Abstract
A wealth of evidence attests to the extensive current and lifetime diagnostic comorbidity of the DSM-IV anxiety and mood disorders. Research has shown that the considerable cross-sectional covariation of DSM-IV emotional disorders is accounted for by common higher-order dimensions such as neuroticism/behavioral inhibition (N/BI) and low positive affect/behavioral activation. Longitudinal studies have indicated that the temporal covariation of these disorders can be explained by changes in N/BI and in some cases, initial levels of N/BI are predictive of the temporal course of emotional disorders. Moreover, the marked phenotypal overlap of the DSM-IV anxiety and mood disorder constructs is a frequent source of diagnostic unreliability (e.g., temporal overlap in the shared features of generalized anxiety disorder and mood disorders, situation specificity of panic attacks in panic disorder and specific phobia). Although dimensional approaches have been considered as a method to address the drawbacks associated with the extant prototypical nosology (e.g., inadequate assessment of individual differences in disorder severity), these proposals do not reconcile key problems in current classification such as modest reliability and high comorbidity. The current paper considers an alternative approach that emphasizes empirically supported common dimensions of emotional disorders over disorder-specific criteria sets. The selection and assessment of these dimensions are discussed along with how these methods could be implemented to promote more reliable and valid diagnosis, prognosis, and treatment planning. For instance, the advantages of this classification system are discussed in context of current transdiagnostic treatment protocols that are efficaciously applied to a variety of disorders by targeting their shared features.
Keywords: Diagnostic classification of emotional disorders, categorical vs. dimensional assessment of psychopathology, temperament and psychopathology of emotional disorders, comorbidity of anxiety and mood disorders, Diagnostic and Statistical Manual of Mental Disorders
Researchers have long recognized the limitations associated with the predominately categorical approach to diagnostic classification that has been adopted in the various editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM). Although the development of the fifth edition of the DSM is well underway (DSM-V), no well-defined alternative nosological systems have been articulated to address these limitations. After providing an overview of the drawbacks inherent to the current DSM system, this paper will outline alternative approaches to diagnostic classification ranging from systems that incorporate dimensional elements into the extant diagnostic categories to systems that place greater emphasis on empirically supported common dimensions over disorder-specific criteria sets. The selection and operationalization of these dimensions will be discussed with emphasis on how these methods might be implemented to promote more reliable and valid clinical assessment, prognosis, treatment planning, and outcome evaluation.
Limitations to the Current DSM System
Diagnostic reliability
Our nosological systems for mental disorders have moved from vague, ill-defined concepts reflecting hypothetical etiological constructs (DSM-II) to an atheoretical precise set of criteria based on presenting clinical features rather than assumptions about etiology (Brown & Barlow, 2002). This extreme “splitting” approach, present from DSM-III until now, was a necessary intermediate step in our clinical science; that is, becoming familiar with and defining more carefully the specific psychopathological phenomena comprising anxiety and mood disorders was essential to building an adequate nosological system. Indeed, diagnostic reliability studies of the DSM-III-R and DSM-IV disorders have indicated that this endeavor has been largely successful, reflected by the fact that most anxiety and mood disorder categories are associated with favorable reliability (e.g., Brown, Di Nardo, Lehman, & Campbell, 2001; Di Nardo et al., 1993; Mannuzza et al., 1989; Williams et al., 1992). For instance, in our investigation of the diagnostic reliability of current and lifetime DSM-IV anxiety and mood disorders (Brown et al., 2001), 362 outpatients underwent two, independent administrations of the Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994). All DSM-IV principal and lifetime diagnostic categories evidenced good to excellent reliability with the exception of dysthymia (DYS) and posttraumatic stress disorder (PTSD). Moreover, excellent reliability was obtained for each of the specific phobia (SPEC) types introduced in DSM-IV. In comparison to our reliability study of DSM-III-R disorders (Di Nardo et al., 1993), improved reliability was noted for the majority of DSM-IV categories, and no DSM-IV category was associated with a markedly lower reliability estimate. Diagnoses showing the most improvement were panic disorder (PD) and generalized anxiety disorder (GAD). The improvement in GAD was encouraging because this category was in jeopardy of being removed from DSM-IV, in part due to evidence of poor to fair reliability in DSM-III-R (cf. Brown, Barlow, & Leibowitz, 1994).
Although reliability estimates are generally favorable, limitations of the current classification system are evident when examining the sources of diagnostic disagreements. Brown et al. (2001) recorded the primary source of unreliability for each diagnostic disagreement using the following rating system: (a) difference in report – patient gives different information to the two interviewers (e.g., variability in responses to inquiry about the presence, severity, or duration of key symptoms); (b) threshold – consistent symptom report is provided across interviews, but interviewers disagree on whether these symptoms cause sufficient interference and distress to satisfy the DSM-IV threshold for a clinical disorder; (c) change in clinical status – clear change in the severity or presence of symptoms between interviews; (d) interviewer error – interviewer improperly applies DSM-IV diagnostic or exclusion rules or fails to obtain necessary diagnostic information during ADIS-IV-L administration (e.g., skips out of an ADIS-IV-L diagnostic section prematurely); (e) diagnosis subsumed under another condition – disagreement on whether symptoms are attributable to, or better accounted for by, a co-occurring disorder; and (f) DSM-IV inclarity – disagreement stems from limitations of the DSM-IV criteria in providing clear direction for differential diagnosis.
As seen in Table 1, the prevailing sources of unreliability differed substantially across the DSM-IV anxiety and mood disorders. For instance, the majority of disagreements involving social phobia (SOC), SPEC, and obsessive-compulsive disorder (OCD; 62% to 67%) entailed cases where one interviewer assigned the diagnosis at a clinical level, and the other rated the diagnosis as subclinical; for other categories (e.g., panic disorder with agoraphobia [PDA], GAD, major depressive disorder [MDD], DYS), “threshold” disagreements were a relatively rare source of unreliability. “Difference in patient report” was otherwise the most prevalent source of unreliability, although with wide-ranging frequency across the anxiety and mood disorders (i.e., from 22% in SPEC to 100% in PTSD). Considerable variability was also evident across categories for the frequency with which other disorders were involved in diagnostic disagreements. Whereas disagreements with other disorders were relatively uncommon for SOC, OCD, and PTSD (8% to 13%), another clinical diagnosis was involved in over half of the disagreements with DYS, PDA, MDD, and GAD (54% to 74%). As shown in Table 1, disagreements with another clinical diagnosis often involved disorders with overlapping definitional features, and that differed mainly in the duration or severity of symptoms (e.g., PD vs PDA; SPEC vs agoraphobia without a history of panic disorder; MDD vs DYS). Consistent with prior evidence that mood disorders may pose the greatest boundary problem for GAD (cf. Brown et al., 1994), 63% of the GAD disagreements with another diagnosis involved the mood disorders (DYS = 10, MDD = 9, depressive disorder NOS = 2, bipolar = 1). In addition, this overlap was evident in disagreements with anxiety disorder NOS and depressive disorder NOS diagnoses. For example, a category frequently involved in disagreements with GAD was anxiety disorder NOS, where one interviewer noted clinically significant features of GAD, but judged that all criteria for a formal DSM-IV GAD diagnosis had not been met (e.g., number or duration of worries or associated symptoms). This was also the case for the NOS diagnoses associated with disagreements in other disorders [e.g., in the two OCD disagreements involving another disorder, both were with anxiety NOS (OCD)].
Table 1.
Sources of Diagnostic Disagreements for Current DSM-IV Anxiety and Mood Disorders
| Diagnosis: | PD | PDA | SPEC | SOC | GAD | OCD | PTSD | MDD | DYS |
|---|---|---|---|---|---|---|---|---|---|
| Total Disagreements (n) | 13 | 26 | 37 | 39 | 47 | 21 | 8 | 53 | 41 |
| Proportion (and n) of: | |||||||||
| Disagreements Involving Another Clinical Diagnosis | |||||||||
| .38 (5) | .54 (14) | .27 (10) | .08 (3) | .74 (35) | .10 (2) | .13 (1) | .64 (34) | .71 (29) | |
| Disorders involved in the disagreement: | |||||||||
| PD | .15 (4) | -- | -- | .02 (1) | -- | -- | -- | -- | |
| PDA | .31 (4) | .08 (3) | -- | -- | -- | -- | -- | -- | |
| SPEC | -- | .19 (5) | -- | -- | -- | -- | -- | -- | |
| SOC | -- | -- | -- | -- | -- | -- | -- | -- | |
| GAD | -- | .04 (1) | .03 (1) | -- | -- | -- | .04 (2) | .15 (6) | |
| OCD | -- | -- | -- | -- | -- | -- | -- | -- | |
| PTSD | -- | .04 (1) | -- | -- | .02 (1) | -- | -- | -- | |
| MDD | -- | -- | -- | -- | .19 (9) | -- | -- | .39 (16) | |
| DYS | -- | -- | -- | -- | .21 (10) | -- | -- | .23 (12) | |
| Depression NOS | -- | -- | -- | -- | .04 (2) | -- | -- | .28 (15) | .12 (5) |
| Anxiety NOS | .08 (1) | .08 (2) | -- | .05 (2) | .21 (10) | .10 (2) | .13 (1) | .02 (1) | -- |
| AGw/oPD | -- | .04 (1) | .14 (5) | .03 (1) | -- | -- | -- | -- | -- |
| Adjustment Disorder | -- | -- | -- | -- | .02 (1) | -- | -- | .06 (3) | .02 (1) |
| Other | -- | -- | HYPOc | -- | BIP | -- | -- | PAIN | SOM |
| Clinical vs. Subclinical Disagreementsa | |||||||||
| .46 (6) | .12 (3) | .62 (23) | .67 (26) | .13 (6) | .62 (13) | .25 (2) | .17 (9) | -- | |
| Sources of Unreliability | |||||||||
| Thresholdb | .46 (6) | .12 (3) | .46 (17) | .41 (16) | .09 (4) | .29 (6) | -- | .15 (8) | .05 (2)d |
| Difference in patient report | .31 (4) | .50 (13) | .22 (8) | .36 (14) | .55 (26) | .48 (10) | 1.00 (8) | .55 (29) | .66 (27) |
| Interviewer error | .23 (3) | .19 (5) | .14 (5) | .10 (4) | .19 (9) | .14 (3) | -- | .11 (6) | .15 (6) |
| Diagnosis subsumed under comorbid disorder | -- | .15 (4) | .08 (3) | .10 (4) | .15 (7) | .10 (2) | -- | -- | .15 (6) |
| Change in clinical status | -- | .04 (1) | .03 (1) | -- | .02 (1) | -- | -- | .17 (9) | -- |
| DSM-IV inclarity | -- | -- | .05 (2) | .03 (1) | -- | -- | -- | -- | -- |
| Missing | -- | -- | .03 (1) | -- | -- | -- | -- | .02 (1) | -- |
Note. PD = panic disorder; PDA = panic disorder with agoraphobia; SPEC = specific phobia; SOC = social phobia; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder; PTSD = posttraumatic stress disorder; MDD = major depressive disorder; DYS = dysthymia; Depression NOS = depressive disorder not otherwise specified; Anxiety NOS = anxiety disorder not otherwise specified; AGw/oPD = agoraphobia without a history of panic disorder; HYPO = hypochondriasis; BIP = bipolar disorder; PAIN = pain disorder; SOM = somatization disorder.
Cases where both raters recorded the diagnosis, but disagreed on whether it should be assigned at the clinical level;
Note that, for SPEC and other diagnoses, the frequency of cases where “Threshold” was the primary source of unreliability does not necessarily equal the number of disagreements entailing assignment of the disorder at clinical and subclinical levels. This is because each of the other unreliability sources (e.g., change in clinical status, variability in patient report regarding number or severity of symptoms) could also result in clinical vs. subclinical disagreements;
This disagreement pertained to a boundary issue between specific phobia, other type (contracting an illness) and hypochondriasis;
In these 2 cases, disagreements stemmed from a threshold issue of MDD (chronic) vs. DYS; that is, whether the features were sufficiently severe to be classified as a chronic major depressive episode.
Table reproduced from Brown, T.A., Di Nardo, P.A., Lehman, C.L., & Campbell, L.A. (2001). Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110, 49–58.
Comorbidity
Consistent findings of high comorbidity among anxiety and mood disorders underscore the poor distinguishability of the emotional disorders (e.g., Andrews, 1990). Comorbidity studies based on DSM-III-R criteria routinely indicated that at least 50% of patients with a principal anxiety disorder have one or more additional diagnoses at the time of assessment (e.g., Brawman-Mintzer et al., 1993; Brown & Barlow, 1992; Sanderson et al., 1990). Similar findings were obtained in a study of outpatients (N = 1,127) diagnosed with DSM-IV anxiety and mood disorders (Brown et al., 2001). It is important to note that this study, like others, probably yielded conservative estimates of diagnostic co-occurrence due to limits in generalizability stemming from various exclusion criteria (e.g., cases with active suicidality were excluded), the outpatient setting, and so forth. Nevertheless, comorbidity rates for many categories were quite high. Results indicated that 55% of patients with a principal anxiety or mood disorder had at least one additional anxiety or depressive disorder at the time of the assessment (Table 2); this rate increased to 76% when lifetime diagnoses were considered. The principal diagnostic categories of PTSD, MDD, DYS, and GAD had the highest comorbidity rates, and SPEC, the lowest. Analyses examining patterns of covariation among current and lifetime disorders yielded many interesting findings. For example, significant relative risks were obtained for associations between SOC and the mood disorders (MDD, DYS). The differential aggregation of SOC and mood disorders was noteworthy in view of structural findings (Brown, 2007; Brown et al., 1998) indicating that, unlike other DSM-IV disorders, the latent DSM-IV factors of SOC and Depression (DEP) are influenced by the higher-order trait of low positive affect. Thus, the high diagnostic comorbidity between SOC and mood disorders may due to a shared vulnerability dimension such as low positive affect/behavioral activation (cf. Clark et al., 1994; Eley & Brown, 2009). Moreover, PTSD was associated with significantly increased risk of PDA. Temporal sequences analyses indicated that PDA rarely (28%) preceded PTSD. This association is noteworthy because PTSD and PDA are the only two emotional disorders characterized by high levels of autonomic arousal (Brown & McNiff, in press).
Table 2.
Percentage (and Relative Risk) of Current Additional Diagnoses in Patients with Current Principal Anxiety and Mood Disorders (N = 968)
|
DSM-IV Principal Diagnosis (n) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Current Additional Diagnosis | PD (36) | PDA (324) | PD/A (360) | SOC (186) | GAD (120) | OCD (77) | SPEC (110) | PTSD (13) | MDD (81) | DYS (21) | MDD/DYS (102) | Overalla |
| Any Axis I | 42 (.73) | 62 (1.14*) | 60 (1.09) | 46 (.78*) | 68 (1.24*) | 57 (1.01) | 34 (.56*) | 92 (1.64*) | 69 (1.25*) | 76 (1.36*) | 71 (1.28*) | 57 |
| Any anxiety/mood | 42 (.75) | 60 (1.16*) | 59 (1.12) | 45 (.79*) | 65 (1.21*) | 53 (.96) | 33 (.56*) | 92 (1.69*) | 68 (1.26*) | 76 (1.40*) | 70 (1.30*) | 55 |
| Any anxiety disorder | 36 (.84) | 47 (1.17*) | 46 (1.14) | 28 (.61*) | 52 (1.25*) | 39 (.91) | 27 (.61*) | 62 (1.45) | 64 (1.58*) | 57 (1.35) | 63 (1.56*) | 43 |
| Any mood disorder | 17 (.58) | 33 (1.28*) | 31 (1.19) | 29 (1.04) | 36 (1.32*) | 32 (1.17) | 10 (.34*) | 77 (2.79*) | 11 (.37*) | 38 (1.36) | 17 (.56*) | 28 |
| Anxiety Disorders | ||||||||||||
| PD | -- | -- | -- | 01 (.28) | 03 (3.25) | 01 (.86) | 00 (--) | 00 (--) | 04 (3.25) | 00 (--) | 03 (2.48) | 01 |
| PDA | -- | -- | -- | 03 (.24*) | 15 (2.09*) | 08 (.88) | 05 (.58) | 23 (2.75) | 15 (1.90*) | 14 (1.68) | 15 (1.96*) | 09 |
| PD or PDA | -- | -- | -- | 03 (.24*) | 18 (2.24*) | 09 (.88) | 05 (.49) | 23 (2.33) | 19 (2.08*) | 14 (1.42) | 18 (2.03*) | 10 |
| SOC | 08 (.37) | 15 (.58*) | 15 (.53*) | -- | 36 (2.33*) | 26 (1.21) | 09 (.38*) | 15 (.70) | 41 (2.07*) | 48 (2.25*) | 42 (2.24*) | 22 |
| GAD | 19 (1.59) | 16 (1.50*) | 16 (1.64*) | 13 (1.10) | -- | 12 (.93) | 05 (.40*) | 23 (1.87) | 05 (.37*) | 05 (.38) | 05 (.36*) | 13 |
| GAD: no hierarchy | 22 (.87) | 22 (.79) | 22 (.78*) | 21 (.78) | -- | 16 (.59) | 07 (.26*) | 38 (1.52) | 67 (3.16*) | 90 (3.80*) | 72 (3.73*) | 25 |
| OCD | 06 (.83) | 07 (1.12) | 07 (1.08) | 08 (1.29) | 04 (.59) | -- | 03 (.38) | 23 (3.62*) | 09 (1.35) | 05 (.71) | 08 (1.21) | 07 |
| SPEC | 08 (.65) | 15 (1.36) | 15 (1.28) | 08 (.58*) | 12 (.91) | 12 (.91) | 15b (1.17) | 15 (1.21) | 15 (1.18) | 10 (.75) | 14 (1.09) | 13 |
| PTSD | 00 (--) | 04 (2.30*) | 04 (1.95) | 03 (1.09) | 01 (.30) | 00 (--) | 00 (--) | -- | 06 (2.84*) | 00 (--) | 05 (2.20) | 03 |
| Other anxiety | 03 (.92) | 04 (1.86) | 04 (1.81) | 03 (1.10) | 01 (.25) | 03 (.86) | 03 (.90) | 00 (--) | 02 (.81) | 00 (--) | 02 (.63) | 03 |
| Mood Disorders | ||||||||||||
| MDD | 08 (.41) | 24 (1.41*) | 23 (1.28) | 14 (.66*) | 26 (1.39) | 22 (1.14) | 03 (.12*) | 69 (3.67*) | -- | 33 (1.73) | -- | 20 |
| DYS | 08 (.99) | 07 (.73) | 07 (.74) | 13 (1.75*) | 06 (.66) | 10 (1.26) | 04 (.40) | 23 (2.80*) | 11 (1.36) | -- | -- | 08 |
| Other mood | 03 (.74) | 03 (.87) | 03 (.84) | 05 (1.40) | 06 (1.71) | 04 (1.05) | 04 (.98) | 00 (--) | 00 (--) | 05 (1.29) | 01 (.24) | 04 |
| Other Disorders | ||||||||||||
| Somatoform | 00 (--) | 02 (.99) | 01 (.84) | 01 (.65) | 04 (3.53*) | 01 (.83) | 00 (--) | 00 (--) | 02 (1.68) | 00 (--) | 02 (1.31) | 02 |
| Other Axis I | 03 (.92) | 02 (.63) | 02 (.64) | 01 (.31) | 06 (2.25) | 06 (2.41) | 02 (.58) | 00 (--) | 06 (2.28) | 00 (--) | 05 (1.77) | 03 |
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (American Psychiatric Association, 1994); PD = panic disorder; PDA = panic disorder with agoraphobia; PD/A = panic disorder with or without agoraphobia; SOC = social phobia; GAD = generalized anxiety disorder; GAD: no hierarchy = generalized anxiety disorder ignoring DSM-IV hierarchy rule with mood disorders; OCD = obsessive-compulsive disorder; SPEC = specific phobia;; PTSD = posttraumatic stress disorder MDD = major depressive disorder; DYS = dysthymia; MDD/DYS = major depressive disorder or dysthymia.
Overall frequency category was assigned as an additional diagnosis.
Significantly increased or decreased risk of co-occurring disorder (95% confidence interval)
Tabled reproduced from Brown, T.A., Campbell, L.A., Lehman, C.L., Grisham, J.R., & Mancill, R.B. (2001). Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology, 110, 585–599.
However, the findings of Brown et al. (2001) also revealed how the examination of comorbidity at the level of DSM-IV diagnosis can produce misleading findings about the overlap among disorders. For instance, the presence of PDA was associated with decreased relative risk of conditions such as SOC and SPEC. Rather than reflecting a true lack of association between these conditions (indeed, one would expect considerable phenotypic overlap of these disorders; e.g., situational avoidance), such findings can be a byproduct of DSM-IV differential diagnostic guidelines (i.e., features of social or specific fear/avoidance were often judged to be better accounted for and thereby subsumed under the PDA diagnosis). A clear instance of this phenomenon was findings on the comorbidity of GAD and mood disorders. When adhering strictly to DSM-IV diagnostic rules, the comorbidity between GAD and DYS was 5%. However, when ignoring the hierarchy rule that GAD should not be assigned when it occurs exclusively during a course of a mood disorder, the comorbidity estimate rose to 90%. While curtailing (or distorting) comorbidity, DSM’s differential diagnostic guidelines also forfeit salient clinical information. Strict adherence to DSM-IV criteria does not acknowledge the common situation where clinically significant GAD co-resides with a mood disorder or PTSD. Nonetheless, such symptoms are relevant to the overall severity of the clinical presentation, and may have strong implications for treatment planning, untreated course, and so forth (Kessler et al. 2008; Lawrence, Liverant, Rosellini, & Brown, 2009; Zimmerman & Chelminski, 2003).
Categorical classification
Although there are obvious practical advantages to a predominately categorical diagnostic classification system (e.g., use in clinical practice; cf. First, 2005), there are many serious drawbacks to this approach. For instance, as noted earlier, our diagnostic reliability study of the DSM-IV anxiety and mood disorders (Brown, Di Nardo, et al., 2001) found that for many categories (e.g., SOC, OCD), diagnostic disagreements were primarily due to problems in defining and applying a categorical threshold on the number, severity, or duration of symptoms. This threshold problem is also manifested in diagnostic disagreements where both raters concur that the key features of a disorder are present, but disagree as to whether these features cause sufficient interference or distress to satisfy the DSM-IV threshold for a clinical disorder (common with SOC and SPEC). Moreover, the problem is evident in the high rates of disagreements involving NOS diagnoses (both raters agree on the presence of clinically significant features of the disorder, but one rater does not assign a formal anxiety or mood disorder diagnosis due to subthreshold patient report of the number or duration of symptoms; common with generalized anxiety disorder and major depression). A similar problem is at the root of diagnostic disagreements involving MDD vs DYS (core features of clinically significant depression are observed by both raters, but disagreement occurs with regard to the severity or duration of these symptoms).
In addition to introducing measurement error (cf. MacCallum, Zhang, & Preacher, 2003), imposing categories on dimensional phenomena leads to a substantial loss of potentially valuable clinical information. As noted by Widiger and Samuel (2005), DSM does not provide adequate coverage for clinically significant symptom presentations that fail to meet criteria for formal diagnostic categories. This is reflected in part by the high rate in which NOS diagnoses are assigned as current and lifetime conditions (e.g., Brown, Campbell, et al., 2001; Lawrence & Brown, in press), but it is likely that clinically significant subthreshold cases are altogether undetected by the categorical system. Although rarely used in clinical practice and applied research, DSM does provide a coarse mechanism for recording the severity of disorders above the diagnostic threshold (i.e., as detailed in the “Use of the Manual” section of the DSM-IV, the ordinal specifiers of mild, moderate, and severe may be used for any current disorder meeting full diagnostic criteria). The only DSM-IV anxiety and mood disorder category where individual differences in symptom severity are embedded in a disorder’s diagnostic criteria is MDD (i.e., severity specifiers of mild, moderate, and severe with/without psychotic features are recorded when assigning the MDD diagnosis). Yet, whereas the dimensional ratings of the severity of MDD symptoms are reliable (r = .74), the DSM-IV categorical severity specifiers of this disorder are not (e.g., κ = .30; Brown et al., 2001). This further attests to the problem of measurement error associated with imposing nominal or ordinal cutoffs on continuous symptom features.
Summary and illustration of DSM-IV limitations
The preceding sections summarized some of the research that highlighted various limitations associated with DSM’s categorical approach to diagnostic classification (e.g., measurement error due to operationalizing and applying a categorical cutoff on dimensional features such as symptom frequency, severity, and duration; distorted rates of diagnostic comorbidity due to overlapping criteria sets and diagnostic decision rules; inadequate coverage of subthreshold presentations and individual differences in severity of threshold cases). As noted earlier, the issues of modest diagnostic reliability and high comorbidity have been routinely associated with GAD, thus making it an appropriate diagnostic category for further illustrating the shortcomings of the DSM-IV classification system. For clinical presentations entailing the features of GAD (excessive worry and associated features such as muscle tension and irritability), the potential sources of diagnostic unreliability are multifold. As is the case with most disorder categories, DSM-IV’s operationalization of GAD categorical diagnostic threshold is not based on compelling empirical evidence and is difficult to reliably implement in clinical practice. For instance, some of the requirements for a DSM-IV diagnosis of GAD are “excessive anxiety and worry, occurring more days than not for at least 6 months, about a number of events or activities”(Criterion A), “the anxiety and worry are associated with three (or more) of six symptoms (with at least some symptoms present for more days than not for the past 6 months)” (Criterion C), and “does not occur exclusively during a mood disorder” (and other conditions such as PTSD and psychotic disorders) (Criteria D and F). In addition to their dubious scientific basis (e.g., limited evidence to support the symptom number and duration cutoffs specified in Criterion C), the criteria are vaguely worded and thus require considerable clinical judgment in their implementation for establishing the presence/absence of a GAD diagnosis.
While this was intentional (owing in part to the absence of data in support of more specific symptom cutoffs), the DSM-IV approach to operationalizing disorder thresholds introduces considerable measurement error. For instance, what “number” of worry areas are necessary to meet Criterion A (two? several?)?; how many associated symptoms must be present more days than not over the prior 6 months (one? more than one?)? Should Criterion F be interpreted as indicating that GAD can be assigned in context of a co-occurring mood disorder so long as there has been a period of at least a few days or weeks when GAD was present and the mood disorder was not (or is a full 6-month duration of GAD without a co-occurring mood disorder necessary to meet this criterion?). Research laboratories may be inclined to develop more refined operationalizations of these vaguely worded diagnostic criteria in order to foster the reliability of diagnostic judgments within their setting. However, such operationalizations may vary across research laboratories (i.e., variability in the manner in which GAD diagnoses are assigned) which would thus complicate the comparability and interpretability of findings across studies. In addition to obscuring true patterns of symptom and syndrome comorbidity, the diagnostic hierarchy rule stating GAD should not be assigned if it occurs during the course of a mood disorder can lead to instances where GAD cannot be formally assigned despite the fact that it is associated with more distress and impairment than the mood disorder it is subsumed under (e.g., severe GAD occurring during a mild MDD). Finally, as is the case with other disorders, the failure of DSM-IV to recognize individual differences in the frequency, severity, and duration of symptoms can result in clinically salient GAD presentations that are not recognized or a generically coded as anxiety disorder NOS (cf. Lawrence & Brown, in press).
Alternative Classification Systems
For decades, researchers have acknowledged the potential utility of incorporating dimensional elements into our diagnostic classification systems (e.g., Barlow, 1988; Kendell, 1975; Maser & Cloninger, 1990; Widiger, 1992). Over this considerable time span, however, no strong proposals have emerged with regard to exactly how dimensional classification could be introduced in the DSM. In an earlier paper (Brown & Barlow, 2005), we forwarded an initial proposal for this endeavor. Given that clinical practicality is a compelling reason for retaining categorical distinctions in the nosology, we suggested the introduction of dimensional severity ratings to the extant diagnostic categories and/or the constituent symptom criteria (along the lines of the procedures used in the Anxiety Disorders Interview Schedule for DSM-IV; cf. Brown et al., 1998). Compared to more drastic proposals (e.g., multi-dimensional assessment, in which categorical diagnostic labels are subsequently imposed on the basis of quantitative algorithms), it was argued that this alternative would be relatively practical because the categorical system would remain intact and the dimensional rating system could be optional in settings where its implementation is less feasible (e.g., primary care). Several potential advantages of this dimensional system were noted including the ability to address key shortcomings and sources of unreliability in the DSM, such as its failure to convey disorder severity as well as other clinically significant features that are either subsumed by other disorders (e.g., GAD in mood disorders and PTSD) or fall just below conventional thresholds due to a DSM technicality (e.g., subclinical or NOS diagnoses where the clinical presentation is a symptom or two short of a formal disorder). Moreover, because the dimensional ratings would be added to the current diagnostic categories, this approach would have other advantages including: (a) its basis on a pre-existing and widely studied set of constructs; and (b) the ability to retain functional analytic and temporal (duration) aspects of diagnosis that are difficult to capture in a purely psychometric approach. It would also provide a standardized assessment system that would foster across-site comparability in the study of dimensional models of psychopathology. Finally, we argued that this approach could be regarded as a prudent “first step” that would assist in determining the feasibility of more ambitious dimensional systems (e.g., quantifying higher-order dimensions).
Nonetheless, this initial proposal is not without immediately apparent limitations. For instance, as noted earlier, “difference in patient report” (i.e., patient gives different information to independent interviewers in response to inquiries about the presence, severity, or duration of symptoms) is a very common source of diagnostic unreliability that would be relevant to dimensional clinical assessment. In fact, because the dimensional ratings would simply be added onto the existing criteria sets, most sources of unreliability present in the current diagnostic system would continue to be germane (e.g., measurement error associated with vaguely operationalized symptom criteria and differential diagnosis decision rules; see GAD example in preceding paragraph). Perhaps more importantly, because the various disorder categories would remain unchanged, a dimensional system of this nature would not address the problem of high diagnostic comorbidity.
Higher-order models of classification
Thus, more ambitious proposals have been suggested which place emphasis on dimensions corresponding to broader biologically and environmentally based constructs of temperament and personality (e.g., neuroticism/negative affectivity; Clark, 2005). These strategies follow from the theories and evidence that the observed overlap in families of disorders (e.g., comorbidity and symptom overlap in anxiety and mood disorders) is due to the fact that these conditions emerge from shared biologic/genetic and psychosocial diatheses (e.g., Barlow, 2002; Kendler et al., 1992; Mineka et al., 1998). Under this framework, the DSM disorders represent different manifestations of these core vulnerabilities, and such variability stems from the influence of other, more specific etiologic agents (e.g., environmentally based psychological vulnerabilities, other genetic or biological influences; cf. Barlow, 2002; Suárez, Bennett, Goldstein, & Barlow, 2009).
Two genetically based core dimensions of temperament have been posited as instrumental in the etiology and course of the emotional disorders: neuroticism/negative affectivity and extraversion/positive affectivity. Extensive evidence indicates these constructs are strongly heritable (e.g., Fanous, Gardner, Prescott, Cancro, & Kendler, 2002; Fulker, 1981; Hettema, Prescott, & Kendler, 2004; Tellegen et al., 1988; Viken, Rose, Kaprio, & Koskenvuo, 1994) and stable over time (Costa & McCrae, 1988; Kasch, Rottenberg, Arnow, & Gotlib, 2002; Watson & Clark, 1984). Whereas neuroticism/negative affect is considered to be etiologically relevant to the full range of emotional disorders, the influence of extraversion/positive affect appears to be more specific to depression,, SOC, and mania, with depression and SOC associated with low positive affect and mania with high positive affect (e.g., Brown, 2007; Brown, Chorpita, & Barlow, 1998; Gruber, Johnson, Oveis, & Keltner, 2008; Johnson, Gruber, & Eisner, 2007; Mineka et al., 1998; Watson, Clark, & Carey, 1988). Although the theoretical frameworks were developed independently (cf. Eysenck, 1981; Tellegen, 1985), neuroticism/negative affect and extraversion/positive affect are closely related to Gray’s (1987) constructs of behavioral inhibition and behavioral activation, respectively, at both the conceptual and empirical levels (e.g., Campbell-Sills, Liverant, & Brown, 2004; Carver & White, 1994; Clark et al., 1994; Fowles, 1994; Kasch et al., 2002).
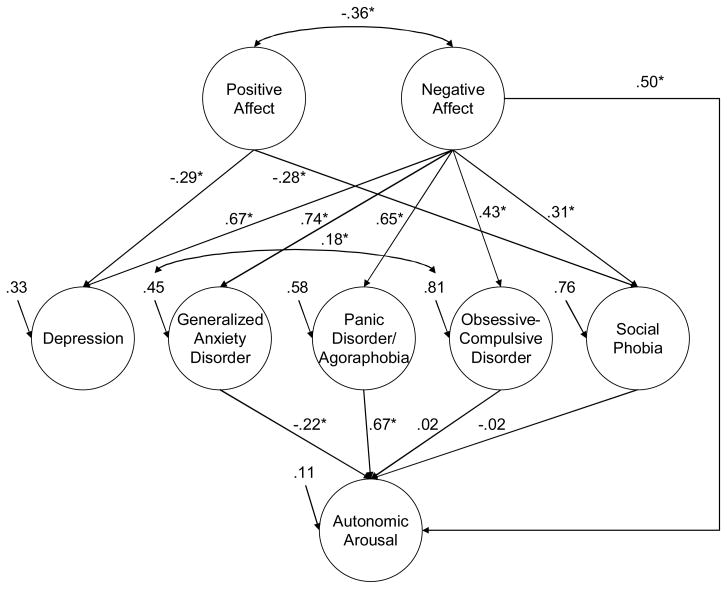
A substantial literature underscores the roles of these constructs in accounting for the onset, overlap, and maintenance of anxiety and depression (e.g., Brown, 2007; Brown et al., 1998; Gershuny & Sher, 1998; Kasch et al., 2002; Watson et al., 1988). For instance, in a sample of outpatients, Brown et al. (1998) found that virtually all the considerable covariance among latent variables corresponding to the DSM-IV constructs of unipolar depression (DEP), social phobia (SOC), generalized anxiety disorder (GAD), obsessive-compulsive disorder (OCD), and panic disorder/agoraphobia (PD/A) was explained by the higher-order dimensions of negative affect and positive affect (bipolar disorder was not included). Although the results were consistent with the notion of neuroticism/negative affect as a broadly relevant dimension of vulnerability, results indicated the DSM-IV disorders were differentially related to negative affect, with DEP and GAD evidencing the strongest associations (see also Brown & McNiff, in press). In accord with a reformulated hierarchical model of anxiety and depression (Mineka et al., 1998), positive affect was predictive of DEP and SOC only (see Figure 1).
Figure 1. Structural Model of the Interrelationships of DSM-IV Disorder Constructs and Negative Affect, Positive Affect, and Autonomic Arousal.
Completely standardized estimates are shown (path coefficients with asterisks are statistically significant, p < .01). Figure reproduced from Brown, T.A., Chorpita, B.F., & Barlow, D.H. (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107, 179–192.
Brown (2007) extended these findings by examining the temporal course and temporal structural relationships of dimensions of temperament (neuroticism/behavioral inhibition, N/BI; behavioral activation/positive affect, BA/P) and selected DSM-IV disorder constructs (DEP, SOC, GAD). Outpatients with anxiety and unipolar mood disorders (N = 606) were reassessed at one-year (T2) and two-year (T3) follow-ups. As the majority (76%) of patients received treatment after intake, the overall rate of anxiety and mood disorders declined significantly over follow-up (e.g., 100% to 58% for T1 and T3, respectively). Nonetheless, each of the five constructs examined (N/BI, BA/P, DEP, GAD, SOC) evidenced a favorable level of longitudinal measurement invariance. Despite the marked decline in DSM-IV diagnoses by T3, test-retest correlations of the factors and unconditional latent growth models (LGMs) indicated that BA/P evidenced a very high degree of temporal stability, consistent with its conceptualization as a trait vulnerability construct that is relatively unaffected by treatment. However, of the five constructs examined, N/BI evidenced the greatest amount of temporal change and was the dimension associated with the largest treatment effect. In addition to its inconsistency with prior research (e.g., Kasch et al., 2002), this finding seems at odds with conceptual speculations that core dimensions of temperament may be more resilient to psychological treatment. As discussed in Brown (2007), this result may partly reflect the fact that the assessment of temperament is prone to mood-state distortion (cf. Clark et al., 2003; Widiger et al., 1999). That is, it is likely the measurement of N/BI consists of some combination of stable temperament variance (i.e., vulnerability) and variability attributable to generalized distress (i.e., more prone to mood-state distortion, subject to greater temporal fluctuation). Thus, the considerable covariance between N/BI and the emotional disorders is due partly to a temperamental component (N/BI acts as vulnerability, is relatively stable), but also because of the distress associated with having a disorder (mood-state distortion). Presumably, the latter aspect is less temporally unstable and more apt to covary with temporal fluctuations in the severity of disorders.
Indeed, findings indicated that N/BI operated differently than the DSM-IV disorder constructs in several ways. For instance, unconditional LGMs of each DSM-IV disorder construct revealed inverse relations between the Intercept and Slope; i.e., higher initial disorder severity was associated with greater change over time. However, the Intercept and Slope of N/BI were positively correlated (r = .47), indicating that patients with higher initial levels of N/BI tended to show less change in this dimension over time; and conversely, patients with lower initial levels of N/BI tended to evidence greater change. Thus, unlike the DSM-IV disorders, the stability of N/BI increased as a function of initial severity. This may indicate the influence of mood-state distortion/general distress on the measurement of N/BI is most pronounced at the lower end of its continuum (i.e., it is the lower range of N/BI that is less temporally stable and presumably more apt to covary with temporal change in disorder severity). In addition, parallel-process LGMs indicated that higher initial levels of N/BI were associated with less change in the DSM-IV constructs of GAD and SOC. Moreover, lower BA/P predicted poorer outcome of SOC, although this effect only approached statistical significance (p = .07) with N/BI in the analysis. Although no temporal relations were obtained for DEP, these results are in line with in earlier work and theory that N/BI and BA/P have directional temporal effects on Axis I psychopathology (cf. Gershuny & Sher, 1998; Kasch et al., 2002; Meyer, Johnson, & Winters, 2001). Consistent with prediction and theory, initial levels of the DSM-IV disorders did not predict increases in temperament over time. Finally, Brown (2007) found that temporal change in DEP, SOC, and GAD was significantly related to change in N/BI. Of particular interest is the finding that all the temporal covariance of the DSM-IV disorder constructs was accounted for by change in N/BI; i.e., when N/BI was specified as a predictor, the temporal overlap among disorder constructs was reduced to zero. The correlational nature of these findings precludes firm conclusions about the direction of these effects. Although counter to earlier initial evidence and conceptualization (Brown et al., 1995; Kasch et al., 2002), N/BI may be therapeutically malleable and this in fact mediates the extent of change in the emotional disorders. Alternatively or additively, a reduction in disorder severity is associated with a decrease in general distress, a feature shared by the emotional disorders and is partially reflected in the measurement of N/BI. Finally, in the case of bipolar disorder, Johnson and colleagues (Gruber et al., 2008; Johnson et al., 2007; Meyer et al., 2001) have demonstrated that risk for mania is associated with stable, elevated BA/P.
A nosological emphasis on shared dimensions
Compared to the more modest proposal of adding dimensional elements to the extant diagnostic categories (cf. Brown & Barlow, 2005), the inclusion of higher-order dimensions in the nosology would address the considerable overlap that exists among the current DSM-IV anxiety and mood disorder constructs. As we noted previously (Brown & Barlow, 2005), because dimensions such as N/BI and BA/P reflect general vulnerability constructs, their inclusion would make the diagnostic system germane to the primary and secondary prevention of mental disorders (e.g., identification of individuals with elevated N/BI who thus may be at risk for psychopathology if exposed to other vulnerability factors such as life stressors). Of course, this is a far more challenging endeavor because these broader phenotypes are not currently recognized by the DSM and thus must be further validated and measured in a manner that is feasible in clinical practice and research. Moreover, an exclusive focus on higher-order dimensions could be viewed as overly reductionistic because there is considerable variability in which these core vulnerabilities are manifested as clinical psychopathology. Although the covariance of SOC and MDD can be fully explained by the shared vulnerability dimensions of N/BI and BA/P (Brown, 2007; Brown et al., 1998), further differentiation is important because constructs more specific to these disorders provide information about treatment planning, risk of complications (e.g., suicidality), and so forth, than does only knowing a patient’s standing on the continuum of these nonspecific higher-order dimensions. However, while more germane to some DSM-IV disorder constructs than to others, these lower-order dimensions are also present in varying degrees across the emotional disorders (e.g., while fear of negative social evaluation is the defining feature of SOC, it is germane to other DSM-IV disorder constructs such as PD/A, mood disorders, and body dysmorphic disorder). While having the advantage of providing important additional information about the nature of an individual’s psychopathology, the inclusion of these lower-order dimensions would perpetuate the rather weak boundaries among the DSM disorder constructs. But by also including broader dimensions such as N/BI and B/PA, the nosological system would possess a hierarchical framework that accounts for the overlap at the lower-order level.
Indeed, current conceptual models assert that dimensions of temperament do not act alone in determining the etiology, course, and complications of emotional disorders (e.g., Barlow, 2002; Carver, Johnson, & Joormann, 2008; Clark et al., 1994; Mineka et al., 1998). For instance, Barlow (2000, 2002; Suárez et al., 2009) has formulated a triple vulnerability model of emotional disorders, which draws from and integrates the rich literatures of genetics, personality, cognitive and neuroscience, and emotion and learning theories. This model specifies the existence of a generalized biological vulnerability to experience anxiety consisting of a well-established genetic contribution to this diathesis accounting for approximately 30% to 50% of the variance. In addition, a generalized psychological vulnerability emerges from early childhood experience characterized by a stressful, unpredictable environment and/or the influence of specific parenting styles described in detail in the attachment theory literature that inhibit the development of effective coping procedures and the emergence of self efficacy. These early experiences lead to a general sense of unpredictability and uncontrollability over life events that, along with elevated sympathetic nervous system arousal, forms the core of the process of anxiety (Barlow, 2002). If these two generalized vulnerabilities or diatheses line up, the individual is at increased risk for experiencing generalized anxiety and/or depression, in the context of triggering stressful events (Chorpita & Barlow, 1998; Suárez et al., 2009). But a third diathesis, referred to as a specific psychological vulnerability, comes into play in the form of learning a particular focus for anxiety, or learning that some situations, objects, or internal somatic states are potentially dangerous even if objectively they are not. These early learning experiences can be as straightforward as watching parents’ model severe fears of specific objects or situations such as small animals (e.g., as in SPEC), or more subtle such as experiencing heightened attention from caregivers to the potential danger of experiencing unexplained somatic sensations (e.g., as in PD/A or hypochondriasis).
One may notice that the two generalized vulnerabilities, one biological and the other psychological, describe a more stable disposition to experience anxiety, and thus, could be considered more accurately as a temperament. Indeed we consider anxiety in this regard as simply the expression of the temperament of N/BI with the addition, in many cases, of a specific focus (or several specific foci) dictated by the learning experiences that comprise the third vulnerability. Evidence for this relationship is presented in detail elsewhere (Barlow, 2002; Suárez et al., 2009).
A New Proposal for a Dimensional Classification System
These considerations, then, lead to a dimensional classification system for emotional disorders emphasizing common features but encompassing the variety of phenotypic expressions emerging from different foci of anxiety. At the highest level, an individual would experience various levels of severity in terms of intensity, frequency, and distress associated with anxiety or N/BI (which we now refer to as anxiety/neuroticism/behavioral inhibition, or AN). This temperament is associated with chronic generalized distress, particularly involving the hypothalamic-pituitary-adrenocortical axis, perceptions of uncontrollability regarding future threatening and challenging events, excessive vigilance, and low self confidence/self-efficacy over one’s ability to cope with future threatening events.
In addition to assessing the presence and severity of AN, the second higher-order dimension of behavioral activation/positive affectivity (BA/P) must also be considered (see Figure 1). Low positive affect reflects principally low enthusiasm, interest, and an overriding pessimistic sense, and is associated with the DSM-IV disorder constructs of MDD and SOC, as noted above. Once again, structural models demonstrate that AN provides substantial contributions to these two DSM-IV disorder constructs, but that low BA/P is also part of the picture. In the case of SOC, this may well be associated with the chronically impoverished network of social relationships and support which contributes so substantially to positive affect based on the work of scientists studying the determinants of positive affect in the normal population (e.g., Diener & Seligman, 2002; Gilbert, 2006). In clinical populations, low-level manifestations of BA/P merge into a presentation that has been referred to as “mixed anxiety depression” (Moras et al., 1996; Zinbarg et al., 1994). High level manifestations of BA/P are associated with euthymic stages of bipolar and cyclothymic disorders.
Each individual experiencing varying degrees of AN would also almost certainly display substantial avoidance behaviors in all of its behavioral and cognitive manifestations. These manifestations would include situational avoidance, most obviously, in the case of phobic avoidance. Because SPEC in isolation is not characterized by marked AN, specification of situational avoidance could simply be represented on this dimension. A variant of situational avoidance that is common across the anxiety disorders is the avoidance of internal somatic cues such as avoiding a hot and stuffy room, physical exertion, and situations provoking perceptual distortions associated with dissociation. Although much of this behavioral avoidance may appear to be situational, the cues for avoidance are actually interoceptive (e.g., a hot and stuffy room). But more subtle cognitive and or emotional avoidance exemplified most commonly by attempts at distraction or the presence of safety signals or talismans meant to (magically) protect against the occurrence of AN and/or the eruptions of discrete emotions such as panic attacks comprise another facet of avoidance. The extent of this avoidance could also be dimensionalized, leading to further specification with implications for treatment planning. Table 3 provides examples of various avoidant strategies.
Table 3.
Examples of Avoidance Strategies
| Avoidance Strategy | Disorder Often Associated |
|---|---|
| I. Behavioral and Interoceptive Avoidance | |
| Situational avoidance/escape | |
| Avoidance/escape from phobic situations (e.g., crowds, parties, elevators, public speaking, theaters, animals) | PD/A, SOC, SPEC |
| Subtle behavioral avoidance | |
| Avoidance of eye contact (e.g., wearing sunglasses) | SOC |
| Avoidance of sensation-producing activities (e.g., physical exertion, caffeine, hot rooms) | PD/A |
| Avoidance of “contaminated” objects (e.g., sinks, toilets, doorknobs, money) | OCD |
| Perfectionistic behavior at work or home | GAD, SOC, OCD |
| Procrastination (avoidance of emotionally salient tasks) | GAD, DEP |
| Repetitive or ritualistic behaviors | |
| Compulsive acts (e.g., excessive checking, cleaning) | OCD |
| II. Cognitive and Emotional Avoidance | |
| Cognitive avoidance/escape | |
| Distraction (e.g., reading a book, watching television) | GAD, DEP, PD/A |
| Avoidance of thoughts or memories about trauma | PTSD |
| Effort to prevent thoughts from coming into mind | OCD, PTSD |
| Worry | GAD |
| Rumination | DEP |
| Thought suppression | All disorders |
| Safety signals | |
| Carrying a cell phone | PD/A, GAD |
| Holding onto “good luck” charms | OCD |
| Carrying water or empty medication bottles | PD/A |
| Having reading material always on hand | SOC, GAD |
| Carrying self-protective materials (e.g., mace, siren) | PTSD |
Note. PD/A = panic disorder with/without agoraphobia, SOC = social anxiety disorder, SPEC = specific phobia, OCD = obsessive-compulsive disorder, GAD = generalized anxiety disorder, DEP = depressive disorders (e.g., major depression, dysthymic disorder), PTSD = posttraumatic stress disorder.
Having established the presence and dimensional severity of AN, BA/P, and avoidance behavior, it then becomes important to examine the functional relationships of AN with specific facets of emotional expression or other experiences that have traditionally been considered as “key features” of existing criteria sets. As noted above, for GAD, stressful life events trigger the diathesis of AN to produce a clinical syndrome. While GAD is simply a pathologically strong expression of AN, depression (e.g., MDD, DYS), which is characterized by cognitive and motor slowing, hopelessness, and marked anhedonia, emerges from AN in combination with (low) BA/P when activated by life stressors (cf. Mineka et al., 1998). Mania (and hypomania), on the other hand, emerges from high BA/P when triggered by life stressors.
For the anxiety disorders other than GAD, the third (specific) vulnerability is activated in which AN, through a process of learning, is specifically associated with an object or event. This process results in one or more key diagnostic features that become the principal focus or foci of AN. These major features are described next.
The occurrence of discrete eruptions of emotion leads to several common manifestations of key features (Barlow, 2002). One manifestation is evident in the form of an ethologically primitive sympathetic nervous system surge known as the flight/fight response, which is the action tendency of the basic emotion of fear. When fear is triggered by relatively non-dangerous internal or external cues and therefore occurs at an inappropriate time, the experience is called a panic attack. The fact that panic attacks subsequently may become a major focus of AN has been explicated in considerable detail in the case of PD/A (Bouton, Mineka, & Barlow, 2001; White & Barlow, 2002). But the same phenomenon has been demonstrated to occur in PTSD where it is referred to as “flashbacks” (Brown & McNiff, in press; Jones & Barlow, 1990). We refer to the object of this focus as panic and related autonomic surges.
Somatic symptoms or experiences can become functionally related to AN and may become a second focus. For example, in the case of hypochondriasis, certain unexplained physical symptoms are associated in a chronic manner with potential threatening illness or disease. Similarly, sensations of unreality, if they become the focus of AN, can evolve into a prominent feature of PTSD and depersonalization disorder. Apprehension about the physical symptoms of anxiety and panic attacks is a key feature of PD/A (Clark, 1986; Taylor, 1999; White & Barlow, 2002). We refer to this focus as somatic anxiety.
A third common focus of AN is ego-dystonic intrusive cognitions. Although most characteristic of OCD and body dysmorphic disorder (BDD), studies have shown that these types of ego-dystonic intrusive thoughts are fairly common in the normal population as a function of stressful life events (e.g., Fullana et al., 2009; Parkinson & Rachman, 1981; Rachman & de Silva, 1978), but can reach substantial levels of severity in the context of a wide range of emotional disorders even in the absence of a diagnosis of OCD or BDD. Thus, it is common to see intrusive ego-dystonic thoughts of, for example, harming one’s children in cases where the principal diagnosis is PD/A or GAD, and these are associated with varying amounts of AN (Barlow, 2002).
A fourth dimension could be described as social evaluation. Once again, although typically associated with SOC where it becomes the key diagnostic feature, it is common for this focus to be represented on a dimension of severity across most emotional disorders (e.g., Rapee, Sanderson, & Barlow, 1988).
A fifth focus of AN is past trauma with all of its ramifications. When the focus is on past trauma, it also quite common, as noted above, to experience sympathetic surges in the form of flashbacks triggered by internal or external cues originally associated with the trauma. But the focus of AN on past traumatic experience in those individuals already vulnerable to the expression of AN is the key feature of the disorder (Keane & Barlow, 2002; Steenkamp, McLean, Arditte, & Litz, in press).
Thus, it becomes essential through a functional analysis to determine the focus of AN. One would accomplish this by first ascertaining the severity of AN along with the particular key features that might be the focus of AN to varying degrees. Following past precedent, the focus would correspond to current DSM-IV categories, but one could also determine the extent to which other key features are present on dimensions of severity that would include intensity, frequency, and distress, thereby providing potentially important information for treatment planning and prediction of course. In this way, information that is currently discarded in the system of prototypes that comprises DSM-IV (unless patients happen to meet all of the criteria for a comorbid diagnosis) would be saved and incorporated into the clinical picture.
In sum, AN, and BA/P, as well as types of avoidant strategies, would be rated on severity dimensions for each individual presenting with emotional disorders. If severe enough or exacerbated by stress, these diatheses present as GAD and, in the presence of low BA/P, unipolar depression (e.g., MDD, DYS). High BA/P is, of course, uniquely associated with bipolar disorder. It is also important to determine any foci of anxiety and avoidance. An example of a recent patient presenting to our Center, whose presenting clinical symptoms are organized in this way, is presented below.
Case example
The patient was a male high school teacher in his mid-fifties, who was referred to the Center after worsening symptoms following a severe car accident some four months previously. Symptoms included intrusive memories of the crash, images of his wife’s injured face, very clear flashbacks to certain aspects of the accident itself, accompanied by some memory difficulties for other aspects of the accident, and hypervigilance to his surroundings as well as a strong startle reaction to cues relating to the accident. These symptoms intermingled with a similar set of symptoms emerging from multiple traumatic events experienced during the Vietnam War. In addition, he reported spending a great deal of the day worrying about a variety of life events, including his own health and that of his family, as well as his performance at work. He noted that he worried approximately one-third of the day and had been like this since returning from the war. He had previously sought treatment after suffering an episode of severe grief following the death of his parents some 15 years earlier. He continued to exhibit relatively mild symptoms of depression. In addition, he was concerned about interacting inappropriately with his students and that he would be evaluated badly by other staff members leading to dismissal form his teaching job.
On the basis of this clinical presentation, the only DSM-IV diagnosis formally assigned was PTSD. Although the patient met all the key and associated features of GAD, this diagnosis could not be assigned if adhering to a DSM-IV hierarchy rule (i.e., the disturbance occurred during the course of PTSD). In addition, whereas mild depression including some lethargy was part of the clinical picture, the patient’s symptoms were not sufficiently severe to meet the diagnostic threshold for a unipolar mood disorder such as MDD or DYS.
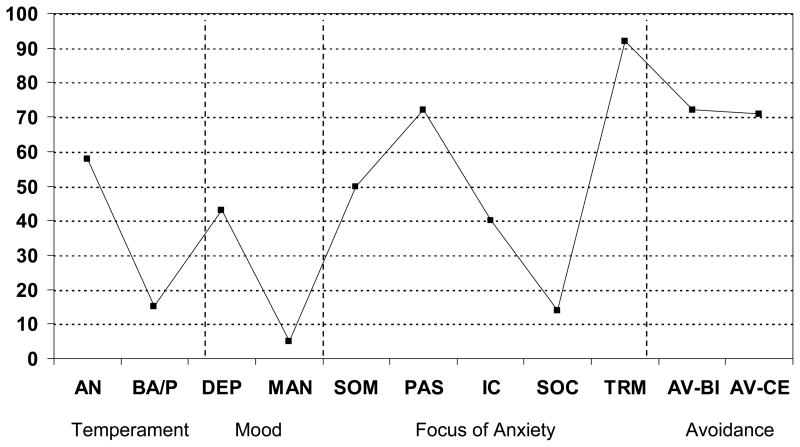
In Figure 2, we present the patient’s diagnostic profile using the scheme described above. As seen in this figure, the patient presented with high levels of AN and moderately low BA/P. Behavioral avoidance was also elevated as reflected in avoidance of driving in certain locations, driving long distances, or engaging in activities or conversations associated with war. Although avoidance of intense emotion (blunting) and interoceptive cures were present for a time after the war, this type of cognitive/emotional avoidance had lessened considerably over the years. The foci of anxiety were primarily on past trauma, along with elevations for panic-related autonomic surges (which in this case represented flashbacks) and somatic anxiety. Because all intrusive thoughts were related to trauma, ego-dystonic intrusive thoughts were largely absent. Anxiety focused on social evaluation was present at moderate intensity in the context of evaluation at work. Accordingly, this dimensional profile provides a more complete portrayal of the patient’s clinical presentation relative to a single categorical diagnosis of PTSD. The profile captures the dimensional severity of the key features of PTSD (i.e., focus on past trauma, panic-related autonomic surges, avoidance), in addition to clinical features that are often associated and functionally related to PTSD but not recognized by the DSM-IV definition of this disorder (e.g., temperament, somatic anxiety). Moreover, although GAD could not be assigned under the DSM-IV framework, the profile recognizes the presence of high AN that may be relevant to prognosis and treatment planning. A sub-diagnostic threshold level of depression is also reflected that would be missed by DSM-IV diagnosis but which may be nonetheless clinically salient. Notably, while providing a richer depiction of the patient’s presenting symptoms and their severity, the dimensional profile avoids the various diagnosis decision rules (e.g., diagnostic hierarchy, temporal overlap, symptom counts, determination of whether symptoms are better accounted for by another condition) that are a common sources of DSM-IV diagnostic unreliability and that often result in non-veridical patterns of diagnostic comorbidity.
Figure 2. Example Profile of Patient Evaluated with a Dimensional Classification System.
Note. AN = anxiety-neuroticism, BA/P = behavioral activation-positive affect, DEP = unipolar depression, MAN = mania, SOM = somatic anxiety, PAS = panic and related autonomic surges, IC = intrusive cognitions, SOC = social evaluation, TRM = past trauma, AV-BI = behavioral and interoceptive avoidance, AV-CE = cognitive and emotional avoidance; higher scores on the Y-axis (0–100) indicate higher levels of the X-axis dimension, but otherwise the Y-axis metric is arbitrary and used for illustrative purposes.
Transdiagnostic treatment protocols
This diagnostic conception also has implications for treatment. Elsewhere, we have described the conceptual underpinnings of a unified, transdiagnostic treatment for emotional disorders (Barlow et. al., 2004; Fairholme, Boisseau, Ellard, Ehrenreich, & Barlow, in press; Moses & Barlow, 2006). These developments arise from work over the last few decades that has empirically supported a number of psychological treatments targeting individual anxiety and mood disorders, usually organized around specific DSM IV criteria sets (Barlow, 2008, Nathan & Gorman, 2007). However, the aforementioned conceptualizations of diagnosis and psychopathology emphasize commonalities rather than their differences among these disorders. In addition, treatment outcome research points to generalization of treatment response from a treated disorder (such as PDA) across other comorbid anxiety and mood disorders (e.g., Brown et al., 1995). Careful analysis also highlights a common set of therapeutic operations across these disparate protocols (Barlow et. al., 2004). Thus, research lends support to a unified, transdiagnostic approach to emotional disorders that considers these commonalities and distills common therapeutic procedures across evidenced-based protocols.
At the same time, research on emotion regulation has provided a novel perspective on the treatment of anxiety and mood disorders, which are essentially disorders of emotion (Barlow, 1991, 2002). It is now clear that emotion regulation, or how individuals influence the occurrence, intensity, expression, and experience of emotions, plays an important role in phenomenology of anxiety and mood disorders (Campbell-Sills & Barlow, 2007; Gross, 2007). Deficits in emotion regulation are found in each of these disorders, as individuals with anxiety and mood disorders often use maladaptive regulation strategies that contribute to the persistence of symptoms. Thus, increased attention to emotional dysregulation in treatment is grounded in current research findings and is consistent with emerging conceptualizations emphasizing underlying commonalities among emotional disorders.
Based on these advances, we have developed a treatment designed to be applicable to all anxiety and unipolar mood disorders, and possibly other disorders with strong emotional components (e.g., many somatoform and dissociative disorders) that addresses core affective properties rather than narrowly construed DSM-IV key features. The unified protocol capitalizes on the contributions made by cognitive-behavioral theorists by distilling and incorporating the common principles among existing evidenced based psychological treatments such as restructuring maladaptive cognitive appraisals, changing action tendencies associated with the disordered emotion, preventing emotional avoidance, and utilizing emotional exposure procedures. It also draws on the innovations from the field of emotion science, incorporating and addressing the deficits in emotion regulation common in emotional disorders.
Because this transdiagnostic intervention addresses core psychopathological features that cut across the DSM-IV disorders, the proposed nosological scheme described above facilitates a more comprehensive conceptualization and assessment of temperaments and associated foci of AN. Some evidence suggests that changes in AN may be substantial in some patients during successful psychological treatment (e.g., Brown, 2007), and this change may be associated with the widely noted outcome of enduring treatment effects from successful psychological treatment relative to drug treatment (e.g., Barlow et. al., 2000). Furthermore, we have previously reported that generalized improvement in comorbid emotional disorders after treatment of the principal disorder is not necessarily sustained over time, even if improvement in the “target” disorder is sustained (Brown et al., 1995). Transdiagnostic treatment and comprehensive conceptualization and assessment may obviate the outcome of incomplete treatment and the necessity of repeated, sequential, and narrowly targeted courses of intervention for each DSM-IV disorder.
Practical Considerations and Future Directions
The goal of this paper was to outline our vision of how a dimensional classification system based on common features might look for the anxiety and mood disorders. Clearly, this clinical assessment system is more radical than a previous proposal to simply incorporate dimensional severity ratings into the existing DSM disorder criteria sets (cf. Brown & Barlow, 2005). While this assessment system possesses several advantages over comparatively modest dimensional alternatives (e.g., better capture salient clinical features that would not be recognized when adhering to DSM differential diagnosis decision rules; evaluation of core dimensions of temperament), researchers would be faced with many challenges in the development and implementation of this approach. A key consideration is clinical utility and all its components (e.g., acceptability and proper use by clinicians; First, 2005; First et al., 2004). Based on practical considerations, it may be difficult to envision a diagnostic classification system that is fully devoid of nominal elements. For instance, it has been argued that categorical diagnoses have greater clinical utility for endeavors such as clinical communication among practitioners and medical record keeping (First, 2005). Thus, the question arises as to what level could a dimensional system best exist in the formal nosology. A less radical approach would entail using the dimensional system to complement categorical diagnosis. In other words, although the primary emphasis would remain on the extant DSM classification system, a dimensional profile such as the one illustrated in Figure 2 could be used in tandem with categorical diagnoses to recognize important clinical features that would otherwise be ignored by DSM (e.g., core dimensions of temperament, symptoms subsumed by another condition). However, this intermediate position could be viewed as unsatisfactory because it would perpetuate many of the most serious practical and empirical drawbacks associated with the categorical system (e.g., high comorbidity and modest reliability of disorders).
Akin to proposals for the personality disorders (e.g., Widiger, Costa, & McCrae, 2002), a bolder approach would entail a nosological system that is driven by dimensional assessment and classification. In this scenario, a profile such as the one illustrated in Figure 2 would be generated for a patient via the administration of dimensional measures. Subsequently, categorical diagnostic labels, guided by empirically derived cut-points, would be assigned that characterize the patient’s dimensional profile (along the lines of the methods used in the MMPI). If a viable assessment system was developed, this approach would reconcile many common sources of diagnostic unreliability as well as the problem of high or distorted disorder comorbidity. But considerable work would be required to develop and validate an assessment system that is accepted and used in clinical and research settings alike.
While the constructs in Figure 2 are firmly established in the empirical literature and are well-known by most practitioners, they are currently assessed by a disparate array of clinician-administered and self-report measures. To be implemented feasibly in clinical practice, a single multidimensional measure of temperament, mood, avoidance, and foci of AN would have to be developed and validated. Another practical issue is that the dimensional system would require evaluation of the full spectrum of emotional disorder psychopathology. This would be a distinct departure from the manner by which diagnoses are currently made in clinical practice (i.e., determination of whether a patient’s clinical presentation corresponds to the criteria set for a specific DSM disorder). To avoid unreasonable time demands on the clinician, a greater emphasis on self-report may be required to assess each component of the dimensional profile (cf. Widiger et al., 2002). In addition to its own practical issues (e.g., cost, availability, time demand on patient), self-report assessment is often less capable than clinical interviewing in capturing some aspects of a clinical presentation such as the duration, temporal sequence, and functional relationships of symptoms. However, whereas these aspects are germane to the DSM (e.g., determination of whether the symptoms of a disorder are better accounted for or occur during another disorder), they would be less relevant to a nosology based on dimensional profiling where the emphasis is on the patterning and severity of common features rather than differential or hierarchical diagnosis and symptom counts.
Nevertheless, as has been repeatedly evidenced in the personality disorders literature (cf. Samuel & Widiger, 2006; Verheul, 2005), various concerns about clinical utility would likely be cited as primary reasons for why a dimensionally based classification system should not replace categorical DSM anxiety and mood diagnoses. These objections often pertain to concerns that clinicians would find a dimensional system unacceptable because they are unfamiliar with the dimensions, they perceive the dimensional classification system as overly cumbersome, they believe it will hinder communicating clinical information to patients and mental health professionals, or that the dimensions could not be used to guide treatment decisions or predict clinical course and prognosis (First et al., 2004; Samuel & Widiger, 2006; Verheul, 2005). However, there is some evidence that these concerns may be unfounded. For instance, in a study by Samuel and Widiger (2006), 245 practicing psychologists evaluated personality disorder cases using both the dimensional five-factor model (FFM) and the DSM-IV and then rated both assessment systems on several aspects of clinical utility. Despite the fact that the clinicians indicated that they were much less familiar with the FFM than DSM-IV, ratings on the ease of application of these assessment systems did not differ. Interestingly, the FFM was consistently rated as significantly more useful than the DSM-IV assessment model on several dimensions of clinical utility (e.g., better at providing a global description of the patient’s personality, communicating information to patients, capturing all of the patient’s clinically salient personality difficulties, and assisting the clinician in developing effective treatments).
It would be important to ascertain whether a dimensional classification system for anxiety and mood disorders is associated with comparable levels of clinical utility and acceptability found in the personality disorders literature (e.g., Blais, 1997; Samuel & Widiger, 2006; Sprock, 2003). Key to this endeavor would be the explication and validation of nominal cut-points or dimensional profiles necessary to inform clinical decisions (e.g., treatment planning and prognosis) and to facilitate communication among clinicians, patients, third-party payors, and so forth. Indeed, it might be argued that this empirical necessity is daunting to an extent that it undermines the potential realization of a dimensional system. However, as has been detailed in this article, one must be mindful of the fact that the DSM’s categorical diagnostic thresholds for mental disorders (i.e., the cut-point indicating the presence/absence of psychopathology) were set primarily by panel consensus (i.e., the various DSM workgroups) but are not grounded by strong empirical evidence. Indeed, the existence of a dimensional assessment system would launch the quest to establish empirically supported cut-points, an endeavor that has not been undertaken in DSM and perhaps which could not be compellingly addressed under this system (e.g., given the DSM’s reliance on nominal diagnoses and diagnostic criteria, cut-points in DSM are predetermined). Moreover, the possibility exists that this scientific venture would identify different sets of cut-points for a given dimension or dimensional profile to guide different clinical judgments, decisions, and predictions (e.g., inform the appropriate level or type of clinical intervention). This can only be accomplished through the analysis of the rich array of clinical information garnered by dimensional assessment, but which is lost or distorted by binary judgments of the presence or absence of psychopathology.
Acknowledgments
The authors thank Ben Emmert-Aronson for his assistance with this paper.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/pas.
References
- Andrews G. Classification of neurotic disorders. Journal of Royal Society of Medicine. 1990;83:606–607. doi: 10.1177/014107689008301003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G. Comorbidity in neurotic disorders: The similarities are more important than the differences. In: Rapee RM, editor. Current controversies in the anxiety disorders. New York: Guilford Press; 1996. pp. 3–20. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford Press; 1988. [Google Scholar]
- Barlow DH. Disorders of emotion. Psychological Inquiry. 1991;2:58–71. [Google Scholar]
- Barlow DH. Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist. 2000;55:1247–1263. doi: 10.1037//0003-066x.55.11.1247. [DOI] [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. [Google Scholar]
- Barlow DH, editor. Clinical handbook of psychological disorders: A step-by-step treatment manual. 4. New York: Guilford Press; 2008. [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. Journal of American Medical Association. 2000;283:2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Blais MA. Clinician ratings of the five-factor model of personality and the DSM-IVpersonality disorders. Journal of Nervous and Mental Disease. 1997;185:388–393. doi: 10.1097/00005053-199706000-00005. [DOI] [PubMed] [Google Scholar]
- Bouton ME, Mineka S, Barlow DH. A modern learning theory perspective on the etiology of panic disorder. Psychological Review. 2001;108:4–32. doi: 10.1037/0033-295x.108.1.4. [DOI] [PubMed] [Google Scholar]
- Brawman-Mintzer O, Lydiard RB, Emmanuel N, Payeur R, Johnson M, Roberts J, Jarrell MP, Ballenger JC. Psychiatric comorbidity in patients with generalized anxiety disorder. American Journal of Psychiatry. 1993;150:1216–1218. doi: 10.1176/ajp.150.8.1216. [DOI] [PubMed] [Google Scholar]
- Brown TA. Validity of the DSM-III-Rand DSM-IVclassification systems for anxiety disorders. In: Rapee RM, editor. Current controversies in the anxiety disorders. New York: Guilford Press; 1996. pp. 21–45. [Google Scholar]
- Brown TA. Temporal course and structural relationships among dimensions of temperament and DSM-IVanxiety and mood disorder constructs. Journal of Abnormal Psychology. 2007;116:313–328. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Diagnostic comorbidity in panic disorder: Effect on treatment outcome and course of comorbid diagnoses following treatment. Journal of Consulting and Clinical Psychology. 1995;63:408–418. doi: 10.1037//0022-006x.63.3.408. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Comorbidity among anxiety disorders: Implications for treatment and DSM-IV. Journal of Consulting and Clinical Psychology. 1992;60:835–844. doi: 10.1037//0022-006x.60.6.835. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Classification of anxiety and mood disorders. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. pp. 292–327. [Google Scholar]
- Brown TA, Barlow DH. Categorical vsdimensional classification of mental disorders in DSM-Vand beyond. Journal of Abnormal Psychology. 2005;114:551–556. doi: 10.1037/0021-843X.114.4.551. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH, Liebowitz MR. The empirical basis of generalized anxiety disorder. American Journal of Psychiatry. 1994;151:1272–1280. doi: 10.1176/ajp.151.9.1272. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IVanxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IVanxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IVanxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Brown TA, McNiff J. Specificity of autonomic arousal to DSM-IV panic disorder and posttraumatic stress disorder. Behaviour Research and Therapy. doi: 10.1016/j.brat.2009.02.016. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In: Gross JJ, editor. Handbook of emotion regulation. New York: Guilford Press; 2007. pp. 542–560. [Google Scholar]
- Campbell-Sills LA, Liverant G, Brown TA. Psychometric evaluation of the Behavioral Inhibition/Behavioral Activation Scales (BIS/BAS) in large clinical samples. Psychological Assessment. 2004;16:244–254. doi: 10.1037/1040-3590.16.3.244. [DOI] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, Joormann J. Serotonergic function, two-mode models of self-regulation, and vulnerability to depression: What depression has in common with impulsive aggression. Psychological Bulletin. 2008;134:912–943. doi: 10.1037/a0013740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. Journal of Personality and Social Psychology. 1994;67:319–333. [Google Scholar]
- Chorpita BF, Barlow DH. The development of anxiety: The role of control in the early environment. Psychological Bulletin. 1998;124:3–21. doi: 10.1037/0033-2909.124.1.3. [DOI] [PubMed] [Google Scholar]
- Clark DM. A cognitive approach to panic. Behaviour Research and Therapy. 1986;24:461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clark LA, Vittengl J, Kraft D, Jarrett RB. Separate personality traits from states to predict depression. Journal of Personality Disorders. 2003;17:152–172. doi: 10.1521/pedi.17.2.152.23990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Personality in adulthood: A six-year longitudinal study of self-reports and spouse ratings on the NEO Personality Inventory. Journal of Personality and Social Psychology. 1988;54:853–863. doi: 10.1037//0022-3514.54.5.853. [DOI] [PubMed] [Google Scholar]
- Diener E, Seligman MEP. Very happy people. Psychological Science. 2002;13:81–84. doi: 10.1111/1467-9280.00415. [DOI] [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) New York: Oxford University Press; 1994. [Google Scholar]
- Di Nardo PA, Moras K, Barlow DH, Rapee RM, Brown TA. Reliability of DSM-III-Ranxiety disorder categories using the Anxiety Disorders Interview Schedule-Revised (ADIS-R) Archives of General Psychiatry. 1993;50:251–256. doi: 10.1001/archpsyc.1993.01820160009001. [DOI] [PubMed] [Google Scholar]
- Eley TC, Brown TA. Phenotypic and genetic/environmental structure of anxiety and depressive disorder symptoms in adolescence. 2009. Mansucript submitted for publication. [Google Scholar]
- Eysenck HJ. A model for personality. New York: Springer; 1981. [Google Scholar]
- Fairholme CP, Boisseau CL, Ellard KK, Ehrenreich JT, Barlow DH. Emotions, emotion regulation, and psychological treatment: A unified perspective. In: Kring AM, Sloan DM, editors. Emotion regulation and psychopathology. New York: Guilford Press; in press. [Google Scholar]
- Fanous A, Gardner CO, Prescott CA, Cancro R, Kendler KS. Neuroticism, major depression, and gender: A population-based twin study. Psychological Medicine. 2002;32:719–728. doi: 10.1017/s003329170200541x. [DOI] [PubMed] [Google Scholar]
- First MB. Clinical utility: A prerequisite for the adoption of a dimensional approach in DSM. Journal of Abnormal Psychology. 2005;114:560–564. doi: 10.1037/0021-843X.114.4.560. [DOI] [PubMed] [Google Scholar]
- First MB, Pincus HA, Levine JB, Williams JBW, Ustun B, Peele R. Clinical utility as a criterion for revising psychiatric diagnoses. American Journal of Psychiatry. 2004;161:946–954. doi: 10.1176/appi.ajp.161.6.946. [DOI] [PubMed] [Google Scholar]
- Fowles DC. A motivational theory of psychopathology. In: Spaulding W, editor. Nebraska Symposium on Motivation: Integrated views of motivation, cognition, and emotion. Vol. 41. Lincoln, NE: University of Nebraska Press; 1994. pp. 181–238. [PubMed] [Google Scholar]
- Fulker DW. The genetic and environmental architecture of psychoticism, extroversion, and neuroticism. In: Eysenck HJ, editor. A model for personality. New York: Springer-Verlag; 1981. pp. 88–122. [Google Scholar]
- Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, Poulton R. Obsessions and compulsions in the community: Prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. American Journal of Psychiatry. 2009;166:329–336. doi: 10.1176/appi.ajp.2008.08071006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershuny BS, Sher KJ. The relation between personality and anxiety: Findings from a 3-year prospective study. Journal of Abnormal Psychology. 1998;107:252–262. doi: 10.1037//0021-843x.107.2.252. [DOI] [PubMed] [Google Scholar]
- Gilbert DT. Stumbling on happiness. New York: Knopf; 2006. [Google Scholar]
- Gross JJ, editor. Handbook of emotion regulation. New York: Guilford Press; 2007. [Google Scholar]
- Gruber J, Johnson SL, Oveis C, Keltner D. Risk for mania and positive emotional responding: Too much of a good thing? Emotion. 2008;8:23–33. doi: 10.1037/1528-3542.8.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, Kendler KS. Genetic and environmental sources of covariation between generalized anxiety disorder and neuroticism. American Journal of Psychiatry. 2004;161:1581–1587. doi: 10.1176/appi.ajp.161.9.1581. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Gruber J, Eisner LR. Emotion and bipolar disorder. In: Rottenberg J, Johnson SL, editors. Emotion and psychopathology: Bridging affective and clinical science. Washington, DC: American Psychological Association; 2007. pp. 123–150. [Google Scholar]
- Jones JC, Barlow DH. The etiology of posttraumatic stress disorder. Clinical Psychology Review. 1990;10:299–328. [Google Scholar]
- Kasch KL, Rottenberg J, Arnow BA, Gotlib IH. Behavioral activation and inhibition systems and the severity and course of depression. Journal of Abnormal Psychology. 2002;111:589–597. doi: 10.1037//0021-843x.111.4.589. [DOI] [PubMed] [Google Scholar]
- Keane TM, Barlow DH. Posttraumatic stress disorder. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. pp. 418–453. [Google Scholar]
- Kendell RE. The role of diagnosis in psychiatry. Oxford: Blackwell; 1975. [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Major depression and generalized anxiety disorder: Same genes, (partly) different environments? Archives of General Psychiatry. 1992;49:716–722. doi: 10.1001/archpsyc.1992.01820090044008. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, Yonkers KA. Comorbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. Psychological Medicine. 2008;38:365–374. doi: 10.1017/S0033291707002012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence AE, Brown TA. Differentiating generalized anxiety disorder from anxiety disorder not otherwise specified. Journal of Nervous and Mental Disease. doi: 10.1097/NMD.0b013e3181c29992. in press. [DOI] [PubMed] [Google Scholar]
- Lawrence AE, Liverant GI, Rosellini AJ, Brown TA. Generalized anxiety disorder within the course of major depressive disorder: Examining the utility of the DSM-IV hierarchy rule. 2009. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Zhang S, Preacher KJ. On the practice of dichotomization of quantitative variables. Psychological Methods. 2003;7:19–40. doi: 10.1037/1082-989x.7.1.19. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Fyer AJ, Martin LY, Gallops MS, Endicott J, Gorman JM, Liebowitz MR, Klein DF. Reliability of anxiety assessment: I. Diagnostic agreement. Archives of General Psychiatry. 1989;46:1093–1101.9. doi: 10.1001/archpsyc.1989.01810120035007. [DOI] [PubMed] [Google Scholar]
- Maser JD, Cloninger CR, editors. Comorbidity of mood and anxiety disorders. Washington, DC: American Psychiatric Press; 1990. [Google Scholar]
- Meyer B, Johnson SL, Winters R. Responsiveness to threat and incentive in bipolar disorder: Relations of the BIS/BAS scales with symptoms. Journal of Psychopathology and Behavioral Assessment. 2001;23:133–143. doi: 10.1023/A:1010929402770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Moras K, Clark LA, Katon W, Roy-Byrne P, Watson D, Barlow DH. Mixed anxiety-depression. In: Widiger TA, Frances AJ, Pincus HA, Ross R, First MB, Davis WW, editors. DSM-IV sourcebook. 2. Washington DC: American Psychiatric Association; 1996. pp. 623–643. [Google Scholar]
- Moses EB, Barlow DH. A new unified treatment approach for emotional disorders based on emotion science. Current Directions in Psychological Science. 2006;15:146–150. [Google Scholar]
- Nathan PE, Gorman JM, editors. A guide to treatments that work. 3. New York: Oxford University Press; 2007. [Google Scholar]
- Parkinson L, Rachman S. Intrusive thoughts: The effects of an uncontrived stress. Advances in Behaviour Research and Therapy. 1981;3:111–118. [Google Scholar]
- Rachman S, de Silva P. Abnormal and normal obsessions. Behaviour Research and Therapy. 1978;16:233–248. doi: 10.1016/0005-7967(78)90022-0. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Sanderson WC, Barlow DH. Social phobia features across the DSM-III-Ranxiety disorders. Journal of Psychopathology and Behavioral Assessment. 1988;10:287–299. [Google Scholar]
- Samuel DB, Widiger TA. Clinician’s judgments of clinical utility: A comparison of the DSM-IVand five-factor models. Journal of Abnormal Psychology. 2006;115:298–308. doi: 10.1037/0021-843X.115.2.298. [DOI] [PubMed] [Google Scholar]
- Sanderson WC, Di Nardo PA, Rapee RM, Barlow DH. Syndrome comorbidity in patients diagnosed with a DSM-III-Ranxiety disorder. Journal of Abnormal Psychology. 1990;99:308–312. doi: 10.1037//0021-843x.99.3.308. [DOI] [PubMed] [Google Scholar]
- Sprock J. Dimensional versus categorical classification of prototypic and nonprototypic cases of personality disorder. Journal of Clinical Psychology. 2003;59:991–1014. doi: 10.1002/jclp.10184. [DOI] [PubMed] [Google Scholar]
- Steenkamp M, McLean CP, Arditte KA, Litz BT. Assessment of adults exposed to trauma. In: Antony MM, Barlow DH, editors. Handbook of assessment, treatment planning, and outcome evaluation: Empirically supported strategies for psychological disorders. 2. New York: Guilford Press; in press. [Google Scholar]
- Suárez L, Bennett S, Goldstein C, Barlow DH. Understanding anxiety disorders from a “triple vulnerabilities” framework. In: Antony MM, Stein MB, editors. Oxford handbook of anxiety and related disorders. New York: Oxford; 2009. pp. 153–172. [Google Scholar]
- Taylor S. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- Tellegen A. Structures of mood and personality and their relevance to assessing anxiety with an emphasis on self-report. In: Tuma AH, Maser JD, editors. Anxiety and the anxiety disorders. Hillsdale, NJ: Erlbaum; 1985. pp. 681–706. [Google Scholar]
- Tellegen A, Lykken DT, Bouchard TJ, Wilcox KJ, Segal NL, Rich S. Personality similarity in twins reared apart and together. Journal of Personality and Social Psychology. 1988;54:1031–1039. doi: 10.1037//0022-3514.54.6.1031. [DOI] [PubMed] [Google Scholar]
- Verheul R. Clinical utility of dimensional models for personality pathology. Journal of Personality Disorders. 2005;19:283–302. doi: 10.1521/pedi.2005.19.3.283. [DOI] [PubMed] [Google Scholar]
- Viken RJ, Rose RJ, Kaprio J, Koskenvuo M. A developmental genetic analysis of adult personality: Extraversion and neuroticism from 18 to 59 years of age. Journal of Personality and Social Psychology. 1994;66:722–730. doi: 10.1037//0022-3514.66.4.722. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin. 1984;96:465–490. [PubMed] [Google Scholar]
- Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to the anxiety and depressive disorders. Journal of Abnormal Psychology. 1988;97:346–353. doi: 10.1037//0021-843x.97.3.346. [DOI] [PubMed] [Google Scholar]
- White KS, Barlow DH. Panic disorder and agoraphobia. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. pp. 328–379. [Google Scholar]
- Widiger TA. Categorical versus dimensional classification: Implications from and for research. Journal of Personality Disorders. 1992;6:287–300. [Google Scholar]
- Widiger TA, Costa PT, McCrae RR. A proposal for Axis II: Diagnosing personality disorders using the five-factor model. In: Costa PT, Widiger TA, editors. Personality disorders and the five-factor model of personality. 2. Washington, DC: American Psychological Association; 2002. pp. 431–456. [Google Scholar]
- Widiger TA, Samuel DB. Diagnostic categories or dimensions: A question for DSM-V. Journal of Abnormal Psychology. 2005;114:494–504. doi: 10.1037/0021-843X.114.4.494. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Verheul R, van den Brink W. Personality and psychopathology. In: Pervin LA, John OP, editors. Handbook of personality: Theory and research. New York: Guilford Press; 1999. pp. 347–366. [Google Scholar]
- Williams JBW, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, Howes MJ, Kane J, Pope HG, Rounsaville B, Wittchen H. The Structured Clinical Interview for DSM-III-R(SCID) II. Multisite test-retest reliability. Archives of General Psychiatry. 1992;49:630–636.2. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I. Generalized anxiety disorder in patients with major depression: Is DSM-IV’s hierarchy correct? American Journal of Psychiatry. 2003;160:504–521. doi: 10.1176/appi.ajp.160.3.504. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Barlow DH, Liebowitz M, Street L, Broadhead E, Katon W, et al. The DSM-IV field trial for mixed anxiety-depression. American Journal of Psychiatry. 1994;151:1153–1162. doi: 10.1176/ajp.151.8.1153. [DOI] [PubMed] [Google Scholar]