Although intracerebral haemorrhage causes prolonged or permanent focal neurological dysfunction, neurological deficits1 and lesions2 may sometimes resolve within a few days. To my knowledge no one has reported resolution of the symptoms and signs of intracerebral haemorrhage within 24 hours, although the possibility has been recognised.3 Intracerebral haemorrhage is therefore not considered to be a cause of transient focal neurological attacks and is not included in the differential diagnosis of transient ischaemic attacks.4 Clinicians tend to diagnose transient ischaemic attacks on symptoms alone and to start antiplatelet drug treatment pending the results of computed tomography. This is particularly the case in developing countries where computed tomography is scarce. I report two cases of intracerebral haemorrhage in which the focal neurological symptoms and signs resolved within 24 hours.
Case reports
Case 1—
A 58 year old woman awoke one night with a numbness and weakness of her left arm and leg. By the morning these had slightly improved. Her doctor diagnosed a transient ischaemic attack. She started aspirin treatment and was advised to see a specialist. By evening she was admitted to hospital. On examination her symptoms had resolved completely and she did not have weakness or sensory impairment. A computed tomogram showed a small intracerebral haemorrhage in the region of the putamen (figure a).
•
Case 2
—A 65 year old man was admitted 2 hours after he had developed a headache, weakness of the left arm and leg, deviation of the mouth, and slurring of speech. He had a history of hypertension and had been drinking alcohol excessively during the 2 weeks before admission. His blood pressure was 190/100 mm Hg—he had recently stopped taking antihypertensive drugs. He had a mild facial weakness and weakness of the left arm and leg. He was unable to use his left hand to button his shirt, and he dragged his leg when walking. He did not have sensory impairment or a hemianopia. A computed tomogram showed a small intracerebral haemorrhage in the region of the putamen (figure b). The next morning he was symptom free and did not have any weakness on testing.
Comment
The possibility that symptoms and signs of small intracerebral haemorrhages can resolve within 24 hours has been recognised.3 Although rare, clinicians should be aware that an intracerebral haemorrhage may cause a transient neurological deficit. To start antiplatelet drugs before having the results of computed tomography may be illogical in such cases although I know of no reports of patients with intracerebral haemorrhage becoming worse clinically after receiving aspirin. A computed tomogram should, however, be mandatory before starting anticoagulant treatment in any patient with features of transient ischaemic attack. It is also rational management to arrange computed tomography early in patients who have started antiplatelet treatment as features of an intracerebral haemorrhage may not be apparent on a late scan. Thus if patients with transient focal neurological symptoms are to be treated appropriately they should have computed tomography soon after the onset of symptoms.
Figure.
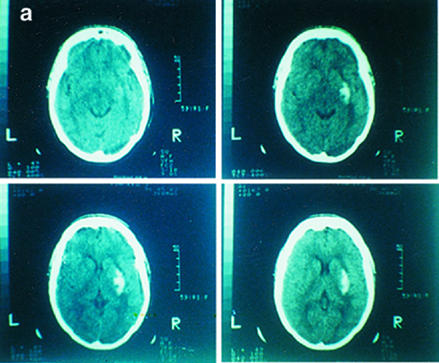

Computed tomograms showing putamen haemorrhage in case 1 (a) and case 2 (b)
Footnotes
Funding: None.
Conflict of interest: None.
References
- 1.Scott WR, Miller BR. Intracerebral haemorrhage with rapid recovery. Arch Neurol. 1985;42:133–136. doi: 10.1001/archneur.1985.04060020043013. [DOI] [PubMed] [Google Scholar]
- 2.Dennis MS, Bamford JM, Molyneux AJ, Warlow CP. Rapid resolution of signs of primary intracerebral haemorrhage in computed tomograms of the brain. BMJ. 1987;295:379–381. doi: 10.1136/bmj.295.6594.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hankey GJ, Warlow CP. Transient ischaemic attacks of the brain and eye. In: Warlow CP, Van Gijn J, editors. Major problems in neurology. Vol. 27. Philadelphia: Saunders; 1994. [Google Scholar]
- 4.Warlow CP, Dennis MS, van Gijn J, Hankey GJ, Sandercock PAG, Bamford JM, et al. Stroke—a practical guide to management. Oxford: Blackwell Science; 1996. [Google Scholar]


