SUMMARY
Both influenza and respiratory syncytial virus (RSV) cause epidemics of respiratory illness of variable severity during the winter season. Influenza in particular has been blamed for hospital winter bed pressures, although it is thought that RSV may also play a role. Human metapneumovirus (hMPV) is a new respiratory virus reported to be important in children; only a limited number of studies are available for adult populations. We aimed to determine initially the burden of virologically confirmed infections, i.e. influenza, RSV and hMPV using polymerase chain reaction (PCR) technology and, in addition, to assess the feasibility of this approach as a surveillance tool for these respiratory viruses. Adult patients admitted to hospital in the previous 24 hours with onset of acute respiratory symptoms in the last 14 days were asked to participate. Informed written consent was obtained and nose and throat swabs taken. Multiplex PCR for influenza A (H1N1 and H3N2), influenza B and RSV A and B were carried out together with a separate PCR for hMPV. A total of 219 patients in 2001–2002 and 216 in 2002–2003 were tested and the combined results for both seasons were: 8 positive for influenza A/H1N1, 14 for influenza A/H3N2, 2 for influenza B, 14 for RSV A and 6 for RSV B. Most patients (261/435) were >65 years and most positives (30/44) were found within this age group. A number of patients aged >65 years who were positive for influenza (12/15) reported having had vaccine. In total, 373 samples were tested for hMPV and 20 were found positive across all age groups except the 45–54 years age group. As influenza activity was low during the study period the impact of infection on admissions could not be assessed. Nevertheless the viruses studied accounted for 15% of hospital admissions for respiratory infection. Most patients were aged >65 years, as expected. In the two years studied RSV and hMPV were each responsible for as many hospitalized cases of respiratory infection as influenza. Influenza infection must be considered even in those who give a history of vaccination. The molecular methods used in this study showed that surveillance of these respiratory viruses can be conducted and may help in the management of patients.
INTRODUCTION
Influenza is an acute, usually self-limiting febrile illness that occurs in epidemics of varying severity almost every winter. However, other respiratory viruses, e.g. respiratory syncytial virus (RSV) can cause similar symptoms. In addition a new metapneumovirus has been described in children with bronchiolitis [1] and the role of this virus in adult respiratory illness needs to be established.
Influenza and RSV infections can be severe in elderly patients, those with underlying respiratory or cardiac disease and the immunocompromised. During periods of maximum respiratory virus activity, i.e. the winter months, these infections can account for many of the acute medical admissions to hospitals, causing ‘winter bed pressures’. Excess hospital admissions attributed to these viruses have not been widely studied or quantified. Available studies have not been based on laboratory-confirmed cases [2, 3].
Traditionally influenza was considered to be the main cause of winter bed pressures. In the 1980s it was realized that RSV may be a more important respiratory pathogen in the elderly than had previously been thought [4–7]. These reports used serological testing methods, which take time; it was also often difficult to obtain both acute and convalescent sera from patients. Carman et al. [8], using polymerase chain reaction (PCR), showed that results could be available within 36 h of receipt of specimens compared to serology which took up to 3 weeks. PCR assays are now much more widely used for diagnosis and the rapid provision of results is also useful for surveillance purposes.
Several studies on the prevalence of human metapneumovirus (hMPV) in children with respiratory symptoms [1, 9–11] have found that it varies between 5·5% and 25% with most between 5% and 8%. Only a limited number of studies have included adult populations and the prevalence varied widely between 4·5% and 52% [12, 13].
Aims
The aim of this study was to determine initially the burden of virologically confirmed respiratory infections in patients admitted to hospital following an acute respiratory illness, using PCR. We specifically investigated influenza A, B, RSV and hMPV infection. In addition we assessed the feasibility of using this approach as a surveillance tool for respiratory viral infection during the winter period.
PATIENTS, M0ATERIALS AND METHODS
Patients
We studied a total of 435 patients during two winter seasons (from November to the end of February) – 219 in the 2001–2002 season and 216 in 2002–2003. All were over 18 years of age, admitted in the previous 24 h with acute respiratory symptoms to one of four hospitals in the West Midlands region. Date of onset should have been within the previous 14 days. However, several samples taken outside this time were included in the study. Ethical approval was obtained for the study from all participating sites. A qualified nurse was employed at each site to explain the objectives of the study using an information sheet, to answer any patient queries and obtain written consent. We intended to collect up to 20 specimens from each site per week, equivalent to 80 samples per week from across the West Midlands for surveillance purposes. Bias was minimized by the nurse at each site, who reviewed admissions for the previous 24-h period on a daily basis. Candidates fulfilling the entry criteria were approached to take part in the study.
Separate nose and throat swabs were collected from each patient and placed into one vial of viral transport media (VTM). Information on the patients’ sex, date of birth, date of onset of symptoms, duration and nature of symptoms, history of influenza vaccine and antiviral treatment was recorded.
Nucleic acid extraction and RT–PCR
A 200-μl aliquot of each sample was extracted using the Roche MagNApure automated nucleic acid extraction system (Roche Diagnostics, Lewes, UK) employing the total nucleic acid isolation kit. RT–PCR was carried out using a reaction mixture that contained 20 mm Tris–HCl, 50 mm KCl, 7·5 mm MgCl2 (5×buffer; Promega UK Ltd, Southampton, UK) each dNTP at a concentration of 1·5 mm (Invitrogen Life Technologies, Strathclyde, UK), 250 ng of each random primer (Amersham Biosciences UK Ltd, Little Chalfont, Bucks, UK), 1·6 U of Rnasin (Promega) and 200 U of MMLV–RT (Promega) [14]. Amplification conditions consisted of 20°C for 10 min, 37°C for 1 h and 95°C for 5 min.
Influenza/RSV PCR
A multiplex nested PCR for influenza A (H1N1 and H3N2), influenza B, RSV A and B was performed following the procedure described by Stockton et al. [14]. Briefly, the first round mix consisted of 10 mm Tris–HCl, 3·5 mm MgCl2, 2·5 mm KCl, 1·5 U Taq polymerase (Qiagen Taq PCR master mix kit, Qiagen Ltd, Crawley, UK), 5 pmol of each primer pair (Oswel DNA Service, Southampton, Hampshire, UK) and 20 μl of extracted DNA in a total volume of 100 μl. The amplification conditions consisted of 94°C for 2 min followed by 35 cycles of 1 min each at 94, 50 and 72°C.
Two microlitres of the first round product were added to 48 μl of a second round mix similar to the above but with the second primer pairs at a concentration of 25 pmol. The amplification conditions consisted of 94°C for 2 min followed by 35 cycles of 1 min each at 94, 60 and 72°C.
hMPV PCR
hMPV PCR was performed according to the procedure described by Stockton et al. [22]. Briefly 20 μl of extracted DNA was added to 80 μl of a reaction mix containing 20 mm Tris–HCl, 50 mm KCl, 10 mm MgCl2, 3 U Taq polymerase (Taq DNA polymerase, recombinant; Invitrogen Life Technologies Ltd) and 50 pmol of each primer (MWG Biotech, Milton Keynes, UK). Amplification conditions consisted of 94°C for 2 min, followed by 35 cycles of 1 min each at 94, 58 and 72°C.
Detection
PCR products were detected by agarose gel electrophoresis with ethidium bromide staining (Sigma-Aldrich Co. Ltd, Shaftesbury, UK) using a 2% gel for the influenza/RSV PCR and 1% gels for the hMPV PCR. Amplification product sizes were: influenza A/H1N1 944 bp, influenza B 767 bp, influenza A/H3N2 591 bp, RSV A 334 bp, RSV B 186 bp and hMPV 171 bp.
RESULTS
Prevalence of influenza and RSV
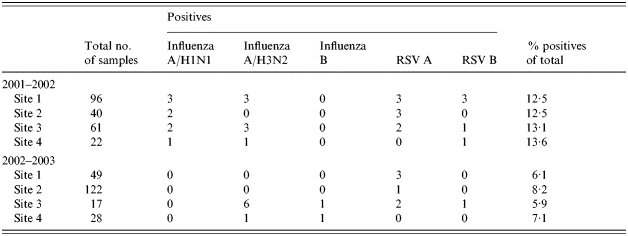
In the 2001–2002 season 28 out of 219 (12·8%) samples were positive by PCR. There were eight samples which were initially reactive for influenza A/H1N1, but subsequently three were found to be H1N2. In addition there were seven influenza A/H3N2, eight RSV A and five RSV B. In the 2002–2003 season only 16 out of 216 (7·4%) samples were positive by PCR. Seven were influenza A/H3N2, two influenza B, six RSV A and one was RSV B. The number of positive samples from each of the four sites was proportional to the number of samples collected in both seasons 12·5% in 2001–2002 and 6·5% in 2002–2003 (Table 1).
Table 1.
Total number of samples and positives from each site for both years/seasons
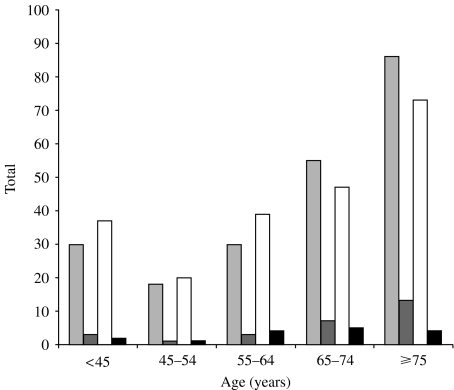
Similar results were found in each of the study years, most patients (261/435, 60·0%), were over 65 years of age and most positive samples were found within this age group (30/44, 68·2%).
All patients over the age of 65 years in the United Kingdom are routinely offered influenza vaccination before the start of the winter season. In our cohort, 209 out of 255 (78·0%) patients over 65 years of age reported having had vaccine. This included 12 out of 15 (80·0%) patients in this age group found positive for influenza. The attack rates for influenza were 12 out of 209 (5·7%) in the vaccinated and 3 out of 46 in the unvaccinated; this difference was not significant. Date of vaccination was available for six of the 12 and infection occurred 3–4 months post vaccine. In comparison in the under 65 years age group only 42·5% of patients gave a history of vaccination, 2/9 (22·2%) which were positive for influenza (Fig. 1).
Fig. 1.
Distribution of patient age and RSV/influenza positives in both seasons.
 , No. of patients 2001–2002;
, No. of patients 2001–2002;
 , no. of positives 2001–; □, no. of patients 2002–2003; ■, no. of positives 2002–2003.
, no. of positives 2001–; □, no. of patients 2002–2003; ■, no. of positives 2002–2003.
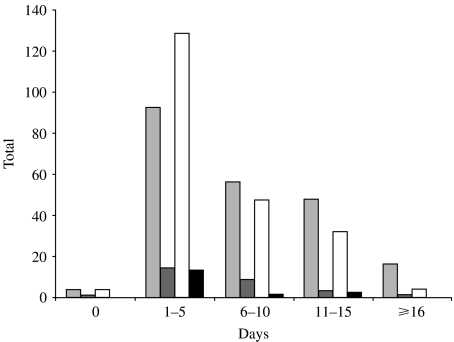
Most patients were admitted within 14 days of onset of symptoms (94·5%). Only one patient with positive results was detected later than 14 days and this was at 29 days (Fig. 2).
Fig. 2.
Distribution of days after onset of symptoms and positives in both seasons.
 , No. of patients 2001–2002;
, No. of patients 2001–2002;
 , no. of positives 2001–2002; □, no. of patients 2002–2003; ■, no. of positives 2002–2003.
, no. of positives 2001–2002; □, no. of patients 2002–2003; ■, no. of positives 2002–2003.
Metapneumovirus results
Sufficient material to test for hMPV was available from 373 samples. Twenty samples (5·4%) proved positive. Positive samples were found from all four sites included in the study and across all age groups with the exception of those aged 45–54 years (Table 2).
Table 2.
Total samples collected and total hMPV positives
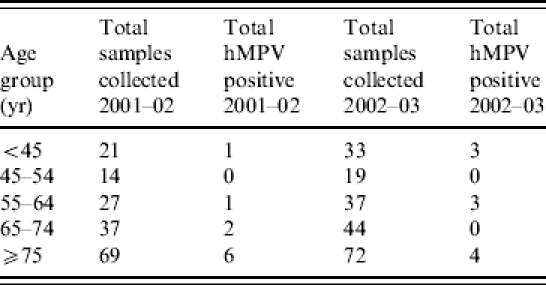
There were no multiple infections in any group.
DISCUSSION
There are many factors that appear to influence winter bed pressures [3]. It is generally felt that hospitals suffer bed pressures throughout the year. Hence, a high level of respiratory viral activity during winter seasons would be needed to test the hypothesis that they have a major impact on hospital admissions.
In the United Kingdom, during both years of this study, influenza activity was below baseline level (<50 cases/100 000) as reported by the Communicable Disease Surveillance Centre (CDSC), Health Protection Agency (HPA). In addition, hospital admission data available for three of the hospitals included in this study showed that there was no seasonal increase in medical or respiratory admissions (Service Development Unit, Heartlands Hospital, Birmingham and Shropshire County and Telford and Wrekin Primary Care Trusts). This affected our ability to recruit patients and, therefore, to assess objectively the burden of virologically confirmed cases of influenza and RSV on winter bed pressures.
The impact of influenza vaccination on hospital admissions also needs to be considered. Ahmed et al. [15] showed that vaccination reduced hospital admissions by 63% in the elderly when the uptake of vaccine was only 46%. Uptake in 2001–2002 and 2002–2003 was just under the government’s target of 70% for the over-65s (65% and 69% respectively, Department of Health). This improved uptake could have played a role in reducing hospital admissions during the period of the study.
Although patient recall may have led to some inaccuracy, in the information we collected about previous influenza vaccination we found that 12 of the 15 (80·0%) influenza-positive patients >65 years had been vaccinated. In comparison only two out of nine (22·2%) vaccinated patients <65 years were found positive for influenza. This underlines the fact that vaccination in the elderly does not always provide protection probably because of waning immune responses. In a recent study Fleming et al. [16] concluded that hospital admissions due to influenza will remain a burden, especially in the elderly, and that although vaccination programmes are needed, they will not on their own have the impact expected on this problem.
Most of the patients tested (60·0%) were >65 years and most patients found positive for influenza (62·5%) and RSV (75·0%) were also in this age group. This agrees with the results of Agius et al. [6] and Falsey et al. [7] that RSV as well as influenza can be an important pathogen in the elderly. The data also strengthens the findings of a number of epidemiologically based studies [2–5].
One of the inclusion criteria for entrants to our study was that onset of symptoms was <14 days before admission although several samples (20) were collected outside this time frame. We decided to test these samples because of the small number of patients recruited. However, apart from one exception, viruses were only detected in samples taken up to 15 days after the onset of symptoms.
In the 2001–2002 season a new strain of influenza A (H1N2), which is a recombinant of the H1N1 and H3N2 strains, was reported to be circulating in the United Kingdom. Six of our ‘H1N1’ positive samples were referred to the Specialist and Reference Microbiology Division (SRMD) laboratory at the Central Public Health Laboratory (CPHL), London for further characterization. Three were found to be the new H1N2 strain. The multiplex PCR we used in this study was able to detect viruses related to H1N1 and H3N2 strains and it is reassuring that we managed to diagnose infections with the newly described strain.
Studies on metapneumovirus in children with respiratory symptoms report a prevalence of 5–25% [1, 9] and in hospitalized children of 6·5–25% [17–20]. Chan et al. [13] reported a high positivity rate of 52·1% in patients investigated during the SARS outbreak in Hong Kong. A study carried out in Canada [21] showed that the prevalence of hMPV was 14·8% in patients of all ages (2 months to 93 years) with most positives seen in the <5 and >50 years age groups and Falsey et al. [12] reported a prevalence of 4·5% among patients >18 years of age.
Our study showed an average prevalence of 5·4% over the two winter seasons (2001–2002: 5·6%; 2002–2003: 4·9%). All those found positive for hMPV were negative for influenza and RSV. Stockton et al. [22] investigated patients who had visited their GP with influenza-like illness (ILI) and showed that 2·2% of people were positive for hMPV. This included both children and adults, but as in our study there were no co-infections with influenza and RSV. Our data suggest that in years when influenza activity is low, hMPV can account for as many cases of respiratory infections admitted to hospital as influenza and RSV, particularly among the elderly.
The results of this study indicated that testing respiratory samples by molecular techniques can be used as a surveillance tool and that results can be generated quickly. This was one of the objectives of the study, although with the addition of other viruses, e.g. rhinovirus and parainfluenza virus, this approach could provide rapid, comprehensive diagnosis. This method could provide an early warning system for influenza epidemics that can overwhelm hospitals. Carman et al. [8] compared PCR with two standard techniques (culture and serology) for monitoring outbreaks of influenza. In a follow-up study they extended this to include RSV and picornavirus. They conclude that molecular techniques can improve surveillance of respiratory viruses in a community setting [23] and that they should be the method of choice for diagnosing infections with these viruses. Other studies have demonstrated different variations on multiplex PCRs able to detect up to nine respiratory viruses and all have proven to be sensitive and specific (see e.g. refs [24–26]).
Substituting verbal for written consent would streamline the process of informed consent – an informal audit of patients suggested that verbal consent would be acceptable. However, consideration must also be given to the recommendation that these samples become part of the routine diagnostic assessment. This is particularly important now that results can be provided within a time frame which is useful in patient management, unlike in the past where diagnosis was a slow process.
In conclusion, although influenza activity was low during the two seasons of this study, we found that in adult patients admitted to hospital with respiratory symptoms at least 15% of infections were caused by respiratory viruses. We have shown that the use of molecular techniques can be useful in the surveillance of respiratory virus activity and potentially in the management of affected patients.
ACKNOWLEDGEMENTS
The authors thank the following nurses and staff for their technical help in this study: Allison Bradley, Angela Brennan, Jan Heath, Annette Littlewood, Lynne Marston, Odette Mbuy, Amy Page, Steve Wilson and Priti Palmer.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Van den Hoogen BG, deJong JC, Groen J et al. A newly discovered human metapneumovirus isolated from young children with respiratory tract disease. Nat Med. 2001;7:719–724. doi: 10.1038/89098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fleming DM. The contribution of influenza to combined acute respiratory infections, hospital admissions and deaths in winter. Commun Dis Public Health. 2000;3:32–38. [PubMed] [Google Scholar]
- 3.Nguyen-van Tam JS, Brockway CR, Pearson JCG, Hayward AC, Fleming DM. Excess hospital admissions for pneumonia and influenza in person years associated with influenza epidemics in 3 English health districts: 1987–1995. Epidemiol Infect. 2001;126:71–79. doi: 10.1017/s0950268801005076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathur U, Bentley DW, Hall CB. Concurrent respiratory syncitial virus and influenza A infections in the institutionalised elderly and chronically ill. Ann Intern Med. 1980;93:49–52. doi: 10.7326/0003-4819-93-1-49. [DOI] [PubMed] [Google Scholar]
- 5.Sorvillo FJ, Huie SF, Strassburg MA, Butsumyo A, Shandora WX, Fannin SI. An outbreak of respiratory syncitial virus pneumonia in a nursing home for the elderly. J Infect. 1984;9:252–256. doi: 10.1016/s0163-4453(84)90530-9. [DOI] [PubMed] [Google Scholar]
- 6.Agius G, Dindinaud G, Biger RJ et al. An epidemic of respiratory syncitial virus in elderly people: clinical and serological findings. J Med Virol. 1990;30:117–127. doi: 10.1002/jmv.1890300208. [DOI] [PubMed] [Google Scholar]
- 7.Falsey AR, Treanor JJ, Betts RF, Walsh EE. Viral respiratory infections in the institutionalised elderly: clinical and epidemiological findings. J Am Geriatr Soc. 1992;40:115–119. doi: 10.1111/j.1532-5415.1992.tb01929.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carman WF, Wallace L, Walker J et al. Rapid virological surveilance of community influenza infection in general practice. BMJ. 2000;321:736–737. doi: 10.1136/bmj.321.7263.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freymouth F, Vabret A, Legrand L et al. Presence of the new human metapneumovirus in French children with bronchiolitis. Pediatr Infect Dis J. 2003;22:92–94. doi: 10.1097/00006454-200301000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Greensill J, McNamara PS, Dove W, Flanagan B, Smyth RL, Hart CA. Human metapneumovirus in severe respiratory syncitial virus bronchiolitis. Emerg Infect Dis. 2003;9:372–375. doi: 10.3201/eid0903.020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takao S, Shimozono H, Kashiwa H et al. Clinical study of Paediatric cases of acute respiratory diseases associated with human metapneumovirus in Japan. Jpn J Infect Dis. 2003;56:127–129. [PubMed] [Google Scholar]
- 12.Falsey AR, Erdman D, Anderson LJ, Walsh EE. Human metapneumovirus infections in young and elderly adults. J Infect Dis. 2003;187:785–790. doi: 10.1086/367901. [DOI] [PubMed] [Google Scholar]
- 13.Chan PKS, Tam JS, Lam CW et al. Human metapneumovirus detection in patients with severe acute respiratory syndrome. Emerg Infect Dis. 2003;9:1058–1063. doi: 10.3201/eid0909.030304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stockton J, Ellis JS, Saville M, Clewley JP, Zambon MC. Multiplex PCR for typing and subtyping influenza and respiratory syncytial viruses. J Clin Microbiol. 1998;36:2990–2995. doi: 10.1128/jcm.36.10.2990-2995.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed AH, Nicholson KG, Nguyen-van Tam JS, Pearson JC. Effectiveness of influenza vaccine in reducing hospital admissions during the 1989–90 epidemic. Epidemiol Infect. 1997;118:27–33. doi: 10.1017/s0950268896007121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fleming D, Harcourt S, Smith G. Influenza and adult hospital admissions for respiratory conditions in England 1989–2001. Commun Dis Public Health. 2003;6:213–237. [PubMed] [Google Scholar]
- 17.Viazov S, Ratjen F, Scheidhauer R, Fiedler M, Roggendorf M. High prevalence of human metapneumovirus infection in young children and genetic heterogeneity of the viral isolates. J Clin Microbiol. 2003;41:3043–3045. doi: 10.1128/JCM.41.7.3043-3045.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maggi F, Pifferi M, Vatteroni M et al. Human Metapneumovirus associated with respiratory tract infections in a 3-year study of nasal swabs from infants in Italy. J Clin Microbiol. 2003;41:2987–2991. doi: 10.1128/JCM.41.7.2987-2991.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Esper F, Boucher D, Weibel C, Martinello R, Kahn J. Human metapneumovirus infection in the United States: clinical manifestations associated with a newly emerging respiratory infection in children. Paediatrics. 2003;111:1407–1410. doi: 10.1542/peds.111.6.1407. [DOI] [PubMed] [Google Scholar]
- 20.Boivin G, De Serres G, Cote S et al. Human metapneumovirus infections in hospitalised children. Emerg Infect Dis. 2003;9:634–640. doi: 10.3201/eid0906.030017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bastien N, Ward D, Van Caeseele P et al. Human metapneumovirus infection in the Canadian population. J Clin Microbiol. 2003;41:4642–4646. doi: 10.1128/JCM.41.10.4642-4646.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stockton J, Stephenson I, Fleming D, Zambon M. Human metapneumovirus as a cause of community acquired respiratory illness. Emerg Infect Dis. 2002;8:897–901. doi: 10.3201/eid0809.020084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wallace LA, Collins TC, Douglas JDM, McIntyre S, Millar J, Carman WF. Virological surveillance of influenza-like illness in the community using PCR and serology. J Clin Virol. 2004;3:40–45. doi: 10.1016/j.jcv.2003.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Puppe W, Weigl JA, Aron G et al. Evaluation of a multiplex reverse transcriptase PCR ELISA for detection of nine respiratory tract pathogens. J Clin Virol. 2004;30:165–174. doi: 10.1016/j.jcv.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Templeton KE, Scheltinga SA, Beersma MF, Kroes AC, Claas EC. Rapid and sensitive method using multiplex real-time PCR for diagnosis of infection by influenza A and influenza B viruses, respiratory syncitial virus and parainfluenza viruses 1, 2, 3 and 4. J Clin Microbiol. 2004;42:1564–1569. doi: 10.1128/JCM.42.4.1564-1569.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Syrmis MW, Whiley DM, Thomas M et al. A sensitive, specific and cost effective multiplex reverse transcriptase-PCR assay for the detection of seven common respiratory viruses in respiratory samples. J Mol Diagn. 2004;6:125–131. doi: 10.1016/S1525-1578(10)60500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]