Abstract
Objectives: To provide a contemporary account of the treatment and outcomes of acute coronary attacks in England and Wales and to identify strategies that might improve the outcome.
Design: Two year community and hospital based study in three British health districts.
Setting: Health districts of Brighton (population 282 000), South Glamorgan (408 000), and York (264 000).
Subjects: 3523 men and women under 75 years of age who died outside hospital from acute coronary causes, who were admitted to hospital with acute myocardial infarction, or who developed acute infarction or died unexpectedly from acute coronary causes while they were already in hospital.
Interventions: Attempted resuscitation in people having a cardiac arrest outside hospital.
Main outcome measures: Total case fatality, case fatality outside and inside hospital, and the effect of resuscitation on case fatality outside hospital.
Results: 1589 patients died within 30 days of the acute event. Case fatality was 45% (95% confidence interval 43% to 47%), rising from 27% (160/595) (23% to 31%) at age <55 years to 53% (1019/1916) (51% to 55%) at 65-74 years. Overall, 74% (1172/1589) (72% to 76%) of fatal events happened outside hospital, and there was a negative age gradient (P<0.001) such that 91% (145/160) (87% to 95%) of fatalities occurred outside hospital at age <55 compared with 70% (710/1019) (67% to 73%) at 65-74 years. Without successful resuscitation of 55 patients outside hospital, total case fatality at 30 days would have risen from 45% to 46.7%.
Conclusion: Opportunities for reducing fatality from acute coronary attacks lie mainly outside hospital. These results and others imply that survival from cardiac arrest outside hospital might be trebled by improved ambulance and patient response. Proper application of secondary preventive measures for patients with coronary disease could have an even larger impact.
Key messages
In three health districts during 1994-5 total case fatality for people under 75 years of age was 45% and 74% of fatal events happened outside hospital
The likelihood of a fatal event occurring outside hospital was greater for people under 55 years of age (91%) than for those aged 65-74 years (70%)
Total fatality was reduced appreciably (by 1.7%) by resuscitation outside hospital, but this proportion might possibly be trebled by further upgrading of ambulance services
Because 46% of people who died were already known to have coronary heart disease, improved secondary prevention may have a major part in further reducing mortality
Introduction
Twenty five years ago at least two thirds of deaths from acute coronary heart disease happened outside hospital,1–3 and data from the monitoring trends and determinants in cardiovascular disease (MONICA) study showed that this was still the case in many countries during the 1980s.4 Mortality from coronary heart disease has, however, declined by about 30% in England and Wales since 1980.5 Moreover, devolution of prehospital care to paramedical staff, public training in cardiopulmonary resuscitation, and efforts to reduce delay in giving thrombolytic treatment should all ensure that the benefits of therapeutic advances are more readily available to victims of acute heart attack.
The aim of the United Kingdom heart attack study is to re-examine the incidence, treatment, and outcome of acute heart attacks by studying events in three health districts in England and Wales during 1994-5. This report describes total case fatality, with particular reference to events occurring outside hospital and the impact of resuscitation attempts outside hospital. The outcome of myocardial infarction in patients admitted to hospital is reported elsewhere.6
Subjects and methods
All deaths from acute episodes of ischaemic heart disease and all cases of acute myocardial infarction in hospital in people under 75 years of age were recorded over two years (January 1994 to December 1995) in the three health districts of Brighton, South Glamorgan, and York. Methods were established during a pilot study carried out in Brighton during 19937,8 and, in the light of the experience gained, were agreed on before the main study was started.
Definition of population
To avoid bias from recording deaths outside and inside hospital in different populations, we selected our catchment population to include only the areas served by the study hospitals (one each in Brighton and York and two in South Glamorgan); patients were classed by postcode. Population figures broken down by age and sex were supplied by the Office for National Statistics. Defined in this way, the population of Brighton (Brighton, Hove, and Lewes) was 282 000, that of South Glamorgan (Cardiff and the Vale of Glamorgan) 408 000, and that of York (city and surrounding, mainly rural, area) 264 000. The total study population (all ages) was 954 000. People whose events occurred within the study area who were visitors to the area (275, or 8% of total cases) were recorded as non-resident but were included on the assumption that similar numbers of events occurred in visitors as in residents who had gone outside the area.
Selection and identification of cases
Deaths outside hospital were included if ischaemic heart disease was the principal cause of death at coroners’ necropsy (86% (959/1114)) or, when there was no necropsy, if the patient had a history of ischaemic heart disease and had died suddenly or after prolonged chest pain and had no other apparent cause of death (14% (155/1114)). Cases at necropsy were required to have at least 50% stenosis of the diameter of one major epicardial coronary artery, with or without recent coronary thrombus or old or recent myocardial infarction. Deaths from chronic heart failure due to ischaemic heart disease were recorded in one centre (Brighton) but were not included in this analysis. They comprised 11% of all coronary deaths in Brighton in the age range studied, and only 29% occurred outside hospital.
We identified deaths outside hospital from transcripts of death certificates provided regularly to the health authorities by the local registrars of deaths. The date and place of death, the name of the practitioner who signed the certificate, and the name and address of the person who informed the registrar of deaths (usually the next of kin) were recorded. With permission from coroners in the three centres, we regularly reviewed copies of all necropsy reports and checked them against data from the transcripts. We then wrote to the general practitioners asking for details of the medical history and of current cardiac drugs, if any. With permission from the general practitioners, we retrieved case notes if necessary from the family health services authority. Circumstances of death were taken either from summaries made by coroners’ officers and recorded on necropsy reports or from forms made out by ambulance paramedical staff who had been summoned to the cardiac arrest. In some cases in which these approaches failed, permission was sought from the general practitioner to contact the next of kin directly. We sought whether death had been witnessed, the nature and approximate duration of any symptoms which the victim might have reported before death, whether resuscitation had been attempted, the cardiac rhythm, and the outcome. Resuscitation was considered to have been successful when the patient was discharged from hospital and survived for at least 30 days without serious neurological deficit. Necropsy details were recorded from pathologists’ reports.
Cases of myocardial infarction in hospital showed at least two of the following three features: typical or compatible clinical history, sequential electrocardiographic changes, and a rise in serum enzyme concentrations to at least twice the upper limit of normal values for the hospital laboratory. Sudden deaths from ischaemic heart disease in patients who had been admitted to hospital for another reason were also included as deaths in hospital. Survivors of myocardial infarction were not included when the infarction was diagnosed and treated outside hospital.4 We confirmed from questionnaires returned by general practitioners that these circumstances were rare.
Data were recorded on standardised forms, stored on computers at all three centres using a Paradox database, and sent regularly on disk to the coordinating centre in Brighton for amalgamation. Quality control was achieved by checking data for internal consistency locally, at the coordinating centre, and by a member of the steering committee (DGJ), who visited the three centres to audit a random selection of cases. Differences were resolved and progress assessed at investigators’ meetings, which were held every three to six months throughout the study.
Case fatality and statistics
Case fatality rates were calculated as the total number of deaths divided by the total number of events as defined and were expressed as percentages. Events occurring more than 30 days after a previous non-fatal episode were considered to be new events. Patients who were brought into hospital after having had a cardiac arrest outside hospital who were pronounced dead or who later died in hospital were included as deaths outside hospital because the event directly leading to death had occurred before arrival at hospital.
Results
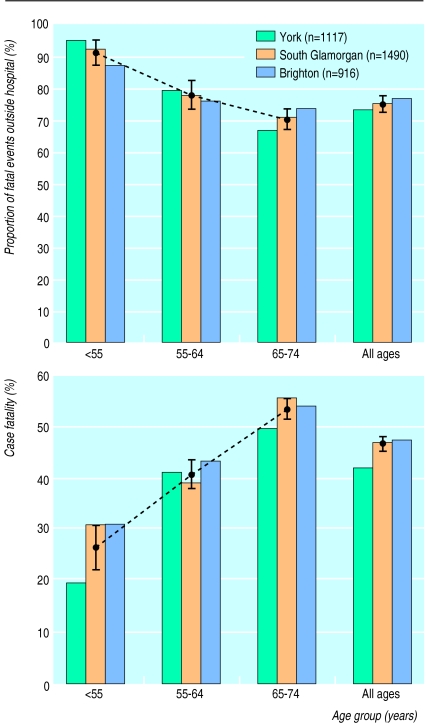
Figure 1 shows the numbers of cases, case fatality rates, and the proportion of fatal events occurring outside hospital for the individual centres. Of the 3523 events which we recorded, 3476 occurred in white people and 934 in women; 1589 (45% (95% confidence interval 43% to 47%)) were fatal within 30 days of the event. Case fatality was lower in York than in the other centres for all age groups (42% (466/1117) v 47% (1123/2406); P=0.02) and for ages <55 years (19% (40/206) v 31% (120/389); P=0.01) but not for age groups 55-64 and 65-74 years.
Figure 1.
Case fatality and proportion of fatal events occurring outside hospital in the three centres. Circles indicate mean values and bars 95% confidence intervals
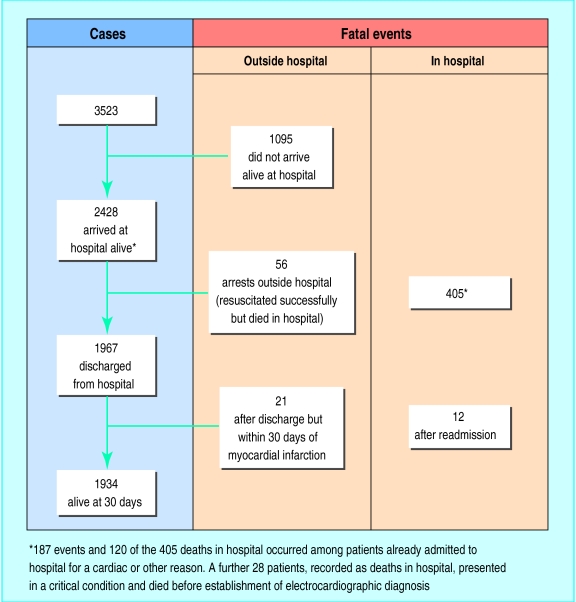
Figure 2 shows the numbers of survivors and deaths at each stage of the illness. Overall, 1172 of the 1589 fatal events (74% (72% to 76%)) occurred outside hospital. Of these, 1095 occurred in people who were not admitted to hospital, 21 occurred after discharge from hospital but within 30 days of the infarction, and 56 occurred in patients who were resuscitated outside hospital but later died in hospital. The remaining 417 (26%) fatal events occurred in hospital. Forty six per cent of the patients who died (737/1589) were known to have ischaemic heart disease, and this proportion rose with age from 31% (50/160) at <55 years to 49% (503/1019) at age 65-74.
Figure 2.
Flow diagram showing numbers of survivors and deaths at each stage
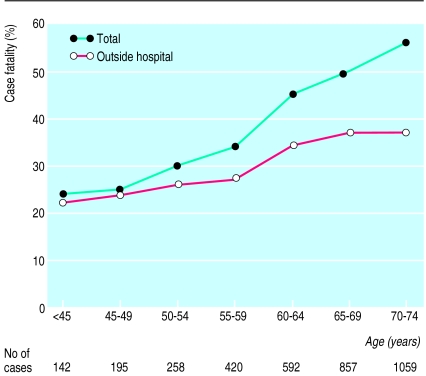
Table 1 shows the relation between the place of occurrence of the fatal event, age, and sex, and figure 3 shows the relation with age alone. Total 30 day fatality (upper line in fig 3) rose with age from 27% (23% to 31%) at age <55 to 53% (51% to 55%) at 65-74 years. The lower line in figure 3 represents fatality outside hospital. Thus the portion between the two lines represents fatality in hospital, which was very low (3% of those admitted to hospital) for patients under 55 years of age but rose to 29% for those aged 70-74 years. Corresponding figures for fatality outside hospital were 24% and 37%, so that the increase in fatality outside hospital with age was much less than the increase in fatality in hospital. Consequently, the proportion of fatal events occurring outside hospital was age dependent, falling from 91% (87% to 95%) at age <55 years to 77% (73% to 81%) at 55-64 years and 70% (67% to 73%) at 65-74 years. The (negative) gradient for age as a determinant of whether death occurred outside or inside hospital was highly significant (P<0.001) for men (table 1) and for both sexes combined (fig 3), but it was not significant for women.
Table 1.
Case fatality from acute coronary events in men and women outside and inside hospital
| Age (years) | Total No of cases
|
No of fatal events outside hospital
|
No of deaths in hospital
|
Total case fatality (%)
|
Proportion of case fatality outside hospital (%)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | |||||
| <45 | 124 | 18 | 25 | 6 | 3 | 0 | 23 | 33 | 89 | 100 | ||||
| 45-49 | 173 | 22 | 44 | 3 | 1 | 1 | 26 | 18 | 98 | 75 | ||||
| 50-54 | 221 | 37 | 55 | 12 | 9 | 1 | 29 | 35 | 86 | 92 | ||||
| 55-59 | 335 | 85 | 97 | 18 | 17 | 11 | 34 | 34 | 85 | 62 | ||||
| 60-64 | 453 | 139 | 163 | 39 | 45 | 20 | 46 | 42 | 78 | 66 | ||||
| 65-69 | 602 | 255 | 234 | 79 | 76 | 38 | 51 | 46 | 75 | 68 | ||||
| 70-74 | 681 | 378 | 258 | 139 | 125 | 70 | 56 | 55 | 67 | 67 | ||||
| Total | 2589 | 934 | 876 | 296 | 276 | 141 | 44 | 47 | 76 | 68 | ||||
Figure 3.
Total case fatality and case fatality outside hospital by age group
Premonitory symptoms, usually chest pain, during the few hours before the cardiac arrest were reported by bereaved relatives in 38% of deaths outside hospital (441/1172), while death seemed to be truly sudden in 13% (150/1172). In 49% of cases (581/1172) it was impossible to establish whether symptoms had been present, usually because the victim was found dead, having last been seen alive several hours (median 7 hours) previously. The commonest symptom was chest pain, but symptoms of “breathlessness,” “indigestion,” or “feeling unwell” were also reported frequently. There was a tendency for premonitory symptoms to be reported more often in younger than in older subjects, but this was not significant.
Effect of resuscitation outside hospital on case fatality
Of the 1227 cardiac arrests outside hospital, 920 occurred at home, 203 in a public place, 79 in doctors’ surgeries, ambulances, or nursing homes, and 25 at work. Fifty five of the 111 people who were successfully resuscitated outside hospital recovered in hospital and survived to 30 days. Of these, 51 had documented ventricular fibrillation, pulseless ventricular tachycardia, or asystole, while 4 responded to basic life support and were thought to have had a cardiac arrest on clinical grounds. Had these 55 patients not been resuscitated, the total case fatality would have been 46.7% not 45%.
Of great importance for successful resuscitation was whether the arrest was witnessed and by whom (table 2). In 39% of cases there was no witness, and no patient survived. Fifty four per cent of arrests were witnessed by a relative or bystander; cardiopulmonary resuscitation was attempted in less than one third of these cases, but when it was attempted the success rate rose from 2% to 8% (P<0.001). The best result occurred when the arrest was witnessed by a paramedic equipped with a defibrillator; this happened in only 5% of cases, but the success rate increased to 40% (28% to 53%) (table 2).
Table 2.
Success of resuscitation outside hospital in relation to witness of arrest
| Witness | No (%) of cases* | No (%) given ALS by paramedical staff | No (%; 95% CI) who survived up to 30 days |
|---|---|---|---|
| None | 474 (39) | 70 (15) | 0 |
| Relative or bystander: | |||
| CPR given | 177 (15) | 169 (95) | 14 (8; 4 to 13) |
| No CPR given | 476 (39) | 331 (70) | 8 (2; 1 to 3) |
| General practitioner | 27 (2) | 15 (56) | 7 (26; 11 to 46) |
| Paramedical staff | 65 (5) | 57 (88) | 26 (40; 28 to 53) |
| Total cases | 1219 | 642 (53) | 55 (4.5; 3 to 6) |
1184 fatal + 55 non-fatal arrests. Data not available for 8 cases.
ALS=advanced life support. CPR=cardiopulmonary resuscitation.
Discussion
The most important findings in this study were the high proportion (74%) of fatal events that occurred outside hospital and the inverse relation with age, 91% of fatalities at age <55 and 70% at age 65-74 happening outside hospital. A similar age trend has been reported from the United States on the basis of data from death certificates9 and was also observed in the pilot Brighton heart attack study.7 In the Glasgow MONICA study men were more likely than women to die outside hospital10; whether the likelihood of fatal events occurring outside hospital was related to age was not stated, but patients aged >64 years are not included in MONICA studies.
What is the reason for this disturbing finding? Hospital treatment has improved greatly over the past 20 years, resulting in a fatality rate in hospital for our patients who were under 55 years of age of only 3% (fig 3). If fatality outside hospital has not improved to the same extent, this would increase the proportion of deaths outside hospital for younger patients. Again, we did not record unclassifiable deaths outside hospital—that is, those in which death was attributed to coronary disease without results from necropsy or a history of clinical manifestation.4 We found such cases to be confined mainly to those aged 65-74, who were not included in the MONICA study.11 Inclusion of such cases would have increased the proportion of deaths outside hospital and diminished the age gradient.
The high proportion of deaths outside hospital shows the potential limitations of further improvements in hospital treatment, particularly for younger patients. It emphasises that further large reductions in mortality can be accomplished only by primary prevention, secondary prevention, or intervention before admission.
Three potential strategies exist to improve intervention before admission: improved responses by ambulance crews, intensified training of members of the public in cardiopulmonary resuscitation, and public education on the importance of dialling 999 for prolonged chest pain. These strategies might result in more cardiac arrests being witnessed by paramedical staff and more patients having successful defibrillation.
Improved ambulance response
The most successful centres have a dual12 or triple13 response system in which the immediate response to an emergency call is made by a normal ambulance or by the fire service, followed by paramedical staff trained in advanced life support who may have to travel a longer distance. A previous analysis found that dual response provides an optimum success rate,14 and success is enhanced by providing those who first attend the scene with automatic defibrillators.15 In the United Kingdom all frontline ambulances carry defibrillators, and one member of the ambulance crew has usually had paramedical training. The NHS is planned to continue with a single paramedic response system but with prioritisation of emergency calls so that response times for life threatening emergencies will be reduced from the present 14 minutes in 95% of urban areas to 8 minutes for 90% of calls in all areas.16
Comparison of our results with the best of those reported suggests a considerable potential for improvement. Thus, in Seattle (population 500 000) about 10 lives per 100 000 of the population were saved each year12 compared with 3 per 100 000 in our study. In Helsinki (population 516 000) cardiac arrests witnessed by paramedical staff were not reported on,13 and about 7 lives per 100 000 were saved by resuscitation compared with 1.5 per 100 000 in our report when we excluded cardiac arrests witnessed by paramedical staff. Moreover, in Brighton during the 1980s about 8 lives per 100 000 were saved.17 Had these results been replicated over the two years in our three health districts at least three times as many lives as the 55 which we recorded might have been saved. Fatality might have been reduced from 46.5% to 42% rather than to 45% by the saving of 110 extra lives.
Citizen training in cardiopulmonary resuscitation
Basic life support was given by bystanders in 27% of witnessed arrests in our series, and it reduced fatality modestly but significantly (table 2). Interestingly, the proportions receiving bystander life support were little different at 22% in Helsinki,13 18% in Gothenburg,18 and 36% in Seattle.14 In the unlikely event that the proportion receiving basic life support could be doubled in the United Kingdom, and assuming that the proportions in table 2 were replicated, the reduction in fatality would be less than 0.5%. These figures support previous opinions that present benefits from bystander cardiopulmonary resuscitation are real but limited.19 Protocols need to be rigorously taught, retaught, and remembered; failure by bystanders to dial the emergency number before doing anything else is another problem.19 The ideal place to start training may be in school.20 Notwithstanding the above, the contribution of bystander life support to survival would very likely be larger if ambulance response times could be improved.16
Public education
A much more impressive result (40% (28% to 53%) survival) was seen among those of our patients who experienced cardiac arrest in the presence of paramedical staff equipped with a defibrillator. These people, comprising only 5% of those who had arrests outside hospital, were fortunate enough to have reported premonitory symptoms in time, and the ambulance responded promptly. We have shown in a pilot study that there is a marked deficiency in public knowledge about the causation of myocardial infarction and in particular the differentiation of heart attack from cardiac arrest.21 Many, and probably most, people who died outside hospital in our series had premonitory symptoms, usually chest pain, often lasting for several hours. Similar findings have been reported recently from Glasgow.22 Although the success of media campaigns to induce patients with prolonged chest pain to seek help early has been limited,23 we believe that provision of information to the general public so that they can make informed decisions about the action to take for suspected heart attack can only be beneficial. Fresh initiatives in public education are necessary. A useful message is to dial an emergency number (999) for chest pain lasting 15 minutes or more.
Prevention of death outside hospital
Primary prevention of coronary heart disease is the ideal, and reduction in coronary risk factors has been a major contributory factor to the declining mortality from coronary heart disease.24 A recent analysis suggests, however, that more has been achieved and is still achievable by secondary than by primary prevention.25 An important finding from our study was that 46% of the patients who died were already known to have ischaemic heart disease. Recent advances in secondary prevention, particularly in lowering cholesterol concentration with drugs that inhibit 3-hydroxy-3-methylglutaryl coenzyme A reductase,26,27 have shown a 20-30% reduction in total deaths in patients with a history of angina or previous myocardial infarction. A reduction in mortality by 25% among those in our study who were known to have coronary heart disease and who died from events occurring outside hospital would have saved about 183 further lives. Additional benefits might also have been obtained from more strenuous advice to stop smoking and wider use of antiplatelet drugs and β blockers, none of which seemed to have been used to their full potential in subjects known to have coronary disease (data not shown).
A recent survey of secondary prevention, sponsored by the British Cardiac Society and carried out in specialist cardiac centres and district general hospitals, has shown remarkable deficiencies in recording and efforts to modify other known risk factors.28 Perhaps the greatest potential for reduction in the burden of fatality outside hospital lies in better application of secondary preventive measures.
Acknowledgments
We thank the many general practitioners who supplied data on their patients who died.
Editorial by Evans
Footnotes
Statistical adviser: DR Robinson, School of Mathematical Sciences, University of Sussex.
Steering committee: R Vincent (Brighton, chairman), RM Boyle (York), DA Chamberlain (Brighton), DG Julian (London), RM Norris (Brighton), WJ Penny (Cardiff), CFM Weston (Swansea).
Publications committee: RM Norris, DG Julian, CFM Weston.
RMN is guarantor for the study.
Funding: The study was supported by audit funds from the Department of Health, and by a grant to RMN from the Private Patients Plan (PPP) Medical Trust.
References
- 1.Armstrong A, Duncan B, Oliver MF, Julian DG, Donald KW, Fulton M, et al. Natural history of acute coronary attacks: a community study. Br Heart J. 1972;34:67–80. doi: 10.1136/hrt.34.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kinlen LJ. Incidence and presentation of myocardial infarction in an English community. Br Heart J. 1973;35:616–622. doi: 10.1136/hrt.35.6.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tunstall-Pedoe H. Coronary heart attacks in East London. Lancet. 1975;ii:833–838. doi: 10.1016/s0140-6736(75)90233-0. [DOI] [PubMed] [Google Scholar]
- 4.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveier D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA registration project: registration procedures, event rates and case fatality rates in 30 populations from 21 countries in 4 continents. Circulation. 1994;90:583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 5.British Heart Foundation. Coronary heart disease statistics. London: BHF, 1997.
- 6.UK Heart Attack Study Collaborative Group. Effect of time from onset to coming under care on fatality of patients with acute myocardial infarction: effect of resuscitation and thrombolytic therapy. Heart (in press). [PMC free article] [PubMed]
- 7.Norris RM, Dixon GF, Chamberlain DA, Vincent R. Mortality from ischaemic heart disease outside and inside hospital : the Brighton heart attack study. Br Heart J. 1994;71:P33. [Google Scholar]
- 8.Norris RM, Roy S, Dixon GF. What proportion of patients with acute myocardial infarction should receive thrombolytic therapy? Br Heart J. 1994;71:P40. [Google Scholar]
- 9.Gillum RF. Sudden coronary death in the United States 1980-1985. Circulation. 1989;79:756–765. doi: 10.1161/01.cir.79.4.756. [DOI] [PubMed] [Google Scholar]
- 10.Tunstall-Pedoe H, Morrison C, Woodward M, Fitzpatrick B, Watt G. Sex differences in myocardial infarction and coronary deaths in the Scottish MONICA population of Glasgow 1985 to 1991. Presentation diagnosis, treatment, and 28-day case fatality of 3991 events in men and 1551 events in women. Circulation. 1996;93:1981–1992. doi: 10.1161/01.cir.93.11.1981. [DOI] [PubMed] [Google Scholar]
- 11.UK Heart Attack Study Collaborative Group. The falling mortality from coronary heart disease: a clinical perspective. Heart (in press).
- 12.Cobb LA, Weaver WD, Fahrenbruch CE, Hallstrom AP, Copass MK. Community-based interventions for sudden cardiac death. Impact limitations and changes. Circulation. 1992;85(suppl 1):98–102. [PubMed] [Google Scholar]
- 13.Kuisma M, Maatha T. Out-of-hospital cardiac arrests in Helsinki: Utstein style reporting. Heart. 1996;76:18–23. doi: 10.1136/hrt.76.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eisenberg MS, Horwood BT, Cummins RO, Reynolds-Haertle R, Hearne TR. Cardiac arrest and resuscitation: a tale of 29 cities. Am J Emerg Med. 1990;19:179–186. doi: 10.1016/s0196-0644(05)81805-0. [DOI] [PubMed] [Google Scholar]
- 15.Weaver WD, Hill D, Fahrenbruch CE, Copass MK, Martin JS, Cobb LA, et al. Use of the automatic external defibrillator in the management of out-of-hospital cardiac arrest. N Engl J Med. 1988;319:661–666. doi: 10.1056/NEJM198809153191101. [DOI] [PubMed] [Google Scholar]
- 16.NHS Executive. Review of ambulance performance standards. Final report of steering group. London: NHS Executive, 1996.
- 17.Lewis SJ, Holmberg S, Quinn E, Baker K, Grainger R, Vincent R, Chamberlain DA. Out-of-hospital resuscitation in East Sussex 1981-89. Br Heart J. 1993;70:568–573. doi: 10.1136/hrt.70.6.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herlitz J, Ekstrom L, Wennerblom B, Axelsson A, Bang A, Holmberg S. Effect of bystander-initiated cardiopulmonary resuscitation on ventricular fibrillation and survival after witnessed cardiac arrest outside hospital. Br Heart J. 1994;72:408–412. doi: 10.1136/hrt.72.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weston CF, Hughes DW, Donnelly MDI. Potential impact upon community mortality rates of training citizens in cardiopulmonary resuscitation. J R Coll Physicians. 1994;28:402–406. [PMC free article] [PubMed] [Google Scholar]
- 20.Lester C, Donnelly P, Weston C, Morgan M. Teaching school children cardiopulmonary resuscitation. Resuscitation. 1996;31:33–38. doi: 10.1016/0300-9572(95)00912-4. [DOI] [PubMed] [Google Scholar]
- 21.Dixon GF, Norris RM, Vincent R. Heart Attack Action!: a campaign to improve community knowledge. Heart. 1996;76:P80. [Google Scholar]
- 22.Leslie WS, Fitzpatrick B, Morrison CE, Watt GCM, Tunstall-Pedoe H. Out-of-hospital cardiac arrest due to coronary heart disease before and after the introduction of defibrillators in ambulances. Heart. 1996;75:195–199. doi: 10.1136/hrt.75.2.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blohm M, Hartford M, Karlson BW, Luepker RV, Herlitz J. An evaluation of the results of media and educational campaigns designed to shorten the time taken by patients with acute myocardial infarction to decide to go to hospital. Heart. 1996;76:430–434. doi: 10.1136/hrt.76.5.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson CL, Rifkind BM, Sempos CT. Declining cholesterol levels among US adults: the National Health and Nutrition Examination Surveys. JAMA. 1993;269:3002–3008. [PubMed] [Google Scholar]
- 25.Hunink MGM, Goldman L, Tosteson ANA, Mittleman MA, Goldman PA, Williams L, et al. The recent decline in mortality from coronary heart disease 1980-1990. The effect of secular trends in risk factors and treatment. JAMA. 1997;277:535–542. [PubMed] [Google Scholar]
- 26.Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 27.Sacks FM, Pfeffer MA, Moye lA, Rouleau JL, Rutherford JD, Cole TG, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med 1996;335:1001-9. [DOI] [PubMed]
- 28.ASPIRE Steering Group. A British Cardiac Society survey of the potential for secondary prevention of coronary disease: ASPIRE (Action on Secondary Prevention through Intervention to Reduce Events) Heart. 1996;75:334–342. doi: 10.1136/hrt.75.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]