Abstract
Aims
Connexins (Cxs) play a role in the contractility of the aorta wall. We investigated how connexins of the endothelial cells (ECs; Cx37, Cx40) and smooth muscle cells (SMCs; Cx43, Cx45) of the aorta change during renin-dependent and -independent hypertension.
Methods and results
We subjected both wild-type (WT) mice and mice lacking Cx40 (Cx40−/−), to either a two-kidney, one-clip procedure or to N-nitro-l-arginine-methyl-ester treatment, which induce renin-dependent and -independent hypertension, respectively. All hypertensive mice featured a thickened aortic wall, increased levels of Cx37 and Cx45 in SMC, and of Cx40 in EC (except in Cx40−/− mice). Cx43 was up-regulated, with no effect on its S368 phosphorylation, only in the SMCs of renin-dependent models of hypertension. Blockade of the renin–angiotensin system of Cx40−/− mice normalized blood pressure and prevented both aortic thickening and Cx alterations. Ex vivo exposure of WT aortas, carotids, and mesenteric arteries to physiologically relevant levels of angiotensin II (AngII) increased the levels of Cx43, but not of other Cx. In the aortic SMC line of A7r5 cells, AngII activated kinase-dependent pathways and induced binding of the nuclear factor-kappa B (NF-κB) to the Cx43 gene promoter, increasing Cx43 expression.
Conclusion
In both large and small arteries, hypertension differently regulates Cx expression in SMC and EC layers. Cx43 is selectively increased in renin-dependent hypertension via an AngII activation of the extracellular signal-regulated kinase and NF-κB pathways.
Keywords: Gap junctions, Cx37, Cx40, Cx43, Cx45, Aorta, Arteries, Angiotensin II, Renin, NF-κB, Transgenic mice, Hypertension
1. Introduction
The connexin (Cx) channels of gap junctions provide pathways for the communication of both endothelial cells (ECs) and smooth muscle cells (SMCs) along the vascular system,1 in patterns which vary in different species and vessels.2,3 Gap junctions allow for spreading of signals coordinating both vasoconstriction and vasodilation. ECs predominantly express Cx37, Cx40, and some Cx43, whereas SMCs are coupled by Cx43 and Cx45, sometimes with minimal levels of Cx40 and Cx37.1,4 Conditions leading to alterations in the arterial wall and/or associated with altered mechanical stress of ECs and SMCs induce changes of several Cx1,5,6 and, conversely, mice lacking Cx40 or Cx43 feature abnormal regulation of blood pressure.5,7–11
Chronic hypertension results in hypertrophic remodelling of the aortic and carotid walls in humans and animals,12–14 as an adaptation to altered hemodynamic.15 These alterations, which result in increased isobaric stiffness16 predominantly in the aorta and proximal elastic arteries15 and in cardiac after-load,17 also modify vascular Cx. However, it is still unclear whether different Cxs similarly change in various forms of hypertension. We have investigated these questions by comparing mice lacking Cx40, a genetic, renin-dependent model of hypertension,7,8,11 with wild-type (WT) mice. Both types of mice were induced to develop a renin-dependent or -independent hypertension by clipping one renal artery (two-kidney, one-clip model; 2K1C)5 and by inhibiting nitric oxide synthase (N-nitro-l-arginine methyl ester model; l-NAME),5,7,10,18 respectively.
Our data show that chronic hypertension specifically regulates Cxs in distinct layers of large and small size arteries, by mechanisms that vary for different Cxs. Chronic hypertension up-regulates Cx40 in ECs, and Cx37 and Cx45 in SMCs. In contrast, Cx43 is selectively up-regulated in the SMCs of the renin-dependent models of hypertension, by a hitherto unknown mechanism, which we now demonstrate involves the AngII activation of the ERK and NF-κB pathways.
2. Methods
2.1. Animal experiments
The investigation confirms with the Guide for the Care and Use of Laboratory Animals published by US National Institution of Health (NIH Publication No. 85-23, revised 1996), mouse care, surgery, and euthanasia procedures were approved by our institution and the Veterinary Office (Lausanne, Switzerland), and confirms with the guide for the care and use of laboratory animals (University of Lausanne, A5552-01). The generation of Cx40−/− mice and their genotypic characterization have been described.7,11,19 Breeding pairs were crossed with control C57BL6 partners. Identification of WT and homozygous Cx40−/− mice was performed by PCR of genomic DNA.7,11 Three- to 4-month-old animals, from litters obtained after at least 10 backcrosses into the C57/BL6 background, were used in all the experiments. WT and Cx40−/− mice (5–17 mice per group) with a comparable genetic background were compared in each of the following protocols: (i) for the 2K1C model, the left renal artery was clipped with a 0.12 mm internal diameter U-shaped silver clip for 4 weeks;5,7,11 (ii) addition to drinking water of either 3 mg/kg/day candesartan (Cilexetil®, Astra Zeneca) or 10 mg/kg/day ramipril (Aventis),7 addition to drinking water of 80 mg/kg/day l-NAME (Sigma), for 3 weeks.
2.2. Measurement of blood pressure
One day before sacrifice, the right carotid artery was penetrated with a catheter connected to a pressure transducer and a computerized data acquisition system,5,7,11,18,20 which recorded heart rate and both diastolic and systolic intra-arterial pressure in conscious mice, every 20 s. The system comprised a pressure transducer 156 PC PK 87802 (Honeywell Micro-Switch, Richardson, TX, USA), an HP9000-300 computer (Hewlett-Packard, Palo Alto, CA, USA), and a PP3852A scanner (Hewlett-Packard).21 All data are shown as the mean of the diastolic and systolic values (MBP). In some experiments, MBP was monitored in 7-day pre-trained mice by a non-invasive computerized tail cuff method (BP-2000, Visitech Systems). The system automatically performs a cuff inflation and deflation cycle and records pulse rate and blood pressure.5,7,11 Records were provided for an average evaluation of blood pressure over a 10-day period. In awake mice, these measurements correlated well with those made by the intra-arterial method (data not shown).
2.3. Measurement of plasma renin
Plasma renin activity (PRA) was measured by a microassay based on angiotensin I (AngI) trapping by an antibody.5,7 The amounts of AngI produced during the incubation period were then determined using a sensitive radioimmunoassay with commercially available 125I-angiotensin I (Anawa Trading SA).5,7
2.4. Measurement of aorta thickness
Euthanized mice were perfused with PBS through the left ventricle and the aortas were excised for cryosectioning. The combined thickness (intima and media) and the internal diameter of the aorta were measured.22
2.5. Ex vivo studies
Fragments of freshly excised aortas, carotids, and superior mesenteric arteries were opened longitudinally in DMEM and exposed to various concentrations of angiotensin II (AngII; Calbiochem), in the presence or absence of either 20 µM candesartan or 20 µM PD98059 (Calbiochem) for the durations given below.
2.6. Cells
A7r5 cells, a line derived from rat embryonic aorta SMCs,23 were obtained from Urs Ruegg (University of Geneva and Lausanne, Switzerland)24,25 and cultured in Dulbecco's medium. The clone we used in this study expressed the AngII receptor AT1a (see Supplementary material online, Figure S1).
2.7. Connexin analysis
RNA was analysed by real-time qPCR,5,7,11 using specific primers (see Supplementary material online, Table S1). For en face immunostaining, aortas were fixed, opened longitudinally, and labelled for Cx40, Cx37,2,26 and Cx43, using antibodies AB1726 (Chemicon) and AB1738 (Chemicon), diluted 1:50, respectively. For immunolabelling of sections and western blots, the freshly excised vessels were processed as reported.5,27 To prepare enriched ECs or SMCs, aortas were longitudinally opened in 100 µL PBS, pinned on silicone, and ECs were scraped with a scalpel. The remaining tissue provided enriched SMCs. Samples were homogenized in SDS lysis buffer and run on a 12.5% gel. Membranes were incubated overnight with the antibodies listed above, or antibodies against Cx45 (AB1748, Chemicon), α-tubulin (T5168, Sigma), or β-actin (A5441, Sigma), p-ERK1/2 and ERK1/2 (9101 and 4695, Cell Signaling). To detect phosphorylated Cx43, we used antibodies AB3841 (Chemicon) and sc-22267-r (Santa Cruz), directed against the Ser368 and Ser262 forms, respectively. Immunolabelled proteins were detected by chemiluminescence, and Cx signals normalized to either tubulin or β-actin levels (given that we could not detect tubulin in purified ECs).11
2.8. Mechanism of Cx43 up-regulation
A7r5 cells were transiently transfected using TRANSFAST (Catalys).28 Reporter plasmids consisted of the luciferase gene fused downstream of 699 or 258 bp fragments of the promoter of the rat Gja1 gene, both of which included a κB-binding site. The following day, cells were incubated for 4 h in the presence or absence of 2 µM AngII, and extracts were prepared for dual-luciferase reporter assay (Promega).28 A mutation of the putative nuclear factor-kappa B (NF-κB)-binding site was generated in the Cx43 promoter by Quick Site-directed mutagenesis (Stratagene, Europe). The PCR amplification was performed using pGL3-258 and pGL3-699 as templates, and the following forward and reverse primers: 5′-TAGTAGGGCTTGTTTCAGtatATGACCAGGGGGAGGGAGAAG-3′ (NF-κB sequence underlined and mutagenized nucleotides in lowercase), and 5′-CTTCTCCCTCCCCCTGGTCATATACTGAAACAAGCCCTACTA-3′.
A7r5 cells were cross-linked and processed for chromatin immunoprecipitation.28,29 Lysates were immunoprecipitated overnight with antibodies against either NF-κB p65 (sc-372 X; Santa Cruz Biotechnology) or NF-κB p50 (sc-1190 X; Santa Cruz). Complexes were eluted, purified, and DNA PCR-amplified to give a 246 bp fragment containing the κB site of the rat Gja1 promoter. For ERK and IκBα western blots, A7r5 cells were processed as described above. To detect NF-κB, nuclear extracts were prepared using an NE-PER kit (Pierce). The following antibodies were used: p-IκBα and IκBα (SC-7977 and SC-203, Santa Cruz), and p-ERK1/2 and ERK1/2 (9101 and 4695, Cell Signaling).
2.9. Statistical analysis
All western blot and qPCR experiments were quantitatively analysed and results are shown as mean + SEM. One-way analysis of variance (ANOVA) was performed to compare the mean values between groups, using the post hoc Bonferroni test, as provided by The Statistical Package for the Social Science (SPSS 17.0, Chicago, IL, USA).
3. Results
3.1. Mouse characteristics
Compared with WT, Cx40−/− mice featured the changes previously reported,7,11 including increased blood pressure due to elevated circulating renin (PRA), and a thickening of the aortic media (see Supplementary material online, Table S2). Treatment with candesartan, an antagonist of the AT1 AngII receptor, or ramipril, an inhibitor of the AngII-converting enzyme, did not alter the blood pressure or the aorta thickness of WT mice, in spite of a significant increase in PRA. Both treatments reduced to control the values of blood pressure and aorta thickness of Cx40−/− mice, without altering PRA (see Supplementary material online, Table S2).
The 2K1C treatment increased the blood pressure, PRA, and aorta thickness of WT mice to the levels observed in Cx40−/− mice, which were not affected by this protocol (see Supplementary material online, Table S2).The administration of l-NAME increased blood pressure by 19% and aorta thickness, but not PRA of WT mice. A smaller (8%) increase in blood pressure was observed in Cx40−/− mice, whose PRA remained significantly higher than that in WT littermates (see Supplementary material online, Table S2). The expression of the AT1a receptor was lower in aortas of Cx40−/− mice than in those of WT littermates, and, in the latter animals, was increased by the candesartan and ramipril treatments. In WT mice, the 2K1C procedure decreased the levels of the AT1a receptor to the levels of Cx40−/− animals, which were not significantly affected by this procedure. The l-NAME treatment did not alter the expression of the AT1a receptor (see Supplementary material online, Table S2).
3.2. Multiple connexins increase in the aorta of hypertensive mice
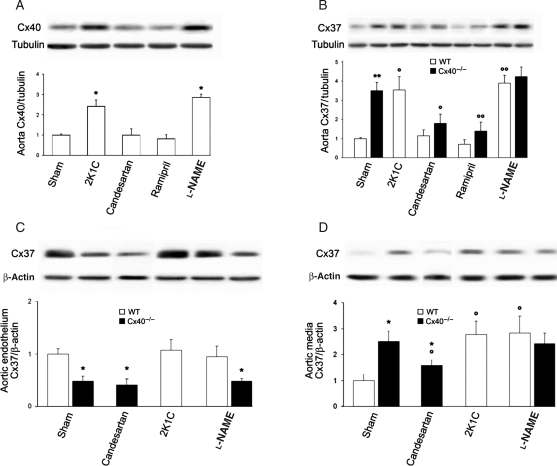
After 4 weeks of hypertension, Cx40 increased in WT mice submitted to either the 2K1C or l-NAME treatment (Figure 1A), due to a transcriptional up-regulation (see Supplementary material online, Figure S2A). Immunostaining showed that Cx40 was increased solely between ECs (Figure 1E and F, left panels). At the same time point, Cx37 was also increased in the aortas of all WT mice made hypertensive, as well as in hypertensive Cx40−/− mice (Figure 1B and see Supplementary material online, Figure S2B), due to an up-regulation in SMCs (Figure 1C and D). Accordingly, immunostaining and western blot revealed no significant change of Cx37 in ECs, except for the expected2 decrease in Cx40−/− mice (Figure 1C, E and F, right panels). Treatment with either candesartan or ramipril reduced Cx37 expression in Cx40−/−, but not WT mice (Figure 1B and see Supplementary material online, Figure S2B). The SMC, but not the EC, distribution was altered after both the candesartan (Figure 1C and D) and the ramipril treatments (data not shown). Cx45 was also increased in the aortic SMCs of all hypertensive mice (Figure 2A) and was reduced under treatment with either candesartan or ramipril in Cx40−/− but not WT mice (Figure 2A, left panel, and see Supplementary material online, Figure S2C).
Figure 1.
Cx40 and Cx37 increase in the aorta of hypertensive mice. (A) Western blots showed increased Cx40 in renin-dependent and -independent hypertensive WT mice. (B) Cx37 was also higher in the aortas of hypertensive animals. Treatment with candesartan or ramipril reduced the expression of Cx37 in the spontaneously hypertensive Cx40−/− mice. (C) Western blots demonstrated that Cx37 levels did not change in the aortic intima of either 2K1C or l-NAME hypertensive mice, and were lower in Cx40−/− than in WT animals. Treatment with candesartan did not affect Cx37 levels in the endothelium of Cx40−/− mice. (D) Cx37 was less abundant in the SMCs than in the ECs of WT controls, whereas it increased in the SMCs of Cx40−/− mice. A Cx37 increase occurred in the media of all hypertensive mice. The levels of SMC Cx37 were also altered after candesartan treatment in Cx40−/− mice. Data represent mean + SEM of four experiments. *P < 0.05, **P < 0.01 vs. the respective WT animals; °P < 0.05, °°P < 0.01 vs. WT or Cx40−/− untreated or sham-operated animals. (E) En face immunostaining showed that Cx40, but not Cx37, was increased between ECs of hypertensive mice. (F) Sections confirmed that Cx40 was solely expressed in ECs, whereas Cx37 was detectable in ECs and in the SMCs of hypertensive mice. L, lumen; M, media. Bar represents 30 µm.
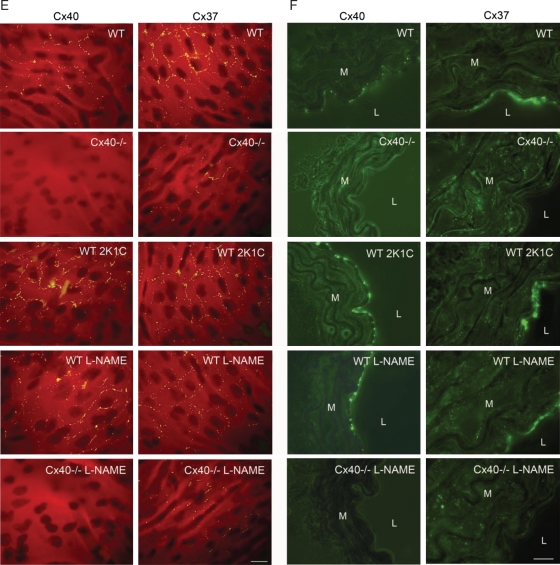
Figure 2.
Cx43 and Cx45 are differently affected by renin-dependent and -independent hypertension. (A) Cx45 increased in all WT mice made hypertensive, and this increase was blocked in Cx40−/− mice by RAS inhibitors (left panel). Cx45 was specifically increased in the aortic SMCs of hypertensive mice (right panel). (B) In contrast, Cx43 increased only in aortas of renin-dependent models (Cx40−/− and 2K1C). Data represent mean + SEM of four experiments. *P < 0.05, **P < 0.01 vs. the respective WT animals; °P < 0.05, °°P < 0.01 vs. WT or Cx40−/− untreated or sham-operated animals. (C) Immunostaining showed Cx43 throughout the media of all aortas. Increased numbers of immunospots were observed in the media of all Cx40−/− and hypertensive 2K1C WT mice. M, media; L, lumen. Bar represents 30 µm.
Cx43 increased only in renin-dependent hypertension (Figure 2B), due to a transcriptional up-regulation (see Supplementary material online, Figure S2D) which, as judged by its blockade under candesartan or ramipril treatment, required activation of the renin–angiotensin system (RAS) (Figure 2B and see Supplementary material online, Figure S2D). Immunostaining showed that most of Cx43 was expressed by aortic SMCs (Figure 2C). Antibodies to Ser262 and Ser368 showed that these changes did not affect the proportion of phosphorylated Cx43 (see Supplementary material online, Figure S3). These results show that chronic hypertension is associated with an up-regulation of all major aortic Cxs, which are differentially regulated by renin-dependent and -independent mechanisms.
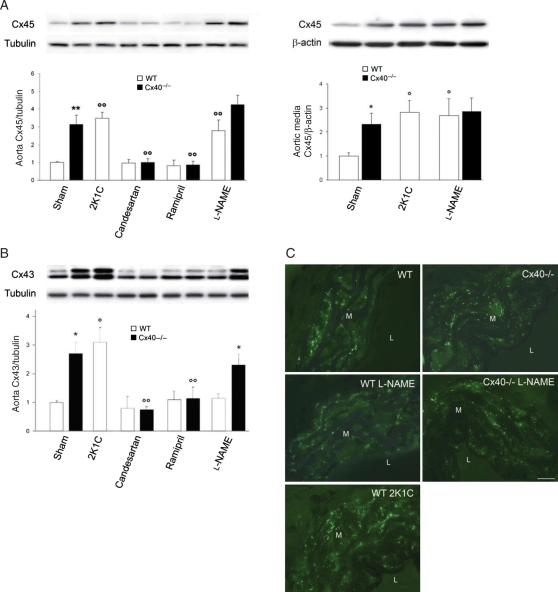
3.3. Cx43 is increased by AngII
Given that Cx43 was the only Cx which selectively increased in renin-dependent hypertension, and that AngII is the main RAS activator in this form of hypertension,30,31 we investigated the relationship between these two peptides. By exposing freshly isolated aortas of WT mice to AngII, we observed that within 4 h, 10 nM AngII, a concentration that mimics the physiological levels of the vasoconstricting peptide,18,32–35 significantly increased the levels of Cx43. However, the two- to three-fold increase in this protein which was observed in vivo was only reached with micromolar concentrations (Figures 3A and B). Therefore, we selected a concentration of 2 µM AngII for all other experiments. Western blots showed that within 2 h, 2 µM AngII increased Cx43 in WT SMCs (Figure 3C), and the phosphorylation of ERK1/2 (Figure 3D). This phosphorylation was not increased following the l-NAME treatment (Figure 3E), which also did not alter Cx43 expression (Figure 2B). In the aortas of Cx40−/− mice, AngII induced a smaller and delayed increase in Cx43, and prevented the down-regulation of Cx43 expression which occurred in the absence of the hormone (Figure 3F). Under this condition, the levels of Cx43 decreased in the aorta of Cx40−/− mice to reach control values within 48 h. (Figure 3F), due to rundown of AngII, which is natively high in these animals.7,8 These results show that Cx43 is up-regulated in parallel with the ERK pathway, due to RAS activation.
Figure 3.
AngII stimulates Cx43 expression in a dose-dependent manner. (A and B) Western blots of WT aortas exposed for 4 h to AngII showed that the peptide increased the levels of Cx43 and P-ERK1/2, at physiologically nanomolar concentrations, and reproduced the two-fold Cx43 increase observed in vivo, at concentrations >0.1 µM. (C and D) Exposure of WT aortas to 2 µM AngII increased within 2 h Cx43 (C), and P-ERK1/2 (D). (E) The levels of the P-ERK1/2 increased in aortas of Cx40−/− and 2K1C mice, but not in those of l-NAME-treated mice. (F) A smaller and delayed effect was observed with aortas of Cx40−/− mice. In the absence of AngII, the levels of Cx43 decreased in this tissue to reach control values within 48 h. Data represent mean + SEM of three experiments. *P < 0.05, **P < 0.01, °P < 0.05 vs. respective untreated WT or Cx40−/− aortas. §P < 0.05 vs. untreated Cx40−/− aortas at t = 0 h.
3.4. The AngII-induced regulation is seen in smaller arteries
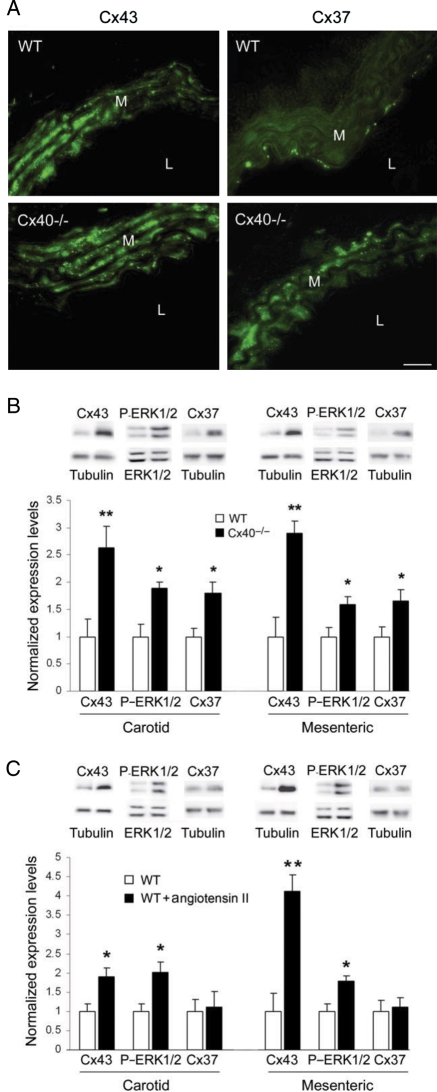
Using carotid and mesenteric arteries, which express a Cx pattern analogous to that of the aorta (Figure 4A), we also observed increased levels of Cx43 and ERK1/2 phosphorylation in Cx40−/− mice (Figure 4B). When exposed in vitro to AngII, the two types of WT vessels featured an increased expression of Cx43 and phosphorylation of ERK1/2 (Figure 4C), as observed in the aorta (Figure 3C and D). This change was significantly higher in the small-diameter mesenteric arteries than in the larger carotids (Figure 4C). These experiments show that chronic hypertension similarly targets the aorta and the smallest arteries we could test in mice.
Figure 4.
Carotid and mesenteric arteries show a Cx pattern and responsiveness to AngII similar to those of aorta. (A, left panels) Immunostaining showed punctate Cx43 throughout the carotid media. Increased numbers of immunospots were observed in the media of Cx40−/− mice. (A, right panels) Cx37 was detectable in the media of hypertensive but not control mice. L, lumen; M, media. Bar represents 10 µm. (B) Western blots showed that Cx37, Cx43, and P-ERK1/2 were increased in carotid and mesenteric arteries of Cx40−/− mice. (C) After a 4 h exposure of WT carotids and mesenteric arteries to 2 µM AngII, Cx43 and P-ERK1/2, but not Cx37, were increased. Data represent mean + SEM of three experiments. *P < 0.05, **P < 0.01 vs. respective untreated vessels or WT animals.
3.5. A7r5 cells represent a convenient model of aortic SMCs
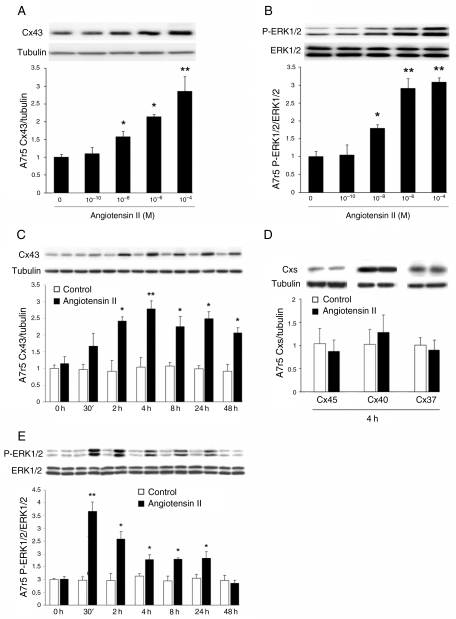
To further investigate the molecular mechanism of the AngII induction of Cx43, we searched a cell line that would mimic the main features of primary SMCs. We found that A7r5 expressed a Cx pattern alike that of aortic SMCs (Figure 5A, C, D) and responded to physiologically relevant concentrations of AngII with a similar increase in Cx43 and phosphorylated ERK1/2 (P-ERK1/2) (Figure 5A and B). At a 2 µM concentration, which induced in A7r5 cells a two- to three-fold increase in Cx43 similar to that observed in vivo and in isolated aortas, A7r5 cells also increased the expression of Cx43, but not that of Cx37, Cx40, and Cx45 (Figure 5C and D) and showed a rapid, AngII-dependent activation of the ERK pathway (Figure 5E). Thus, A7r5 cells reproduced the main Cx and signalling changes observed in native aortas.
Figure 5.
A7r5 cells feature the same Cx43 and signalling changes observed in aortic SMCs. (A and B) Western blots of A7r5 cells exposed for 2 h to increasing concentrations of AngII showed that the peptide increased the levels of Cx43 and P-ERK1/2 at concentrations similar to those that elicited comparable changes in aortic SMCs. (C and D) Western blots showed that A7r5 cells expressed Cx43, Cx37, Cx40, and Cx45. Two-micromolar AngII increased Cx43, but not Cx37, Cx40, and Cx45. (E) AngII also increased the levels of P-ERK1/2. Results are means + SEM of three experiments. *P < 0.05, **P < 0.01 vs. untreated cells.
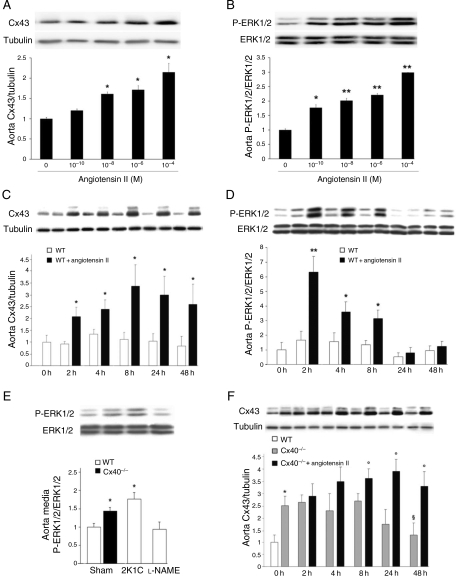
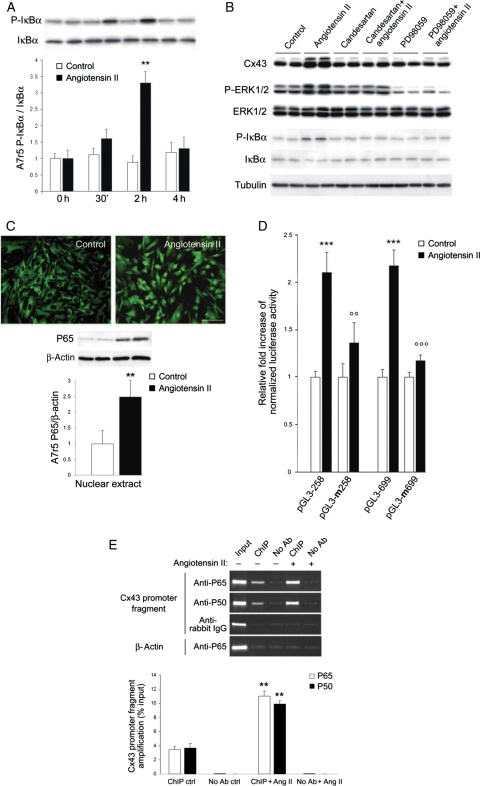
3.6. AngII increases Cx43 via activation of the NF-κB pathway
A7r5 cells exposed to AngII increased the proportion of phosphorylated IκBα36,37 (Figure 6A and B), with a time course consistent with that of the Cx43 changes (Figure 5A). Immunostaining demonstrated that AngII induced the nuclear translocation of the p65-NF-κB transcription factor (Figure 6C). Candesartan, and the inhibitor of the ERK1/2 pathway PD98059, prevented the AngII-dependent induction of Cx43 expression, and ERK1/2 and IκBα phosphorylation (Figure 6B). These results suggest that AngII up-regulates Cx43 via the activation of the ERK and NF-κB pathways.
Figure 6.
The AngII-induced increase in Cx43 requires the activation of ERK and NF-κB pathways. (A) Within 2 h, AngII increased the phosphorylation of IκBα in A7r5 cells. Results are means + SEM of three experiments. **P < 0.01 vs. untreated cells. (B) Within 2 h, AngII also increased Cx43, P-ERK1/2, and P-IκBα levels. Both candesartan and PD98059 prevented these effects. (C) After 4 h, 2 µM AngII induced a translocation of the P65 phosphorylated form of NF-κB into the nucleus of A7r5 cells. Bar, 20 µm. (D) AngII increased luciferase activity of A7r5 cells transfected with either a short or long Gja1 promoter fragment. Mutation of the NF-κB motif in either one of the two promoter fragments prevented the increased in the luciferase activity observed after AngII stimulation. (E) Quantitative RT–PCR showed that AngII increased the amount of the Gja1 promoter fragment, recovered using antibodies against either the P65 or the P50 forms of NF-κB. Results are means + SEM of three experiments. **P < 0.01, ***P < 0.001 vs. untreated cells; °°P < 0.01, °°°P < 0.001 vs. AngII-treated cells.
3.7. NF-κB binds to the promoter of the Cx43 gene and activates its transcription
We found a canonical κB site between −312 and −301 bp of the promoter of the rat Gja1 gene. Therefore, we transfected A7r5 cells with a luciferase cDNA, under control of two fragments of the rat Cx43 promoter, each containing a κB site. After 4 h in the presence of 2 µM AngII, we observed an increase in luciferase activity, whether the reporter gene was driven by the short (258 bp) or long (699 bp) promoter fragment (Figure 6D). This increase was prevented by mutating the κB site (Figure 6D).
We incubated chromatin from control and AngII-stimulated A7r5 cells with antibodies against either the P65 or P50 form of NF-κB. Both antibodies immunoprecipitated fragments which, by PCR, yielded a sequence corresponding to −433 and −187 bp (relative to the transcription initiation site38) of the Cx43 promoter (Figure 6E). After a 2 h exposure to AngII, the recovery of this fragment increased in the presence, but not in the absence, of antibodies against NF-κB (Figure 6E). These data document that AngII enhances the binding of NF-κB to the Gja1 promoter.
4. Discussion
The multiple Cxs which are expressed by vascular ECs and SMCs4,6 have been implicated in the physiological function of arteries,39 and their adaptation to chronic hypertension.22,40 Still, it is not clear whether and how all vascular Cxs are similarly affected by all forms of hypertension.41 Comparing models of renin-dependent5 and -independent hypertension,5,7,10,18 we now show that all hypertensive mice featured a thickening of the media, which was associated with increased levels of Cx40 in the intimal ECs, and of Cx37 and Cx45 in the media SMCs. In contrast, Cx43 was up-regulated in the latter layer, without obvious changes in its phosphorylation, only under conditions of renin-dependent hypertension. These observations document that multiple Cx changes are associated with the remodelling of the arterial wall which occurs in response to the altered mechanical and hormonal environment of hypertension. They further show that although the control of Cx37, Cx40, and Cx45 expression does not depend on the circulating levels of renin and AngII, these hormones are required for the control of Cx43. Given that AngII ultimately mediates the vasoconstriction and SMC changes42 that result from RAS activation,31 we have investigated the effects of this peptide. Consistent with previous data in rats and cultured SMCs,42 we have found that within a few hours, physiologically relevant levels of AngII increased the expression of Cx43, but not of Cx37, Cx40, and Cx45. This change is induced by the activation of ERK1/2 which, by causing the phosphorylation of IκBα,43,44 results in the nuclear translocation of NF-κB. We now document that NF-κB directly and specifically binds in situ to the promoter of the Gja1 gene which codes for Cx43, and that the NF-κB binding is enhanced by AngII. The Cx43 changes are rapidly induced by the ERK1/2 activation, but persist even after the ERK activity has returned to basal levels, indicating that other mechanisms contribute to the sustained elevation of Cx43 expression.
These experiments provide the first coherent explanation of how a renin increase enhances Cx43: (i) the activation of RAS increases the circulating levels of AngII; (ii) elevated AngII results in peripheral vasoconstriction, causing hypertension, and triggering SMC hypertrophy and proliferation; (iii) in parallel, AngII promotes, via phosphorylation of ERK1/2, the binding of NF-κB to the Gja1 promoter; (iv) this binding trans-activates the Gja1 gene, leading to increased production of Cx43 in the SMCs (see Supplementary material online, Figure S4). The finding of comparable Cx43 changes in the aorta, the carotids, and the small mesenteric arteries suggests that our observations apply to the many vascular compartments targeted by hypertension.15,45 Our data further implicate that other mechanisms, possibly dependent on the mechanical forces that impinge on the arterial walls during hypertension,1,46,47 in the control of Cx37, Cx40, and Cx45, as well as in the sustained elevation of Cx43, once the activation of ERK1/2 ends.
The significance of the increase in Cx43 in renin-dependent hypertension remains to be elucidated. Beside its major vasoconstrictor effect, AngII also stimulates vascular remodelling by promoting SMC growth and the production of extra cellular matrix, which contribute to increased aortic stiffness,48 a frequent consequence of hypertension.49 Increased Cx43 expression in the presence of elevated AngII may therefore contribute to regulate the elasticity of the vascular wall. If so, the pharmacological targeting of Cx43 may be therapeutically useful, in addition to the standard anti-hypertensive drugs which aim at counteracting the AngII effects.50
In summary, by comparing control and Cx40-lacking mice, under conditions of renin-dependent (2K1C) and renin-independent hypertension (l-NAME administration), we have found that Cx37, Cx40, and Cx45 are up-regulated in the wall of different types of arteries, probably as a result of the increased mechanical forces impinging on the vessels' wall. In contrast, Cx43 was up-regulated only in the renin-dependent model of hypertension, due to an AngII-dependent mechanism, which specifically activates the transcription of the Cx43 gene. These findings document that the expression of several vascular connexins is affected by chronic hypertension, though by different mechanisms, and in different compartments of the arterial wall.
Supplementary material
Supplementary material is available at Cardiovascular Research online.
Conflict of interest: none declared.
Funding
Supported by grants from the SNF (310000-122423; 310000-109402), the JDRF (1-2007-158), the EU (BETAIMAGE 222980; IMIDIA, C2008-T7), the NIH HL64232, the Octav and the Marcella Botnar Foundation, the Novartis Foundation, and the Emma Muschamp Foundation.
Supplementary Material
References
- 1.Haefliger JA, Nicod P, Meda P. Contribution of connexins to the function of the vascular wall. Cardiovasc Res. 2004;62:345–356. doi: 10.1016/j.cardiores.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 2.Simon AM, McWhorter AR. Decreased intercellular dye-transfer and downregulation of non-ablated connexins in aortic endothelium deficient in connexin37 or connexin40. J Cell Sci. 2003;116:2223–2236. doi: 10.1242/jcs.00429. [DOI] [PubMed] [Google Scholar]
- 3.Kruger O, Beny JL, Chabaud F, Traub O, Theis M, Brix K, et al. Altered dye diffusion and upregulation of connexin37 in mouse aortic endothelium deficient in connexin40. J Vasc Res. 2002;39:160–172. doi: 10.1159/000057764. [DOI] [PubMed] [Google Scholar]
- 4.Brisset AC, Isakson BE, Kwak BR. Connexins in vascular physiology and pathology. Antioxid Redox Signal. 2009;11:267–282. doi: 10.1089/ars.2008.2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haefliger JA, Krattinger N, Martin D, Pedrazzini T, Capponi A, Doring B, et al. Connexin43-dependent mechanism modulates renin secretion and hypertension. J Clin Invest. 2006;116:405–413. doi: 10.1172/JCI23327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Figueroa XF, Duling BR. Gap junctions in the control of vascular function. Antioxid Redox Signal. 2009;11:251–266. doi: 10.1089/ars.2008.2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krattinger N, Capponi A, Mazzolai L, Aubert JF, Caille D, Nicod P, et al. Connexin40 regulates renin production and blood pressure. Kidney Int. 2007;72:814–822. doi: 10.1038/sj.ki.5002423. [DOI] [PubMed] [Google Scholar]
- 8.Wagner C, de Wit C, Kurtz L, Grunberger C, Kurtz A, Schweda F. Connexin40 is essential for the pressure control of renin synthesis and secretion. Circ Res. 2007;100:556–563. doi: 10.1161/01.RES.0000258856.19922.45. [DOI] [PubMed] [Google Scholar]
- 9.Kurtz L, Schweda F, de Wit C, Kriz W, Witzgall R, Warth R, et al. Lack of connexin 40 causes displacement of renin-producing cells from afferent arterioles to the extraglomerular mesangium. J Am Soc Nephrol. 2007;18:1103–1111. doi: 10.1681/ASN.2006090953. [DOI] [PubMed] [Google Scholar]
- 10.Wagner C. Function of connexins in the renal circulation. Kidney Int. 2008;73:547–555. doi: 10.1038/sj.ki.5002720. [DOI] [PubMed] [Google Scholar]
- 11.Krattinger N, Alonso F, Capponi A, Mazzolai L, Nicod P, Meda P, et al. Increased expression of renal cyclooxygenase-2 and neuronal nitric oxide synthase in hypertensive Cx40-deficient mice. J Vasc Res. 2009;46:188–198. doi: 10.1159/000156704. [DOI] [PubMed] [Google Scholar]
- 12.Zanchi A, Wiesel P, Aubert JF, Brunner HR, Hayoz D. Time course changes of the mechanical properties of the carotid artery in renal hypertensive rats. Hypertension. 1997;29:1199–1203. doi: 10.1161/01.hyp.29.5.1199. [DOI] [PubMed] [Google Scholar]
- 13.Fitch RM, Rutledge JC, Wang YX, Powers AF, Tseng JL, Clary T, et al. Synergistic effect of angiotensin II and nitric oxide synthase inhibitor in increasing aortic stiffness in mice. Am J Physiol Heart Circ Physiol. 2006;290:H1190–H1198. doi: 10.1152/ajpheart.00327.2005. [DOI] [PubMed] [Google Scholar]
- 14.Yasmin, O'Shaughnessy KM. Genetics of arterial structure and function: towards new biomarkers for aortic stiffness? Clin Sci (Lond) 2008;114:661–677. doi: 10.1042/CS20070369. [DOI] [PubMed] [Google Scholar]
- 15.Laurent S, Boutouyrie P, Lacolley P. Structural and genetic bases of arterial stiffness. Hypertension. 2005;45:1050–1055. doi: 10.1161/01.HYP.0000164580.39991.3d. [DOI] [PubMed] [Google Scholar]
- 16.Safar ME, Thuilliez C, Richard V, Benetos A. Pressure-independent contribution of sodium to large artery structure and function in hypertension. Cardiovasc Res. 2000;46:269–276. doi: 10.1016/s0008-6363(99)00426-5. [DOI] [PubMed] [Google Scholar]
- 17.Safar ME, Boudier HS. Vascular development, pulse pressure, and the mechanisms of hypertension. Hypertension. 2005;46:205–209. doi: 10.1161/01.HYP.0000167992.80876.26. [DOI] [PubMed] [Google Scholar]
- 18.Wiesel P, Mazzolai L, Nussberger J, Pedrazzini T. Two-kidney, one clip and one-kidney, one clip hypertension in mice. Hypertension. 1997;29:1025–1030. doi: 10.1161/01.hyp.29.4.1025. [DOI] [PubMed] [Google Scholar]
- 19.Kirchhoff S, Nelles E, Hagendorff A, Kruger O, Traub O, Willecke K. Reduced cardiac conduction velocity and predisposition to arrhythmias in connexin40-deficient mice. Curr Biol. 1998;8:299–302. doi: 10.1016/s0960-9822(98)70114-9. [DOI] [PubMed] [Google Scholar]
- 20.Mazzolai L, Nussberger J, Aubert JF, Brunner DB, Gabbiani G, Brunner HR, et al. Blood pressure-independent cardiac hypertrophy induced by locally activated renin-angiotensin system. Hypertension. 1998;31:1324–1330. doi: 10.1161/01.hyp.31.6.1324. [DOI] [PubMed] [Google Scholar]
- 21.Fluckiger JP, Gremaud G, Waeber B, Kulik A, Ichino A, Nussberger J, et al. Measurement of sympathetic nerve activity in the unanesthetized rat. J Appl Physiol. 1989;67:250–255. doi: 10.1152/jappl.1989.67.1.250. [DOI] [PubMed] [Google Scholar]
- 22.Haefliger JA, Castillo E, Waeber G, Bergonzelli GE, Aubert JF, Sutter E, et al. Hypertension increases connexin43 in a tissue-specific manner. Circulation. 1997;95:1007–1014. doi: 10.1161/01.cir.95.4.1007. [DOI] [PubMed] [Google Scholar]
- 23.Mederos y, Schnitzler M, Storch U, Meibers S, Nurwakagari P, Breit A, et al. Gq-coupled receptors as mechanosensors mediating myogenic vasoconstriction. EMBO J. 2008;27:3092–3103. doi: 10.1038/emboj.2008.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skutella M, Ruegg UT. Studies on capacitative calcium entry in vascular smooth muscle cells by measuring 45CA2+ influx. J Recept Signal Transduct Res. 1997;17:163–175. doi: 10.3109/10799899709036601. [DOI] [PubMed] [Google Scholar]
- 25.Skutella T, Savaskan NE, Ninnemann O, Nitsch R. Target- and maturation-specific membrane-associated molecules determine the ingrowth of entorhinal fibers into the hippocampus. Dev Biol. 1999;211:277–292. doi: 10.1006/dbio.1999.9295. [DOI] [PubMed] [Google Scholar]
- 26.Simon AM, Chen H, Jackson CL. Cx37 and Cx43 localize to zona pellucida in mouse ovarian follicles. Cell Commun Adhes. 2006;13:61–77. doi: 10.1080/15419060600631748. [DOI] [PubMed] [Google Scholar]
- 27.Haefliger JA, Demotz S, Braissant O, Suter E, Waeber B, Nicod P, et al. Connexins 40 and 43 are differentially regulated within the kidneys of rats with renovascular hypertension. Kidney Int. 2001;60:190–201. doi: 10.1046/j.1523-1755.2001.00786.x. [DOI] [PubMed] [Google Scholar]
- 28.Allagnat F, Alonso F, Martin D, Abderrahmani A, Waeber G, Haefliger JA. ICER-1gamma overexpression drives palmitate-mediated connexin36 down-regulation in insulin-secreting cells. J Biol Chem. 2008;283:5226–5234. doi: 10.1074/jbc.M708181200. [DOI] [PubMed] [Google Scholar]
- 29.Martin D, Allagnat F, Chaffard G, Caille D, Fukuda M, Regazzi R, et al. Functional significance of repressor element 1 silencing transcription factor (REST) target genes in pancreatic beta cells. Diabetologia. 2008;51:1429–1439. doi: 10.1007/s00125-008-0984-1. [DOI] [PubMed] [Google Scholar]
- 30.Burnier M. Spotlight on renin. The renin-angiotensin-aldosterone system and metabolic syndrome. J Renin Angiotensin Aldosterone Syst. 2006;7:184. doi: 10.3317/jraas.2006.030. [DOI] [PubMed] [Google Scholar]
- 31.Mehta PK, Griendling KK. Angiotensin II cell signaling: physiological and pathological effects in the cardiovascular system. Am J Physiol Cell Physiol. 2007;292:C82–C97. doi: 10.1152/ajpcell.00287.2006. [DOI] [PubMed] [Google Scholar]
- 32.Mazzolai L, Pedrazzini T, Nicoud F, Gabbiani G, Brunner HR, Nussberger J. Increased cardiac angiotensin II levels induce right and left ventricular hypertrophy in normotensive mice. Hypertension. 2000;35:985–991. doi: 10.1161/01.hyp.35.4.985. [DOI] [PubMed] [Google Scholar]
- 33.Stanton AV, Gradman AH, Schmieder RE, Nussberger J, Sarangapani R, Prescott MF. Aliskiren monotherapy does not cause paradoxical blood pressure rises. meta-analysis of data from 8 clinical trials. Hypertension. 2010;55:54–60. doi: 10.1161/HYPERTENSIONAHA.109.135772. [DOI] [PubMed] [Google Scholar]
- 34.Abe F, Omata K, Yamada M, Tsunoda K, Sato T, Shimizu T, et al. Specific direct radioimmunoassay of angiotensin II (AT II) in human plasma and the effect of angiotensin converting enzyme (ACE) inhibitor. Immunopharmacology. 1999;44:199–204. doi: 10.1016/s0162-3109(99)00090-9. [DOI] [PubMed] [Google Scholar]
- 35.Kiribayashi K, Masaki T, Naito T, Ogawa T, Ito T, Yorioka N, et al. Angiotensin II induces fibronectin expression in human peritoneal mesothelial cells via ERK1/2 and p38 MAPK. Kidney Int. 2005;67:1126–1135. doi: 10.1111/j.1523-1755.2005.00179.x. [DOI] [PubMed] [Google Scholar]
- 36.Ghosh S, Karin M. Missing pieces in the NF-kappaB puzzle. Cell. 2002;109(Suppl.):S81–S96. doi: 10.1016/s0092-8674(02)00703-1. [DOI] [PubMed] [Google Scholar]
- 37.Levrand S, Pesse B, Feihl F, Waeber B, Pacher P, Rolli J, et al. Peroxynitrite is a potent inhibitor of NF-{kappa}B activation triggered by inflammatory stimuli in cardiac and endothelial cell lines. J Biol Chem. 2005;280:34878–34887. doi: 10.1074/jbc.M501977200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Teunissen BE, Jansen AT, van Amersfoorth SC, O'Brien TX, Jongsma HJ, Bierhuizen MF. Analysis of the rat connexin 43 proximal promoter in neonatal cardiomyocytes. Gene. 2003;322:123–136. doi: 10.1016/j.gene.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 39.Fanchaouy M, Bychkov R, Meister JJ, Beny JL. Stretch-elicited calcium responses in the intact mouse thoracic aorta. Cell Calcium. 2007;41:41–50. doi: 10.1016/j.ceca.2006.04.030. [DOI] [PubMed] [Google Scholar]
- 40.Haefliger JA, Meda P, Formenton A, Wiesel P, Zanchi A, Brunner HR, et al. Aortic connexin43 is decreased during hypertension induced by inhibition of nitric oxide synthase. Arterioscler Thromb Vasc Biol. 1999;19:1615–1622. doi: 10.1161/01.atv.19.7.1615. [DOI] [PubMed] [Google Scholar]
- 41.Figueroa XF, Isakson BE, Duling BR. Vascular gap junctions in hypertension. Hypertension. 2006;48:804–811. doi: 10.1161/01.HYP.0000242483.03361.da. [DOI] [PubMed] [Google Scholar]
- 42.Cheng G, Kim MJ, Jia G, Agrawal DK. Involvement of chloride channels in IGF-I-induced proliferation of porcine arterial smooth muscle cells. Cardiovasc Res. 2007;73:198–207. doi: 10.1016/j.cardiores.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cui R, Tieu B, Recinos A, Tilton RG, Brasier AR. RhoA mediates angiotensin II-induced phospho-Ser536 nuclear factor kappaB/RelA subunit exchange on the interleukin-6 promoter in VSMCs. Circ Res. 2006;99:723–730. doi: 10.1161/01.RES.0000244015.10655.3f. [DOI] [PubMed] [Google Scholar]
- 44.Bonizzi G, Karin M. The two NF-kappaB activation pathways and their role in innate and adaptive immunity. Trends Immunol. 2004;25:280–288. doi: 10.1016/j.it.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 45.Safar ME, Jankowski P. Central blood pressure and hypertension: role in cardiovascular risk assessment. Clin Sci (Lond) 2009;116:273–282. doi: 10.1042/CS20080072. [DOI] [PubMed] [Google Scholar]
- 46.Haefliger JA, Tissieres P, Tawadros T, Formenton A, Beny JL, Nicod P, et al. Connexins 43 and 26 are differentially increased after rat bladder outlet obstruction. Exp Cell Res. 2002;274:216–225. doi: 10.1006/excr.2001.5465. [DOI] [PubMed] [Google Scholar]
- 47.Sakurabayashi-Kitade S, Aoka Y, Nagashima H, Kasanuki H, Hagiwara N, Kawana M. Aldosterone blockade by spironolactone improves the hypertensive vascular hypertrophy and remodeling in angiotensin II overproducing transgenic mice. Atherosclerosis. 2009;206:54–60. doi: 10.1016/j.atherosclerosis.2009.01.039. [DOI] [PubMed] [Google Scholar]
- 48.Tham DM, Martin-McNulty B, Wang YX, Da Cunha V, Wilson DW, Athanassious CN, et al. Angiotensin II injures the arterial wall causing increased aortic stiffening in apolipoprotein E-deficient mice. Am J Physiol Regul Integr Comp Physiol. 2002;283:R1442–R1449. doi: 10.1152/ajpregu.00295.2002. [DOI] [PubMed] [Google Scholar]
- 49.Wang YX, Fitch RM. Vascular stiffness: measurements, mechanisms and implications. Curr Vasc Pharmacol. 2004;2:379–384. doi: 10.2174/1570161043385448. [DOI] [PubMed] [Google Scholar]
- 50.Dzau VJ. Mechanism of protective effects of ACE inhibition on coronary artery disease. Eur Heart J. 1998;19(Suppl. J):J2–J6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.