SUMMARY
Objective
To serve as a conceptual map of the role of new interventions designed to reduce the burden of late life depression.
Methods
We identified three needs to be addressed by intervention research: 1) The need for novel interventions given that the existing treatments leave many older adults depressed and disabled; 2) the need for procedures enabling community-based agencies to offer interventions of known efficacy with fidelity; and 3) the need to increase access of depressed older adults to care.
Results
Our model orders novel interventions according to their role in serving depressed older adults and according to their position in the efficacy, effectiveness, implementation, dissemination testing continuum. We describe three interventions designed by our Institute to exemplify intervention research at different level of the model. A common element is that each intervention personalizes care both at the level of the individuals served and the level of community agencies providing care. To this end, each intervention is designed to accommodate the strengths and limitations of both patients and agencies and introduces changes in the patients’ environment and community agencies needed in order to assimilate the new intervention.
Conclusions
We suggest that this model provides conceptual guidance on how to shorten the testing cycle and bring urgently needed novel treatments and implementation approaches to the community. While replication studies are important, propose that most of support should be directed to those projects that take rational risks, and after adequate preliminary evidence, make the next step along the testing continuum.
A MODEL FOR INTERVENTION RESEARCH IN LATE-LIFE DEPRESSION
Depression is a health hazard because it is common and has devastating outcomes. These include personal suffering, disability, increased medical burden, and family disruption. In late life, depression is also fatal as it increases both suicide and non-suicide mortality (Conwell et al., 2002; Schulz et al., 2000). Research that can have an impact here and now needs to produce comprehensive interventions targeting the clinical and biological complexity and the social context of late life depression. In addition, such interventions should facilitate access to treatment, minimize the splintering of care, and have the potential to be implemented by currently available community-based agencies supported by the current health reimbursement system.
An assumption in traditional health services research is that the available treatments are “good treatments” and its main objective is to find ways to overcome barriers to their dissemination. However, this assumption is far from safe in late-life depression, which is group of syndromes with low remission rate (Alexopoulos et al., 2005) and complex medical, cognitive, and psychosocial problems requiring integrated multi-targeted interventions of which antidepressant treatment is only one part.
Central to developing interventions with public health impact is personalization of care both at the level of the individual but also at the level of community agencies that serve them. Late life depression is the clinical expression of complex interactions among biological factors and adversity (stressors) experienced by the older person. The prevalence and impact of these factors vary across subgroups of depressed older persons. Thus personalizing treatment by targeting the most common and/or harmful biopsychosocial offending factors in depressed older individuals or subgroups has the highest chance of success. Similarly, community-based agencies serving older adults have their own history, dynamics, strengths and limitations. Therefore, developing interventions jointly with community agencies and taking into account their resources and limitations may lead to treatments and strategies likely to be broadly implemented by professionals and agencies (scalability) and help large numbers of depressed older adults (reach).
Traditionally, intervention and health services research has divided research designs into distinct categories. Randomized control “efficacy” trials have been the gold standard for testing whether a new treatment is more efficacious than placebo or another active treatment under ideal experimental conditions, e.g. recruiting individuals most likely to respond, using highly trained research staff to administer the treatment, and the most sensitive outcome measures. Once a treatment is found efficacious, a next step is to conduct an “effectiveness” trial to see whether this treatment retains its benefits when administered in the “real world”, e.g. in primary care practices, nursing homes, senior citizen centers, etc. “Implementation” and “dissemination” research usually focuses on interventions with demonstrated effectiveness and focuses on organizational and policy changes, incentives, and financial barriers that may increase the scalability and reach of an intervention.
While the traditional division of intervention and services research is dictated by experimental rigor, it has drawbacks. First, the biological, clinical, and psychosocial heterogeneity of late-life depression and the diversity of agencies responsible for its care demand diverse personalized interventions, of which few are likely to go though the efficacy-effectiveness-implementation-dissemination chain of testing. Second, the traditional sequence of research delays intervention development and leaves many victims on its way, i.e. interventions never find their way to the community and those that reach the community, do so when new treatments have superseded them.
Arguably, an effective and efficient model of intervention development should be personalized based both on the heterogeneity of biopsychosocial aspects of late-life depression and the characteristics of available treatment agencies and tested in the community. What follows is a research development model for late-life depression that integrates our biopsychosocial model of late-life depression (Alexopoulos, 2005) with a traditional health behaviors model of access to care (Andersen, 1995).
Late-Life Depression as a Biopsychosocial Entity
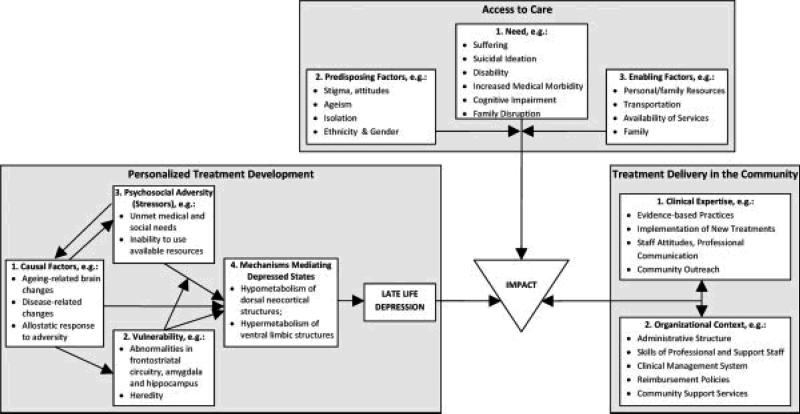
The syndrome of late-life depression is mediated by metabolic brain changes. These changes are more likely to develop in predisposed persons with abnormalities in brain structures responsible for emotional regulation. Aging and disease-related processes may serve as etiological factors by either directly promoting metabolic changes associated with depression or by increasing brain abnormalities predisposing to late-life depression. Chronically experienced adversity (stress) may lead to depression by promoting biological changes acting as etiological factors of depression, or by facilitating metabolic brain changes in predisposed individuals (Figure 1).
Figure 1.
INTERVENTION DEVELOPMENT MODEL FOR THE TREATMENT OF LATE -LIFE DEPRESSION
During depressive episodes, several dorsal neocortical structures are hypometabolic while some ventral limbic structures are hypermetabolic (Alexopoulos, 2002) suggesting that these changes mediate the depressive syndrome. Similar metabolic changes occur during experimentally induced sadness (Alexopoulos, 2002). However, these brain changes are quickly normalized in non-depressed individuals. The persistence of metabolic changes during depressive episodes suggests that other biological abnormalities predispose to depression and sustain the metabolic changes mediating the depressive syndrome.
Abnormalities in frontolimbic structures may predispose to the brain metabolic changes underlying the expression of depressive symptoms. There are two reasons for this assertion. First, some of the functions of these structures are relevant to depression and second abnormalities of these structures have been observed in some, but not all, patients with late-life depression.
Frontolimbic structures are part of distributed networks that facilitate the processing of task-relevant stimuli and protect them from interference by task-irrelevant stimuli. Two distinct networks have been proposed. A cognitive control system, including the dorsal anterior cingulate gyrus and the lateral prefrontal cortex is activated when a person is presented with conflicted non-emotional stimuli. Activation of this system selectively enhances task-relevant stimulus representations in sensory cortices (Egner et al., 2008). A second control system is responsible for processing conflict between task-relevant and non-relevant emotional stimuli. When this system is engaged, the rostral anterior cingulate is activated followed by reduced activation of the amygdala (Etkin et al., 2006). Engagement of the amygdala by emotional stimuli up-regulates hippocampal response resulting in enhancement of memory for affect-laden events (Smith et al., 2006). The hippocampus encodes associations among stimuli, mediates the sequential organization of an episode, and links common features of disparate memory episodes to create flexible representations (Wagar and Thagard, 2004).
Frontolimbic dysfunction may predispose to late-life depression (Alexopoulos, 2005). Low volumes (Ballmaier et al., 2004), hyperintensities (Krishnan et al., 1997), and macromolecular abnormalities (Kumar et al., 2004) in frontolimbic structures have been reported in late-life depression. Executive dysfunction, a clinical expression of frontolimbic abnormalities, is common (Elderkin-Thompson et al., 2003; Lockwood et al., 2002) and persistent (Butters et al., 2000; Murphy and Alexopoulos, 2004; Nebes et al., 2003) in late life depression. Depression accompanied with executive dysfunction has a clinical presentation resembling medial frontal lobe syndrome (Alexopoulos et al., 2002b; Krishnan et al., 1997; Alexopoulos et al., 1997) and is associated with slow, poor response to antidepressants (Simpson et al., 1998; Kalayam and Alexopoulos, 1999; Alexopoulos et al., 2004; Sneed et al., 2007). White matter abnormalities have been associated both with executive dysfunction (Aizenstein et al., 2002) and with poor outcomes of late-life depression (Alexopoulos et al., 2002a; Simpson et al., 1998; Hickie et al., 1995; O'Brien et al., 1998). Patients experiencing their first episode of major depression have large amygdala volumes (Frodl et al., 2003) but the volume declines in those with recurrent depression (Drevets, 2003; Sheline, 2003). Low hippocampal volume has been reported in patients with first episode of major depression suggesting that hippocampal abnormalities pose a risk for depression (Frodl et al., 2003; Sheline, 2003).
Heredity may lead to late-life depression through mechanisms different than those of younger adults. Depressed older adults are less likely to have family history of depression than younger patients (Brodaty et al., 2001). However, personal or family history of depression increases the incidence of depression following structural brain abnormalities (Morris et al., 1992). Another path to late life depression may be through hereditary factors promoting cerebrovascular disease. For example, some serotonin transporter 5-HTTLPR polymorphisms are associated with increased risk for vascular disease. Older short 5-HTTLPR allele (S) carriers have increased cholesterol, triglycerides and risk for heart disease, angina, and heart attacks than long allele (L) homozygotes (Comings et al., 1999). Moreover, cardiac events including cardiac death, revascularization, heart failure, reinfarction, arrhythmia, and unstable angina are more frequent after acute myocardial infarction in S-allele carriers than in L homozygotes (Nakatani et al., 2005).
Some polymorphisms are associated with brain abnormalities hypothesized to predispose to late-life depression. It is beyond the scope of this paper to offer a comprehensive review of these findings. However, studies on 5-HTTLPR polymorphisms exemplify some of these relationships. Specifically, brain structure studies have shown that depressed elderly S allele carriers have lower caudate nucleus volume than L homozygotes (Hickie et al., 2007). Depressed elderly patients with the SL genotype have more total brain lesions and white matter lesions than depressed who are either L or S homozygotes (Steffens et al., 2008). Finally, non-depressed S carriers have reduced gray matter in the perigenual cingulate and amygdala and increased sensitivity while processing fearful stimuli (Pezawas et al., 2005). Finally, S allele carrier status influences serotonin function in the same direction as in depression (Smith et al., 2002).
The proposed model classifies as etiological factors aging- and disease-related stages likely to initiate metabolic changes mediating the depressive syndrome or to lead to brain abnormalities predisposing to depression. For example, the hippocampus is vulnerable to ischemia (MacQueen et al., 2003) and to hypercortisolemia resulting from stress and chronic medical illness(McEwen, 2003; Miller and O'Callaghan, 2003). Reduced hippocampal volume is correlated with long exposure to depression (Sheline, 2000). Vascular and subcortical disorders, may damage the connections between the amygdala and the prefrontal cortex and predispose to depression. Hypercortisolemia occurring during chronic medical illnesses is associated with amygdalar activation and conversely, amygdalar activation stimulates cortisol release (Erickson et al., 2003; McEwen, 2003). Inflammatory markers such as C-reactive protein, interleukin (IL)-6, IL-1, and IL-1ra are increased during depressive syndromes (Howren et al., 2009) and may serve as yet another mechanism contributing to late-life depression and mediating in part the rise in medical morbidity and mortality in depressed older adults.
It should be pointed out that the distinction between etiological and predisposing factors is arbitrary. We include among etiological factors conditions for which preventive interventions exist or likely to be developed, while predisposing factors are rather permanent conditions. Clearly, interactions among predisposing factors have been identified, i.e. hereditary factors increase the probability to develop brain abnormalities predisposing to late-life depression as discussed above.
Chronically experienced adversity is common in older adults and may promote depressive symptoms directly. Animal studies suggest that chronic stress leads to neuroadaptation at the mesolimbic dopamine pathway level expressed as depression-like symptomatology (Nestler, 2009). Chronic stress in a “social defeat” animal model was associated with enhanced ventral tegmental neuron excitability resulting in increased activity-dependent release of brain derived neurotrophic factor (BDNF) in the nucleus accumbens (Krishnan and Nestler, 2008). These events were associated with anhedonia, social avoidance, weight loss, and circadian abnormalities. Preventing increase of ventral tegmental firing and BDNF signaling in the nucleus acumbens was shown to reduce vulnerability to chronic stress.
Beyond a direct relationship, experienced adversity may interact with etiological and predisposing factors and lead to late-life depression. Poverty is associated with both unmet social needs and limited access to high quality health care. Educational and cultural deprivation limits the development of problem solving skills and maximizes the experience of adversity. Furthermore, poverty is associated is associated with poor health behaviors as well as scarce health resources leading to inadequate prevention and care of medical illnesses contributing to late-life depression, e.g. vascular disease. Similarly, experienced adversity may interact with hereditary factors and facilitate development of depression. For example, the serotonin transporter S-allele increases the likelihood of developing depression in the presence of stress (Caspi et al., 2003). Moreover, S-allele carrier status interacts with waking cortisol and is associated with impaired memory and lower hippocampal volume, an abnormality associated with vulnerability to depression (O'Hara et al., 2007). These observations suggest that the S allele confers increased vulnerability to hyperactivity of the hypothalamic-pituitary-adrenal axis.
Developing an Intervention Research Program
We propose an intervention development model integrating current biopsychosocial concepts of late-life depression with strategies needed to upgrade the quality of existing community services and a model of health behavior influencing access to them (Figure 1). Strengthening community-based services requires identification of incentives, mainstreamed training, and administrative measures that make interventions “organic” to each service. The access model conceptualizes healthcare utilization as the end-product of interactions among three domains, i.e. predisposing and enabling factors as well as the need for care. Need for care is the most proximal determinant of utilization. In depressed older adults, the need domain may include personal suffering, suicidal ideation, disability, medical morbidity, cognitive impairment, and family disruption. The domain of factors predisposing (positively or negatively) depressed older person to seek care may include stigma, misinformation, ageism, isolation, ageism, ethnicity and gender. The domain of factors enabling depressed older persons to receive care may include personal and family resources, availability of transportation, treatment services, and family able and willing to help.
Goals
The existing treatments for geriatric depression do not address its clinical heterogeneity, are moderately efficacious, and are often poorly implemented in the community. For this reason, a far reaching research program must address access to care, but go above and beyond access, and aim to develop novel treatments for subgroups of older adults with distinct biological, clinical and social characteristics and improve the way they are implemented in the community. Guided by the above integrated model, optimal development of intervention research in late-life depression may proceed in three directions: 1) Develop personalized interventions at the patient/client level mitigating the impact of experienced adversity; 2) improve the delivery of traditional and novel treatments by community-based agencies, supported by the current reimbursement system, so that they can be disseminated; and 3) facilitate access to care by improving the identification of those in need and by addressing barriers to care.
Reaching the “Real World”
Studying an intervention for late-life depression needs to be mindful of the time required to make the intervention available to the community. The design of intervention studies depends on where the intervention lies in the proposed model. Novel interventions for subgroups of depressed older adults need to start from the biopsychosocial model of late-life depression and identify moderators of treatment response, i.e. patient characteristics assessed at baseline associated with differential effectiveness in the intervention arm than the comparison arm. The results of these analyses may then be used to guide the design of the intervention. Initial testing of a novel treatment usually depends on well trained research staff to deliver the intervention. We argue, however, that this initial testing should focus mainly on feasibility, fidelity of administration, and identification of aspects of the intervention that can be mainstreamed, simplified, and sharpened. If there is a signal of efficacy during this initial testing, the next step should be a larger effectiveness trial involving community-based professionals.
A different experimental approach can be taken when the research goal is to identify whether an intervention with known efficacy needs to be tested in services supported by the current reimbursement system. Such interventions need to focus not only on training of community-based health workers but also on organizational changes that would make an intervention organic to the community setting. A similar approach may be taken by interventions aiming to improve identification and referral of patients late-life depression to community agencies.
Making an intervention organic to the community agency in which it is offered requires that the intervention itself may need to change so that it accommodates to the organization and practice of the community agency and makes maximal use of its assets. Furthermore, the community-based agency needs to introduce changes in its operation to assimilate the new intervention. These requirements create a dialectic tension. On the one hand, the intervention's theoretical and empirical principles need to be safeguarded. On the other hand, community-based services may face competing demands on how they structure routine practice and demand that the intervention changes drastically to fit them.
Resolution of the above tension necessitates a dialogue between investigators and their community partners setting forward a process that would inform decisions ensuring that the intervention maintains its core features and enhances the agencies’ ability to implement it with fidelity. Working with separate agencies within a single sector of care, one can arrive to an intervention that reflects common elements of healthcare practice rather than the idiosyncrasies of a single agency, e.g. compliance with insurance regulations, alignment with patient needs derived from the biopsychosocial model of depression, compatibility with the skill set of community providers, and use of language consistent with routine practice of community agencies. Even agencies treating the same patient population have differences in their procedures and structure necessitating changes on how an intervention is implemented in order to “fit” each agency (accommodation of the intervention to the agency). Along with changes in the intervention to accommodate to the agency, the agency needs to assimilate the intervention into its practices, e.g. make decisions about task allocation, add questions in screening or routine assessments or develop additional database queries to support supervision.
What follows describes three interventions that exemplify distinct experimental approaches necessitated by their different stage of their development.
Developing a Novel Intervention for a Subgroup of Late-Life Depression
An intervention was developed for post-stroke depression, a subgroup of “vascular depression”. Among stroke patients in acute and rehabilitation hospitals, the mean frequency of major and minor depression is 39% (Morris et al., 1990) . However, 37% of patients who are not depressed after stroke develop depression during a 2-year follow-up(Robinson et al., 1987) . Antidepressants reduce mood symptoms but it is unclear whether they can lead to remission of post-stroke stroke (Hackett et al., 2005). Even the reduction of depressive symptoms by antidepressants is of uncertain clinical value (Hackett et al., 2005) . Furthermore, many depressed stroke patients have executive dysfunction, a cognitive abnormality associated with disability and poor and slow response to antidepressants (Kiosses et al., 2001; Kalayam and Alexopoulos, 1999; Alexopoulos et al., 2004). Finally, the success of antidepressants depends on individualization of treatment requiring frequent appointments that demoralized stroke victims and their families may not attend.
While pathophysiological processes of stroke may contribute to post-stroke depression (Lyketsos et al., 1998), non-pharmacological interventions may play an important role in its treatment (Hibbard et al., 1990)),(Watzlawick and Coyne, 1980). Recently, an RCT showed that a care management program resulted in higher remission rates than usual care in stroke survivors with major or minor depression (Williams et al., 2007); the intervention helped patients to recognize depression and accept treatment, offered an antidepressant, and monitored and adjusted treatment. These findings serve as a signal of the potential value of psychosocial interventions.
Ecosystem Focused Therapy (EFT) is a new intervention, based on the concept that depression and stroke introduce novel problems and, at the same time, reduce the patients’ ability to solve them. Both conditions impair various functions and both lead to cognitive impairment and impersistence thus interfering with rehabilitation efforts. Improving the patients’ problem solving skills is helpful but often insufficient to reduce adversity experienced by depressed stroke victims and mobilize them to use rehabilitation treatment. For this reason, EFT focuses on the “ecosystem” (patient + environment + family member/ caregiver) of which the patient is part. Accordingly, EFT: a) imparts to the patient skills maximizing his/her remaining functions; b) modifies the patient's physical environment; c) engages family members/caregivers in helping the patient bring to bear his/her skills. EFT uses problem solving therapy as its framework along with a “kit” with tools that can be used by patients and caregivers to make the environment conducive to adaptation. Enabling the patient to assimilate new skills and changing the patient's environment, including caregivers, to accommodate to the patients’ state, offers patients a good chance at adaptation, increases their sense of mastery, and may reduce depression. EFT is consistent with Lawton's model of adaptive functioning, according to which adaptive behavior is a function of the person's competence and the demands of the environment to which he/she is exposed (Lawton et al., 1982) . Using the WHO concepts, we expect that EFT will not influence neurological impairment, but reduce disability, and handicap (ability to function within societal roles in the family, community and workplace).
By intervening at the “ecosystem” level, EFT acts in synergy with specialized rehabilitation treatments needed by depressed stroke survivors. It does so in three ways: 1) It increases the patients’ engagement in rehabilitation treatments; 2) It modifies the “ecosystem” so that the patient can maximally utilize the functional gains made during specific rehabilitation treatments; 3) It enables the patient to utilize community resources, e.g. support groups, community-based exercise programs and recreational services for physically challenged, and religious institutions.
The first study of EFT should optimally use therapists, members of the research team with experience in manualized interventions and ability to identify aspects of EFT that can be mainstreamed and improved. The focus of the initial trial should be on fidelity of administration, acceptance of patients, caregivers and providers. The trial may include a control so that it can yield preliminary data on efficacy as well as moderators of treatment response. If a signal of efficacy is identified, arguably the ensuing definitive effectiveness trial may be implemented in the community. After training and organizational changes, EFT may be integrated in the treatment armamentarium of outpatient stroke rehabilitation centers (for ambulatory patients) and home healthcare agencies (for homebound patients) and administered by the social workers of these organizations who are reimbursed for their services. While this approach entails the risk of a false negative result (incorrectly show that EFT is ineffective), it has the advantage of bringing EFT closer to dissemination.
Bringing an Intervention of Known Effectiveness to the Community
Most depressed older adults are treated by primary care physicians (PCPs) thus making primary care a strategic front in the war against geriatric depression. Studies, including those of our Center, have shown that collaborative care offered at the primary care setting has superior outcomes to usual care. However, inadequate third-party reimbursements restrict collaborative care to large providers, e.g. Health Maintenance Organizations, which serve a minority of the US population. This project address this barrier by developing a depression care management model (C-DCM) relying on collaboration of PCPs with trained social workers (MSWs) employed by community-based, public and nonprofit mental health clinics. While widely available, mental health clinics are rarely connected to primary care practices and underutilized by depressed elders. To utilize this resource, collaborative care needs to be revised in a way that satisfies three conditions. First, it should meet the clinical needs of depressed elders. Second, it should be modified in a way that can be used by MSWs and bring to bear their special skills in helping these patients. Third, it should include procedures reimbursed by existing insurance codes so that it adds no cost to PCPs or mental health clinics.
Comorbid medical illnesses and need for pharmacotherapy necessitate collaboration of MSWs with primary care physicians. Stressors such as poverty, isolation, and transportation problems perpetuate depression, and need to be addressed (Figure 1). Depression is a dynamic state requiring monitoring of both symptoms and contributing factors and proper targeting of interventions. Misinformation and bias reduce treatment adherence of depressed elders. Involving patients in treatment decisions sooner than later is critical since most patients ultimately decide for themselves what treatment they will accept (Wills and Holmes-Rovner, 2006). Exploration of a patient's understanding is central to involving patients in clinical decision-making and may improve treatment adherence and satisfaction.
MSWs often have training in assessment, in principles of psychotherapy and in linking their clients with needed services. However, they have limited experience in collaborating with PCPs around medical problems and psychopharmacology. Moreover, they often lack experience in the problems of depressed elderly patients, including special needs, misinformation, bias, and treatment adherence. Based on the assimilation/accommodation principle, C-DCM needs to be a parsimonious intervention that trains MSWs to: 1. Establish a relationship with the referring PCP; 2. Monitor the course of depressive disorder and offer ongoing information to PCPs on the patients’ status and the treatment recommended by pharmacotherapy guidelines; 3. Communicate with the patient's PCP about medical complaints as they emerge; 4. Identify stressors affecting the patients’ depression and functioning; 5. Link patients to services when needed; 6. Provide supportive therapy; 7. Identify misinformation and bias and offer psychoeducation; and 8. Work with the patient to select an appropriate treatment based on informed treatment preferences, and encourage adherence. On an organizational level, the intervention will help PCP practices to screen for depression, develop a referral process to mental health clinics in which MSWs participate, and collaborate with MSWs in offering care.
The first step in developing C-DCM is a project to identify whether and to whom C-DCM can be taught and whether and whom C-DCM can help within a narrow set of practices and clinics. The definitive study that follows should use this knowledge to mainstream C-DCM and training and conduct a multi-site study with PCP practices and MH clinics serving heterogeneous populations. Such study will yield information generalizable to large real world patients, practices and clinics, assess cost and support efforts at dissemination.
Increasing Access to Depression Care of Low Income Older Persons
Ethnically-diverse, low-income, older adults are at high risk for depression, have limited access and low acceptance of mental health care, and receive fragmented health services. Drawing from our model (Figure 1), barriers to connecting seniors to mental health evaluation, and to subsequent engagement in treatment fall in three domains: 1. attitudinal (stigma, misattribution of symptoms, denial of need for treatment) and concrete barriers (access, transportation, cost); 2. failure to integrate individuals’ preferences and values concerning mental health services into the referral process; and 3. a gap between community social service and mental health agencies. In designing an intervention to accommodate to these barriers, one challenge is the need to understand and address the unique experience of each older person and what prevents him/her from receiving evaluation and engaging in treatment. Of the clinically sound treatment options, one needs to assist the person in selecting one that suits his/her preferences and circumstances. The next challenge is simplifying this complex decision-making process so that community workers can successfully implement it.
The ENGAGE intervention targets social service agencies that serve low income older persons but themselves do not provide treatment. It consists of training bachelors level workers in addressing attitudinal and concrete barriers of referring depressed older patients to treatment and in increased treatment adherence. It also incorporates the shared decision-making approach, which unlike traditional medical decision-making, involves a collaborative process whereby individuals articulate personal values and preferences and clinicians provide information to arrive at a mutually-agreed upon, informed decision (Simon et al., 2006; Adams and Drake, 2006). Shared decision making may provide the added benefit of enhancing autonomy and empowerment of depressed older persons. Finally, ensuring connection to appropriate mental health settings may increase the likelihood that an individual will implement their decision. Based on the accommodation/assimilation principle, investigators work with the agencies’ administrators and staff to develop procedures that enable workers to assimilate into their practices screen for depression and to develop relationships with treatment services and facilitate referrals.
The first step in testing the ENGAGE intervention is a study aimed to test the feasibility of training MSWs, the implementation of organizational changes facilitating referrals, and the acceptability of ENGAGE by older clients, MSWs and administrators of social services. The definitive study will be a randomized controlled trial in agencies around the country, that will study the effectiveness of ENGAGE integrated into the practices of these agencies and administered by their case worker staff.
Conclusion
The proposed intervention development model may serve as a conceptual map of the role of new interventions designed to reduce the burden of late life depression. We suggest that our model provides conceptual guidance on how to shorten the testing cycle and bring urgently needed novel treatments and implementation approaches to the community. Replication studies will happen at any stage of the efficacy-effectiveness-implementation-dissemination continuum. We propose, however, that most of support should be directed to those studies that take rational risks, and after adequate preliminary evidence, make the next step along the testing continuum.
ACKNOWLEDGEMENTS
This work was supported by NIMH grants P30 MH085943, RO1 MH079414, the TRU and the Sanchez Foundations.
Footnotes
CONFLICT OF INTEREST
George S. Alexopoulos has recieved grants from Cephalon, Forest and is a consultant at Scientific Advisory Board of Forest, Sanofi-Aventis. He is also a stockholder of Johnson & Johnson and is a member of Speakers’ Bureau: Forest, Lilly, Bristol Meyers Squibb, Pfizer, Janssen. Martha L. Bruce has no conflict of interest.
REFERENCES
- Adams J, Drake R. Shared Decision Making and Evidence-Based Practice. Community Mental Health Journal. 2006;42:87–105. doi: 10.1007/s10597-005-9005-8. [DOI] [PubMed] [Google Scholar]
- Aizenstein HJ, Nebes RD, Meltzer CC, Fukui MB, Williams RL, Saxton J, Houck PR, Carter CS, Reynolds CF, 3rd, DeKosky ST. The relation of White Matter Hyperintensities to implicit learning in healthy older adults. Int J Geriatr Psychiatry. 2002;17:664–9. doi: 10.1002/gps.685. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS. Frontostriatal and limbic dysfunction in late-life depression. Am J Geriatr Psychiatry. 2002;10:687–95. [PubMed] [Google Scholar]
- Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–70. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Katz IR, Bruce ML, Heo M, Ten Have T, Raue P, Bogner HR, Schulberg HC, Mulsant BH, Reynolds CF., 3rd Remission in depressed geriatric primary care patients: a report from the PROSPECT study. Am J Psychiatry. 2005;162:718–24. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexopoulos GS, Kiosses DN, Choi SJ, Murphy CF, Lim KO. Frontal white matter microstructure and treatment response of late-life depression: a preliminary study. Am J Psychiatry. 2002a;159:1929–32. doi: 10.1176/appi.ajp.159.11.1929. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Kiosses DN, Klimstra S, Kalayam B, Bruce ML. Clinical presentation of the “depression-executive dysfunction syndrome” of late life. Am J Geriatr Psychiatry. 2002b;10:98–106. [PubMed] [Google Scholar]
- Alexopoulos GS, Kiosses DN, Murphy C, Heo M. Executive dysfunction, heart disease burden, and remission of geriatric depression. Neuropsychopharmacology. 2004;29:2278–84. doi: 10.1038/sj.npp.1300557. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Silbersweig D, Charlson M. Clinically defined vascular depression. Am J Psychiatry. 1997;154:562–5. doi: 10.1176/ajp.154.4.562. [DOI] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- Ballmaier M, Toga AW, Blanton RE, Sowell ER, Lavretsky H, Peterson J, Pham D, Kumar A. Anterior cingulate, gyrus rectus, and orbitofrontal abnormalities in elderly depressed patients: an MRI-based parcellation of the prefrontal cortex. Am J Psychiatry. 2004;161:99–108. doi: 10.1176/appi.ajp.161.1.99. [DOI] [PubMed] [Google Scholar]
- Brodaty H, Luscombe G, Parker G, Wilhelm K, Hickie I, Austin MP, Mitchell P. Early and late onset depression in old age: different aetiologies, same phenomenology. J Affect Disord. 2001;66:225–36. doi: 10.1016/s0165-0327(00)00317-7. [DOI] [PubMed] [Google Scholar]
- Butters MA, Becker JT, Nebes RD, Zmuda MD, Mulsant BH, Pollock BG, Reynolds CF., 3rd Changes in cognitive functioning following treatment of late-life depression. Am J Psychiatry. 2000;157:1949–54. doi: 10.1176/appi.ajp.157.12.1949. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–9. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Comings DE, MacMurray JP, Gonzalez N, Ferry L, Peters WR. Association of the serotonin transporter gene with serum cholesterol levels and heart disease. Mol Genet Metab. 1999;67:248–53. doi: 10.1006/mgme.1999.2870. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52:193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Neuroimaging abnormalities in the amygdala in mood disorders. Ann N Y Acad Sci. 2003;985:420–44. doi: 10.1111/j.1749-6632.2003.tb07098.x. [DOI] [PubMed] [Google Scholar]
- Egner T, Etkin A, Gale S, Hirsch J. Dissociable neural systems resolve conflict from emotional versus nonemotional distracters. Cereb Cortex. 2008;18:1475–84. doi: 10.1093/cercor/bhm179. [DOI] [PubMed] [Google Scholar]
- Elderkin-Thompson V, Kumar A, Bilker WB, Dunkin JJ, Mintz J, Moberg PJ, Mesholam RI, Gur RE. Neuropsychological deficits among patients with late-onset minor and major depression. Arch Clin Neuropsychol. 2003;18:529–49. doi: 10.1016/s0887-6177(03)00022-2. [DOI] [PubMed] [Google Scholar]
- Erickson K, Drevets W, Schulkin J. Glucocorticoid regulation of diverse cognitive functions in normal and pathological emotional states. Neurosci Biobehav Rev. 2003;27:233–46. doi: 10.1016/s0149-7634(03)00033-2. [DOI] [PubMed] [Google Scholar]
- Etkin A, Egner T, Peraza DM, Kandel ER, Hirsch J. Resolving emotional conflict: a role for the rostral anterior cingulate cortex in modulating activity in the amygdala. Neuron. 2006;51:871–82. doi: 10.1016/j.neuron.2006.07.029. [DOI] [PubMed] [Google Scholar]
- Frodl T, Meisenzahl EM, Zetzsche T, Born C, Jager M, Groll C, Bottlender R, Leinsinger G, Moller HJ. Larger amygdala volumes in first depressive episode as compared to recurrent major depression and healthy control subjects. Biol Psychiatry. 2003;53:338–44. doi: 10.1016/s0006-3223(02)01474-9. [DOI] [PubMed] [Google Scholar]
- Hackett ML, Anderson CS, House AO. Management of depression after stroke: a systematic review of pharmacological therapies. Stroke. 2005;36:1098–103. doi: 10.1161/01.STR.0000162391.27991.9d. [DOI] [PubMed] [Google Scholar]
- Hibbard MR, Grober SE, Gordon WA, Aletta EG. Modification of cognitive psychotherapy for the treatment of post-stroke depression. Behav Therapist. 1990;29:618–624. [Google Scholar]
- Hickie I, Scott E, Mitchell P, Wilhelm K, Austin MP, Bennett B. Subcortical hyperintensities on magnetic resonance imaging: clinical correlates and prognostic significance in patients with severe depression. Biol Psychiatry. 1995;37:151–60. doi: 10.1016/0006-3223(94)00174-2. [DOI] [PubMed] [Google Scholar]
- Hickie IB, Naismith SL, Ward PB, Scott EM, Mitchell PB, Schofield PR, Scimone A, Wilhelm K, Parker G. Serotonin transporter gene status predicts caudate nucleus but not amygdala or hippocampal volumes in older persons with major depression. J Affect Disord. 2007;98:137–42. doi: 10.1016/j.jad.2006.07.010. [DOI] [PubMed] [Google Scholar]
- Howren MB, Lamkin DM, Suls J. Associations of Depression With C-Reactive Protein, IL-1, and IL-6: A Meta-Analysis. Psychosom Med. 2009 doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- Kalayam B, Alexopoulos GS. Prefrontal dysfunction and treatment response in geriatric depression. Arch Gen Psychiatry. 1999;56:713–8. doi: 10.1001/archpsyc.56.8.713. [DOI] [PubMed] [Google Scholar]
- Kiosses DN, Klimstra S, Murphy C, Alexopoulos GS. Executive dysfunction and disability in elderly patients with major depression. Am J Geriatr Psychiatry. 2001;9:269–74. [PubMed] [Google Scholar]
- Krishnan KR, Hays JC, Blazer DG. MRI-defined vascular depression. Am J Psychiatry. 1997;154:497–501. doi: 10.1176/ajp.154.4.497. [DOI] [PubMed] [Google Scholar]
- Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. 2008;455:894–902. doi: 10.1038/nature07455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A, Gupta RC, Albert Thomas M, Alger J, Wyckoff N, Hwang S. Biophysical changes in normal-appearing white matter and subcortical nuclei in late-life major depression detected using magnetization transfer. Psychiatry Res. 2004;130:131–40. doi: 10.1016/j.pscychresns.2003.12.002. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Moss M, Fulcomer M, Kleban MH. A research and service oriented multilevel assessment instrument. J Gerontol. 1982;37:91–9. doi: 10.1093/geronj/37.1.91. [DOI] [PubMed] [Google Scholar]
- Lockwood KA, Alexopoulos GS, van Gorp WG. Executive dysfunction in geriatric depression. Am J Psychiatry. 2002;159:1119–26. doi: 10.1176/appi.ajp.159.7.1119. [DOI] [PubMed] [Google Scholar]
- Lyketsos CG, Treisman GJ, Lipsey JR, Morris PL, Robinson RG. Does stroke cause depression? Journal of Neuropsychiatry & Clinical Neurosciences. 1998;10:103–7. doi: 10.1176/jnp.10.1.103. [DOI] [PubMed] [Google Scholar]
- MacQueen GM, Campbell S, McEwen BS, Macdonald K, Amano S, Joffe RT, Nahmias C, Young LT. Course of illness, hippocampal function, and hippocampal volume in major depression. Proc Natl Acad Sci U S A. 2003;100:1387–92. doi: 10.1073/pnas.0337481100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS. Mood disorders and allostatic load. Biol Psychiatry. 2003;54:200–7. doi: 10.1016/s0006-3223(03)00177-x. [DOI] [PubMed] [Google Scholar]
- Miller DB, O'Callaghan JP. Effects of aging and stress on hippocampal structure and function. Metabolism. 2003;52:17–21. doi: 10.1016/s0026-0495(03)00296-8. [DOI] [PubMed] [Google Scholar]
- Morris PL, Robinson RG, Raphael B. Prevalence and course of depressive disorders in hospitalized stroke patients. Int J Psychiatry Med. 1990;20:349–64. doi: 10.2190/N8VU-6LWU-FLJN-XQKV. [DOI] [PubMed] [Google Scholar]
- Morris PL, Robinson RG, Raphael B, Samuels J, Molloy P. The relationship between risk factors for affective disorder and poststroke depression in hospitalised stroke patients. Aust N Z J Psychiatry. 1992;26:208–17. [PubMed] [Google Scholar]
- Murphy CF, Alexopoulos GS. Longitudinal association of initiation/perseveration and severity of geriatric depression. Am J Geriatr Psychiatry. 2004;12:50–6. [PubMed] [Google Scholar]
- Nakatani D, Sato H, Sakata Y, Shiotani I, Kinjo K, Mizuno H, Shimizu M, Ito H, Koretsune Y, Hirayama A, Hori M. Influence of serotonin transporter gene polymorphism on depressive symptoms and new cardiac events after acute myocardial infarction. Am Heart J. 2005;150:652–8. doi: 10.1016/j.ahj.2005.03.062. [DOI] [PubMed] [Google Scholar]
- Nebes RD, Pollock BG, Houck PR, Butters MA, Mulsant BH, Zmuda MD, Reynolds CF., 3rd Persistence of cognitive impairment in geriatric patients following antidepressant treatment: a randomized, double-blind clinical trial with nortriptyline and paroxetine. J Psychiatr Res. 2003;37:99–108. doi: 10.1016/s0022-3956(02)00085-7. [DOI] [PubMed] [Google Scholar]
- Nestler EJ. Epigenetic mechanisms in psychiatry. Biol Psychiatry. 2009;65:189–90. doi: 10.1016/j.biopsych.2008.10.030. [DOI] [PubMed] [Google Scholar]
- O'Brien J, Ames D, Chiu E, Schweitzer I, Desmond P, Tress B. Severe deep white matter lesions and outcome in elderly patients with major depressive disorder: follow up study. Bmj. 1998;317:982–4. doi: 10.1136/bmj.317.7164.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Hara R, Schroder CM, Mahadevan R, Schatzberg AF, Lindley S, Fox S, Weiner M, Kraemer HC, Noda A, Lin X, Gray HL, Hallmayer JF. Serotonin transporter polymorphism, memory and hippocampal volume in the elderly: association and interaction with cortisol. Mol Psychiatry. 2007;12:544–55. doi: 10.1038/sj.mp.4001978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pezawas L, Meyer-Lindenberg A, Drabant EM, Verchinski BA, Munoz KE, Kolachana BS, Egan MF, Mattay VS, Hariri AR, Weinberger DR. 5-HTTLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nat Neurosci. 2005;8:828–34. doi: 10.1038/nn1463. [DOI] [PubMed] [Google Scholar]
- Robinson RG, Bolduc PL, Price TR. Two-year longitudinal study of poststroke mood disorders: diagnosis and outcome at one and two years. Stroke. 1987;18:837–43. doi: 10.1161/01.str.18.5.837. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ. Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2000;160:1761–8. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- Sheline YI. 3D MRI studies of neuroanatomic changes in unipolar major depression: the role of stress and medical comorbidity. Biol Psychiatry. 2000;48:791–800. doi: 10.1016/s0006-3223(00)00994-x. [DOI] [PubMed] [Google Scholar]
- Sheline YI. Neuroimaging studies of mood disorder effects on the brain. Biol Psychiatry. 2003;54:338–52. doi: 10.1016/s0006-3223(03)00347-0. [DOI] [PubMed] [Google Scholar]
- Simon D, Schorra G, Wirtzb M, Vodermaierc A, Casparic C, Neunerd B, Spiesd C, Kronese T, Kellere H, Edwardsf A, Loha A, Härtera M. Development and first validation of the shared decision-making questionnaire (SDM-Q) Patient Education and Counseling. 2006;63:319–327. doi: 10.1016/j.pec.2006.04.012. [DOI] [PubMed] [Google Scholar]
- Simpson S, Baldwin RC, Jackson A, Burns AS. Is subcortical disease associated with a poor response to antidepressants? Neurological, neuropsychological and neuroradiological findings in late-life depression. Psychol Med. 1998;28:1015–26. doi: 10.1017/s003329179800693x. [DOI] [PubMed] [Google Scholar]
- Smith APR, Stephan KE, Rugg MD, Dolan RJ. Task and Content Modulate Amygdala-Hippocampal Connectivity in Emotional Retrieval. Neuron. 2006;49:631–638. doi: 10.1016/j.neuron.2005.12.025. [DOI] [PubMed] [Google Scholar]
- Smith GS, Kramer E, Hermann CR, Goldberg S, Ma Y, Dhawan V, Barnes A, Chaly T, Belakhleff A, Laghrissi-Thode F, Greenwald B, Eidelberg D, Pollock BG. Acute and chronic effects of citalopram on cerebral glucose metabolism in geriatric depression. Am J Geriatr Psychiatry. 2002;10:715–23. [PubMed] [Google Scholar]
- Sneed JR, Roose SP, Keilp JG, Krishnan KR, Alexopoulos GS, Sackeim HA. Response inhibition predicts poor antidepressant treatment response in very old depressed patients. Am J Geriatr Psychiatry. 2007;15:553–63. doi: 10.1097/JGP.0b013e3180302513. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Taylor WD, McQuoid DR, Krishnan KR. Short/long heterozygotes at 5HTTLPR and white matter lesions in geriatric depression. Int J Geriatr Psychiatry. 2008;23:244–8. doi: 10.1002/gps.1869. [DOI] [PubMed] [Google Scholar]
- Wagar BM, Thagard P. Spiking Phineas Gage: a neurocomputational theory of cognitive-affective integration in decision making. Psychol Rev. 2004;111:67–79. doi: 10.1037/0033-295X.111.1.67. [DOI] [PubMed] [Google Scholar]
- Watzlawick P, Coyne JC. Depression following stroke: brief, problem-focused family treatment. Family Process. 1980;19:13–8. doi: 10.1111/j.1545-5300.1980.00013.x. [DOI] [PubMed] [Google Scholar]
- Williams LS, Kroenke K, Bakas T, Plue LD, Brizendine E, Tu W, Hendrie H. Care management of poststroke depression: a randomized, controlled trial. Stroke. 2007;38:998–1003. doi: 10.1161/01.STR.0000257319.14023.61. [DOI] [PubMed] [Google Scholar]
- Wills CE, Holmes-Rovner M. Integrating Decision Making and Mental Health Interventions Research: Research Directions. Clin Psychol (New York) 2006;13:9–25. doi: 10.1111/j.1468-2850.2006.00002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]