Ramos 200861 | Unclear (not stated) | Adequate (sealed envelopes) | Evaluator | Yes | Wound infection (graft loss with swelling, erythema, increased temperature, tenderness or purulent discharge) | NA. Wound surveillance |
| Rodgers 199762 | Adequate (table of random numbers) | Unclear (not stated) | DB (placebo used, only pharmacist and one un-blinded investigator in the operating room aware of treatment assignment) + evaluator | Yes | Wound infection (clinical indication of infection with positive quantitative skin, wound biopsy, or blood cultures); candida wound infection; bacteraemia; P aeruginosa and S aureus infections | NA. Wound and blood surveillance |
| Steer 199763 | Unclear (not stated) | Unclear (not stated) | DB (placebo used, teicoplanin colour masked, only pharmacist aware of treatment assignment) | Yes, but analysis based on episodes | Wound infection (biopsy and quantitative tissue or skin cultures); pneumonia (respiratory infection manifested by sepsis and increase of purulent tracheobronchial secretions or worsening pulmonary gas exchange); P aeruginosa and S aureus infections; bacteraemia; candidaemia | Related and unrelated; infections caused by teicoplanin-resistant staphylococci and MRSA. Wound and blood surveillance |
| Ugburo 200464 | Adequate (table of random numbers) | Unclear (not stated) | Open | Yes | Wound infection (clinical infection using previously proposed criteria 68, with histological and microbiological confirmation); P aeruginosa and S aureus infections | NA. Wound surveillance |
*DB=double blind; patient and carer were blinded to treatment; NA=not assessed.
†Resistance trait and types of infections reported and relation to study drugs (related: assessment of resistance to one or more of the study drugs; unrelated: assessment of a resistance trait unrelated to the study antibiotics) and surveillance cultures reported.
Fig 2 Assessment of overall risk of bias
Primary outcome
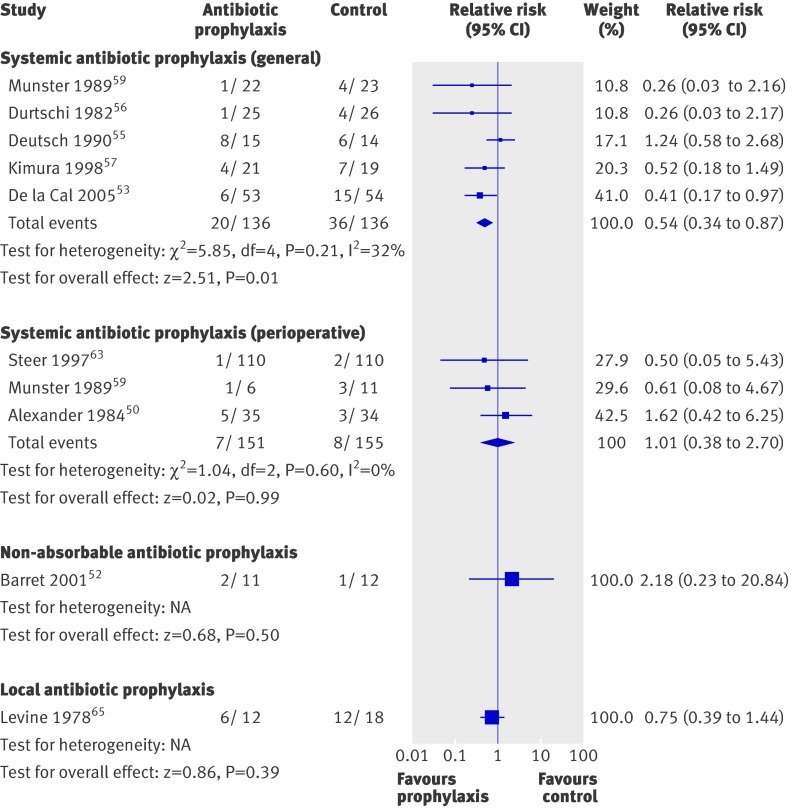
Nine trials reported all cause, in hospital mortality (fig 3). Systemic prophylaxis in the general setting was associated with a significant reduction in all cause mortality (risk ratio 0.54, 95% confidence interval 0.34 to 0.87, five trials, 272 patients), without significant heterogeneity (P=0.21, I2=32%). The corresponding number needed to treat was 8 (5 to 33), with a control event rate of 26%. The antibiotics used included cefotaxime, trimethoprim-sulfamethoxazole, penicillin, polymyxin B, and a combination of oral neomycin, erythromycin, and nystatin. The exclusion of trials with inadequate allocation concealment increased benefit (0.42, 0.22 to 0.79, three trials). There were no significant differences in mortality for perioperative non-absorbable or topical antibiotic prophylaxis.
Fig 3 All cause mortality in burns patients according to type of antibiotic prophylaxis
Secondary outcomes
Outcome definitions varied between the trials; table 4 summarises the results. Seven trials comprising 4835 patient days reported on bacteraemia. One trial administering perioperative teicoplanin prophylaxis showed a highly significant reduction (rate ratio 0.26, 0.15 to 0.45),63 while all other trials, including those of the general setting, showed no significant differences, both individually and pooled. Five trials reported on pneumonia (mainly ventilator associated) (103 events, 2624 patient days). Use of systemic antibiotics in the general or perioperative setting showed a significant reduction in pneumonia (0.55 (0.36 to 0.84), three trials). Eleven trials reported on burn wound infection (not colonisation) (295 events, 7357 patient days). Perioperative systemic antibiotic prophylaxis had an advantage of borderline significance (0.72 (0.52 to 1.01), four trials), while general systemic and topical antibiotics had no effect. Most trials did not report on length of admission to hospital in a manner that could be pooled.
Table 4.
Secondary outcomes in burns patients according to antibiotic treatment
| Outcome | No of trials | Rate ratio (95% CI) | Heterogeneity | |
|---|---|---|---|---|
| χ2 P value | I2 | |||
| Bacteraemia* | ||||
| Systemic general | 453 55 56 62 | 1.30 (0.91 to 1.85) | 0.56 | 0% |
| Topical, inhalation | 165 | 0.92 (0.39 to 2.16) | — | — |
| Wound infection | ||||
| Systemic general | 553 55 56 62 64 | 1.13 (0.82 to 1.55) | 0.92 | 0% |
| Systemic perioperative | 450 51 61 63 | 0.72 (0.52 to 1.01) | 0.17 | 40% |
| Topical | 221 54 | 1.49 (0.67 to 3.34) | 0.83 | 0% |
| Pneumonia | ||||
| Total systemic | 3 | 0.55 (0.36 to 0.84) | 0.28 | 21% |
| Systemic general | 253 57 | 0.52 (0.33 to 0.83) | 0.12 | 58% |
| Systemic perioperative | 163 | 0.71 (0.23 to 2.23) | — | — |
| Non-absorbable | 152 | 2.70 (0.11 to 66.10) | — | — |
| Topical, inhalation | 165 | 1.00 (0.42 to 2.37) | — | — |
| P aeruginosa infections | ||||
| Total | 12 | 0.95 (0.71 to 1.27) | 0.94 | 0% |
| With anti-pseudomonal activity | 455 58 64 65 | 1.06 (0.66 to 1.71) | 0.97 | 0% |
| Without anti-pseudomonal activity | 751 53 56 57 62-64 | 0.89 (0.62 to 1.28) | 0.61 | 0% |
| S aureus infections | ||||
| With anti-staphylococcal activity | 651 57 58 62-64 | 0.58 (0.43 to 0.76) | 0.72 | 0% |
| Without anti-staphylococcal activity | 353 55 56 | 1.70 (1.09 to 2.64) | 0.13 | 51% |
| Fungal infection | ||||
| Total | 7 | 1.58 (0.63 to 3.99) | 0.56 | 0% |
| Antibacterials and antifungals | 352 53 55 | 1.26 (0.26 to 6.14) | 0.49 | 0% |
| Antibacterials without antifungals | 421 56 62 63 | 1.78 (0.56 to 5.59) | 0.34 | 11% |
| Resistance development† | ||||
| Resistance trait related to prophylaxis | 353 54 63 | 2.15 (1.25 to 3.70) | 0.50 | 0% |
| Resistance trait unrelated to prophylaxis | 321 56 58 | 0.42 (0.18 to 0.98) | 0.70 | 0% |
| Adverse events requiring discontinuation† | ||||
| Total | 3 | 4.97 (1.08 to 22.96) | 0.41 | 0% |
| Systemic general | 155 | 13.10 (0.65 to 265.42) | — | — |
| Systemic perioperative | 251 63 | 2.99 (0.47 to 19.02) | 0.32 | 0 |
*With systemic prophylaxis in perioperative setting, one trial63 showed highly significant advantage with prophylaxis (0.26, 0.15 to 0.45), while other50 showed no difference (1.16, 0.79 to 1.70), thus this category was not pooled and nor was overall assessment of systemic antibiotic prophylaxis.
†Risk ratios shown.
Microbiological assessment showed that infection or colonisation by P aeruginosa was not significantly different, both in trials assessing antibiotics with and without an anti-pseudomonal spectrum of coverage (1.06, 0.66 to 1.71, four trials; and 0.89, 0.62 to 1.28, seven trials, respectively). S aureus infections significantly decreased with anti-staphylococcal prophylaxis (0.58, 0.43 to 0.76, six trials), while the three trials assessing an antibiotic without anti-staphylococcal coverage showed an overall increase but with significant heterogeneity (I2=51%). Similarly, MRSA infections significantly decreased when anti-MRSA prophylaxis was used (0.36, 0.19 to 0.70, three trials). Fungal infections were documented more often with antibiotic prophylaxis, but without a significant difference (1.58, 0.63 to 3.99, seven trials).
While most trials performed routine surveillance cultures, at least of burn wounds (table 2), results pertaining to induction of resistance were scarce (table 3). Isolation of bacteria resistant to the study antibiotics from any site was significantly higher in the intervention arm (2.84, 1.38 to 5.83, three trials, one topical, two systemic). Three trials reported on resistant infections unrelated to the intervention antibiotic (MRSA or resistance to gentamicin), which was lower in the intervention arm (0.42, 0.18 to 0.98).
Six trials addressed adverse events comparatively, of which three reported no events. Adverse events requiring discontinuation of antibiotic treatment were specified; these consisted of rash in two trials51 63 and diarrhoea in one.55 There was higher rate of discontinuation because of adverse events with treatment overall (4.97, 1.08 to 22.96). Pseudomembraneous colitis was not reported.
Discussion
The pooled evidence in our systematic review shows a significant decrease in all cause mortality with systemic antibiotic prophylaxis for 4-14 days among patients with burns (mostly severe), with a number needed to treat of 8 (5 to 33). Systemic prophylaxis was associated with a reduced rate of pneumonia and, when administered perioperatively, with a reduced rate of burn wound infections. Resistance of bacteria to the antibiotic used for prophylaxis increased. Our findings are based on a few small trials and in most randomisation methods were unclear or clearly inadequate. These results stand in contrast with the current consensus regarding antibiotic prophylaxis for patients with severe burns.14 15 16 17 18
Comparison with studies conducted in intensive care units
More evidence on the effects of antibiotic prophylaxis is available from studies on other critically ill patients in intensive care units. In this setting prophylaxis with non-absorbable or topical (oropharyngeal) antibiotics aims to decontaminate the digestive tract of Gram negative bacteria, S aureus, and candida. Most trials assessing antibiotic prophylaxis in intensive care units, however, also used broad spectrum systemic antibiotics for the first few days. The full (systemic plus non-absorbable) selective digestive decontamination regimen achieves a larger reduction in mortality (odds ratio 0.71, 0.61 to 0.82) than the non-absorbable intervention alone (0.94, 0.71 to 1.24).11 69 Selective decontamination regimens reduce mainly Gram negative infections,70 and induction of resistance has not been shown in trials conducted in low resistance settings.12 In the trials that assessed burns patients, systemic antibiotics alone were used in all the perioperative trials and some of the general prophylaxis trials. A recent trial, independently showing a reduction in mortality and ventilator associated pneumonia, used the full selective decontamination regimen.53 S aureus infections were reduced with prophylaxis in the perioperative setting. Considering similar risk factors for intensive care and burns patients, the unique susceptibility of burns patients to infections caused by skin flora, and the available evidence, it seems that the optimal regimen for prophylaxis among burns patients would be a full selective decontamination regimen including systemic and non-absorbable antibiotics. Antibiotics targeting Gram positive bacteria might be of added value perioperatively after discontinuation of the systemic antibiotic.
Strengths and limitations of study
We included systemic, non-absorbable, and topical antibiotics to inspect the effects of each separately and to fully appraise their combined effect on resistance induction. We included all types of burns, although the question of prophylaxis applies mainly to patients with severe burns. Most trials recruited patients with burns over more than 20% of total body surface area, and the mortality rate of the control group was 25% in trials that assessed general systemic prophylaxis and 17% in all trials reporting on mortality (fig 3). The paucity of trials precluded separate analyses for patients with severe or full thickness burns only.
Included trials span a long period, starting before 1968 and the last published in 2008. During this period advances in support and surgical treatment and changes in antibiotic treatment and resistance have occurred, limiting the validity of the pooled evidence. Randomisation methods were inadequate (quasi-randomisation) in three trials, and most others did not report the methods used. Although exclusion of the quasi-randomised trials did not reduce the effect on mortality, results should be interpreted with caution. Finally, although we performed a comprehensive search, we cannot be sure that we did not miss unpublished trials or older trials that were not labelled as randomised. The paucity of trials in each category precluded the assessment of publication bias.
Implications for practice
Infections are the leading cause of death in patients with severe burns, even given contemporary resuscitation protocols and surgical techniques.5 The onset of infection is difficult to pinpoint because patients with severe burns often present with systemic inflammatory signs and shock. Inhalation injury masks the appearance of pneumonia. This difficulty has been addressed by the American Burn Association’s consensus definitions for sepsis, designed specifically for burns patients.71 Even with improved definitions, it is difficult to ensure early appropriate antibiotic treatment for these patients; thus the appeal of antibiotic prophylaxis. In hospitals, burn units have notoriously been known as a source for outbreaks of multidrug resistant bacteria. Historically the appearance of MRSA and multidrug resistant Pseudomonas and Acinetobacter species were linked to burn units72 73 74 and more recently vancomycin resistant Enterococcus species and S aureus.75 76 Thus, the fear of further induction of resistance with antibiotic prophylaxis is real. Weighting a survival benefit against possible harm to future patients through cross infection with resistant strains is difficult. Most clinicians would probably opt for the individual’s immediate gain. The reduction in mortality shown in the current analysis, however, needs to be confirmed in a larger contemporary trial.
Implications for further research
Future trials should assess a full selective decontamination regimen including systemic and non-absorbable antibiotics. The duration of the systemic component can probably be limited to the first four days, similar to the regimen used in the most recent trial and in trials in the intensive care unit.12 53 77 Limited perioperative prophylaxis targeting Gram positive bacteria can be considered. Optimal resuscitation protocols and local care should be provided uniformly to both arms to assess the added benefit of antibiotic prophylaxis to current best practice.14 15 16 17 18 Special attention should be drawn to infection control practices during the trial to avoid cross infection between the trial arms. Contemporary methods used in multicentre trials should ensure adequate sequence generation and allocation concealment. Although randomised controlled trials might not be the optimal platform to assess development of resistance (randomised patients are in the same unit and the timeframe is inadequate),78 special attempts should be placed on documenting the effect of prophylaxis on colonisation (using surveillance cultures) and clinical infections caused by multidrug resistant bacteria. Other adverse effects including C difficile colitis and fungal infections should be addressed. Ultimately, however, a patient’s survival incorporates both ill effects and the benefit of prophylaxis and is the goal of managing burns patients. The current analysis (26% mortality in the control arm and relative risk of 0.54) suggests that an individual multicentre trial can be powered to assess all cause mortality as the primary outcome (about 200 patients per arm for a power of 80%). In hospital mortality among burns patients is highly variable; a fixed point in time relevant to the assessment of benefit and harm should be used.
In summary, we have shown a discrepancy between current guidelines for management of burns patients recommending against antibiotic prophylaxis and the evidence showing a reduction of about 50% in all cause mortality with systemic antibiotic prophylaxis. Given the paucity and limitations of the available evidence, this should serve mainly as an urgent call for a large randomised controlled trial.
What is already known on this topic
Antibiotic prophylaxis reduces all cause mortality among patients in intensive care
Current guidelines for management do not recommend systemic antibiotic prophylaxis for burns patients, stating lack of evidence for efficacy and induction of antibiotic resistance
What this study adds
In burns patients systemic antibiotic prophylaxis administered in the first 4-14 days significantly reduces all cause mortality by nearly a half; limited perioperative prophylaxis reduces wound infections but not mortality
Topical antibiotic prophylaxis applied to burn wounds, commonly recommended, had no beneficial effects
The methodological quality of the evidence is weak, however, so a large, robust randomised controlled trial is now needed
Contributors: MP was responsible for conception of the trial and is guarantor. TA, AL, and MP wrote the protocol, carried out searches, extracted and analysed the data, and wrote the manuscript. All authors critically revised the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing interests: None declared.
Ethical approval: Not required.
Data sharing: Analyses in RevMan software are available from the corresponding author at paulm@post.tau.ac.il.
Cite this as: BMJ 2010;340:c241
References
- 1.Enoch S, Roshan A, Shah M. Emergency and early management of burns and scalds. BMJ 2009;338:b1037. [DOI] [PubMed] [Google Scholar]
- 2.Sanghavi P, Bhalla K, Das V. Fire-related deaths in India in 2001: a retrospective analysis of data. Lancet 2009;373:1282-8. [DOI] [PubMed] [Google Scholar]
- 3.Chim H, Tan BH, Song C. Five-year review of infections in a burn intensive care unit: high incidence of Acinetobacter baumannii in a tropical climate. Burns 2007;33:1008-14. [DOI] [PubMed] [Google Scholar]
- 4.Wibbenmeyer L, Danks R, Faucher L, Amelon M, Latenser B, Kealey GP, et al. Prospective analysis of nosocomial infection rates, antibiotic use, and patterns of resistance in a burn population. J Burn Care Res 2006;27:152-60. [DOI] [PubMed] [Google Scholar]
- 5.Fitzwater J, Purdue GF, Hunt JL, O’Keefe GE. The risk factors and time course of sepsis and organ dysfunction after burn trauma. J Trauma 2003;54:959-66. [DOI] [PubMed] [Google Scholar]
- 6.Sharma BR. Infection in patients with severe burns: causes and prevention thereof. Infect Dis Clin North Am 2007;21:745-59,ix. [DOI] [PubMed] [Google Scholar]
- 7.Herndon DN, Lal S. Is bacterial translocation a clinically relevant phenomenon in burns? Crit Care Med 2000;28:1682-3. [DOI] [PubMed] [Google Scholar]
- 8.Gamelli RL, He LK, Liu LH. Macrophage mediated suppression of granulocyte and macrophage growth after burn wound infection reversal by means of anti-PGE2. J Burn Care Rehabil 2000;21:64-9. [DOI] [PubMed] [Google Scholar]
- 9.Hunt JP, Hunter CT, Brownstein MR, Giannopoulos A, Hultman CS, deSerres S, et al. The effector component of the cytotoxic T-lymphocyte response has a biphasic pattern after burn injury. J Surg Res 1998;80:243-51. [DOI] [PubMed] [Google Scholar]
- 10.Shoup M, Weisenberger JM, Wang JL, Pyle JM, Gamelli RL, Shankar R. Mechanisms of neutropenia involving myeloid maturation arrest in burn sepsis. Ann Surg 1998;228:112-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silvestri L, van Saene HK, Milanese M, Gregori D, Gullo A. Selective decontamination of the digestive tract reduces bacterial bloodstream infection and mortality in critically ill patients. Systematic review of randomized, controlled trials. J Hosp Infect 2007;65:187-203. [DOI] [PubMed] [Google Scholar]
- 12.De Smet AM, Kluytmans JA, Cooper BS, Mascini EM, Benus RF, van der Werf TS, et al. Decontamination of the digestive tract and oropharynx in ICU patients. N Engl J Med 2009;360:20-31. [DOI] [PubMed] [Google Scholar]
- 13.Evidence-Based Guidelines Group; American Burn Association. Practice guidelines for burn care. J Burn Care Rehabil 2001;suppl:1-67s.
- 14.Rice PL. Emergency care of moderate and severe thermal burns in adults. In: Marx JA, Grayzel J, eds. 2008. www.uptodate.com/patients/content/topic.do?topicKey=~Ay/xsdTHiuaQHr.
- 15.White CE, Renz EM. Advances in surgical care: management of severe burn injury. Crit Care Med 2008;36:S318-24. [DOI] [PubMed] [Google Scholar]
- 16.D’Avignon LC, Saffle JR, Chung KK, Cancio LC. Prevention and management of infections associated with burns in the combat casualty. J Trauma 2008;64:S277-86. [DOI] [PubMed] [Google Scholar]
- 17.Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn wound infections. Clin Microbiol Rev 2006;19:403-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silver GM, Klein MB, Herndon DN, Gamelli RL, Gibran NS, Altstein L, et al. Standard operating procedures for the clinical management of patients enrolled in a prospective study of inflammation and the host response to thermal injury. J Burn Care Res 2007;28:222-30. [DOI] [PubMed] [Google Scholar]
- 19.Ressner RA, Murray CK, Griffith ME, Rasnake MS, Hospenthal DR, Wolf SE. Outcomes of bacteremia in burn patients involved in combat operations overseas. J Am Coll Surg 2008;206:439-44. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions: version 5.0.1 Cochrane Collaboration, 2008.
- 21.Livingston DH, Cryer HG, Miller FB, Malangoni MA, Polk HC Jr, Weiner LJ. A randomized prospective study of topical antimicrobial agents on skin grafts after thermal injury. Plast Reconstr Surg 1990;86:1059-65. [PubMed] [Google Scholar]
- 22.Greminger RF, Elliott RA Jr, Rapperport A. Antibiotic iontophoresis for the management of burned ear chondritis. Plast Reconstr Surg 1980;66:356-60. [PubMed] [Google Scholar]
- 23.Jarrett F, Balish E, Moylan JA, Ellerbe S. Clinical experience with prophylactic antibiotic bowel suppression in burn patients. Surgery 1978;83:523-7. [PubMed] [Google Scholar]
- 24.Jarrett F, Chan CK, Balish E, Moylan J. Antibiotic bowel preparation and burn wound colonization. Surg Forum 1976;27:67-8. [PubMed] [Google Scholar]
- 25.LaForest NT, Cofrancesco C. Antibiotic iontophoresis in the treatment of ear chondritis. Phys Ther 1978;58:32-4. [DOI] [PubMed] [Google Scholar]
- 26.Manson WL, Westerveld AW, Klasen HJ, Sauer EW. Selective intestinal decontamination of the digestive tract for infection prophylaxis in severely burned patients. Scand J Plast Reconstr Surg Hand Surg 1987;21:269-72. [DOI] [PubMed] [Google Scholar]
- 27.Rizzo A. [Use of cortisone-antibiotic ointment in the treatment of burns in pediatric surgery]. Minerva Chir 1974;29:463-9. [PubMed] [Google Scholar]
- 28.Kuzin MI, Kolker, II, Vares A, Fillippovich Iu V, Makarenkova RV. [Antibacterial effect of preparations for the local treatment of burns and suppurative wounds]. Khirurgiia (Mosk) 1987:14-8. [PubMed]
- 29.Desai MH, Rutan RL, Heggers JP, Herndon DN. Candida infection with and without nystatin prophylaxis. An 11-year experience with patients with burn injury. Arch Surg 1992;127:159-62. [DOI] [PubMed] [Google Scholar]
- 30.Iakovlev VP, Krutikov MG, Alekseev AA, Grishina IA, Izotova GN, Kashin Iu D. [A trial of using sulperazone (cefoperazone/sulbactam) in the combined treatment of patients with a burn infection]. Antibiot Khimioter 1995;40:38-41. [PubMed] [Google Scholar]
- 31.Krutikov MG. [A trial of the clinical use of Cifran in treating infections in burn wounds and the infectious complications of burns]. Antibiot Khimioter 2000;45:37-40. [PubMed] [Google Scholar]
- 32.Xu W, Deng S, Han C, Li X, Liao Z, Wang W. [A multicenter clinical trial of piperacillin/tazobactam in burn infection]. Zhonghua Shao Shang Za Zhi 2002;18:75-7. [PubMed] [Google Scholar]
- 33.Iakovlev VP, Blatun LA, Krutikov MG, Puchkova LS, Izotova GN, Svetukhin AM, et al. [Use of cefpirome in the treatment of patients with skin and soft tissue infections]. Antibiot Khimioter 1996;41:24-9. [PubMed] [Google Scholar]
- 34.Barret JP, Dziewulski P, Ramzy PI, Wolf SE, Desai MH, Herndon DN. Biobrane versus 1% silver sulfadiazine in second-degree pediatric burns. Plast Reconstr Surg 2000;105:62-5. [DOI] [PubMed] [Google Scholar]
- 35.Donati L, Periti P. Antibiotic treatment of burned patients: an Italian multicentre study. Intensive Care Med 1994;20 Suppl 4:S30-4. [DOI] [PubMed]
- 36.Donati L, Periti P, Andreassi A, Dioguardi D, Gliori A, Landi G, et al. Increased burn patient survival with once-a-day high dose teicoplanin and netilmicin. An Italian multicenter study. J Chemother 1998;10:47-57. [DOI] [PubMed] [Google Scholar]
- 37.Lawrence JC, Cason JS, Kidson A. Evaluation of phenoxetol-chlorhexidine cream as a prophylactic antibacterial agent in burns. Lancet 1982;i:1037-40. [DOI] [PubMed]
- 38.Lowbury EJ, Lilly HA, Cason JS, Jackson DM, Bull JP, Davies JW, et al. Alternative forms of local treatment for burns. Lancet 1971;ii:1105-11. [DOI] [PubMed]
- 39.Demling RH, DeSanti L. Management of partial thickness facial burns (comparison of topical antibiotics and bio-engineered skin substitutes). Burns 1999;25:256-61. [DOI] [PubMed] [Google Scholar]
- 40.Sinha R, Agarwal RK, Agarwal M. Povidone iodine plus neosporin in superficial burns—a continuing study. Burns 1997;23:626-8. [DOI] [PubMed] [Google Scholar]
- 41.Soroff HS, Sasvary DH. Collagenase ointment and polymyxin B sulfate/bacitracin spray versus silver sulfadiazine cream in partial-thickness burns: a pilot study. J Burn Care Rehabil 1994;15:13-7. [DOI] [PubMed] [Google Scholar]
- 42.Miller LM, Carroll WB, Hansbrough JF. The effect of antimicrobial prophylaxis for burn wound excision: ceforanide versus cefazolin. Curr Ther Res 1987;41:946-51. [Google Scholar]
- 43.Proctor DS. The treatment of burns: a comparative trial of antibiotic dressings. S Afr Med J 1971;45:231-6. [PubMed] [Google Scholar]
- 44.Steer JA, Papini RP, Wilson AP, McGrouther DA, Parkhouse N. Teicoplanin versus flucloxacillin in the treatment of infection following burns. J Antimicrob Chemother 1997;39:383-92. [DOI] [PubMed] [Google Scholar]
- 45.Kunst MW. Ceftazidime treatment in severe burns. Serious infections in patients with severe burns treated with ceftazidime. Scand J Plast Reconstr Surg Hand Surg 1987;21:281-2. [DOI] [PubMed] [Google Scholar]
- 46.Periti P, Stringa G, Donati L, Mazzei T, Mini E, Novelli A. Teicoplanin—its role as systemic therapy of burn infections and as prophylaxis for orthopaedic surgery. Italian Study Groups for Antimicrobial Prophylaxis in Orthopaedic Surgery and Burns. Eur J Surg Suppl 1992:567:3-8. [PubMed]
- 47.Theron EJ, Nel CJ. Treatment of septic burns with a third-generation cephalosporin (cefatriaxon). S Afr Med J 1983;64:816-7. [PubMed] [Google Scholar]
- 48.Culbertson GR, McManus AT, Conarro PA, McManus WF, Mason AD Jr, Pruitt BA Jr. Clinical trial of imipenem/cilastatin in severely burned and infected patients. Surg Gynecol Obstet 1987;165:25-8. [PubMed] [Google Scholar]
- 49.Alekseev AA, Krutikov MG, Smirnov SV, Malakhov SF, Filimonov AA. [Clinical results of Fortum and Zinacef trial in burn centers of Russia]. Khirurgiia (Mosk) 1996:55-9. [PubMed]
- 50.Alexander JW, MacMillan, BG. Lack of beneficial effects of restricted prophylactic antibiotics for debridement and/or grafting of seriously burned patients. Bull Clin Rev Burn Injuries 1984;1:20. [Google Scholar]
- 51.Alexander JW, MacMillan BG, Law EJ, Krummel R. Prophylactic antibiotics as an adjunct for skin grafting in clean reconstructive surgery following burn injury. J Trauma 1982;22:687-90. [DOI] [PubMed] [Google Scholar]
- 52.Barret JP, Jeschke MG, Herndon DN. Selective decontamination of the digestive tract in severely burned pediatric patients. Burns 2001;27:439-45. [DOI] [PubMed] [Google Scholar]
- 53.De La Cal MA, Cerda E, Garcia-Hierro P, van Saene HK, Gomez-Santos D, Negro E, et al. Survival benefit in critically ill burned patients receiving selective decontamination of the digestive tract: a randomized, placebo-controlled, double-blind trial. Ann Surg 2005;241:424-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Desai MH, Rutan RL, Heggers JP, Alvarado MI, McElroy K, Henrdon DN. The role of gentamicin iontophoresis in the treatment of burned ears. J Burn Care Rehabil 1991;12:521-4. [DOI] [PubMed] [Google Scholar]
- 55.Deutsch DH, Miller SF, Finley RK, Jr. The use of intestinal antibiotics to delay or prevent infections in patients with burns. J Burn Care Rehabil 1990;11:436-42. [DOI] [PubMed] [Google Scholar]
- 56.Durtschi MB, Orgain C, Counts GW, Heimbach DM. A prospective study of prophylactic penicillin in acutely burned hospitalized patients. J Trauma 1982;22:11-4. [DOI] [PubMed] [Google Scholar]
- 57.Kimura A, Mochizuki T, Nishizawa K, Mashiko K, Yamamoto Y, Otsuka T. Trimethoprim-sulfamethoxazole for the prevention of methicillin-resistant Staphylococcus aureus pneumonia in severely burned patients. J Trauma 1998;45:383-7. [DOI] [PubMed] [Google Scholar]
- 58.Lowbury EJ, Jackson DM. Local chemoprophylaxis for burns with gentamicin and other agents. Lancet 1968;1:654-7. [DOI] [PubMed] [Google Scholar]
- 59.Munster AM, Xiao GX, Guo Y, Wong LA, Winchurch RA. Control of endotoxemia in burn patients by use of polymyxin B. J Burn Care Rehabil 1989;10:327-30. [DOI] [PubMed] [Google Scholar]
- 60.Piel P, Scarnati S, Goldfarb IW, Slater H. Antibiotic prophylaxis in patients undergoing burn wound excision. J Burn Care Rehabil 1985;6:422-4. [DOI] [PubMed] [Google Scholar]
- 61.Ramos G, Resta M, Machare Delgado E, Durlach R, Fernandez Canigia L, Benaim F. Systemic perioperative antibiotic prophylaxis may improve skin autograft survival in patients with acute burns. J Burn Care Res 2008;29:917-23. [DOI] [PubMed] [Google Scholar]
- 62.Rodgers GL, Fisher MC, Lo A, Cresswell A, Long SS. Study of antibiotic prophylaxis during burn wound debridement in children. J Burn Care Rehabil 1997;18:342-6. [DOI] [PubMed] [Google Scholar]
- 63.Steer JA, Papini RP, Wilson AP, McGrouther DA, Nakhla LS, Parkhouse N. Randomized placebo-controlled trial of teicoplanin in the antibiotic prophylaxis of infection following manipulation of burn wounds. Br J Surg 1997;84:848-53. [PubMed] [Google Scholar]
- 64.Ugburo AO, Atoyebi OA, Oyeneyin JO, Sowemimo GO. An evaluation of the role of systemic antibiotic prophylaxis in the control of burn wound infection at the Lagos university teaching hospital. Burns 2004;30:43-8. [DOI] [PubMed] [Google Scholar]
- 65.Levine BA, Petroff PA, Slade CL, Pruitt BA Jr. Prospective trials of dexamethasone and aerosolized gentamicin in the treatment of inhalation injury in the burned patient. J Trauma 1978;18:188-93. [DOI] [PubMed] [Google Scholar]
- 66.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control 1988;16:128-40. [DOI] [PubMed] [Google Scholar]
- 67.Peck MD, Weber J, McManus A, Sheridan R, Heimbach D. Surveillance of burn wound infections: a proposal for definitions. J Burn Care Rehabil 1998;19:386-9. [DOI] [PubMed] [Google Scholar]
- 68.Pruitt BA, Goodwin CW, Pruitt SK, Cleon W. Burn, including cold, chemical and electric injuries. In: Sabiston DC, ed. Textbook of surgery. 15th ed. Saunders, 1997:221-52.
- 69.Silvestri L, van Saene HK, Weir I, Gullo A. Survival benefit of the full selective digestive decontamination regimen. J Crit Care 2009;24:474 e7-14. [DOI] [PubMed] [Google Scholar]
- 70.Silvestri L, van Saene HK, Casarin A, Berlot G, Gullo A. Impact of selective decontamination of the digestive tract on carriage and infection due to Gram-negative and Gram-positive bacteria: a systematic review of randomised controlled trials. Anaesth Intensive Care 2008;36:324-38. [DOI] [PubMed] [Google Scholar]
- 71.Greenhalgh DG, Saffle JR, Holmes JH 4th, Gamelli RL, Palmieri TL, Horton JW, et al. American Burn Association consensus conference to define sepsis and infection in burns. J Burn Care Res 2007;28:776-90. [DOI] [PubMed] [Google Scholar]
- 72.Boyce JM, White RL, Causey WA, Lockwood WR. Burn units as a source of methicillin-resistant Staphylococcus aureus infections. JAMA 1983;249:2803-7. [PubMed] [Google Scholar]
- 73.Richard P, Le Floch R, Chamoux C, Pannier M, Espaze E, Richet H. Pseudomonas aeruginosa outbreak in a burn unit: role of antimicrobials in the emergence of multiply resistant strains. J Infect Dis 1994;170:377-83. [DOI] [PubMed] [Google Scholar]
- 74.Simor AE, Lee M, Vearncombe M, Jones-Paul L, Barry C, Gomez M, et al. An outbreak due to multiresistant Acinetobacter baumannii in a burn unit: risk factors for acquisition and management. Infect Control Hosp Epidemiol 2002;23:261-7. [DOI] [PubMed] [Google Scholar]
- 75.Oliveira GA, Dell’Aquila AM, Masiero RL, Levy CE, Gomes MS, Cui L, et al. Isolation in Brazil of nosocomial Staphylococcus aureus with reduced susceptibility to vancomycin. Infect Control Hosp Epidemiol 2001;22:443-8. [DOI] [PubMed] [Google Scholar]
- 76.Falk PS, Winnike J, Woodmansee C, Desai M, Mayhall CG. Outbreak of vancomycin-resistant enterococci in a burn unit. Infect Control Hosp Epidemiol 2000;21:575-82. [DOI] [PubMed] [Google Scholar]
- 77.De Jonge E, Schultz MJ, Spanjaard L, Bossuyt PM, Vroom MB, Dankert J, et al. Effects of selective decontamination of digestive tract on mortality and acquisition of resistant bacteria in intensive care: a randomised controlled trial. Lancet 2003;362:1011-6. [DOI] [PubMed] [Google Scholar]
- 78.Gafter-Gvili A, Paul M, Fraser A, Leibovici L. Effect of quinolone prophylaxis in afebrile neutropenic patients on microbial resistance: systematic review and meta-analysis. J Antimicrob Chemother 2007;59:5-22. [DOI] [PubMed] [Google Scholar]