Abstract
Aims
Individuals with both diabetes mellitus (DM) and the Haptoglobin (Hp) 2-2 genotype are at increased risk of cardiovascular disease. As the antioxidant function of the Hp 2-2 protein is impaired, we sought to test the pharmacogenomic hypothesis that antioxidant vitamin E supplementation would provide cardiovascular protection to Hp 2-2 DM individuals.
Materials & methods
We determined the Hp genotype on DM participants from two trials (HOPE and ICARE) and assessed the effect of vitamin E by Hp genotype on their common prespecified outcome, the composite of stroke, myocardial infarction and cardiovascular death. Data was analyzed with a fixed-effect model. These results were input into a simulation model, the Evidence Based Medicine Integrator, in order to estimate their long-term implications in a real-world population from Kaiser Permanente (CA, USA).
Results
Meta-analysis of the two trials demonstrated a significant overall reduction in the composite end point in Hp 2-2 DM individuals with vitamin E (odds ratio: 0.58; 95% CI: 0.40–0.86; p = 0.006). There was a statistically significant interaction between the Hp genotype and vitamin E on the composite end point. In these trials, Hp typing of 69 DM individuals and treating those with the Hp 2-2 with vitamin E prevented one myocardial infarct, stroke or cardiovascular death. Lifelong administration of vitamin E to Hp 2-2 DM individuals in the Kaiser population would increase their life expectancy by 3 years.
Conclusion
A pharmacogenomic strategy of screening DM individuals for the Hp genotype and treating those with Hp 2-2 with vitamin E appears to be highly clinically effective.
Keywords: antioxidants, cardiovascular disease, diabetes mellitus, haptoglobin, hemoglobin, pharmacogenomics, vitamin E
Cardiovascular disease (CVD) is the leading cause of death in individuals with diabetes mellitus (DM) [1]. The oxidative modification hypothesis of atherosclerosis would suggest that the increased burden of CVD in individuals with DM is the result of an increased production of reactive oxygen species that produce structural changes in lipoproteins that markedly increase their atherogenic potential [2]. While preclinical and observational studies at one time motivated more than 40% of all cardiologists to prescribe the antioxidant vitamin E, particularly in DM [3], clinical trials have demonstrated that vitamin E supplementation does not provide any measure of cardiovascular protection in genetically unselected populations with DM [4–11].
However, a total rejection of the oxidation modification hypothesis may be premature. Benefit from high-dose antioxidant therapy may only be demonstrable when delivered to a population that suffers from particularly high levels of oxidative stress owing to, for example, a dysfunctional allelic polymorphism (mutation) in a gene encoding an antioxidant protein. One such polymorphism may exist at the haptoglobin (Hp) genetic locus [12]. The primary function of Hp is to prevent extracorpuscular hemoglobin (Hb) from mediating oxidative injury. There exist two classes of alleles at the Hp locus, 1 and 2, defined by the presence or absence of intragenic duplication [12]. The Hp 1 allele has five exons and is remarkably conserved over the animal kingdom (the exonic structure of the Hp 1 allele is entirely conserved and there is over 90% homology at the amino acid level between murine and human Hp 1). The Hp 2 allele is present only in man and is believed to have originated from the Hp 1 allele by an inframe duplication of exons 3 and 4 of the Hp 1 allele approximately 100,000 years ago, early in human evolution. The importance of SNPs in this genomic region and whether or not they are in linkage disequilibrium (LD) with the absence or presence of the intragenic duplication giving rise to the Hp 1 or Hp 2 alleles is not known. As a result of the duplication event the biophysical properties of the Hp 1 and Hp 2 alleles are remarkably different [12]. Specifically, the Hp 2 protein provides inferior antioxidant protection against Hb compared with the Hp 1 protein [13,14]. Hp polymorphism is common, with the prevalence of Hp genotypes in Western populations being 16% Hp 1-1, 36% Hp 2-2 and 48% Hp 2-1 [12]. We and others have demonstrated in five longitudinal studies that Hp 2-2 DM individuals have a markedly increased risk of incident CVD as compared with non-Hp 2-2 DM individuals [15–19]. In the present study we sought to directly test the pharmacogenomic hypothesis that the antioxidant vitamin E selectively provides cardiovascular protection to Hp 2-2 DM individuals.
Materials & methods
Clinical trials examined & analysis of blood specimens
We assessed the relationship between Hp type, vitamin E supplementation and cardiovascular end points in DM participants from two clinical trials that investigated the role of vitamin E on cardiovascular end points – the Heart Outcomes Prevention Evaluation (HOPE) [4], and the Israel Cardiovascular Events Reduction with Vitamin E (ICARE) trial [18]. All of the participants from ICARE were included in this study. In ICARE only the Hp 2-2 participants (n = 1434) were randomized to vitamin E or placebo; Hp 1-1 and Hp 2-1 participants were followed concurrently for the prespecified study end points. For HOPE, a Hp type was obtained for 1078 DM HOPE participants (all of whom had been randomized to vitamin E or placebo) representing approximately 30% of the HOPE DM cohort. The HOPE DM participants who were used in this study were all those for whom serum had been stored at the initiation of the HOPE study (Canadian cohort only). Hp type was determined from serum by gel electrophoresis, which provides a signature banding pattern for each of the three Hp types (1-1, 2-1 or 2-2) [12]. We previously demonstrated a 100% correspondence between Hp genotype determined by gel electrophoresis and PCR [20].
Meta-analysis investigating the predictive value of Hp typing on CVD risk & the interaction between Hp type & vitamin E on CVD events
We combined data from the HOPE and ICARE studies. Both HOPE and ICARE used the same predefined clinical end points of nonfatal myocardial infarction (MI), stroke and CVD death and the composite of these events. Both trials and analyses were conducted according to the intention-to-treat principle. The studies did not differ with regard to type or dosage of vitamin E used (natural source 400 IU per day), type of DM (Type 2), or age of participants at enrollment (aged over 55 years). A third of the participants in HOPE and a half of the participants in ICARE were women. A prior history of MI existed in 14% of ICARE participants and 35% of HOPE participants. The prevalence of CVD in the ICARE study cohort at baseline was approximately 25% and in the HOPE cohort was approximately 65%.
Body fat and physical activity were not measured in HOPE or ICARE. Published data from ICARE has shown that there were no differences in any demographic variable by Hp type or treatment allocation [18]. Moreover, adjusted Cox regression models of the ICARE data have shown that none of the measured demographic variables had any effect on the study results [18]. Therefore, a randomization-based analysis of ICARE is justified. We did not have access to baseline demographic data segregated by vitamin E status and Hp genotype from the HOPE participants used in this analysis. Furthermore, while incidence rate (as well as cumulative incidence as used in this analysis) was available from ICARE data, only the cumulative incidence of major cardiovascular events was available from HOPE.
The primary end point used in this analysis was the same as that used in HOPE and ICARE, neither of which corrected for multiple comparisons. Moreover, we have not queried the interaction between vitamin E and multiple SNPs in searching for one that yielded a significant interaction. Our a priori hypothesis and the only polymorphism that we assessed in our analysis was the Hp polymorphism defined by the duplication of exons 3 and 4.
Heterogeneity between the studies was assessed using the formal χ2 test, with a p-value of less than 0.10 considered statistically significant. We analyzed the data with a fixed-effect model. I2 provides the percentage of the variability in effect estimates between subgroups that is due to heterogeneity between the subgroups rather than due to sampling error (chance). In general a high I2 reflects higher heterogeneity between studies. Dichotomous data (events per population) were analyzed with Mantel–Haenszel methods in order to calculate the odds ratio with a 95% CI. In order to normalize for differences in duration of the studies (1.5 years for ICARE and 4.5 years for HOPE), data were also adjusted for years of patient treatment with results reported as the number of events per 1000 patient-years. Mean differences between groups in numbers of events per 1000 patient-years were calculated using the Inverse Variance method. We performed these analyses using Review Manager (RevMan) Version 5.0 (Nordic Cochrane Centre, Copenhagen, Denmark, Cochrane Collaboration, 2008).
Simulation of long-term effects of vitamin E in Hp 2-2 DM
Long-term extrapolation of meta-analytic findings was carried out using version 7.0.1 of the Evidence-Based Medicine Integrator, an opensource discrete-event person-level simulator of DM and its treatment, as more fully described in ONLINE APPENDIX A (www.futuremedicine.com/doi/suppl/10.2217/pgs.10.17/suppl_file/Online_Appendix_A.doc). Evidence-Based Medicine Integrator combines interacting event-risk equations estimated from data describing the population to which the model is applied, with estimates of treatment effects taken directly from systematic reviews and randomized trial results. Version 7.0.1 is optimized to predict clinical events and medical expenditures in the membership of the Kaiser Permanente (CA, USA) Northwest region (KPNW) health system. Subjects for the simulation were all 8632 KPNW members on 1 January 2005 and aged 55 years or over with Type 2 DM and sufficient historical data. Model simulated individuals (simulands) could experience up to 25 kinds of microvascular and macrovascular adverse events, procedures and death over a period of 50 years of in silico follow-up. To minimize stochastic variation, ten lives were simulated for each subject. Subjects were simulated to receive standard DM related and other medical care, which in KPNW is evidence driven and includes aggressive use of aspirin, statins and blood pressure medications, as well as blood glucose control. We set up the model to assume the same effects of vitamin E and Hp genotype as those that emerged from the meta-analysis. We assumed that 65% of simulated death was caused by CVD.
Results
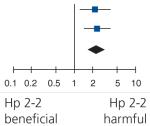
Risk of CVD death, MI & stroke is increased in Hp 2-2 DM
In a meta-analysis of the participants of ICARE who did not receive vitamin E with the participants of HOPE who did not receive either vitamin E or ramipril (double placebo group) the composite end point was significantly increased in Hp 2-2 DM as compared with non-Hp 2-2 DM (odds ratio [OR]: 2.29; 95% CI: 1.57–3.34; p < 0.0001) (Table 1). Analysis of the components of the composite end point showed that the incidence of CVD death (OR: 3.52; 95% CI: 1.72–7.20; p = 0.0006) and MI (OR: 1.95; 95% CI: 1.23–3.10; p = 0.004) were significantly increased in Hp 2-2 DM study participants, with a trend towards an increased incidence of stroke in Hp 2-2 DM (OR: 1.79; 95% CI: 0.96–3.31; p = 0.07).
Table 1. Hp 2-2 diabetes mellitus individuals are at higher risk of cardiovascular disease.
| Study | Hp 2-2 |
Non-Hp 2-2 |
Weight (%) | Odds ratio (M–H, fixed effect, 95% CI) | |||
|---|---|---|---|---|---|---|---|
| Events | Total | Events | Total | ||||
| HOPE | 29 | 91 | 33 | 187 | 44.1 | 2.18 (1.22–3.90) |
|
| ICARE | 33 | 708 | 31 | 1533 | 55.9 | 2.37 (1.44–3.90) | |
| Total (95% CI) | 799 | 1720 | 100 | 2.29 (1.57–3.34) | |||
| Total events | 62 | 64 | |||||
Comparison of the composite end point of stroke, nonfatal myocardial infarction and cardiovascular disease death in Hp 2-2 diabetes mellitus and non-Hp 2-2 diabetes mellitus individuals who did not receive vitamin E in ICARE and who received neither ramipril nor vitamin E in HOPE. There was no significant heterogeneity between trials in this composite end point. The overall harmful effect of Hp 2-2 on the composite end point was statistically significant, odds ratio: 2.29; 95% CI: 1.57–3.34; p < 0.0001.
HOPE: Heart Outcomes Prevention Evaluation; Hp: Haptoglobin; ICARE: Israel Cardiovascular Events Reduction with Vitamin E; M-H: Mantel–Haenszel.
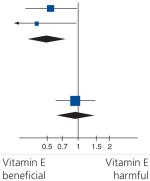
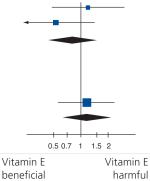
Vitamin E reduces CVD death, MI & stroke in Hp 2-2 DM
Meta-analysis of the 1833 HOPE and ICARE Hp 2-2 DM study participants randomized to vitamin E or placebo demonstrated a significant overall reduction in the composite end point in Hp 2-2 DM individuals who received vitamin E (OR: 0.58; 95% CI: 0.40–0.86; p = 0.006) (Table 2). In the 679 non-Hp 2-2 DM HOPE participants randomized to vitamin E or placebo there was no significant benefit with vitamin E (OR: 1.02; 95% CI: 0.69–1.50; p = 0.93). There was a statistically significant interaction (p = 0.05) between Hp type (yes or no Hp 2-2) and vitamin E on the composite end point. As derived in ONLINE APPENDIX B (www.futuremedicine.com/doi/suppl/10.2217/pgs.10.17/suppl_file/Online_Appendix_B.doc), the results from the meta-analysis indicate that only 31 Hp 2-2 DM individuals would need to be treated with vitamin E in order to prevent one MI, stroke or CVD death. As the prevalence of the Hp 2-2 genotype in this pooled analysis was 45%, this implies that only 69 DM individuals would need to be Hp typed (and those with Hp 2-2 treated with vitamin E) in order to prevent one MI, stroke or CVD death.
Table 2. Vitamin E reduces the risk of the composite outcome in Hp 2-2 diabetes mellitus individuals.
| Study | Vitamin E |
Placebo |
Weight (%) |
Odds ratio (IV, fixed effect, 95% CI) | |||
|---|---|---|---|---|---|---|---|
| Events | Total | Events | Total | ||||
| Hp 2-2 | |||||||
| HOPE | 37 | 222 | 40 | 177 | 59.6 | 0.69 (0.42–1.13) |

|
| ICARE | 16 | 726 | 33 | 708 | 40.4 | 0.46 (0.25–0.85) | |
| Subtotal (95% CI) | 948 | 885 | 100 | 0.58 (0.40–0.86) | |||
| Total events | 53 | 73 | |||||
| Non-Hp 2-2 | |||||||
| HOPE | 60 | 326 | 64 | 353 | 100 | 1.02 (0.69–1.50) | |
| Subtotal (95% CI) | 326 | 353 | 100 | 1.02 (0.69–1.50) | |||
| Total events | 60 | 64 | |||||
Meta-analysis of the composite outcome of stroke, nonfatal myocardial infarction and cardiovascular death in HOPE and ICARE stratified by Hp type. There was significant benefit from vitamin E in Hp 2-2 individuals, odds ratio: 0.58; 95% CI: 0.40–0.86; p = 0.006. There was a statistically significant interaction between Hp 2-2 and non-Hp 2-2 individuals on the composite end point (p = 0.05).
Test for subgroup differences: χ2 = 3.97, degrees of freedom = 1 (p = 0.05), I2 = 74.8%.
HOPE: Heart Outcomes Prevention Evaluation; Hp: Haptoglobin; ICARE: Israel Cardiovascular Events Reduction with vitamin E; IV: Inverse variance.
Normalization of the studies for events per 1000 patient-years was also performed to take into account differences in the duration of the trials (Table 3). In this normalized analysis vitamin E was associated with a significant reduction in the number of CVD events in Hp 2-2 (reduction of 15.98; 95% CI: 15.52–16.45; events per 1000 patient-years [p < 0.0001]).
Table 3. Mean difference in the number of cardiovascular events per 1000 patient-years.
| Study | Vitamin E |
Placebo |
Weight (%) |
Odds ratio (IV, fixed effect, 95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Total | Mean | SD | Total | ||||
| Hp 2-2 | |||||||||
| HOPE | 37.03 | 6.08 | 222 | 50.21 | 7.08 | 177 | 12.5 | −13.18 (−14.49– −11.87) |

|
| ICARE | 14.69 | 3.83 | 726 | 31.07 | 5.57 | 708 | 87.5 | −16.38 (−16.88– −15.88) | |
| Subtotal (95% CI) |
948 | 885 | 100 | −15.98 (−16.45– −15.52) | |||||
| Non-Hp 2-2 | |||||||||
| HOPE | 40.89 | 6.39 | 326 | 40.28 | 6.34 | 353 | 100 | 0.61 (−0.35–1.57) | |
| Subtotal (95% CI) |
326 | 353 | 100 | 0.61 (−0.35–1.57) | |||||
| Total events | |||||||||
The number of composite cardiovascular events in each study was adjusted for years of patient exposure to vitamin E (1.5 years in ICARE and 4.5 years in HOPE).
Vitamin E was favorably associated with a significant reduction in the number of cardiovascular disease events in Hp 2-2 individuals (overall reduction of 15.98; 95% CI: 15.52–16.45; events per 1000 patient-years [p < 0.001]).
Test for subgroup differences: χ2 = 932.58, degrees of freedom = 1 (p < 0.00001), I2 = 99.9%.
HOPE: Heart Outcomes Prevention Evaluation; Hp: Haptoglobin; ICARE: Israel Cardiovascular Events Reduction with vitamin E; IV: Inverse variance.
Meta-analysis of individual components of the composite end point demonstrated that vitamin E had a significant benefit in Hp 2-2 individuals in reducing MI (OR: 0.49; 95% CI: 0.30–0.80; p = 0.004) and CVD death (OR: 0.46; 95% CI: 0.24–0.88; p = 0.02) with a trend towards benefit on stroke (OR: 0.82; 95% CI: 0.42–1.59; p = 0.56) (Tables 4–6). In all these analyses no significant heterogeneity between trials was observed.
Table 4. Individual end points of the composite outcome in Hp 2-2 and non-Hp 2-2 diabetes mellitus individuals randomized to vitamin E or placebo in the three trials: nonfatal myocardial infarction.
| Study | Vitamin E |
Placebo |
Weight (%) |
Odds ratio (IV, fixed effect, 95% CI) | |||
|---|---|---|---|---|---|---|---|
| Events | Total | Events | Total | ||||
| Hp 2-2 | |||||||
| HOPE | 23 | 222 | 31 | 177 | 64.5 | 0.54 (0.30–0.97) |
|
| ICARE | 7 | 726 | 17 | 708 | 35.5 | 0.40 (0.16–0.96) | |
| Subtotal (95% CI) |
948 | 885 | 100 | 0.49 (0.30–0.80) | |||
| Total events | 30 | 48 | |||||
| Non-Hp 2-2 | |||||||
| HOPE | 42 | 326 | 48 | 353 | 100 | 0.94 (0.60–1.47) | |
| Subtotal (95% CI) |
326 | 353 | 100 | 0.94 (0.60–1.47) | |||
| Total events | 42 | 48 | |||||
There was a significant reduction in myocardial infarction in Hp 2-2 individuals with vitamin E, odds ratio: 0.49; 95% CI: 0.30–0.80; p = 0.004. There was no benefit of vitamin E on myocardial infarction in non-Hp 2-2 individuals, odds ratio: 0.94; 95% CI: 0.60–1.47; p = 0.78.
HOPE: Heart Outcomes Prevention Evaluation; Hp: Haptoglobin; ICARE: Israel Cardiovascular Events Reduction with vitamin E; IV: Inverse variance.
Table 6. Individual end points of the composite outcome in Hp 2-2 and non-Hp 2-2 diabetes mellitus individuals randomized to vitamin E or placebo in the three trials: cardiovascular death.
| Study | Vitamin E |
Placebo |
Weight (%) |
Odds ratio (IV, fixed effect, 95% CI) | |||
|---|---|---|---|---|---|---|---|
| Events | Total | Events | Total | ||||
| Hp 2-2 | |||||||
| HOPE | 13 | 222 | 22 | 177 | 82.1 | 0.44 (0.21–0.90) |

|
| ICARE | 3 | 726 | 5 | 708 | 17.9 | 0.58 (0.14–2.45) | |
| Subtotal (95% CI) | 948 | 885 | 100 | 0.46 (0.24–0.88) | |||
| Total events | 16 | 27 | |||||
| Non-Hp 2-2 | |||||||
| HOPE | 23 | 326 | 28 | 353 | 100 | 0.88 (0.50–1.56) | |
| Subtotal (95% CI) | 326 | 353 | 100 | 0.88 (0.50–1.56) | |||
| Total events | 23 | 28 | |||||
There was a significant reduction in cardiovascular death in Hp 2-2 individuals with vitamin E, odds ratio: 0.46; 95% CI: 0.24–0.88; p = 0.02. There was no benefit of vitamin E on cardiovascular death in non-Hp 2-2 individuals, odds ratio: 0.88; 95% CI: 0.56–1.56; p = 0.67.
HOPE: Heart Outcomes Prevention Evaluation; Hp: Haptoglobin; ICARE: Israel Cardiovascular Events Reduction with vitamin E; IV: Inverse variance.
Incidence of MI increased 4.5-fold in Hp 2-2 DM ICARE participants after vitamin E discontinuation
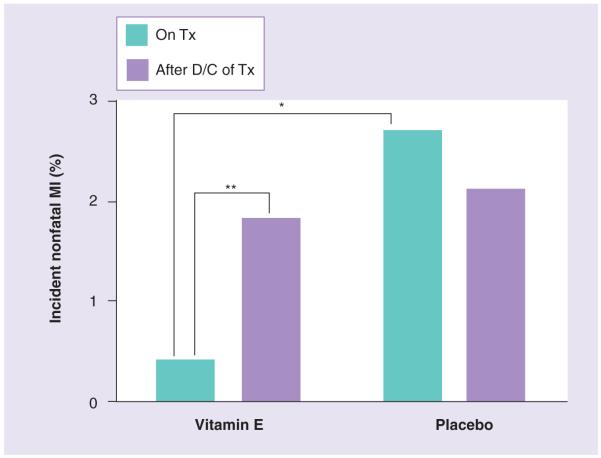
At the conclusion of the treatment phase of ICARE the study drug (placebo or vitamin E) was terminated but surveillance for CVD events was continued for an additional 18 months (clinicaltrials.gov NCT00448487) as described in ONLINE APPENDIX B (www.futuremedicine.com/doi/suppl/10.2217/pgs.10.17/suppl_file/Online_Appendix_B.doc). For individuals who had been previously treated with vitamin E the rate of MI was 4.5-fold higher in the post-treatment phase (0.4% on vitamin E vs 1.8% after discontinuation of vitamin E, p = 0.03) (Figure 1). There was no change in the rate of MI in individuals who had been treated with placebo after the placebo was discontinued (2.7% on placebo vs 2.1% after placebo discontinuation, p = 0.55).
Figure 1. Discontinuation of vitamin E was associated with a 4.5-fold increase in the incidence of myocardial infarction in Hp 2-2 diabetes mellitus individuals in ICARE.
In the Tx phase of Israel Cardiovascular Events Reduction with Vitamin E (ICARE), Hp 2-2 diabetes mellitus (DM) individuals who received vitamin E had a significantly lower rate of MI as compared with Hp 2-2 DM individuals who received placebo (* denotes comparison by: 2.7% on placebo vs 0.4% on vitamin E, p = 0.003). At the conclusion of the ICARE study the study drug (placebo or vitamin E) was D/C in all Hp 2-2 DM individuals, but surveillance of all participants for cardiovascular disease events was continued for an additional 18 months. The rate of MI was 4.5-fold higher in the post-treatment phase for those individuals who had been previously treated with vitamin E (** denotes comparison by: 0.4% on vitamin E vs 1.8% after discontinuation of vitamin E, p = 0.03). There was no change in the rate of MI in individuals who had been treated with placebo after the placebo was discontinued (2.7% on placebo vs 2.1% after discontinuation of placebo; p = 0.55).
D/C: Discontinued; MI: Myocardial infarction; Tx: treatment.
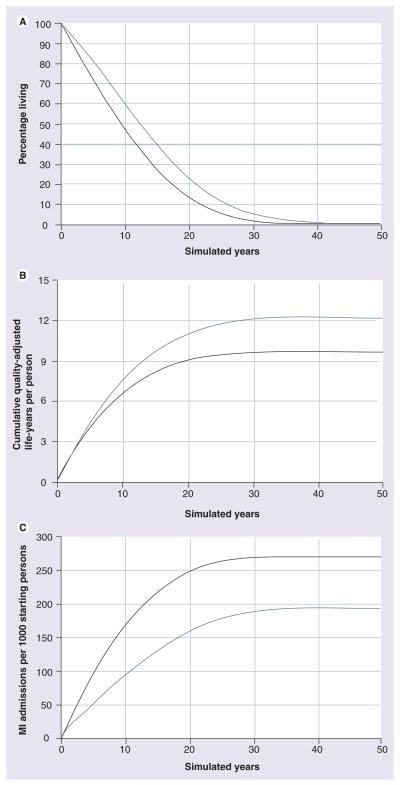
Simulated lifetime treatment of Hp 2-2 DM with vitamin E
Simulation of these meta-analytic results over 50 years in the KPNW population demonstrated that Hp typing all DM individuals and then only treating Hp 2-2 DM individuals with vitamin E would add 1.09 years/person and 0.89 qualityadjusted life-years/person in the population as a whole, and 3.04 life-years and 2.49 quality-adjusted life-years in Hp 2-2 DM individuals (Figure 2a & 2b). Per 1000 Hp 2-2 DM individuals, treatment would prevent 75 MI admissions (Figure 2C), 31 cardiac surgical procedures and 19 percutaneous coronary interventions; and in the total population screened for Hp 2-2, 27 MI admissions, 11 cardiac surgical procedures, and seven percutaneous coronary interventions per 1000 persons. For details and sensitivity analyses see ONLINE APPENDIX A (www.futuremedicine.com/doi/suppl/10.2217/pgs.10.17/suppl_file/Online_Appendix_A.doc).
Figure 2. Simulation of the long-term effects of Hp typing all diabetes mellitus individuals and providing vitamin E to those with the Hp 2-2 genotype in Kaiser Permanente (CA, USA) Northwest region.
All subjects were simulated for 50 years of treatment or until death. 50-year simulation results are shown for Hp 2-2 individuals only. Results when treated with vitamin E are shown in black and results when not treated with vitamin E are shown in gray. For survival (A) the incremental benefit of vitamin E therapy was ascertained by determining the area between the two survival curves. For cumulative qualityadjusted life-years (QALYs) per person (B) and for cumulative MI admissions per 1000 starting persons (C), differences between policies are summarized by the differences in the values at year 50. (A) Percentage survival. The cumulative gain in life expectancy in Hp 2-2 individuals treated with vitamin E was 3.04 years (gray) as compared with Hp 2-2 individuals who were not treated with vitamin E (black). (B) Cumulative QALYs. Total QALYs were increased 2.49 years in Hp 2-2 individuals treated with vitamin E (gray) as compared with Hp 2-2 individuals who were not treated with vitamin E (black). (C) Cumulative hospital admissions for MI. For every 1000 Hp 2-2 diabetes mellitus individuals treated with vitamin E, for up to 50 years, 75 hospital admissions for MI would be prevented (gray) as compared with not treating with vitamin E (black).
MI: Myocardial infarction.
Discussion
This study provides strong evidence that vitamin E provides significant clinical benefit to DM individuals with the Hp 2-2 genotype. In metaanalysis of two independent placebo controlled clinical trials Hp 2-2 DM individuals (representing approximately 36% of all DM individuals) derived significant cardiovascular protection from vitamin E supplementation, with an overall reduction of over 40% in the combined end point of stroke, MI and CVD death. Simulation of the meta-analytic results over 50 years in a nonresearch population predicted an exceptionally large improvement in life expectancy that would be achieved by treating Hp 2-2 DM individuals with vitamin E, comparable to the benefits predicted from smoking cessation [21] and much larger than the lifetime benefits of statin therapy in very high-risk patients [22,23], and of blood pressure and glucose control in DM [24]. While recognizing the limitations of this simulation analysis, these simulation results illustrate the public health implications from a very inexpensive treatment approach using pharmacogenomics. We hope that the implications will be recognized to be of sufficient importance to justify a large prospective clinical trial to refute or confirm the current study.
Epidemiological studies have established that the Hp gene is a determinant of CVD risk in DM. Including the present analysis, six longitudinal studies assessing incident CVD in DM individuals stratified by Hp genotype have shown an increased rate of CVD in Hp 2-2 as compared with non-Hp 2-2 individuals [15–19]. This epidemiological association between Hp genotype and CVD risk is supported by transgenic studies showing dysfunctional proatherogenic high-density lipoprotein (HDL) and atherosclerotic plaque instability in Hp 2-2 mice [25,26].
Mechanistic studies have provided an explanation for the interaction between Hp genotype and DM on CVD risk. Hb is continuously released into the bloodstream as a result of the turnover of red cells. Hp rapidly binds to extracorpuscular Hb and reduces the ability of Hb to mediate oxidative injury [12]. The Hp– Hb complex is rapidly cleared from the blood by the monocyte/macrophage scavenger receptor CD163 [27]. However, the Hp–Hb complex can also bind to circulating HDL via a specific association between Hp and ApoA1 [26,28]. CD163-mediated clearance of Hp–Hb is delayed in Hp 2-2 DM, resulting in an increase in the amount of Hp–Hb associating with HDL [26,29,30]. As the Hp 2-2 protein is inferior to the Hp 1–1 protein at blocking Hb-induced oxidation [13,14], Hb tethered to the HDL of Hp 2-2 DM individuals mediates an increased oxidative modification of HDL and an impairment in HDL function [26,31]. A major factor accounting for the interaction between Hp genotype and DM is the synergy between DM and the Hp 2-2 genotype in down regulating CD163 leading to increased Hb content in HDL [26,29,30].
Interventional studies with vitamin E assessing HDL oxidation and function have provided a mechanism for the pharmacogenomic interaction between Hp type and vitamin E on CVD outcomes. In both Hp 2-2 DM humans and mice, supplementation with vitamin E rapidly reduced HDL oxidation and corrected HDL dysfunction [26]. Notably, no effect of vitamin E was found in non-Hp 2-2 DM on HDL oxidation or function [26]. The restorative effect of vitamin E on HDL oxidation and function in Hp 2-2 DM individuals was reversible with a return of HDL to its prior oxidized and dysfunctional state within two months of its discontinuation [26]. These data are consistent with the experience of Hp 2-2 DM participants of ICARE, who experienced a rapid increase in the rate of MI soon after vitamin E was discontinued.
While vitamin E provides protection to Hp 2-2 DM individuals, vitamin C appears to be harmful to this population. The Women’s Angiographic Vitamin Estrogen (WAVE) study investigated the effect of high-dose vitamin C and vitamin E on coronary artery plaque progression using serial angiography [6]. WAVE participants were Hp typed and angiographic progression was greater in Hp 2-2 DM individuals who received vitamin C and vitamin E [32]. Vitamin C and vitamin E promote or inhibit oxidative stress mediated by iron, respectively [33], which is the key oxidant in Hp 2-2 DM [34]. In vitro vitamin C promotes the reduction–oxidation cycling of iron while vitamin E does not [33]. Vitamin C increases the oxidative activity of Hp 2-2–Hb bound to HDL, thereby not only increasing HDL oxidation but also resulting in an HDL particle that is pro-oxidative, pro-inflammatory and proatherogenic [26]. Vitamin E, on the other hand, blocks Hb-mediated oxidation and prevents the oxidation of HDL by Hp 2-2–Hb. Finally, vitamin C supplementation to Hp 2-2 DM mice does not improve HDL function and blocks the ability of vitamin E to correct their HDL dysfunction [35]. Our meta-analytical results do not demonstrate that vitamin E is harmful to non-Hp 2-2 DM individuals. However, because trials of vitamin E in DM have generally shown no benefit overall, there remains the possibility that vitamin E is harmful to some individuals, while helping Hp 2-2 DM individuals. Therefore, additional pharmacogenomic outcomes studies prospectively designed to assess not only clinical efficacy but also cost–effectiveness will be needed to determine whether a pharmacogenomic strategy of typing all individuals for Hp and then giving vitamin E only to those with the Hp 2-2 genotype is superior to providing all DM individuals with vitamin E without testing for Hp type.
Conclusion
In conclusion, Hp typing represents a once in a lifetime test that identifies those DM individuals at exceptionally high risk of CVD. The Hp type may be used to more effectively focus the attention of the clinician and the utilization of healthcare resources on those DM individuals for whom more aggressive risk factor modification is most needed. The Hp genotype also appears to identify a very large subgroup of DM individuals who may receive marked clinical benefit from an extremely inexpensive therapy. We hope that the public health implications of this study will be recognized to be of sufficient importance to warrant a large prospective clinical trial that could constitute the basis for conclusive treatment guidelines.
Executive summary.
Haptoglobin genotype & diabetic cardiovascular disease
-
■
The haptoglobin (Hp) genotype is an independent determinant of susceptibility to cardiovascular disease in individuals with diabetes mellitus (DM).
-
■
Individuals with the Hp 2-2 genotype and diabetes have an increased risk of myocardial infarction (MI), cardiovascular death and stroke.
Pharmacogenomic application of the Hp genotype
-
■
Vitamin E has not been shown to provide benefit to genetically unselected populations of individuals with diabetes, and may have increased mortality.
-
■
Retrospective analysis of the Heart Outcomes Prevention Evaluation (HOPE) study demonstrated a significant reduction in cardiovascular disease (CVD) death and MI in individuals with the Hp 2-2 genotype who received vitamin E.
-
■
Israel Cardiovascular Events Reduction with vitamin E (ICARE), a prospective study in which Hp 2-2 DM individuals were randomized to vitamin E or placebo, demonstrated a significant reduction in CVD death, MI and stroke in Hp 2-2 DM individuals who received vitamin E.
-
■
Combined analysis of ICARE and HOPE demonstrates a significant interaction between the Hp genotype and vitamin E on CVD.
-
■
Extrapolation of the results of the ICARE and HOPE studies to a real-life population over 50 years demonstrates that a pharmacogenomic algorithm of administering vitamin E to Hp 2-2 DM individuals would prolong life by approximately 3 years in these individuals.
Conclusion
-
■
The Hp genotype identifies those DM individuals at exceptionally high risk of CVD.
-
■
The Hp genotype appears to identify very large subgroups of DM individuals (~a third of the DM population) who may receive great clinical benefit from an extremely inexpensive therapy.
Supplementary Material
Table 5. Individual end points of the composite outcome in Hp 2-2 and non-Hp 2-2 diabetes mellitus individuals randomized to vitamin E or placebo in the three trials: stroke.
| Study | Vitamin E |
Placebo |
Weight (%) |
Odds ratio (IV, fixed effect, 95% CI) | |||
|---|---|---|---|---|---|---|---|
| Events | Total | Events | Total | ||||
| Hp 2-2 | |||||||
| HOPE | 12 | 222 | 8 | 177 | 43.3 | 1.21 (0.48–3.02) |
|
| ICARE | 6 | 726 | 11 | 708 | 56.7 | 0.53 (0.19–1.44) | |
| Subtotal (95% CI) |
948 | 885 | 100 | 0.82 (0.42–1.59) | |||
| Total events | 18 | 19 | |||||
| Non-Hp 2-2 | |||||||
| HOPE | 16 | 326 | 15 | 353 | 100 | 1.16 (0.57–2.39) | |
| Subtotal (95% CI) |
326 | 353 | 100 | 1.16 (0.57–2.39) | |||
| Total events | 16 | 15 | |||||
There was a nonsignificant reduction in stroke in Hp 2-2 individuals with vitamin E, odds ratio: 0.82; 95% CI: 0.42–1.59; p = 0.56. There was a trend towards increased stroke with vitamin E in non-Hp 2-2 individuals, odds ratio: 1.16; 95% CI: 0.51–2.39; p = 0.68.
HOPE: Heart Outcomes Prevention Evaluation; Hp: Haptoglobin; ICARE: Israel Cardiovascular Events Reduction with vitamin E; IV: Inverse variance.
Footnotes
Financial & competing interests disclosure
This work was supported by grants from the United States–Israel Binational Science Foundation, Israel Science Foundation, Juvenile Diabetes Research Foundation, the Kennedy Leigh Charitable Trust and RO1KD085226 from the NIH to Dr Levy; grant R21HS017643-01 from the US Agency for Healthcare Research and Quality and the Kaiser Permanente Center for Health Research to Jonathan B Brown. Dr Levy has served as a consultant with Synvista Therapeutics. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
Bibliography
Papers of special note have been highlighted as:
■ of interest
■■ of considerable interest
- 1.Moreno P, Fuster V. New aspects in the pathogenesis of diabetic atherosclerosis. J. Am. Coll. Card. 2004;44:2293–2300. doi: 10.1016/j.jacc.2004.07.060. [DOI] [PubMed] [Google Scholar]
- 2.Steinberg D, Parthasarathy S, Carew TE, Khoo JC, Witztum JL. Beyond cholesterol: modifications of low-density lipoprotein that increase its atherogenicity. N. Engl. J. Med. 1989;320:915–924. doi: 10.1056/NEJM198904063201407. ■ Initial description of the oxidation modification hypothesis of atherosclerosis.
- 3.Vivekananthan DP, Penn MS, Sapp SK, Hsu A, Topol EJ. Use of antioxidant vitamins for the prevention of cardiovascular disease: meta-analysis of randomized trials. Lancet. 361:2017–2023. doi: 10.1016/S0140-6736(03)13637-9. [DOI] [PubMed] [Google Scholar]
- 4.The Heart Outcomes Prevention Evaluation (HOPE) Study Investigators Vitamin E supplementation and cardiovascular events in high risk patients. N. Engl. J. Med. 2000;342:154–160. doi: 10.1056/NEJM200001203420302. [DOI] [PubMed] [Google Scholar]
- 5.Heart Protection Study Collaborative Group MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20,536 high risk individuals; a randomized placebo controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 6.Waters DD, Alderman EL, Hsia J, et al. Effects of hormone replacement therapy and antioxidant vitamin supplements on coronary atherosclerosis in post menopausal women: a randomized controlled trial. JAMA. 2002;288:2432–2440. doi: 10.1001/jama.288.19.2432. [DOI] [PubMed] [Google Scholar]
- 7.Collaborative Group of the Primary Prevention Project Low dose aspirin and vitamin E in people at cardiovascular risk: a randomized trial in general practice. Lancet. 2001;357:89–95. doi: 10.1016/s0140-6736(00)03539-x. [DOI] [PubMed] [Google Scholar]
- 8.GISSI-Prevenzione Investigators Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet. 1999;354:447–455. [PubMed] [Google Scholar]
- 9.Stephens NG, Parsons A, Schofeld PM, Kelly F, Cheeseman K, Mitchonson MJ. Randomized controlled trial of vitamin E in patients with coronary disease: Cambridge Heart Antioxidant Study (CHAOS) Lancet. 1996;347:781–786. doi: 10.1016/s0140-6736(96)90866-1. [DOI] [PubMed] [Google Scholar]
- 10.Lee IM, Cook NR, Gaziano JM, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer. The Women’s Health Study: a randomized controlled trial. JAMA. 2005;294:56–65. doi: 10.1001/jama.294.1.56. [DOI] [PubMed] [Google Scholar]
- 11.Sesso HD, Buring JE, Christen WG, et al. Vitamins E and C in the prevention of cardiovascular disease in men: the Physicians Health Study II randomized controlled trial. JAMA. 2008;300:2123–2133. doi: 10.1001/jama.2008.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowman BH, Kurosky A. Haptoglobin: the evolutionary product of duplication, unequal crossing over, and point mutation. Adv. Hum. Genet. 1982;12:189–261. doi: 10.1007/978-1-4615-8315-8_3. ■■ Reviews the physiology and epidemiology of the haptoglobin (Hp) polymorphism.
- 13.Bamm VV, Tsemakhovich VA, Shaklai M, Shaklai N. Haptoglobin phenotypes differ in their ability to inhibit heme transfer from hemoglobin to LDL. Biochemistry. 2004;43:3899–3906. doi: 10.1021/bi0362626. [DOI] [PubMed] [Google Scholar]
- 14.Melamed-Frank M, Lache O, Enav B, et al. Structure/function analysis of the anti-oxidant properties of haptoglobin. Blood. 2001;98:3693–3698. doi: 10.1182/blood.v98.13.3693. [DOI] [PubMed] [Google Scholar]
- 15.Levy AP, Hochberg I, Jablonski K, et al. Haptoglobin phenotype and the risk of cardiovascular disease in individuals with diabetes: The Strong Heart Study. J. Am. Coll. Card. 2002;40:1984–1990. doi: 10.1016/s0735-1097(02)02534-2. [DOI] [PubMed] [Google Scholar]
- 16.Roguin A, Koch W, Kastrati A, Aronson D, Schomig A, Levy AP. Haptoglobin genotype is predictive of major adverse cardiac events in the one year period after PTCA in individuals with diabetes. Diab. Care. 2003;26:2628–2631. doi: 10.2337/diacare.26.9.2628. [DOI] [PubMed] [Google Scholar]
- 17.Suleiman M, Aronson D, Asleh R, et al. Haptoglobin polymorphism predicts 30-day mortality and heart failure in patients with diabetes and acute myocardial infarction. Diabetes. 2005;54:2802–2806. doi: 10.2337/diabetes.54.9.2802. [DOI] [PubMed] [Google Scholar]
- 18.Milman U, Blum S, Shapira C, et al. Vitamin E supplementation reduces cardiovascular events in a subgroup of middle-aged individuals with both Type 2 diabetes mellitus and the haptoglobin 2-2 genotype: a prospective, double-blinded clinical trial. Art. Thromb. Vasc. Biol. 2008;28:341–347. doi: 10.1161/ATVBAHA.107.153965. ■■ Original report of the Israel Cardiovascular Events Reduction with Vitamin E (ICARE) study showing that vitamin E provides significant protection to diabetes mellitus (DM) individuals with the Hp 2-2 genotype.
- 19.Costacou T, Ferrell RE, Orchard TJ. Haptoglobin genotype: a determinant of cardiovascular complications in Type 1 Diabetes. Diabetes. 2008;257:1702–1706. doi: 10.2337/db08-0095. [DOI] [PubMed] [Google Scholar]
- 20.Koch W, Latz W, Eichinger M, et al. Genotyping of common haptoglobin polymorphism Hp1/2 based on the polymerase chain reaction. Clin. Chem. 2002;48:1377–1382. [PubMed] [Google Scholar]
- 21.Boyd K, Briggs A. Cost–effectiveness of pharmacy and group behavioral support smoking cessation services in Glasgow. Addiction. 2009;104:317–325. doi: 10.1111/j.1360-0443.2008.02449.x. [DOI] [PubMed] [Google Scholar]
- 22.Pletcher MJ, Lazar L, Bibbins-Domingo K, et al. Comparing impact and cost–effectiveness of primary prevention strategies for lipid-lowering. Ann. Intern. Med. 2009;150:243–254. doi: 10.7326/0003-4819-150-4-200902170-00005. [DOI] [PubMed] [Google Scholar]
- 23.Mihaylova B, Briggs A, Armitage J, Parish S, Gray A, Collins R. Cost–effectiveness of simvastatin in people at different levels of vascular disease risk: economic analysis of a randomized trial in 20,536 individuals. Lancet. 2005;365:1779–1785. doi: 10.1016/S0140-6736(05)63014-0. [DOI] [PubMed] [Google Scholar]
- 24.Clarke PM, Gray AM, Briggs A, Stevens RJ, Matthews DR, Holman RR. Cost-utility analyses of intensive blood glucose and tight blood pressure control in Type 2 diabetes (UKPDS 72) Diabetologia. 2005;48:868–877. doi: 10.1007/s00125-005-1717-3. [DOI] [PubMed] [Google Scholar]
- 25.Levy AP, Levy JE, Kalet-Litman S, et al. Haptoglobin genotype is a determinant of iron, lipid peroxidation and macrophage accumulation in the atherosclerotic plaque. Arterioscl. Thromb. Vasc. Biol. 2007;27:134–140. doi: 10.1161/01.ATV.0000251020.24399.a2. [DOI] [PubMed] [Google Scholar]
- 26.Asleh R, Blum S, Kalet-Litman S, et al. Correction of HDL dysfunction in individuals with diabetes and the haptoglobin 2-2 genotype. Diabetes. 2008;57:2794–2800. doi: 10.2337/db08-0450. ■ Provides mechanistic basis for the ability of vitamin E to provide cardiovascular disease benefit selectively to Hp 2-2 DM individuals via its correction of high-density lipoprotein dysfunction.
- 27.Kristiansen M, Graversen JH, Jacobsen C, et al. Identification of the hemoglobin scavenger receptor. Nature. 2001;409:198–201. doi: 10.1038/35051594. [DOI] [PubMed] [Google Scholar]
- 28.Spagnuolo MS, Cigliano L, D’Andrea LD, Pedone C, Abrescia P. Assignment of the binding site for haptoglobin on apolipoprotein A-1. J. Biol. Chem. 2005;280:1193–1198. doi: 10.1074/jbc.M411390200. [DOI] [PubMed] [Google Scholar]
- 29.Asleh R, Marsh S, Shiltruck M, et al. Genetically determined heterogeneity in hemoglobin scavenging and susceptibility to diabetic cardiovascular disease. Circ. Res. 2003;92:1193–1200. doi: 10.1161/01.RES.0000076889.23082.F1. ■ Demonstrates that functional differences between exist the Hp allelic protein products in the trafficking of hemoglobin.
- 30.Levy AP, Purosothaman KR, Levy NS, et al. Downregulation of the hemoglobin scavenger receptor in individuals with diabetes and the Hp 2-2 genotype: implications for the response to intraplaque hemorrhage and plaque vulnerability. Circ. Res. 2007;101:106–110. doi: 10.1161/CIRCRESAHA.107.149435. [DOI] [PubMed] [Google Scholar]
- 31.Asleh R, Guetta J, Kalet-Litman S, Miller-Lotan R, Levy AP. Haptoglobin genotype and diabetes dependent differences in iron mediated oxidative stress in vitro and in vivo. Circ. Res. 2005;96:435–441. doi: 10.1161/01.RES.0000156653.05853.b9. ■ Provides the mechanistic basis for why vitamin C may be harmful to individuals with the Hp 2-2 genotype and DM.
- 32.Levy AP, Friedenberg P, Lotan R, et al. The effect of vitamin therapy on the progression of coronary artery atherosclerosis varies by haptoglobin type in post-menopausal women. Diabetes Care. 2004;27:925–930. doi: 10.2337/diacare.27.4.925. [DOI] [PubMed] [Google Scholar]
- 33.Poljsak B, Raspor P. The antioxidant and pro-oxidant activity of vitamin C and trolox in vitro: a comparative study. J. Appl. Toxicol. 2008;28:183–188. doi: 10.1002/jat.1264. [DOI] [PubMed] [Google Scholar]
- 34.Asleh R, Miller-Lotan R, Aviram M, et al. Haptoglobin genotype is a regulator of reverse cholesterol transport in diabetes in vitro and in vivo. Circ. Res. 2006;99:1419–1425. doi: 10.1161/01.RES.0000251741.65179.56. ■ Demonstrates in transgenic mice that the Hp genotype is a determinant of high-density lipoprotein function in vivo.
- 35.Asleh R, Levy AP. Divergent effects of α-tocopherol and vitamin C on the generation of dysfunctional HDL associated with diabetes and the Hp 2-2 genotype. Antioxid. Redox Signal. 2010;12(2):209–217. doi: 10.1089/ars.2009.2829. ■ Demonstrates that not only patient selection but also the type of antioxidant are important in determining whether antioxidant supplementation will be beneficial.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.