Abstract
Background
Alendronate is known for its ability to reduce bone loss in osteoporotic and osseous metastatic conditions. Its long-term effects remain unclear although several reports describe cases of proximal femur stress fractures associated with long-term alendronate use.
Case Description
We report the cases of four women who sustained low-energy subtrochanteric or femoral shaft stress fractures while being on alendronate therapy for more than 5 years. All radiographs showed typical patterns consisting of a transverse fracture line with external cortical bone reaction and medial cortical spike. Alendronate discontinuation along with nonoperative treatment was sufficient for one patient, whereas surgical stabilization was required in three patients.
Literature Review
The side effects of alendronate therapy include osteonecrosis of the jaw, esophageal irritation, and musculoskeletal pain. Several cases of insufficiency femoral fractures associated with prolonged alendronate use have been reported. Their radiographic pattern and clinical presentation are consistent with our observations. Although various hypotheses have been suggested, the physiopathogenesis of these stress fractures is not completely understood.
Purposes and Clinical Relevance
Although bisphosphonates play an important role in preventing pathologic fractures in patients with cancer, these subtrochanteric stress fractures associated with prolonged use of alendronate should not be ignored.
Introduction
Fractures related to osteoporosis are a major public health problem in the elderly population [28]. For the past 20 years, preventing and treating osteoporosis has become an important challenge. Many treatment options have been explored, including some drugs taken off the market for their undesirable effects, including sodium fluoride, associated with the paradoxical risk of vertebral and lower limb stress fractures [21, 26].
Alendronate reportedly reduces the risk of osteoporotic fractures and reduces bone resorption from metastatic bone lesions [4]. Since its approval by the US FDA in 1995, the optimum duration of alendronate therapy has not been clearly established. Available data suggest the treatment should be continued for 5 years [5]. The decision to maintain the patient on therapy should be made on a case-by-case approach, guided by individual fracture risk assessed by bone mineral density [5, 13]. Therefore, many patients have been receiving this medication for more than 5 years.
The side effects of bisphosphonates include osteonecrosis of the jaw, esophageal irritations, gastrointestinal discomfort, atrial fibrillation, acute inflammatory response, and severe musculoskeletal pain [9]. However, the long-term effects on bone remain unclear as the longest followup of placebo-controlled trials varies from 6 to 10 years [5, 22], and little attention has been paid to deleterious side effects on bone mineralization such as oversuppression of bone turnover and impaired ability to repair skeletal microfractures [9, 20]. In addition, discontinuation of a 5-year alendronate therapy reportedly results in prolonged suppression of bone resorption and bone formation for as much as another 5 years [5, 10].
Numerous recent reports describe cases of stress fractures of the proximal femur associated with long-term alendronate [14, 15, 17, 20, 24, 25, 27]. Clinical presentation and radiographic description of these fractures show a specific pattern consisting of external cortical reaction, transverse fracture line, and medial cortical spike in the subtrochanteric area. The physiopathology of these fractures remains unclear, although one paper suggested tensile stresses on the lateral cortex of the femur are associated with this particular type of fracture [6]. The preferred treatment also is unclear, particularly in patients with painful cortical reaction but without a clear fracture line.
We report the cases of four women who sustained low-energy subtrochanteric or femoral shaft stress fractures while being on alendronate therapy for more than 5 years.
Case Reports
Patient 1
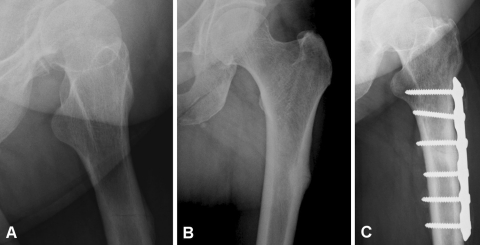
A 64-year-old woman presented with pain in her left thigh of 3 months’ duration. She was considered in complete remission after having been treated 6 years earlier with chemotherapy and bone marrow autograft for multiple myeloma. Alendronate therapy was initiated 5.5 years earlier by the hematologist to reduce pain and slow osteolysis progression. An extensive medical workup excluded any sign of recurrence, metastatic bone involvement, or metabolic disorder. Radiographs of the femur showed a thickened lateral cortex of the subtrochanteric region with a transverse nondisplaced incomplete fracture (Fig. 1A–B). Alendronate was stopped and she was treated for 2 months with activity restriction. As pain continued and the fracture line worsened, internal fixation was performed. One month after surgery, she had complete pain relief. At 6 months’ followup, radiographs showed signs of bone healing (Fig. 1C).
Fig. 1A–C.
(A) An AP radiograph shows a nondisplaced incomplete fracture of the left femur with an (B) external cortical reaction. (C) An AP radiograph shows the femur after plate fixation of the fracture.
Patient 2
A 70-year-old woman, treated previously for breast cancer, experienced pain in both thighs. She had been receiving alendronate therapy for postmenopausal primary osteoporosis for 6 years. She had no sign of osseous metastasis or metabolic disorder at presentation. Radiographs showed bilateral hypertrophy at the junction of the first and second thirds of the lateral femoral cortex without fracture (Fig. 2A–B). Analgesic treatment and partial activity restriction were initiated, but we did not discontinue bisphosphonates. Six months later, she experienced a spontaneous fracture of the right femur. There was a transverse lateral fracture line and a medial cortical spike (Fig. 2C). Treatment consisted of intramedullary nailing (Fig. 2D). Two months later, a similar fracture occurred in the left femur and she was treated with a gamma intramedullary nailing system (Fig. 2E). Four months postoperatively, no sign of consolidation was seen on plain radiographs on the left side, whereas healing was achieved on the right side. Removal of the distal left locking screw led to subsequent healing 3 months later (Fig. 2F).
Fig. 2A–F.
AP radiographs show (A) right and (B) left femoral shaft cortical reactions. (C) An AP radiograph shows a right femur transverse fracture with medial spike. (D) Right and (E) left AP radiographs show the femurs after intramedullary nailing. (F) Removal of the distal left locking screw led to subsequent healing.
Patient 3
A 77-year-old woman presented with pain in her left thigh. She had been treated with alendronate for 12 years for postmenopausal osteoporosis. She had no history of major trauma or neoplasm. A biopsy had been performed at another institution; the report suggested nonspecific bone tissue without any sign of tumor. Imaging workup showed thickening of the external cortex of the proximal left femoral shaft (Fig. 3A–D). At the time of consultation, she had persistent pain and no sign of fracture. Therefore, we recommended partial weightbearing and restricted activity for 3 months. As she did not return for followup, we called her 1 year later. At that time, she was free of pain and had resumed normal walking activities. The radiographic appearance did not change (Fig. 3E).
Fig. 3A–E.
(A) AP and (B) lateral radiographs show an external cortical shaft reaction without an evident fracture line. The cortical reaction is identified on a (C) MR image and (D) CT scan. (E) An AP radiograph taken 1 year after initial presentation shows a similar image despite clinical improvement.
Patient 4
A 59-year-old woman presented with a spontaneous fracture of the right femur after a minor fall. She had been treated with alendronate for osteoporosis for the previous 10 years. She had no history of previous pain in her thigh, no known metabolic disorder, and no neoplastic condition. Radiographs showed a displaced transverse subtrochanteric fracture with a local thick external cortex and a small spike on the medial cortex (Fig. 4A). The fracture was treated with an intramedullary nail (Fig. 4B) and alendronate therapy was stopped. Five months after surgery, the patient was pain free and showed radiographic signs of bone healing.
Fig. 4A–B.

(A) An AP radiograph shows a displaced transverse subtrochanteric fracture of the right femur with external cortex thickening and spiking of the medial cortex. (B) Another AP radiograph shows the right femur after intramedullary nailing of the fracture.
Discussion
Osteoporosis is estimated to affect 13% to 18% of women in the United States. Its prevention and treatment therefore are a major public health concern [28]. Current treatment options include calcitonins, estrogen receptor modulators, parathyroid hormone, and bisphosphonates, the latter providing the most benefit at the lowest cost [28]. Despite the known ability of alendronate to reduce the risk of osteoporotic fractures and osseous resorption in metastatic bone [3, 4, 14], recent cases of low-energy subtrochanteric and femoral shaft fractures have been described in association with long-term alendronate use [3, 14, 15, 17, 20, 24, 25, 27].
Three retrospective studies [14, 17, 19] reviewed all low-energy subtrochanteric fractures and confirmed an association with alendronate use. Goh et al. [14] reviewed 13 patients, nine of whom had been receiving alendronate therapy for a mean of 4.2 years. More recently, Lenart et al. [17] performed a case-control study identifying 41 cases of low-energy subtrochanteric or femoral shaft fractures and matched these for comparison to a group of intertrochanteric and femoral neck fractures. Among the patients with 41 subtrochanteric and femoral shaft fractures, 15 (36%) were using alendronate compared with 11% of the control group, and the duration of use also was longer in the former group. However, the most recent cohort series studying Danish national registers reports identical types of fractures and treatment in patients receiving alendronate and in control subjects regardless of the length of treatment [1].
Subtrochanteric stress fractures are rather uncommon and have been described occasionally in athletic patients or in isolated cases such as hypophosphatemic osteomalacia [7, 11, 16].
Prodromal pain in the thigh area of several months’ duration is a common complaint in 55% to 76% of the reported cases [14, 15, 17, 20, 24]. Three of our patients encountered this type of pain 4 to 12 months before fracture. During this period of latent pain, isolated thickening of the external cortex was diagnosed in the subtrochanteric region for these three patients.
Radiographic characteristics of these fractures are thickening of the external cortex associated with transverse fracture and medial cortical spike [14, 15, 17, 20, 24]. This pattern also was encountered in three of our patients, whereas the fourth patient presented with a painful stress reaction of the external cortex without an obvious fracture line. Contralateral similar lesions were seen in one of our patients, who had bilateral fractures. Goh et al. [14] and Kwek et al. [15] described this tendency toward bilateral reactions, with respectively, 33% and 53% of bilateral cases.
Alendronate acts as a strong inhibitor of bone resorption by suppressing the activity of osteoclasts [20], and although this improves osteoporotic conditions, it also reduces the overall bone turnover. The reduced bone turnover can be part of the reason why many of these fractures have delayed healing [20, 24], as was the case for one of our patients. A recent report suggests individual sensitivity to bisphosphonates and that patients having physiologically vulnerable osteoclasts tolerate alendronate poorly [29].
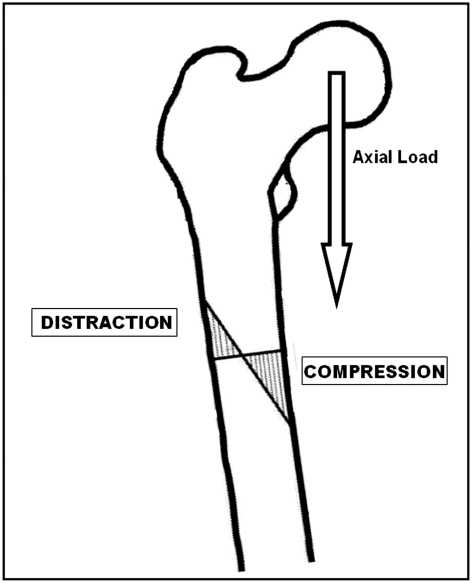
In animal experiments, bone turnover suppression reportedly leads to accumulation of microdamage, resulting in reduced bone toughness in the rib cortex [18]. Furthermore, accumulation of microdamage caused by alendronate seems to affect preferentially cortical rather than cancellous bone, explaining partially why fractures occur on the proximal cortex of the femur [17]. Odvina et al. [20] discussed this harmful effect of long-term alendronate use, suggesting severe suppression of bone turnover induces enhanced secondary mineralization, leading to skeletal fragility. This type of “marble bone” with higher Young modulus of elasticity has an increased risk of fracture [8]. Bisphosphonate treatment reportedly alters collagen cross-linking, with a substantial increase in nonenzymatic cross-links (pentosidine), which are associated with increased bone brittleness [2, 17]. The proximal portion of the femur is submitted to the large bending forces [23, 24], with compression stresses on the medial cortex and tensile stresses on the external cortex [6, 12] (Fig. 5). Given fractures occur mostly by tension, we presume these particular stress fractures occur from such stresses.
Fig. 5.
A diagram illustrates the distraction and compression areas in the proximal femoral shaft as suggested by Blaimont et al. [6].
The specific pattern of these fractures, prodromal pain, and bilateral tendency reinforce the hypothesis that these stress fractures result more likely from a systemic skeletal disorder than from an isolated local condition.
We believe the treatment of complete fractures should include internal fixation with either plating or nailing devices. However, for a patient who had been a long-term alendronate user, with a painful thigh, thickened lateral cortex, and eventually an incomplete stress fracture, the preferred treatment is unclear. In this situation, no treatment recommendations are discussed in the literature. Should these patients be treated prophylactically with surgery or should nonoperative treatment be used? We observed failure of nonoperative management in two patients. Surgery to prevent worsening of these stress reactions could be considered although one of our patients had pain relief after several months of nonoperative treatment and alendronate cessation.
Although bisphosphonates play an important role in reducing the risk of osteoporotic fractures and treatment of bone metastasis, four of our patients had subtrochanteric insufficiency fractures associated with prolonged use of alendronate. Knowledge of this potential complication is important to allow for rapid diagnosis and management. We recommend treatment of obvious fractures with internal fixation and management of a painful isolated cortical stress reaction without evident fracture should be tailored to each patient.
Acknowledgments
We thank Martine Piccart, PhD, and Thierry Gil, MD, for assistance in reviewing this manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abrahamsen B, Eiken P, Eastell R. Subtrochanteric and diaphyseal femur fractures in patients treated with alendronate: a register-based national cohort study. J Bone Miner Res. 2009;24:1095–1102. doi: 10.1359/jbmr.081247. [DOI] [PubMed] [Google Scholar]
- 2.Allen MR, Gineyts E, Leeming DJ, Burr DB, Delmas PD. Bisphosphonates alter trabecular bone collagen cross-linking and isomerization in beagle dog vertebra. Osteoporos Int. 2008;19:329–337. doi: 10.1007/s00198-007-0533-7. [DOI] [PubMed] [Google Scholar]
- 3.Aspenberg P. Bisphosphonate-induced fractures: nature strikes back? Acta Orthop. 2008;79:459–460. doi: 10.1080/17453670710015427. [DOI] [PubMed] [Google Scholar]
- 4.Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541. doi: 10.1016/S0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 5.Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, Satterfield S, Wallace RB, Bauer DC, Palermo L, Wehren LE, Lombardi A, Santora AC, Cummings SR, FLEX Research Group Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA. 2006;296:2927–2938. doi: 10.1001/jama.296.24.2927. [DOI] [PubMed] [Google Scholar]
- 6.Blaimont P, Halleux P, Jedwab J. [Distribution of bony restraints in the femur] [in French] Rev Chir Orthop Reparatrice Appar Mot. 1968;54:303–319. [PubMed] [Google Scholar]
- 7.Butler JE, Brown SL, McConnell BG. Subtrochanteric stress fractures in runners. Am J Sports Med. 1982;10:228–232. doi: 10.1177/036354658201000407. [DOI] [PubMed] [Google Scholar]
- 8.Currey JD. Effects of differences in mineralization on the mechanical properties of bone. Philos Trans R Soc Lond B Biol Sci. 1984;304:509–518. doi: 10.1098/rstb.1984.0042. [DOI] [PubMed] [Google Scholar]
- 9.Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc. 2008;83:1032–1045. doi: 10.4065/83.9.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ensrud KE, Barrett-Connor EL, Schwartz A, Santora AC, Bauer DC, Suryawanshi S, Feldstein A, Haskell WL, Hochberg MC, Torner JC, Lombardi A, Black DM, Fracture Intervention Trial Long-Term Extension Research Group Randomized trial of effect of alendronate continuation versus discontinuation in women with low BMD: results from the Fracture Intervention Trial long-term extension. J Bone Miner Res. 2004;19:1259–1269. doi: 10.1359/JBMR.040326. [DOI] [PubMed] [Google Scholar]
- 11.Esterberg J, Kassim RA, Redmon J, Coad J, Macari GS, Saleh KJ. Hip pain in a case of hypophosphatemic osteomalacia. Am J Orthop. 2003;32:455–458. [PubMed] [Google Scholar]
- 12.Garbuio P, Pernin JN. The biomechanics of the hip and hip implants. Cahier d’enseignement de la SOFCOT. 1999;69:37–48. [Google Scholar]
- 13.Geusens P. Bisphosphonates for postmenopausal osteoporosis: determining duration of treatment. Curr Osteoporos Rep. 2009;7:12–17. doi: 10.1007/s11914-009-0003-6. [DOI] [PubMed] [Google Scholar]
- 14.Goh SK, Yang KY, Koh JS, Wong MK, Chua SY, Chua DT, Howe TS. Subtrochanteric insufficiency fractures in patients on alendronate therapy: a caution. J Bone Joint Surg Br. 2007;89:349–353. doi: 10.1302/0301-620X.89B3.18146. [DOI] [PubMed] [Google Scholar]
- 15.Kwek EB, Goh SK, Koh JS, Png MA, Howe TS. An emerging pattern of subtrochanteric stress fractures: a long-term complication of alendronate therapy? Injury. 2008;39:224–231. doi: 10.1016/j.injury.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 16.Leinberry CF, McShane RB, Stewart WG, Jr, Hume EL. A displaced subtrochanteric stress fracture in a young amenorrheic athlete. Am J Sports Med. 1992;20:485–487. doi: 10.1177/036354659202000425. [DOI] [PubMed] [Google Scholar]
- 17.Lenart BA, Neviaser AS, Lyman S, Chang CC, Edobor-Osula F, Steele B, Meulen MC, Lorich DG, Lane JM. Association of low-energy femoral fractures with prolonged bisphosphonate use: a case control study. Osteoporos Int. 2009;20:1353–1362. doi: 10.1007/s00198-008-0805-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mashiba T, Turner CH, Hirano T, Forwood MR, Johnston CC, Burr DB. Effects of suppressed bone turnover by bisphosphonates on microdamage accumulation and biomechanical properties in clinically relevant skeletal sites in beagles. Bone. 2001;28:524–531. doi: 10.1016/S8756-3282(01)00414-8. [DOI] [PubMed] [Google Scholar]
- 19.Neviaser AS, Lane JM, Lenart BA, Edobor-Osula F, Lorich DG. Low-energy femoral shaft fractures associated with alendronate use. J Orthop Trauma. 2008;22:346–350. doi: 10.1097/BOT.0b013e318172841c. [DOI] [PubMed] [Google Scholar]
- 20.Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90:1294–1301. doi: 10.1210/jc.2004-0952. [DOI] [PubMed] [Google Scholar]
- 21.Orcel P, Vernejoul MC, Prier A, Miravet L, Kuntz D, Kaplan G. Stress fractures of the lower limbs in osteoporotic patients treated with fluoride. J Bone Miner Res. 1990;5(suppl 1):S191–S194. doi: 10.1002/jbmr.5650051392. [DOI] [PubMed] [Google Scholar]
- 22.Ott SM. Long-term safety of bisphosphonates. J Clin Endocrinol Metab. 2005;90:1897–1899. doi: 10.1210/jc.2005-0057. [DOI] [PubMed] [Google Scholar]
- 23.Pauwels F. Die Bedeutung der Bauprinzipien des Stutz- und Bewegungsapparates für die Beanspruchung der Rohrenknochen; erster Beitrag zur funktionellen Anatomie und kausalen Morphologie des Stutzapparates. Z Anat Entwicklungsgesch. 1948;114:129–166. doi: 10.1007/BF00523560. [DOI] [PubMed] [Google Scholar]
- 24.Sayed-Noor AS, Sjoden GO. Subtrochanteric displaced insufficiency fracture after long-term alendronate therapy: a case report. Acta Orthop. 2008;79:565–567. doi: 10.1080/17453670710015580. [DOI] [PubMed] [Google Scholar]
- 25.Sayed-Noor AS, Sjoden GO. Case reports: two femoral insufficiency fractures after long-term alendronate therapy. Clin Orthop Relat Res. 2009;467:1921–1926. doi: 10.1007/s11999-009-0725-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schnitzler CM, Wing JR, Gear KA, Robson HJ. Bone fragility of the peripheral skeleton during fluoride therapy for osteoporosis. Clin Orthop Relat Res. 1990;261:268–275. [PubMed] [Google Scholar]
- 27.Somford MP, Draijer FW, Thomassen BJ, Chavassieux PM, Boivin G, Papapoulos SE. Bilateral fractures of the femur diaphysis in a patient with rheumatoid arthritis on long-term treatment with alendronate: clues to the mechanism of increased bone fragility. J Bone Miner Res. 2009;24:1736–1740. doi: 10.1359/jbmr.090408. [DOI] [PubMed] [Google Scholar]
- 28.Tosteson AN, Burge RT, Marshall DA, Lindsay R. Therapies for treatment of osteoporosis in US women: cost-effectiveness and budget impact considerations. Am J Manag Care. 2008;14:605–615. [PubMed] [Google Scholar]
- 29.Visekruna M, Wilson D, McKiernan FE. Severely suppressed bone turnover and atypical skeletal fragility. J Clin Endocrinol Metab. 2008;93:2948–2952. doi: 10.1210/jc.2007-2803. [DOI] [PubMed] [Google Scholar]