SUMMARY
Surveillance is an important component of influenza control. This report describes the establishment and first results of the Korean Influenza Surveillance Scheme (KISS), an integrated clinical and laboratory surveillance network involving 622 public health centres (PHCs) and private clinics. Sentinel physicians reported cases of influenza-like illness (ILI) weekly and forwarded specimens for virus isolation and characterization. Influenza activity during the opening 2000–2001 season was milder and delayed compared with previous years. The ILI consultation rate corresponded well with the number of influenza virus isolates, both peaking in week 10 of 2001. Influenza A(H3N2) was the dominant isolate. The peak ILI consultation rate was higher in private clinics than in PHCs (5·04 vs 1·79 cases/1000 visits). An evaluation questionnaire generated potential enhancements to the scheme. KISS appears to represent the pattern of influenza activity accurately and will have a valuable role in monitoring and preventing epidemics in Korea.
INTRODUCTION
Influenza is a highly communicable disease affecting large numbers of people each year. While self-limiting in the majority of cases, influenza is associated with an increased risk of complications, hospitalization and death in the elderly, young children, and those with chronic medical conditions [1–4]. Immunity to influenza is short-lived as the virus is continually undergoing antigenic change. Influenza outbreaks occur nearly every year due to antigenic drift, while novel influenza strains with the potential to cause a pandemic emerge at unpredictable intervals as a result of antigenic shift [5]. The variable epidemiology of influenza and the potentially serious threat to public health highlight the need for close monitoring of influenza activity and early detection of epidemics.
An effective national surveillance system is an important component of an influenza control strategy. A limited influenza surveillance sentinel network was launched in Korea in 1997, but this was unable to provide a satisfactory picture of national influenza activity [6]. An enhanced network known as the Korean Influenza Surveillance Scheme (KISS) was therefore established nationwide in 2000 and commenced surveillance in the 2000–2001 influenza season. KISS consists of an integrated clinical and laboratory surveillance system, in which a sentinel network of public and private clinics compiles data on patients with an influenza-like illness (ILI) and refers specimens from suspected cases for virus isolation. Data analysis is performed by the Korean National Institute of Health (KNIH), which disseminates the results to health practitioners.
The KISS scheme aims to monitor influenza activity and circulating influenza virus strains closely, enabling early detection of epidemics; to provide recommendations on future influenza vaccine formulation and monitor vaccine effectiveness; and to contribute to the development of influenza control measures that may reduce influenza-related morbidity and mortality. This paper, which provides the first report of influenza surveillance in Korea, describes the establishment and initial results of the KISS scheme.
METHODS
Clinical surveillance network
A total of 622 county public health centres (PHCs) and private clinics were recruited throughout South Korea (see Table), representing approximately one institute per 75 000 people based on a population of 47 million. Participation was mandatory for all 239 PHCs nationwide. PHCs are government institutes providing a range of primary health-care programmes, with an emphasis on the prevention and management of chronic diseases and provision of services for low-income patients. The recruitment target for private clinics was one clinic per 100 000 people. During the first year of the scheme, 383 out of 20 692 private clinics participated, representing approximately 1/123 000 people and 1/50 of all private clinics. Most private clinics were included based on recommendations from a PHC or local medical association, while others responded to advertisements placed in medical journals. The private clinics included some general practitioners, but the majority were clinics specializing in internal, paediatric, or family medicine. Centres were recruited on the basis of population size throughout the country, thus the majority was located in cities.
Table.
Institutions participating in the Korean Influenza Surveillance Scheme, 2000–2001
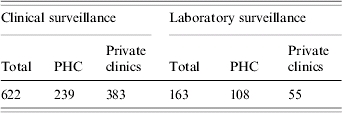
PHC, Public health centre.
Surveillance was initiated on 25 September 2000 (week 39) and results were reported weekly throughout the following year. Private clinics were able to participate from week 50 and adequate data were available from the first week of 2001. The ILI case definition was sudden onset of fever >37·8°C, together with at least one respiratory (e.g. cough, sore throat, rhinorrhoea) or constitutional (e.g. headache, malaise, myalgia) symptom. Sentinel physicians provided weekly reports detailing the total number of patient visits, the number of patients presenting with ILI and the age group of these patients (0–2, 3–6, 7–19, 20–49, 50–64, or ⩾65 years). These were completed on the form provided and submitted to a local PHC by fax, telephone or post.
PHCs compiled the data reported by the clinics in their area and sent it to KNIH via an electronic data exchange system. The KNIH calculated the mean number of patients with ILI per 1000 visits at each institute and analysed the age distribution of ILI cases. The analysed data were distributed weekly by various means, including email, Communicable Disease Monthly Reports (http://dis.cdc.go.kr/cdmr/cdmr.asp) and the influenza surveillance homepage (http://dis.cdc.go.kr/influenza/english/index.asp).
A questionnaire was sent at the end of the 2000–2001 season to all participating clinics in order to evaluate the functioning of the KISS scheme in its first year.
Laboratory surveillance network
Throat or nasal swabs were taken from patients presenting with ILI and submitted to Provincial Health and Environmental Research Institutes (PHERIs) for influenza virus isolation using cell culture. Eight PHERIs with the capacity to perform virus isolation participated and quality control was performed annually. All 108 PHCs associated with a PHERI able to perform virus isolation participated in the laboratory surveillance scheme, together with 55 private clinics, thus 26% of centres provided specimens for virus isolation. Physicians at participating institutions were requested to take samples from up to 20% of patients presenting with a probable ILI in a given day.
Positive samples were forwarded to KNIH, where viruses were characterized by haemagglutination inhibition assay or multiplex reverse transcriptase–polymerase chain reaction (RT–PCR). The characteristics of circulating influenza viruses were compared with existing vaccine strains and this information contributed to decisions on the vaccine composition for the coming season.
RESULTS
ILI consultation rate
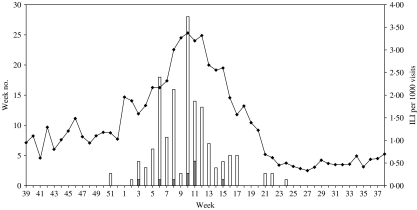
The number of patient consultations per week at each institution ranged from approximately 200 to 1000. The weekly ILI consultation rate increased gradually from the beginning of the 2000–2001 season, peaking during weeks 9–12 of 2001 and decreasing rapidly thereafter (see Fig. 1). At the peak of the influenza season (week 10, ending 10 March), patient visits totalled 209 379, the number of ILI cases was 706 and the proportion of patients presenting with an ILI was 3·37/1000 visits. There was a good correspondence between the trend for the total number of ILI cases and the ILI consultation rate, despite substantial fluctuations in the total number of patient visits (data not shown).
Fig. 1.
Comparison of the weekly influenza-like illness (ILI) consultation rate and the number of influenza virus isolates, Korea, 2001–2002.  , A(H1N1); □, A(H3N2); –◆–, ILI cases per 1000 visits.
, A(H1N1); □, A(H3N2); –◆–, ILI cases per 1000 visits.
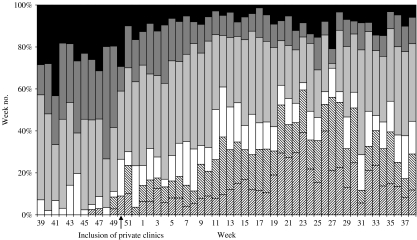
Distribution of ILI cases by age
The majority of patients presenting with an ILI were aged >50 years at the start of the season, but children accounted for an increasing proportion of cases following the inclusion of private clinics in week 50 (see Fig. 2). These two age groups together accounted for over 50% of patients with an ILI.
Fig. 2.
Weekly age group distribution among patients with an influenza-like illness (ILI), Korea, 2000–2001.  , 0–2;
, 0–2;  , 3–6; □, 7–19;
, 3–6; □, 7–19;  , 20–49;
, 20–49;  , 50–64; ■, ⩾65 years.
, 50–64; ■, ⩾65 years.
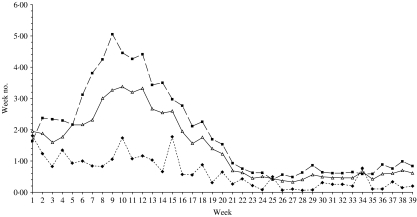
Comparison of public and private clinics
Comparative data were available for the period of weeks 1–39 in 2001. Compliance with weekly reporting was higher in PHCs than in private clinics, with a mean weekly participation rate of 60% and 41% respectively. The ILI consultation rate was markedly higher in private clinics, with a peak rate of ILI cases of 5·04 and 1·79/1000 visits in private clinics and PHCs respectively, and corresponding mean values of 1·88 and 0·63 (see Fig. 3). While the PHC data appeared to show a second peak at week 15, the significance of this was unclear due to the consistently low ILI consultation rate among PHCs, the absence of a second peak in the private clinic data and the overall trend of the graphs.
Fig. 3.
Comparison of the weekly influenza-like illness (ILI) consultation rate (cases per 1000 visits) in public health centres (PHCs) and private clinics, Korea, 2001–2002. ––△––, Total; - -◆- -, PHCs; ––■––, private clinics.
Laboratory results
KNIH and PHERIs tested 2972 respiratory specimens from 25 September 2000 to 31 October 2001. The number of specimens tested was approximately 26% of the total number of ILI cases. Influenza virus was isolated from 144 specimens (4·6%). Of these, 134 isolates (93·1%) were type A(H3N2) and 10 (6·9%) were type A(H1N1); there were no type B isolates.
The first virus isolate was obtained in the week ending 23 December 2000 (week 51). A gradual increase in the number of influenza virus isolates was observed from this time, with a small peak in week 6 followed by a larger peak in week 10 and a subsequent decline to baseline levels (see Fig. 1). The pattern of virus isolation correlated well with changes in the ILI consultation rate and peak values were reached simultaneously.
Twelve randomly selected isolates were antigenically characterized. Of these, eight influenza A(H3N2) isolates were similar to A/Panama/2007/99 and four influenza A(H1N1) isolates were similar to A/New Caledonia/20/99, indicating that their antigenicities were similar to those of the 2000–2001 vaccine strains.
Evaluation questionnaire
A total of 211 institutes responded to the questionnaire, including 102 PHCs (43% response rate) and 109 private clinics (29% response rate). The burden of weekly ILI reporting was considered to be moderate by 55·0% of institutes, with the remainder reporting the burden to be heavy (8·1%), light (30·3%) or none (5·2%); 1·4% did not respond to the question.
Participants were asked to identify problems with the KISS scheme using a multi-choice format. A total of 204 clinics responded, clearly identifying mandatory weekly ILI reporting (65·2%) and an ambiguous definition of ILI (62·3%) as the major perceived problems. Other issues identified were the feedback system (14·2%), lack of incentives (12·7%) and a complicated reporting process (7·4%).
The issue of incentives was further explored, with private clinics asked to choose their preferred incentive(s) from a list provided. Among the 95 responding clinics, the strongly preferred incentive was provision of rapid antigen kits that allow early detection of influenza (81·1%), followed by continuing medical education credits (41·1%), a KISS nameplate (24·2%) and a testimonial (7·4%).
DISCUSSION
The impact of influenza on public health cannot be overemphasized and an influenza surveillance system is essential for the monitoring and control of influenza epidemics.
KNIH has performed influenza virus isolation since 1968 as part of the World Health Organization's influenza surveillance network. In March 1997, the Korean government drafted plans encompassing the establishment of an influenza surveillance system and preparations for a pandemic scenario. These efforts led to the initiation in 1997 of an influenza sentinel physician network involving KNIH and approximately 70 volunteer physicians [6]. However, the network did not adequately represent nationwide influenza activity due to the small number and uneven geographical distribution of sentinel physicians, together with a low reporting rate. Influenza was designated a notifiable communicable disease following a law change in 2000 [7] and the surveillance system was subsequently revised and expanded. The enhanced KISS scheme began surveillance in the 2000–2001 season.
Influenza activity in Korea during the 2000–2001 season appeared to be lower than in previous seasons, consistent with data from the United States, Europe and Japan [6, 8–11]. However, in these countries influenza activity increased throughout December and peaked at the end of January, whereas in Korea the weekly ILI consultation rate peaked in week 10, ending 10 March. This was delayed compared with previous seasons, in which peak influenza activity generally occurred from the final week of November through to the final week of January [6]. It was not possible to determine the epidemic threshold based on data from a single season, but the peak incidence is generally reached within 4 weeks after an epidemic is recognized [12].
The ILI consultation rate was lower than that reported in other countries for the 2000–2001 season [8, 10]. Unexpectedly, physicians who completed the KISS evaluation questionnaire reported difficulty applying the ILI case definition; lack of familiarity with the diagnostic criteria and reporting procedures in the first year of the scheme may have contributed to the low rate of ILI diagnosis. The ILI consultation rate was markedly higher in private clinics than in PHCs (see Fig. 3). The private sector is the dominant health-care provider in Korea, where most individuals have health insurance and attend private clinics for the treatment of acute illnesses such as influenza. Furthermore, patients who usually attend PHCs frequently visit private clinics for acute illnesses such as influenza, for reasons that include ease of access and a perception that medical treatment for acute or severe illnesses is most appropriately obtained at a private clinic. This suggests that the private clinic data may provide a more accurate representation of influenza activity than the PHC or combined data. However, compliance with weekly reporting was higher in PHCs than in private clinics (mean 60% vs. 41%), probably because participation was mandatory for PHCs. The evaluation questionnaire results indicated that physicians considered the weekly reporting interval to be too short and disliked having to file reports for weeks during which they had encountered no ILI cases.
The majority of ILI cases in the 2000–2001 season occurred in children and older adults (aged >50 years). Although influenza epidemics typically affect children first [13, 14], the disease spread more rapidly among adults in the 1989 and 1993 epidemics [15], thus it is necessary to monitor the age distribution of cases closely. At the beginning of the season, most ILI cases occurred in older adults. This was because participation in KISS was initially limited to PHCs, which typically care for patients of lower socioeconomic status with chronic medical conditions, many of whom are elderly. Private clinics, including paediatricians, were recruited from week 50 and children accounted for an increasing proportion of ILI cases thereafter (see Fig. 2).
Influenza virus was first isolated in the week ending 23 December 2000. There was a good correspondence between the influenza virus isolation trend and the ILI consultation rate, with peak values achieved simultaneously in week 10 of 2001 (see Fig. 1). This suggests that the ILI consultation rate, while lower than expected, accurately represented the pattern of influenza activity. A total of 2972 respiratory specimens were tested. At ∼26% of the total number of ILI cases, the sampling rate was consistent with the proportion of centres participating in the laboratory surveillance scheme. Possible reasons for the low influenza virus isolation rate (4·6% of ILI specimens tested) include incorrect diagnosis of ILI, delayed sampling from symptom onset and improper sample handling.
Early virus isolation is an essential component of an influenza surveillance system. PHERIs initially used cell culture for virus detection. PCR is considered to be a more reliable and sensitive test for influenza than viral culture and, perhaps most importantly, reduces the time between specimen sampling and obtaining a result [16]. Furthermore, using multiplex PCR to identify additional pathogens enables estimation of both the true extent to which the ILI consultation rate represents influenza cases and the impact of each influenza subtype [17]. In order to facilitate earlier virus isolation, a PCR assay for influenza was set up for all participating PHERIs in 2000.
The majority of influenza virus isolates in the 2000–2001 season were A(H3N2), with no B type isolates, whereas A(H1N1) and B types predominated in the United States, Japan and Europe [8–11]. The isolates were antigenically similar to the vaccine strains used in Korea that season. Compared with influenza A outbreaks, influenza B epidemics typically last longer and produce lower clinical incidence peaks [18, 19]. Although the two types may be isolated simultaneously, more often one follows another, with type B usually isolated later than type A [12]. These differences in the dominant viral isolates are not understood and further research is needed with respect to the influenza virus itself and the epidemiological aspects of viral spread.
The close proximity of Hong Kong and mainland China to Korea and the extensive trade between these countries increases the potential for a new virus type to spread throughout Korea. There are major concerns regarding this region as the most likely area for emergence of a new virus. Two of the three twentieth-century pandemics, namely A(H2N2) in 1957 and A(H3N2) in 1968, were probably caused by strains originating from China [20]. Moreover, in 1997 an outbreak of the avian influenza A(H5N1) virus in Hong Kong resulted in six deaths among 18 infected patients [21]. In 1999, human cases infected by the avian influenza virus A(H9N2) were reported in Hong Kong and China, but these cases were mild [22]. Widespread outbreaks of the A(H5N1) virus in poultry occurred throughout China, Korea and other Asian countries in 2004, with human infections and deaths reported in Vietnam and Thailand [22]. These events underline the importance of rigorous surveillance for both human and animal influenza, together with strict quarantine procedures to prevent the introduction of new influenza strains. In the near future, an integrated human and animal influenza surveillance system will be implemented in Korea in order to better monitor the emergence of new viruses.
Enhancements to the KISS scheme since the 2000–2001 season include the expansion of virus isolation capability to all PHERIs, provision of rapid influenza antigen detection kits (the preferred incentive in the evaluation survey) to participating clinics, introduction of an internet-based system for ILI reporting, and simplification of the ILI case definition to ‘fever >38°C and cough or sore throat’. Participation in the laboratory surveillance scheme increased from 163 clinics in 2001 to 396 in 2004. The number of PHCs involved rose from 108 to 239 once all PHERIs were able to perform virus isolation, while increased interest from private clinics led to a further 102 clinics joining the laboratory surveillance network.
The results from the first year of influenza surveillance under KISS indicate that the scheme satisfactorily represents influenza activity in Korea. With further consolidation and accumulation of surveillance data, KISS will have a valuable role in the prevention and control of influenza epidemics in Korea.
ACKNOWLEDGEMENTS
We gratefully thank all sentinel physicians and the staff of Public Health Centres and Provincial Health and Environmental Research Institutes for their contribution to KISS.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Housworth J, Langmuir AD. Excess mortality from epidemic influenza, 1957–1966. American Journal of Epidemiology. 1974;100:40–48. doi: 10.1093/oxfordjournals.aje.a112007. [DOI] [PubMed] [Google Scholar]
- 2.Glezen WP. Serious morbidity and mortality associated with influenza epidemics. Epidemiologic Reviews. 1982;4:25–44. doi: 10.1093/oxfordjournals.epirev.a036250. [DOI] [PubMed] [Google Scholar]
- 3.Lui KJ, Kendal AP. Impact of influenza epidemics on mortality in the United States from October 1972 to May 1985. American Journal of Public Health. 1987;77:712–716. doi: 10.2105/ajph.77.6.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson WW et al. Influenza-associated hospitalizations in the United States. Journal of the American Medical Association. 2004;292:1333–1340. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Geneva: WHO; 1999. . Influenza pandemic preparedness plan. The role of WHO and guidelines for national or regional planning. . Report No.: WHO/CDS/CSR/EDC/99.1 ( ). Accessed 10 May 2006. [Google Scholar]
- 6.Lee JY et al. National surveillance of influenza outbreak during winter of 1997 and 1998 in Korea. Korean Journal of Infectious Diseases. 1999;31:1–8. [Google Scholar]
- 7.National Institute of Health, Korea. The revision of the infectious disease control law and the future. Communicable Diseases Monthly Report. 2000;11:123–130. [Google Scholar]
- 8.Centers for Disease Control and Prevention. Update: influenza activity – United States and worldwide, 2000–01 season, and composition of the 2001–02 influenza vaccine. Morbidity and Mortality Weekly Report. 2001;50:466–470. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Influenza activity – United States, 2000–01 season. Morbidity and Mortality Weekly Report. 2001;50:207–209. [PubMed] [Google Scholar]
- 10.Manuguerra JC, Mosnier A, Paget WJ [EISS (European Influenza Surveillance Scheme)] Monitoring of influenza in the EISS European network member countries from October 2000 to April 2001. Eurosurveillance. 2001;6:127–135. [PubMed] [Google Scholar]
- 11.Infectious Disease Surveillance Center, Japan http://idsc.nih.go.jp/idwr/kanja/weeklygraph/01flu-e.html. http://idsc.nih.go.jp/idwr/kanja/weeklygraph/01flu-e.html . Infectious Diseases Weekly Report. Weekly reported cases per sentinel in comparison with past 10 years ( ). Accessed 10 May 2006.
- 12.Fleming DM et al. The duration and magnitude of influenza epidemics: a study of surveillance data from sentinel general practices in England, Wales and the Netherlands. European Journal of Epidemiology. 1999;15:467–473. doi: 10.1023/a:1007525402861. [DOI] [PubMed] [Google Scholar]
- 13.Glezen WP et al. Epidemiologic observations of influenza B virus infections in Houston, Texas, 1976–1977. American Journal of Epidemiology. 1980;111:13–22. doi: 10.1093/oxfordjournals.aje.a112865. [DOI] [PubMed] [Google Scholar]
- 14.Nicholson KG, Nicholson KG, Hay AJ, Webster RG. Textbook of Influenza. Oxford: Blackwell Science; 1998. Epidemiology of influenza; pp. 181–206. , pp. [Google Scholar]
- 15.Aymard M et al. Epidemiology of viral infections and evaluation of the potential benefit of OM-85 BV on the virologic status of children attending day-care centers. Respiration. 1994;61:24–31. doi: 10.1159/000196377. (Suppl. 1): [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carman WF et al. Rapid virological surveillance of community influenza infection in general practice. British Medical Journal. 2000;321:736–737. doi: 10.1136/bmj.321.7263.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Curran M, Hampson A. National influenza surveillance 1997. Communicable Diseases Intelligence. 1998;22:69–74. [PubMed] [Google Scholar]
- 18.Tillett HE, Smith JW, Gooch CD. Excess deaths attributable to influenza in England and Wales: age at death and certified cause. International Journal of Epidemiology. 1983;12:344–352. doi: 10.1093/ije/12.3.344. [DOI] [PubMed] [Google Scholar]
- 19.Barker WH. Excess pneumonia and influenza associated hospitalization during influenza epidemics in the United States, 1970–78. American Journal of Public Health. 1986;76:761–765. doi: 10.2105/ajph.76.7.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oshitani H, Osterhaus ADME, Cox N, Hampson AW. Options for the Control of Influenza IV: Proceedings of the World Congress on Options for the Control of Influenza IV, Crete, Greece, 23–28 September 2000. Amsterdam: Elsevier; 2001. Further development of influenza surveillance in China and global impact on influenza control; pp. 119–122. , pp. [Google Scholar]
- 21.Chan PK. Outbreak of avian influenza A(H5N1) virus infection in Hong Kong in 1997. Clinical Infectious Diseases. 2002;34:S58–64. doi: 10.1086/338820. (Suppl. 2): [DOI] [PubMed] [Google Scholar]
- 22.Lipatov AS et al. Influenza: emergence and control. Journal of Virology. 2004;78:8951–8959. doi: 10.1128/JVI.78.17.8951-8959.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]