Short abstract
Adrenaline (epinephrine) is the recommended first line treatment for patients with anaphylaxis. This review discusses the safety and efficacy of adrenaline in the treatment of anaphylaxis in the light of currently available evidence. A pragmatic approach to use of adrenaline auto-injectors is suggested.
Anaphylaxis is the clinical syndrome representing the most severe systemic allergic reactions. Mediator release results in smooth muscle contraction, vasodilation, increased vascular permeability, and activation of vagal pathways, leading to the classic features of anaphylaxis, including urticaria and angioedema, bronchoconstriction and hypotension. Owing to the nature of anaphylaxis there are few controlled clinical trials, and therapeutic recommendations are based on clinical observation and animal models. We look at the current evidence for the use of adrenaline (epinephrine) in anaphylaxis, including its safety and route and timing of administration. We also discuss adrenaline auto-injectors and their role in patients with anaphylaxis.
Methods
We searched Medline using the key words adrenaline, anaphylaxis, epinephrine, and Epipen, and articles from the authors' personal collection. When necessary we accessed cross references and related articles. Evidence has been graded, where possible (see bmj.com). Only studies with clinical outcomes have been classified (see table on bmj.com); those showing in vitro improvements have not been graded.
Anaphylaxis
Anaphylaxis is a severe, life threatening systemic reaction that can affect all ages. The clinical syndrome may involve multiple target organs, including skin, respiratory, gastrointestinal, and cardiovascular systems. The essential underlying mechanism is the presence of biologically active chemical mediators released from mast cells or basophils.1 If this occurs in the context of a classic IgE mediated reaction from previously sensitised mast cells or basophils then anaphylactic reaction is the preferred term. Degranulation of mast cells or basophils may also occur in non-IgE mediated mechanisms, and these reactions are termed anaphylactoid reactions. Clinically it is not possible to distinguish the two, and treatments for both mechanisms are identical. Invalid assumptions of an anaphylactoid cause have led to fatal re-exposure.2
Summary points
Anaphylaxis is a severe life threatening reaction that can affect all age groups
The severity of previous reactions does not predict the severity of subsequent reactions
Intramuscular adrenaline is the first line treatment for anaphylaxis, with intravenous adrenaline reserved for unresponsive anaphylaxis or circulatory collapse
Early use of adrenaline in anaphylaxis is associated with improved outcomes
Any patient with a systemic allergic reaction should be considered for an adrenaline auto-injector, depending on risk of further reactions
There is a clear need to improve education of both patient and physician on the use of and indications for adrenaline auto-injectors
Anaphylaxis occurs in an acute and unexpected manner. The true incidence is unknown. Epidemiological studies have shown differing results owing to differences in both definitions of anaphylaxis and the population groups studied. A retrospective population based study in Olmsted County, United States showed an incidence of 21 cases per 100 000 person years.3 A retrospective study in a UK accident and emergency department suggested an incidence of between 1 in 2300 and 1 in 1500 attendances, and retrospective analysis in a US emergency room has shown an incidence of 1 in 1100 attendances.4,5 Most data for the incidence have been derived from hospital databases, and it is widely believed anaphylaxis is under-recognised and under-reported.5-7 Anaphylaxis remains an important cause of mortality. Of 164 fatal reactions identified between 1992 and 1998 in the United Kingdom, around half were iatrogenic.8 Of the non-iatrogenic causes, half were related to venom (for example, wasp sting) and most of the remainder to food.
Adrenaline has physiological benefits in the treatment of anaphylaxis: stimulation of α adrenoceptors increases peripheral vascular resistance thus improving blood pressure and coronary perfusion, reversing peripheral vasodilation, and decreasing angioedema. Stimulation of β1 adrenoceptors has both positive inotropic and chronotropic cardiac effects. Stimulation of β2 receptors causes bronchodilation as well as increasing intracellular cyclic adenosine monophosphate production in mast cells and basophils, reducing release of inflammatory mediators.9 However, given the speed of onset, the often unexpected occurrence and rapid response to treatment, there are few controlled clinical trials in acute anaphylaxis, and this is unlikely to change. Most treatment recommendations have therefore been based on clinical observation, interpretation of the pathophysiology and, to an extent, animal models.9 w1
Adrenaline
Is adrenaline safe?
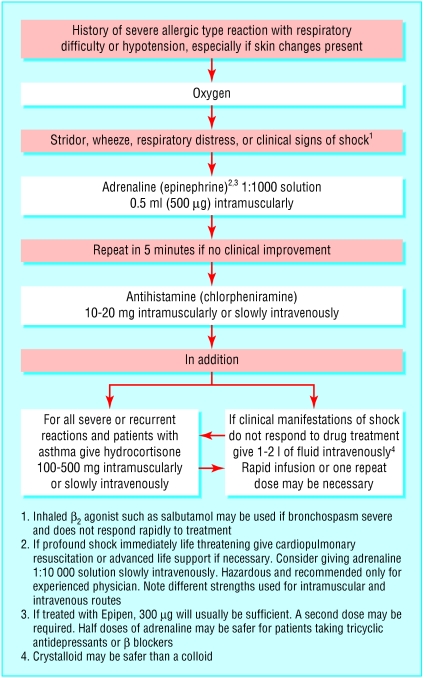
Adrenaline is the recommended first line treatment in anaphylaxis (fig 1).10 Confusion arises because systemic allergic reactions can be mild, moderate, or severe. For example, generalised angioedema and urticaria without airway involvement would not be described as anaphylaxis. A good working definition is that an anaphylactic reaction involves one or both of the two severe features: respiratory difficulty (which may be due to laryngeal oedema or asthma) and hypotension (which may present as fainting, collapse, or loss of consciousness). Inappropriate use of adrenaline may be dangerous. Most adverse events with adrenaline usage occur when it is given in overdose or intravenously. Those particularly at risk include elderly patients and patients with hypertension, arteriopathies, or known ischaemic heart disease.7,8,10 w2 w3 As there are no controlled trials there is no way to estimate the risk in relation to benefit. Based on the current evidence, the benefit of using appropriate doses of intramuscular adrenaline far exceeds the risk (grade C). It should be stressed that adrenaline is not contraindicated in individuals with underlying ischaemic heart disease, as the decrease in filling pressure due to anaphylaxis is likely to result in further coronary ischaemia (grade C).1 Careful monitoring and avoidance of adrenaline overdose is necessary in these patients.
Fig 1.
Algorithm for the treatment of anaphylaxis. Reproduced with permission of UK Resuscitation Council
What is the best route for administering adrenaline?
Subcutaneous and intramuscular routes
The correct route of administration and dose of adrenaline has been under debate. One study showed that subcutaneous administration of adrenaline was associated with a striking difference in the time of maximum plasma adrenaline concentrations of children compared with the intramuscular route (average time: intramuscular group, 8 minutes; subcutaneous group, 34 minutes).11 The average maximum plasma concentration was also significantly higher for the intramuscular group than for the subcutaneous group, and this has been shown elsewhere (grade B).11,12
Inhaled adrenaline
Studies using inhaled adrenaline by way of a pressurised aerosol have given conflicting results.w4-w6 One report showed that adrenaline was present systemically after an inhaled 3 mg dose but not after 1.5 mg and that the clinical effect was less pronounced and shorter lasting than by subcutaneous injection.w4 Other studies have shown the reverse.w6 No direct comparisons have been made between the inhaled and intramuscular route. Such findings have only been shown in healthy volunteers and have, as yet, not been confirmed in patients during anaphylaxis.
Intravenous route
Intravenous adrenaline has been associated with the induction of fatal cardiac arrythmias and myocardial infarction. Major adverse effects usually occur when adrenaline has been given too rapidly, inadequately diluted, or in excessive dose (grade C).1,2,8,9 Such published reports often fail to state clearly that other factors, including hypoxia, acidosis, or the direct action of inflammatory mediators, may be, at least in part, responsible for the cardiovascular complications. Given all of this, the intravenous route should be reserved for those with unresponsive anaphylaxis. This includes any patient who deteriorates despite receiving intramuscular adrenaline or those in whom there is doubt about the circulation. It should only be given in a resuscitation area during electrocardiography by medical staff who are trained in its use (grade C).7
What dose of adrenaline is appropriate?
Some disagreement exists about the recommended dose of adrenaline. Although almost all of the literature agrees on 0.01 mg/kg in infants and children, North American guidelines suggest a dose in adults of 0.3-0.5 ml of adrenaline diluted 1:1000 (0.3-0.5 mg), whereas European literature suggests 0.5-1.0 mg.13 w1 w7 No comparative trials have been conducted. For most patients only one dose is needed, although repeat doses may be given at five minute intervals until symptoms improve.
Does adrenaline have any important drug interactions?
Anaphylaxis may be made worse by β blockers, and these drugs decrease the effectiveness of adrenaline (grade C).14 Paradoxically the dose of adrenaline should be halved owing to the increased risks associated with unopposed stimulation of α adrenoceptors and reflex vagotonic effects, including bradycardia, hypertension, coronary artery constriction, and bronchoconstriction.15 β Blockers, including eye drops containing them, should therefore be withdrawn and substituted in any patient who is considered at risk of anaphylaxis.16 Tricyclic antidepressants and monoamine oxidase inhibitors potentiate adrenaline and increase the risk of cardiac arrhythmias. The dose of adrenaline should be halved in these patients (grade C). Cocaine sensitises the heart to catecholamines (as does uncontrolled hyperthyroidism), and adrenaline is therefore relatively contraindicated (grade C).10
When should adrenaline be given?
Evidence in the literature suggests that a poor outcome from anaphylaxis is associated with late administration of adrenaline. In a series of 13 fatal and near fatal anaphylactic reactions over a 14 month period, only two of the six patients who died received adrenaline within the first hour compared with six of the seven survivors (grade C).17 In a retrospective study of 27 patients with anaphylaxis occurring outside hospital, all those treated within 30 minutes recovered compared with two deaths in those in whom treatment was delayed by more than 45 minutes (grade C).18 One study showed that whereas adrenaline was used in the treatment of 62% of fatal reactions it was used in only 14% before cardiac arrest (grade C).8 This may, however, be due in some part to both the speed of reactions and the availability of treatment. As a result current guidelines suggest adrenaline should be given as soon as possible.19
Which patients have the worst outcomes?
The severity of previous reactions does not determine the severity of future reactions, and subsequent reactions could be the same, better, or worse. The unpredictability depends on the degree of allergy and the dose of allergen.8,20 A series of paediatric anaphylaxis showed that in two of the three fatal reactions and five of the six near fatal reactions, the previous allergic event had not required urgent hospital intervention (grade C).19 Studies have also shown a significant increased risk of near fatal and fatal reactions in patients with coexistent asthma.17,19 In one study, 13 of the 14 fatal or near fatal reactions occurred in patients with known asthma (grade C). It is not clear if this is related to the severity of the underlying asthma.
Auto-injectors
Who should be prescribed adrenaline auto-injectors?
Studies have shown that only 50-75% of patients prescribed auto-injectors for self administration of adrenaline carry them around at all times.21-24 w8 Of these, only 30-40% were able to correctly demonstrate how they would administer adrenaline to themselves. A retrospective analysis showed that only 29% of children with recurrent anaphylaxis were treated with their adrenaline auto-injector.25 The subsequent need for adrenaline and admission to hospital was reduced in those patients who did receive the appropriate dose by auto-injector (grade C).25 Adrenaline auto-injectors proved unsuccessful in nine of 14 patients with severe reactions, either due to unavailability (n = 4), rapidity of reaction (n = 1), incorrect dose (n = 1), or despite correct treatment (n = 2) (grade C).8 In another study, 23% (n = 22) of adult patients admitted that they would probably not be brave enough to self administer adrenaline—half would seek medical assistance and the other half would ask another person.22
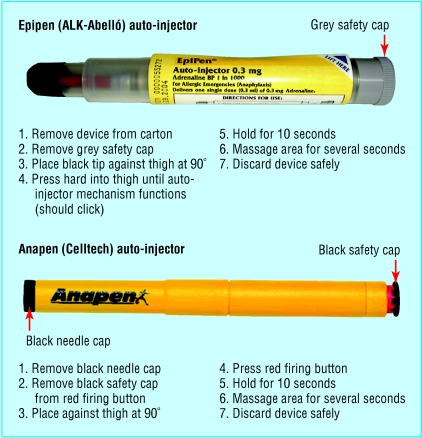
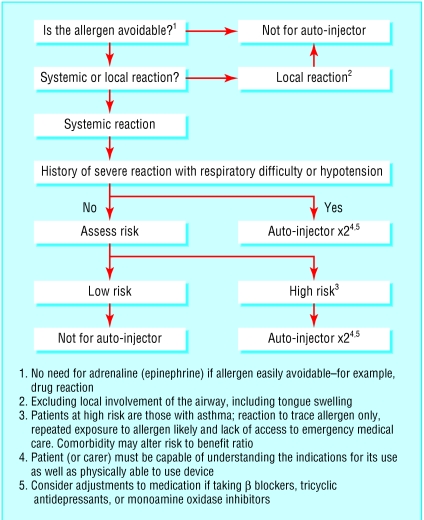
Studies in primary and secondary care have shown that most doctors are themselves uncertain about the correct method for use of auto-injectors.24 w8 Only instruction provided by an allergy specialist has been shown to have any effect on proper injection technique (grade C).23,24 Patients need to be aware about expiry dates for their auto-injectors, although studies have shown adrenaline content and bioavailabilty in outdated auto-injectors.w9 Instruction by a physician familiar with auto-injectors and regular review of technique and reinforcement of the issues surrounding their use is therefore vital for these patients (fig 2). Current opinion on prescription of auto-injectors is divided. American opinion suggests that all patients with an episode of major allergy should be prescribed an auto-injector.13,15 In the United Kingdom some people believe auto-injectors are over-prescribed.22 Current UK paediatric guidelines suggest auto-injectors should be given only to patients with previous severe reaction or reactions involving the airway.21 Given that current evidence supports the relative safety of intramuscular adrenaline, and early administration is associated with an improved survival, any patient with a systemic allergic reaction should be a candidate for adrenaline by auto-injector. The prescription of auto-injectors, however, needs to be targeted to those most likely to use the adrenaline and in whom the benefit outweighs the risk. We propose an algorithm for identifying patients who may benefit from an adrenaline auto-injector (fig 3). Further careful epidemiological research is needed to clarify who benefits most from such treatment.
Fig 2.
Techniques for use of two auto-injectors
Fig 3.
Algorithm for identifying patients who may benefit from an adrenaline auto-injector
Additional educational resources
Websites
Resuscitation Council UK (www.resus.org.uk/siteindx.htm)—details current UK resuscuitation guidelines for anaphylaxis
American Academy of Allergy, Asthma and Immunology (www.aaaai.org)—good section on recent literature, with summary and editorial comment
Joint Council of Allergy, Asthma, and Immunology (www.jcaai.org/Param/Anaphylax.htm)—provides guidelines for investigation and management of the common allergic conditions
British Allergy Foundation (www.allergyfoundation.com)—source of information about allergen avoidance
Information for patients
The Anaphylaxis Campaign (www.anaphylaxis.org.uk)—provides useful information about anaphylaxis, including practical advice on avoidance of allergens and support services, as well as information about adrenaline auto-injectors and instructions for their use
Supplementary Material
See also Primary care p 1328
 Grades of evidence, details of studies with clinical outcomes, and web references w1-w9 appear on
bmj.com
Grades of evidence, details of studies with clinical outcomes, and web references w1-w9 appear on
bmj.com
We thank the reviewer for his comments.
Contributors: APCMcL-T is the primary author. All authors contributed to all aspects of this review. GSP will act as guarantor for the paper.
Funding: None.
Competing interests: AF and GS have received funding from ALK-Abelló to attend academic meetings.
References
- 1.Montanaro A, Bardana EJ Jr. The mechanisms, causes and treatment of anaphylaxis. J Invest Clin Immunol 2002;2: 2-11. [PubMed] [Google Scholar]
- 2.Fischer M. Fortnightly review: treatment of acute anaphylaxis. BMJ 1995;311: 731-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yocum MW, Butterfield JH, Klein JS, Volcheck GW, Schroeder DS, Silverstein MD. Epidemiology of anaphylaxis in Olmsted County: a population based study. J Allergy Clin Immunol 1999;104: 452-6. [DOI] [PubMed] [Google Scholar]
- 4.Stewart AJ, Ewan PJ. The incidence, aetiology and management of anaphylaxis presenting to an accident and emergency department. Q J Med 1996;89: 859-64. [DOI] [PubMed] [Google Scholar]
- 5.Klein JS, Yocum MW. Underreporting of anaphylaxis in a community emergency room. J Allergy Clin Immunol 1995;95: 637-8. [DOI] [PubMed] [Google Scholar]
- 6.Neugut AI, Ghatak AT, Miller RL. Anaphylaxis in the United States—an investigation into its epidemiology. Arch Intern Med 2001;161: 15-21. [DOI] [PubMed] [Google Scholar]
- 7.Johnston SL, Unsworth J, Gompels M. Adrenaline given outside the context of life threatening allergic reactions. BMJ 2003;326: 589-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pumphrey RSH. Lessons for the management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy 2000;30: 1144-50. [DOI] [PubMed] [Google Scholar]
- 9.Brown AFT. Therapeutic controversies in the management of acute anaphylaxis. J Accident Emerg Med 1998;15: 89-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Project Team of the Resuscitation Council (UK). The emergency medical treatment of anaphylactic reactions for first medical responders and for community nurses. Revised Jan 2002. www.resus.org.uk/pages/reaction.htm (accessed Apr 2003).
- 11.American Association of Allergy, Asthma, and Immunology. Media resources: position statement 26. The use of epinephrine in the treatment of anaphylaxis. www.aaaai.org/media/resources/advocacy_statements/ps26.stm (accessed Apr 2003).
- 12.Simons F. Epinephrine absorption in children with a history of anaphylaxis. J Clin Immunol 1998;101: 33-7. [DOI] [PubMed] [Google Scholar]
- 13.Simons FE, Gu X, Simons KJ. Epinephrine absorption in adults: intramuscular versus subcutaneous injection. J Allergy Clin Immunol 2001;108: 871-3. [DOI] [PubMed] [Google Scholar]
- 14.Lang DM. Anaphylactoid and anaphylactic reactions. Hazards of beta-blockers. Drug Safety 1995;12(5): 299-304. [DOI] [PubMed] [Google Scholar]
- 15.Ellis MD, Day JH. The role of epinephrine in the treatment of anaphylaxis. Curr Allergy Asthma Rep 2003;3: 11-4. [DOI] [PubMed] [Google Scholar]
- 16.Moneret Vautrin DA, Kanny G, Faller JP, Levan D, Kohler C. Severe anaphylactic shock with cardiac arrest caused by coffee and gum Arabic potentiated by beta-blocking eyedrops. Rev Med Interne 1993;14(2): 107-11. [DOI] [PubMed] [Google Scholar]
- 17.Sampson HA, Mendelson L, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med 1992;327: 380-4. [DOI] [PubMed] [Google Scholar]
- 18.Soreide E, Buxrud T, Harboe S. Severe anaphylactic reactions outside hospital: aeitiology, symptoms and treatment. Acta Anaesthesiol Scand 1988;32: 339-42. [DOI] [PubMed] [Google Scholar]
- 19.Macdougall CF, Cant AJ, Colver AF. How dangerous is allergy in childhood? The incidence of severe and fatal allergic reactions across the UK and Ireland. Arch Dis Child 2002;86: 236-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zimmerman B, Urch B, Mercardo B. Food allergy: frequency of adrenaline administration. Can J Allergy Clin Immunol 2001;6: 159-61. [Google Scholar]
- 21.Injectable adrenaline for children. Drug Ther Bull 2003;41(3): 21-4. [DOI] [PubMed] [Google Scholar]
- 22.Unsworth DJ. Adrenaline syringes are vastly over prescribed. Arch Dis Child 2001;84: 410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldberg A, Confino-Cohen R. Insect sting-inflicted systemic reactions: attitudes of patients with insect venom allergy regarding after-sting behaviour and proper administration of epinephrine. J Allergy Clin Immunol 2000;106: 1184-9. [DOI] [PubMed] [Google Scholar]
- 24.Sicherer S. Self-injectable epinephrine: no size fits all! Ann Allergy, Asthma Immunol 20001;86: 597-8. [DOI] [PubMed] [Google Scholar]
- 25.Gold MS, Sainsbury R. First aid anaphylaxis management in children prescribed an epinephrine autoinjector device. J Allergy Clin Immunol 2000.106; 171-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.