Abstract
Objective
To examine the relationship between alcohol consumption and risk of mortality and incident coronary heart disease (CHD) taking account of variation in intake during follow up
Method
Prospective cohort study of 5,411 male civil servants aged 35-55 years at entry to the Whitehall II study in 1985-88. Alcohol consumption was reported five times over a 15 year period. Mortality, fatal CHD, clinically verified incident non-fatal myocardial infarction and definite angina were ascertained during follow-up.
Results
We found evidence that drinkers who vary their intake during follow-up, regardless of average level, have increased risk of total mortality (hazard ratio of high versus low variability 1.52: 95% CI 1.07 to 2.17), but not of incident CHD. Using average consumption level, as opposed to just a baseline measure, gave slightly higher risk estimates for CHD compared to moderate drinkers, at the extremes of the drinking range.
Conclusions
Multiple repeated measures are required to explore the effects of variation in exposure over time. Caution is needed when interpreting risks of exposures measured only once at baseline, without consideration of changes over time.
Introduction
The lower risk of coronary heart disease (CHD) associated with moderate alcohol consumption has been widely reported1,2,3,4 and the U-shaped curve seen with all-cause mortality owes much to its cardioprotective attributes.2,5 Suggested mechanisms include favourable changes in lipids and haemostatic factors,6 inhibition of platelet reactivity,7 lower levels of inflammation8 and improved vascular function.9
Much of the evidence comes from prospective cohort studies. Exposure to alcohol is typically measured among participants at baseline and health outcomes are tracked during the follow up period. It is assumed that the initial consumption level reported at baseline is an accurate measure of exposure throughout the study period (which may be several decades). However, there is evidence from descriptive alcohol studies that consumption levels change throughout the lifecourse.10,11,12 Large, longitudinal datasets with repeated measures on the same individuals are needed in order to explore whether the chronic health consequences of alcohol consumption are affected by varying intake during follow-up. Such studies are rare13 and most only have two measures of alcohol.14,15,16,17,18. Estimates of change derived from two time points will not provide an accurate exposure assessment during follow-up. Multiple repeated measures are also needed to establish the heterogeneity of the “non-drinking” group as the concern that non-drinkers will include former drinkers who quit due to ill-health is now well founded.14,19,20
In this paper we attempt to look at the affect of alcohol on CHD and mortality risk utilizing repeated measures of alcohol intake. First, we use a baseline exposure; secondly, we use an average alcohol exposure level during follow-up and finally we compare consistent drinkers with those who vary their intake over time. The Whitehall II cohort has repeated measures of socioeconomic and behavioural factors, including 5 measures of alcohol consumption, from early midlife over a 15 year period. It also has detailed phenotypic measures every five years (biological risk factors, measures of sub-clinical disease and disease endpoints) and objective and subjective measures of physical and mental functioning.
Methods
The Whitehall II study was established in 1985 as a longitudinal study to examine the socioeconomic gradient in health and disease among 10,308 civil servants (6,895 men and 3,413 women). Full details of the cohort and its follow up have been published elsewhere.21 All civil servants aged 35-55 years in 20 London based departments were invited to participate by letter and 73 percent of those invited agreed to take part. Baseline examination (Phase 1) took place during 1985-1988, and involved a clinical examination and a self-administered questionnaire containing sections on demographic characteristics, health, lifestyle factors, work characteristics, social support and life events. Subsequent phases of data collection have alternated between postal questionnaire alone and postal questionnaire accompanied by a clinical examination. The University College London ethics committee approved the study.
The analyses in this paper were restricted to those who were free of CHD at baseline and to men as there were too few CHD events in women. Participants had to have attended three or more phases in order to look at variability in alcohol intake and therefore, follow-up for incident events and mortality was from phase 3 onwards.
Alcohol consumption
At baseline (1985-88), phase 2 (1989-90), phase 3 (1991-94), phase 5 (1997-99), and phase 7 (2003-04) participants were asked to report the frequency of their drinking over the last 12 months by circling one of six specified options (twice a day or more/ almost daily/ once or twice a week/ once or twice a month/ special occasions only/ none). Participants were then asked to report the number of alcoholic drinks they had consumed in the last seven days. This was divided into “measures” of spirits, “glasses” of wine, and “pints” of beer. In the UK a standard measure of spirit and a small glass of wine are considered to contain 8 grams of alcohol, whilst a pint of beer typically contains 16 grams of alcohol. The amounts were converted to units (one unit is 8 grams alcohol) and grouped into seven levels, from 0-6, as:- 0=no units in past week, 1=1-7, 2=8-14, 3=15-21, 4=22-28, 5=28-35, 6=36+. These levels were used as the basis for calculating average alcohol intake and variability in alcohol intake and ensured that participants with very high alcohol intakes were not too influential in the analyses.
Average alcohol intake
To minimise the affects of reverse causality, only those alcohol measurements which were available prior to any CHD incidence were used by setting all other alcohol measurements as missing. The average alcohol consumption was then calculated by averaging the grouped alcohol levels for those participants who had three or more non-missing alcohol measurements remaining. These averaged levels were then partitioned into seven alcohol categories (0=0.0-0.4, 1=0.5-1.4, 2=1.5-2.4, 3=2.5-3.4, 4=3.5-4.4, 5=4.5-5.4, 6=5.5-6.0). The 112 participants who reported on three or more separate occasions that their alcohol frequency in the last year was ‘none’ were deemed to be ‘never’ drinkers and have been excluded from all analyses. These exclusions resulted in a sample size of 5,411 men.
Variability in alcohol intake
Variability in alcohol intake was calculated (for the same participants for which average alcohol was computed) by calculating the standard deviation of the grouped alcohol levels. Participants were classified as having low alcohol variability (SD≤ 0.5), medium variability (0.5<SD≤ 1.1) or high alcohol variability (SD>1.1).
Sensitivity analyses
All analyses have excluded alcohol measures that were reported after any CHD events had occurred. Nevertheless, the use of alcohol measures obtained during the period of follow-up for events could still introduce bias into our estimates since these measures are only used for participants while they remain free from CHD. We therefore repeated all the analyses using only those alcohol measures reported during Phases 1, 2 and 3 prior to the start of the follow-up period for events. We defined average alcohol intake and alcohol variability using the same cut-points as in the main analyses but excluded a further 49 men who had insufficient alcohol measures.
In recognition that drink sizes have increased and that those poured at home may be larger measures,22 we also assessed the sensitivity of the results to the assumption that spirit and wine drinks contain 1 unit, by repeating all the analyses assuming that spirit and wine drinks contain 2 units.
Outcome measures
Information on mortality was ascertained through the National Health Services Central Registry, by using their unique NHS identification number. Follow-up for total mortality was available up to the end of April 2009. CHD incidence was based on clinically verified events and included fatal CHD (ICD9 codes 410-414 or ICD10 I20-25) from the mortality follow-up or incident non fatal myocardial infarction (MI). Non-fatal MI was defined following MONICA criteria23 based on questionnaires, study electrocardiograms, hospital acute ECGs, cardiac enzymes and physician records. Classification of MI was carried out blind to other study data, independently by two trained coders, with adjudication by a third in the (rare) event of disagreement. Angina was assessed on the basis of participants' reports of symptoms and diagnoses with corroboration in medical records or abnormalities on a resting ECG, exercise ECG, or coronary angiogram. Outcomes based solely on self-reported data were not included in the analyses. Follow-up for incident CHD was available to the end of Phase 7 (September 2004).
Statistical methods
The associations between baseline, average and variability of alcohol intakes on incident CHD and total mortality were assessed using hazard ratios and 95% confidence intervals estimated from Cox proportional hazard models using follow-up time from phase 3 as the underlying time variable. Analyses using age as the underlying time variable gave virtually the same estimates as those presented. For analyses of baseline and average alcohol intake the reference group was set as 8-14 units of alcohol per week. Age adjusted means and percentages across the variability in alcohol intake groups were computed using least squares means and direct standardisation respectively. Trends in these estimates were tested using a linear trend term for alcohol variability in the regression models for the continuous variables and the Cochran-Mantel-Haenszel test for the dichotomous variables.
Results
The extent of variation in drinking level during follow-up is summarised in Table 1. The majority of men reported the same level of consumption at subsequent follow-ups (percentages shown in bold in the table) or shifted only one or two categories. A small proportion reported changing from high consumption to very low or vice versa.
Table 1.
Change in alcohol consumption between phases (row percentages):
| Nth follow-up: Units per week |
N+1th follow up: units per week |
|||||||
|---|---|---|---|---|---|---|---|---|
| None | 1-7 | 8-14 | 15-21 | 22-28 | 29-35 | ≥36 | Total* | |
| None | 47.3 | 39.0 | 8.7 | 2.9 | 1.0 | 0.6 | 0.6 | 1455 |
| 1-7 | 13.0 | 53.8 | 24.2 | 5.6 | 2.4 | 0.5 | 0.5 | 4294 |
| 8-14 | 3.6 | 24.8 | 40.2 | 19.6 | 8.3 | 1.9 | 1.6 | 3140 |
| 15-21 | 2.3 | 7.8 | 26.6 | 29.9 | 21.3 | 7.0 | 5.2 | 1770 |
| 22-28 | 2.2 | 4.0 | 15.2 | 25.0 | 31.1 | 11.0 | 11.6 | 1160 |
| 29-35 | 2.4 | 4.9 | 8.2 | 16.4 | 11.1 | 36.0 | 21.0 | 675 |
| ≥36 | 2.3 | 2.1 | 5.0 | 8.4 | 7.4 | 8.5 | 66.2 | 1092 |
Each person can contribute more than once to this table
Row percentages may not total 100% due to rounding
Drinkers with higher variability in their alcohol intake during follow-up were found to be slightly younger, more likely to smoke and to have higher average alcohol intake than those with more stable intake (table 2). There was no difference in terms of risk of CHD when comparing high/medium variability drinkers to more stable drinkers. However high variability drinkers had a 52% higher mortality hazard than stable drinkers, after adjustment for average alcohol intake during follow-up and smoking at baseline (table 3). In post-hoc analyses we further explored this high variability group. The group was sub-divided into three groups according to whether the trend in participants' alcohol consumption across the five phases: (i) decreased, (ii) showed no trend or (iii) increased. Compared to low variability drinkers, the mortality hazard ratios in these three groups were 2.11 (1.35-3.31), 1.34 (0.79-2.26) and 1.28 (0.82-2.00) respectively.
Table 2.
Characteristics of different variability in alcohol intake groups
| Alcohol intake variability |
||||
|---|---|---|---|---|
| Baseline characteristics | Low | Medium | High | P-value |
| No. of men | 1686 | 2556 | 1169 | |
| Mean Age (y) | 44.3 | 43.9 | 43.1 | <0.001 |
| High employment grade (%)* | 38.2 | 42.4 | 37.2 | 0.92 |
| Current smoker* | 12.3 | 12.8 | 18.5 | <0.001 |
| Average alcohol consumption (unit/wk)* | 10.8 | 12.8 | 20.3 | <0.001 |
adjusted for age
Table 3.
Hazard ratios of incident CHD and all cause mortality by alcohol variability group – adjusted for age, average alcohol intake during follow-up and smoking at baseline
| Alcohol variability |
|||
|---|---|---|---|
| Outcome | Low (N=1686) |
Medium (N=2556) |
High (N=1169) |
| Fatal CHD / Non-fatal MI | |||
| No. events | 62 | 85 | 28 |
| Hazard ratio (95% CI) | 1.0 | 1.05 (0.74-1.49) | 0.80 (0.47-1.36) |
| All CHD (excluding self-reported) | |||
| No. events | 119 | 169 | 68 |
| Hazard ratio (95% CI) | 1.0 | 1.08 (0.83-1.38) | 1.06 (0.74-1.51) |
| Total mortality | |||
| No. events | 118 | 145 | 82 |
| Hazard ratio (95% CI) | 1.0 | 1.00 (0.77-1.29) | 1.52 (1.07-2.17) |
Sensitivity analyses (not shown) using only the measures of alcohol reported at Phases 1, 2 and 3 showed similar results to those reported above. In additional sensitivity analyses where we increased the number of units in wine and spirits, the finding that high variability drinkers with a downward trend in alcohol intake are at increased risk of mortality was even stronger. Compared to low variability drinkers, the mortality hazard ratios in those with downward trend, no trend and increasing trend were 1.75 (1.13-2.72), 1.04 (0.63-1.71) and 1.12 (0.72-1.71) respectively.
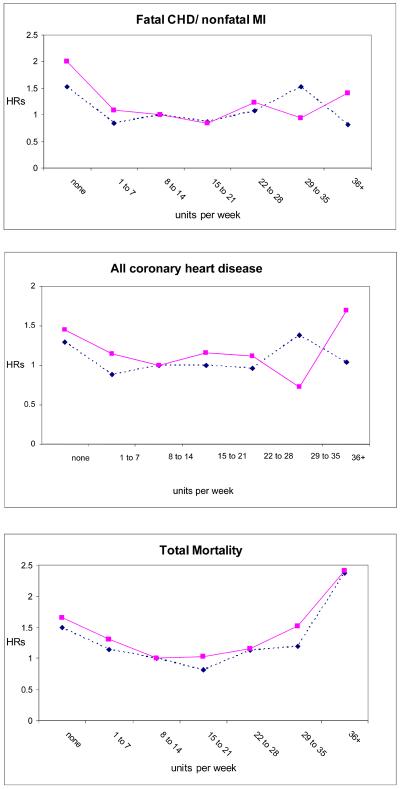
A comparison of the associations between baseline and average alcohol levels with CHD outcomes and total mortality is shown in figure 1. The relationships with CHD and total mortality are similar using either measure, although there is a suggestion that the CHD risks, compared to the moderate drinkers (8-14 units per week), are underestimated at the extremes of consumption (none and more than 35 units per week) when using baseline measures alone.
Fig 1.
Hazard ratios† (HRs) for CHD and all-cause mortality using baseline (dotted line) and average (solid line) alcohol consumption among drinkers
† Reference category for hazard ratios is the 8 – 14 units per week group (moderate drinkers)
Discussion
We found that, independent of average levels, drinkers with variable alcohol intake during follow-up, have an increased risk of total mortality, but not of incident CHD. This finding needs to be confirmed or refuted by other studies and it raises interesting questions such as whether there is a direct biological effect of the variability in alcohol intake, perhaps including periods of more heavy drinking, or whether there are other confounding factors in the relationship with mortality. We found evidence to suggest that the higher mortality risk among those with high variability in drinking was mainly due to those participants whose drinking was on a downward trend over time. These men may be “sick-quitters” who have decreased their alcohol drinking concomitant with disease. If only baseline measures of alcohol are used, these effects will be missed.
We also show that using average consumption level, as opposed to just a baseline measure gave slightly higher risk estimates, compared to the moderate drinkers, for CHD, particularly at the extremes of the drinking range. This is partly supported by an earlier study by Emberson et al who used data from the British Regional Heart Study.13 With 5 measures of alcohol intake, they showed that risks for CHD, stroke and all cause mortality among moderate and heavy drinkers compared to light drinkers were increased when looking at average consumption versus baseline consumption. That different risk estimates are found when change in consumption is taken into consideration is supported by others14, 17 and this reinforces the need for studies with multiple repeated measures so that variation can be explored.
There are several limitations with our study. First, we do not have enough statistical power, at present, to explore gender effects and were forced to restrict the analyses to men. In future, when more deaths and CHD events accrue among the women we will repeat the analyses.
Second, although our study spans some 15 years, the participants were all aged over 34 years at entry. The risk function differences between baseline and repeated alcohol measures are likely to be much larger when a broader age range is included. Descriptive studies have shown that baseline measures of drinking are especially unreliable for younger samples, longer follow-ups and heavier drinkers.24 Whilst our study is a population based cohort and includes a range of socio-economic backgrounds, the participants do not exhibit extremes in drinking behaviour. All were in employment and based around London. It would be informative to explore much heavier drinkers and to look at patterns of drinking in addition to average intake reported per week.
Third, restricting our analyses to those who had participated in three or more data collection phases, in order to assess variability in consumption, resulted in a healthier sub-sample of the original cohort. This raises the problem of how to look at individual level change in prospective cohort studies without being subjected to the potential biases that arise with selective attrition.25
A particular strength of our study is that we were able to identify “non-drinkers” more accurately than most studies. Respondents who repeatedly (with a minimum of three occasions) reported to have consumed no alcohol in the last 12 months were deemed to be “non-drinkers” and were excluded from the analyses. This meant that the lightest drinking group (none in the past week) were not abstainers. This is important as it has been shown that abstainers may have very different health profiles to drinkers which makes for a difficult assessment of the biological effects of alcohol intake.26
In conclusion, we have shown, using one of the very few datasets with multiple repeated alcohol measures, long follow-up and verified CHD endpoints, that it is important not to rely on baseline measures alone. This observation is likely to be more important in cohorts with a broader age range and less stable consumption. The implications of our findings are relevant for many causal investigations using prospective cohort studies and caution is needed when interpreting risks of exposures measured only once at baseline, without consideration of changes over time.
Acknowledgements
We thank all participating men and women in the Whitehall II Study; all participating Civil Service departments and their welfare, personnel, and establishment officers; the Occupational Health and Safety Agency; and the Council of Civil Service Unions. The Whitehall II Study team comprises research scientists, statisticians, study coordinators, nurses, data managers, administrative assistants and data entry staff, who make the study possible.
The Whitehall II study is supported by grants from the Medical Research Council; British Heart Foundation; Department of Health; National Heart Lung and Blood Institute, US, NIH; National Institute on Aging, US, NIH. The funding sources had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
Conflict of interest: None.
References
- 1.Corrao G, Rubbiati L, Bagnardi V, et al. Alcohol and coronary heart disease: a meta-analysis. Addiction. 2000;95:1505–1523. doi: 10.1046/j.1360-0443.2000.951015056.x. [DOI] [PubMed] [Google Scholar]
- 2.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to alcohol consumption: a prospective study among male British doctors. Int J Epidemiol. 2005;34:199–204. doi: 10.1093/ije/dyh369. [DOI] [PubMed] [Google Scholar]
- 3.Thun MJ, Peto R, Lopez AD, et al. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Eng J Med. 1997;337:1705–14. doi: 10.1056/NEJM199712113372401. [DOI] [PubMed] [Google Scholar]
- 4.Doll R, Peto R, Hall E, Wheatley K, Gray R. Mortality in relation to consumption of alcohol: 13 years' observations on male British doctors. Br Med J. 1994;309:911–18. doi: 10.1136/bmj.309.6959.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marmot MG, Rose G, Shipley MJ, Thomas BJ. Alcohol and mortality: a U-shaped curve. Lancet. 1981;1:580–3. doi: 10.1016/s0140-6736(81)92032-8. [DOI] [PubMed] [Google Scholar]
- 6.Rimm EB, Williams P, Fosher K, et al. Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. Br Med J. 1999;319:1523–1528. doi: 10.1136/bmj.319.7224.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Renaud S, de Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet. 1992;339:1523–6. doi: 10.1016/0140-6736(92)91277-f. [DOI] [PubMed] [Google Scholar]
- 8.Stewart SH. Alcohol and inflammation: a possible mechanism for protection against ischemic heart disease. Nutr Metab Cardiovasc Dis. 2002;12:148–51. [PubMed] [Google Scholar]
- 9.Mattace-Raso FUS, van der Cammen TJM, van den Elzen APM, et al. Moderate alcohol consumption is associated with reduced arterial stiffness in older adults: the Rotterdam Study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2005;60:1479–1483. doi: 10.1093/gerona/60.11.1479. [DOI] [PubMed] [Google Scholar]
- 10.Midanik LT, Klatsky AL, Armstrong MA. Changes in drinking behaviour: demographic, psychosocial, and biomedical factors. Int J Addiction. 1990;25:599–619. doi: 10.3109/10826089009061323. [DOI] [PubMed] [Google Scholar]
- 11.Mulder M, Ranchor AV, Sanderman R, Bouma J, van den Heuvel WJA. The stability of lifestyle behaviour. Int J Epidemiol. 1998;27:199–207. doi: 10.1093/ije/27.2.199. [DOI] [PubMed] [Google Scholar]
- 12.Fillmore KM. Prevalence, incidence and chronicity of drinking patterns and problems among men as a function of age: a longitudinal and cohort analysis. Br J Addiction. 1987;82:77–83. doi: 10.1111/j.1360-0443.1987.tb01440.x. [DOI] [PubMed] [Google Scholar]
- 13.Emberson JR, Shaper AG, Wannamethee SG, Morris RW, Whincup PH. Alcohol intake in middle age and risk of cardiovascular disease and mortality: accounting for intake variation over time. Am J Epidemiol. 2005;161:856–863. doi: 10.1093/aje/kwi111. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus NB, Kaplan GA, Cohen RD, Leu D-J. Change in alcohol consumption and risk of death from all causes and from ischaemic heart disease. Br Med J. 1991;303:553–6. doi: 10.1136/bmj.303.6802.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wannamethee SG, Shaper AG. Taking up regular drinking in middle age: effect on major coronary heart disease events and mortality. Heart. 2002;87:32–36. doi: 10.1136/heart.87.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fillmore KM, Kerr WC, Bostrom A. Changes in drinking status, serious illness and mortality. J Stud Alcohol. 2003;64:278–285. doi: 10.15288/jsa.2003.64.278. [DOI] [PubMed] [Google Scholar]
- 17.Gronbaek M, Johansen D, Becker U, Hein HO, Schnohr P, Jensen G, Vestbo J, Sorensen TIA. Changes in alcohol intake and mortality. A longitudinal population-based study. Epidemiology. 2004;15:222–228. doi: 10.1097/01.ede.0000112219.01955.56. [DOI] [PubMed] [Google Scholar]
- 18.Wellmann J, Heidrich J, Berger K, Doring A, Heuschmann PU, Keil U. Changes in alcohol intake and risk of coronary heart disease and all-cause mortality in the MONICA/KORA-Augsburg cohort 1987-97. European J Cardiovascular Prevention and Rehabilitation. 2004;11:48–55. doi: 10.1097/01.hjr.0000118174.70522.20. [DOI] [PubMed] [Google Scholar]
- 19.Shaper AG, Wannamethee SG. Alcohol and cardiovascular diseases. Wiley; Chichester: 1998. The J-shaped curve and changes in drinking habit; pp. 173–192. Novartis Foundation Symposium 216. [DOI] [PubMed] [Google Scholar]
- 20.Fillmore KM, Stockwell T, Chikritzhs, Bostrom A, Kerr W. Moderate alcohol use and reduced mortalitiy risk: systematic error in prospective studies and new hypotheses. Ann Epidemiol. 2007;17:S16–S23. doi: 10.1016/j.annepidem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 21.Marmot M, Smith GD, Stansfeld S, Patel C, North F, Head J, White I, Brunner E, Feeney A. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337:1387–93. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- 22.Gill JS, Donaghy M. Variation in the alcohol content of a ‘drink’ of wine and spirit poured by a sample of the Scottish population. Health Educ. Res. 2004;19(5):484–491. [PubMed] [Google Scholar]
- 23.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, et al. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 24.Kerr WC, Fillmore KM, Bostrom A. Stability of alcohol consumption over time: evidence from three longitudinal surveys from the United States. J Stud Alcohol. 2002;63:325–33. doi: 10.15288/jsa.2002.63.325. [DOI] [PubMed] [Google Scholar]
- 25.Grenfield TK, Kerr WC. Tracking alcohol consumption over time. Alcohol Research and Health. 2003;71:30–38. [PMC free article] [PubMed] [Google Scholar]
- 26.Rehm J, Irving H, Ye Y, Kerr WC, Bond J, Greenfield TK. Are lifetime abstainers the best control group in alcohol epidemiology? On the stability and validity of reported lifetime abstention. Am J Epidemiol. 2008;168:866–71. doi: 10.1093/aje/kwn093. [DOI] [PMC free article] [PubMed] [Google Scholar]