Abstract
It has been suggested that chemotherapy treatment for cancer may contribute to cognitive decline in older cancer survivors. This issue is particularly important given that subtle cognitive impairment, particularly in cognitive processing speed, can affect functional status and quality of life for older adults. Multivariate regression of data from a longitudinal randomized controlled trial of older adults revealed a trend toward decreased performance after cancer treatment with chemotherapy on several functional measures associated with processing speed (as compared to matched individuals who did not have cancer). Additional analyses revealed that a subset of the chemotherapy treated adults demonstrated a reliable negative change on several measures of processing speed. While inconclusive, this hypothesis generating work suggests that cognitive dysfunction following cancer treatment may contribute to disability observed in older cancer survivors. Further research is needed to determine the significance of the relationship between cognitive and functional impairment in older cancer survivors.
Keywords: Cancer survivor, cognition, speed of processing, functional impairment, quality of life
Introduction
Coupled with the growing aging population, increases in life expectancy following cancer treatment have extensive implications for increased burdens of cancer survivorship in healthcare systems. Cancer survivorship is associated with disability and poorer health in older adults(Keating et al., 2005, Ness et al., 2006, Chirikos et al., 2002). Older cancer survivors identify more mobility and instrumental activity of daily living (IADL) limitations than peers without such history(Hewitt et al., 2003). Although cancer type and medical co-morbidity are predictors of diminished health status, other modifiable predictors of poor functional outcomes in cancer survivorship have not been identified(Hewitt et al., 2003).
A number of studies indicate that cancer chemotherapy may contribute to cognitive impairment in cancer survivors(Ahles and Saykin, 2001, Castellon et al., 2004, Hurria et al., 2006b, Schagen et al., 2001, Wefel et al., 2004). The literature suggests that cognitive impairments may occur in all cognitive domains, including processing speed, and that a meaningful proportion of older chemotherapy treated breast cancer patients have measurable deficits on formal neuropsychological testing(Hurria et al., 2006b). In geriatric populations even subtle cognitive impairments, particularly deficits in processing speed, are associated with functional declines(Comijs et al., 2005). Thus, the impact of chemotherapy on processing speed in older cancer patients may be an important contributor to functional impairment and diminished quality of life in survivorship.
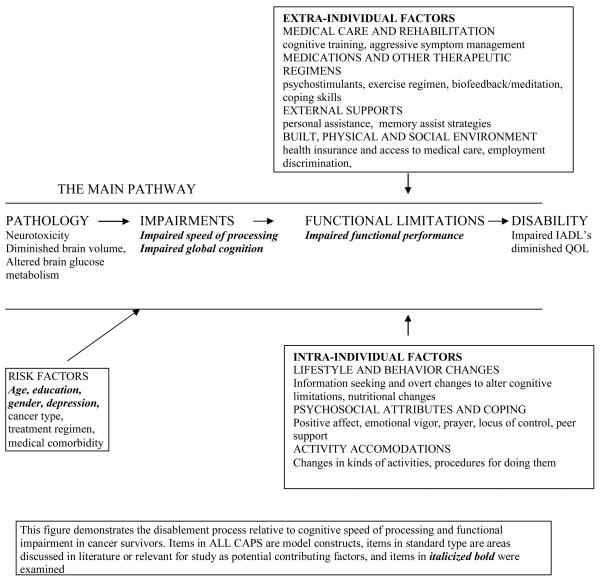
The functional declines observed in older cancer survivors are likely to be multifactorial and complex. They may include a profound impairment in directly affected body systems (for example continence and sexual function in prostate cancer survivors) as well as subtle impairment in global function as the result of poorly defined systemic effects of illness or treatment. Important issues impacting function in older cancer survivors may include disease state, treatment received, comorbidities, subclinical conditions, nutritional status, activity level, social involvement, emotional functioning, and cognitive function. Because of the complex and interrelated contribution of each of these factors to functioning/disability in cancer survivorship, a structured approach to conceptualizing the role of processing speed impairment is helpful. The Disablement Process Model developed by Verbrugge and Jette (Verbrugge and Jette, 1994) provides a relevant theoretical model that links functioning in the speed of processing domain to functioning and activities of daily life, and describes the personal and environmental factors that may impact disablement. Figure 1 reflects how this model might be adapted to conceptualize the complex factors contributing to functioning/disability in older cancer survivors. The design of the current study allowed us to address issues related to processing speed and performance-based functional measures. As demonstrated in Figure 1, disruption of these components interacts with internal and external environmental factors, and may have a marked influence on subsequent function and disability.
FIGURE 1.
Disablement Process Model demonstrating relationship between cognitive impairment and disability in cancer survivors
One prospective longitudinal trial examined functional status in recent older breast cancer survivors, and did not identify functional declines(Hurria et al., 2006a). This study, however, utilized self-report functional assessments, which may not be sensitive to early decline. Other longitudinal studies of function relying on self-report measures have not identified diminished function in older cancer patients(Given et al., 2001, Watters et al., 2003). No reports were identified in the literature utilizing performance-based functional assessments to identify subtle functional decline in cancer survivors. The ACTIVE database provides the opportunity to address this issue with measures rigorously designed to assess cognition and function.
Methods
The ACTIVE Study
The University of Alabama at Birmingham Institutional Review board approved all study procedures. The ACTIVE study was a randomized controlled trial to test the effects of cognitive training on daily function enrolling a total of 2,802 persons (age 65-94) in a four-group design (Memory, Reasoning, Speed of Processing Training interventions and the no-contact control group) between March 1998 and October 1999 at 6 different study sites. ACTIVE enrolled adults (age 65-94) who had not experienced functional decline and who did not have health conditions that would limit longitudinal follow-up. Treatment for cancer with chemotherapy or radiation therapy prior to baseline assessment was an exclusion factor for the parent study. For extensive detail on ACTIVE screening procedure, see Jobe et al (Jobe et al., 2001).
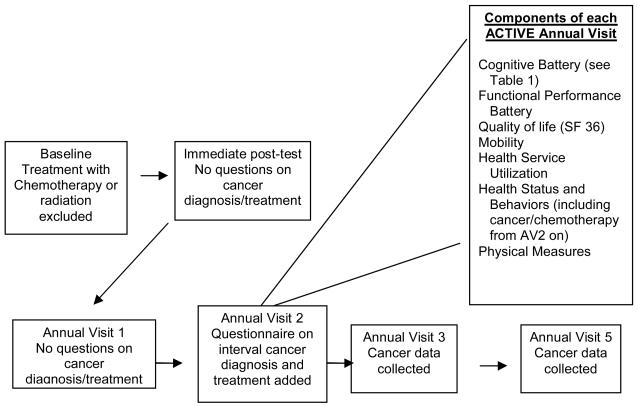
To investigate the effects of chemotherapy treatment on cognitive and functional outcomes in older adults, data from the 704 participants in the no-contact control group of the ACTIVE study were analyzed. ACTIVE participants completed questionnaires at annual visits regarding whether they had received a diagnosis of cancer in the interval since the last study visit. If they had, they were asked to identify cancer site and treatment received. These data are limited to patient self-report. The study initially included three annual follow-up visits (Annual Visit 1,2,3; denoted as AV1 etc.), and was subsequently extended to include a fifth annual visit, AV5. Questions to assess chemotherapy utilization were included in AV2, AV3, and AV5, (no data was collected for AV4) (Figure 2). For these analyses, data from the assessment two years prior to the individual's report of cancer were utilized as the baseline for the individual participant. Data from the visit at which they reported treatment with chemotherapy was utilized as the post-chemotherapy time-point. Among participants randomized to the no-contact control group, 39 reported treatment with chemotherapy subsequent to their baseline assessment Data from two individuals had incomplete depression measures and were excluded from analyses. A comparison group of 37 age, education, and gender-matched participants was identified among control group participants who did not report a cancer treatment history. The matched individual was also from the no contact control group. For the matched untreated participant, the corresponding assessments were analyzed. This approach was utilized to ensure similar exposure to practice effects in both the cancer group and their matched untreated participant. For example, if an individual reported being treated with chemotherapy at AV5, AV3 data were analyzed as pre-chemotherapy data and AV5 data were analyzed as post-chemotherapy data. For the corresponding matched participant who was not treated with chemotherapy, AV3 data were analyzed as the initial assessment and AV5 data were analyzed as post-test data.
FIGURE 2.
Timing of assessments in the ACTIVE Study
2802 Persons aged 65-94 were enrolled in ACTIVE between March 1998 and October 1999 at 6 different study sites. The study was initially funded through Annual Visit 3 (AV3), and was extended through AV5. No data was collected for AV4, however. In addition, questions concerning cancer treatment were not asked at Annual Visit 1. For this analysis, data from the assessment 2-years prior to the individual's report of cancer were utilized as the baseline for the individual participant and their matched untreated participant, and data from the visit at which they reported treatment with chemotherapy was utilized as the post-chemotherapy time-point. Thus individuals reporting chemotherapy treatment may have been approaching 2 years post-chemotherapy.
Measures
The cognitive and functional measures completed by ACTIVE participants at each annual visit are detailed by Ball et al(2002) and Jobe et al(2001). The measures utilized for this analysis assess demographics, depressive symptoms, cognitive speed of processing, and functional performance. They are described below:
Demographics
Upon study entry, participants reported demographic characteristics including age, gender, race, and education. Education was assessed by the number of years of formal education reported by each participant.
Depressive Symptoms
The Center for Epidemiological Studies-Depression (CES-D) is a self-report measure used to assess depressive symptomology(Radloff, 1977). Participants are given 12 statements, such as ‘I felt depressed’ and ‘I had crying spells’. They are asked to rate how frequently they have experienced such symptoms over the last week. Frequency ratings range from ‘never (0)’ to ‘5 to 7 days (3)’ with a range of 0 to 36. Higher scores indicate more depressive symptoms.
UFOV
The Useful Field of View (UFOV®) is a computerized visual information processing speed assessment consisting of four subtests that increase in complexity(Edwards et al., 2006, Edwards et al., 2005). Visual targets (cars and trucks) are presented at increasingly briefer display speeds (between 16 and 500 ms) via the double-staircase method controlled by a full-field, backward mask. The first subtest requires identification of a central target (car or truck); the second subtest requires this central task along with localization of a second peripheral target (car); the third subtest requires the same identification and localization tasks, but also includes distractors (triangles of the same luminance and size as the targets). The final subtest also contains the distractors, but requires participants to discriminate whether two central targets are the same or different while simultaneously locating a peripheral target. Scores are given for each subtest representing the 75% threshold display speed. A composite sum of subtests 1 through 4 was created to assess Cognitive Processing Speed.
WAIS Digit Symbol Substitution is a measure of processing speed that consists of a grid of 93 empty squares, each paired with a number ranging from 1 to 9(Weschler, 1981). Each number is associated with a specific symbol on a key at the top of the page. Subjects are given 90 seconds to record the correct symbol associated with each number above the grid of empty squares. The total number of correctly substituted symbols was used in the analyses, with higher scores indicating better performance.
Timed Instrumental Activities of Daily Living (TIADL)(Owsley et al., 2001, Owsley et al., 2002) assesses performance of laboratory-simulated everyday activities through performance accuracy and time needed to complete each task. Tasks included (a) looking up and repeating a telephone number from a telephone book, (b) counting out change, (c) reading ingredients from labels of cans of food, (d) finding food items on a crowed grocery shelf, and (e) reading instructions from prescription medication bottles. Time penalties are assessed for errors such that more accurate and faster performance is indicated by smaller scores.
The Road Sign Test is a computerized measure of everyday complex reaction time requiring quick and accurate response to road signs(Ball and Owsley, 2000). Combinations of three or six road signs with and without slashes (left arrow, right arrow, bicycle sign or pedestrian sign) are simultaneously presented in different locations on the screen. Participants are instructed to react whenever a sign without a slash appears on the screen, and to ignore, or not react, to the signs with slashes. Participants were required to either click the computer mouse (to pedestrian or bicycle signs without slashes), or move the mouse in the direction of the turn arrow as quickly as possible. The amount of time from the stimulus presentation to the correct reaction from the participant is recorded, resulting in average reaction times for both the three-sign and six-sign displays.
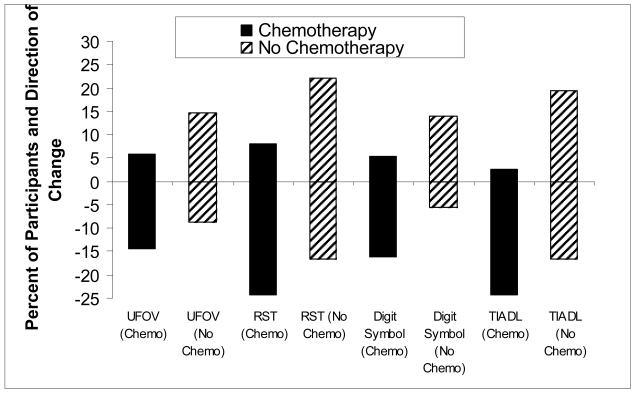
Statistical Analysis
All analyses were performed using SAS software version 9.1.(2006) Normative data derived from baseline scores for the 2802 subjects enrolled in ACTIVE were utilized to convert participant's raw scores on the UFOV®, RST, digit symbol, and TIADL measures at their pre-chemotherapy assessment to z-scores in an attempt to identify individuals who exhibited initial impairment on any of the four_tests. Z-scores of ≤ −1.5 were classified as indicating impairment. Multivariate regression analysis of group means was undertaken to test the association between treatment with chemotherapy and cognitive/functional score at the post-chemotherapy assessment. Composite scores for Everyday Speed and Cognitive Processing Speed were assessed in the multivariate analysis to reduce test-specific performance differences in the assessment of cognitive domains. Age at the pre-chemotherapy assessment, depressive symptoms, chemotherapy/no chemotherapy, and cognitive/functional score at the pre-chemotherapy assessment were included as predictors in the model for each outcome. Additional analyses focused on the identification of an affected subset of participants with regard to processing speed measures and measures of functional performance. The analytic approach was similar to that reported in prospective studies of the impact of chemotherapy on cognition(Wefel et al., 2004, Hurria et al., 2006b). Raw scores and the reliable change index (RCI) were used to identify the proportion of individuals demonstrating negative change within each group. The RCI was computed by dividing the difference between the scores at the pre-chemotherapy and post chemotherapy time-points by the standard error of the measure(Jacobson and Truax, 1991, McSweeny et al., 1993)(see Figure 3 notes). Consistent with the procedure for identifying individuals with impairment at baseline, a RCI of −1.5 or less signified a reliable decline and a RCI of 1.5 or greater signified a reliable improvement. Negative scores for the RCI represented worse performance on the measure.
Figure 3.
Change on Speed of Processing Batteries from Pre-Chemotherapy to Post-Chemotherapy Assessment
Note: This figure demonstrates the percent of participants demonstrating a reliable change and the direction of change for each speed of processing test by treatment group.
RCI = (posttest − pretest) / SEmeas; SEmeas = SD * √(1 − r11)
SD = standard deviation of the measure
r11 = the reliability of the measure (Cronbach's alpha from sample for UFOV and RST; test-retest reliability for TIADL composite; reliability found in WAIS-R manual for digit symbol).
Results
The cancer types reported by ACTIVE participants comprised a heterogeneous group. They reflect a distribution that would be predicted by studies of prevalence in the population, with the notable absence of lung cancers. It is hypothesized that lung cancer patients were lost to attrition because of the rapidly progressive nature of that disease. Of the 39 individuals reporting any type of cancer: breast (n = 14), prostate (n =7), colorectal (n = 3), lymphoma (n = 3), bladder (n = 2), uterine (n = 2), head and neck (n = 2), ovarian (n = 2), multiple myeloma (n = 1), breast/uterine (n = 1), breast/colon (n = 1), breast/cervical/ovarian (n = 1). There were missing depression scores for two individuals, therefore these individuals were excluded from the analyses. A comparison group of 37 age, education, and gender-matched participants was identified among control group participants who did not report a cancer treatment history. No differences between the groups were found for mean age (76.04 for cancer treated with chemotherapy group 75.81 for control, p= .83), gender (28 of 37 female in both groups, p=1.0), education (14.14 years vs. 14.08, p=.93) and depressive symptoms mean score (3.68 vs. 3.79, p=.9).
At the pre-chemotherapy assessment one untreated participant was classified as impaired based on UFOV® performance, and one additional chemotherapy-treated participant was classified as impaired based on the RST. Multivariate regression analysis revealed a trend toward worse post-chemotherapy performance for the chemotherapy group on the Everyday Speed Composite score, a processing speed-related daily function composite comprised of The Road Sign Test (RST) and Timed Instrumental Activities of Daily Living (TIADL), F(1,68) = 3.31, p=.07. Increased age at baseline and poor performance at baseline were each associated with slow processing speed at the post chemotherapy assessment, p's < .02. The analysis for the Cognitive Processing Speed Composite, comprised of subsets 1, 2, 3, and 4 of the UFOV® undertaken in the same manner was not significant (p=.47). Poor UFOV® performance at baseline, older age, and more depressive symptoms were each individually predictive of slower processing speed, p's <.04. A post-hoc power analysis of the unadjusted mean differences in change scores revealed that if the same 1:1 matching design were maintained it would be necessary to have 67 individuals in each chemotherapy group to have power = .80 for finding a significant group difference (alpha level = .05, two-sided) on the Everyday Speed Composite score and 210 in each group to have the same power for finding a difference on the Cognitive Processing Speed Composite.
Analyses of reliable change in performance demonstrated that UFOV® performance declined for 5 of 35 (14%) chemotherapy treated individuals compared to 3 of 34 (9%) non-treated individuals. Similar trends were shown for RST (24% vs. 17%), digit symbol (16% vs. 6%) and TIADL's (24% vs. 17%). Overall, a larger percentage of chemotherapy treated individuals consistently showed reliable declines in functional and processing speed domains as compared to untreated peers (Figure 3). The odds ratio for these changes did not achieve statistical significance (Table 1). The odds ratio of significant negative change in at least one of the speed of processing/functional measures for the chemotherapy treated group was 1.66 (95% CI .65 – 4.20).
Table 1.
Changes in Cognitive and Functional Performance from Pre-Chemotherapy to Post-Chemotherapy Assessment Assessed by the Reliable Change Index.
| Measure | Chemotherapy, n (%) |
No chemotherapy, n (%) |
Odds Ratio* Decline vs. Same and Improve (95% CI) |
p-value* |
|---|---|---|---|---|
| UFOV (n=69) | 1.72 (0.37-7.84) | .4824 | ||
| Improve | 2 (5.71) | 5 (14.71) | ||
| Same | 28 (80.00) | 26 (76.47) | ||
| Decline | 5 (14.29) | 3 (8.82) | ||
| RST (n=73) | 1.61 (0.50-5.09) | .4205 | ||
| Improve | 3 (8.11) | 8 (22.22) | ||
| Same | 25 (67.57) | 22 (61.11) | ||
| Decline | 9 (24.32) | 6 (16.67) | ||
| Digit Symbol (n=73) | 3.29 (0.62-17.52) | .1629 | ||
| Improve | 2 (5.41) | 5 (13.89) | ||
| Same | 29 (78.38) | 29 (80.56) | ||
| Decline | 6 (16.22) | 2 (5.56) | ||
| TIADL (n=73) | 1.61 (0.50-5.09) | .4205 | ||
| Improve | 1 (2.70) | 7 (19.44) | ||
| Same | 27 (72.97) | 23 (63.89) | ||
| Decline | 9 (24.32) | 6 (16.67) |
Odds ratio and p-value were computed using logistic regression analyses with dichotomous outcomes (decline=1 vs. no decline =0) and group as the only predictor.
Discussion
Prematurely diminished cognitive and functional abilities in older adults have significant societal, healthcare utilization, and economic implications. Processing speed, or mental quickness, is a cognitive ability that may predict functional ability in older cancer patients. A great deal of research has documented that normal age-related cognitive changes include declines in the speed at which one can process information (Ball et al., 2002, Salthouse, 1996, Finkel et al., 2005, Levitt et al., 2006). Furthermore, research has indicated that cognitive slowing causes difficulty with the timed performance of everyday tasks that are vital to independence (Owsley et al., 2002) (commonly referred to as TIADLs) such as grocery shopping, medication management, and driving. Quicker processing speed has also been associated with maintained health status (Hultsch et al., 1993) with advancing age as well as improved health-related quality of life (Wolinsky et al., 2006). This study suggests that chemotherapy treatment has a reliably negative impact on measures of cognitive processing speed and related functional performance measures. Consistent trends in the predicted direction in this study raise important questions about the relationship between cancer associated cognitive decline and the disablement process in older cancer survivors.
This study suggests a trend toward decreased performance after cancer treatment with chemotherapy on several functional measures associated with processing speed. Strengths of this analysis include both the longitudinal design of the ACTIVE study and the comprehensive nature of the cognitive and functional performance assessments. Prior studies of older cancer patients utilizing self-report functional performance measures have not demonstrated an effect of chemotherapy(Hurria et al., 2006a, Hurria et al., 2006b, Given et al., 2001), perhaps indicating that the initial impact of cancer treatment on functional outcomes is subtle enough that commonly used measures are not adequately sensitive to detect small but meaningful impairment.
Limitations of this study include the small sample size, the heterogenous group of cancer patients evaluated, and variability in time from exposure to chemotherapy, which may have approached two years in the majority of participants. As a result of these limitations the findings reported here may reflect an underestimation of the impact of cancer and chemotherapy on cognition and function in older adults. This may account for the fact that the proportion of participants with chemotherapy-treated cancer who demonstrated reliable negative change on the cognitive measures evaluated was markedly less than would be predicted based on existing prospective trials with breast cancer patients (Wefel et al., 2004). We attempted to control for practice effects by utilizing data from the same time points from both chemotherapy treated cancer patients and their controls, however the improvement of scores with the repeated administration of cognitive tests is a recognized phenomenon in longitudinal cognitive trials. A reliance on patient self-report of cancer and cancer treatment introduces an element of patient interpretation of their illness and treatment that may impact accuracy of reporting. Additionally, it is important to note that the comparison group participants did not have cancer, thus the analysis does not isolate an exposure to chemotherapy, but rather exposure to cancer treated with chemotherapy.
The descriptive information provided by this study can be used to aid future investigators in formulating studies targeted specifically towards older cancer patients who experience cognitive and functional decline. Further evaluation of the relationship between cognitive decline and functional impairment are called for, as is the development of interventions to explore whether these impairments are responsive to rehabilitation. Indeed, the speed of processing training intervention evaluated in ACTIVE was found to significantly improve performance on the everyday speed measures(Willis et al., 2006) and health-related quality of life(Wolinsky et al., 2006) in predominantly healthy older adults receiving booster training. This type of training has not yet, however, been evaluated in cancer patients.
ACKNOWLEDGEMENT
With respect to the submitted manuscript “Cognitive Speed of Processing and Functional Declines in Older Cancer Survivors: An Analysis of Data from the ACTIVE Trial,” Dr. Ball discloses a financial involvement (stock ownership and consulting) with Visual Awareness, Inc. This company owns the patent to the “Useful Field of View Visual Attention Analyzer,” one of the test instruments that was used in the described study to evaluate speed of processing.
Sponsor's Role: The ACTIVE study was supported by grants from the National Institute on Aging and the National Institute of Nursing Research to Hebrew Senior Life U01 NR04507, Indiana University School of Medicine U01 NR04508, Johns Hopkins University U01 AG14260, New England Research Institutes U01 AG14282, Pennsylvania State University U01 AG14263, University of Alabama-Birmingham U01 AG14289, and University of Florida U01 AG014276.
References
- AHLES TA, SAYKIN A. Cognitive effects of standard-dose chemotherapy in patients with cancer. Cancer Invest. 2001;19:812–20. doi: 10.1081/cnv-100107743. [DOI] [PubMed] [Google Scholar]
- BALL K, BERCH DB, HELMERS KF, JOBE JB, LEVECK MD, MARSISKE M, MORRIS JN, REBOK GW, SMITH DM, TENNSTEDT SL, UNVERZAGT FW, WILLIS SL. Effects of cognitive training interventions with older adults: a randomized controlled trial. Jama. 2002;288:2271–81. doi: 10.1001/jama.288.18.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BALL K, OWSLEY C. Increasing mobility and reducing accidents of older drivers. In: SCHAIE KW, PIETRUCHA M, editors. Mobility and Transportation in the Elderly. Springer Publishing Company, Inc; New York: 2000. [Google Scholar]
- CASTELLON SA, GANZ PA, BOWER JE, PETERSEN L, ABRAHAM L, GREENDALE GA. Neurocognitive performance in breast cancer survivors exposed to adjuvant chemotherapy and tamoxifen. J Clin Exp Neuropsychol. 2004;26:955–69. doi: 10.1080/13803390490510905. [DOI] [PubMed] [Google Scholar]
- CHIRIKOS TN, RUSSELL-JACOBS A, JACOBSEN PB. Functional impairment and the economic consequences of female breast cancer. Women Health. 2002;36:1–20. doi: 10.1300/J013v36n01_01. [DOI] [PubMed] [Google Scholar]
- COMIJS HC, DIK MG, AARTSEN MJ, DEEG DJ, JONKER C. The impact of change in cognitive functioning and cognitive decline on disability, well-being, and the use of healthcare services in older persons. Results of Longitudinal Aging Study Amsterdam. Dement Geriatr Cogn Disord. 2005;19:316–23. doi: 10.1159/000084557. [DOI] [PubMed] [Google Scholar]
- EDWARDS JD, ROSS LA, WADLEY VG, CLAY OJ, CROWE M, ROENKER DL, BALL KK. The useful field of view test: normative data for older adults. Arch Clin Neuropsychol. 2006;21:275–86. doi: 10.1016/j.acn.2006.03.001. [DOI] [PubMed] [Google Scholar]
- EDWARDS JD, VANCE DE, WADLEY VG, CISSELL GM, ROENKER DL, BALL KK. Reliability and validity of useful field of view test scores as administered by personal computer. J Clin Exp Neuropsychol. 2005;27:529–43. doi: 10.1080/13803390490515432. [DOI] [PubMed] [Google Scholar]
- FINKEL D, REYNOLDS CA, MCARDLE JJ, PEDERSEN NL. The longitudinal relationship between processing speed and cognitive ability: genetic and environmental influences. Behav Genet. 2005;35:535–49. doi: 10.1007/s10519-005-3281-5. [DOI] [PubMed] [Google Scholar]
- GIVEN B, GIVEN C, AZZOUZ F, STOMMEL M. Physical functioning of elderly cancer patients prior to diagnosis and following initial treatment. Nurs Res. 2001;50:222–32. doi: 10.1097/00006199-200107000-00006. [DOI] [PubMed] [Google Scholar]
- HEWITT M, ROWLAND JH, YANCIK R. Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58:82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- HULTSCH DF, HAMMER M, SMALL BJ. Age differences in cognitive performance in later life: relationships to self-reported health and activity life style. J Gerontol. 1993;48:P1–11. doi: 10.1093/geronj/48.1.p1. [DOI] [PubMed] [Google Scholar]
- HURRIA A, HURRIA A, ZUCKERMAN E, PANAGEAS KS, FORNIER M, D'ANDREA G, DANG C, MOASSER M, ROBSON M, SEIDMAN A, CURRIE V, VANPOZNAK C, THEODOULOU M, LACHS MS, HUDIS C. A prospective, longitudinal study of the functional status and quality of life of older patients with breast cancer receiving adjuvant chemotherapy. J Am Geriatr Soc. 2006a;54:1119–24. doi: 10.1111/j.1532-5415.2006.00789.x. [DOI] [PubMed] [Google Scholar]
- HURRIA A, ROSEN C, HUDIS C, ZUCKERMAN E, PANAGEAS KS, LACHS MS, WITMER M, VAN GORP WG, FORNIER M, D'ANDREA G, MOASSER M, DANG C, VAN POZNAK C, HURRIA A, HOLLAND J. Cognitive function of older patients receiving adjuvant chemotherapy for breast cancer: a pilot prospective longitudinal study. J Am Geriatr Soc. 2006b;54:925–31. doi: 10.1111/j.1532-5415.2006.00732.x. [DOI] [PubMed] [Google Scholar]
- JACOBSON NS, TRUAX P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–9. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- JOBE JB, SMITH DM, BALL K, TENNSTEDT SL, MARSISKE M, WILLIS SL, REBOK GW, MORRIS JN, HELMERS KF, LEVECK MD, KLEINMAN K. ACTIVE: a cognitive intervention trial to promote independence in older adults. Control Clin Trials. 2001;22:453–79. doi: 10.1016/s0197-2456(01)00139-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KEATING NL, NORREDAM M, LANDRUM MB, HUSKAMP HA, MEARA E. Physical and mental health status of older long-term cancer survivors. J Am Geriatr Soc. 2005;53:2145–52. doi: 10.1111/j.1532-5415.2005.00507.x. [DOI] [PubMed] [Google Scholar]
- LEVITT T, FUGELSANG J, CROSSLEY M. Processing speed, attentional capacity, and age-related memory change. Exp Aging Res. 2006;32:263–95. doi: 10.1080/03610730600699118. [DOI] [PubMed] [Google Scholar]
- MCSWEENY A, CHELUNE G, NAUGLE R, LADERS H. T-scores for change: An illustration of a regression approach to depicting change in clinical neuropsychology. The Clinical Neuropsychologist. 1993;7:300–312. [Google Scholar]
- NESS KK, WALL MM, OAKES JM, ROBISON LL, GURNEY JG. Physical performance limitations and participation restrictions among cancer survivors: a population-based study. Ann Epidemiol. 2006;16:197–205. doi: 10.1016/j.annepidem.2005.01.009. [DOI] [PubMed] [Google Scholar]
- OWSLEY C, MCGWIN G, JR., SLOANE ME, STALVEY BT, WELLS J. Timed instrumental activities of daily living tasks: relationship to visual function in older adults. Optom Vis Sci. 2001;78:350–9. doi: 10.1097/00006324-200105000-00019. [DOI] [PubMed] [Google Scholar]
- OWSLEY C, SLOANE M, MCGWIN G, JR., BALL K. Timed instrumental activities of daily living tasks: relationship to cognitive function and everyday performance assessments in older adults. Gerontology. 2002;48:254–65. doi: 10.1159/000058360. [DOI] [PubMed] [Google Scholar]
- RADLOFF LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- SALTHOUSE TA. The processing-speed theory of adult age differences in cognition. Psychol Rev. 1996;103:403–28. doi: 10.1037/0033-295x.103.3.403. [DOI] [PubMed] [Google Scholar]
- SAS 9.1.3 . Procedures Guide. SAS 9.1.3 ed. SAS Institute Inc; Cary, NC: 2006. [Google Scholar]
- SCHAGEN SB, HAMBURGER HL, MULLER MJ, BOOGERD W, VAN DAM FS. Neurophysiological evaluation of late effects of adjuvant high-dose chemotherapy on cognitive function. J Neurooncol. 2001;51:159–65. doi: 10.1023/a:1010635229762. [DOI] [PubMed] [Google Scholar]
- VERBRUGGE LM, JETTE AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- WATTERS JM, YAU JC, O'ROURKE K, TOMIAK E, GERTLER SZ. Functional status is well maintained in older women during adjuvant chemotherapy for breast cancer. Ann Oncol. 2003;14:1744–50. doi: 10.1093/annonc/mdg497. [DOI] [PubMed] [Google Scholar]
- WEFEL JS, LENZI R, THERIAULT RL, DAVIS RN, MEYERS CA. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer. 2004;100:2292–9. doi: 10.1002/cncr.20272. [DOI] [PubMed] [Google Scholar]
- WESCHLER D. Manual for the Wechsler Adult Intelligence Scale-Revised. The Psychological Corporation; NY: 1981. [Google Scholar]
- WILLIS SL, TENNSTEDT SL, MARSISKE M, BALL K, ELIAS J, KOEPKE KM, MORRIS JN, REBOK GW, UNVERZAGT FW, STODDARD AM, WRIGHT E. Long-term effects of cognitive training on everyday functional outcomes in older adults. Jama. 2006;296:2805–14. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WOLINSKY FD, UNVERZAGT FW, SMITH DM, JONES R, WRIGHT E, TENNSTEDT SL. The effects of the ACTIVE cognitive training trial on clinically relevant declines in health-related quality of life. J Gerontol B Psychol Sci Soc Sci. 2006;61:S281–7. doi: 10.1093/geronb/61.5.s281. [DOI] [PubMed] [Google Scholar]