Abstract
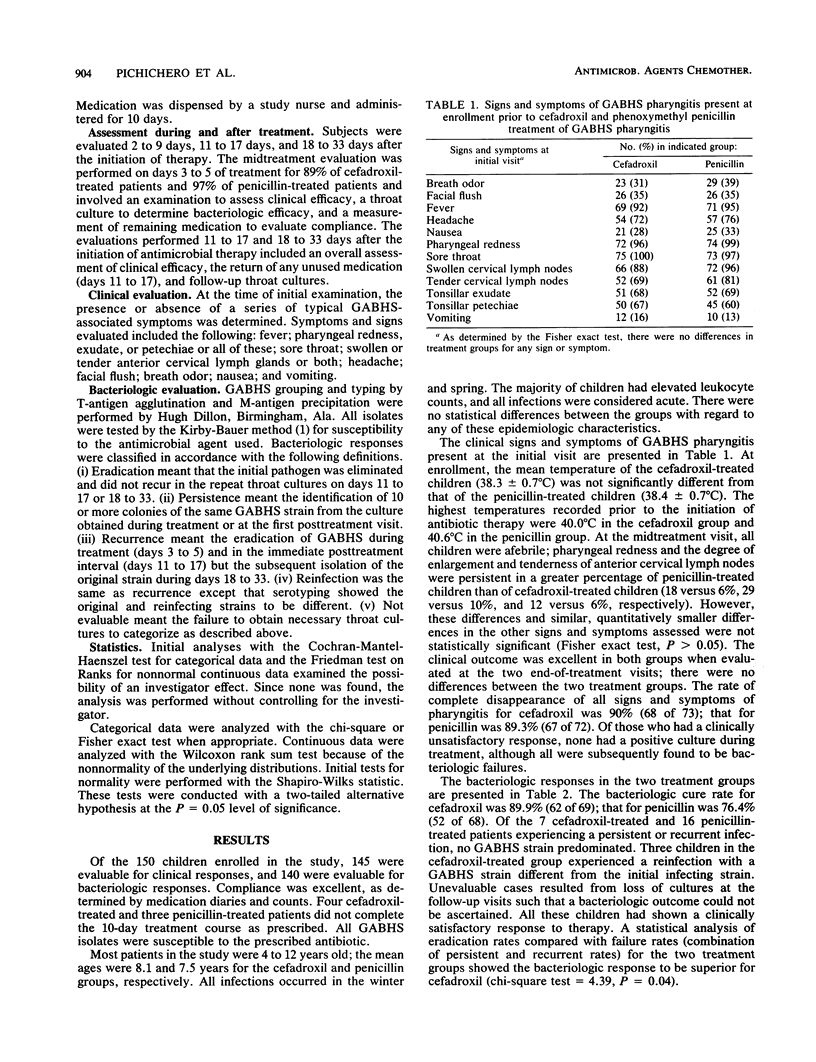
A total of 150 children from two pediatric practices with clinical and bacteriologic evidence of acute group A beta-hemolytic streptococcal (GABHS) pharyngitis randomly received cefadroxil monohydrate (75 children) or phenoxymethyl penicillin (75 children). Cefadroxil was given once daily, while penicillin was given three times daily. The treatment groups were similar in age, sex, race, illness severity, and acute GABHS symptomatology. Throat cultures were routine 3 to 5 days after the start of therapy and 2 and 14 days after the end of therapy. The bacterial cure rates were 90% (62 of 69) for cefadroxil-treated patients and 76% (52 of 68) for penicillin-treated patients. This difference was significant (P less than 0.04). The clinical response was satisfactory in 91% of cefadroxil-treated patients and 89% of penicillin-treated patients. We conclude that once-daily cefadroxil is at least as effective as three-times-daily penicillin in producing bacteriologic eradication and clinical symptomatic improvement in children with GABHS pharyngitis.
Full text
PDF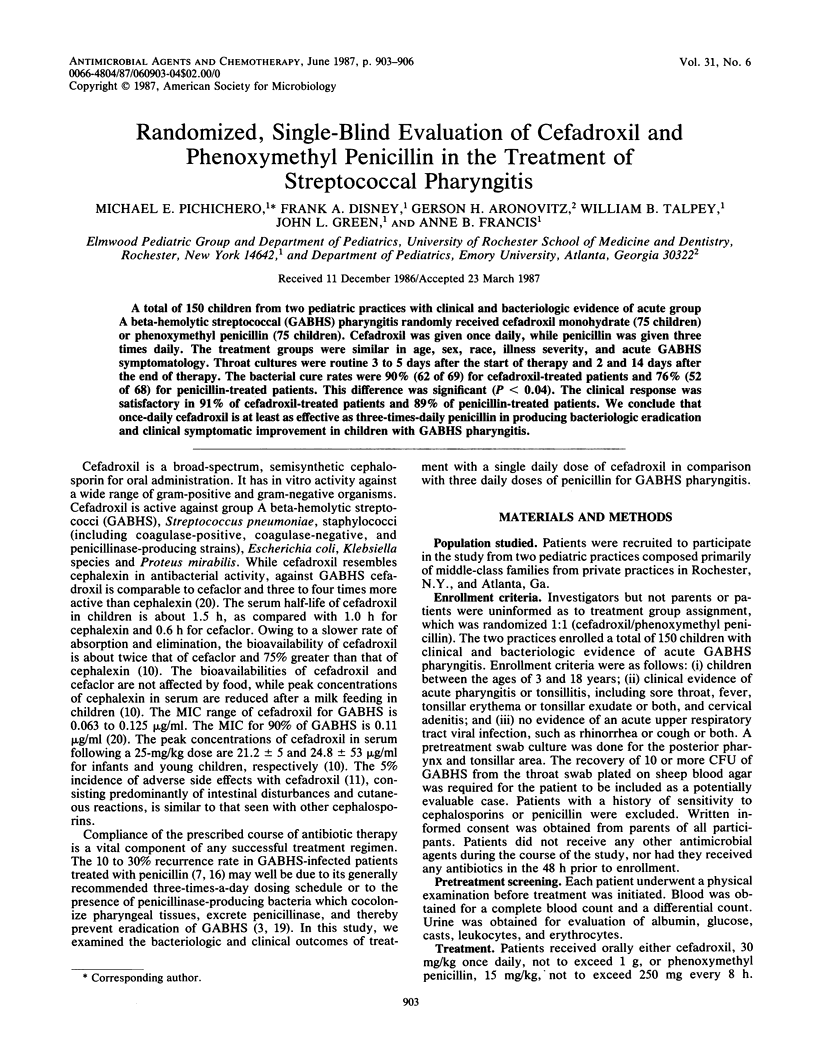
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BREESE B. B., DISNEY F. A., TALPEY W. B. The prevention of type specific immunity to streptococcal infections due to the therapeutic use of penicillin. Occurrence of second attacks due to the same type of group A hemolytic streptococci. Am J Dis Child. 1960 Sep;100:353–359. doi: 10.1001/archpedi.1960.04020040355007. [DOI] [PubMed] [Google Scholar]
- Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966 Apr;45(4):493–496. [PubMed] [Google Scholar]
- Brook I., Pazzaglia G., Coolbaugh J. C., Walker R. I. In-vivo protection of group A beta-haemolytic streptococci from penicillin by beta-lactamase-producing Bacteroides species. J Antimicrob Chemother. 1983 Dec;12(6):599–606. doi: 10.1093/jac/12.6.599. [DOI] [PubMed] [Google Scholar]
- Disney F. A., Breese B. B., Francis A. B., Green J. L., Talpey W. B. The use of cefaclor in the treatment of beta-haemolytic streptococcal throat infections in children. Postgrad Med J. 1979;55 (Suppl 4):50–52. [PubMed] [Google Scholar]
- Disney F. A., Breese B. B., Green J. L., Talpey W. B., Tobin J. R. Cephalexin and penicillin therapy of childhood beta-hemolytic streptococcal infections. Postgrad Med J. 1971 Feb;47(Suppl):47–51. [PubMed] [Google Scholar]
- Gastanaduy A. S., Kaplan E. L., Huwe B. B., McKay C., Wannamaker L. W. Failure of penicillin to eradicate group A streptococci during an outbreak of pharyngitis. Lancet. 1980 Sep 6;2(8193):498–502. doi: 10.1016/s0140-6736(80)91832-2. [DOI] [PubMed] [Google Scholar]
- Gau D. W., Horn R. F., Solomon R. M., Johnson P., Leigh D. A. Streptococcal tonsillitis in general practice. A comparison of cephalexin and penicillin therapy. Practitioner. 1972 Feb;208(244):276–281. [PubMed] [Google Scholar]
- Gerber M. A., Randolph M. F., Chanatry J., Wright L. L., Anderson L. R., Kaplan E. L. Once daily therapy for streptococcal pharyngitis with cefadroxil. J Pediatr. 1986 Sep;109(3):531–537. doi: 10.1016/s0022-3476(86)80139-1. [DOI] [PubMed] [Google Scholar]
- Ginsburg C. M. Comparative pharmacokinetics of cefadroxil, cefaclor, cephalexin and cephradine in infants and children. J Antimicrob Chemother. 1982 Sep;10 (Suppl B):27–31. doi: 10.1093/jac/10.suppl_b.27. [DOI] [PubMed] [Google Scholar]
- Ginsburg C. M., McCracken G. H., Jr, Clahsen J. C., Thomas M. L. Clinical pharmacology of cefadroxil in infants and children. Antimicrob Agents Chemother. 1978 May;13(5):845–848. doi: 10.1128/aac.13.5.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg C. M., McCracken G. H., Jr, Crow S. D., Steinberg J. B., Cope F. A controlled comparative study of penicillin V and cefadroxil therapy of group A streptococcal tonsillopharyngitis. J Int Med Res. 1980;8(Suppl 1):82–86. [PubMed] [Google Scholar]
- Ginsburg C. M., McCracken G. H., Jr, Steinberg J. B., Crow S. D., Dildy B. F., Cope F., Zweighaft T. Treatment of Group A streptococcal pharyngitis in children. Results of a prospective, randomized study of four antimicrobial agents. Clin Pediatr (Phila) 1982 Feb;21(2):83–88. doi: 10.1177/000992288202100203. [DOI] [PubMed] [Google Scholar]
- Ginsburg C. M., McCracken G. H., Petruska M. Once-daily cefadroxil versus twice-daily cefaclor for treatment of acute urinary tract infections in children. J Antimicrob Chemother. 1982 Sep;10 (Suppl B):53–56. doi: 10.1093/jac/10.suppl_b.53. [DOI] [PubMed] [Google Scholar]
- Henness D. M. A clinical experience with cefadroxil in upper respiratory tract infection. J Antimicrob Chemother. 1982 Sep;10 (Suppl B):125–135. doi: 10.1093/jac/10.suppl_b.125. [DOI] [PubMed] [Google Scholar]
- Howie V. M., Ploussard J. H. Treatment of group A streptococcal pharyngitis in children. Comparison of lincomycin and penicillin G given orally and benzathine penicillin G given intramuscularly. Am J Dis Child. 1971 Jun;121(6):477–480. doi: 10.1001/archpedi.1971.02100170059005. [DOI] [PubMed] [Google Scholar]
- KUNDSIN R. B., MILLER J. M. SIGNIFICANCE OF THE STAPHYLOCOCCUS AUREUS CARRIER STATE IN THE TREATMENT OF DISEASE DUE TO GROUP A STREPTOCOCCI. N Engl J Med. 1964 Dec 31;271:1395–1397. doi: 10.1056/NEJM196412312712705. [DOI] [PubMed] [Google Scholar]
- Kaplan E. L., Top F. H., Jr, Dudding B. A., Wannamaker L. W. Diagnosis of streptococcal pharyngitis: differentiation of active infection from the carrier state in the symptomatic child. J Infect Dis. 1971 May;123(5):490–501. doi: 10.1093/infdis/123.5.490. [DOI] [PubMed] [Google Scholar]
- Kim K. S., Kaplan E. L. Association of penicillin tolerance with failure to eradicate group A streptococci from patients with pharyngitis. J Pediatr. 1985 Nov;107(5):681–684. doi: 10.1016/s0022-3476(85)80392-9. [DOI] [PubMed] [Google Scholar]
- Leitner F., McGregor M. C., Pursiano T. A. Comparative antibacterial spectrum of cefadroxil. J Antimicrob Chemother. 1982 Sep;10 (Suppl B):1–9. doi: 10.1093/jac/10.suppl_b.1. [DOI] [PubMed] [Google Scholar]
- Malaka-Zafiriu K., Papadopoulos F., Augoustidousavvopoulou P., Papachristos F., Cassimos C. Oral once-daily cefadroxil compared with ampicillin in the treatment of urinary tract infection in children. J Antimicrob Chemother. 1982 Sep;10 (Suppl B):47–51. doi: 10.1093/jac/10.suppl_b.47. [DOI] [PubMed] [Google Scholar]
- Matsen J. M., Torstenson O., Siegel S. E., Bacaner H. Use of available dosage forms of cephalexin in clinical comparison with phenoxymethyl penicillin and benzathine penicillin in the treatment of streptococcal pharyngitis in children. Antimicrob Agents Chemother. 1974 Oct;6(4):501–506. doi: 10.1128/aac.6.4.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinovitch M., MacKenzie R., Brazeau M., Marks M. I. Treatment of streptococcal pharyngitis. I. Clinical evaluation. Can Med Assoc J. 1973 May 19;108(10):1271–1274. [PMC free article] [PubMed] [Google Scholar]
- Stillerman M., Aronovitz G. H., Durnell M. D., Rosenberg R. Comparison between cephalexin two- and four-time per day regimens in group A streptococcal pharyngitis. Clin Pediatr (Phila) 1984 Jun;23(6):348–351. doi: 10.1177/000992288402300610. [DOI] [PubMed] [Google Scholar]
- Stillerman M. Comparison of cephaloglycin and penicillin in streptococcal pharyngitis. Clin Pharmacol Ther. 1970 Mar-Apr;11(2):205–213. doi: 10.1002/cpt1970112205. [DOI] [PubMed] [Google Scholar]
- Stillerman M., Isenberg H. D., Moody M. Streptococcal pharyngitis therapy. Comparison of cephalexin, phenoxymethyl penicillin, and ampicillin. Am J Dis Child. 1972 May;123(5):457–461. doi: 10.1001/archpedi.1972.02110110085005. [DOI] [PubMed] [Google Scholar]


