Abstract
Objective: To compare the implications of four widely used cholesterol screening and treatment guidelines by applying them to a population in the United Kingdom.
Design: Guidelines were applied to population based data from a cross sectional study of cardiovascular disease and risk factors.
Setting: Newcastle upon Tyne, United Kingdom.
Subjects: General population sample (predominantly of European origin) of 322 men and 319 women aged 25-64 years.
Main outcome measures: Proportions recommended for screening and treatment.
Methods: Criteria from the British Hyperlipidaemia Association, the British Drugs and Therapeutics Bulletin (which used the Sheffield table), the European Atherosclerosis Society, and the American national cholesterol education programme were applied to the population.
Results: Proportions recommended for treatment varied appreciably. Based on the British Drugs and Therapeutics Bulletin guidelines, treatment was recommended for 5.3% (95% confidence interval 2.9% to 7.7%) of men and 3.3% (1.5% to 5.3%) of women, while equivalent respective values were 4.6 (2.3 to 6.9) and 2.8 (1.0 to 4.6) for the British Hyperlipidaemia Association, 23% (18.4% to 27.6%) and 10.6% (7.3% to 14.0%) for the European Atherosclerosis Society, and 37.2% (31.9% to 42.5%) and 22.2% (17.6% to 26.8%) for the national cholesterol education programme. Only the British Hyperlipidaemia Association and Drugs and Therapeutics Bulletin guidelines recommend selective screening. Applying British Hyperlipidaemia Association guidelines, from 7.1% (4.3% to 9.9%) of men in level one to 56.7% (51.3% to 62.1%) of men in level three, and from 4.4% (2.1% to 6.7%) of women in level one to 54.4% (48.9% to 59.9%) of women in level three would have been recommended for cholesterol screening. Had the Drugs and Therapeutics Bulletin guidelines been applied, 22.2% (16.5% to 27.9%) of men and 12.2% (8.6% to 15.8%) of women would have been screened.
Conclusions: Without evidence based guidelines, there are problems of variation. A consistent approach needs to be developed and agreed across the United Kingdom.
Key messages
Several widely available guidelines give different advice for managing hyperlipidaemia
Proportions of the population deemed eligible for screening and treatment can differ considerably between guidelines
Even when the proportions eligible for treatment are similar, the individuals often differ
There are probably inconsistences in the management of hyperlipidaemia in the United Kingdom
Explicitly derived, scientifically valid guidelines that include a consideration of costs are urgently needed
Introduction
Considerable attention has been focused recently on promoting evidence based practice and the potential of guidelines to inform and support appropriate care and changes in clinical behaviour.1–3 Guidelines have been drawn up on the prevention of coronary heart disease—in particular, on the screening and management of patients with lipid disorders. Guidance on the use of statins, based on the Sheffield table,4 was recently circulated to all doctors in the United Kingdom.5 There are important differences in the recommendations of the major guidelines, however, yet neither these differences nor the implications for clinical practice have been studied.
We have applied data from a population based survey to the different guidelines for a population aged 25-64 years.6 We aimed to describe the potential implications of differences in commonly available and widely promoted guidelines produced by the British Hyperlipidaemia Association,7 the British Drugs and Therapeutics Bulletin,8 the European Atherosclerosis Society,9 and the American national cholesterol education program.10
Methods
Recruitment and data collection
The data used in this paper are from the Newcastle heart project—a population based study of coronary heart disease, diabetes, and associated risk factors in the general (predominantly of European origin), Chinese, and South Asian populations of Newcastle upon Tyne.6 We have used data from the general population for this paper. This was a population based sample from the patient register of the Newcastle Family Health Services Authority, the list of all individuals in Newcastle registered with a general practitioner. We took an age and sex stratified random sample of those aged 25 to 64 years after removing any Chinese sounding names (less than 0.5% of the sample).11
Lipid analyses
Subjects were recruited to the study between April 1993 and November 1994. After overnight fasting, subjects’ height and weight were measured, their body mass index (kg/m2) was computed, and a fasting blood sample was taken. Until May 1994 the lipid analyses were performed on a Cobas Bio centrifugal analyser (Roche Products Ltd, Welwyn Garden City) and after this date a DAX analyser was used (Bayer plc, Basingstoke). Throughout the study period, the laboratory participated in an external quality assurance scheme. This showed no changes in bias (inaccuracy) for cholesterol or high density lipoprotein cholesterol. However, the data for triglycerides confirmed that the DAX data showed a positive bias relative to the Cobas Bio data and therefore results obtained with the DAX were adjusted as previously described.12 The low density lipoprotein cholesterol concentration was calculated using the Friedewald formula.7
Cardiovascular data
Subjects had two blood pressure measurements. These were made by trained observers using a standard mercury sphygmomanometer with an alternate size cuff.13 A 12 lead electrocardiogram was recorded with the subjects at rest. The findings were coded according to the Minnesota manual by two independent observers; a third observer was used where the two disagreed.14 Each subject completed a questionnaire, which included items on diabetes, hypertension, coronary heart disease, and stroke (all diagnosed by a doctor); smoking status; causes of death in any parents or siblings who had died; and the World Health Organisation questionnaire on intermittent claudication.15 For women, the questionnaire also inquired about age at the time of the menopause, and any factors affecting its onset. Local ethical committee approval was received for the study and all subjects gave informed consent before participating.
Applying the guidelines
Space does not permit a detailed description of the guidelines. Here, we have focused on the people for whom the guidelines recommend intensive treatment in the form of rigorous dietary intervention underpinned by professional dietetic advice, with or without drug treatment. Table 1 summarises how we applied each of the guidelines to the data. The European Atherosclerosis Society and national cholesterol education program guidelines specify two target levels for active intervention: one for drug treatment (if a trial of dietary intervention fails) and the other for intensive dietary intervention only. Table 2 gives the definitions of the different conditions and risk factors we used in applying the guidelines to the study population.
Table 1.
Application of guidelines to data*
| Population to be screened | Population to be treated |
|---|---|
| British Hyperlipidaemia Association | |
| In order of priority: | Presence of coronary heart disease and LDL cholesterol >3.4 mmol/l |
| Vascular disease | Presence of ⩾2 out of: diabetes, hypertension (1)*, current smoker, or obesity and LDL cholesterol >5.0 mmol/l |
| Family history (1)* of coronary heart disease | Male sex and LDL cholesterol >6.0 mmol/l |
| Diabetes, hypertension (1)*, current smoker, or obesity | Female sex, postmenopausal, and LDL cholesterol >6.0 mmol/l |
| Drugs and Therapeutics Bulletin | |
| Vascular disease, or a family history (1)* of coronary heart disease; or | Presence of vascular disease and LDL cholesterol ⩾3.4 mmol/l |
| Particular combination of age, sex, hypertension (1)*, left ventricular hypertrophy, smoking, and diabetes from risk table | If no overt vascular disease, decision from table based on combination of age, sex, diabetes, smoking, hypertension (1)*, left ventricular hypertrophy, and total cholesterol value |
| European Atherosclerosis Association | |
| All | Presence of vascular disease and total cholesterol >5 mmol/l (<6 mmol/l dietary therapy only) |
| Coronary heart disease risk >20% over 10 years (determined by risk chart according to age, sex, smoking status, blood pressure, and total cholesterol) and total cholesterol >5 mmol/l (<7 mmol/l dietary therapy only) | |
| Coronary heart disease risk ⩽20% and total cholesterol >7 mmol/l (<8 mmol/l dietary therapy only) | |
| National cholesterol education programme | |
| All | Presence of coronary heart disease and LDL cholesterol ⩾2.6 mmol/l (<3.4 mmol/l dietary therapy only) |
| LDL cholesterol ⩾3.4 mmol/l (<4.1 mmol/l dietary therapy only) and presence of ⩾2 (3 if HDL cholesterol ⩾1.6 mmol/l) out of: male, age ⩾45, diabetes, hypertension (2)*, current smoker, postmenopausal female, family history of coronary heart disease (2)*, HDL cholesterol <0.9mmol/l | |
| LDL cholesterol ⩾4.1 mmol/l (<4.9 mmol/l dietary therapy only) with < 2 risk factors | |
HDL=high density lipoprotein, LDL=low density lipoprotein.
See table 2 for definitions of the conditions and risk factors. The studies used two definitions—(1) and (2)—for hypertension and family history of coronary heart disease.
Table 2.
Definition of conditions and risk factors used in applying the data to the guidelines
| Condition or risk factor | Definition | Included in guideline
|
|||
|---|---|---|---|---|---|
| British Hyperlipidaemia Association | Drugs and Therapeutics Bulletin | European Atherosclerosis Association | National cholesterol education programme | ||
| Diabetes | Reported doctor diagnosis of diabetes | Yes | Yes | Yes | Yes |
| Hypertension (1) | Blood pressure ⩾160 systolic or ⩾95 diastolic or receiving medication | Yes | Yes | - | - |
| Hypertension (2) | Blood pressure ⩾140 systolic or ⩾90 diastolic or receiving medication | - | - | - | Yes |
| Current smoker | Self reported current smoker | Yes | Yes | Yes | Yes |
| Obesity | Body mass index ⩾30 kg/m2 | Yes | - | - | - |
| Vascular disease | Reported doctor diagnosis of stroke, angina, myocardial infarction or heart failure, or positive on WHO intermittent claudication questionnaire | Yes | Yes | Yes | - |
| Coronary heart disease | Reported diagnosis of angina or myocardial infarction | Yes | - | - | Yes |
| Left ventricular hypertrophy | Minnesota codes 3-1 and 3-3 on resting 12 lead electrocardiogram and hypertension (1) | - | Yes | - | - |
| Postmenopausal | Self reported cessation of periods | Yes | Yes | ||
| Family history (1) of coronary heart disease | Death from coronary heart disease in parent or in sibling aged ⩽60 | Yes | Yes | - | - |
| Family history (2) of coronary heart disease | Death from coronary heart disease in father or male sibling aged ⩽55 or in mother or female sibling aged ⩽65 | - | - | - | Yes |
Data analysis
Data were analysed using SPSS software. Results are presented for 20 year age groups and for all ages (25-64 years) for men and women separately. The results for all ages were age adjusted to the 1991 England and Wales male and female populations respectively. Confidence intervals were calculated using Confidence Interval Analysis software (BMJ Publishing, London).
Results
Altogether 322 men and 319 women aged 25-64 were screened, giving a response rate of 67%. Most subjects were European; 10 men and four women had South Asian sounding names.11 Table 3 shows the percentages of men and women with the risk factors and conditions used in the analyses. The age adjusted total cholesterol concentrations were mean (SD) 5.6 (1.1) mmol/l in men and 5.4 (1.2) in women; the mean high density lipoprotein cholesterol concentrations were 1.3 (0.4) mmol/l and 1.6 (0.4) respectively; and the mean low density lipoprotein cholesterol concentrations were 3.4 (1.1) mmol/l and 3.2 (1.0) respectively.
Table 3.
Prevalence of risk factors and coronary heart disease in the study population. Percentages for 25-64 years are directly age standardised to 1991 population of England and Wales
| Condition or risk factor* | Men
|
Women
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age 25-44 (n=128)
|
Age 45-64 (n=194)
|
Age 25-64 (n=322)
|
Age 25-44 (n=112)
|
Age 45-64 (n=207)
|
Age 25-64 (n=319)
|
||||||||||||
| No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | ||||||
| Diabetes | 0 | 8 | 4.4 (0.5 to 7.3) | 8 | 1.9 (0.7 to 4.0) | 3 | 2.7 (0.6 to 7.6) | 5 | 2.4 (0.7 to 5.6) | 8 | 2.6 (0.9 to 4.3) | ||||||
| Hypertension (1) | 11 | 8.6 (3.7 to 13.5) | 51 | 26.3 (20.1 to 32.5) | 62 | 15.4 (11.5 to 19.3) | 2 | 1.8 (0.2 to 6.3) | 36 | 17.4 (12.2 to 22.6) | 38 | 7.8 (4.9 to 10.7) | |||||
| Hypertension (2) | 21 | 16.4 (10.0 to 22.8) | 84 | 43.3 (36.3 to 50.3) | 105 | 26.4 (21.6 to 31.2) | 3 | 2.7 (0.5 to 7.6) | 58 | 28.0 (21.9 to 34.1) | 61 | 12.2 (8.6 to 15.8) | |||||
| Current smoker | 48 | 37.5 (29.1 to 45.9) | 61 | 31.9 (25.3 to 38.5) | 109 | 34.8 (29.6 to 40.0) | 39 | 34.8 (26.0 to 43.6) | 53 | 25.7 (19.7 to 31.7) | 92 | 32.2 (27.1 to 37.3) | |||||
| Obesity | 18 | 14.1 (8.1 to 20.1) | 30 | 15.5 (10.0 to 21.0) | 48 | 14.5 (10.7 to 18.3) | 14 | 12.5 (6.4 to 18.6) | 49 | 23.8 (18.0 to 29.6) | 63 | 16.3 (12.2 to 20.4) | |||||
| Vascular disease | 2 | 1.6 (0.2 to 5.5) | 31 | 16.0 (10.4 to 20.6) | 33 | 7.1 (4.3 to 9.9) | 1 | 0.9 (0 to 4.9) | 22 | 10.6 (6.4 to 14.8) | 23 | 4.4 (2.1 to 6.7) | |||||
| Coronary heart disease | 2 | 1.6 (0.2 to 5.5) | 27 | 13.9 (9.0 to 18.8) | 29 | 6.1 (3.5 to 8.7) | 0 | 15 | 7.2 (3.7 to 10.7) | 15 | 2.7 (0.9 to 4.5) | ||||||
| Left ventricular hypertrophy | 4 | 3.1 (0.8 to 7.8) | 7 | 3.6 (1.6 to 5.8) | 11 | 3.7 (1.6 to 5.8) | 0 | 6 | 2.9 (0.6 to 5.2) | 6 | 1.3 (0.3 to 3.2) | ||||||
| Postmenopausal | — | — | — | 11 | 10.5 (4.8 to 16.2) | 142 | 70.3 (64.1 to 76.5) | 153 | 33.6 (28.4 to 38.8) | ||||||||
| Family history (1) of coronary heart disease | 11 | 8.6 (3.7 to 13.5) | 10 | 5.2 (2.1 to 8.3) | 21 | 7.1 (4.3 to 9.9) | 6 | 5.4 (1.2 to 9.6) | 22 | 10.6 (6.4 to 14.8) | 28 | 7.4 (4.5 to 10.3) | |||||
| Family history (2) of coronary heart disease | 6 | 4.7 (1.0 to 8.4) | 12 | 6.2 (2.8 to 9.6) | 18 | 5.4 (2.9 to 7.9) | 5 | 4.5 (1.5 to 10.1) | 20 | 9.7 (5.7 to 13.7) | 25 | 6.5 (3.8 to 9.2) | |||||
See table 2 for definitions of the conditions and risk factors.
Table 4 shows the proportions of men and women who would be screened for cholesterol concentration if the guidelines of the British Hyperlipidaemia Association and the Drugs and Therapeutics Bulletin were followed. The proportions vary widely from 4.4% in women of all ages on the first level of the British Hyperlipidaemia Association guidelines to over 50% for both men and women on the third level.
Table 4.
Proportions recommended for cholesterol screening* according to the British Hyperlipidaemia Association and Drugs and Therapeutics Bulletin guidelines. Percentages for 25-64 years are directly age standardised to 1991 population of England and Wales
| Men
|
Women
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age 25-44 (n=128)
|
Age 45-64 (n=194)
|
Age 25-64 (n=322)
|
Age 25-44 (n=112)
|
Age 45-64 (n=207)
|
Age 25-64 (n=319)
|
||||||||||||
| No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | ||||||
| British Hyperlipidaemia Association: | |||||||||||||||||
| First screening level | 2 | 1.6 (0.2 to 5.5) | 31 | 16.0 (10.8 to 21.2) | 33 | 7.1 (4.3 to 9.9) | 1 | 0.9 (0.0 to 4.9) | 22 | 10.6 (6.4 to 14.8) | 23 | 4.4 (2.1 to 6.7) | |||||
| Second screening level | 13 | 10.2 (5.0 to 15.4) | 37 | 19.1 (13.6 to 24.6) | 50 | 13.2 (9.5 to 16.9) | 7 | 6.3 (1.8 to 10.8) | 40 | 19.3 (13.9 to 24.7) | 47 | 11.1 (7.7 to 14.5) | |||||
| Third screening level | 69 | 53.9 (45.3 to 62.5) | 123 | 63.4 (56.6 to 70.2) | 192 | 56.7 (51.3 to 62.1) | 55 | 49.1 (39.8 to 58.4) | 128 | 61.8 (55.2 to 68.4) | 183 | 54.4 (48.9 to 59.9) | |||||
| Drugs and Therapeutics Bulletin | 14 | 10.9 (5.5 to 16.3) | 82 | 42.3 (34.3 to 48.1) | 96 | 22.2 (17.7 to 26.7) | 7 | 6.3 (1.8 to 10.8) | 46 | 22.2 (16.5 to 27.9) | 53 | 12.2 (8.6 to 15.8) | |||||
See table 1 for description of criteria for screening
Table 5 shows the percentages of men and women recommended for treatment according to the different guidelines. In both men and women, the highest percentages recommended for treatment are associated with the national cholesterol education program guidelines. Here 37% of men and 22% of women met the criteria for active intervention, approximately evenly divided between those who would be recommended for intensive dietary treatment only and those who would be recommended for drug treatment if dietary measures failed to achieve target levels. The British Hyperlipidaemia Association guidelines produced the lowest percentages recommended for treatment (initially intensive dietary measures with drug treatment if target levels were not reached). These were 4.6% of men and 2.8% of women. Although the percentages recommended for treatment by the British Hyperlipidaemia Association and Drugs and Therapeutics Bulletin were similar, the individuals who would have been treated often differed (see figure). Only 2.2% of the population were recommended for active intervention by both guidelines; an additional 2.1% were recommended by the Drugs and Therapeutics Bulletin guidelines only and 1.5% by the British Hyperlipidaemia Association only.
Table 5.
Proportions recommended for active lipid lowering treatment by the different guidelines. Percentages for 25-64 years are directly age standardised to 1991 population of England and Wales
| Guidelines | Men
|
Women
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age 25-44 (n=128)
|
Age 45-64 (n=194)
|
Age 25-64 (n=322)
|
Age 25-44 (n=112)
|
Age 45-64 (n=207)
|
Age 25-64 (n=319)
|
||||||||||||
| No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | No | % (95% CI) | ||||||
| British Hyperlipidaemia Association | 2 | 1.6 (0.1 to 5.5) | 18 | 9.3 (5.2 to 13.4) | 20 | 4.6 (2.3 to 6.9) | 1 | 0.9 (0 to 4.9) | 13 | 6.3 (3.0 to 9.6) | 14 | 2.8 (1.0 to 4.6) | |||||
| Drugs and Therapeutics Bulletin | 2 | 1.6 (0.1 to 5.5) | 23 | 11.9 (7.3 to 16.5) | 25 | 5.3 (2.9 to 7.7) | 1 | 0.9 (0 to 4.9) | 16 | 7.7 (4.1 to 11.3) | 17 | 3.3 (1.3 to 5.3) | |||||
| European Atherosclerosis Association: | |||||||||||||||||
| Possible drug treatment* | 1 | 0.8 (0 to 4.3) | 20 | 10.3 (6.0 to 14.6) | 21 | 5.0 (2.9 to 7.9) | 1 | 0.9 (0 to 4.9) | 20 | 9.7 (6.0 to 14.5) | 21 | 4.5 (2.4 to 7.3) | |||||
| Intensive dietary measures only | 8 | 6.3 (2.7 to 11.9) | 74 | 38.1 (31.3 to 45.0) | 82 | 18.0 (13.8 to 22.2) | 1 | 0.9 (0 to 4.9) | 31 | 15.0 (10.1 to 19.8) | 32 | 6.0 (3.6 to 9.2) | |||||
| All | 9 | 7.0 (3.3 to 12.9) | 94 | 48.5 (41.4 to 55.5) | 103 | 23.0 (18.4 to 27.6) | 2 | 1.8 (0.2 to 6.3) | 51 | 24.6 (18.8 to 30.5) | 52 | 10.6 (7.3 to 14.0) | |||||
| National cholesterol education program: | |||||||||||||||||
| Possible drug treatment* | 13 | 10.2 (4.9 to 15.4) | 55 | 28.4 (22.0 to 34.7) | 68 | 17.5 (13.3 to 21.5) | 2 | 1.8 (0.2 to 6.3) | 47 | 22.7 (17.0 to 28.4) | 49 | 9.5 (6.4 to 13.2) | |||||
| Intensive dietary measures only | 21 | 16.4 (10.0 to 22.8) | 48 | 24.7 (18.7 to 30.8) | 69 | 19.7 (15.2 to 23.9) | 7 | 6.3 (2.6 to 12.5) | 48 | 23.2 (17.4 to 28.9) | 55 | 12.7 (9.2 to 16.5) | |||||
| All | 34 | 26.6 (18.9 to 34.3) | 103 | 53.1 (46.1 to 60.1) | 137 | 37.2 (31.9 to 42.5) | 9 | 8.0 (3.0 to 13.0) | 95 | 45.9 (39.1 to 52.7) | 104 | 22.2 (17.6 to 26.8) | |||||
If intensive dietary measures fail to lower cholesterol to target values.
The figures for the British Hyperlipidaemia Association guidelines in table 5 apply to the whole population—that is, irrespective of whether the individuals met the criteria for screening by these guidelines. The figures are lower if they are based only on those individuals who meet both the screening and treatment criteria. Thus, the percentage of men and women who met level one screening criteria and treatment criteria were 2.7% and 1.4% respectively, while proportions for level two were 3.0% and 1.4% and those for level three were 3.7% and 2.4%. For the men and women together, the sensitivity (those defined as needing treatment who would be screened divided by all those needing treatment) for screening level three was 83.3%, and the specificity (those defined as not needing treatment who would not be screened, divided by all those not needing treatment) was 45.5%. The criteria for screening and treatment for the Drugs and Therapeutics Bulletin are such that all those who meet the criteria for treatment also meet the criteria for screening, giving, by default, a sensitivity of 100%. The specificity was 86.6% for men and women together.
Discussion
Strengths and weakness
This paper aimed to describe the differing implications of commonly available and widely promoted British (British Hyperlipidaemia Association, Drugs and Therapeutics Bulletin), European (European Atherosclerosis Society), and American (national cholesterol education program) guidelines for the management of hyperlipidaemia. To apply the guidelines to our data we needed to make several assumptions, sometimes because of the vagueness of the guidelines and sometimes because of the limitations of our data. These included, for example, basing “a strong family history of premature coronary disease” on reported death from coronary heart disease in a first degree relative, as we did not have data on non-fatal events in relatives.
Three of the four guidelines considered state explicitly that treatment decisions should be based on more than one cholesterol measurement. Our data are based on a single fasting measurement, and, undoubtedly, repeat measurements on subjects whose initial concentrations had been high would have reduced the numbers recommended for treatment.
In addition, our data are from a population based survey with a response rate of 67%. This survey may have underestimated the prevalence of coronary heart disease and some risk factors. For example, in the health survey of England, those subjects who consented to a blood test had a lower mean systolic blood pressure and lower prevalences of smoking and coronary heart disease.16 Comparing our data, in 10 year age groups, to those from the health survey of England suggests that the prevalences of smoking, obesity, and hypertension (defined as ⩾160/95 mm Hg or taking antihypertensive treatment) in men are similar to those for England as a whole in 1993/94.17 The prevalence of hypertension in women in our sample is around half that found in the health survey. However, the data we used here are broad and have enabled us to apply most criteria from the different guidelines. Thus, although we cannot claim that our results reflect accurately the proportion of the population who require treatment in a clinical context, we are confident that they do reflect reasonably the relative differences between the guidelines for screening and treatment, and this was the primary purpose of this study.
Implications of the findings
There were wide differences between the implications of some of the guidelines. The highest proportions of men (37%) and women (22%) came within the treatment category where the national cholesterol education program guidelines were applied. The proportions of men and women recommended for treatment by the guidelines of the British Hyperlipidaemia Association and Drugs and Therapeutics Bulletin were similar—men 4.6% compared with 5.3% and women 2.8% compared with 3.3% respectively. However, the individuals who would have been treated differed (figure).Thus, it is not simply that some guidelines suggest more aggressive intervention but also that they advise treatment for different subgroups. It is also clear that even the most liberal screening criteria recommended by the British Hyperlipidaemia Association (level three in table 1) would not identify all patients recommended for treatment by those guidelines.
Balancing considerations of sensitivity and specificity is a common problem in defining screening criteria. In this context it is worth noting that the recent Effective Health Care bulletin on cholesterol and coronary heart disease comes down firmly against universal cholesterol screening.18 It also argued cogently that guidance must be based on the assessment and management of overall cardiovascular risk and not just one aspect, such as the cholesterol concentration.
A questionnaire survey of health authorities or boards in the United Kingdom in 1994 found considerable variation and inconsistency in local criteria for cholesterol testing and treatment.19 Our local experience suggests there is much heterogeneity—guidelines of the British Hyperlipidaemia Association, European Atherosclerosis Society, and criteria based on the Sheffield table were used, and, most recently, guidance has been issued from the Standing Medical Advisory Committee based on the Sheffield table.5 The implication is that there are considerable inconsistencies in the management of hyperlipidaemia within the United Kingdom. It has been previously observed that locally produced guidelines for the use of anticoagulants in atrial fibrillation and widely used hypertension guidelines also differ greatly in their implications for numbers treated.20,21
Clear guidance needed
The need for consistent clear guidance on screening for and management of hyperlipidaemia is ever more pressing as evidence of the effectiveness of newer but expensive agents, the statins, accumulates.22–24 Unfortunately, recent guidance issued to all doctors in the United Kingdom5 falls short of what is required—it considers only drug management, fails to present the evidence, and ignores issues of cost effectiveness.25 It adds to the confusing array of guidelines illustrated in this paper rather than helping to identify and resolve the reasons for differences between them.
The major lipid management guidelines published to date have depended upon consensus development processes and not on the systematic evidence linked review of published reports that is now recognised as a necessary part of the process of developing scientifically valid guidelines.26,27 Furthermore, none of the guidelines have addressed the economic and service consequences of their application as part of their development process. The need for explicitly derived, scientifically valid guidelines that include a consideration of costs is clear.
Figure.
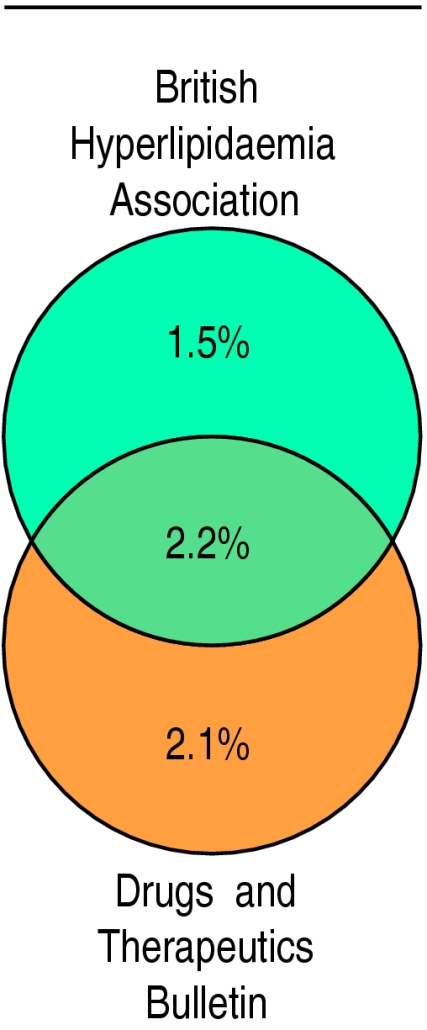
Proportions of men and women aged 25-64 years recommended for active intervention by guidelines from the British Hyperlipidaemia Association and the Drugs and Therapeutics Bulletin
Footnotes
Funding: Newcastle and North Tyneside Health Authority, Barclay Trust, and British Diabetic Association.
Conflict of interest: None.
References
- 1.NHS Centre for Reviews and Dissemination. Implementing clinical practice guidelines. Effective Health Care 1994;4(1).
- 2.Grimshaw J, Russell I. Effect of clinical guidelines on medical practice: A systematic review of rigorous evaluations. Lancet. 1993;342:1317–1322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- 3.Thomson RG, Lavender M, Madhok R. How to ensure that guidelines are effective. BMJ. 1995;311:237–242. doi: 10.1136/bmj.311.6999.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramsay L, Haq I, Jackson P, Yeo W. The Sheffield table for primary prevention of coronary heart disease: corrected. Lancet. 1996;348:1251–1252. doi: 10.1016/s0140-6736(05)65536-5. [DOI] [PubMed] [Google Scholar]
- 5.Standing Medical Advisory Committee. The use of statins. London: Standing Medical Advisory Committee; 1997. [Google Scholar]
- 6.Unwin N, Harland J, White M, Bhopal R, Winocour P, Watson W, et al. Body mass index, waist-hip ratio and glucose intolerance in Chinese and European adults. J Epidemiol Community Health. 1997;51:160–166. doi: 10.1136/jech.51.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Betteridge D, Dodson P, Durrington P, Hughes E, Laker M, Nicholls D, et al. Management of hyperlipidaemia: guidelines of the British Hyperlipidaemia Association. Postgrad Med J. 1993;69:359–369. doi: 10.1136/pgmj.69.811.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Management of Hyperlipidaemia. Drug Therap Bull. 1996;34:89–93. doi: 10.1136/dtb.1996.341289. [DOI] [PubMed] [Google Scholar]
- 9.Pyorala K, Backer GD, Graham I, Poole-Wilson P, Wood D.on behalf of the task force. Prevention of coronary heart disease in clinical practice: recommendations of the task force of the European Society of Cardiology, European Atherosclerosis Society and European Society of Hypertension Eur Heart J 1994151300–1331. [DOI] [PubMed] [Google Scholar]
- 10.National Cholesterol Education Programme. Second report of the expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment panel 2) Circulation. 1994;89:1333–1345. doi: 10.1161/01.cir.89.3.1333. [DOI] [PubMed] [Google Scholar]
- 11.Coldman AJ, Braun T, Gallagher RP. The classification of ethnic status using name information. J Epidemiol Community Health. 1988;42:390–395. doi: 10.1136/jech.42.4.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harland JO, Unwin N, Bhopal RS, White M, Watson W, Laker M, et al. Low levels of cardiovascular risk factors and coronary heart disease in a UK Chinese population. J Epidemiol Community Health. 1997;51:636–642. doi: 10.1136/jech.51.6.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Petrie JC, O’Brien ET, Littler WA, Swiet MD, Dillon MJ, Padfield PL. Recommendations on blood pressure measurements. 2nd ed. London: BMJ Publishing Group; 1990. [Google Scholar]
- 14.Prineas R, Crow R, Blackburn H. The Minnesota code manual of electrocardiographic findings. London: John Wright; 1982. [Google Scholar]
- 15.Rose G, Blackburn A, Gillum R, Prineas R. Cardiovascular survey methods. 2nd ed. Geneva: World Health Organisation; 1982. [Google Scholar]
- 16.Bennett N, Dodd T, Flatley J, Freeth S, Boiling K.for the Office of Population Censuses and Surveys. Health survey for England 1993. 1995London: HMSO [Google Scholar]
- 17.Department of Health. Health survey for England ’96. London: Stationery Office; 1998. [Google Scholar]
- 18.NHS Centre for Reviews and Dissemination. Cholesterol and coronary heart disease: screening and treatment. Effective Health Care 1998; No 4.
- 19.Raine R, Streetly A, Davis AM. Variation in local policies and guidelines for cholesterol management: national survey. BMJ. 1996;313:1368–1369. doi: 10.1136/bmj.313.7069.1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomson R, McElroy H, Sudlow M. Guidelines on anticoagulant treatment in atrial fibrillation in Great Britain: variation in content and implications for treatment. BMJ. 1998;316:509–513. doi: 10.1136/bmj.316.7130.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fahey TP, Peters TJ. What constitutes controlled hypertension? Patient based comparison of hypertension guidelines. BMJ. 1996;313:93–96. doi: 10.1136/bmj.313.7049.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pedersen TR, Kjekshus J, Berg K, Haghfelt T, Faergeman O, Thorgeirsson G, et al. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian simvastatin survival study (4S) Lancet. 1994;344:1383–1389. [Google Scholar]
- 23.Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 24.Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, Macfarlane PW, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med. 1995;333:1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 25.Freemantle N, Barbour R, Johnson R, Marchment M, Kennedy A. The use of statins: a case of misleading priorities? National guidance that does not link costs and benefits is worthless. BMJ. 1997;315:826–828. doi: 10.1136/bmj.315.7112.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grimshaw J, Russell I. Achieving health gain through clinical guidelines I: Developing scientifically valid guidelines. Qual Health Care. 1993;2:243–248. doi: 10.1136/qshc.2.4.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eccles M, Clapp Z, Grimshaw J, Adams PC, Higgins B, Purves I, et al. North of England evidence based guidelines development project: methods of guideline development. BMJ. 1996;312:760–761. doi: 10.1136/bmj.312.7033.760. [DOI] [PMC free article] [PubMed] [Google Scholar]


