Abstract
Objective: To test the hypotheses that children with abdominal pain have anxious parents and come from families with high rates of physical illness and that they grow up to suffer from high rates of medically unexplained symptoms and psychiatric disorders.
Design: Population based birth cohort study.
Setting: General population.
Subjects: Participants in the Medical Research Council (MRC) national survey of health and development, a population based birth cohort study established in 1946.
Main outcome measures: Abdominal pain present throughout childhood in the absence of defined organic disease, and measures of physical symptoms and psychiatric disorder at age 36 years.
Results: There were high rates of complaints about physical health among the parents of children with persistent abdominal pain, and the mothers had higher neuroticism scores. Children with persistent abdominal pain were more likely to suffer from psychiatric disorders in adulthood (odds ratio 2.72 (95% confidence interval 1.65 to 4.49)) but were not especially prone to physical symptoms once psychiatric disorder was controlled for (odds ratio 1.39 (0.83 to 2.36)).
Conclusions: Persistent abdominal pain is associated with poor health and emotional disorder in the parents. Children with abdominal pain do not necessarily continue to experience physical symptoms into adulthood but are at increased risk of adult psychiatric disorders.
Key messages
Persistent abdominal pain in childhood is more common in families with high rates of reported physical illness and psychological symptoms
The outcome for persistent abdominal pain is good in terms of mortality
Children with persistent abdominal pain are not at greatly increased risk of developing physical symptoms in adulthood
Abdominal pain in childhood is associated with considerably increased risk of psychiatric disorders in adulthood
Introduction
Recurrent abdominal pain is a common reason for children to see a doctor.1–3 In most cases no defined organic diagnosis can be found, and this has led researchers to seek psychosocial explanations for recurrent abdominal pain.4 Children presenting with abdominal pain may come from anxious families5–8 and from families in which one or more members suffer from physical health complaints.9–12 Most studies have drawn from relatively small clinical samples, which may introduce selection bias with, for example, the most severely symptomatic children and the most anxious parents being overrepresented.
There is comparatively little literature on the long term outcome of children with recurrent abdominal pain. Studies from clinical samples suggest that between 25% and 50% continue to experience symptoms into adulthood.13–15 It seems plausible that children with recurrent abdominal pain might also grow up to suffer from irritable bowel syndrome and other functional (or medically unexplained) symptoms. As one of the commonest functional symptoms in childhood, it is tempting to view it as a precursor to non-specific physical symptoms in adulthood. In addition, the evidence that childhood recurrent abdominal pain is associated with a range of psychosocial risk factors suggests that common mental disorders (such as anxiety and depression) may be more common in later life.
This study describes the results of the Medical Research Council’s national survey of health and development, a birth cohort which has followed the same group of 5362 subjects from birth in 1946 until the most recent wave of data gathering in 1989 (at age 43 years). We used this long follow up to test the hypotheses that children with persistent abdominal pain come from families with high rates of psychiatric disorder and neuroticism and physical illness and that children with persistent abdominal pain will have high rates of psychiatric disorders and medically unexplained symptoms in adulthood.
Subjects and methods
The MRC national survey of health and development
—The national survey of health and development is a national birth cohort study set up in 1946.16 The survey was based on a sample stratified for social class of all single legitimate births that occurred in England, Wales, and Scotland in one week of March 1946. The sampling procedure and follow up has been described in detail elsewhere.16 The stratification was based on father’s social class: all children born to non-manual workers and agricultural workers were surveyed, while those born to other manual labourers were sampled in a ratio of 1:4. Since 1946, 19 waves of data gathering have been performed. At each wave, information on admission to hospital has been sought. Whenever admission is reported the hospital is contacted for details of diagnosis and treatment.
Definition of cases of recurrent abdominal pain and controls
—The usual definition of recurrent abdominal pain is of pain severe enough to affect activities and that occurs at least three times over a period of at least 3 months.1 The data collected in the survey did not allow for this precise definition. Abdominal pain over the previous year was asked about on three occasions in childhood (at ages 7, 11, and 15 years). We therefore defined persistent abdominal pain as abdominal pain reported at each of these three points in time, which suggested that the pain was chronic. Hospital records for all such children were scrutinised by a paediatrician (SC), and those with a defined organic cause of pain that was judged to have been present throughout childhood were excluded from the sample. Controls were defined as survey members who participated in the same waves of data collection during childhood but in whom either no abdominal pain was reported or it occurred only once or twice.
Parental illness in childhood
—Parental illness was assessed when the survey members were aged 15. The mother was given a list of seven physical illnesses and asked to indicate whether she or her husband had any of them. The illnesses were asthma, cough, rheumatism in joints, anaemia, heart trouble, kidney trouble, and other health complaints. From this list it was possible to determine the number of health complaints each parent suffered from. The mother was also asked to indicate if either parent had “nervous” complaints. In addition, information was collected on the mother’s perception of her and her husband’s health. This was rated on a questionnaire as “excellent, good, average, not very good, bad.” Finally, maternal neuroticism was assessed with the Maudsley personality inventory.17
Absence from school
—Absence from school was assessed twice during childhood. Firstly, school records from the period 1952-6 (at ages 6-10 years) were used to determine the number and distribution of 1 week periods off school over that time. Secondly, the teachers were asked whether the child was below average, average, or above average in terms of absences at the age of 13 years and again at 15 years.
Childhood personality and behaviour
—Two main sources of information were used. The children had the Pintner personality inventory administered at the age of 13, which defined personality according to two dimensions “neuroticism” and “extroversion.”18 The second source of information on personality was from the child’s form teacher, who was asked to rate the survey members on the following items: lying, disobedience, being a disciplinary problem, restlessness, quality of work, and energy levels. For each item they were asked to say whether the child was above average, average, or below average.
Other variables
—Sex and social class were possible confounders. Social class was assessed according to the father’s occupation in 1961 (when survey members were aged 15) and was classified as manual versus non-manual social group.
Adulthood variables
—Outcomes during adulthood were measured at 36 years. Two main outcomes were used: psychiatric disorder and physical symptoms. The present state examination, a semistructured psychiatric interview which generates levels of severity of psychiatric disorder (the index of definition), was used for the first outcome.19 An index of definition of 5 is considered to be threshold for psychiatric disorder. The second outcome was self reported physical symptoms. These were headache, back pain, abdominal pain, dizziness, chest pain, and rheumatism. We identified survey members who suffered from inflammatory bowel disease during adulthood from self report and hospital notes. The survey collects death records for all survey members, and these were available to determine whether persistent abdominal pain in childhood was associated with increased mortality.
Analytical strategy and statistical methods
—Odds ratios and 95% confidence intervals were calculated to assess the strength of associations between childhood risk factors and persistent abdominal pain. These were subsequently controlled for father’s social class and sex in a logistic regression analysis weighted for the sampling. Likelihood trend tests were used for ordered categorical variables. Ordinal regression was used for the adult outcomes, which were ordered categorical variables (index of definition and number of physical symptoms). This generated a single odds ratio for ordered categorical outcomes which represent the odds of having the outcome for those in the group with pain relative to those unaffected by pain.20 Cox’s proportional hazards were used to determine whether death rates for those with abdominal pain in childhood (corrected for sex, social class, and sampling weights) were raised during adulthood.
Results
At the age of 7 years, a fifth of survey members had suffered abdominal pain; at 11 years it was 19% and at 15 years it was 17%. Two fifths were reported to have suffered abdominal pain at least once in childhood and 10% at least twice. Seventy six (2.1%) of the 3637 children who participated at the three points in time had recurrent abdominal pain. Of these, three had hospital records that suggested that the pain was caused by a chronic disease, leaving 73 (2.0%) with persistent pain of unexplained origin. Of this group, 52 (71%) had consulted a doctor at least once during childhood. The follow up and representativeness of the survey have been described in more detail elsewhere.16 Of the risk set, 32 were followed up to the age of 36 years, and this proportion did not differ according to pain status in childhood (χ2=0.001; P=0.97).
Children with persistent abdominal pain were evenly distributed between the sexes (odds ratio for girls 0.97; 95% confidence interval 0.56 to 1.68). Children whose fathers had manual occupations were more likely to suffer from pain (1.75; 1.02 to 3.03). Table 1 shows the relation between persistent abdominal pain and various measures of parental and family health during childhood. There was a strong association between pain and parental health complaints, parental ratings of health, maternal “nerves,” maternal neuroticism, and reporting of the family being prone to “colds.” Because the relation between pain and parental physical health complaints and health ratings could have been due to maternal neuroticism an additional logistic model, which included maternal neuroticism with these complaints, was included, but this caused only a modest reduction in these associations (results not shown).
Table 1.
Relation between childhood abdominal pain and parental health complaints and maternal neuroticism
| Risk factor (age (years) of child at assessment) | No exposed | No (%) cases | Odds ratio (95% CI)* | Ir χ2 for trend; P value |
|---|---|---|---|---|
| Maternal neuroticism on Maudsley personality inventory (13) | ||||
| 0 | 1144 | 16 (1.4) | 1.00 | 13.62; 0.0002 |
| 1 | 765 | 11 (1.4) | 0.76 (0.37 to 1.12 | |
| 2–3 | 1037 | 23 (2.2) | 1.05 (0.49 to 2.24) | |
| ⩾4 | 511 | 21 (4.1) | 2.61 (1.23 to 5.52) | |
| Parental ailments (15) | ||||
| 0 | 1604 | 15 (0.9) | 1.00 | 13.62; 0.0002 |
| 1 | 1055 | 25 (2.4) | 2.37 (1.12 to 5.01) | |
| 2 | 500 | 16 (3.2) | 3.01 (1.31 to 6.91) | |
| 3 | 204 | 7 (3.4) | 2.57 (0.85 to 7.74) | |
| 125 | 8 (6.4) | 4.96 (1.73 to 14.17) | ||
| Mother’s perception of own health (15) | ||||
| Excellent/good | 2353 | 24 (1.4) | 1.00 | 13.64; 0.0002 |
| Average | 920 | 27 (2.9) | 1.39 (0.75 to 2.58) | |
| Not very good/bad | 171 | 1 (5.9) | 4.54 (2.00 to 10.30) | |
| Mother’s perception of father’s health (15) | ||||
| Excellent/good | 2453 | 37 (1.5) | 1.00 | 6.13; 0.01 |
| Average | 723 | 22 (3.0) | 1.69 (0.89 to 3.20) | |
| Not very good/bad | 204 | 7 (3.4) | 2.06 (0.80 to 5.29) | |
| Mother’s self reporting of “nerves” (15) | ||||
| No | 3059 | 54 (1.8) | 1.00 | 6.13; 0.01 |
| Yes | 394 | 17 (4.3) | 2.12 (1.05 to 4.31) | |
| Mother reports “nerves” in father (15) | ||||
| No | 3193 | 64 (2.0) | 1.00 | 0.46; 0.5 |
| Yes | 148 | 4 (2.7) | 1.44 (0.43 to 4.79) | |
| Reported continual or repeated colds in other family members (6) | ||||
| No | 2181 | 24 (1.1) | 1.00 | 14.2; 0.0002 |
| Yes | 1427 | 48 (3.4) | 2.48 (1.39 to 4.41) |
Ir = likelihood ratio test.
Odds ratios corrected for sex and father’s social class, weighted for sampling.
Childhood personality and its association with persistent abdominal pain is shown in table 2. Neuroticism and introversion were not associated. The teacher’s ratings suggested that persistent abdominal pain was no more common in children with antisocial traits such as lying, disobedience, or having disciplinary problems. There was a modest association between traits such as day dreaming in class and having low levels of energy and persistent abdominal pain. Children with abdominal pain had more absence from school between the ages of 6 and 10 years, but only a modest non-significant increase in absence was evident at 13 years.
Table 2.
Relation between abdominal pain and childhood personality and behaviour and school absences
| Risk factor (assessor) | No exposed | No (%) affected | Odds ratio (95% CI)* | lr χ2 for trend; P value |
|---|---|---|---|---|
| Neuroticism on Pintner personality inventory | ||||
| Non-neurotic | 1183 | 21 (1.8) | 1.00 | 0.99; 0.32 |
| Mid-neurotic | 1042 | 19 (1.8) | 1.07 (0.50 to 2.25) | |
| Neurotic | 1026 | 23 (2.2) | 1.34 (0.67 to 2.68) | |
| Introversion on Pinter personality inventory | ||||
| Introvert | 975 | 24 (2.5) | 1.00 | 0.57; 0.45 |
| Ambivert | 1104 | 17 (1.5) | 0.83 (0.40 to 1.68) | |
| Extravert | 1172 | 22 (1.9) | 0.79 (0.39 to 1.60) | |
| Energy level at age 13 (teacher) | ||||
| Never tired | 233 | 1 (0.4) | 1.00 | 1.82; 0.18 |
| Normally energetic | 3026 | 62 (2.1) | 2.48 (0.34 to 18.12) | |
| Always tired | 187 | 5 (2.7) | 3.33 (0.37 to 30.08) | |
| Day dreaming in class at age 13 (teacher) | ||||
| Seldom or never | 1664 | 25 (1.5) | 1.00 | 4.77; 0.03 |
| Sometimes | 1602 | 36 (2.3) | 1.55 (0.84 to 2.87) | |
| Frequently | 212 | 8 (3.8) | 2.37 (0.88 to 6.33) | |
| Disobedience in class at age 13 (teacher) | ||||
| Seldom or never | 3145 | 64 (2.0) | 1.00 | 0.74; 0.4 |
| Sometimes | 321 | 321 (0.9) | 0.45 (0.19 to 1.02) | |
| Frequently | 26 | 2 (7.7) | 2.90 (0.77 to 10.93) | |
| Lying in class at age 13 (teacher) | ||||
| Seldom or never | 2926 | 55 (1.9) | 1.00 | 0.04; 0.83 |
| Sometimes | 483 | 13 (2.7) | 1.36 (0.61 to 2.60) | |
| Frequently | 49 | 1 (2.0) | 0.36 (0.05 to 2.71) | |
| Periods of absence (weeks) at ages 6-10 (school doctor) | ||||
| 0-2 | 855 | 14 (1.6) | 1.00 | 5.3; 0.02 |
| 3-4 | 717 | 9 (1.3) | 0.61 (0.22 to 1.69) | |
| 5-8 | 851 | 22 (2.6) | 1.66 (0.76 to 3.66) | |
| ⩾9 | 622 | 19 (3.1) | 1.75 (0.77 to 4.01) | |
| School absence at age 13 (teacher) | ||||
| Seldom or never | 824 | 12 (1.5) | 1.00 | 2.24; 0.13 |
| Sometimes | 888 | 13 (1.5) | 1.07 (0.41 to 2.79) | |
| Frequently | 851 | 24 (2.8) | 1.71 (0.70 to 4.14) |
lr = likelihood ratio test.
Odds ratios corrected for sex and father’s social class, weighted for sampling.
The outcome of children with pain is shown in table 3. Persistent abdominal pain in childhood was associated with psychiatric disorder, and this association remained after correction for potential confounders in an ordinal regression model. Childhood pain was only very weakly associated with abdominal pain and headache at 36 years but was associated with increasing numbers of physical symptoms at this age. Because there is a strong association between psychiatric disorder and physical symptoms, psychiatric disorder was added to the model, and this led to the association between persistent abdominal pain and physical symptoms in adulthood failing to reach significance. None of the children with persistent abdominal pain developed inflammatory bowel disease during the period of follow up. Only one subject with abdominal pain in childhood died over the follow up period, and this was lower than the rate for the rest of the cohort (hazard ratio (controlled for sex and social class) 0.15; 0.02 to 1.06).
Table 3.
Relation between childhood abdominal pain and adult psychiatric disorder and physical symptoms at age 36 years
| Outcome | No of children | No (%) with abdominal pain | Odds ratio (95% CI) * |
|---|---|---|---|
| Persistent abdominal pain | |||
| No | 2383 | 45 (1.9) | 1.30 (0.50 to 3.38) |
| Yes | 226 | 7 (3.1) | 1.03 (0.39 to 2.73)† |
| Persistent headache | |||
| No | 2045 | 38 (1.9) | 1.51 (0.73 to 3.13) |
| Yes | 563 | 14 (2.5) | 1.20 (0.57 to 2.56)† |
| Index of definition on present state examination | |||
| 1 | 1239 | 13 (1.1) | 2.72 (1.65 to 4.49)‡ |
| 2 | 811 | 19 (2.3) | |
| 3 | 225 | 9 (4.0) | |
| 4 | 158 | 5 (3.2) | |
| 5 | 129 | 1 (0.8) | |
| 6 | 24 | 4 (16.7) | |
| 7 | 6 | 1 (16.7) | |
| No of common somatic symptoms | |||
| 0 | 1312 | 20 (1.5) | 1.74 (1.04 to 2.92)‡ |
| 1 | 786 | 16 (2.0) | 1.39 (0.83 to 2.36)†‡ |
| 2 | 345 | 9 (2.6) | |
| 3 | 130 | 5 (3.9) | |
| 4 | 30 | 1 (3.3) | |
| 5 | 7 | 1 (14.3) |
Derived by logistic regression unless marked otherwise.
Corrected for psychiatric disorder at age 36 (see text).
Ordinal regression, corrected for sex, father’s social class, marital status at age 36, and educational status. Note that ordinal regression derives single odds ratio describing increased risk of having outcome in abdominal pain group compared with “no pain” group, independent of level of severity of outcome.
Discussion
This study used population based data to follow up a group of children with persistent abdominal pain over a period of 20 years. There were three main findings. Firstly, persistent abdominal pain in childhood was associated with physical ill health in the parents. Secondly, persistent abdominal pain in childhood did not predict abdominal pain in adulthood but was modestly associated with other common physical symptoms in adulthood. Thirdly, persistent abdominal pain in childhood was a predictor of psychiatric disorder in adulthood.
Methodological concerns
We were not able to define recurrent abdominal pain in the conventional manner. We believe, however, that our sample of children was likely to be symptomatic for much of childhood and to reflect clinical samples of children with recurrent abdominal pain. They were somewhat more likely to have been absent from school for long periods during middle childhood. The population base of this sample and the lack of differences in follow up rates for children with abdominal pain and those without make it unlikely that these results are due to selection bias. The results reported here compare those with persistent abdominal pain with children who never experienced pain. When those who had experienced pain once or twice in childhood were included in the control group the results were not substantially altered, although some of the odds ratios were slightly reduced (results not shown).
Family ill health and symptoms
The relation between sickness in the family and medically unexplained symptoms in adulthood has been reported in several retrospective studies. The relation between persistent abdominal pain present in childhood and ill health in the parents suggests that the parental anxiety and preoccupations with physical health may reinforce the child’s concern about physiological and minor medical bodily sensations. From the clinical viewpoint this suggests that in the treatment of children with persistent abdominal pain it is important to understand parental beliefs and experiences and to avoid behaviours that might reinforce pain behaviour in the child. This is a component of treatments which have been shown to be effective.4,21
While the parents of children with persistent abdominal pain were more likely to have psychiatric disorders, the children themselves did not seem especially maladjusted. They did not score especially high on neuroticism but were more likely to be “day dreamers” and there was a non-significant trend for them to be lacking in energy. These behaviours may be akin to inhibited traits (such as shyness, fearfulness, and being easily upset), which are recognised to be predictors of adult depression.22
So far as we know, this is the largest and longest follow up of abdominal pain in children to date. The survey members were growing up in the 1950s, and it is interesting to speculate whether the same associations would have been detected in a modern sample. With an increasingly health conscious population the parents of children with abdominal pain may be less readily reassured than they were 40 years ago. Modern medical advances may mean that these children would be more extensively investigated today than previously and that a proportion may avoid unnecessary operations, but it may also reinforce illness beliefs.
Overall the results suggest that the outcome in terms of symptoms of persistent pain is good. Though there is some evidence that persistent abdominal pain in childhood is associated with medically unexplained physical symptoms in adult life it is a more powerful predictor of adult psychiatric disorder. Apley’s “little belly-achers”13 do not grow up to be big belly achers but do grow up to suffer from anxiety or depression.
Figure.
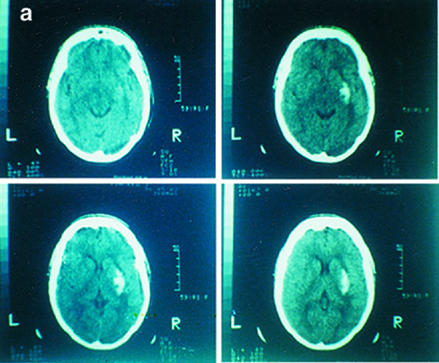
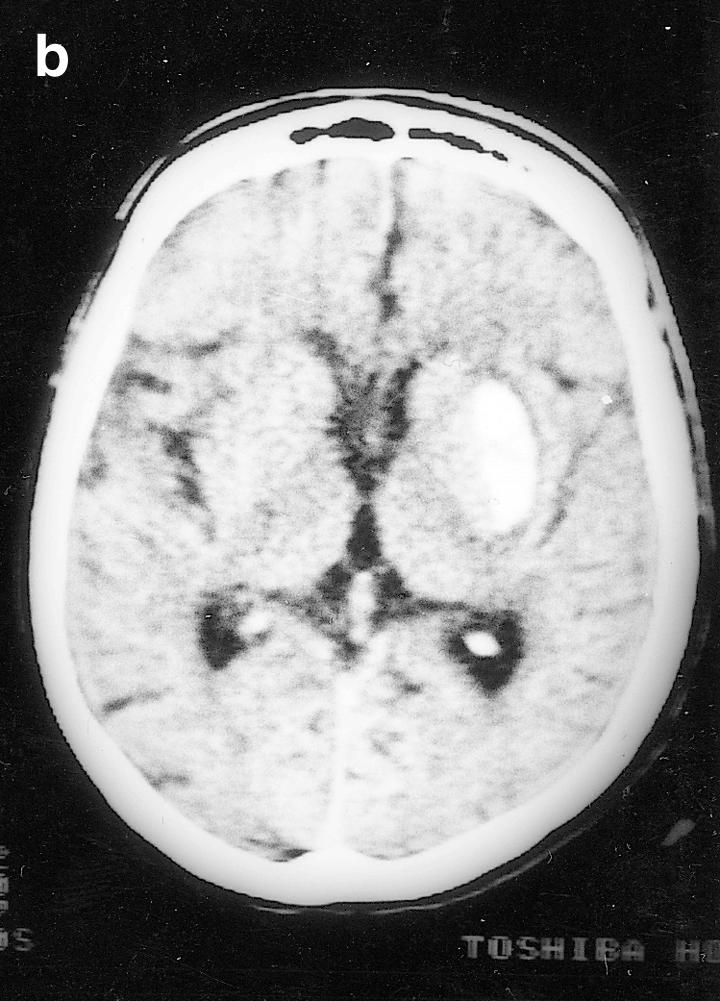
Computed tomograms showing putamen haemorrhage in case 1 (a) and case 2 (b)
Figure.
Computed tomograms showing putamen haemorrhage in case 1 (a) and case 2 (b)
Acknowledgments
We thank Warren Hilder and Erol Yusef for their assistance in data handling.
Footnotes
Funding: MH is a clinical training fellow funded by the Medical Research Council. The national survey of health and development is funded by the Medical Research Council.
Conflict of interest: None.
References
- 1.Apley J, Naish N. Recurrent abdominal pains: a field study of 1000 school children. Arch Dis Child 1957;165-70. [DOI] [PMC free article] [PubMed]
- 2.Goodman JE, McGrath PJ. The epidemiology of pain in children and adolescents: a review. Pain. 1991;46:247–264. doi: 10.1016/0304-3959(91)90108-A. [DOI] [PubMed] [Google Scholar]
- 3.Campo JV, Fritsch SL. Somatization in children and adolescents. J Am Acad Child Adol Psychiatry. 1994;33:1223–1235. doi: 10.1097/00004583-199411000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Scharff L. Recurrent abdominal pain in children: a review of psychological factors and treatment. Clin Psychol Rev. 1997;17:145–166. doi: 10.1016/s0272-7358(96)00001-3. [DOI] [PubMed] [Google Scholar]
- 5.Woodbury MM. Recurrent abdominal pain in child patients seen at a pediatric gastroenterology clinic. Psychosomatics. 1993;34:485–493. doi: 10.1016/S0033-3182(93)71822-8. [DOI] [PubMed] [Google Scholar]
- 6.Walker LS, Greene JW. Children with recurrent abdominal pain and their parents: more somatic complaints, anxiety, and depression than other patient families? J Pediatr Psychol. 1989;14:231–243. doi: 10.1093/jpepsy/14.2.231. [DOI] [PubMed] [Google Scholar]
- 7.Hodges K, Kline JJ, Barbero G, Flanery R. Depressive symptoms in children with recurrent abdominal pain and in their families. J Pediatr. 1985;107:622–626. doi: 10.1016/s0022-3476(85)80037-8. [DOI] [PubMed] [Google Scholar]
- 8.Garber J, Zeman J, Walker LS. Recurrent abdominal pain in children: psychiatric diagnoses and parental psychopathology. J Am Acad Child Adol Psychiatry. 1990;29:648–656. doi: 10.1097/00004583-199007000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Walker LS, Garber J, Greene JW. Psychosocial correlates of recurrent childhood pain: a comparison of pediatric patients with recurrent abdominal pain, organic illness and psychiatric disorders. J Abnorm Psychol. 1993;102:248–258. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- 10.Hodges K, Kline JJ, Barbero G, Flanery R. Life events occurring in families of children with recurrent abdominal pain. J Psychosom Res. 1984;28:185–188. doi: 10.1016/0022-3999(84)90018-7. [DOI] [PubMed] [Google Scholar]
- 11.Robinson JO, Alvarez JH, Dodge JA. Life events and family history in children with recurrent abdominal pain. J Psychosom Res. 1990;34:171–181. doi: 10.1016/0022-3999(90)90051-5. [DOI] [PubMed] [Google Scholar]
- 12.Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol. 1991;19:379–394. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- 13.Apley J, Hale B. Children with recurrent abdominal pains: how do they grow up? BMJ. 1973;iii:7–9. doi: 10.1136/bmj.3.5870.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Magni G, Pierri M, Donzelli F. Recurrent abdominal pain in children: a long term follow-up. Eur J Pediatr. 1987;146:72–74. doi: 10.1007/BF00647291. [DOI] [PubMed] [Google Scholar]
- 15.Christensen MF, Mortensen O. Long-term prognosis in children with recurrent abdominal pain. Arch Dis Child. 1975;50:110–114. doi: 10.1136/adc.50.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wadsworth MEJ, Mann SL, Rodgers B, Kuh DJL, Hilder WS, Yusef EJ. Loss and representativeness in a 43 year follow up of a national birth cohort. J Epidemiol Comm Health. 1992;46:300–304. doi: 10.1136/jech.46.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eysenck HJ. A short questionnaire to measure two dimensions of personality. J Appl Psychol. 1958;42:14–17. [Google Scholar]
- 18.Pintner R, Forlaner G. Four retests of a personality inventory. J Educ Psychol. 1938;29:93–100. [Google Scholar]
- 19.Wing JK, Cooper JE, Sartorius N. The measurement and classification of psychiatric symptoms. Cambridge: Cambridge University Press; 1974. [Google Scholar]
- 20.Scott SC, Goldberg MS, Mayo NE. Statistical assessment of ordinal outcomes in comparative studies. J Clin Epidemiol. 1997;50:45–55. doi: 10.1016/s0895-4356(96)00312-5. [DOI] [PubMed] [Google Scholar]
- 21.Sanders MR, Shepherd RW, Cleghorn G, Woolford H. The treatment of recurrent abdominal pain in children: a controlled comparison of cognitive-behavioral family intervention and standard pediatric care. J Cons Clin Psychol. 1994;62:306–314. doi: 10.1037//0022-006x.62.2.306. [DOI] [PubMed] [Google Scholar]
- 22.Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorder. Arch Gen Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]


