Abstract
Persistent viral infections are often associated with inefficient T cell responses and sustained high-level expression of inhibitory receptors, such as the NK cell receptor 2B4 (also known as CD244), on virus-specific T cells. However, the role of 2B4 in T cell dysfunction is undefined, and it is unknown whether NK cells contribute to regulation of these processes. We show here that persistent lymphocytic choriomeningitis virus (LCMV) infection of mice lacking 2B4 resulted in diminished LCMV-specific CD8+ T cell responses, prolonged viral persistence, and spleen and thymic pathologies that differed from those observed in infected wild-type mice. Surprisingly, these altered phenotypes were not caused by 2B4 deficiency in T cells. Rather, the entire and long-lasting pathology and viral persistence were regulated by 2B4-deficient NK cells acting early in infection. In the absence of 2B4, NK cells lysed activated (defined as CD44hi) but not naive (defined as CD44lo) CD8+ T cells in a perforin-dependent manner in vitro and in vivo. These results illustrate the importance of NK cell self-tolerance to activated CD8+ T cells and demonstrate how an apparent T cell–associated persistent infection can actually be regulated by NK cells.
Introduction
Tolerance of NK cells to self-tissue is predominately maintained through inhibitory signals derived from interaction of certain NK cell receptors (e.g., Ly49C) with self class I major histocompatibility complex (MHC) molecules (e.g., H-2Kb) (1, 2). However, MHC-independent inhibitory signals may also contribute to tolerance, including inhibitory signals provided via interaction of CD244 (2B4) with its ligand on hematopoietic cells, CD48 (3). 2B4 is a member of the signaling lymphocyte activation molecule (SLAM) receptor family (4–6). Expression of 2B4 is restricted to NK cells, γδ T cells, basophils, monocytes, and a subset of CD8+ αβ T cells, where both activating and inhibitory signals have been observed upon 2B4 engagement in vitro (7, 8). The recent generation of 2B4 (CD244)–deficient mice has established an inhibitory function for this receptor on NK cells both in vitro and in vivo (9, 10).
Expression of 2B4 on CD8+ T cells strongly parallels that of the T cell exhaustion marker programmed death 1 (PD-1) and has been postulated to contribute to the dysfunction of antiviral CD8+ T cells during persistent viral infection of mice with the clone 13 strain of lymphocytic choriomeningitis virus (LCMV) (11, 12). Although expression of 2B4 is limited on naive CD8+ T cells and only transiently upregulated during acute virus infections, sustained high-level expression of 2B4 on virus-specific CD8+ T cells is characteristic of persistent viral infections in both humans and mice (12–14). For example, 2B4 is upregulated on CD8+ T cells from patients with persistent HIV infection (15).
In this study, we sought to determine the role of 2B4 in the development and functionality of LCMV-specific CD8+ T cell responses during LCMV infection of WT and 2B4-KO mice. Persistent LCMV infection of 2B4-KO mice resulted in significantly diminished LCMV-specific CD8+ T cell responses, prolonged viral persistence, and altered tissue pathology. Surprisingly, this abnormal phenotype of 2B4-KO mice was not directly related to 2B4 expression by CD8+ T cells but was instead mediated through cytolytic targeting of activated CD8+ T cells by activated NK cells in a 2B4-regulated and perforin-dependent manner. These results identify an important role for 2B4 in maintaining tolerance of highly activated NK cells during the early stages of persistent infection that is nonredundant with the role of MHC in self-tolerance. Moreover, NK cell–mediated killing of highly activated virus-specific CD8+ T cells in the absence of 2B4 hampers host defenses during persistent viral infection.
Results
Effects of 2B4 deficiency on antiviral T cell responses during persistent LCMV infection.
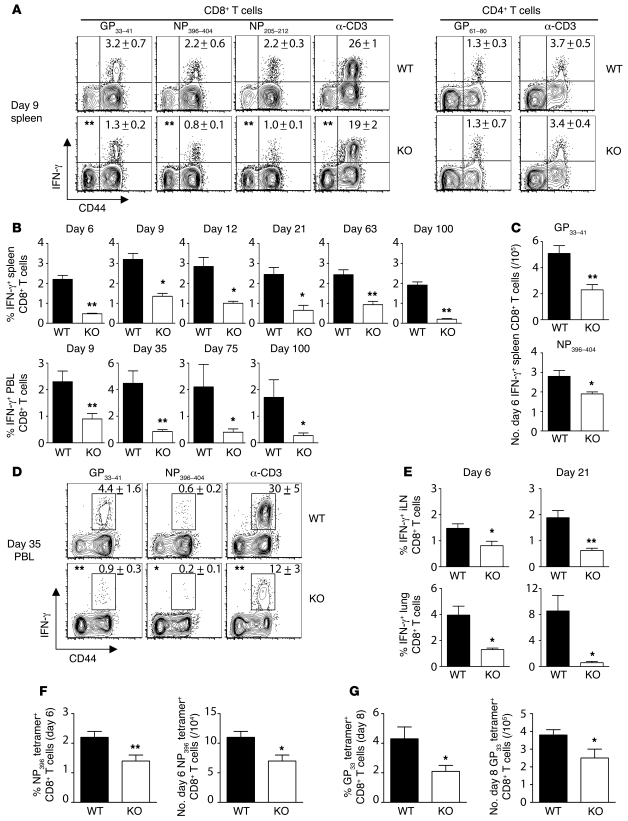
2B4 deficiency had a pronounced effect on CD8+ T cell responses during a persistent, highly disseminated infection induced by i.v. inoculation with 2 × 106 PFU of the clone 13 variant of LCMV (Figure 1). The proportion of LCMV-specific, IFN-γ–producing CD8+ T cells was reduced in the spleen and peripheral blood of 2B4-KO mice at all times analyzed (Figure 1, A and B). Likewise, there were reduced total numbers of splenic GP33-41–specific (Figure 1C), NP396-404–specific (WT: 2.8 ± 0.3 × 105 vs. KO: 1.9 ± 0.1 × 105, n = 10, P = 0.015), and GP276-286–specific (WT: 2.5 ± 0.3 × 105 vs. KO: 1.4 ± 0.2 × 105, n = 10, P = 0.0058) IFN-γ+ CD8+ T cells at day 6 of infection in 2B4-KO mice.
Figure 1. Reduced magnitude of the LCMV-specific CD8+ T cell response during persistent LCMV clone 13 infection of 2B4-KO mice.
(A) Representative viral peptide–induced IFN-γ expression by splenic T cells 9 days after infection with 2 × 106 PFU LCMV clone 13 i.v. Numbers represent mean ± SD of the percentage of IFN-γ+ CD4+ or CD8+ T cells from all the similarly treated mice in the experiment (n = 4). (B) Proportions of LCMV GP33-41–stimulated IFN-γ+ splenic or peripheral blood CD8+ T cells are plotted as mean ± SEM (n = 3–8/group) across a range of time points during persistent LCMV clone 13 infection. (C) Total numbers (mean ± SEM) of GP33-41– and NP396-404–specific IFN-γ+ splenic CD8+ T cells in WT and 2B4-KO mice (n = 10–15/group) at day 6 of infection. (D) Representative CD8+ T cell IFN-γ expression (mean ± SD) in the blood (n = 4) at day 35 of LCMV clone 13 infection. (E) IFN-γ responses (mean ± SD) by GP33-41–specific CD8+ T cells in the iLNs and lungs of WT and 2B4-KO mice (n = 3–4/group) at days 6 and 21 of LCMV clone 13 infection. (F and G) Frequencies (mean ± SEM) of day 6 (n = 6–11/group) LCMV NP396/Db (F) and day 8 (n = 8/group) GP33/Db (G) tetramer-binding CD8+ T cells in the spleen. *P < 0.05, **P < 0.01 (2-tailed unpaired Student’s t test). Data are from 1 of 3–4 experiments with similar results.
Despite a diminished magnitude, LCMV-specific CD8+ T cell responses in 2B4-KO mice had a characteristic hierarchy (i.e., GP33 > NP205 > NP396) of partial exhaustion (Figure 1A), including clonal deletion of NP396-404–specific T cells (Figure 1D), similar to WT mice. Moreover, LCMV-specific IFN-γ–producing CD8+ T cells in WT and 2B4-KO mice failed to coproduce either TNF or IL-2 (data not shown), a hallmark of virus-induced T cell exhaustion (16). LCMV-specific CD8+ T cell responses were also reduced in the lungs and inguinal lymph nodes (iLNs) of 2B4-KO mice (Figure 1E), and the intense foci of infiltrating lymphocytes surrounding the portal areas of WT livers were largely absent in 2B4-KO mice (Supplemental Figure 1; supplemental material available online with this article; doi: 10.1172/JCI41264DS1). LCMV GP61-80–specific and anti-CD3–induced CD4+ T cell IFN-γ responses did not differ between WT and 2B4-deficient mice (Figure 1A).
As T cells can become dysfunctional during persistent LCMV infection and fail to produce cytokines (16, 17), we also determined antiviral CD8+ T cell frequencies using LCMV peptide–loaded MHC class I tetramer staining. The proportion and number of CD8+ T cells staining positive for H-2Db LCMV NP396-404 (Figure 1F) and H-2Db LCMV GP33-41 (Figure 1G) tetramers were significantly reduced in 2B4-KO mice at days 6 and 8 of infection, respectively. Despite differences in frequency, LCMV-specific CD8+ T cells in WT and 2B4-KO mice displayed similar functional avidities in regard to IFN-γ production in response to a range of peptide doses (Supplemental Figure 2).
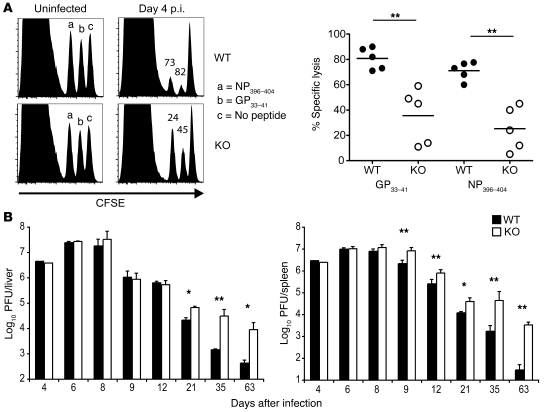
The cytolytic activity of virus-specific CTLs was also assessed in LCMV clone 13–infected mice using a conventional in vivo cytotoxicity assay (18). Consistent with the reduced frequency of LCMV-specific CD8+ T cells in the absence of 2B4 (Figure 1), lysis of LCMV GP33-41– (n = 5, P = 0.0025) and NP396-404–labeled (n = 5, P = 0.0006) targets was significantly reduced in 2B4-KO mice as compared with WT controls (Figure 2A) at postinfection day 4 (day 4 p.i.). Thus, 2B4 may play a role in regulating activation, expansion, or acquisition of effector functions of CD8+ T cells in the context of disseminated infection and high viral loads.
Figure 2. Reduced LCMV-specific CTL activity and increased viral burden in the absence of 2B4 in vivo.
Splenocytes from uninfected WT donor mice were loaded with LCMV peptides (GP33-41 or NP396-404) or no peptide, labeled with various concentrations (2.5, 1, or 0.4 μM) of CFSE, mixed at equal ratios, and injected (2 × 106 total targets) i.v. into LCMV clone 13–infected recipients (day 4 p.i.) or uninfected WT or 2B4-KO control mice. After 20 hours, spleens were harvested from WT and 2B4-KO recipient mice and analyzed for recovery of each CFSE-labeled target population. (A) Representative histograms demonstrate recovery of NP396-404–labeled (low CFSE), GP33-41–labeled (middle CFSE), and unlabeled (high CFSE) peaks. Numbers represent the percent specific lysis of LCMV peptide–coated targets relative to unlabeled control targets within each experimental mouse. Specific lysis of LCMV peptide–coated targets within individual mice is plotted on the right. Each circle represents an individual mouse, and horizontal lines denote the mean. (B) At various time points after infection, organs were harvested from LCMV clone 13–infected mice, and infectious virus was quantified by standard plaque assay. Titers are plotted as the arithmetic mean ± SD of the log10 of PFU per organ (n = 3–10 mice/group). The y axis lower limit is set at the limit of detection for the liver (log10 2.0) and spleen (log10 1.0) assays. *P < 0.05, **P < 0.01 (2-tailed unpaired Student’s t test). Data are from 1 of 3 experiments with similar results.
Elevated viral loads and prolonged viral persistence in 2B4-KO mice.
At early time points after infection (e.g., day 4 p.i.), viral loads were comparably high in the spleen and liver of WT and 2B4-KO mice (Figure 2B). However, an increased viral burden was evident in 2B4-KO mice, beginning 9 days after infection, when viral loads began to slowly decline in WT mice. By day 63, most WT mice (3 of 4) but not 2B4-KO mice (0 of 4) had cleared LCMV from these tissues. By day 92, all 8 2B4-KO mice had detectable virus within the spleen and liver, while 7 of 8 WT mice had cleared LCMV.
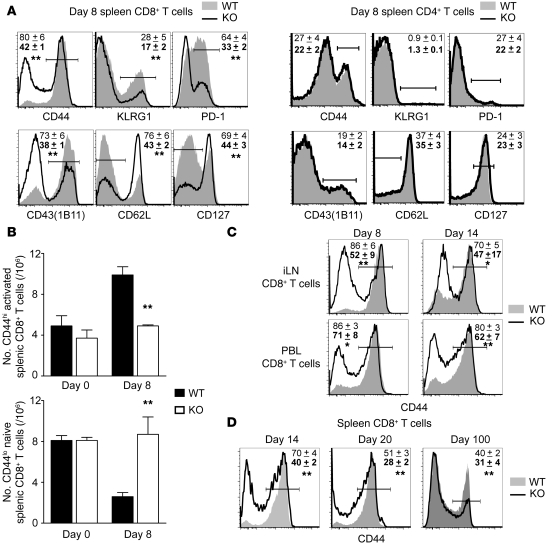
Accumulation of naive-phenotype CD8+ T cells and enhanced spleen size in LCMV clone 13–infected 2B4-KO mice.
In addition to a reduction in the frequency of LCMV-specific CD8+ T cells, a large proportion (Figure 3A) of 2B4-deficient splenic CD8+ T cells displayed a naive phenotype (CD44loCD62Lhi CD127hiPD-1–KLRG1–CD43[1B11]–), whereas WT CD8+ T cells had a predominately activated phenotype (CD44hiCD62LloCD127loPD-1+KLRG1+CD43[1B11]+) at day 8 of infection. This discrepancy in activation marker expression resulted in a significant accumulation of splenic CD8+ T cells with a naive phenotype (CD44lo) and a reduction in the total number of activated-phenotype (CD44hi) CD8+ T cells in 2B4-KO mice in comparison to WT control mice at day 8 of infection (Figure 3B). An enhanced population of naive-phenotype CD8+ T cells was also evident in peripheral blood and in iLNs (Figure 3C) and persisted into late time points (e.g., day 100 p.i.) after infection (Figure 3D). Changes in activation marker expression were not observed on CD4+ T cells (Figure 3A).
Figure 3. Elevated frequency of naive-phenotype (CD44lo) CD8+ T cells in LCMV clone 13–infected 2B4-KO mice.
(A) Representative histograms demonstrate the expression of various activation receptors by CD8+ and CD4+ T cells at day 8 of LCMV clone 13 infection in WT (shaded histograms) and 2B4-KO (solid line) mice. The y axis represents percent of maximum. Numbers are mean proportion ± SD of WT (non-bold type) and 2B4-KO (bold type) T cells (n = 4 mice/group) falling with the gated expression range of each activation marker. (B) The mean ± SEM total number of naive (CD44lo) or activated (CD44hi) phenotype CD8+ T cells in the spleen of uninfected (n = 4/group) or day 8 clone 13–infected (n = 8/group) is plotted. (C) Histograms demonstrating reduced expression of CD44 by CD8+ T cells in the iLNs and lungs of 2B4-KO mice (n = 3–4/group, mean ± SD) at days 8 and 14 p.i. (D) Representative plots demonstrating a reduced frequency of CD44hi activated phenotype CD8+ T cells in 2B4-KO mice (n = 4/group, mean ± SD) at later time points of LCMV clone 13 infection. *P < 0.05, **P < 0.01 (2-tailed unpaired Student’s t test). Data are from 1 of 3 experiments with similar results.
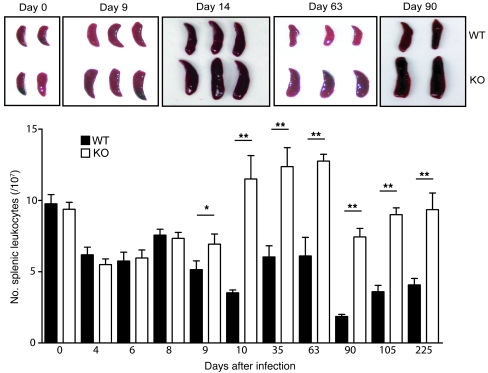
Spleen size is usually reduced during infection with the immunosuppressive clone 13 strain of LCMV (19), but we observed strikingly greater spleen size and leukocyte cellularity in LCMV clone 13–infected 2B4-KO mice compared with their infected WT counterparts as early as day 9 after infection, and these were still evident at 32 weeks after infection (Figure 4). The spleens of infected 2B4-KO mice were slightly larger than spleens of either uninfected WT or 2B4-KO mice. Although the increased numbers (Figure 3B) of CD8+ T cells with a naive phenotype (CD44lo) present in 2B4-KO mice contributed to the increased spleen size and leukocyte count (Figure 4), the frequencies of erythrocytes (WT: 3.7 × 108 ± 0.7 × 108 vs. KO: 11.1 × 108 ± 3.6 × 108, n = 3), CD11c+ DCs (WT: 1.1 × 105 ± 0.7 × 105 vs. KO: 3.5 × 105 ± 1.4 × 105, n = 4, P = 0.02), CD11b+ macrophages (WT: 5.4 × 106 ± 3.2 × 106 vs. KO: 17.0 × 106 ± 7.0 × 106, n = 4, P = 0.03), CD3+ T cells (WT: 2.9 × 106 ± 1.6 × 106 vs. KO: 5.3 × 106 ± 2.1 × 106, n = 4, P = 0.07), and CD19+ B cells (WT: 1.2 × 107 ± 0.6 × 107 vs. KO: 2.3 × 107 ± 0.9 × 107, n = 4, P = 0.08) were also increased at day 9 of infection in the spleens of 2B4-KO mice relative to WT controls. In contrast, lymphocyte numbers were not increased in the iLNs, liver, or lungs (data not shown) of 2B4-KO mice relative to WT controls at any time point after infection.
Figure 4. Splenomegaly during persistent LCMV clone 13 infection of 2B4-KO mice.
At various time points after LCMV clone 13 infection, spleens were photographed and the total number of splenic leukocytes determined after red blood cell lysis. Mean splenocyte counts (±SEM) are plotted for WT and KO mice (n = 4–10/group) throughout the course of infection. *P < 0.05, **P < 0.01 (2-tailed unpaired Student’s t test).
Reduced activation of CD8+ T cells during LCMV infection of 2B4-KO mice is not an intrinsic defect of 2B4-deficient CD8+ T cells.
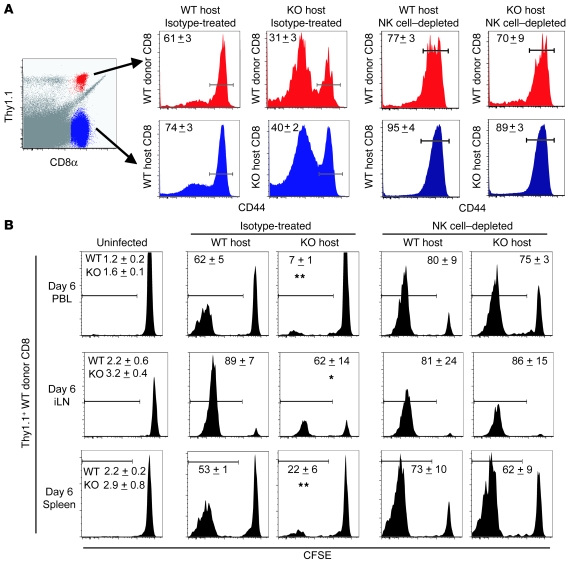
To test whether a 2B4-associated signaling defect in T cells was responsible for the weak T cell response and altered pathogenesis in 2B4-KO mice, we isolated bulk splenocytes from WT congenic mice (Thy1.1+) and transferred them into either Thy1.2+ WT or Thy1.2+ 2B4-KO mice prior to infection of recipient mice with LCMV clone 13. In WT recipients, both WT donor (Thy1.1+) and WT host (Thy1.2+) CD8+ T cells displayed a primarily activated phenotype (CD44hi) at day 6 of infection (Figure 5A). In contrast, WT donor CD8+ T cells transferred into a 2B4-deficient mouse maintained a principally naive phenotype (CD44lo), similar to that observed among host 2B4-KO CD8+ T cells after infection (Figure 5A). Reciprocal transfers of 2B4-deficient splenocytes (Ly5.2+) into congenic WT mice (Ly5.1+) resulted in both donor 2B4-KO (Ly5.2+) and host WT (Ly5.1+) CD8+ T cells at day 6 of infection displaying a predominantly activated (CD44hiCD43[1B11]+) phenotype similar to that of WT donor (Ly5.2+) CD8+ T cells transferred into WT (Ly5.1+) host mice (Supplemental Figure 3). Together these results indicated that the high frequency of naive phenotype CD8+ T cells in 2B4-KO mice (Figure 3) was not an intrinsic defect of 2B4-deficient CD8+ T cells.
Figure 5. Reduced activation of CD8+ T cells in 2B4-KO mice is caused by NK cells rather than defects in CD8-intrinsic 2B4 signaling.
WT congenic (Thy1.1+) splenocytes (3 × 107) were i.v. transferred into WT and 2B4-KO mice (Thy1.2+ host) 1 day before infection with LCMV clone 13. Two days before transfer, some groups of recipient mice received 25 μg of either isotype (IgG2a) control or anti-NK1.1 mAb. (A) Representative gating of Thy1.1+ (donor, red) and Thy1.1– (host, blue) CD8+ T cells in WT and 2B4-KO recipient mice at day 6 p.i. is shown at left. Expression of CD44 on donor (red histograms) and host (blue histograms) CD8+ T cells is shown, with numbers representing mean ± SD of CD44hi CD8+ T cells. (B) CFSE dilution (mean ± SD CFSElo) is shown for Thy1.1+ (donor) CD8+ T cells in the spleen, iLN, and blood of recipient mice. *P < 0.05, **P < 0.01 (2-tailed unpaired Student’s t test). Data are from 1 of 3 experiments with similar results.
In order to assess whether loss of 2B4 affects the activation and expansion of virus-specific CTLs, WT Thy1.1+ CD8+ T cells were labeled with CFSE and transferred into both WT (Thy1.2+) and 2B4-KO (Thy1.2+) mice. Following infection with LCMV clone 13, the proportion of WT donor CD8+ T cells that diluted CFSE was greater in WT mice than in 2B4-KO mice at day 6 of infection (Figure 5B). Moreover, the proportion of tetramer-defined LCMV NP205-212–specific WT donor CD8+ T cells was higher in WT hosts than in 2B4-KO recipients (WT: 13.7% ± 0.2% vs. KO: 2.0% ± 0.5%, n = 3, P = 0.0001). Consistent with the unaltered phenotype of endogenous CD4+ T cells in 2B4-KO mice, WT donor CD4+ T cells transferred into 2B4-KO mice upregulated CD44 and diluted CFSE in a similar fashion to WT CD4+ T cells transferred into WT mice (data not shown).
Role for NK cells in regulating LCMV-specific CD8+ T cell responses.
As NK cells constitutively express 2B4 (7), we tested whether NK cells may regulate CD8+ T cell activation in 2B4-KO mice. Specific depletion of NK cells was achieved through i.p. administration at 1 day before LCMV infection of a single dose of 25 μg anti-NK1.1, which, because of their lower expression of NK1.1 in comparison to NK cells, did not reduce numbers of γδ T cells (data not shown) or NK T cells (Supplemental Figure 4). Depletion of NK cells in 2B4-KO mice prior to transfer of WT donor splenocytes and subsequent LCMV infection resulted in restoration of both host (2B4-KO) and donor (WT) CD44 expression to levels observed on CD8+ T cells in WT mice at day 6 p.i. (Figure 5A), when most of the cells expressed an activated (CD44hi) phenotype. In addition, the dilution of CFSE by donor CD8+ T cells in 2B4-KO mice was similar to WT levels following depletion of NK cells (Figure 5B). Of note, depletion of NK cells in either strain of recipient mice appeared to slightly increase the proportion of host and donor CD8+ T cells that display high CD44 or low CFSE expression (Figure 5, A and B), suggesting that there is also a role for WT NK cells in regulating CD8+ T cell responses during LCMV clone 13 infection.
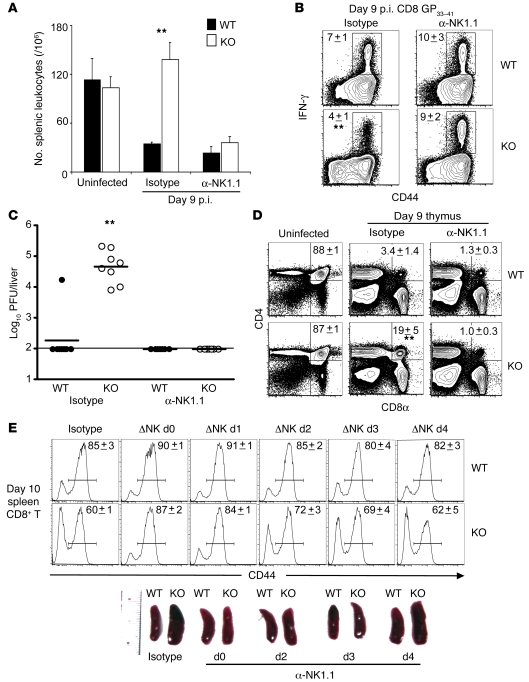
The enhancement of spleen size and splenocyte number (Figure 6A), reduction of LCMV GP33-41–specific IFN-γ responses (Figure 6B), and increase in numbers of naive phenotype CD8+ T cells in 2B4-KO mice (Figure 5A) were all abrogated by transient depletion of NK cells at the time of LCMV clone 13 inoculation. The reduced cytolysis of CTL targets in 2B4-KO mice during in vivo cytotoxicity assays was also restored to WT levels by NK cell depletion (data not shown). Moreover, the prolonged viral persistence evident at day 90 of infection in 2B4-KO mice was completely prevented by NK cell depletion just prior to infection (Figure 6C). In order to confirm the role of NK cells in regulating CD8+ T cell responses in 2B4-KO mice, NK cells were selectively depleted with a carefully titrated dose of anti-asialo GM1 antibody, as described previously (20). Similar to anti-NK1.1 antibody administration, the decreased numbers of LCMV GP33-41–specific IFN-γ–producing splenic CD8+ T cells (WT: 3.9 × 105 ± 1.3 × 105 vs. KO: 0.7 × 105 ± 0.2 × 105, n = 3) at day 6 of infection in 2B4-KO mice were restored to WT levels by NK cell depletion using anti-asialo GM1 antibody (WT: 5.8 × 105 ± 0.4 × 105 vs. KO: 4.6 × 105 ± 0.5 × 105, n = 3).
Figure 6. Depletion of NK cells restores LCMV-specific CD8+ T cell responses and viral clearance in 2B4-KO mice to WT levels.
(A–D) One day prior to infection, WT and 2B4-KO mice (n = 4–8/group) were treated with 25 μg isotype (IgG2a) or anti-NK1.1 mAb i.p. (A) Splenic leukocytes (mean ± SD) were enumerated on day 9 p.i. in WT and 2B4-KO mice. (B) Mean proportion (±SD) of IFN-γ+ CD8+ T cells in spleen after GP33-41 stimulation. (C) Viral titers at day 90 p.i. (n = 7–8/group) are displayed as log10 PFU/liver. The horizontal line represents the limit of detection for the plaque assay (log10 2.0). (D) Mean (±SD) fraction of DP thymocytes within thymus of uninfected or day 9 p.i. WT and 2B4-KO mice. (E) A single injection of anti-NK1.1 mAb was administered at various time points (day 0 to day 4) relative to the time of infection with LCMV clone 13. Representative spleen size (photo) and CD44 expression (y axis represents percent of maximum) on splenic CD8+ T cells was determined at day 10 of infection (n = 2 mice/group, mean ± SD). *P < 0.05, **P < 0.01 (2-tailed unpaired Student’s t test). Data are from 1 of 3 experiments with similar results.
By day 10 of LCMV clone 13 infection, the thymus underwent dramatic involution, with a greater than 90% reduction in total thymic cellularity in both WT and 2B4-KO mice (data not shown). Nevertheless, the frequency of CD4/CD8 double-positive (DP) thymocytes was higher in 2B4-deficient mice (Figure 6D). The numbers of DP thymocytes were restored to infected WT levels after NK cell depletion of 2B4-KO mice (Figure 6D). Thus, NK cells appear to play a critical role in all of the phenotypes of 2B4-KO mice described in this article.
Time requirements for NK cell depletion.
Administration of anti-NK1.1 depleting mAbs at 0, 1, or 2 days after infection converted the day 10 phenotype of CD8+ T cells in 2B4-deficient hosts to the WT infection phenotype (Figure 6E); however, this treatment began to lose its efficacy when anti-NK1.1 antibody was administered at 3 or 4 days after infection. Figure 6E shows the enhanced naive CD44lo phenotype and reappearance of large spleens characteristic of 2B4-KO mice when NK cells were depleted from these mice at day 3 or 4. Taken together, these data suggest that 2B4-deficient NK cells have an inhibitory effect on CD8+ T cell activation in the first few days of persistent infection.
2B4-deficient NK cells cytolytically target activated CD8+ T cells.
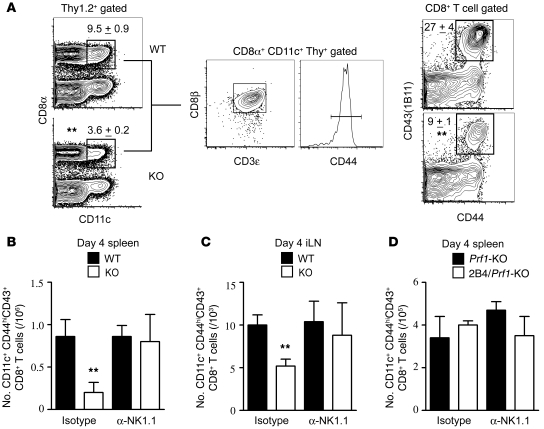
In order to determine whether reduced CD8+ T cell responses in 2B4-KO mice were a result of NK cell targeting of CD8+ T cells directly or through disruption of antigen presentation by NK cell targeting of DCs, we determined the frequencies of various DC subpopulations as well as the expression of T cell activation markers on CD8+ T cells in WT and 2B4-KO mice at early time points after infection. At very early stages of infection (day 4 p.i.), we began to see accumulation of highly activated CD8+ T cells (CD3+Thy1.2+CD8αβ+CD44hi) in the spleen (Figure 7, A and B) and iLN (Figure 7C) of WT mice. These activated CD8+ T cells were characterized by upregulated expression of both the activation-associated isoform (1B11) of CD43 (21) and the DC marker CD11c (22) (Figure 7A).
Figure 7. NK cells mediate early loss of highly activated CD8+ T cells in 2B4-KO mice in a perforin-dependent manner.
(A) At day 4 of LCMV clone 13 infection, splenocytes (n = 4/group) were gated on Thy 1.2-expressing cells, and the proportion of CD8α+ T cells expressing CD11c was determined. The Thy1.2+CD8α+CD11c+ events were uniformly CD8β+, CD3ε-expressing, and CD44hi. Right: Proportion of CD44hiCD43(1B11)+ events among gated CD8αβ+ T cells. Numbers represent mean (±SD) proportion of gated events. Total numbers (mean ± SEM) of Thy1.2+CD11c+CD8α+ cells were determined in the spleens (B) as well as iLNs (C) of isotype-treated or anti-NK1.1–treated WT and 2B4-KO mice (n = 5/group), as well as in the spleens (D) of similarly treated Prf1-KO and 2B4/Prf1-KO (n = 3–4/group) mice. **P < 0.01 (2-tailed unpaired Student’s t test). Data are from 1 of 3 experiments with similar results.
The frequency of these highly activated CD8+ T cells (CD3+Thy1.2+CD8αβ+CD44hiCD43[1B11]+CD11c+) was significantly reduced in both the spleen (Figure 7, A and B) and iLNs (Figure 7C) of 2B4-KO mice. Depletion of NK cells prior to infection restored the frequency of these highly activated CD8+ T cells in 2B4-KO mice to WT levels (Figure 7, B and C). In addition, the frequencies of several DC subsets were decreased in the spleens of both WT and 2B4-KO mice after LCMV infection (Supplemental Figure 5), but in contrast to frequencies of activated CD8+ T cells, DC loss at this time point was not prevented by NK cell depletion (data not shown).
We previously demonstrated that 2B4-deficient NK cells kill other NK cells upon activation with IL-2 in vitro and CpG DNA in vivo, resulting in reduced peripheral NK cell numbers (23). However, splenic NK cell frequencies (WT: 1.8 × 106 ± 0.9 × 106 [3.3% ± 0.2%] vs. KO: 1.4 × 106 ± 0.8 × 106 [3.2% ± 0.3%], n = 15, P = 0.3) were not significantly reduced in the spleen of 2B4-KO mice at day 4 of LCMV clone 13 infection. NK cell frequencies were also similar in the spleens of WT and 2B4-KO mice at day 3 (WT: 9.0 × 105 ± 1.9 × 105 [1.5% ± 0.3%] vs. KO: 8.6 × 105 ± 1.8 × 105 [1.4% ± 0.3%], n = 11, P = 0.9) and day 6 (WT: 1.3 × 106 ± 0.4 × 106 [2.0% ± 0.3%] vs. KO: 1.0 × 106 ± 0.1 × 106 [2.4% ± 0.1%], n = 3) of infection. Thus, the importance of NK cell fratricide in the absence of 2B4 (23) may be dependent upon the context of NK cell activation.
In order to determine whether NK cells may directly target activated CD8+ T cells for cytolysis, perforin-deficient (Prf1-KO) and 2B4/perforin double-KO (2B4/Prf1-KO) mice were infected with LCMV clone 13. At day 4 p.i., the two strains of mice displayed similar numbers (Figure 7D) and proportions (Supplemental Figure 6) of highly activated (CD44hiCD11c+) CD8+ T cells. Importantly, depletion of NK cells in Prf1-KO and of 2B4/Prf1-KO mice had minimal impact on the frequency of activated CD8+ T cells at day 4 (Figure 7D).
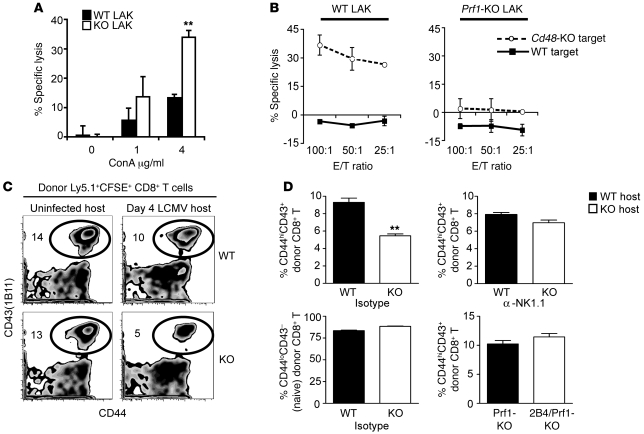
In order to determine whether NK cell killing accounts for the decrease of the virus-specific T cell responses, we first assessed the activity of WT and 2B4-KO NK cells against activated CD8+ T cells in vitro. WT lymphokine-activated killer (LAK) cells displayed low levels of cytolytic activity against WT concanavalin A–activated (ConA-activated) syngeneic CD8+ T cells, but 2B4-deficient LAK cells readily lysed these activated CD8+ T cell targets (Figure 8A). Likewise, WT LAK cells mediated killing of activated CD8+ T cells when these targets were derived from Cd48-KO mice, which lack the ligand for 2B4 (Figure 8B). The killing of Cd48-KO target cells was abrogated by perforin deficiency within the effector cell population (Figure 8B). Importantly, the ability of 2B4-deficient NK cells to kill CD8+ T cells was dependent upon activation of these T cells, as very little killing of nonactivated (0 μg/ml ConA) T cells occurred (Figure 8A). These experiments directly demonstrate a perforin-dependent killing of activated T cells by activated 2B4-KO NK cells in vitro.
Figure 8. NK cells mediate specific lysis of activated CD8+ T cells in the absence of 2B4 in vitro and in vivo.
(A) WT (black bars) or 2B4-KO (white bars) LAK cell killing (mean ± SD) of WT CD8+ T cell targets, activated in vitro with various doses of ConA. (B) Specific lysis (mean ± SD) of WT or CD48-KO ConA-activated CD8+ T cells by WT (left) or by Prf1-KO (right) LAK cells is shown at various effector to target (E/T) ratios. (C and D) A modified in vivo cytotoxicity assay was done by injecting CFSE-labeled splenocytes (3 × 107) from LCMV-infected (day 4 p.i.) congenic (Ly5.1+) WT mice into uninfected or LCMV-infected (day 4 p.i.) WT and 2B4-KO mice (Ly5.2+, n = 5–6/group), some of which were depleted of NK cells 1 day prior to infection. Five hours after transfer, the proportion of activated (CD44hiCD43[1B11]+) donor (Ly5.1+CFSE+) cells was determined in each mouse. (C) Representative CD44 and CD43(1B11) expression by donor Ly5.1+CFSE+ CD8+ T cells. Numbers are the percentage of donor (Ly5.1+CFSE+) CD8+ T cells that are CD44hiCD43(1B11)+ for the representative sample shown. (D) Top graphs depict the percentage of activated CD44hiCD43(1B11)+ donor (Ly5.1+CFSE+) CD8+ T cells in isotype- (left) or anti-NK1.1–treated (right) WT and 2B4-KO mice. Lower left plot demonstrates the proportion of naive phenotype (CD44loCD43[1B11]–) donor (Ly5.1+CFSE+) CD8+ T cells in isotype-treated WT and 2B4-KO mice. Lower right plot depicts the percentage of activated CD44hiCD43(1B11)+ donor (Ly5.1+CFSE+) CD8+ T cells in Prf1-KO and 2B4/Prf1-KO mice. Results are presented as mean ± SD. **P < 0.01 (2-tailed unpaired Student’s t test). Data are from 1 of 3 similar experiments.
We next asked whether a similar NK cell–mediated elimination of activated CD8+ T cells would occur in vivo. In a modified in vivo cytotoxicity assay, mixed populations of naive and activated CD8+ T cells from LCMV-infected congenic (Ly5.1+) WT mice (day 4 p.i.) were labeled with CFSE and transferred into WT or 2B4-KO mice at day 4 of LCMV clone 13 infection. The survival of donor (Ly5.1+CFSE+) CD8+ T cells with an activated (CD44hiCD43+) or naive (CD44loCD43–) phenotype was examined 5 hours after transfer (Figure 8, C and D). Over the course of this 5-hour assay, there was no detectable target cell division (i.e., dilution of CFSE) among the donor CD8+ T cell populations (data not shown). Importantly, the frequencies of activated but not naive phenotype donor CD8+ T cells were reduced in 2B4-KO host mice (Figure 8, C and D), and this loss was abrogated by NK cell depletion of 2B4-KO recipient mice prior to infection (Figure 8D). Similar transfers of activated CD8+ T cell–containing populations were conducted in Prf1-KO and 2B4/Prf1-KO mice, with comparable survival of activated donor CD8+ T cells in both strains (Figure 8D). T cell targets from LCMV-infected Cd48-KO mice were not tested in this system because Cd48-KO mice have a defect in T cell activation (24). Taken together, these results suggest that activated 2B4-deficient NK cells kill activated CD8+ T cells in a perforin-dependent manner in vitro and in vivo.
Discussion
Here we demonstrate that a long-term persistent viral infection associated with altered T cell activation may actually be regulated by NK cells acting during the first few days of infection. This NK cell–mediated regulation of T cell responses is itself regulated by 2B4 on the NK cells, not the T cells, which also can express 2B4. In the absence of 2B4-mediated inhibition, activated NK cells cytolytically targeted highly activated CD8+ T cells, resulting in a significant culling of these LCMV-specific effectors. This loss of virus-specific CD8+ T cells impaired control of virus replication, causing delayed viral clearance and altered immune pathologies. Therefore, our results suggest that 2B4-mediated regulation of NK cell activity within a highly inflammatory lymphoid environment is both crucial for antiviral defense and nonredundant with the role of MHC in maintaining self-tolerance of NK cells.
Recently, much emphasis has been placed on the role of inhibitory receptors such as PD-1 in CD8+ T cell exhaustion during chronic virus infections in mice (LCMV clone 13) (25) and humans (HIV, HCV) (26–28). Blockade of PD-1 in vitro and in vivo results in “rescue” of the proliferation and effector functions of exhausted virus-specific CD8+ T cells, thereby leading to enhanced control of virus (25, 26, 29–31). However, exhausted CD8+ T cells express a number of different inhibitory receptors, including 2B4, which have been suggested to synergistically contribute to the severity of T cell dysfunction (11, 12). We demonstrate here that 2B4-deficient LCMV-specific CD8+ T cells underwent clonal exhaustion and were deleted (e.g., NP396-404) similarly to 2B4-sufficient T cells in WT mice. However, the magnitude of the total LCMV-specific CTL response was reduced by NK cells lacking 2B4. Although 2B4 expressed on CD8+ T cells has been suggested to both augment (13) and inhibit (11) T cell activation, our adoptive transfers of WT as well as 2B4-KO lymphocytes into 2B4-deficient and 2B4-sufficient environments demonstrated that deficiencies in CD8+ T cell activation associated with genetic ablation of 2B4 were CD8+ T cell extrinsic and regulated by NK cells. In fact, WT and 2B4-KO CD8+ T cells from infected mice were phenotypically indistinguishable in the absence of NK cells. These experiments demonstrate that despite similar expression patterns of 2B4 and PD-1 on LCMV-specific T cells, it is the inhibition of NK cell cytolytic activity by 2B4 expressed on NK cells that regulates antiviral T cell responses during persistent infection. Therefore, the effect of 2B4 blockade on NK cell activity should be considered when designing therapies for persistent virus infection that are based on antibody blockade of 2B4 expressed on exhausted CD8+ T cells.
Several recent studies have also suggested that NK cells indirectly regulate antiviral T cell responses during murine cytomegalovirus (MCMV) infection through interactions with DCs (32–34). However, interpretation of these results is hampered because NK cells are vital to control of MCMV replication (35, 36), and high viral loads in the absence of NK cells may adversely affect virus-specific CD8+ T cell responses (37). In the case of LCMV, NK cells do not play a role in direct control of early viral loads (38, 39). In our study, the NK cell–independent reduction of DC numbers in both WT and 2B4-KO mice suggested that NK cell–mediated regulation of CD8+ T cells was not a result of NK cell–DC interactions. Moreover, CD4+ T cell frequencies were not altered after NK cell depletion, indicating that they were getting sufficient stimulation from antigen-presenting cells. These data indicate that NK cells did not control activated CD8+ T cell responses through a DC intermediary in this system, though they do not rule out NK cell–mediated regulation of immune responses via interaction with DCs in other circumstances.
Activated CD8+ T cells transferred into LCMV-infected 2B4-KO mice were rapidly (within 5 hours) lost in an NK cell– and perforin-dependent manner. This rapid loss of CD8+ T cells without evidence of cellular division (e.g., CFSE dilution) argues for a direct mechanism whereby NK cells eliminate activated CD8+ T cells. In mice with a combined genetic deficiency of perforin and 2B4, NK cells did not mediate a reduction of highly activated CD8+ T cells within lymphoid tissues. NK cell depletion did not further augment the number of activated CD8+ T cells present in lymphoid organs of 2B4/Prf1-KO mice, suggesting that perforin is a crucial component of the NK cell–mediated regulation of CD8+ T cell activation. Of note, the frequencies of activated CD8+ T cells were also marginally increased in perforin-deficient and NK cell–depleted WT mice relative to nondepleted WT controls. Indeed, we have found that under certain conditions of infection, NK cells may shape the kinetics and functionality of antiviral CD8+ T cell responses in WT mice (S.N. Waggoner and R.M. Welsh, unpublished observations).
In contrast to the reduced spleen size typically observed during infection of WT C57BL/6 mice with the immunosuppressive clone 13 strain of LCMV (19), we observed an increase in both the size and leukocyte cellularity of the spleen during LCMV clone 13 infection of 2B4-deficient mice. Increased frequencies of multiple lymphocyte lineages contributed to the enhanced splenic leukocyte counts in 2B4-KO mice, including T cells, B cells, macrophages, and DCs. Acute infection of WT mice with the Armstrong strain of LCMV characteristically results in splenomegaly associated with the accumulation of large numbers of activated, LCMV-specific T cells (40, 41). In contrast, the majority of CD8+ T cells in the enlarged spleens of LCMV clone 13–infected 2B4-KO mice displayed a naive phenotype (CD44lo), and these naive cells accumulated in 2B4-KO mice to 3-fold-higher levels than in their infected WT counterparts. The enhanced frequency of CD4/CD8-DP thymocytes in 2B4-KO mice may be indicative of increased thymic output of naive CD8-single-positive lymphocytes during LCMV infection of 2B4-KO mice, which could contribute to increased numbers of peripheral CD8+ T cells with a naive phenotype. However, the frequency of naive-phenotype 2B4-KO CD4+ T cells was not increased in a similar fashion. Through depletion of NK cells, we established that NK cells play an important role in regulating both the altered splenic and thymic compositions of 2B4-KO mice, although the exact mechanism driving augmented naive CD8+ T cell as well as total lymphocyte accumulation in the spleen remains to be determined.
According to the missing self hypothesis, loss or reduction of MHC class I molecule expression renders cells susceptible to NK cell–mediated killing (42). We found that the highly activated CD8+ T cells susceptible to NK cell–mediated killing in LCMV-infected 2B4-KO mice actually expressed increased levels of class I MHC molecules (S.N. Waggoner and R.M. Welsh, unpublished observations), indicating that the protective effect of MHC class I molecule expression is insufficient for self-tolerance to activated NK cells in the absence of 2B4. Thus, as described elsewhere (3), the protective effect of MHC class I and CD48 on control of self-killing are nonredundant. Of interest is that the numbers and phenotype of LCMV-specific CD4+ T cells were not altered in 2B4-deficient mice. This suggests that the features of activated CD8+ T cells that target them for NK cell–mediated cytolysis may not be shared by activated CD4+ T cells, or that the kinetic delay of LCMV-specific CD4+ T cells responses previously described (43, 44) may temporally separate activated NK and CD4+ T cells.
We demonstrate that, in the absence of 2B4, NK cells cytolytically targeted activated (CD44hi) but not naive (CD44lo) CD8+ T cells during persistent LCMV infection. This suggests that although 2B4 can both enhance and suppress NK cell activation (7, 8), 2B4-mediated inhibitory signals are of greater significance in the regulation of antiviral immune responses during virus infection in vivo. Furthermore, the specificity of NK cell–dependent killing of activated CD8+ T cells but not other 2B4 ligand (CD48)–expressing lymphocytes in 2B4-KO mice suggested that additional NK cell receptor ligands must be present on activated CD8+ T cells that distinguish these cells for killing. A previous report suggested that ligands of the activating NK cell receptor NKG2D are transiently upregulated during in vitro activation of CD8+ T cells (45). To date, our investigation of CD8+ T cells (WT and 2B4-KO) activated during LCMV infection in vivo has failed to detect expression of NKG2D ligands by these activated lymphocytes, regardless of the presence or absence of NK cells (S.N. Waggoner and R.M. Welsh, unpublished observations). In addition, our vivo blockade of NKG2D by i.p. anti-NKG2D antibody (CX5) administration did not restore CD8+ T cell activation in 2B4-KO mice to WT levels (data not shown). Further study is required to identify the features of activated CD8+ T cells that distinguish these lymphocytes from naive lymphocytes as targets for NK cell killing.
We further sought to examine whether NK cell regulation of antiviral CD8+ T cell responses in the absence of 2B4 is restricted to persistent LCMV clone 13 infection or is a characteristic of multiple virus infections. Our preliminary data demonstrated an NK cell–dependent 50% reduction in the frequency of LCMV-specific splenic CD8+ T cells in 2B4-KO mice relative to WT controls at day 6 of acute LCMV Armstrong infection (S.N. Waggoner and R.M. Welsh, unpublished observations). However, both strains of mice mediated clearance of replicating virus by day 9 of infection, and 2B4-KO mice established LCMV-specific T cell memory populations that were similar to those present in immune WT mice. Our preliminary experiments also revealed that 2B4 deficiency altered T cell responses to Pichinde virus, MCMV, and mouse hepatitis virus infections. Therefore, although NK cell regulation of T cell responses in the absence of 2B4 is characteristic of numerous virus infections, the impact of this regulation on antiviral immunity may be virus strain–dependent.
Signaling in NK or CD8+ T cells following 2B4 engagement depends in part upon association of 2B4 with the SLAM-associated protein (SAP/SH2D1A) (46, 47). In patients with the rare genetic immunodeficiency X-linked lymphoproliferative syndrome (XLP), the SH2D1A (SAP) gene is altered or absent (48), resulting in a cytolytic defect of NK cells and CTLs. Frequent childhood fatality in XLP patients is associated with uncontrolled virus infections and activated CD8+ T cell–mediated hepatic necrosis (49). Persistent, but not acute, LCMV or herpesvirus infections of SAP-deficient (Sh2d1a–/–) mice recapitulate many facets of XLP disease (50, 51). Recently, we demonstrated that low expression levels of SAP result in strong suppression of NK cell activation following 2B4 engagement (52). Although 2B4 has not been directly implicated in the phenotypes of XLP patients or SAP-deficient mice, 2B4-induced inhibitory signals in the absence of SAP may contribute to the cytolytic defects of NK and CD8+ T cells. Moreover, 2B4-mediated inhibitory signals may prevent NK cells from restraining the activated antiviral CTLs responsible for tissue destruction. Of note, polymorphisms associated with increased expression of 2B4 correlate with increased incidence of autoimmune diseases (53). The importance of 2B4 in restricting NK cell killing of activated lymphocytes during pathogenesis of human disease remains to be determined.
Our results therefore demonstrate that NK cells acting early in infection can alter the magnitude and duration of viral persistence through regulation of developing antiviral T cell responses. The two persistent human infections with greatest similarity to that of LCMV in the mouse are HIV, whose infections are characterized by distinct antigen load set points per individual (54), and HCV, whose infections are characterized by wide variations in timing of clearance. We suggest that NK cells acting early in these infections should be considered as possible contributors to these T cell–regulated events.
Methods
Mice.
WT C57BL/6, B6.PL Thy-1a/Cy (Thy1.1), and perforin-deficient mice (10) were obtained from The Jackson Laboratory. Ly5.1 congenic mice on a C57BL/6 background (B6.SJL-Ptprc<a>) were purchased from Taconic Farms. 2B4-deficient mice were generated in C57BL/6-derived embryonic stem cells as previously described (10). 2B4-deficient mice were bred and maintained at the University of Massachusetts Medical School (UMMS). Perforin- and 2B4-deficient (2B4/Prf1-KO) mice were bred and maintained at the University of Chicago. CD48-deficient mice were provided by Arlene Sharpe (Harvard University, Cambridge, Massachusetts, USA) (24). Experiments were routinely done using male mice at 6–12 weeks of age. All mice were maintained under specific pathogen–free conditions within either the Department of Animal Medicine at UMMS or at the University of Chicago. All experiments were performed according to a protocol approved by the Institutional Animal Care and Use Committee of UMMS.
Virus infections and in vivo NK cell depletion.
The highly disseminating clone 13 variant of LCMV was propagated in baby hamster kidney BHK21 cells (55, 56). Virus was titrated by plaque assay on Vero cells. Persistent infections were initiated by infecting mice i.v. with 2 × 106 PFU of the clone 13 strain of LCMV. In order to specifically deplete NK cells, mice received a single i.p. injection of 25 μg anti-NK1.1 (PK136) or control rat IgG2a produced by Bio-X-Cell, 1 day before virus infection. Alternatively, mice received 10 μl of anti-asialo GM1 antibody (Wako Pure Chemical) diluted in 200 μl PBS i.p. 1 day prior to virus infection.
Antibodies and FACS analysis.
Fluorescently labeled mAbs purchased from BD Biosciences were the following: CD3 (145-2C11), CD4 (RM4-5), CD8α (clone 53-6.7), CD8β (clone 53-5.8), CD48 (HM48-1), H-2Kb (AF6-88.5), CD90.2 (clone 53-2.1), CD45.2 (1D4), I-Ab (AF6-120.1), CD11c (HL3), CD11b (M1/70), NK1.1 (PK136), CD44 (IM7), CD62L (MEL-14), CD69 (H1.2F3), IL-2 (3C7), IFN-γ (XMG1.2), TNF (MP6-XT22), CD107a (1D4B), CD107b (ABL-93), B220 (RA3-6B2), CD19 (1D3), and CD49b (DX5). mAbs purchased from eBioscience were the following: CD90.1 (OX-7), PD-1 (J43), CD127 (A7R34), CD45.1 (A20), KLRG1 (2F1), PDCA-1 (eBio927), 2B4 (eBio244F4), and granzyme B (16G6). Antibodies purchased from BioLegend include F4/80 (BM8), CD43 (1B11), and CD44 (IM7). Antibodies purchased from R&D Systems included anti-NKp46. For flow cytometric analysis, cells were analyzed on an LSR II cytometer (BD Biosciences), and data were analyzed using FlowJo software (Tree Star).
Tetramers and peptides.
Several previously defined T cell epitopes encoded by LCMV were used in this study (57, 58). LCMV-specific epitopes included NP396-404 (FQPQNGQFI), GP33-41 (KAVYNFATC), GP276-286 (SGVENPGGYCL), NP205-212 (YTVKYPNL), GP118-125 (ISHNFCNL), and GP61-80 (GLKGPDIYKGVYQFKSVEFD). All peptides listed were purchased from 21st Century Biochemicals and were purified with reverse-phase HPLC to 90% purity. MHC class I peptide tetramers specific for LCMV NP205/Kb, LCMV NP396/Db, and LCMV GP33/Db were generated as described previously (59). CD1d-PBS57-allophycocyanin tetramers were provided by the National Institute of Allergy and Infectious Diseases Tetramer Facility and were a gift of Leslie J. Berg (UMMS).
CFSE labeling and adoptive transfer.
Single-cell suspensions were prepared from spleens of congenic (Thy1.1+ or Ly5.1+) WT mice or 2B4-KO and WT mice (Thy1.2+Ly5.2+), and erythrocytes were removed by lysis using a 0.84% NH4Cl solution. Splenocytes were labeled with the 2 μM fluorescent dye CFSE (CFDA-SE, Molecular Probes, Invitrogen) for 15 minutes at 37°C, washed, and transferred i.v. (107 donor cells) to recipient mice.
In vitro cytotoxicity assay.
NK LAK cells were prepared by culturing splenocytes for 4 days in 1,000 U/ml recombinant human IL-2 (rhIL-2) (60). CD8+ T cells used as targets were enriched from spleen by coating splenocytes with FITC anti-CD8α mAb and using the EasySep FITC Selection Kit from StemCell Technologies. Enriched CD8+ T cells (75%–90% CD8+) were incubated for 24–48 hours in 4 μg/ml ConA from Sigma-Aldrich, unless otherwise described.
Target cells were labeled with 100 μC of sodium chromate (51Cr) for 1 hour at 37°C, washed, and then plated at 2,000 cells per well. Effector NK LAK cells were added at the indicated ratios to triplicate wells. After 5 hours of incubation at 37°C, supernatants were collected for analysis, and percent specific lysis was calculated using standard methods.
In vivo cytotoxicity assays.
Assays to measure T cell cytolytic activity in vivo were done as described previously (18). Briefly, spleens were harvested from uninfected WT mice, and single-cell suspensions were prepared. Separate populations of splenocytes were then loaded with LCMV peptides (1 μM) for 10 minutes at 37°C before labeling with different concentrations of CFSE (2.5, 1, or 0.4 μM, Molecular Probes, Invitrogen) for 15 minutes at 37°C. These populations were then washed and combined at equal ratios and adoptively transferred i.v. into naive or infected recipients. Spleens from recipient mice were harvested 4–20 hours later, and the survival of each transferred population was assessed by flow cytometry. Specific lysis was calculated using the following equation: 100 – ([% LCMV target population in infected experimental/% unlabeled population in infected experimental) ÷ (% LCMV target population in naive control/% unlabeled population in naive control)] × 100).
An unconventional in vivo cytotoxicity assay was adapted to determine NK cell killing of lymphocyte populations in vivo as follows. Congenic (Ly5.1) WT mice were infected with 2 × 106 PFU LCMV clone 13 i.v., and at day 4 p.i., single-cell suspensions were made from the spleens of these infected donor mice. These cells were then labeled, for ease of detection, with CFSE, and 2 × 107 bulk splenocytes containing both activated- and naive-phenotype populations of CD8+ T cells were transferred into experimental recipient mice on day 4 of LCMV clone 13 infection. The recipient mice were WT (Ly5.2), 2B4-KO (Ly5.2), Prf1-KO (Ly5.2), or 2B4/Prf1-KO (Ly5.2) mice that were administered anti-NK1.1 or isotype control antibodies 1 day prior to infection with 2 × 106 PFU LCMV clone 13 i.v. Some recipient mice were uninfected and served as controls. CFSE-labeled target cells were transferred at day 4 of infection, and after 5 hours, spleens of recipient mice were harvested for analysis of survival of donor CD8+ T cells.
Lymphocyte preparation and intracellular cytokine assay.
Single-cell leukocyte suspensions were prepared from spleens, iLNs, and peripheral blood by lysing erythrocytes using a 0.84% NH4Cl solution. Lung and liver lymphocytes were harvested by mechanical and enzymatic digestion of tissues, as described previously (61, 62). Briefly, livers were homogenized and then digested for 10 minutes at 37°C in HBSS containing 10 U/ml DNase I and 0.5 mg/ml collagenase type II (Sigma-Aldrich), and 10% fetal bovine serum. These homogenates were washed and leukocytes isolated by centrifugation on a Lympholyte M (Cedarlane Laboratories) gradient. Prepared single-cell suspensions from various tissues were plated at 2 × 106 cells per well in 96-well plates and stimulated for 5 hours at 37°C with either 1 μM viral peptide or 2.5 μg/ml anti-CD3 mAb in the presence of brefeldin A and 0.2 U/ml rhIL-2. Following stimulation, cells were preincubated with a 1:200 dilution of Fc Block (2.4G2) in FACS buffer (HBBS, 2% FCS, 0.1% NaN3) and then stained for 20 minutes at 4°C with various combinations of fluorescently tagged mAbs. After washing, cells were permeabilized using BD Cytofix/Cytoperm solution and then stained in BD Perm/Wash using mAbs specific for various cytokines.
Statistics.
Results are displayed as mean ± SD (for variation within individual experiments) or SEM (for variation between experiments), with statistical differences between experimental groups determined using a 2-tailed unpaired Student’s t test, where a P value less than 0.05 was considered significant.
Supplementary Material
Acknowledgments
We thank Michael A. Brehm and Liisa K. Selin for helpful discussions and Keisha Mathurin and Keith Daniels for technical support. We also thank Arlene Sharpe (Harvard University) for CD48-deficient mice and Leslie Berg (UMMS) for NK T cell tetramer. We thank Lewis Lanier (UCSF) for providing us with anti-NKG2D blocking antibody (CX5). We appreciate the role of Susan E. Stepp in initiating these studies. This work was supported by NIH training grant AI07349 (to S.N. Waggoner) and research grants AI-17672, AR-35506, and CA34461 (to R.M. Welsh). The views expressed are those of the authors and do not necessarily express the views of the NIH.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2010;120(6):1925–1938. doi:10.1172/JCI41264.
Ruth T. Taniguchi’s present address is: Diabetes Center, UCSF, San Francisco, California, USA.
References
- 1.Yokoyama WM, Kim S. How do natural killer cells find self to achieve tolerance? Immunity. 2006;24(3):249–257. doi: 10.1016/j.immuni.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Raulet DH, Vance RE. Self-tolerance of natural killer cells. Nat Rev Immunol. 2006;6(7):520–531. doi: 10.1038/nri1863. [DOI] [PubMed] [Google Scholar]
- 3.McNerney ME, Guzior D, Kumar V. 2B4 (CD244)-CD48 interactions provide a novel MHC class I-independent system for NK-cell self-tolerance in mice. Blood. 2005;106(4):1337–1340. doi: 10.1182/blood-2005-01-0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwartzberg PL, Mueller KL, Qi H, Cannons JL. SLAM receptors and SAP influence lymphocyte interactions, development and function. Nat Rev Immunol. 2009;9(1):39–46. doi: 10.1038/nri2456. [DOI] [PubMed] [Google Scholar]
- 5.Ma CS, Nichols KE, Tangye SG. Regulation of cellular and humoral immune responses by the SLAM and SAP families of molecules. Annu Rev Immunol. 2007;25:337–379. doi: 10.1146/annurev.immunol.25.022106.141651. [DOI] [PubMed] [Google Scholar]
- 6.Veillette A. Immune regulation by SLAM family receptors and SAP-related adaptors. Nat Rev Immunol. 2006;6(1):56–66. doi: 10.1038/nri1761. [DOI] [PubMed] [Google Scholar]
- 7.McNerney ME, Lee KM, Kumar V. 2B4 (CD244) is a non-MHC binding receptor with multiple functions on natural killer cells and CD8+ T cells. Mol Immunol. 2005;42(4):489–494. doi: 10.1016/j.molimm.2004.07.032. [DOI] [PubMed] [Google Scholar]
- 8.Assarsson E, Kambayashi T, Persson CM, Chambers BJ, Ljunggren HG. 2B4/CD48-mediated regulation of lymphocyte activation and function. J Immunol. 2005;175(4):2045–2049. doi: 10.4049/jimmunol.175.4.2045. [DOI] [PubMed] [Google Scholar]
- 9.Lee KM, et al. 2B4 acts as a non-major histocompatibility complex binding inhibitory receptor on mouse natural killer cells. J Exp Med. 2004;199(9):1245–1254. doi: 10.1084/jem.20031989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaidya SV, et al. Targeted disruption of the 2B4 gene in mice reveals an in vivo role of 2B4 (CD244) in the rejection of B16 melanoma cells. J Immunol. 2005;174(2):800–807. doi: 10.4049/jimmunol.174.2.800. [DOI] [PubMed] [Google Scholar]
- 11.Blackburn SD, et al. Coregulation of CD8+ T cell exhaustion by multiple inhibitory receptors during chronic viral infection. Nat Immunol. 2009;10(1):29–37. doi: 10.1038/ni.1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wherry EJ, et al. Molecular signature of CD8+ T cell exhaustion during chronic viral infection. Immunity. 2007;27(4):670–684. doi: 10.1016/j.immuni.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Kambayashi T, Assarsson E, Chambers BJ, Ljunggren HG. Cutting edge: regulation of CD8(+) T cell proliferation by 2B4/CD48 interactions. J Immunol. 2001;167(12):6706–6710. doi: 10.4049/jimmunol.167.12.6706. [DOI] [PubMed] [Google Scholar]
- 14.Sayos J, et al. Potential pathways for regulation of NK and T cell responses: differential X-linked lymphoproliferative syndrome gene product SAP interactions with SLAM and 2B4. Int Immunol. 2000;12(12):1749–1757. doi: 10.1093/intimm/12.12.1749. [DOI] [PubMed] [Google Scholar]
- 15.Ostrowski SR, Ullum H, Pedersen BK, Gerstoft J, Katzenstein TL. 2B4 expression on natural killer cells increases in HIV-1 infected patients followed prospectively during highly active antiretroviral therapy. Clin Exp Immunol. 2005;141(3):526–533. doi: 10.1111/j.1365-2249.2005.02869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wherry EJ, Blattman JN, Murali-Krishna K, van der MR, Ahmed R. Viral persistence alters CD8 T-cell immunodominance and tissue distribution and results in distinct stages of functional impairment. J Virol. 2003;77(8):4911–4927. doi: 10.1128/JVI.77.8.4911-4927.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zajac AJ, et al. Viral immune evasion due to persistence of activated T cells without effector function. J Exp Med. 1998;188(12):2205–2213. doi: 10.1084/jem.188.12.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oehen S, Brduscha-Riem K, Oxenius A, Odermatt B. A simple method for evaluating the rejection of grafted spleen cells by flow cytometry and tracing adoptively transferred cells by light microscopy. J Immunol Methods. 1997;207(1):33–42. doi: 10.1016/S0022-1759(97)00089-6. [DOI] [PubMed] [Google Scholar]
- 19.Moskophidis D, Lechner F, Pircher H, Zinkernagel RM. Virus persistence in acutely infected immunocompetent mice by exhaustion of antiviral cytotoxic effector T cells. Nature. 1993;362(6422):758–761. doi: 10.1038/362758a0. [DOI] [PubMed] [Google Scholar]
- 20.Yang H, Yogeeswaran G, Bukowski JF, Welsh RM. Expression of asialo GM1 and other antigens and glycolipids on natural killer cells and spleen leukocytes in virus-infected mice. Nat Immun Cell Growth Regul. 1985;4(1):21–39. [PubMed] [Google Scholar]
- 21.Jones AT, et al. Characterization of the activation-associated isoform of CD43 on murine T lymphocytes. J Immunol. 1994;153(8):3426–3439. [PubMed] [Google Scholar]
- 22.Lin Y, Roberts TJ, Sriram V, Cho S, Brutkiewicz RR. Myeloid marker expression on antiviral CD8+ T cells following an acute virus infection. Eur J Immunol. 2003;33(10):2736–2743. doi: 10.1002/eji.200324087. [DOI] [PubMed] [Google Scholar]
- 23.Taniguchi RT, Guzior D, Kumar V. 2B4 inhibits NK-cell fratricide. Blood. 2007;110(6):2020–2023. doi: 10.1182/blood-2007-02-076927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gonzalez-Cabrero J, Wise CJ, Latchman Y, Freeman GJ, Sharpe AH, Reiser H. CD48-deficient mice have a pronounced defect in CD4(+) T cell activation. Proc Natl Acad Sci U S A. 1999;96(3):1019–1023. doi: 10.1073/pnas.96.3.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barber DL, et al. Restoring function in exhausted CD8 T cells during chronic viral infection. Nature. 2006;439(7077):682–687. doi: 10.1038/nature04444. [DOI] [PubMed] [Google Scholar]
- 26.Day CL, et al. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature. 2006;443(7109):350–354. doi: 10.1038/nature05115. [DOI] [PubMed] [Google Scholar]
- 27.Urbani S, et al. PD-1 expression in acute hepatitis C virus (HCV) infection is associated with HCV-specific CD8 exhaustion. J Virol. 2006;80(22):11398–11403. doi: 10.1128/JVI.01177-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boni C, et al. Characterization of hepatitis B virus (HBV)-specific T-cell dysfunction in chronic HBV infection. J Virol. 2007;81(8):4215–4225. doi: 10.1128/JVI.02844-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ha SJ, et al. Enhancing therapeutic vaccination by blocking PD-1-mediated inhibitory signals during chronic infection. J Exp Med. 2008;205(3):543–555. doi: 10.1084/jem.20071949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakamoto N, et al. Functional restoration of HCV-specific CD8 T cells by PD-1 blockade is defined by PD-1 expression and compartmentalization. Gastroenterology. 2008;134(7):1927–1937, 1937e1–e2. doi: 10.1053/j.gastro.2008.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Velu V, et al. Enhancing SIV-specific immunity in vivo by PD-1 blockade. Nature. 2009;458(7235):206–210. doi: 10.1038/nature07662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andrews DM, Scalzo AA, Yokoyama WM, Smyth MJ, gli-Esposti MA. Functional interactions between dendritic cells and NK cells during viral infection. Nat Immunol. 2003;4(2):175–181. doi: 10.1038/ni880. [DOI] [PubMed] [Google Scholar]
- 33.Andoniou CE, et al. Interaction between conventional dendritic cells and natural killer cells is integral to the activation of effective antiviral immunity. Nat Immunol. 2005;6(10):1011–1019. doi: 10.1038/ni1244. [DOI] [PubMed] [Google Scholar]
- 34.Robbins SH, et al. Natural killer cells promote early CD8 T cell responses against cytomegalovirus. PLoS Pathog. 2007;3(8):e123. doi: 10.1371/journal.ppat.0030123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bukowski JF, Warner JF, Dennert G, Welsh RM. Adoptive transfer studies demonstrating the antiviral effect of natural killer cells in vivo. J Exp Med. 1985;161(1):40–52. doi: 10.1084/jem.161.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bukowski JF, Woda BA, Habu S, Okumura K, Welsh RM. Natural killer cell depletion enhances virus synthesis and virus-induced hepatitis in vivo. J Immunol. 1983;131(3):1531–1538. [PubMed] [Google Scholar]
- 37.Bukowski JF, Woda BA, Welsh RM. Pathogenesis of murine cytomegalovirus infection in natural killer cell-depleted mice. J Virol. 1984;52(1):119–128. doi: 10.1128/jvi.52.1.119-128.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tay CH, Szomolanyi-Tsuda E, Welsh RM. Control of infections by NK cells. Curr Top Microbiol Immunol. 1998;230:193–220. doi: 10.1007/978-3-642-46859-9_12. [DOI] [PubMed] [Google Scholar]
- 39.Biron CA, Nguyen KB, Pien GC, Cousens LP, Salazar-Mather TP. Natural killer cells in antiviral defense: function and regulation by innate cytokines. Annu Rev Immunol. 1999;17:189–220. doi: 10.1146/annurev.immunol.17.1.189. [DOI] [PubMed] [Google Scholar]
- 40.Masopust D, Murali-Krishna K, Ahmed R. Quantitating the magnitude of the lymphocytic choriomeningitis virus-specific CD8 T-cell response: it is even bigger than we thought. J Virol. 2007;81(4):2002–2011. doi: 10.1128/JVI.01459-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lau LL, Jamieson BD, Somasundaram T, Ahmed R. Cytotoxic T-cell memory without antigen. Nature. 1994;369(6482):648–652. doi: 10.1038/369648a0. [DOI] [PubMed] [Google Scholar]
- 42.Karre K. NK cells, MHC class I molecules and the missing self. Scand J Immunol. 2002;55(3):221–228. doi: 10.1046/j.1365-3083.2002.01053.x. [DOI] [PubMed] [Google Scholar]
- 43.de Boer RJ, Homann D, Perelson AS. Different dynamics of CD4+ and CD8+ T cell responses during and after acute lymphocytic choriomeningitis virus infection. J Immunol. 2003;171(8):3928–3935. doi: 10.4049/jimmunol.171.8.3928. [DOI] [PubMed] [Google Scholar]
- 44.Whitmire JK, Benning N, Whitton JL. Precursor frequency, nonlinear proliferation, and functional maturation of virus-specific CD4+ T cells. J Immunol. 2006;176(5):3028–3036. doi: 10.4049/jimmunol.176.5.3028. [DOI] [PubMed] [Google Scholar]
- 45.Rabinovich BA, et al. Activated, but not resting, T cells can be recognized and killed by syngeneic NK cells. J Immunol. 2003;170(7):3572–3576. doi: 10.4049/jimmunol.170.7.3572. [DOI] [PubMed] [Google Scholar]
- 46.Tangye SG, Lazetic S, Woollatt E, Sutherland GR, Lanier LL, Phillips JH. Cutting edge: human 2B4, an activating NK cell receptor, recruits the protein tyrosine phosphatase SHP-2 and the adaptor signaling protein SAP. J Immunol. 1999;162(12):6981–6985. [PubMed] [Google Scholar]
- 47.Sayos J, et al. The X-linked lymphoproliferative-disease gene product SAP regulates signals induced through the co-receptor SLAM. Nature. 1998;395(6701):462–469. doi: 10.1038/26683. [DOI] [PubMed] [Google Scholar]
- 48.Engel P, Eck MJ, Terhorst C. The SAP and SLAM families in immune responses and X-linked lymphoproliferative disease. Nat Rev Immunol. 2003;3(10):813–821. doi: 10.1038/nri1202. [DOI] [PubMed] [Google Scholar]
- 49.Morra M, et al. X-linked lymphoproliferative disease: a progressive immunodeficiency. Annu Rev Immunol. 2001;19:657–682. doi: 10.1146/annurev.immunol.19.1.657. [DOI] [PubMed] [Google Scholar]
- 50.Crotty S, McCausland MM, Aubert RD, Wherry EJ, Ahmed R. Hypogammaglobulinemia and exacerbated CD8 T-cell-mediated immunopathology in SAP-deficient mice with chronic LCMV infection mimics human XLP disease. Blood. 2006;108(9):3085–3093. doi: 10.1182/blood-2006-04-018929. [DOI] [PubMed] [Google Scholar]
- 51.Yin L, et al. Mice deficient in the X-linked lymphoproliferative disease gene sap exhibit increased susceptibility to murine gammaherpesvirus-68 and hypo-gammaglobulinemia. J Med Virol. 2003;71(3):446–455. doi: 10.1002/jmv.10504. [DOI] [PubMed] [Google Scholar]
- 52.Chlewicki LK, Velikovsky CA, Balakrishnan V, Mariuzza RA, Kumar V. Molecular basis of the dual functions of 2B4 (CD244). J Immunol. 2008;180(12):8159–8167. doi: 10.4049/jimmunol.180.12.8159. [DOI] [PubMed] [Google Scholar]
- 53.Suzuki A, et al. Functional SNPs in CD244 increase the risk of rheumatoid arthritis in a Japanese population. Nat Genet. 2008;40(10):1224–1229. doi: 10.1038/ng.205. [DOI] [PubMed] [Google Scholar]
- 54.Mellors JW, et al. Plasma viral load and CD4+ lymphocytes as prognostic markers of HIV-1 infection. Ann Intern Med. 1997;126(12):946–954. doi: 10.7326/0003-4819-126-12-199706150-00003. [DOI] [PubMed] [Google Scholar]
- 55.Welsh RM, Jr, Lampert PW, Burner PA, Oldstone MB. Antibody-complement interactions with purified lymphocytic choriomeningitis virus. Virology. 1976;73(1):59–71. doi: 10.1016/0042-6822(76)90060-X. [DOI] [PubMed] [Google Scholar]
- 56.Yang HY, Dundon PL, Nahill SR, Welsh RM. Virus-induced polyclonal cytotoxic T lymphocyte stimulation. J Immunol. 1989;142(5):1710–1718. [PubMed] [Google Scholar]
- 57.Oxenius A, Bachmann MF, Ashton-Rickardt PG, Tonegawa S, Zinkernagel RM, Hengartner H. Presentation of endogenous viral proteins in association with major histocompatibility complex class II: on the role of intracellular compartmentalization, invariant chain and the TAP transporter system. Eur J Immunol. 1995;25(12):3402–3411. doi: 10.1002/eji.1830251230. [DOI] [PubMed] [Google Scholar]
- 58.van der Most RG, et al. Identification of Db- and Kb-restricted subdominant cytotoxic T-cell responses in lymphocytic choriomeningitis virus-infected mice. Virology. 1998;240(1):158–167. doi: 10.1006/viro.1997.8934. [DOI] [PubMed] [Google Scholar]
- 59.Mylin LM, et al. Quantitation of CD8(+) T-lymphocyte responses to multiple epitopes from simian virus 40 (SV40) large T antigen in C57BL/6 mice immunized with SV40, SV40 T-antigen-transformed cells, or vaccinia virus recombinants expressing full-length T antigen or epitope minigenes. J Virol. 2000;74(15):6922–6934. doi: 10.1128/JVI.74.15.6922-6934.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Assarsson E, et al. NK cells stimulate proliferation of T and NK cells through 2B4/CD48 interactions. J Immunol. 2004;173(1):174–180. doi: 10.4049/jimmunol.173.1.174. [DOI] [PubMed] [Google Scholar]
- 61.Chen HD, Fraire AE, Joris I, Welsh RM, Selin LK. Specific history of heterologous virus infections determines anti-viral immunity and immunopathology in the lung. Am J Pathol. 2003;163(4):1341–1355. doi: 10.1016/S0002-9440(10)63493-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Daniels KA, Devora G, Lai WC, O’Donnell CL, Bennett M, Welsh RM. Murine cytomegalovirus is regulated by a discrete subset of natural killer cells reactive with monoclonal antibody to Ly49H. J Exp Med. 2001;194(1):29–44. doi: 10.1084/jem.194.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.