Abstract
Objective
To investigate the risks of the sudden infant death syndrome and factors that may contribute to unsafe sleeping environments.
Design
Three year, population based case-control study. Parental interviews were conducted for each sudden infant death and for four controls matched for age, locality, and time of sleep.
Setting
Five regions in England with a total population of over 17 million people.
Subjects
325 babies who died and 1300 control infants.
Results
In the multivariate analysis infants who shared their parents' bed and were then put back in their own cot had no increased risk (odds ratio 0.67; 95% confidence interval 0.22 to 2.00). There was an increased risk for infants who shared the bed for the whole sleep or were taken to and found in the parental bed (9.78; 4.02 to 23.83), infants who slept in a separate room from their parents (10.49; 4.26 to 25.81), and infants who shared a sofa (48.99; 5.04 to 475.60). The risk associated with being found in the parental bed was not significant for older infants (>14 weeks) or for infants of parents who did not smoke and became non-significant after adjustment for recent maternal alcohol consumption (>2 units), use of duvets (>4 togs), parental tiredness (infant slept ⩽4 hours for longest sleep in previous 24 hours), and overcrowded housing conditions (>2 people per room of the house).
Conclusions
There are certain circumstances when bed sharing should be avoided, particularly for infants under four months old. Parents sleeping on a sofa with infants should always be avoided. There is no evidence that bed sharing is hazardous for infants of parents who do not smoke.
Key messsages
Cosleeping with an infant on a sofa was associated with a particularly high risk of sudden infant death syndrome
Sharing a room with the parents was associated with a lower risk
There was no increased risk associated with bed sharing when the infant was placed back in his or her cot
Among parents who do not smoke or infants older than 14 weeks there was no association between infants being found in the parental bed and an increased risk of sudden infant death syndrome
The risk linked with bed sharing among younger infants seems to be associated with recent parental consumption of alcohol, overcrowded housing conditions, extreme parental tiredness, and the infant being under a duvet
Introduction
In most non-westernised cultures the mother commonly shares a bed with her infant.1 Postulated physiological benefits of close contact between infants and care givers include improved cardiorespiratory stability and oxygenation, fewer episodes of crying, better thermoregulation, an increased prevalence and duration of breast feeding, and enhanced milk production.2,3
Before the reduction in the rate of the sudden infant death syndrome there was conflicting evidence on the effect of bed sharing.4–6 Early observational studies suggested parental alcohol consumption, drug ingestion, obesity, and fatigue to support the concept that parents may lie on an infant who shares the bed with them.7–9 Data from New Zealand implicated bed sharing as a risk factor for sudden infant death.10
The importance of socioeconomic deprivation and bed sharing has been highlighted in New Zealand among the Maori population,11 which has high rates of smoking and alcohol consumption, and in the United States among poor black populations.12 In certain Asian cultures, however, where particular forms of mother-infant cosleeping are common such as in Japan13 and Hong Kong,14 the rates of cot death are low, corresponding to findings in the Bangladeshi15 and Asian16 communities in the United Kingdom and the Pacific Island communities in New Zealand.17
While the benefits of the supine sleeping position for infants are now clear, there is no consensus on where the infant should sleep in relation to the parents. The study of sudden unexpected deaths in infancy (part of the confidential inquiry into stillbirths and deaths in infancy: CESDI SUDI study) is the first to be conducted after the fall in the rate of cot death in the United Kingdom and was specifically designed to identify whether known risk factors had changed or new factors had emerged.
We investigated the risks associated with different sleeping environments and how factors relating to parenting practice, both routine and specific, affect the infant.
Methods
The methodological detail of the study and sociodemographic details have been fully described elsewhere18 and the results from the first two years published.19 Briefly, it was a large population based case-control study initially conducted in three former health regions (South West, Northern, and Yorkshire) for two years (February 1993 to January 1995) and expanded (Wessex and Northern regions) for a third year (April 1995 to March 1996). The study aimed to include all cases of sudden unexpected deaths of infants aged 7 to 364 days from a total study population of 17.7 million. Data were collected on a questionnaire by research interviewers and from medical records. Bereaved families were visited within days of the death for a narrative account and again within two weeks to complete the questionnaire. Four controls for each case were selected. The health visitor for the infant who died was asked to identify two babies on her case list born in the two weeks before the index baby and two babies born in the two weeks after the index baby. In the few instances when the family identified was not available or declined to be interviewed or when the health visitor thought inclusion inappropriate—for example, because of recent bereavement—then the family with the baby next closest in age was substituted. The interviewer visited each control family within a week of the index death to collect the same data as for the index case. A period of sleep (the “reference sleep”) was identified in the control infant's life in the 24 hours before the interview corresponding to the time of day during which the index baby had died. The questionnaire included a total of over 600 fields, including demographic and social data; the medical history of the infant and other family members; use of cigarettes, alcohol, and drugs; the precise sleeping arrangements for the infant; and full details of the events preceding and the circumstances surrounding the death (or relevant sleep).
Cause of death was established by a multidisciplinary committee after a full paediatric necropsy to a standard protocol was performed. All deaths were classified according to the Avon clinicopathological system.18
Statistical methods
Data that were not normally distributed were described by using medians and interquartile ranges. Odds ratios, 95% confidence intervals, and P values for the univariate and multivariate analysis were calculated, taking into account matching with conditional logistic regression by using the statistical package sas.20 The age of the control infant was taken as the age at the reference sleep in the 24 hours before the interview. Because of the time lag to arrange four control interviews the control infants were on avereage about 10 days older than the index infants. The variable for infant age was therefore included in all univariate and multivariate analyses. Models were constructed with the backward stepwise procedure for variables significant at the 5% level in the univariate analysis. When the data were split for analysis (for example, younger and older infants) the four controls were partitioned, regardless of age, into the same subgroup as the corresponding index infant.
Results
Ascertainment
In the three year period there were 456 sudden unexpected deaths in infancy, of which 363 were classified as the sudden infant death syndrome.18 Of these 363 families, 24 refused an interview and 14 were excluded from the analysis because of police involvement (suspected non-accidental injury), because they lived outside the study regions, or because they could not be traced. Each excluded control family (7.9%) was immediately replaced, yielding 325 cases and 1300 controls.
Where the infant slept: usual night time practice
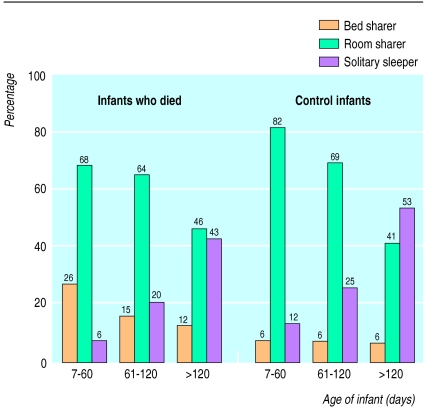
For all families the most common night time sleeping arrangement was that the infant slept in a cot in the parents' bedroom. Table 1 examines room sharing, solitary sleeping, and bed sharing in relation to social class. Infants who usually shared the parents' bed were at increased risk in this univariate analysis, regardless of the socioeconomic breakdown. The figure shows the same data, dividing infants into three age bands. The difference in the prevalence of bed sharing between infants who died and the control infants was greatest for those aged less than 60 days.
Table 1.
Infant's sleeping environment* in relation to parents: usual night time practice and socioeconomic breakdown. Figures are numbers (percentage) of babies
| Detail | Babies who died | Controls | Univariate odds ratio† (95% CI) |
|---|---|---|---|
| All socioeconomic classes‡ | |||
| No of babies | 320§ | 1299§ | |
| Usual room sharer | 189 (59.1) | 813 (62.6) | 1.00 |
| Usual solitary sleeper | 77 (24.1) | 410 (31.6) | 0.88 (0.62 to 1.25) |
| Usual bed sharer | 54 (16.9) | 76 (5.90) | 2.99 (1.94 to 4.63) |
| Socioeconomic classes I, II, III non-manual‡ | |||
| No of babies | 128¶ | 850¶ | |
| Usual room sharer | 69 (53.9) | 497 (58.5) | 1.00 |
| Usual solitary sleeper | 42 (32.8) | 312 (36.7) | 1.33 (0.78 to 2.27) |
| Usual bed sharer | 17 (13.3) | 41 (4.8) | 4.07 (1.75 to 9.46) |
| Socioeconomic classes III manual, IV, V, and unemployed‡ | |||
| No of babies | 190¶ | 446¶ | |
| Usual room sharer | 118 (62.1) | 315 (70.6) | 1.00 |
| Usual solitary sleeper | 35 (18.4) | 97 (21.7) | 0.67 (0.30 to 1.48) |
| Usual bed sharer | 37 (19.5) | 34 (7.6) | 2.66 (1.19 to 5.98) |
Usual room sharer: infants who usually shared parental bedroom but not bed; usual solitary sleeper: infants who usually slept in room separate from parents either alone or with other siblings; usual bed sharer: infants who usually shared parental bed for more than two nights/week.
Adjusted for infant age.
Socioeconomic classes based on highest occupational classification (I being highest, V being lowest) of parents and take previous occupation into account (thus unemployed classification comprises households that have never received waged income).
For five infants who died and one control infant insufficient information on sleeping environment was collected to include them in analysis.
For two infants who died and three control infants socioeconomic class of family could not be accurately ascertained.
Where the infant slept: last or reference sleep
Table 2 shows the infants' sleeping environment for the last or reference sleep. A greater proportion of index infants slept in the same bed or in a separate room from their parents. This breakdown is different from the usual night time practice (table 1), partly because of the broad definition of bed sharing and partly because some of the deaths and matched reference sleeps occurred during the day (54 (16.9%) deaths and 205 (15.8%) controls), when the routine was different. Restriction of the analysis to night time deaths yielded virtually identical results to those detailed here.
Table 2.
Infant's sleeping environment in relation to parents: last or reference sleep. Figures are numbers (percentage) of babies
| Infant details | Infants who died (n=321)* | Controls (n=1299)* | Univariate odds ratio† (%5 CI) |
|---|---|---|---|
| Room sharer | 81 (25.3) | 506 (39.0) | 1.00 |
| Solitary sleeper | 114 (35.6) | 420 (32.3) | 1.94 (1.33 to 2.81) |
| Bed sharer‡ | 126 (39.4) | 373 (28.7) | 2.00 (1.38 to 2.90) |
For four infants who died and one control infant insufficient information on sleeping environment was collected to include them in analysis.
Adjusted for infant age.
Includes all infants who shared same sleeping place (bed or sofa) with at least one parent for any part of last or reference sleep.
Table 3 shows a multicategorical variable that differentiates bed sharers into those infants who shared the bed but were put back in their own cot, those infants who shared the bed either for the whole sleep or were found in the parental bed at the end of the sleep, and those infants who slept on a sofa with a parent. The multivariate model is based on all factors significant in the univariate analysis.
Table 3.
Infant's sleeping environment in relation to parents: last or reference sleep. Figures are numbers (percentage) of babies
| Infant details | Infants who died (n=321) | Controls (n=1299) | Univariate odds ratio* (95% CI) | Multivariate odds ratio† (95% CI) |
|---|---|---|---|---|
| Room sharer | 81 (25.2) | 506 (39.0) | 1.00 | 1.00 |
| Solitary sleeper | 114 (35.5) | 420 (32.3) | 1.92 (1.32 to 2.80) | 10.49 (4.26 to 25.81) |
| Bed sharer (put back in own cot)‡ | 24 (7.5) | 178 (13.7) | 0.66 (0.38 to 1.13) | 0.67 (0.22 to 2.00) |
| Bed sharer (at end of sleep)§ | 82 (25.5) | 189 (14.5) | 2.75 (1.85 to 4.08) | 9.78 (4.02 to 23.83) |
| Sofa sharer¶ | 20 (6.2) | 6 (0.5) | 31.25 (8.78 to 111.23) | 48.99 (5.04 to 475.60) |
Adjusted for infant age.
Controlled for maternal age (continuous variable); parity (including index or control: 1 child v 2, 3 or 4, 5 or more); gestational age (⩾39 weeks v 37-38 weeks, <37 weeks); birth weight (continuous variable); multiple births (singleton v twin or triplets); unemployment (at least one parent employed v both or single mother unemployed); overcrowding (number of people per room excluding toilet, bathroom, hallway, and kitchen if not dining room (<2 v ⩾2); maternal smoking during pregnancy (no v yes); paternal smoking (no v yes); paternal drug use (since baby was born: never or only once taken illegal substance v two or more times); daily postnatal exposure to tobacco smoke (parental estimate of hours infant exposed per day: 0 v 1 or more hours); previous episode of apparent life threatening event according to parents (none v 1 or more); maternal anxiety over infant becoming too hot (not anxious v anxious); infant put down in prone or side position for last sleep (supine v prone, side); infant being found after last sleep with bedcovers over head (no v yes); use of dummy for any part of last sleep (no v yes); use of pillow (no v yes); recent maternal alcohol consumption before last sleep (⩽2 units v >2 units); parental estimate of poor health (good or fair v poor); parental tiredness (longest period of infant sleep in previous 24 hours before last sleep (>4 v ⩽4 hours); change in routine affecting infant (not at home, having visitors, non-parental carer, etc: no v yes); sleeping under duvet and thickness (0 tog v 1-4 tog, 5-8 tog, ⩽9 tog). All of these factors were significant in multivariate model with exception of last variable, which was just above 5% significance.
12 infants who died and 39 control infants then put back in own room, rest put back in parental bedroom.
54/82 infants who died shared bed for whole sleep compared with 74/189 control infants.
Two control infants did not share sofa by end of sleep.
There was no increased risk of death for infants who shared the bed but were put back in their own cot but a significant association with those infants who bed shared for the whole sleep or were taken to and found in the parental bed, infants who slept in a separate room from their parents, and infants who shared a sofa. The strengths of these associations increased dramatically in the multivariate model. Some factors in the multivariate model predominantly involved infants sleeping in a cot rather than the parental bed, such as infants being put down in the prone sleeping position (20.8% deaths in a cot v 2.5% deaths in a shared bed), placed on a pillow (11.6% v 1.2%), or infants being found with their heads covered (19.0% v 6.9%). Removal of these three variables halved the strength of the association with being found in a shared bed (multivariate odds ratio 4.62; 95% confidence interval 2.34 to 9.09). The proportion of index infants found in the prone position was three times higher among infants found in a cot compared with the parental bed (45.4% v 14.1%).
Of those infants found in the parental bed for the last or reference sleep, some parents brought their infants to bed for breast feeding (14.8% v 21.2% controls) or bottle feeding (14.8% v 7.4%); more of the index parents did so because they usually slept that way (44.4% v 31.2%) and more of the control parents because the baby would not settle (19.8% v 30.7%). Few parents had brought the infant into bed because the baby was unwell (1.2% v 3.7%), because the baby was cold (1.2% v 1.6%), or for a cuddle and extra time in bed (3.7% v 4.2%).
A similar proportion of these infants slept with just one parent in the bed (18.9% v 17.3%), almost always the mother. Most infants slept next to one parent (73.1% v 63.0%), but more control infants slept between parents (22.0% v 37.0%). Two index infants were found under a parent, one was found at the bottom of the bed, and one was found on the floor.
The infants who died in the parental bed (median (interquartile range) age 8 (4-13) weeks) were much younger than those who were found elsewhere (15 (10-23) weeks). When the data were split into younger and older infants by using the median age of all study infants (14 weeks 2 days), the risk associated with bed sharing for older infants found in the parental bed (odds ratio 1.08; 95% confidence interval 0.55 to 2.11) was almost unity but for the younger infants the associated risk was significant(4.65; 2.70 to 7.99).
The index infants who shared a sofa with a parent (median age 9 weeks; 6 to 15 weeks) were similar in age to those who died in the parental bed. Sofa sharing was as common with mothers as fathers. The narrative account suggests that for four deaths the infant was wedged between the parent and the back of the sofa, while for five the parent and infant lay at opposite ends, although we do not have data on the size of the sofa or the position of the adult's legs. Seven of the index parents had not intended to fall asleep on the sofa, but for nine this practice was not unusual. In five of these deaths the cosleeping parent had consumed up to 2 units of alcohol, and three had consumed much more than this.
Associated risks
Table 4 examines the relation between parental smoking and infants found bed sharing. The proportion of index infants found dead in bed with parents who did not smoke was much lower than for control families who did not smoke (2.2% v 7.9% controls). The high prevalence of smoking among index parents (84.2%) was even higher among those parents whose infant was found in the parental bed at the end of the last or reference sleep (91.4%). Among index mothers who smoked, more of those whose infants shared the bed smoked more than 20 cigarettes a day (23.2% v 1.5% controls) compared with those who did not bed share (16.6% v 5.9%).
Table 4.
Infants found bed sharing at end of sleep and parental smoking. Figures are numbers (percentage) of infants unless stated otherwise
| At least one parent smokes* | Infant found bed sharing | Infants who died (n=321) | Controls (n=1299) | Univariate odds ratio† (95% CI) |
|---|---|---|---|---|
| No | No | 44 (13.7) | 582 (44.8) | 1.00 |
| No | Yes | 7 (2.2) | 103 (7.9) | 1.08 (0.45 to 2.58) |
| Yes | No | 195 (60.7) | 528 (40.6) | 5.34 (3.61 to 7.90) |
| Yes | Yes | 75 (23.4) | 86 (6.6) | 12.35 (7.41 to 20.59) |
Mother or partner at time of interview.
Adjusted for infant age.
The multivariate analysis suggests that there are some variables for which the risk is exclusively associated with the cot environment yet increase the significance of the risk associated with the bed sharing environment. Table 5 shows the more restricted model of factors that were predominantly associated with being found in the parental bed after the last or reference sleep. These included recent maternal alcohol consumption of more than 2 units (21.0% deaths in a shared bed v 8.6% deaths in a cot), infants covered by a duvet (61.0% v 31.9%), parental tiredness (54.6% v 20.3%), and sleeping environments in overcrowded conditions (8.5% v 2.5%). Individually each of these variables reduced the significance of the risk associated with bed sharing, and when all were put into a collective model, being found in a shared bed was no longer significant.
Table 5.
Multivariate model controlling for adverse bed sharing conditions. Figures are numbers (percentage) of infants unless stated otherwise
| Details for infant* | Infants who died (n=312) | Controls (n=1295) | Multivariate odds ratio (95% CI) | P value |
|---|---|---|---|---|
| Solitary sleeper | 111 (35.6) | 419 (32.4) | 1.96 (1.31 to 2.93) | 0.001 |
| Bed sharer (put back in cot) | 24 (7.7) | 178 (13.7) | 0.60 (0.33 to 1.08) | 0.09 |
| Bed sharer (at end of sleep) | 79 (25.3) | 186 (14.4) | 1.35 (0.83 to 2.20) | 0.23 |
| Sofa sharer | 20 (6.4) | 6 (0.5) | 25.86 (6.72 to 99.47) | <0.0001 |
| Parental tiredness† | 86 (27.6) | 191 (14.7) | 2.42 (1.61 to 3.63) | <0.0001 |
| Maternal alcohol consumption‡ | 37 (11.9) | 41 (3.2) | 3.40 (1.88 to 6.16) | <0.0001 |
| Overcrowding§ | 13 (4.2) | 4 (0.3) | 18.49 (3.62 to 94.48) | 0.0005 |
| Duvet tog: | ||||
| 1-4 | 37 (11.9) | 139 (10.7) | 1.47 (0.90 to 2.39) | 0.12 |
| 5-8 | 59 (18.9) | 91 (7.0) | 3.97 (2.43 to 6.46) | <0.0001 |
| ⩾9 | 26 (8.3) | 32 (2.5) | 3.26 (1.54 to 6.90) | 0.002 |
Reference group for sleeping environment (first four variables) was infants who shared room, reference group for duvet thickness (last three variables) was infants who did not use duvet.
Defined as longest period of infant sleep in previous 24 hours before last sleep: >4 v ⩽4 hours).
>2 units of alcohol in 24 hours before last or reference sleep.
Defined as >2 people per room (excluding kitchen not used for dining, toilet, bathroom, and hallways).
Discussion
Study findings
Our results show that infants sharing a sofa with an adult during sleep is associated with a particularly high and previously unrecognised risk of the sudden infant death syndrome. The apparent risk associated with infants sleeping in a separate room from the parents and sharing a bed for the whole or last part of sleep is less clear because of potential confounding. We found no increase in risk for older infants who share the parents' bed, infants of parents who do not smoke, or when the infant is returned to his or her cot. In the more restricted model, which incorporated factors for which there was an a priori expectation of their potential effects on the sleep environment, the independent significance of sharing the bed at the end of sleep disappeared. This result suggests that the risk of death may be associated with other potentially modifiable adverse conditions rather than the practice of bed sharing itself, although interpretation should be cautious given the prior expectation of this particular analysis.
The increased relative risk of death among infants who sleep in a separate room, regardless of infant age or risks associated with the cot environment, is consistent with the findings of the New Zealand study,21 although for a third of both cases and controls, this was a day time practice and not necessarily the night time routine. Cosleeping in terms of room sharing increases the sensory exchanges possible between parent and infants,22 but further research is required to investigate whether room sharing is protective in itself or merely a marker for hidden confounders not measured in this study.
Problems with interpretation
Our results highlight some of the methodological difficulties inherent in multivariate modelling. In the large multivariate model the infant who was found sharing the bed at the end of the sleep seemed to be an important risk factor. Within this model, however, it was difficult to quantify the strength of the risk given that the interaction of certain cofactors was based on the environment in which the infant slept; nor is it possible to generalise these multivariate findings to the whole population. Certain factors characteristic of infants found in the parental bed were systematically different from those where the infant was found in a cot: bed sharing infants were much younger, few were put down in the prone position, and few were found with their heads covered. Conversely these factors were reversed among infants who slept separately from their parents.
The high prevalence of smokers among the bed sharing parents of infants who died confirms the findings of Mitchell21 and makes it impossible to derive precise estimates of the risk associated with bed sharing for families who do not smoke.
Informed evidence
The practices of sharing the bed and cosleeping are culturally diverse. For example, a baby sleeping at arm's length from the mother on a firm surface, as is often the case in Hong Kong,23 or a Pacific Island baby sleeping on the bed rather than in the bed21 is in a different environment from a baby sleeping in direct contact with the mother on a soft mattress and covered by a thick duvet. Previous observational studies have highlighted contributory factors such as parental alcohol consumption, parental fatigue, a lack of an alternative sleeping place, and the use of thick duvets10–12; our data have extended these observations and given quantitative estimates of the relative risks for these factors.
Unlike cots, which are designed to meet safety standards for infants, adult beds are not so designed and may, at least in theory, carry a risk of accidental entrapment and suffocation. This and the conflicting evidence for harm or benefit from bed sharing shown in previous studies have generated strong professional beliefs about the appropriateness or otherwise of sharing a bed and cosleeping.
The debate on the safety, advantages, and disadvantages of bed sharing and cosleeping must be informed by evidence from epidemiology, physiology, and anthropology if it is to become more than the exchange of mere opinion. There has been little in the way of direct observational data until recently, but it is becoming clear that sharing a bed both for infants and mothers results in complex interactions that are completely different from isolated sleeping and that need to be understood in detail before application of simplistic labels such as “safe” or “unsafe.”24,25 Our results suggest that, as McKenna has argued, perhaps it is not bed sharing per se that is hazardous but rather the particular circumstances in which bed sharing occurs. That some of these circumstances may be modifiable has important implications in terms of social policy and health education.
Figure.
Usual night time sleeping environment by infant age. Numbers of infants: 7-60 days—88 index infants and 352 controls; 61-120 days —188 and 472; ⩾120 days—113 and 452. Each age band represents third of whole dataset and nearest whole month in age
Footnotes
Funding: The National Advisory Body for CESDI and the Foundation for the Study of Infant Deaths.
Competing interests: None declared.
References
- 1.Mosko S, McKenna J, Dickel M, Hunt L. Parent-infant co-sleeping: the appropriate context for the study of infant sleep and implications for sudden infant death syndrome (SIDS) research. J Behav Med. 1993;16:589–610. doi: 10.1007/BF00844721. [DOI] [PubMed] [Google Scholar]
- 2.Anderson GC. Current knowledge about skin-to-skin (kangaroo) care for preterm infants. J Perinatol. 1991;11:216–226. [PubMed] [Google Scholar]
- 3.Ludington-Hoe SM, Hadeed AJ, Anderson GC. Physiological responses to skin-to-skin contact in hospitalised premature infants. J Perinatol. 1991;11:19–24. [PubMed] [Google Scholar]
- 4.Luke JL. Sleeping arrangements of sudden infant death syndrome victims in the District of Columbia—a preliminary report. J Forensic Sci. 1978;23:379–383. [PubMed] [Google Scholar]
- 5.Klonoff-Cohen HS, Edelstein SL. Bed sharing and the sudden infant death syndrome. BMJ. 1995;311:1269–1272. doi: 10.1136/bmj.311.7015.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee NNY, Chan YF, Davis DP, Lau E, Yip DCP. Sudden infant death syndrome in Hong Kong: confirmation of a low incidence. BMJ. 1989;298:721–722. doi: 10.1136/bmj.298.6675.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carpenter RG. Sudden and unexpected deaths in infancy (cot death) In: Camps FE, Carpenter RG, editors. Sudden and unexpected deaths in infancy (cot death). Bristol: John Wright; 1972. pp. 7–15. [Google Scholar]
- 8.Bass M, Kravath RE, Glass LG. Death-scene investigation in sudden infant death. N Engl J Med. 1986;315:100–105. doi: 10.1056/NEJM198607103150206. [DOI] [PubMed] [Google Scholar]
- 9.Rintahaka PJ, Hirvonen J. The epidemiology of sudden infant death syndrome in Finland in 1969-80. Forens Sci Int. 1986;30:219–233. doi: 10.1016/0379-0738(86)90017-4. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell EA, Taylor BJ, Ford RPK, Stewart AW, Becroft DM, Thompson JM, et al. Four modifiable and other major risk factors for cot death: the New Zealand study. NJ Paediatr Child Health. 1992;28:1. doi: 10.1111/j.1440-1754.1992.tb02729.x. :3-S8. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell EA, Stewart AW, Scragg R, Ford RPK, Taylor BJ, Becroft DMO, et al. Ethnic differences in mortality from sudden infant death syndrome in New Zealand. BMJ. 1993;306:13–16. doi: 10.1136/bmj.306.6869.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffman HJ, Hunter JC, Ellish NJ, Janerich DT, Goldberg J. Adverse reproductive factors and the sudden infant death syndrome. In: Harper RM, Hoffman HJ, editors. Sudden infant death syndrome. Risk factors and basic mechanisms. New York: PMA Publishing; 1988. pp. 153–175. [Google Scholar]
- 13.Takeda KA. A possible mechanism of sudden infant death syndrome (SIDS) J Kyoto Prefecture University Med. 1987;96:965–968. [Google Scholar]
- 14.Davies DP. Cot death in Hong Kong. A rare problem? Lancet. 1985;ii:1346–1347. doi: 10.1016/s0140-6736(85)92637-6. [DOI] [PubMed] [Google Scholar]
- 15.Gantley M, Davies DP, Murcott A. Sudden infant death syndrome. Links with infant care practices. BMJ. 1993;16:263–222. doi: 10.1136/bmj.306.6869.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Farooqi S, Lip GYH, Beevers DG. Bed sharing and smoking in sudden infant death syndrome. BMJ. 1994;308:204–205. doi: 10.1136/bmj.308.6922.204b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tuohy PG, Counsell AM, Geddis DC. Sociodemographic factors associated with sleeping position and location. Arch Dis Child. 1993;69:664–666. doi: 10.1136/adc.69.6.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leach CEA, Blair PS, Fleming PJ, Smith IJ, Ward Platt M, Berry PJ, et al. Sudden unexpected deaths in infancy: similarities and differences in the epidemiology of SIDS and explained deaths. Pediatrics (in press).
- 19.Fleming PJ, Blair PS, Bacon C, Bensley D, Smith I, Taylor E, et al. Environment of infants during sleep and risk of sudden infant death syndrome: results of 1993-5 case-control study for confidential inquiry into stillbirths and deaths in infancy. BMJ. 1996;313:191–195. doi: 10.1136/bmj.313.7051.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.SAS Institute. SAS technical report P-229, SAS/STAT software: changes and enhancements, release 6.07. Cary, NC: SAS Institute; 1992. [Google Scholar]
- 21.Mitchell EA, Thompson JMD. Co-sleeping increases the risk of SIDS, but sleeping in the parents' bedroom lowers it. In: Rognum TO, editor. Sudden infant death syndrome. New trends in the nineties. Oslo: Scandanavian University Press; 1995. [Google Scholar]
- 22.McKenna J, Mosko S, Richard C, Drummond S, Hunt L, Cetel MB, et al. Experimental studies of infant-parent co-sleeping: mutual physiological and behavioural influences and their relevance to SIDS (sudden infant death syndrome) Early Hum Dev. 1994;38:187–201. doi: 10.1016/0378-3782(94)90211-9. [DOI] [PubMed] [Google Scholar]
- 23.Nelson EAS, Chan PH. Child care practices and cot death in Hong Kong. N Z Med J. 1996;109:144–146. [PubMed] [Google Scholar]
- 24.McKenna Sudden infant death syndrome in cross-cultural perspective. Is infant-parent cosleeping protective? Ann Rev Anthropol. 1996;25:201–216. [Google Scholar]
- 25.Ball HL, Hooker E, Kelly PJ. Where will the babies sleep? Attitudes and practices of new and experienced parents regarding co-sleeping with their new- born infant. Am Anthropol (in press).