Abstract
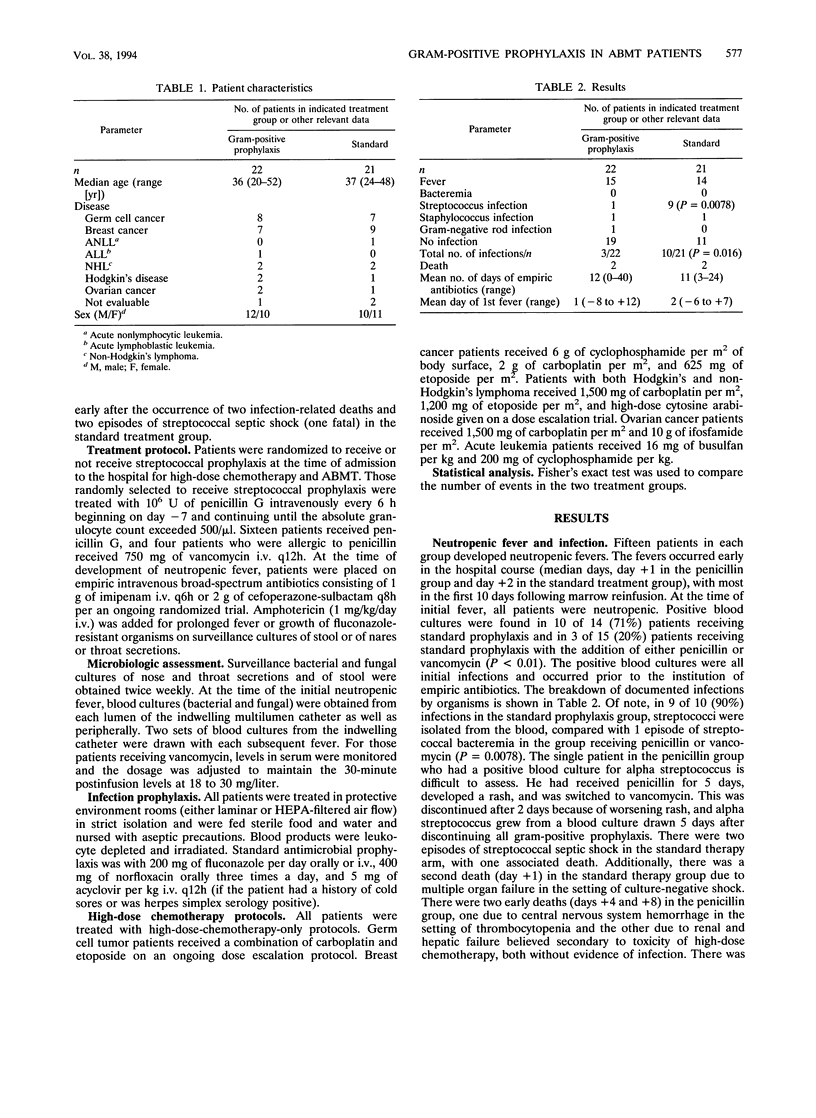
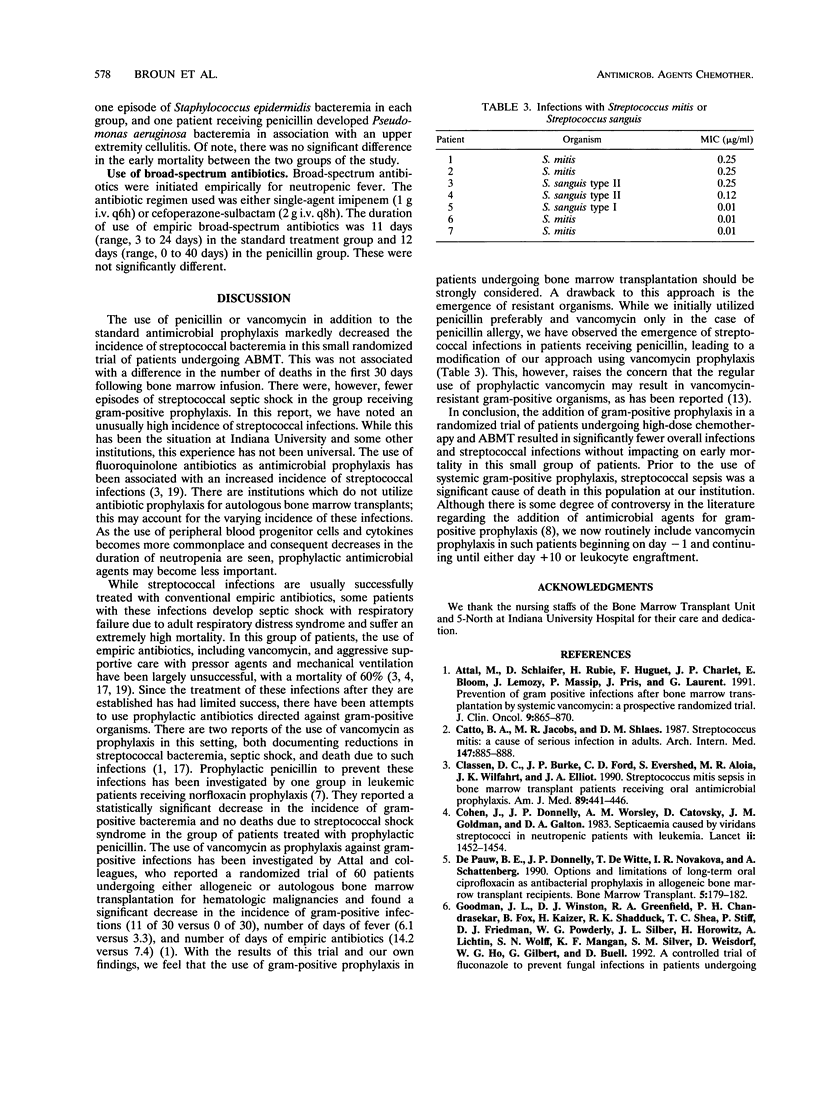
The purpose of the study reported here was to investigate the impact of prophylaxis against gram-positive infections in patients undergoing high-dose chemotherapy and autologous bone marrow transplantation in a randomized trial. Forty-three patients undergoing high-dose chemotherapy with autologous bone marrow transplant were enrolled in a nonblinded randomized trial to receive or not to receive prophylaxis for gram-positive infections with 10(6) U of penicillin intravenously (i.v.) every 6 h (q6h) (if penicillin allergic, 750 mg of vancomycin i.v. q12h) in addition to standard antimicrobial prophylaxis with 400 mg of norfloxacin orally three times a day, 200 mg of fluconazole orally once a day, and 5 mg of acyclovir per kg of body weight i.v. q12h. The patients were being treated for germ cell cancer (n = 15), breast cancer (n = 16), Hodgkin's disease (n = 3), non-Hodgkin's lymphoma (n = 4), acute myeloid leukemia (n = 1), acute lymphoblastic leukemia (n = 1), and ovarian cancer (n = 3). The trial was stopped because of excess morbidity in the form of streptococcal septic shock in the group not receiving gram-positive prophylaxis. There were significantly fewer overall infections (10 versus 3; P = 0.016) and streptococcal infections (9 versus 1; P = 0.0078) in the group receiving gram-positive prophylaxis. There were no significant differences in the numbers of deaths, duration of broad-spectrum antibiotics, or incidence of neutropenic fever between the two groups. Prophylaxis for gram-positive infections with penicillin or vancomycin is effective in reducing the incidence of streptococcal infections in patients undergoing high-dose chemotherapy and autologous bone marrow transplant. However, this approach may carry a risk of fostering resistance among streptococci to penicillin or vancomycin.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Attal M., Schlaifer D., Rubie H., Huguet F., Charlet J. P., Bloom E., Lemozy J., Massip P., Pris J., Laurent G. Prevention of gram-positive infections after bone marrow transplantation by systemic vancomycin: a prospective, randomized trial. J Clin Oncol. 1991 May;9(5):865–870. doi: 10.1200/JCO.1991.9.5.865. [DOI] [PubMed] [Google Scholar]
- Catto B. A., Jacobs M. R., Shlaes D. M. Streptococcus mitis. A cause of serious infection in adults. Arch Intern Med. 1987 May;147(5):885–888. doi: 10.1001/archinte.147.5.885. [DOI] [PubMed] [Google Scholar]
- Classen D. C., Burke J. P., Ford C. D., Evershed S., Aloia M. R., Wilfahrt J. K., Elliott J. A. Streptococcus mitis sepsis in bone marrow transplant patients receiving oral antimicrobial prophylaxis. Am J Med. 1990 Oct;89(4):441–446. doi: 10.1016/0002-9343(90)90373-l. [DOI] [PubMed] [Google Scholar]
- Cohen J., Donnelly J. P., Worsley A. M., Catovsky D., Goldman J. M., Galton D. A. Septicaemia caused by viridans streptococci in neutropenic patients with leukaemia. Lancet. 1983 Dec 24;2(8365-66):1452–1454. doi: 10.1016/s0140-6736(83)90799-7. [DOI] [PubMed] [Google Scholar]
- De Pauw B. E., Donnelly J. P., De Witte T., Nováková I. R., Schattenberg A. Options and limitations of long-term oral ciprofloxacin as antibacterial prophylaxis in allogeneic bone marrow transplant recipients. Bone Marrow Transplant. 1990 Mar;5(3):179–182. [PubMed] [Google Scholar]
- Goodman J. L., Winston D. J., Greenfield R. A., Chandrasekar P. H., Fox B., Kaizer H., Shadduck R. K., Shea T. C., Stiff P., Friedman D. J. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med. 1992 Mar 26;326(13):845–851. doi: 10.1056/NEJM199203263261301. [DOI] [PubMed] [Google Scholar]
- Guiot H. F., Peters W. G., van den Broek P. J., van der Meer J. W., Kramps J. A., Willemze R., van Furth R. Respiratory failure elicited by streptococcal septicaemia in patients treated with cytosine arabinoside, and its prevention by penicillin. Infection. 1990 May-Jun;18(3):131–137. doi: 10.1007/BF01642100. [DOI] [PubMed] [Google Scholar]
- Guiot H. F., van der Meer J. W., van den Broek P. J., Willemze R., van Furth R. Prevention of viridans-group streptococcal septicemia in oncohematologic patients: a controlled comparative study on the effect of penicillin G and cotrimoxazole. Ann Hematol. 1992 Jun;64(6):260–265. doi: 10.1007/BF01695467. [DOI] [PubMed] [Google Scholar]
- Heimdahl A., Mattsson T., Dahllöf G., Lönnquist B., Ringdén O. The oral cavity as a port of entry for early infections in patients treated with bone marrow transplantation. Oral Surg Oral Med Oral Pathol. 1989 Dec;68(6):711–716. doi: 10.1016/0030-4220(89)90160-6. [DOI] [PubMed] [Google Scholar]
- Jones P. G., Kauffman C. A., McAuliffe L. S., Liepman M. K., Bergman A. G. Efficacy of ketoconazole v nystatin in prevention of fungal infections in neutropenic patients. Arch Intern Med. 1984 Mar;144(3):549–551. [PubMed] [Google Scholar]
- Karp J. E., Merz W. G., Hendricksen C., Laughon B., Redden T., Bamberger B. J., Bartlett J. G., Saral R., Burke P. J. Oral norfloxacin for prevention of gram-negative bacterial infections in patients with acute leukemia and granulocytopenia. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1987 Jan;106(1):1–7. doi: 10.7326/0003-4819-106-1-1. [DOI] [PubMed] [Google Scholar]
- Menichetti F., Felicini R., Bucaneve G., Aversa F., Greco M., Pasquarella C., Moretti M. V., Del Favero A., Martelli M. F. Norfloxacin prophylaxis for neutropenic patients undergoing bone marrow transplantation. Bone Marrow Transplant. 1989 Sep;4(5):489–492. [PubMed] [Google Scholar]
- Peetermans W. E., Sebens F. W., Guiot H. F. Vancomycin-resistant Enterococcus faecalis in a bone-marrow transplant recipient. Scand J Infect Dis. 1991;23(1):105–109. doi: 10.3109/00365549109023382. [DOI] [PubMed] [Google Scholar]
- Pizzo P. A., Ladisch S., Simon R. M., Gill F., Levine A. S. Increasing incidence of Gram-positive sepsis in cancer patients. Med Pediatr Oncol. 1978;5(1):241–244. doi: 10.1002/mpo.2950050133. [DOI] [PubMed] [Google Scholar]
- Pizzo P. A., Ladisch S., Witebsky F. G. Alpha-hemolytic streptococci: clinical significance in the cancer patient. Med Pediatr Oncol. 1978;4(4):367–370. doi: 10.1002/mpo.2950040414. [DOI] [PubMed] [Google Scholar]
- Saral R., Burns W. H., Laskin O. L., Santos G. W., Lietman P. S. Acyclovir prophylaxis of herpes-simplex-virus infections. N Engl J Med. 1981 Jul 9;305(2):63–67. doi: 10.1056/NEJM198107093050202. [DOI] [PubMed] [Google Scholar]
- Valteau D., Hartmann O., Brugieres L., Vassal G., Benhamou E., Andremont A., Kalifa C., Lemerle J. Streptococcal septicaemia following autologous bone marrow transplantation in children treated with high-dose chemotherapy. Bone Marrow Transplant. 1991 Jun;7(6):415–419. [PubMed] [Google Scholar]
- Villablanca J. G., Steiner M., Kersey J., Ramsay N. K., Ferrieri P., Haake R., Weisdorf D. The clinical spectrum of infections with viridans streptococci in bone marrow transplant patients. Bone Marrow Transplant. 1990 Jun;5(6):387–393. [PubMed] [Google Scholar]
- Wade J. C., Schimpff S. C., Newman K. A., Wiernik P. H. Staphylococcus epidermidis: an increasing cause of infection in patients with granulocytopenia. Ann Intern Med. 1982 Oct;97(4):503–508. doi: 10.7326/0003-4819-97-4-503. [DOI] [PubMed] [Google Scholar]
- Winston D. J., Ho W. G., Nakao S. L., Gale R. P., Champlin R. E. Norfloxacin versus vancomycin/polymyxin for prevention of infections in granulocytopenic patients. Am J Med. 1986 May;80(5):884–890. doi: 10.1016/0002-9343(86)90633-9. [DOI] [PubMed] [Google Scholar]


