Abstract
Common causes of blindness are diseases that affect the ocular structures, such as glaucoma, retinitis pigmentosa, and macular degeneration, rendering the eyes no longer sensitive to light. The visual pathway, however, as a predominantly central structure, is largely spared in these cases. It is thus widely thought that a device-based prosthetic approach to restoration of visual function will be effective and will enjoy similar success as cochlear implants have for restoration of auditory function. In this article the authors review the potential locations for stimulation electrode placement for visual prostheses, assessing the anatomical and functional advantages and disadvantages of each. Of particular interest to the neurosurgical community is placement of deep brain stimulating electrodes in thalamic structures that has shown substantial promise in an animal model. The theory of operation of visual prostheses is discussed, along with a review of the current state of knowledge. Finally, the visual prosthesis is proposed as a model for a general high-fidelity machine-brain interface.
Keywords: visual prosthesis, deep brain stimulation, visual function
In this article we review the current state of visual prosthetics with particular attention to the approaches that include neurosurgical methodologies.
Background: Causes of Blindness
Blindness has many causes, from diseases of the eye to cancer and TBI. With causes that affect only the sensory organ, and therefore induce blindness by interfering with the normal translation of incoming light to neural activity, the remainder of the visual pathway is often largely intact in individuals with previously normal visual function.30 The field of visual prosthetics seeks to develop devices to restore lost, or to support failing, visual function. In contemporary approaches, a man-made imaging device, nominally silicon based, is used to translate visual scenes into electrical activity that gets applied in coordinated form at some point along the early visual pathway. The primary differences between the various efforts, of which there are currently some 2 dozen, rest upon where external stimulation is applied to the visual pathway.
Evaluating Points Along the Early Visual Pathway as Stimulation Targets
There are 6 locations along the visual pathway with potential for functional restoration of sight through microstimulation as depicted in Fig. 1: the retina, the optic nerve, the optic tract, the dorsal LGN of the thalamus, the optic radiation, and the primary visual cortex. The following paragraphs will briefly assess the advantages and disadvantages of each location, and are summarized in Table 1.
Fig. 1.
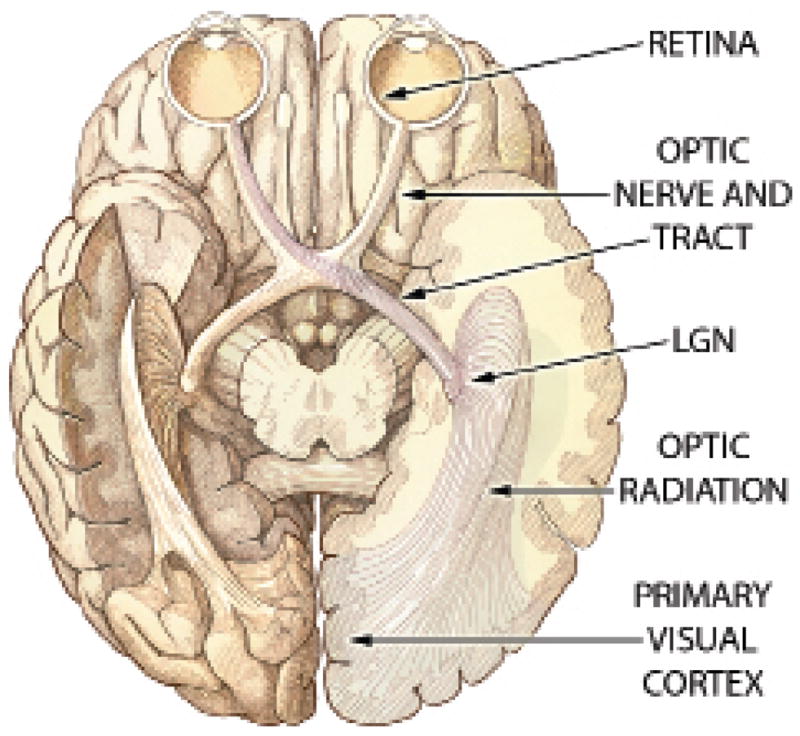
Illustration showing the early visual pathway. Ventral view of the human brain illustrating the early visual pathway from retina through primary visual cortex. Labeled structures are evaluated in the text as potential stimulation targets for a visual prosthesis.
TABLE 1.
Summary of the advantages and disadvantages of the 6 potential target sites for a visual prosthesis along the early visual pathway from retina to primary visual cortex*
| Location | Advantages | Disadvantages |
|---|---|---|
| retina | extracranial, gaze compensation, simple encoding, full visual field | contraindicated in glaucoma/trauma, high resolution not possible?, very delicate, acceleration forces (not stable), luminance only? |
| optic nerve | stable, extracranial, simple encoding, full visual field | poorly organized, atrophies in many diseases, requires gaze information |
| optic tract | stable, simple encoding | deep, poorly organized, visual hemifield, atrophies in many diseases, requires gaze information |
| LGN | stable, compact, highly organized, M/P/K separation, colors possible?, simple encoding? | deep, compact, visual hemifield, corticothalamic projections, requires gaze information |
| optic radiation | stable, simple encoding? | deep, not compact, visual hemifield, requires gaze information |
| striate cortex (V1) | stable?, large, at surface | often completely within CF, large craniotomy?, some portions in sulci, visual hemifield, complex neural encoding, requires gaze information |
M/P/K refers to the magnocellular, parvocellular, and koniocellular subdivisions of the early visual pathway.
CF refers to the calcarine fissure.
Retina
When blindness is caused by a disease of the photoreceptor cells in the eye, stimulating the remaining healthy cells of the retina, especially the output layer of ganglion cells, is a potential avenue for restoration of function. In cases in which the damage includes the ganglion cells, it is unlikely that this avenue will be fruitful.
Determining whether the ganglion cells are viable can be done with a simple noninvasive test that applies electrical stimulation between a large electrical contact on the eyelid and another at the rear of the skull.4,20
Surgery of the eye to implant arrays of electrode contacts has been under significant development but is still considered experimental.28,41,55,77 The most advanced techniques involve a maintained defect of the globe through which a flat cable passes; there are, however, some projects in which the entirety of circuitry is contained within the globe13,80 or in which the entirety of circuitry is external to the globe.14 For efforts in which the electrodes are placed on the vitreal surface of the retina, so-called epiretinal implants, a small tack is typically used to hold the array fixed against the retina,40 while for efforts in which electrodes are placed at the pigment epithelium surface of the retina, so-called subretinal implants, the electrode array is placed behind the retina, in the subretinal space.13,68,90
Advantages of retinal approaches include that the implantation surgery is entirely extracranial, that a single eye can be implanted with potential coverage of the entire visual field, that there is an even mapping of visual space to the retinal surface, and that, for approaches in which the man-made optical sensor is implanted within the eye or the optics of the eye are still used for imaging, there is no need for tracking eye position to compensate for gaze shifts (see below for a discussion of gaze compensation).
Disadvantages of retinal approaches include the temperamental delicacy of the retina, the requirements to engineer devices that must cope with the limited space available in the eye, and significant weight restrictions to prevent the normal but large acceleration forces as the eyes move about in the orbit from changing the implant-to-retina geometries or, worse, causing damage by pulling at the retina. Furthermore, because of the architectural detail of the fovea at the center of the visual field where the ganglion cell bodies stack up 5–7 layers deep, high-resolution artificial vision may not be possible. Published accounts of human retinal microstimulation to date suggest that it may be possible to convey only luminance information with retinal approaches.39,40,69 And, importantly, while the second and third most common causes of blindness in developed countries, retinitis pigmentosa and macular degeneration, spare the ganglion cells sufficiently to allow treatment with a retinal prosthesis, the most common cause of blindness in developed countries is glaucoma, which affects the ganglion cells, contraindicating a retinal approach.71
Because of the substantial advantages, and despite the substantial disadvantages, the most advanced visual prosthesis projects use the retinal approach, and 4 projects are currently in clinical trials,24,79 suggesting the likelihood that the first visual prosthesis device to market will be a retinal prosthesis.78 While details vary across these 4 projects,35,38,54,89 researchers are currently implanting prostheses with 25–60 electrodes in short- and long-term experiments with volunteers who are blind, including at least 1 Phase II trial in the US (Argus II Retinal Stimulation System Feasibility Protocol, ClinicalTrials.gov NCT00407602). The results generally point to well-tolerated materials,28,46,47,51 little to no tissue alteration from stimulation,25 and at least crude levels of functional restoration. The individuals are reportedly able to recognize objects or patterns67,86,91 and have increased mobility.38
Optic Nerve
In cases of blindness in which the optic nerve is intact, such as the conditions in which a retinal approach is indicated, stimulation can be applied to the optic nerve directly, rather than to the retina, to create phosphenes. One group is pursuing a multicontact cuff-style electrode,4 and 2 are pursuing multiple penetrating microelectrodes.49,72
Advantages of the optic nerve include a relatively straightforward, extracranial surgical approach that provides access to the entire visual field. Despite a possible lack of fine-scale organization of the optic nerve, there is a general organization, leading to the ability to steer percept locations by adjusting electrical bias between different electrodes.88 However, the current cuff-style approach has a highly limited electrode count, and thus has a questionable potential for restoring high-resolution vision. Nevertheless, the minimally invasive surgery required for implantation, mechanical stability, and surprising functional flexibility demonstrated by experiments in pilot studies with volunteers thus far have suggested that this straightforward approach should not be discounted.
At least 2 groups are using penetrating microelectrodes in the optic nerve.49,72 This slightly more invasive approach shares the advantages of the cuff approach and brings along the potential for high contact count and therefore high resolution vision, making it also promising. While these groups are primarily working in animal models, there have been reports of acute experiments in humans with positive results.73
Optic Tract
Located within the cranium and posterior to the optic chiasm, the optic tract combines signals from single visual hemifields of both eyes. As of this writing, it has not been rigorously explored as a potential stimulation target; given that it has many of the disadvantages of the optic nerve combined with disadvantages of the LGN (see below) and few of the advantages of either, while microstimulation of the optic tract would be expected to produce phosphenes, it is unlikely to be a fruitful location to target an electrode array for prosthetic purposes.
Lateral Geniculate Nucleus
Even when there is substantial damage to the eye and possible atrophy of the optic nerve, the LGN remains largely intact.30 Therefore, stimulation of the LGN has the potential to be a viable treatment approach for many causes of blindness, including the most prevalent ones71 as well as blindness caused by trauma to the eye or surgical enucleation. Approximately 10 mm away from the LGN are structures such as the subthalamic nucleus and substantia nigra that are accessed using surgical techniques from DBS for electrical stimulation treatment of movement disorders,19,48,50 suggesting that the same DBS techniques could be used to place stimulating electrodes in the LGN.
Advantages of the LGN as a stimulation target include its deep, central structure, so that electrodes would be stable once placed. The area itself is compact, ~ 10 mm across, so that once an electrode is placed, the full extent of the visual field is accessible. The signals are relatively simple, reflecting the primary input from the retina, and maintain much of the same representation. It is the only portion of the visual stream in which the main subdivisions, the magnocellular, parvocellular, and koniocellular pathways, are macroscopically separated (see below), suggesting that additional functionality might be more amenable to restoration from an LGN approach than other approaches.
Disadvantages of the LGN are that it is located behind the optic chiasm where the visual field becomes vertically segregated, such that each LGN represents only 1 of the 2 hemifields. Therefore, a full visual field prosthesis would necessitate bilateral LGN implants. Stimulation in the LGN would also require image compensation for gaze direction (see below). There is also great uncertainty about the impact of corticothalamic projections and their role in shaping normal ongoing activity, and only limited knowledge about the interaction of microstimulation with ongoing thalamic activity.44
The current state of research into LGN as a stimulation target is discussed in detail below. At present, experiments are being performed in nonhuman primate models.62
Optic Radiation
The optic radiation comprises the efferent projection from the LGN and conveys visual information to the primary visual cortex at the occipital pole. Stimulating the optic radiation for visual prosthetics is a little-explored possibility that would seem to have potential, but as the optic radiation has a complex fan-like 3D structure, the approach suffers substantial disadvantages compared with the LGN. Reports in the literature of optic radiation stimulation are limited to phosphene generation using transcranial magnetic stimulation at the occipital pole that have suggested the visual sensations were caused by magnetic action on the optic radiation.43,52
Primary Visual Cortex
Among the first experiments in visual prosthetics applied microstimulation to the visual cortex as a means to generate patterned phosphenes,7 and investigation continues3,21,22,64,81 (reviewed by Schiller and Tehovnik74). The large physical extent of primary visual cortex makes it attractive for implantation of a large number of electrodes, and, therefore, the area holds the potential for very high resolution restored function, as well as an increased tolerance for the chronic low-grade heating effects of microstimulation. More is understood about the primary visual cortex than perhaps any other brain area (reviewed by Hubel and Wiesel37), revealing a complexity of representation that is substantially more intricate than even one stage previous at the LGN. It is reasonable, therefore, to speculate that it will be more difficult to determine the computations that will be needed to transform a video stream into stimulation signals, and that the computations will themselves be more involved, but this hypothesis may prove wrong as published descriptions of primary visual cortex phosphenes in humans have suggested a relatively simple effect in response to electrical stimulation.2,7,21,75
While none of the disadvantages of the primary visual cortex fundamentally preclude it from being a target for prosthetic use, there are some serious difficulties. The largest difficulty is the location: while the primary visual cortex is a cortical area, and therefore on the surface of the brain, much of the visual field is buried in the calcarine fissure, including, in some individuals, the important foveal representation of central vision.23,83 Furthermore, cortical crenelation creates an uneven accessibility to the parts of the visual field represented on gyral versus sulcal surfaces, and an approach that implants electrodes solely on exposed gyral tissue will miss a large fraction of the visual field. Finally, surface electrodes, even penetrating electrodes that are placed on the surface, show a slow degradation of function over time, hypothesized to be due to micromovements (N. Hatsopoulos, personal communication, 2009).
While electrical microstimulation in extrastriate visual areas produces visual sensations,7,2 the multiple streams that project from the primary visual cortex and the high degree of specialization that emerges even one stage farther along the visual pathway suggest that it will not be productive to explore a visual prosthesis to treat blindness of ocular origin at any stages beyond the primary visual cortex.
While both the seminal experiments in visual prosthetics7 as well as significant follow-up work21,22 placed stimulating electrodes on the surface of human visual cortex, the years since have seen effort concentrated in cat and nonhuman primate models.3,57,74 Most recently, there has been work using virtual reality techniques with sighted humans in preparation for experiments in blind volunteers,74,84 as well as substantial engineering effort to create a complete, portable device.64
Theory of Operation for Visual Prosthetic Devices
The fundamental idea underpinning visual prosthetics is to create an imaging device that, through some artificial means, injects appropriately processed signals into the visual stream (see Fig. 2). While some of the retinal approaches seek to create a device that does little or no image processing or to have no device at all by photosensitizing normal cells,9,29,60,90 most projects have a device that performs a function that is akin to normal retinal image processing. As such, visual prosthetic devices are not unlike bionic eyes: they focus photons onto a light-sensitive surface to create an image, extract salient features from that image, and transmit those features to the brain.
Fig. 2.
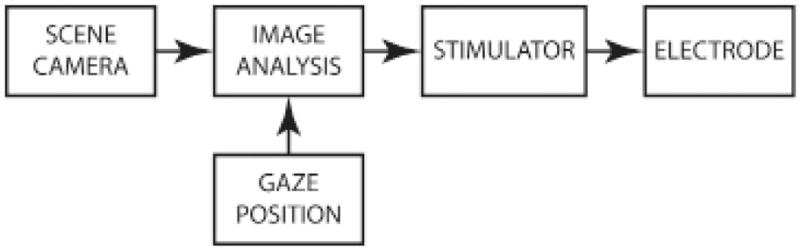
Block diagram of a visual prosthesis. Information flows left to right in this diagram depicting the basic steps in converting a visual scene into patterned stimulation of neural tissue in a visual prosthesis. In contemporary designs, the scene camera, gaze position measurement, and image analysis are external to the body, and wirelessly communicate to chronically implanted multichannel stimulators and multicontact electrodes. Designs that retain the eye as an imaging apparatus do not require gaze position measurement to compensate camera images for movement of the eyes (see main text for discussion of gaze compensation).
In a visual prosthesis device, each electrode contact is typically intended to generate 1 phosphene. If the phosphenes are small and tightly focused, they can be thought of as pixels, although they will likely not be close-packed like in a computer or camera display, but more probably separated by an unstimulated background. Mapping the visual scene to these pixels can be thought of as looking through an opaque screen through which holes have been punched, somewhat like looking through a kitchen colander, although each pixel in a prosthesis will be solid in appearance, or nearly so, and each hole in an opaque screen will show some detail of the scene beyond within the diameter of the hole. Nevertheless, a prosthetic image can be constructed from a collection of pixels where each has been adjusted according to the brightness of the original image, even if there are far fewer pixels in the prosthetic image than in the original, and even if the prosthetic pixels are not arranged in a perfect grid.
How Phosphenes are Distributed in Visual Space
One of the biggest differences in applying stimulation to the retina versus anywhere downstream of the retina is the difference in uniformity of resolution. At the retina, a placement of a regular array of stimulating electrodes, one with an even spacing between contacts, will produce phosphenes that are in a regular pattern across the visual field, just as the pixels in a computer screen form a regular pattern across the screen. However, the primate visual system has a highly nonuniform resolution pattern with ~ 100 times as many photoreceptor cells per square millimeter at the central part of the visual field than at the periphery.5,15,59,65 The biologically compressed density at the retina is relaxed at the optic nerve and the relation is maintained in the LGN, the primary visual cortex, and beyond. During this anatomical decompression, the overall visuotopic relations are retained, so that the fraction of tissue devoted to the central visual field becomes inflated compared with the peripheral field, and an even progression along a neural structure from central to peripheral representations results in an accelerating progression through the visual field.
This retinally created nonuniform representational density is carried through each subsequent stage and gets combined with gaze direction information to create the illusion of uniformly high-resolution vision, despite the highest acuity being only about the point of visual regard.18 A graphic representation of phosphene location in the visual field for a regular grid of electrode contacts in the retina versus the LGN can be seen in Fig. 3. We speculate that a set of phosphenes with an uneven density that matches the endogenous acuity profile of the visual system will be of higher utility than a set of phosphenes with an even visual density.
Fig. 3.
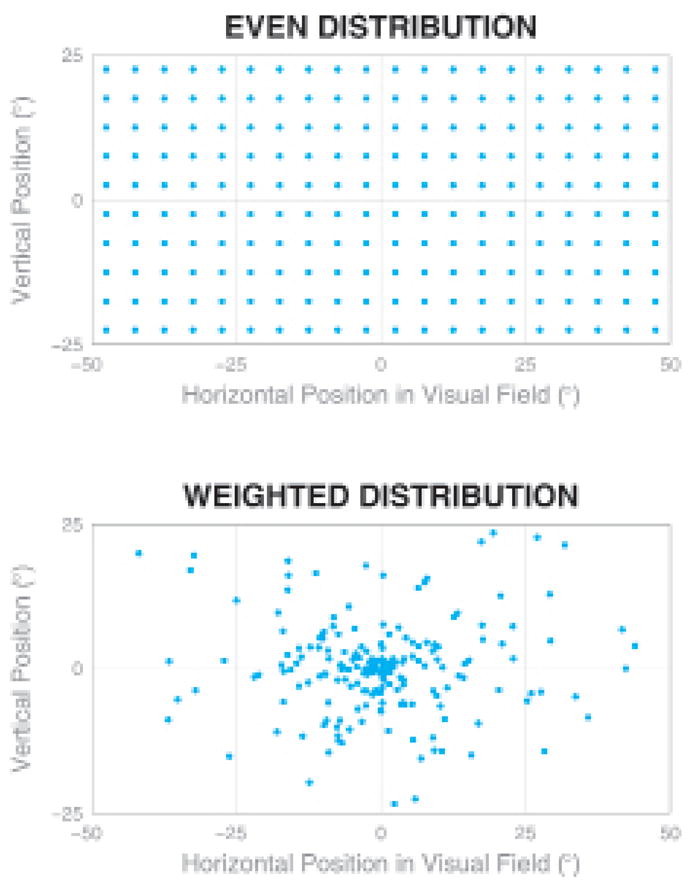
Charts showing simulated phosphene distribution patterns. Vertical and horizontal axes represent the positions along the visual field, and each dot represents a phosphene from an independent electrode contact. While there are equal numbers of contacts in the 2 diagrams, the lower pattern matches the intrinsic acuity profile of the primate visual system, and has a much higher focal acuity than the upper pattern. Upper: When prosthesis electrode contacts are placed on the retina in a regular pattern, the generated phosphenes also appear in a regular pattern across the visual field. Lower: When contacts are placed in a physically regular pattern in tissue downstream of the retina, the phosphenes will appear in a pattern strongly weighted to the center of the visual field.
Compensation for Gaze Direction
The optics of the eye project an image of the external scene onto the retina that changes depending on exactly where the eyes are pointing. For normal, sighted individuals, the eyes move about from one point of visual regard to another 2 to 3 times per second. The visual brain assembles these quick, successive views to create a mental image of a scene by compensating each retinal snapshot with information regarding the direction the eyes were pointing at the time. Although this integration mechanism is not yet fully understood, it is widely hypothesized to require a copy of the motor neuron commands that control eye position, and to occur in cortical areas beyond the primary visual cortex in the visual processing stream. No part of the early visual system, from the retina through the primary visual cortex, shows compensation for eye position.
For the visual prosthesis designer, this observation suggests that to produce as useful a visual experience as possible, the imaging system must deliver stimulation to the brain that includes the effects of changes in eye position on a continuous basis, either by physically re-aiming the camera to point where the eyes are pointing, or by electronic translation of the image. This is somewhat counterintuitive because the brain will undo these changes to produce a stable mental image at a later stage; however, a visual prosthesis must deliver activity as faithful as possible to that produced by the organ it functionally replaces. While some of the retinal prosthesis approaches use the optics of the eye as part of the imaging system13,54,60 and therefore automatically fulfill this criterion, most visual prosthesis designs use a camera mounted on the head or in a set of eyeglasses, and thus require compensation of the image for gaze position.
Patterned Stimulation Across Multiple Electrodes
Retinal and cortical experiments have demonstrated that simultaneous stimulation across multiple electrodes does not necessarily evoke independent phosphenes, and that stimulation of single contacts can sometimes produce a constellation of percepts rather than a single phosphene.69,75 This is problematic for a device that would apply straightforward pinhole-like processing to an image to create a direct visual representation, but there are initial reports of techniques to avoid at least some of the independence issues,36 and suggestions that relaxing the criterion of direct representation may be functionally advantageous.85
Deep Brain Stimulation and the Thalamic Approach to Visual Prosthetics
The LGN is located below the thalamus at Talairach coordinates (22, −23, −5) and (−22 −23, −4).45,53,58 It has a typical size of 250 mm3,1,76,92 although the volume varies by a factor of 2:1 in healthy individuals.34 It has maximum extent of ~ 10 mm along the cardinal axes, with a flattened teardrop form reminiscent of a leg of cured ham.34
The LGN has a laminar structure that carries projections from the 2 eyes, and from the magnocellular (M), parvocellular (P), and koniocellular (K) processing streams. There are typically 3 zones ranging along the anteroposterior axis: a monocular zone with 2 layers (1 magnocellular and 1 parvocellular), a binocular zone with 6 layers (2 magnocellular and 4 parvocellular), and a binocular zone with 4 layers (4 parvocellular).34 Between the magnocellular and parvocellular layers are recently characterized cells that are part of the koniocellular system.33 Although precise functional delineation is difficult in condensed form, generally put, the magnocellular system mediates luminance perception, whereas the parvocellular and koniocellular systems mediate chrominance (color) perception.
Each LGN represents one-half of the visual field, split along the vertical meridian, with a smooth mapping of position within the visual field to anatomical position within the brain area. Progressing along the anteroposterior anatomical axis, the representation moves from peripheral to central visual field. Progressing along the lateromedial axis, the representation moves from upper to lower quadrants.12,66,76 While high-resolution visual mapping of the LGN in macaques has been reported,26 maps of the human LGN have been limited to substantially coarser functional MR imaging methods.12,76 The central 10° of visual angle occupy approximately the posterior half of human LGN.76
As the LGN is the only location within the early visual system where the 3 major pathways (magnocellular, parvocellular, and koniocellular) are macroscopically segregated, it presents the only location where it might be possible to selectively stimulate the 3 pathways, suggesting the possibility of independently controlling luminance and chrominance information.
Based on high-fidelity computer simulations of microwire electrodes placed in the LGN, the physical extent of the area allows for the placement of substantial numbers of fine microwire contacts.63 The most plausible format for implanting large numbers of microwires is to use a mechanism similar to the Ad-Tech Medical Instruments macro-micro system (http://www.adtechmedical.com; see text below and Fig. 4) where a bundle of microwires exits out the distal end of a long cannula. This brush-style electrode would have more flexibility than a rigid structure to compensate for individual variation in LGN morphology, and would ease the need for absolute precision in placement.
Fig. 4.
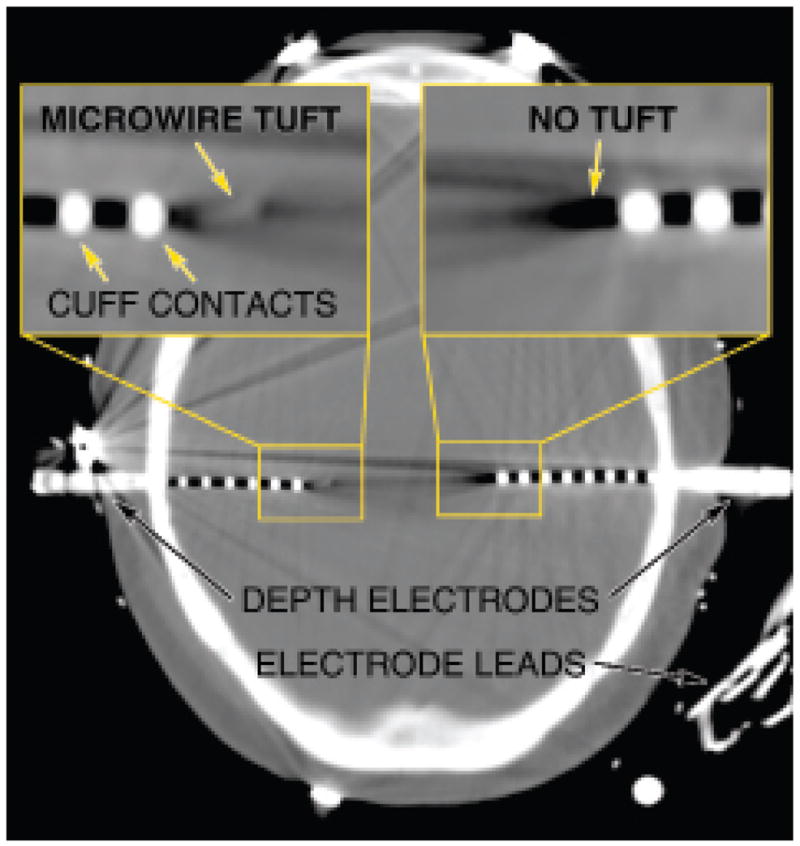
Computed tomography scan showing the implanted depth electrodes. Depth electrodes similar to ones that would be appropriate for use in an LGN-based visual prosthesis are already in clinical use during preparation for surgical treatment of epilepsy such as shown in this image obtained in a patient with bilaterally implanted hippocampus. Left inset: A depth electrode that combines traditional cuff-style contacts with a central bundle of microwires exiting distally. Right inset: A traditional depth electrode without the central bundle.
From published studies in an animal model,62 we know that microstimulation of the LGN can be used to produce small pixel-like phosphenes, and, moreover, the placement of a phosphene in the visual field is determined by the exact anatomical location of the stimulating electrode. Furthermore, experimental animals were able to immediately integrate artificially created percepts into a visual task. Not surprisingly, slightly displaced electrodes could be used to create visually separated phosphenes when stimulated in randomly alternating fashion. However, to date, patterned stimulation across multiple electrodes intended to produce a coherent percept has not been attempted in the LGN.
Mapping Paradigms
Knowledge of the location of each phosphene in visual space is required during a normal prosthesis operation to evaluate the camera images and generate stimulation for each electrode contact according to the location of the phosphene it generates. Because traditional mapping of LGN retinotopy using optically presented stimuli with electrophysiological recordings or functional MR imaging methods to measure neural activity is not readily possible with blind individuals, determination of the visual location of the phosphenes generated by each electrode tip requires a different mapping methodology. Various paradigms have been suggested,7,17,27,56,75,88 most of which have the patient refer visual events to points or regions on a surface at approximately arm’s length. For high-resolution devices with high pixel counts, this task may prove tedious, and a more efficient method will become necessary.
Particular Design Requirements for a Thalamic-Based Device
As the eye moves in the socket, causing gaze position to scan across the visual scene, the brain uses eye position information to build up a composite visual image based on each gaze location. For visual prostheses that have a camera fixed relative to the head, for example, mounted in a pair of eyeglasses, the camera will not track the patient’s eye position, and therefore, eye position will need to be separately measured and the camera image translated to compensate for eye movements. This compensation for gaze direction can be eliminated if the camera is implanted within the eye.
Description of Intended Surgical Implantation
The probable procedure for implantation of a thalamic visual prosthesis electrode and stimulator follows that for traditional DBS implantation. Patients would be placed in a stereotactic frame, or a frameless system could be used. After MR and CT imaging, the target structure would be localized and the approach planned. A bur hole would be placed at the level of the coronal suture. Intraoperative microelectrode recordings would be used to verify the location of LGN based on functional landmarks found while recording through overlying structures, and through microstimulation within LGN to generate phosphenes. The outer electrode casing, similar to a traditional DBS electrode, is then implanted down to a few millimeters above the LGN, and the implanting stylette is withdrawn. A microwire bundle is inserted through the core of the DBS electrode, protected within a cannula until it is near the final position, at which point it is slowly advanced into tissue and the microwires splay out as they exit the protective encasement. Intraoperative assessment of position will be done by microstimulation testing. The electrode lead is then routed subcutaneously to a subclavicular or cranial stimulator.
Open Questions and Contraindications
The field of visual prosthetics has been concentrating on treatments for individuals who have lost sight in adulthood. In part, this is due to the prevalence of acquired blindness in late adulthood, but also because of the rich experimental literature demonstrating the essential role of visual experience in the development of normal visual function, and the uncertainty the lack of normal development would cast upon results from congenitally blind individuals fitted with visual prostheses. However, it is an open question as to whether the higher neural plasticity associated with youth might make congenitally blind children appropriate candidates.
While there have been many studies attempting to evaluate the number of independent phosphenes required to perform selected tasks such as visual navigation or reading,6,8,11,16,31,32,75,79,82,87 a clear determination of the minimum number of phosphenes that would be useful to the patient, or that would justify the risks associated with implantation of a device, has not been reached. There is little consensus due, in part, to the wide range of assessment criteria, modalities, and experimental tasks that have been used. A few researchers have reported their findings in units of acuity, such as the standard Snellen 20/x units used in ophthalmology, but even then, as the distribution of phosphenes used typically provides incomplete or sporadic coverage of the visual field with many approaches, these assessments are not deeply meaningful. It has been suggested that a few hundred pixels are required for navigation,8,16 facial recognition,11,82 and reading.6,32,79 A preliminary simulation study has suggested that 500 pixels across the entire visual field following an endogenous pattern can provide ~ 20/1200 visual acuity (J. Pezaris, unpublished data; see also Fig. 3). In coarse terms, it appears that restoration of vision capable of perceiving form requires a minimum of ~ 100 pixels, while smaller numbers of pixels may still provide benefit to the blind patient.
Although the straightforward and direct mapping of visual scene according to phosphene location would seem a reasonable approach, it requires an accurate assessment of phosphene location. For a device with many hundreds or thousands of stimulation contacts, such measurements may be impractical. It remains an open question as to what extent an approximate initial assessment of phosphene location is sufficient for the visual system to create an interpretable image, and over longer timescales to what extent neural plasticity is able to compensate for phosphene map inaccuracies.
Based on the current understanding of the visual system, the primary contraindication for a thalamic visual prosthesis is cortical blindness such as that due to TBI involving the occipital pole. The early visual system forms an obligate chain so that injury at any point precludes treatment at an earlier, more peripheral stage. Thus, an optic nerve neuropathy contraindicates treatment with a retinal prosthesis, but it does not preclude treatment with a thalamic prosthesis. Similarly TBI with primary visual cortex involvement contraindicates retinal, thalamic, as well as primary visual cortical approaches.
Current State of the Thalamic Visual Prosthesis
At present, microstimulation in the LGN has been used to produce individual pixel-like phosphenes, and it has been hypothesized that, like with other approaches, patterned stimulation across multiple contacts in LGN has the potential to produce a coherent image.62 While brush-style electrodes are readily available with low contact counts from companies like Ad-Tech Medical Instruments, it is unknown exactly how many electrodes will be manufacturable with the same technology (see below). Currently, integration of a camera with an image processing system and stimulator to drive a high contact count electrode to create coherent images is under active development. Furthermore, studying the characteristics of artificial vision from a thalamic prosthesis both in animal models and with healthy human volunteers using a virtual reality simulator is an area of active research.
The number of electrode tips that would fit into human LGN depends on the average tip density and the volume of the area, and has been analyzed in a recent publication.63 The size of the LGN in humans is ~ 250 mm3, with a maximum extent of ~ 10 mm, and with the central 10° of visual space occupying the posterior half (see above). With a spacing of 1 mm in 3 dimensions, ~ 250 electrode tips could be placed per hemisphere (for 500 phosphenes total across both visual hemifields) that would occupy 0.6% of the volume of the area, if 40-μm-diameter wires were used.63 This compares favorably with other technologies that are currently used for chronic neural implants, such as the Utah array42 at 1% of sampled volume, and Medtronic (http://www.medtronic.com) DBS electrodes that when placed in, for example, the globus pallidus or substantia nigra, 2 structures anatomically located near the LGN, occupying 0.7 and 3% of the areas, respectively.63
In the laboratory, experimental brush microwire electrodes with 8 contacts have been inserted into the monkey LGN and have been used to create multiple individual phosphenes, although only one at a time,62 and similar 16-contact electrodes have been used for recording.61 It is currently possible to procure deep brain brush electrodes with a combination of 8 microwire contacts and 4 cuff contacts, to custom-order electrodes with 20 microwire contacts, and it may be possible to manufacture electrodes with a few hundred microwires (personal communication, Ad-Tech Medical, 2009). It is important to recognize that these commercially produced electrodes have not been approved by the FDA for stimulation through their microwire contacts.
The technological barriers to creating a thalamic visual prosthesis are relatively low. Video cameras of sufficient quality and size are a commodity item, as the circuitry is found in contemporary webcams. Hand-held computers with sufficient computational horsepower for real-time video analysis are commonly found in the guise of personal audio and video players. Multichannel stimulators that can be adapted to thalamic prosthesis use are currently undergoing Phase II clinical trials (such as from the Argus II device). Chronic implantation of DBS electrodes has gained wide acceptance as a standard treatment methodology that is considered safe and effective.10,19,70 The primary technical hurdle is development of an electrode technology that is optimized for thalamic prosthesis use, with brush-style contacts or their equivalent, and integration of a full camera-to-electrode system. Independent of the development of brush-style electrodes, it should be possible to use standard 4-contact cuff-style DBS electrodes, such as those manufactured by Medtronic, to restore 8-pixel vision with a bilateral implant; whether the resultant, comparatively simple, and low-resolution prosthesis would provide sufficient benefit to justify the risks associated with DBS therapy requires further study.
The scientific and medical barriers to a pilot study in humans are also relatively low but require careful attention. Of primary scientific interest are the questions of how well-coordinated stimulation across multiple electrodes in LGN works to create coherent, interpretable percepts of objects rather than just points of light, and how to translate from video image to electroneural stimulation to maximize effectiveness of the new sensory modality. From a medical perspective, the effects of chronic implantation of deep microwires are unknown, along with the effects of chronic microstimulation in the thalamus. While we anticipate that a functioning thalamic visual prosthesis system will be demonstrated in a nonhuman primate model in a matter of months, it may be some years before a device based on this approach appears frequently in clinical use.
Other Applications for Technology Developed for Visual Prostheses
Other potential applications for brush-style electrodes appropriate for use with thalamic visual prostheses include high fidelity interfaces into other brain areas for more subtle and responsive control of or modification to ongoing activity. While the creation of a visual prosthesis to treat blindness is an important aim, approaches that apply stimulation to central structures such as the LGN or primary visual cortex have potential applicability in other areas as well. The visual prosthesis becomes a model interface for systems that target other brain areas, not only for restoration of sensory function, but potentially for improved treatment for pathologies such as movement disorders, epilepsy, and addiction.
Conclusions
Visual prosthetics is the field of investigation for devices that provide restoration of function to blind individuals in whom the blindness is caused by disease or defect of the eye as a sensory organ. In cases in which the early visual system is intact, 6 distinct structures along the pathway from retina to primary visual cortex provide potential targets for a device-based approach: the retina, the optic nerve, the optic tract, the LGN, the optic radiation, and the primary visual cortex. Each potential target has advantages and disadvantages for patterned electrical microstimulation. Approaches that use retinal targets have advanced to preliminary clinical trials. The LGN and primary visual cortex are targets that would involve bringing neurosurgical methods to bear on device implantation. The thalamic approach in particular is quite similar to current techniques used for DBS treatment of movement disorders and major depression, suggesting that the development of an LGN-based device for restoration of high-fidelity visual function is not limited by surgical access to the target site. Finally, a high-fidelity thalamic visual prosthesis carries the promise of much wider applicability in which control or modification of ongoing brain activity is required.
Abbreviations in this paper
- DBS
deep brain stimulation
- LGN
lateral geniculate nucleus
- TBI
traumatic brain injury
Footnotes
Disclaimer
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Andrews TJ, Halpern SD, Purves SD. Correlated size variations in human visual cortex, lateral geniculate nucleus, and optic tract. J Neurosci. 1997;17:2859–2868. doi: 10.1523/JNEUROSCI.17-08-02859.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bak M, Girvin JP, Hambrecht FT, Kufta CV, Loeb GE, Schmidt EM. Visual sensations produced by intracortical microstimulation of the human occipital cortex. Med Biol Eng Comput. 1990;28:257–259. doi: 10.1007/BF02442682. [DOI] [PubMed] [Google Scholar]
- 3.Bradley DC, Troyk PR, Berg JA, Bak M, Cogan S, Erickson R, et al. Visuotopic mapping through a multichannel stimulating implant in primate V1. J Neurophysiol. 2005;93:1659–1670. doi: 10.1152/jn.01213.2003. [DOI] [PubMed] [Google Scholar]
- 4.Brelén ME, De Potter P, Gersdorff M, Cosnard G, Veraart C, Delbeke J. Intraorbital implantation of a stimulating electrode for an optic nerve visual prosthesis. J Neurosurg. 2006;104:593–597. doi: 10.3171/jns.2006.104.4.593. [DOI] [PubMed] [Google Scholar]
- 5.Brindley GS. Physiology of the Retina and the Visual Pathway. London: Edward Arnold Ltd; 1960. [Google Scholar]
- 6.Brindley GS. The number of information channels needed for efficient reading. J Physiol. 1964;177:44. [Google Scholar]
- 7.Brindley GS, Lewin WS. The sensations produced by electrical stimulation of the visual cortex. J Physiol. 1968;196:479–493. doi: 10.1113/jphysiol.1968.sp008519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cha K, Horch KW, Normann RA. Simulation of a phosphene- based visual field: visual acuity in a pixelized vision system. Ann Biomed Eng. 1992;20:439–449. doi: 10.1007/BF02368135. [DOI] [PubMed] [Google Scholar]
- 9.Chambers JJ, Banghart MR, Trauner D, Kramer RH. Light- induced depolarization of neurons using a modified shaker K+ channel and a molecular photoswitch. J Neurophysiol. 2006;96:2792–2796. doi: 10.1152/jn.00318.2006. [DOI] [PubMed] [Google Scholar]
- 10.Charles PD, Van Blercom N, Krack P, Lee SL, Xie J, Besson G, et al. Predictors of effective bilateral subthalamic nucleus stimulation for PD. Neurology. 2002;59:932–934. doi: 10.1212/wnl.59.6.932. [DOI] [PubMed] [Google Scholar]
- 11.Chen SC, Hallum LE, Lovell NH, Suaning GJ. Visual acuity measurement of prosthetic vision: a virtual-reality simulation study. J Neural Eng. 2005;2:S135–S145. doi: 10.1088/1741-2560/2/1/015. [DOI] [PubMed] [Google Scholar]
- 12.Chen W, Zhu X-H, Thulborn KR, Ugurbil K. Retinotopic mapping of lateral geniculate nucleus in humans using functional magnetic resonance imaging. Proc Natl Acad Sci U S A. 1999;96:2430–2434. doi: 10.1073/pnas.96.5.2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chow AY, Chow VY, Packo KH, Pollack JS, Peyman GA, Schuchard R. The artificial silicon retina microchip for the treatment of vision loss from retinitis pigmentosa. Arch Ophthalmol. 2004;122:460–469. doi: 10.1001/archopht.122.4.460. [DOI] [PubMed] [Google Scholar]
- 14.Chowdhury V, Morley JW, Coroneo MT. Feasibility of extraocular stimulation for a retinal prosthesis. Can J Ophthalmol. 2005;40:563–572. doi: 10.1016/S0008-4182(05)80048-1. [DOI] [PubMed] [Google Scholar]
- 15.Curcio CA, Sloan KR, Kalina RE, Hendrickson AE. Human photoreceptor topography. J Comp Neurol. 1990;292:497–523. doi: 10.1002/cne.902920402. [DOI] [PubMed] [Google Scholar]
- 16.Dagnelie G, Keane P, Narla V, Yang L, Weiland J, Humayun M. Real and virtual mobility performance in simulated prosthetic vision. J Neural Eng. 2007;4:S92–S101. doi: 10.1088/1741-2560/4/1/S11. [DOI] [PubMed] [Google Scholar]
- 17.Dagnelie G, Vogelstein JV. Phosphene mapping procedures for prosthetic vision, in Vision Science and Its Applications. Washington, DC: Optical Society of America; 1999. [Google Scholar]
- 18.Daniel PM, Witteridge D. The representation of the visual field on the cerebral cortex in monkeys. J Physiol. 1961;159:203–221. doi: 10.1113/jphysiol.1961.sp006803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deep Brain Stimulation for Parkinson’s Disease Study Group: Deep-brain stimulation of the subthalamic nucleus or the parts interna of the globus pallidus in Parkinson’s disease. N Engl J Med. 2001;435:956–963. doi: 10.1056/NEJMoa000827. [DOI] [PubMed] [Google Scholar]
- 20.Delbeke J, Pins D, Michaux G, Wanet-Defalque M-C, Parrini S, Veraart C. Electrical stimulation of anterior visual pathways in retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2001;42:291–297. [PubMed] [Google Scholar]
- 21.Dobelle WH, Mladejvosky MG. Phosphenes produced by electrical stimulation of human occipital cortex, and their application to the development of a prosthesis for the blind. J Physiol. 1974;243:553–576. doi: 10.1113/jphysiol.1974.sp010766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dobelle WH. Artificial vision for the blind by connecting a television camera to the visual cortex. ASAIO J. 2000;46:3–9. doi: 10.1097/00002480-200001000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Dougherty RF, Kich VM, Brewer AA, Fischer B, Modersitzki J, Wandell BA. Visual field representations and locations of visual areas V1/2/3 in human visual cortex. J Vis. 2003;3:586–598. doi: 10.1167/3.10.1. [DOI] [PubMed] [Google Scholar]
- 24.Dowling J. Current and future prospects for optoelectronic retinal prostheses. Eye. 2008 doi: 10.1038/eye.2008.385. [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Eng JG, Agrawal RN, Ross-Cisneros FN, Dagnelie G, Green-berg RJ, Weiland JD, et al. Morphometric analysis of optic nerves from an end-stage retinitis pigmentosa patient implanted with an active epiretinal array. Invest Ophthalmol Vis Sci. 2008;49 doi: 10.1167/iovs.09-4936. e-abstract 1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Erwin E, Baker FH, Busen WF, Malpeli JG. Relationship between laminar toplogoly and retinotopy in the rhesus lateral geniculate nucleus: results from a functional atlas. J Comp Neurol. 1999;407:92–102. [PubMed] [Google Scholar]
- 27.Everitt BS, Rushton DN. A method for plotting the optimum positions of an array of cortical electrical phosphenes. Biometrics. 1978;34:399–410. [PubMed] [Google Scholar]
- 28.Gekeler F, Sachs H, Szurman P, Guelicher D, Wilke R, Reinert S, et al. Surgical procedure for subretinal implants with external connections: the extra-ocular surgery in eight patients. Invest Ophthalmol Vis Sci. 2008;49 e-abstract 4049. [Google Scholar]
- 29.Greenbaum E, Humayun MS, Kuritz T, Lee JW, Sanders CA, Bruce B, et al. IEEE. Nanoscale photosynthesis, the photophysics of neural cells, and artificial sight. Proceedings of the IEEE-EMBS Special Topic Conference on Molecular, Cellular and Tissue Engineering; Genova, Italy. 2002; Los Alamitos: IEEE Computer Society Conference Publishing Services; 2008. pp. 83–85. [Google Scholar]
- 30.Gupta N, Ang L-C, Noel de Tilly L, Bidaisee L, Yucel YH. Human glaucoma and neural degeneration in intracranial optic nerve, lateral geniculate nucleus, and visual cortex. Br J Ophthalmol. 2006;90:674–678. doi: 10.1136/bjo.2005.086769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hallum LE, Suaning GJ, Taubman DS, Lovell NH. Simulated prosthetic visual fixation, saccade and smooth pursuit. Vision Res. 2005;45:775–788. doi: 10.1016/j.visres.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 32.Hayes JS, Yin VT, Piyathaisere D, Weiland JD, Humayun MS, Dagnelie G. Visually guided performance of simple tasks using simulated prosthetic vision. Artif Organs. 2003;27:1016–1028. doi: 10.1046/j.1525-1594.2003.07309.x. [DOI] [PubMed] [Google Scholar]
- 33.Hendry SHC, Reid RC. The koniocellular pathway in primate vision. Annu Rev Neurosci. 2000;23:127–153. doi: 10.1146/annurev.neuro.23.1.127. [DOI] [PubMed] [Google Scholar]
- 34.Hickey TL, Guillery RW. Variability of laminar patterns in the human lateral geniculate nucleus. J Comp Neurol. 1979;183:221–246. doi: 10.1002/cne.901830202. [DOI] [PubMed] [Google Scholar]
- 35.Hornig R, Zehnder T, Velikay-Parel M, Laube T, Feuct M, Richard G. The IMI Retinal Implant System. In: Humayun MS, Weiland JD, Chader G, Greenbaum E, editors. Artificial Sight, Basic Research, Biomedical Engineering, and Clinical Advances. New York: Springer; 2007. pp. 111–128. [Google Scholar]
- 36.Horsager A, Weiland JD, Greenberg RJ, Humayun MS. Fine I:Spatiotemporal integration of perceptual brightness in retinal prosthesis patients. Invest Ophthalmol Vis Sci. 2008;49 e-abstract 3011. [Google Scholar]
- 37.Hubel DH, Wiesel TN. Brain and Visual Perception: The Story of a 25-Year Collaboration. New York: Oxford University Press; 2004. [Google Scholar]
- 38.Humayun MS. Preliminary results from Argus II feasibility study: a 60 electrode epiretinal prosthesis. Invest Ophthalmol Vis Sci. 2009;50 e-abstract 4744. [Google Scholar]
- 39.Humayun MS, de Juan E, Dagnelie G, Greenberg RJ, Propst RH, Phillips DH. Visual perception elicited by electrical stimulation of retina in blind humans. Arch Ophthalmol. 1996;114:40–46. doi: 10.1001/archopht.1996.01100130038006. [DOI] [PubMed] [Google Scholar]
- 40.Humayun MS, Weiland JD, Fuiji GY, Greenberg R, Williamson R, Little J, et al. Visual perception in a blind subject with a chronic microelectronic retinal prosthesis. Vision Res. 2003;43:2573–2581. doi: 10.1016/s0042-6989(03)00457-7. [DOI] [PubMed] [Google Scholar]
- 41.Ivanstinovic D, Langmann G, Nemetz W, Hornig R, Velikay-Parel M. A new method for fixation and explantation of epiretinal implants. Invest Ophthalmol Vis Sci. 2009;50 doi: 10.1111/j.1755-3768.2009.01694.x. e-abstract 4571. [DOI] [PubMed] [Google Scholar]
- 42.Jones KE, Campbell PK, Normann RA. A glass/silicon composite intracortical electrode array. Ann Biomed Eng. 1992;20:423–437. doi: 10.1007/BF02368134. [DOI] [PubMed] [Google Scholar]
- 43.Kammer T, Puls K, Erb M, Grodd W. Transcranial magnetic stimulation in the visual system. II. Characterization of induced phosphenes and scotomas. Exp Brain Res. 2005;160:129–140. doi: 10.1007/s00221-004-1992-0. [DOI] [PubMed] [Google Scholar]
- 44.Kara P, Pezaris JS, Yurgenson S, Reid RC. The spatial receptive field of thalamic inputs to single cortical simple cells revealed by the interaction of visual and electrical stimulation. Proc Natl Acad Sci U S A. 2002;99:16261–16266. doi: 10.1073/pnas.242625499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kastner S, O’Connor DH, Fukui MM, Fehd HM, Herwig U, Pinsk MA. Functional imaging of the human lateral geniculate nucleus and pulvinar. J Neurophysiol. 2004;91:438–448. doi: 10.1152/jn.00553.2003. [DOI] [PubMed] [Google Scholar]
- 46.Keserue M, Feucht M, Post N, Hornig R, Richard G. Clinical study on chronic electrical stimulation of the human retina with an epiretinal electrode array: fluorescein angiography and OCT findings. Invest Ophthalmol Vis Sci. 2008;49 e-abstract 1785. [Google Scholar]
- 47.Koch C, Mokwa W, Goertz M, Walter P. First results of a study on a completely implanted retinal prosthesis in blind humans. IEEE Sensors 2008 Conference; [DOI] [PubMed] [Google Scholar]
- 48.Kumar R, Lozano AM, Kim YJ, Hutchison WD, Sime E, Halket E, et al. Double-blind evaluation of subthalamic nucleus deep brain stimulation in advanced Parkinson’s disease. Neurology. 1998;51:850–855. doi: 10.1212/wnl.51.3.850. [DOI] [PubMed] [Google Scholar]
- 49.Li L, Sun M, Cao P, Cai C, Chai X, Li X, et al. A visual prosthesis based on optic nerve stimulation: in vivo electrophysiological study in rabbits. In: Peng Y, Weng X, editors. APCMBE 2008, IFMBE Proceedings. Vol. 19. New York: Springer; 2008. pp. 54–57. [Google Scholar]
- 50.Limousin P, Pollak P, Benazzouz A, Hoffman D, Broussolle E, Perret JE, et al. Bilateral subthalamic nucleus stimulation for severe Parkinson’s disease. Mov Disord. 1995;10:672–674. doi: 10.1002/mds.870100523. [DOI] [PubMed] [Google Scholar]
- 51.Majji AB, Humayun MS, Weiland JD, Suzsuki S, D’Anna SA, de Juan E. Long-term histological and electrophysiological results of an inactive epiretinal electrode array implantation in dogs. Invest Ophthalmol Vis Sci. 1999;40:2073–2081. [PubMed] [Google Scholar]
- 52.Marg E, Rudiak D. Phosphenes induced by magnetic stimulation over the occipital brain: description and probable site of stimulation. Optom Vis Sci. 1994;71:301–311. doi: 10.1097/00006324-199405000-00001. [DOI] [PubMed] [Google Scholar]
- 53.Miki A, Liu GT, Raz J, Englander SA, Bonhomme GR, Aleman DO, et al. Visual activation in functional magnetic resonance imaging at very high field (4 Tesla) J Neuro-Ophthal. 2001;21:8–11. doi: 10.1097/00041327-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 54.Mokwa W, Goertz M, Koch C, Krisch I, Trieu H-K, Walter P. Intraocular epiretinal prosthesis to restore vision in blind humans. Vancouver, BC. 30th Annual International IEEE Engineering in Medicine and Biology Society Conference; August 20–24, 2008; [DOI] [PubMed] [Google Scholar]
- 55.Montezuma SR, Loewenstein J, Scholz C, Rizzo JF. Biocompatibility of materials implanted into the subretinal space of yucatan pigs. Invest Ophthalmol Vis Sci. 2006;47:3514–3522. doi: 10.1167/iovs.06-0106. [DOI] [PubMed] [Google Scholar]
- 56.Nanduri D, Humayun MS, Greenberg RJ, McMahon MJ, Weiland JD. Retinal prosthesis phosphene shape analysis. Vancouver, BC. 30th Annual International IEEE Engineering in Medicine and Biology Society Conference; August 20–24, 2008; pp. 1785–1788. [DOI] [PubMed] [Google Scholar]
- 57.Normann RA, Maynard EM, Rousche PJ, Warren DJ. A neural interface for a cortical vision prosthesis. Vision Res. 1999;39:2577–2587. doi: 10.1016/s0042-6989(99)00040-1. [DOI] [PubMed] [Google Scholar]
- 58.O’Connor DH, Fukui MM, Pinsk MA, Kastner S. Attention modulates responses in the human lateral geniculate nucleus. Nat Neurosci. 2002;5:1203–1209. doi: 10.1038/nn957. [DOI] [PubMed] [Google Scholar]
- 59.Oban GA. Neuronal Operations in the Visual Cortex. New York: Springer-Verlag; 1984. [Google Scholar]
- 60.Palanker D, Vankov A, Huie P, Baccus S. Design of a high-resolution optoelectronic retinal prosthesis. J Neural Eng. 2005;2:S105–S120. doi: 10.1088/1741-2560/2/1/012. [DOI] [PubMed] [Google Scholar]
- 61.Pezaris JS. Computation and Neural Systems. California Institute of Technology; Pasadena, California: 2000. Responses of Simultaneously Recorded Macaque Area LIP Neurons in a Memory Saccade Task \dissertation] [Google Scholar]
- 62.Pezaris JS, Reid RC. Demonstration of artificial visual percepts generated through thalamic microstimulation. Proc Nat Assoc Sci U S A. 2007;104:7670–7675. doi: 10.1073/pnas.0608563104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pezaris JS, Reid RC. Simulations of electrode placement for a thalamic visual prosthesis. IEEE Trans Biomed Eng. 2009;56:172–178. doi: 10.1109/TBME.2008.2005973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Piedade M, Gerald J, Sousa LA, Tavares G, Tomas P. Visual neuroprosthesis: a non invasive system for stimulating the cortex. IEEE Trans Circuits and Systems I: Regular Papers. 2005;52:2648–2662. [Google Scholar]
- 65.Polyak SL. The Main Afferent Fiber Systems of the Cerebral Cortex in Primates. Berkeley, CA: University of California Press; 1932. [Google Scholar]
- 66.Polyak SL. The Vertebrate Visual System. Chicago, IL: University of Chicago Press; 1957. [Google Scholar]
- 67.Richard G, Keserue M, Feucht M, Post N, Hornig R. Visual perception after long-term implantation of a retinal implant. Invest Ophthalmol Vis Sci. 2008;49 e-abstract 1786. [Google Scholar]
- 68.Rizzo JF, Snebold L, Kenney M. Development of a visual prosthesis: a review of the field and an overview of the Boston Retinal Implant Project. In: Tombran-Tink J, Barnstable C, Rizzo JF, editors. Ophthalmology Research: Visual Prosthesis and Ophthalmic Devices: New Hope in Sight. Totowa, NJ: Humana Press Inc; 2007. [Google Scholar]
- 69.Rizzo JF, Wyatt J, Lowenstein J, Kelly S, Shire D. Perceptual efficacy of electrical stimulation of human retina with a microelectrode array during short-term surgical trials. Invest Ophthalmol Vis Sci. 2003;44:5362–5369. doi: 10.1167/iovs.02-0817. [DOI] [PubMed] [Google Scholar]
- 70.Rodriguez-Oroz MC, Obeso JA, Lang AE, Houeto J-L, Pollak P, Rehncrona S, et al. Bilateral deep brain stimulation in Parkinson’s disease: a multicentre study with 4 years follow-up. Brain. 2005;128:2240–2249. doi: 10.1093/brain/awh571. [DOI] [PubMed] [Google Scholar]
- 71.Roodhooft JMJ. Leading causes of blindness worldwide. Bull Soc Belge Ophtalmol. 2002;283:19–25. [PubMed] [Google Scholar]
- 72.Sakaguchi H, Fujikado T, Kanda H, Osanai M, Fang X, Nakauchi K, et al. Electrical stimulation with a needle-type electrode inserted into the optic nerve in rabbit eyes. Jpn J Ophthalmol. 2004;48:552–557. doi: 10.1007/s10384-004-0114-7. [DOI] [PubMed] [Google Scholar]
- 73.Sakaguchi H, Kamei M, Fujikado T, Yanezawa E, Ozawa M, Cecilia-Gonzalez C, et al. Artificial vision by direct optic nerve electrode (AV-DONE) for a blind patient with retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2008;49 doi: 10.1007/s10047-009-0467-2. e-abstract 4044. [DOI] [PubMed] [Google Scholar]
- 74.Schiller PH, Tehovnik EJ. Visual prosthesis. Perception. 2008;37:1529–1559. doi: 10.1068/p6100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schmidt EM, Bak MJ, Hambrecht FT, Kufta CV, O’Rourke DK. Vallabhanath: feasibility of a visual prosthesis for the blind based on intracortical microstimulation of the visual cortex. Brain. 1996;119:507–522. doi: 10.1093/brain/119.2.507. [DOI] [PubMed] [Google Scholar]
- 76.Schneider KA, Richter MC, Kastner S. Retinotopic organization and functional subdivisions of the human lateral geniculate nucleus: a high-resolution functional magnetic resonance imaging study. J Neurosci. 2004;24:8975–8985. doi: 10.1523/JNEUROSCI.2413-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shire DB, Gingerich M, Rizzo JF, Wyatt JL. Recent development in inflatable prostheses for epiretinal stimulation and/or recording. Invest Ophthalmol Vis Sci. 2005;46 e-abstract 1534. [Google Scholar]
- 78.Sommerhalder J. ARVO annual meeting 2008: visual prosthesis research. Expert Rev Ophthalmol. 2008;3:389–391. [Google Scholar]
- 79.Sommerhalder J, Oueghlani E, Bagnoud M, Leonards U, Safran AB, Pelizzone M. Simulation of artificial vision: I. Eccentric reading of isolated words, and perceptual learning. Vision Res. 2003;43:269–283. doi: 10.1016/s0042-6989(02)00481-9. [DOI] [PubMed] [Google Scholar]
- 80.Szurman P, Warga M, Roters S, Grisanti S, Heimann U, Aisenbrey S, et al. Experimental implantation and long-term testing of an intraocular vision aid in rabbits. Arch Ophthalmol. 2005;123:964–969. doi: 10.1001/archopht.123.7.964. [DOI] [PubMed] [Google Scholar]
- 81.Tehovnik EJ, Slocum WM. Phosphene induction by microstimulation of macaque V1. Brain Res Rev. 2007;53:337–343. doi: 10.1016/j.brainresrev.2006.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thompson RW, Barnett GD, Humayun MS, Dagnelie G. Facial recognition using simulated prosthetic pixelized vision. Invest Ophthalmol Vis Sci. 2003;44:5035–5042. doi: 10.1167/iovs.03-0341. [DOI] [PubMed] [Google Scholar]
- 83.Tootell RBH, Hadjikhani NK, Vanduffel W, Liu AK, Mendola JD, Sereno MI, et al. Functional analysis of primary visual cortex (V1) in humans. Proc Natl Acad Sci U S A. 1998;95:811–817. doi: 10.1073/pnas.95.3.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Troyk PR, Srivastava N, Dagnlelie G, Kufta C, McCreery D, Schmid E, et al. Human psychophysical testing to access the feasibility of an intracortical visual prosthesis. Invest Ophthalmol Vis Sci. 2008;49 e-abstract 5874. [Google Scholar]
- 85.Turicchia L, O’Halloran M, Kumar DP, Sarpeshkar R. A low- power imager and compression algorithms for a brain-machine visual prosthesis for the blind. Biosensing. 2008;7035:703510–703513. [Google Scholar]
- 86.Weiland JD, Yanai D, Mahadevappa M, Williamson R, Mech BV, Fuijii GY, et al. Visual task performance in blind humans with retinal prosthetic implants. San Francisco, CA. Proceedings of the 26th Annual International Conference IEEE Engineering in Medicine and Biology Society; September 1–5, 2004; pp. 4172–4173. [DOI] [PubMed] [Google Scholar]
- 87.Wilms M, Eger M, Schanze T, Eckhorn R. Visual resolution with epi-retinal electrical stimulation estimated from activation profiles in cat visual cortex. Vis Neurosci. 2003;20:543–555. doi: 10.1017/s0952523803205083. [DOI] [PubMed] [Google Scholar]
- 88.Veraart C, Raftopoulos C, Mortimer JT, Delbeke J, Pins D, Michaux G, et al. Visual sensations produced by optic nerve stimulation using an implanted self-sizing spiral cuff electrode. Brain Res. 1998;813:181–186. doi: 10.1016/s0006-8993(98)00977-9. [DOI] [PubMed] [Google Scholar]
- 89.Zrenner E. Will retinal implants restore vision? Science. 2002;295:1022–1025. doi: 10.1126/science.1067996. [DOI] [PubMed] [Google Scholar]
- 90.Zrenner E, Stett A, Weiss S, Aramant RB, Guenther E, Kohler K, et al. Can subretinal microphotodiodes successfully replace degenerated photoreceptors? Vision Res. 1999;39:2555–2567. doi: 10.1016/s0042-6989(98)00312-5. [DOI] [PubMed] [Google Scholar]
- 91.Zrenner E, Wilke R, Bartz-Schmidt K, Benav H, Besch D, Gekeler F, et al. Blind retinitis pigmentosa patients can read letters and recognize the direction of fine stripe patterns with subretinal electronic implants. Invest Ophthalmol Vis Sci. 2009;50 e-abstract 4581. [Google Scholar]
- 92.Zworykin VP. Some new data on individual quantitative peculiarities of the human lateral geniculate body. Arkiv Anatomii Gistologii i Embriologii. 1980;78:24–27. (Rus) [PubMed] [Google Scholar]


