Abstract
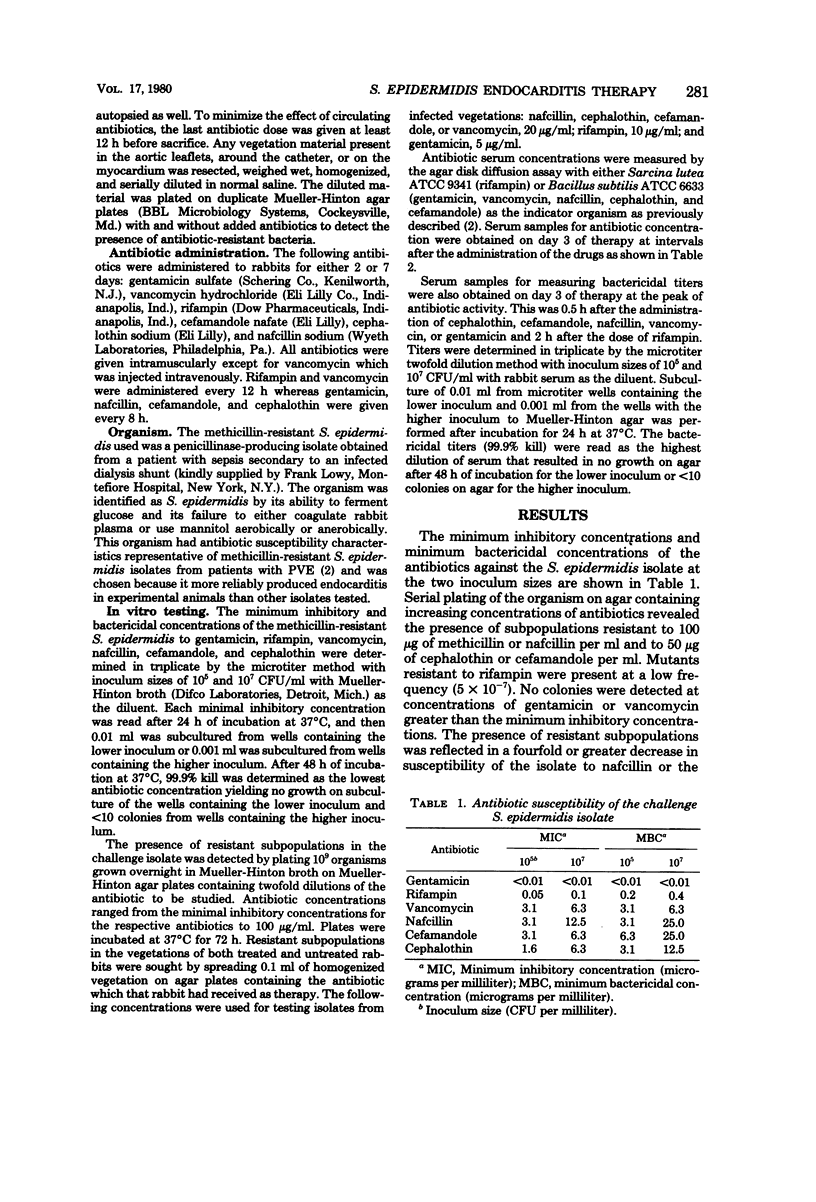
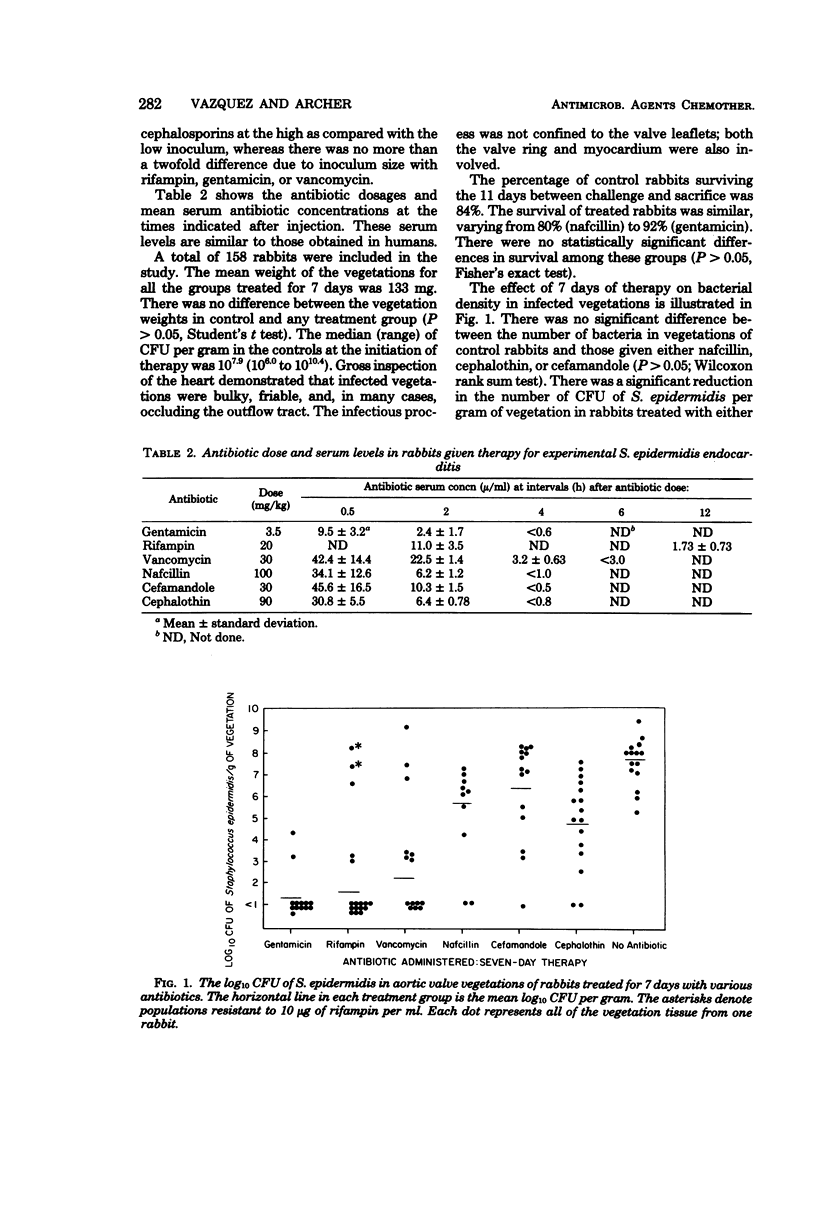
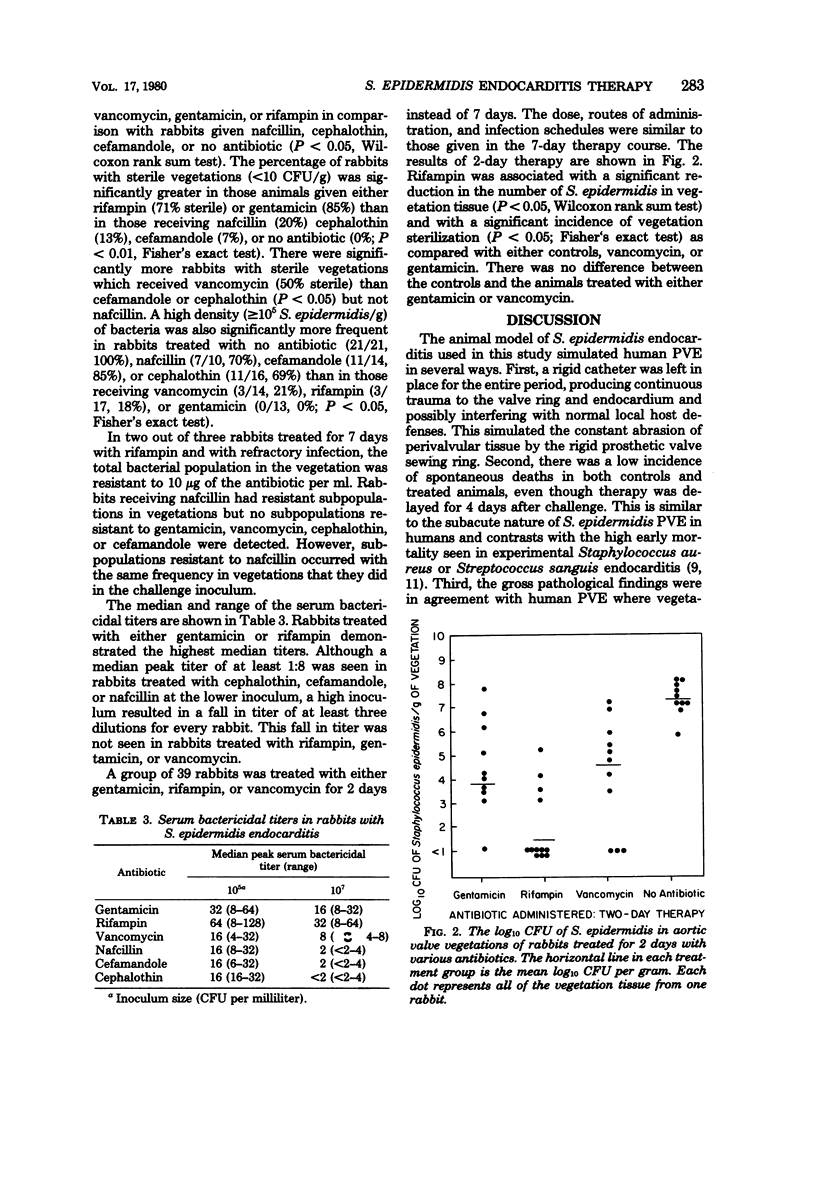
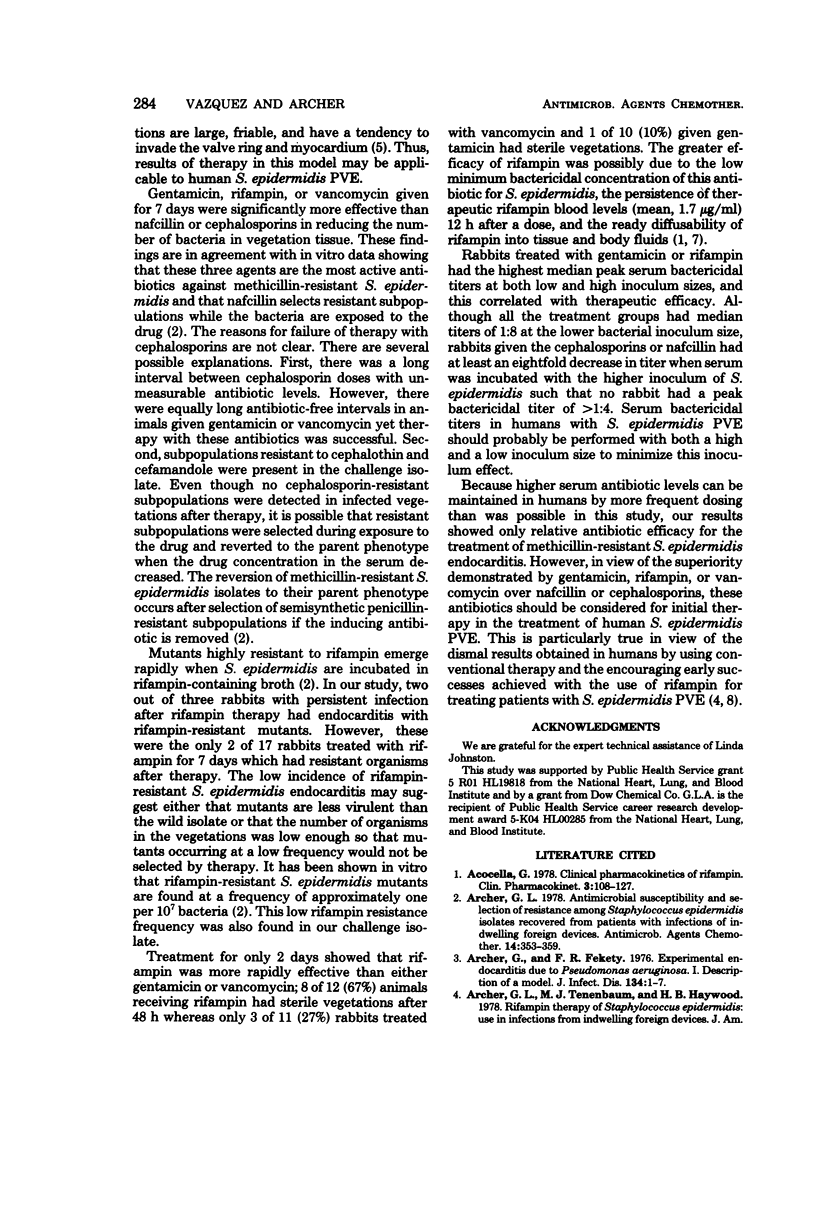
Endocarditis was produced in rabbits with a methicillin-resistant Staphylococcus epidermidis isolate. Subpopulations resistant to other semisynthetic penicillins and cephalosporins were detected in the isolate. Their presence was probably responsible for the increase in minimum bactericidal concentrations and minimum inhibitory concentrations when tests with high inocula, rather than low inocula were pursued. Rabbits were treated for either 2 or 7 days with nafcillin, cephalothin, cefamandole, vancomycin, rifampin, or gentamicin. Spontaneous death was uncommon in either controls (84% survival) or treated animals (80 to 94% survival). There was no significant difference in the number of bacteria in vegetations of rabbits treated for 7 days with cephalothin, cefamandole, nafcillin, or no antibiotic (control). There was a significant reduction in total bacteria in vegetations of rabbits given vancomycin, gentamicin, or rifampin for 7 days as compared with cephalothin, cefamandole, nafcillin or control. Gentamicin or rifampin sterilized significantly more vegetations after 7 days than cephalothin, cefamandole, nafcillin, or control; rifampin was more effective in sterilizing vegetations than either gentamycin or vancomycin after 2 days. Mutants resistant to 10 μg of rifampin per ml comprised the total bacterial population cultured from vegetations of 2 of 17 rabbits treated with this antibiotic for 7 days; there was no change in the susceptibility of vegetation isolates to other antibiotics. Rifampin, vancomycin, or gentamicin may prove to be more effective in humans than cephalosporins or semisynthetic penicillins in the treatment of methicillin-resistant S. epidermidis endocarditis.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Acocella G. Clinical pharmacokinetics of rifampicin. Clin Pharmacokinet. 1978 Mar-Apr;3(2):108–127. doi: 10.2165/00003088-197803020-00002. [DOI] [PubMed] [Google Scholar]
- Archer G. L. Antimicrobial susceptibility and selection of resistance among Staphylococcus epidermidis isolates recovered from patients with infections of indwelling foreign devices. Antimicrob Agents Chemother. 1978 Sep;14(3):353–359. doi: 10.1128/aac.14.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archer G. L., Tenenbaum M. J., Haywood H. B., 3rd Rifampin therapy of Staphylococcus epidermidis. Use in infections from indwelling artificial devices. JAMA. 1978 Aug 25;240(8):751–753. [PubMed] [Google Scholar]
- Archer G., Fekety F. R. Experimental endocarditis due to Pseudomonas aeruginosa. I. Description of a model. J Infect Dis. 1976 Jul;134(1):1–7. doi: 10.1093/infdis/134.1.1. [DOI] [PubMed] [Google Scholar]
- Arnett E. N., Roberts W. C. Prosthetic valve endocarditis: clinicopathologic analysis of 22 necropsy patients with comparison observations in 74 necropsy patients with active infective endocarditis involving natural left-sided cardiac valves. Am J Cardiol. 1976 Sep;38(3):281–292. doi: 10.1016/0002-9149(76)90169-7. [DOI] [PubMed] [Google Scholar]
- D'Oliveira J. J. Cerebrospinal fluid concentrations of rifampin in meningeal tuberculosis. Am Rev Respir Dis. 1972 Sep;106(3):432–437. doi: 10.1164/arrd.1972.106.3.432. [DOI] [PubMed] [Google Scholar]
- Dismukes W. E., Karchmer A. W., Buckley M. J., Austen W. G., Swartz M. N. Prosthetic valve endocarditis. Analysis of 38 cases. Circulation. 1973 Aug;48(2):365–377. doi: 10.1161/01.cir.48.2.365. [DOI] [PubMed] [Google Scholar]
- Massanari R. M., Donta S. T. The efficacy of rifampin as adjunctive therapy in selected cases of staphylococcal endocarditis. Chest. 1978 Mar;73(3):371–375. doi: 10.1378/chest.73.3.371. [DOI] [PubMed] [Google Scholar]
- Pelletier L. L., Jr, Petersdorf R. G., Nielson K. Chemotherapy of experimental streptococcal endocarditis. V. Effect of duration of infection and retained intracardiac catheter on response to treatment. J Lab Clin Med. 1976 Apr;87(4):692–702. [PubMed] [Google Scholar]
- Richardson J. V., Karp R. B., Kirklin J. W., Dismukes W. E. Treatment of infective endocarditis: a 10-year comparative analysis. Circulation. 1978 Oct;58(4):589–597. doi: 10.1161/01.cir.58.4.589. [DOI] [PubMed] [Google Scholar]
- Sande M. A., Johnson M. L. Antimicrobial therapy of experimental endocarditis caused by Staphylococcus aureus. J Infect Dis. 1975 Apr;131(4):367–375. doi: 10.1093/infdis/131.4.367. [DOI] [PubMed] [Google Scholar]
- Slaughter L., Morris J. E., Starr A. Prosthetic valvular endocarditis. A 12-year review. Circulation. 1973 Jun;47(6):1319–1326. doi: 10.1161/01.cir.47.6.1319. [DOI] [PubMed] [Google Scholar]


