Abstract
While the effects of chronic ethanol consumption on liver have been well studied and documented, its effect on the cardiovascular system is bimodal. Thus, moderate drinking in many population studies is related to lower prevalence of coronary artery disease (CAD). In contrast, heavy drinking correlates with higher prevalence of CAD. In several other studies of cardiovascular mortalities, abstainers and heavy drinkers are at higher risk than light or moderate drinkers. The composite of this disparate relation in several population studies of cardiovascular mortality has been a “U-” or “J-”shaped curve. Apart from its ability to eliminate cholesterol from the intima of the arteries by reverse cholesterol transport, another major mechanism by which HDL may have this cardioprotective property is by virtue of the ability of its component enzyme paraoxonase1 (PON1) to inhibit LDL oxidation and/or inactivate OxLDL. Therefore, PON1 plays a central role in the disposal of OxLDL and thus is antiatherogenic. Furthermore, PON1 is a multifunctional antioxidant enzyme that can also detoxify the homocysteine metabolite, homocysteine thiolactone (HTL), which can pathologically cause protein damage by homocysteinylation of the lysine residues, thereby leading to atherosclerosis. We demonstrated that moderate alcohol up regulates liver PON1 gene expression and serum activity, whereas heavy alcohol consumption had the opposite effects in both animal models and in humans. The increase in PON1 activity in light drinkers was not due to preferential distribution of high PON1 genotype in this group. It is well known that wine consumption in several countries shows a remarkable inverse correlation to local rates of CAD mortality. Significantly, apart from its alcohol content, red wine also has polyphenols such as quercetin and resveratrol that are also known to have cardioprotective effects. We have shown that quercetin also up regulates PON1 gene in rats and in human liver cells. The action of quercetin seems to be mediated via the active form of the nuclear lipogenic transcription factor, sterol-regulatory element-binding protein 2 (SREBP2) that is translocated from endoplasmic reticulum to the nucleus. However, the mechanism of action of ethanol-mediated up-regulation of PON1 gene remains to be elucidated. We conclude that both moderate ethanol and quercetin, the two major components of red wine, exhibit cardioprotective properties via the up-regulation of the antiatherogenic gene PON1.
Keywords: Coronary artery disease, Paraoxonase, Homocysteine thiolactonase, Sterol-regulatory element-binding protein, Ethanol, Quercetin
Introduction
While the deleterious effects of chronic heavy ethanol consumption on liver have been well studied and documented, its beneficial versus harmful effects on the cardiovascular system is bimodal. We have previously reviewed the health risks and potential benefits of moderate alcohol consumption, with particular focus on the areas of cardiovascular disease, breast cancer, obesity, birth defects, breastfeeding and aging [1], while a more recent review [2] has summarized the benefits of moderate alcohol consumption even in diabetic subjects. Thus, light to moderate drinking is cardioprotective, whereas heavy drinking is correlated with cardiovascular abnormalities. The main goal of this review is to present the current status of the prevalence of coronary artery disease (CAD) in moderate versus heavy drinkers with special emphasis on the antiatherogenic enzyme, paraoxonase, and its gene regulation by ethanol and flavonoids, mainly quercetin and resveratrol, the main components of red wine.
Alcohol and HDL versus LDL
It is now well known that CAD is the principal cause of mortality and morbidity in developed countries, and several features of this metabolic disorder are due to the accumulation of low-density lipoprotein (LDL), the atherogenic lipoprotein. The role of oxidative stress as a major contributor to the atherogenic process has been elegantly reviewed [3, 4]. Thus, oxidation of LDL to form oxidized LDL (OxLDL) results in its massive uptake by peripheral macrophages (i.e. scavenger pathway), leading to the formation of foam cells. The accumulation of these foam cells in the intima of the arterial wall results in a gradual decrease in arterial lumen and eventually occlusion of the artery causing myocardial infarction (MI). On the other hand, high-density lipoprotein (HDL) is antiatherogenic because of its ability to remove cholesterol from peripheral tissues to the liver for degradation, a process called “Reverse Cholesterol Transport” (RCT).
Numerous cross-sectional and intervention studies including ours have documented an increase in the plasma HDL-C concentration as a result of chronic moderate ethanol consumption [5–8]. Correcting for smoking as another risk factor, it has been found that a strong negative correlation still exists between moderate alcohol consumption and the incidence of CAD [9–11]. There are conflicting reports with regard to whether HDL2 or HDL3 subfraction is increased after moderate alcohol intake [12–14]. According to the current concept, relatively lipid-poor HDL3 acquires free-cholesterol and other phospholipids from the peripheral tissues. In the blood compartment, the free-cholesterol component of HDL3 is esterified by lecithin cholesterol acyltransferase (LCAT) to yield lipid-rich HDL2, which is efficiently taken up by the liver via the HDL receptor, scavenger receptor class B1 (SRB1). Significantly, both HDL2 and HDL3 fractions are markedly decreased in severe alcohol-induced liver diseases [15]. Furthermore, heavy alcohol drinkers do not seem to be protected against CAD [16]. Our ongoing studies have established that chronic ethanol markedly decreased the ApoE content of plasma HDL [17], and this has been confirmed by others [18]. Furthermore, we have shown that the RCT function of HDL is impaired in both chronic alcohol-fed rats [19] and human alcoholics [20].
It has been shown that LDL oxidation is increased in regular alcohol abusers [21]. Acetaldehyde, the first metabolite of ethanol, also modifies lysine residues of LDL [22], and the product is rapidly catabolized in the plasma [23]. Since modified LDL is taken up by macrophages via the scavenger pathway, it is reasonable that the ethanol-mediated increase in modified LDL (either by peroxidative products HNE and MDA or by acetaldehyde, the first product of ethanol oxidation) could be more atherogenic than native LDL. Our studies [24] showed that cholesterol uptake by the macrophage system from acetaldehyde-modified LDL was similar to that from HNE-modified LDL.
Ethanol and lipid peroxidation
Ethanol, in addition to its normal oxidation by the alcohol dehydrogenase (ADH) pathway, is also oxidized by the liver microsomal ethanol-oxidizing system (MEOS) pathway [25] by an ethanol-inducible cytochrome P-450 (Cyp2E1). This contributes to ethanol tolerance and forms toxic-free radicals. The role of free radicals in the manifestation of alcohol-mediated liver damage has been recognized ever since DiLuzio et al. [26–28] showed that antioxidants protected rats from the deleterious effects of fatty liver induced by even an acute dose of ethanol. Cederbaum [29] has pointed out that the formation of hydroxyethyl free radicals during the oxidation of ethanol may cause more damage in biological systems than the hydroxyl radical alone. All these studies point out the importance of lipid peroxidation in the alcohol-mediated human diseases. All of these aspects have been reviewed [30, 31]. Highly reactive aldehydes such as 4-hydroxynonenal (HNE) and malondialdehyde (MDA), generated during the peroxidative process, conjugate with the lysine residues of Apo B (the protein component of LDL) leading to the formation of oxidized LDL (OxLDL), which has a strong emission maximum at 430 nm when excitation is performed at 360 nm [32]. Thus, the formation of OxLDL can be quantitatively monitored fluorimetrically. LDL oxidation in vitro can also be more easily performed by monitoring the formation of conjugated dienes spectrophotometrically at 230 nm [33].
Alcohol and CAD
Whereas heavy drinking is associated with higher prevalence of cardiomyopathy, [34–36], hypertension [37], hemorrhagic stroke [38] and cardiac dysrythmias [39], lighter drinking in many population studies cited in recent reports [40, 41] is related to lower prevalence of CAD. In several other studies of cardiovascular mortalities [42, 43], abstainers and heavy drinkers are at higher risk than light or moderate drinkers, possibly because of favorable effects of moderate alcohol on circulating high-density lipoproteins (HDL) level. The composite of this disparate relation in several population studies of cardiovascular mortality has been a “U-” or a “J-”shaped curve. The possibility that lighter alcohol use protects against CAD is supported by plausible hypothetical mechanisms. These include a favorable effect on HDL cholesterol concentration [44, 45] and apolipoproteins [45, 46]. A number of studies have shown the antiatherogenic effects and decreased incidence of peripheral arterial disease [47], a result of moderate drinking based on coronary angiography [48], coronary calcium evaluated by computerized tomography [49], ultrasound imaging of carotid artery [50]. A widely publicized [51] hypothesis was that many abstainers are former heavy drinkers who abstain because of symptoms (sick quitters), CAD diagnosis or other traits that predispose to CAD. Thus, several studies have clearly demonstrated significant reduction in CAD risk and in the incidence of myocardial infarction (MI) as a result of moderate alcohol intake regardless of the gender [52–55]. Significantly, light to moderate drinking seems to reduce the incidence of MI not only in diabetics with known CAD and in a subpopulation that had healthy lifestyle habits such as eating health foods, exercising approximately 30 min/day, no smoking and body mass index <25 kg/m2, but also in hypertensive subjects [55, 56]. The benefits of moderate drinking to reduce heart failure have been summarized [57]. However, it must be pointed out that even two drinks/day can substantially increase the blood pressure in hypertensive subjects [58].
Frequency of ethanol intake in cardioprotection
Moderate alcohol intake has been shown to improve cardiovascular health regardless of the gender, in contrast to intermittent drinking [53, 59–62]. Thus, daily intake of moderate alcohol has been shown to reduce CAD risk by 37% compared to alcohol consumption just once a week [53]. This has been attributed to alcohol-mediated improvement in insulin sensitivity and HDL cholesterol [60]. It is possible that a better postprandial glucose metabolism associated with light to moderate drinking may be responsible for the benefits associated with moderate drinking prior to or along with meals [61]. In contrast, it should be recognized that occasional drinking as well as binge drinking increase risk of MI and other all-cause mortality [61–63]. It is significant to point out that there was a 2-fold increase in MI in subjects who consumed at least five drinks per day compared to non-drinkers [64]. Cardioprotective dosage of alcohol intake is considered to be 1 or two drinks per day for men and one drink per day for women [53, 65, 66]. A drink is equivalent to approximately 14 g of ethanol, which would be equivalent to 12 oz beer or 5 oz wine or 1.5 oz 80-proof spirits. Again, it must be emphasized that the cardioprotective effects of ethanol is manifested generally when it is consumed in moderate amounts on a daily basis [67]. Nonetheless, because of its addictive nature, caution must be exercised in recommending daily moderate intake of alcohol unless there is no family history of alcohol abuse in spite of the known CVD protection by moderate drinking [53]. Unfortunately, it is impossible to predict the susceptibility of any individual to become alcohol-dependent [47]. Binge drinking as well as alcohol abuse have been reported to have risen in recent years [1]. More importantly, heavy drinking is responsible not only for traffic accidents, but also for the increased incidence of cardiovascular complications, alcoholic liver diseases leading to fibrosis and cirrhosis, breast and GI tract cancers and all-cause mortality [1, 61–63]. It is a well known fact that alcohol abuse is the root cause for innumerable number of individuals ruining their lives and associated burden to the immediate families and the society at large. As a result, prospective randomized clinical trials have been difficult to carry out to truly evaluate the cardioprotective effects of moderate alcohol.
Does alcohol per se or do flavonoid components of alcoholic beverages also protect against heart disease?
A number of studies have reported that alcohol per se has significant protective effect against vascular disease in its own right [53, 59, 68–71]. These effects can probably be attributed to the potential for alcohol to increase protective HDL cholesterol levels and decrease platelet aggregation. However, the possibility of other components, particularly the bioflavonoids in red wine [72] could also confer its cardioprotective property. The Zutphen Elderly Study [73] assessed the flavonoids intake of 805 men aged 65–84 in 1985 and followed them up for 5 years. The flavonoids intake analyzed in tertiles was significantly inversely associated with death from coronary heart disease (P = 0.015) and showed a trend toward an inverse association with myocardial infarction (P = 0.08). The relative risk of coronary heart disease in the highest versus the lowest tertile of flavonoids intake was 0.42 (95% Cl 0.20–0.88). This relationship persisted after controlling for all other relevant coronary risk factors. Knekt et al. [74] studied 5,133 Finnish men and women aged 30–69 recruited between 1967 and 1972. The flavonoids intake was calculated from the reported dietary recall of subjects for the year prior to entry into the study and then related to coronary and total mortality over the subsequent 26 years. For women, there was a significant inverse gradient of risk for coronary and total mortality with flavonoids intake. The relative risk between the highest and lowest quarters of intake after adjusting for other coronary risk factors was 0.69 (95% Cl 0.53–0.90) for total mortality and 0.54 (95% Cl 0.33–0.87) for coronary mortality. For men, the corresponding values were 0.76 (95% Cl 0.63–0.93) and 0.78 (95% Cl 0.56–1.08). It was suggested that since the intake of vitamin C in the Finnish diet was low, dietary flavonoids might offer an alternative source of antioxidants.
Red wine protects against heart disease: the French paradox
Flavonoids are derived from many sources in the human diet including fruit, vegetables, red wine and tea. Red wine is a particularly rich source of flavonoids. Previous calculations have suggested that the addition of two glasses of red wine to the Western diet will increase its flavonoids content by 40% [74]. Studying the potential impact of red wine flavonoids on coronary heart disease is complicated by the presence of other wine constituents such as alcohol and sugars. More importantly, light drinking favors the destruction of OxLDL by up-regulation of antiatherogenic enzyme, paraoxonase (PON1), as shown by us [24].
However, there have been many claims that there may be benefits associated with the flavonoids content of red wine over and above the effect of alcohol. One of the earliest experiments to suggest this examined the effect of feeding rabbits a high cholesterol diet for 3 months while also administering alcohol, beer, white wine, red wine or water. These beverages reduced the atherosclerotic lesions over the subsequent 3 months to 75, 83, 67 and 40%, respectively, of those found in the water-drinking controls [75].
The epidemiological evidence for a specific protective effect of flavonoid-rich alcoholic beverages is rather more confused [76]. In most countries, intakes of saturated fat are directly associated with mortality from coronary heart disease. However, some countries appear to defy this general association. The most notable exception is France where in spite of high fat intakes, there has been a low incidence of coronary heart disease [77]. This circumstance has come to be known as the ‘French Paradox’ and has stimulated interest in local lifestyle factors that may protect the French against heart disease. A likely candidate was the preference of the French for regular consumption of red wine that offers not only the benefits of moderate alcohol consumption but also the potential benefits of a high flavonoids intake. Indeed, it has been reported that wine consumption in several countries shows a remarkable inverse correlation to local rates of coronary heart disease mortality [78]. It must, however, be cautioned that smoking combined with drinking may predispose such individuals to esophageal cancer, while excessive drinking is likely to lead to liver diseases. More recently, there have been reports showing the preservation of serum PON activity and protection against LDL oxidation by wine flavonoids in mice [79, 80]. A recent clinical trial demonstrated the beneficial effects of grape extract on the susceptibility of LDL oxidation in heavy smokers [81].
Central role of paraoxonase
In mammals, the paraoxonase gene family includes at least 3 members: PON1, PON2 and PON3 [82]. PON1 is the most predominant one among these that is tightly associated with HDL and has been shown to play a major role in the protective role of HDL against CAD [83]. Specifically, PON1 is believed to (i) prevent the oxidation of LDL to OxLDL and (ii) destroy the OxLDL to biologically inactive products. It is a calcium-dependent HDL-associated ester hydrolase that catalyzes the hydrolysis of organophosphates, aromatic carboxylic acid esters and carbamates [83].
It is now well known that PON1 is tightly associated with apolipoprotein A-I in HDL and has the highest activity in the liver and blood [83]. It has also been shown that PON is also associated with Apo J and, in fact, copurifies during the purification of Apo J. Serum PON1 activity varies widely between different animal species and among humans [84, 85]. It has also been shown that individuals with familial hypercholesterolemia and insulin-dependent diabetes mellitus have significantly lower levels of PON1 than do normal control individuals [86]. A low level of HDL-associated PON1 is also correlated with susceptibility to myocardial infarction, fish eye disease and tangier disease [87, 88]. A recent study [89] showed that aspirin markedly elevated PON1 activity both in mice and in rat hepatocytes. Most importantly, HDL-associated PON1 has also been reported to inhibit copper-induced lipid peroxidation in LDL [90]. PON2 and PON3 are two other variants that have also been shown to be very effective in protecting against LDL oxidation [91, 92]. However, PON2 has not been detectable in either HDL or VLDL fraction of plasma [91]. Although PON3 has been found in HepG2 cells [92] and rabbit serum, it has been estimated to be much less abundant in rodent and human serum when compared to that of PON1 [92]. Further, unlike PON1, PON3 is not regulated by oxidized lipids [93]. In view of all these, the physiological significance of PON2 and to some extent PON3 in the blood, when compared to that of PON1, in cardioprotection remains to be seen.
Paraoxonase is a multifunctional antiatherogenic enzyme
Paraoxonase is a multifunctional antioxidant enzyme tightly associated with HDL that exhibits not only the capacity to prevent LDL oxidation and destroy oxidized LDL [94–97] but also can detoxify the homocysteine metabolite, homocysteine thiolactone (HTL), which can pathologically cause protein damage by homocysteinylation of the lysine residues, thereby leading to atherosclerosis [98, 99]. The importance of PON1 with respect to cardiovascular disease (CVD) is supported by our demonstration that moderate but not heavy alcohol intake in both animals and humans up regulates PON1 gene and activity accompanied by increased protection capacity of plasma HDL against LDL oxidation [24]. These results are consistent with the reports of increased serum PON1 activity in moderate drinkers [100]. Subsequently, we [101] and others [102] have shown a strong correlation between decreased homocysteine thiolactonase (HCTL) activity and the severity of CVD in type II diabetics.
Regulation of PON1 by sterol-regulatory element-binding proteins
Sterol-regulatory element-binding proteins (SREBPs) have been recognized as a new class of membrane-bound proteins that modulate lipid homeostasis [103]. Currently, three types of SREBPs exist, namely SREBP1a, SREBP1c and SREBP2. While SREBP1a and SREBP1c seem to control fatty acid pathway, SREBP2 regulates cholesterol biosynthetic pathway. SREBP1a and SREBP2 are present in most cultured cell lines, while SREBP1c and SREBP2 are present in liver and most intact tissues. Newly synthesized SREBP is inserted into the ER as an inactive protein. When the cellular cholesterol is low, SREBP is escorted into the Golgi by SREBP cleavage-activating protein (SCAP) where it is proteolytically cleaved by specific proteases S1P and S2P in a two-step process to yield the mature SREBP that is translocated into the nucleus, where it activates transcription by binding to specific SREs in the promoter/enhancer regions of multiple target genes. A previous report [104] indicated that simvastatin, in a dose-dependent manner, up regulated the promoter of PON1 gene by increasing SREBP2. But others have reported quite the opposite effect of statins on the PON1 gene regulation [105]. This controversy of PON1 gene regulation has been further complicated by another report showing that dietary polyphenols up regulate PON1 gene expression by aryl hydrocarbon receptor (AhR)-dependent mechanism [106]. Besides PON1 gene regulation via SREBP2 interaction, PON1 gene is also reported to be regulated by Sp1 and protein kinase C (PKC) alpha or zeta, which interacts with the consensus Sp1-binding site in PON1 promoter −269 to −97 bp upstream of transcription initiation site. Over expression of Sp1 dramatically enhances PON1 promoter activity, whereas over expression of PKC significantly reduces PON1 promoter activity [107].
Possible mechanism of action of ethanol
The reduced risk of coronary artery disease associated with moderate alcohol consumption may be explained by its ability to increase plasma HDL [108]. Apart from this, moderate ethanol increases PON1, an HDL-associated antiatherogenic enzyme, that has its cardioprotective action because it (1) hydrolyzes oxidized lipids in OxLDL in serum and macrophages, a prerequisite for the onset of atherosclerosis, (2) inhibits cholesterol uptake by macrophages from OxLDL [24, 108, 109], (3) attenuates macrophage cholesterol biosynthesis and (4) stimulates macrophage cholesterol efflux [20, 108–111]. Light ethanol feeding caused a 20–25% increase in PON activity in both serum and liver and a 59% increase in the level of liver PON mRNA compared with pair-fed control rats [24]. Light to moderate alcohol consumption in humans increases the activity of paraoxonase in serum, and the enzymatic activity was strongly correlated with concomitant increases in concentrations of HDL-C and Apo A-I [112]. In humans, light drinking up regulates, whereas heavy drinking down regulates PON activity and its expression, irrespective of its genetic polymorphism [24]. Consequently, PON1 activity is a more reliable predictor of vascular disease status than PON1 genotype. Thus, increased serum paraoxonase may be an important component of the mechanisms underlying the reduction in coronary heart disease following moderate alcohol consumption [113, 114]. However, heavy alcohol consumption (70–90 g/d) resulted in a significant decrease in PON1 and protein thiols, and a significant increase in AST, ALT and GGT levels [115]. It is well known that PON1 loses its activity in the oxidative environment. Therefore, any factors that affect the status of oxidative stress will also affect PON1 activity status. For example, antiphospholipid antibodies increase oxidative stress in experimental mouse model with decreased PON activity [108]. On the other hand, statins commonly used for hypercholesterolemia increase serum PON1 activity by reducing oxidative stress [104].
Possible mechanism of action of polyphenols
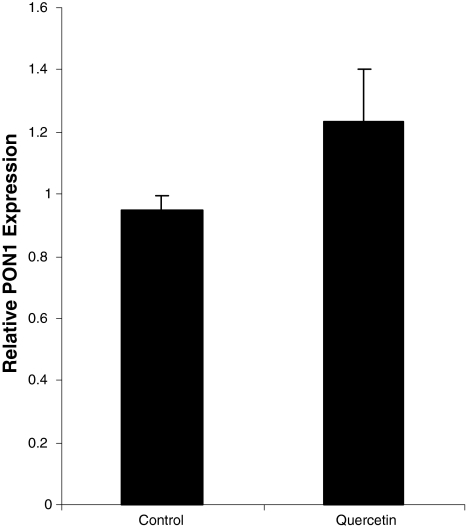
We have recently demonstrated [116] that dietary quercetin markedly up regulates hepatic PON1 expression (Fig. 1) accompanied by stimulation of PON1 activity (Table 1) as well as HCTL activity (Table 2) with concomitant increased protection capacity of HDL against LDL oxidation (Table 3). The increase in PON activity may be partially explained by the ability of quercetin to reduce oxidative stress by scavenging oxidative-free radicals. In this regard, our ongoing studies have demonstrated that supplementation of betaine in chronic alcohol-fed rats on high ω3-PUFA diet restored not only serum PON1 activity but also liver GSH, the natural antioxidant [117]. However, our findings clearly indicate that the action of quercetin is not merely because of its antioxidative properties. The fact that hepatic PON1 mRNA level is also increased by 35% (P < 0.01) implies that the action of quercetin must be at the molecular level either at the transcription rate of PON1 gene or at the stabilization of PON1 mRNA. Our ongoing studies (unpublished) in human liver cells seem to indicate that quercetin up regulates PON1 gene via the activation and nuclear translocation of mature SREBP2, which then interacts with SRE elements of PON1 promoter to stimulate its activity. Resveratrol, another polyphenolic compound in red wine, has been reported to have angiogenic and antihypercholesterolemic and antidiabetic effects [118]. The cardioprotective effects of resveratrol was ascribed to increased expression of phospho-Akt, Bcl-2, eNOS, iNOS, COX-1, COX-2, Trx-1 and Trx-2 [119]. In addition, resveratrol inhibits cardiac hypertrophy via AMPK and Akt [119]. Work is currently in progress to elucidate the possible mechanism of actions of ethanol and quercetin in the up-regulation of PON1 at the molecular level.
Fig. 1.
Influence of quercetin feeding on the expression of rat PON1 mRNA relative to that of actin mRNA by real-time RT-PCR. A sample of the liver from both control and quercetin-fed groups was analyzed for PON1 mRNA and actin mRNA by real-time RT-PCR, and the relative abundance of PON1 mRNA was determined. Each bar is the mean ± SD of six independent experiments
Table 1.
Influence of quercetin feeding on serum and liver PON1 activity
| Group | Serum PON1 activity (nmol paraoxon hydrolyzed/ml/min) | P value | Liver PON1 activity (nmol paraoxon hydrolyzed/g/min) | P value |
|---|---|---|---|---|
| Control | 50.13 ± 3.5 | 41.9 ± 13.7 | ||
| Quercetin | 64.53 ± 9.1 | <0.05 | 65.69 ± 8.2 | <0.01 |
Serum and liver PON1 enzyme activity was determined with paraoxon (Sigma–Aldrich Inc., St. Louis, MO) as the substrate essentially as described by us previously [23]. Results were expressed as IU. One unit of international enzyme activity was equal to 1 nmol of paraoxon hydrolyzed per minute per ml of serum or per g equivalent of liver microsomes
Table 2.
Influence of quercetin feeding on Serum HCTL activity
| Group | Serum HCTL activity (nmol HCTL hydrolyzed/ml/min) | P value |
|---|---|---|
| Control | 6.97 ± 0.52 | |
| Quercetin | 8.57 ± 0.61 | <0.05 |
Serum HCTL activity was determined in an aliquot of the serum of each animal from both control and quercetin-fed groups. Serum HCTL activity was determined essentially as described by us previously [24]. Each value is the mean ± SD of six independent determinations
Table 3.
Influence of quercetin feeding on lag time of LDL oxidation by serum HDL
| Group | Lag time of LDL oxidation (min) | P Value |
|---|---|---|
| Control | 67.3 ± 4.2 | |
| Quercetin | 224.1 ± 1.6 | <0.001 |
HDL was isolated from each animal from both control and quercetin-fed groups, and the lag time for its ability to prolong LDL oxidation was determined. Each value is the mean ± SD of six independent determinations
Summary
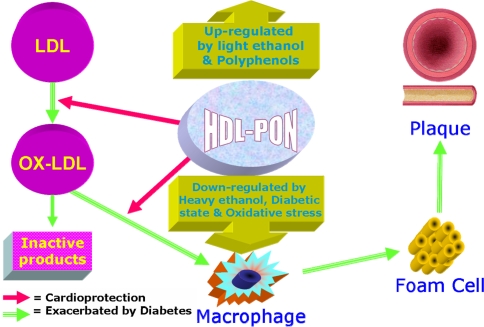
Based on the comprehensive survey of the current literature and on our own studies, we have summarized the current status of beneficial versus deleterious effects of alcohol/polyphenol with respect to cardioprotection in Fig. 2 below: Accordingly, oxidative stress leads to the oxidation of LDL to form oxidized LDL (OxLDL) that is preferentially taken up by peripheral macrophages via the scavenger receptor pathway forming the foam cells. These cholesterol-laden foam cells accumulate in the intima of the arterial wall leading to occlusion of the artery causing MI. PON1 is an antiatherogenic enzyme that is able to inhibit the oxidation of LDL as well as convert the OxLDL to inactive products. Significantly, when consumed in moderate amounts, ethanol and quercetin, the two major wine components, up regulate PON1 gene and associated increased PON1 activity, and thereby confer cardioprotection. In contrast, heavy ethanol consumption, increased oxidative stress and diabetic conditions have quite the opposite effects on cardioprotection by down regulating PON1 gene.
Fig. 2.
Alcohol, polyphenols and PON in CAD protection
Acknowledgments
This work was supported by grants from VA Merit Review as well as from NIH (M.R. Lakshman). Authors gratefully acknowledge the Editors of the journal “Biochemical Biophysical Research Communications” for giving permission to reproduce some of the tables and figures reproduced in this review article.
References
- 1.Gunzerath L, Faden V, Zakhari S, Warren K. National Institutes on alcohol abuse and alcoholism report on moderate drinking. Alcohol Clin Exp Res. 2004;28(6):829–847. doi: 10.1097/01.alc.0000128382.79375.b6. [DOI] [PubMed] [Google Scholar]
- 2.O’Keefe JH, Bybee KA, Lavie CJ. Alcohol and cardiovascular health. J Am Col Cardiol. 2007;50:1009–1014. doi: 10.1016/j.jacc.2007.04.089. [DOI] [PubMed] [Google Scholar]
- 3.Parthasarathy S, Rankin SM. Role of oxidized LDL in atherogenesis. Prog Lipid Res. 1992;31:127–143. doi: 10.1016/0163-7827(92)90006-5. [DOI] [PubMed] [Google Scholar]
- 4.Chisolm GM, Steinberg D. The oxidative modification hypothesis of atherogenesis: an overview. Free Rad Biol Med. 2000;28:1815–1826. doi: 10.1016/S0891-5849(00)00344-0. [DOI] [PubMed] [Google Scholar]
- 5.Lakshman MR, Reda D, Materson BJ. Plasma lipid and lipoprotein profiles in hypertensive black vs white men. Am J Cardiol. 1996;78:1236–1241. doi: 10.1016/S0002-9149(96)00602-9. [DOI] [PubMed] [Google Scholar]
- 6.Belfrage P, Berg B, Hagerstrand I, Nilsson-Ehle P. Alterations of lipid metabolism in healthy volunteers during long-term ethanol intake. Eur J Clin Invest. 1977;7(2):127–131. doi: 10.1111/j.1365-2362.1977.tb01584.x. [DOI] [PubMed] [Google Scholar]
- 7.Hulley SB, Cohen R, Widdowson G. Plasma high density lipoprotein cholesterol level- influence of risk factor intervention. J Am Med Assoc. 1977;238(21):2269–2271. doi: 10.1001/jama.238.21.2269. [DOI] [PubMed] [Google Scholar]
- 8.Jacqueson A, Richard JL, Ducimetiere P, Warnet JM, Claude JR. HDL cholesterol and alcohol consumption in a French male population. Atherosclerosis. 1983;48(2):131–138. doi: 10.1016/0021-9150(83)90099-0. [DOI] [PubMed] [Google Scholar]
- 9.Klatsky AL, Freidman GD, Siegelaub AB. Alcohol consumption before myocardial infarction. Ann Intern Med. 1974;81:294–301. doi: 10.7326/0003-4819-81-3-294. [DOI] [PubMed] [Google Scholar]
- 10.Barboriak JJ, Rimm AA, Anderson AJ, Schmidhoffer M, Tristani FE. Coronary artery occlusion and alcohol intake. Br Heart J. 1977;39:289–293. doi: 10.1136/hrt.39.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Masarei JRL, Puddey IL, Rouse WJ. Effects of alcohol consumption on serum lipoprotein-lipid and apolipoprotein concentrations. Atherosclerosis. 1986;60:79–87. doi: 10.1016/0021-9150(86)90090-0. [DOI] [PubMed] [Google Scholar]
- 12.Haskell WL, Camargo C, Jr, Williams PT. Effect of cessation and resumption of moderate alcohol intake on serum HDL subfractions. N Engl J Med. 1984;310:805–810. doi: 10.1056/NEJM198403293101301. [DOI] [PubMed] [Google Scholar]
- 13.Hartung GH, Foreyt JP, Mitchell RE, Mitchell JG, Reeves RS, Gotto AM. Effect of alcohol intake on HDL cholesterol levels in runners and inactive men. JAMA. 1983;249:747–750. doi: 10.1001/jama.249.6.747. [DOI] [PubMed] [Google Scholar]
- 14.Cushman P, Barboriak J, Kalbfleisch J. Alcohol: high density lipoproteins, apolipoproteins. Alcohol Clin Exp Res. 1986;10(2):154–157. doi: 10.1111/j.1530-0277.1986.tb05063.x. [DOI] [PubMed] [Google Scholar]
- 15.Lieber CS. To drink “moderately” or not to drink? N Engl J Med. 1984;310:846–848. doi: 10.1056/NEJM198403293101309. [DOI] [PubMed] [Google Scholar]
- 16.Kagan A, Yano K, Rhoads GC, et al. Alcohol and cardiovascular disease: the Hawaiian experience. Circulation. 1981;64(3 Pt 2):III 27–III 31. [PubMed] [Google Scholar]
- 17.Lakshman MR, Chirtel SC, Chamber LC. Roles of ω3-fatty acids and ethanol on the regulation of plasma and liver lipids and apo A-I and E in rats. J Nutr. 1988;118:1299–1303. doi: 10.1093/jn/118.11.1299. [DOI] [PubMed] [Google Scholar]
- 18.Lin RC, Lumeng L, Phelps VL. Serum HDL particles of alcohol fed rats are deficient in apolipoprotein E. Hepatology. 1989;9:307–313. doi: 10.1002/hep.1840090224. [DOI] [PubMed] [Google Scholar]
- 19.Marmillot P, Rao MN, Liu Q-H, Chirtel SJ, Lakshman MR. Effect of dietary ω3-fatty acids & ethanol consumption on RCT in rats. Metabolism. 2000;49:508–512. doi: 10.1016/S0026-0495(00)80017-7. [DOI] [PubMed] [Google Scholar]
- 20.Rao MN, Marmillot P, Seeff LB, Strader DB, Lakshman MR. HDL from human alcoholics exhibit impaired RCT function. Metabolism. 2000;49:1406–1410. doi: 10.1053/meta.2000.17728. [DOI] [PubMed] [Google Scholar]
- 21.Croft KD, Puddey IB, Rakic V, Abu-Amsha R, et al. Oxidative susceptibility of LDL-influence of regular alcohol use. Alcohol Clin Exp Res. 1996;20(6):980–984. doi: 10.1111/j.1530-0277.1996.tb01934.x. [DOI] [PubMed] [Google Scholar]
- 22.Kervinen K, Savolainen MJ, Kesaniemi YA. LDL derivatization by acetaldehyde affects lysine residues & B/E receptor binding affinity. Alcohol Clin Exp Res. 1991;15(6):1050–1055. doi: 10.1111/j.1530-0277.1991.tb05210.x. [DOI] [PubMed] [Google Scholar]
- 23.Kesaniemi YA, Kervinen K, Meittinen TA. Acetaldehyde modification of low density lipoprotein accelerates its catabolism in man. Eur J Clin Invest. 1987;17:29–36. doi: 10.1111/j.1365-2362.1987.tb01222.x. [DOI] [PubMed] [Google Scholar]
- 24.Rao MN, Marmillot P, Palmer DA, Seeff LJ, Strader DB, Lakshman MR. Light, but not heavy alcohol drinking stimulates paraoxonase by up regulating liver PON mRNA in both rats and humans. Metabolism. 2003;52:1287–1294. doi: 10.1016/S0026-0495(03)00191-4. [DOI] [PubMed] [Google Scholar]
- 25.Ohnishi K, Lieber CS. Reconstitution of microsomal ethanol-oxidizing system. J Biol Chem. 1977;252:7124–7131. [PubMed] [Google Scholar]
- 26.DiLuzio NR. Prevention of the acute ethanol-induced fatty liver by the simultaneous administration of antioxidants. Life Sci. 1964;3:113–118. doi: 10.1016/0024-3205(64)90189-4. [DOI] [PubMed] [Google Scholar]
- 27.DiLuzio NR, Costales F. Inhibition of ethanol and carbon tetrachloride induced fatty liver by antioxidants. Exp Mol Pathol. 1965;4:141–154. doi: 10.1016/0014-4800(65)90030-4. [DOI] [PubMed] [Google Scholar]
- 28.DiLuzio NR, Kalish GH. Enhanced peroxidation of lipid in the pathogenesis ethanol induced liver injury. Gastroenterology. 1966;50:392–396. [Google Scholar]
- 29.Cederbaum AJ. Microsomal generation of hydroxyl radicals: its role in microsomal ethanol oxidizing system (MEOS) activity and requirement for iron. Ann N Y Acad Sci. 1987;492:35–49. doi: 10.1111/j.1749-6632.1987.tb48651.x. [DOI] [PubMed] [Google Scholar]
- 30.Ahmad FF, Cowan DL, Sun AY. Spin trapping and lipid peroxidation. In: Sun GY, Wood WG, Sun AY, editors. Molecular mechanisms of alcohol. Clifton: Humana Press; 1989. pp. 257–278. [Google Scholar]
- 31.Reinke LA, McCay PB. Alcohol and free radicals. In: Watson RR, editor. Liver pathology and alcohol. Clifton: Humana Press; 1991. pp. 133–168. [Google Scholar]
- 32.Esterbauer H, Jurgens G, Quenhenberger O. Autoxidation of human LDL. J Lip Res. 1987;28:495–509. [PubMed] [Google Scholar]
- 33.Esterbauer H, Striegl G, Puhl H, Rotheneder M. Continuous monitoring of in vitro oxidation of human low density lipoprotein. Free Radic Res Commun. 1989;6:67–75. doi: 10.3109/10715768909073429. [DOI] [PubMed] [Google Scholar]
- 34.Klatsky AL. Alcohol and the cardiovascular system. Ann Rev Nutr. 1982;2:51–71. doi: 10.1146/annurev.nu.02.070182.000411. [DOI] [PubMed] [Google Scholar]
- 35.Regan TJ. Alcoholic cardiomyopathy. Prog Cardiovasc Dis. 1984;27:141–152. doi: 10.1016/0033-0620(84)90001-X. [DOI] [PubMed] [Google Scholar]
- 36.Urbano-Marquez A, Estrich R, Navarro-Lopez F. The effects of alcoholism on skeletal and cardiac muscle. N Engl J Med. 1989;320:409–415. doi: 10.1056/NEJM198902163200701. [DOI] [PubMed] [Google Scholar]
- 37.Klatsky AL. In hypertension: pathophysiology, diagnosis and management. New York: Raven Press; 1990. pp. 277–294. [Google Scholar]
- 38.Donahue RP, Abbott RD, Reed DW, et al. Alcohol and hemorrhagic stroke. The Honolulu heart program. JAMA. 1986;255:2311–2314. doi: 10.1001/jama.255.17.2311. [DOI] [PubMed] [Google Scholar]
- 39.Ettinger PO, Wu CF, Cruz C, et al. Arrhythmias and the “Holiday Heart”: alcohol-associated cardiac rhythm disorders. Am Heart J. 1978;95:555–562. doi: 10.1016/0002-8703(78)90296-X. [DOI] [PubMed] [Google Scholar]
- 40.Stampfer MJ, Colditz GA, Willet WC. A study of moderate alcohol consumption and the risk of coronary disease and stroke in women. N Engl J Ed. 1988;319:267–273. doi: 10.1056/NEJM198808043190503. [DOI] [PubMed] [Google Scholar]
- 41.Klatsky AL, Armstrong MA, Friedman GD. Relations of alcoholic beverage use to subsequent coronary artery disease hospitalization. Am J Cardiol. 1986;58:710–714. doi: 10.1016/0002-9149(86)90342-5. [DOI] [PubMed] [Google Scholar]
- 42.Yano K, Rhoads GG, Kagan A. Coffee, alcohol and risk of coronary heart disease among Japanese men living in Hawaii. N Engl J Med. 1977;297:405–409. doi: 10.1056/NEJM197708252970801. [DOI] [PubMed] [Google Scholar]
- 43.Scragg R, Stewart A, Jackson R. Alcohol and exercise in myocardial infarction and sudden coronary death in men and women. Am J Epidemiol. 1987;126:77–85. doi: 10.1093/oxfordjournals.aje.a114664. [DOI] [PubMed] [Google Scholar]
- 44.Castelli WP, Doyle JT, Gordon T, et al. Alcohol and blood lipids. The cooperative lipoprotein phenotyping study. Lancet. 1977;2:153–155. doi: 10.1016/S0140-6736(77)90176-3. [DOI] [PubMed] [Google Scholar]
- 45.Cauley JA, Kuller LH, LaPorte RE. Studies on the association between alcohol and HDL cholesterol: possible benefits and risks. Adv Alcohol Subst Abuse. 1987;6:53–67. doi: 10.1300/J251v06n03_06. [DOI] [PubMed] [Google Scholar]
- 46.Moore RD, Smith CR, Kwiterovich PO, Pearson TA. Effect of low-dose alcohol use versus abstention on apolipoproteins A-I and B. Am J Med. 1988;84:884–896. doi: 10.1016/0002-9343(88)90067-8. [DOI] [PubMed] [Google Scholar]
- 47.Lucas DL, Brown RA, Wassef M, Giles TD. Alcohol and the cardiovascular system. J Am Coll Cardiol. 2005;45:1916–1924. doi: 10.1016/j.jacc.2005.02.075. [DOI] [PubMed] [Google Scholar]
- 48.Femia R, Natali A, L’Abbate A, Ferrannini E. Coronary atherosclerosis and alcohol consumption: angiographic and mortality data. Arter Thromb Vasc Biol. 2006;26:1607–1612. doi: 10.1161/01.ATV.0000222929.99098.1f. [DOI] [PubMed] [Google Scholar]
- 49.Vliegenthart R, Oei HHS, Elzen APM, et al. Alcohol consumption and coronary calcification in a general population. Arch Intern Med. 2004;164:2355–2360. doi: 10.1001/archinte.164.21.2355. [DOI] [PubMed] [Google Scholar]
- 50.Schminke U, Luedemann J, Berger K, et al. Association between alcohol consumption and subclinical carotid atherosclerosis: the Study of Health in Pomerania. Stroke. 2005;36:1746–1752. doi: 10.1161/01.STR.0000173159.65228.68. [DOI] [PubMed] [Google Scholar]
- 51.Anonymous Alcohol and mortality: myth of U-shaped curve. Lancet. 1988;2:1292–1293. [PubMed] [Google Scholar]
- 52.Kabagambe EK, Baylin A, Ruiz-Narvaez E, Rimm EB, Campos H. Alcohol intake, drinking patterns, and risk of nonfatal acute myocardial infarction in Costa Rica. Am J Clin Nutr. 2005;82:1336–1345. doi: 10.1093/ajcn/82.6.1336. [DOI] [PubMed] [Google Scholar]
- 53.Mukamal KJ, Jensen MK, Grønbæk M, et al. Drinking frequency, mediating biomarkers, and risk of myocardial infarction in women and men. Circulation. 2005;112:1406–1413. doi: 10.1161/CIRCULATIONAHA.105.537704. [DOI] [PubMed] [Google Scholar]
- 54.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (The INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 55.Mukamal KJ, Chiuve SE, Rimm EB. Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Arch Intern Med. 2006;166:2145–2150. doi: 10.1001/archinte.166.19.2145. [DOI] [PubMed] [Google Scholar]
- 56.Beulens JW, Rimm EB, Ascherio A, Spiegelman D, Hendriks HF, Mukamal KJ. Alcohol consumption and risk for coronary heart disease among men with hypertension. Ann Intern Med. 2007;146:10–19. doi: 10.7326/0003-4819-146-1-200701020-00004. [DOI] [PubMed] [Google Scholar]
- 57.Djoussé L, Gaziano JM. Alcohol consumption and risk of heart failure in the Physicians’ Health Study I. Circulation. 2007;115:34–39. doi: 10.1161/CIRCULATIONAHA.106.661868. [DOI] [PubMed] [Google Scholar]
- 58.Beilin LJ, Puddey IB. Alcohol and hypertension: an update. Hypertension. 2006;47:1035–1038. doi: 10.1161/01.HYP.0000218586.21932.3c. [DOI] [PubMed] [Google Scholar]
- 59.Mukamal KJ, Conigrave KM, Mittleman MA, et al. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N Engl J Med. 2003;348:109–118. doi: 10.1056/NEJMoa022095. [DOI] [PubMed] [Google Scholar]
- 60.Veenstra J, Ockhuizen T, Pol H, Wedel M, Schaafsma G. Effects of a moderate dose on blood lipids and lipoproteins postprandially and in the fasting state. Alcohol Alcohol. 1990;25(4):371–377. [PubMed] [Google Scholar]
- 61.Rehm J, Sempos CT, Trevisan M. Alcohol and cardiovascular disease—more than one paradox to consider average volume of alcohol consumption, patterns of drinking and risk of coronary heart disease—a review. J Cardiovasc Risk. 2003;10:15–20. doi: 10.1097/00043798-200302000-00004. [DOI] [PubMed] [Google Scholar]
- 62.Mukamal KJ, Maclure M, Muller JE, Mittleman MA. Binge drinking and mortality after acute myocardial infarction. Circulation. 2005;112:3839–3845. doi: 10.1161/CIRCULATIONAHA.105.574749. [DOI] [PubMed] [Google Scholar]
- 63.Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA. 2003;289:70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- 64.Malyutina S, Bobak M, Kurilovitch S, et al. Relation between heavy and binge drinking and all-cause and CV mortality in Novosibirsk, Russia: a prospective cohort study. Lancet. 2002;360:1448–1454. doi: 10.1016/S0140-6736(02)11470-X. [DOI] [PubMed] [Google Scholar]
- 65.DiCastelnuovo A, Castanzo S, Bagnardi V, Donati MB, Iacoviello L, Gaetano G. Alcohol dosing and total mortality in men and women. Arch Intern Med. 2006;166:2437–2445. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- 66.Bantle JP, et al. Nutrition recommendations and interventions for diabetes—2006: a position statement of the American Diabetes Association. Diabetes Care. 2006;29:2140–2157. doi: 10.2337/dc06-9914. [DOI] [PubMed] [Google Scholar]
- 67.Greenfield JR, Samaras K, Jenkins AB, Kelly PJ, Spector TD, Campbell LV. Moderate alcohol consumption, estrogen replacement therapy, and physical activity are associated with increased insulin sensitivity. Diabetes Care. 2003;26:2734–2740. doi: 10.2337/diacare.26.10.2734. [DOI] [PubMed] [Google Scholar]
- 68.Rimm EB, Giovannucci EL, Willett WC, et al. Prospective study of alcohol consumption and risk of coronary artery disease in men. Lancet. 1991;338(8765):464–468. doi: 10.1016/0140-6736(91)90542-W. [DOI] [PubMed] [Google Scholar]
- 69.Hein HO, Suadicani P, Gyntelberg F. Alcohol consumption, serum low density lipoprotein cholesterol concentration, and risk of ischaemic heart disease: six year follow up in the Copenhagen male study. BMJ. 1996;312(7033):736–741. doi: 10.1136/bmj.312.7033.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lazarus NB, Kaplan GA, Cohen RD, Leu DJ. Change in alcohol consumption and risk of death from all causes & ischaemic heart disease. BMJ. 1991;303(6802):553–556. doi: 10.1136/bmj.303.6802.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Friedman LA, Kimball AW. Coronary heart disease mortality and alcohol consumption in Framingham. Am J Epidemiol. 1986;124(3):481–489. doi: 10.1093/oxfordjournals.aje.a114418. [DOI] [PubMed] [Google Scholar]
- 72.Corder R, Mullent W, Khan NQ, et al. Red wine procyanidins and vascular health. Nature. 2006;444:566. doi: 10.1038/444566a. [DOI] [PubMed] [Google Scholar]
- 73.Hertog MG, Feskens EJM, Hollman P. Dietary antioxidant flavonoids and risk of coronary heart disease: the Zutphen Elderly Study. Lancet. 1993;342(8878):1007–1011. doi: 10.1016/0140-6736(93)92876-U. [DOI] [PubMed] [Google Scholar]
- 74.Knekt P, Jarvinen R, Reunanen A, Maatela J. Flavonoid intake and coronary mortality in Finland: a cohort study. BMJ. 1996;312(7029):478–481. doi: 10.1136/bmj.312.7029.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Klurfeld DM, Kritchevsky D. Differential effects of alcoholic beverages on experimental atherosclerosis in rabbits. Exp Mol Pathol. 1981;34(1):62–71. doi: 10.1016/0014-4800(81)90036-8. [DOI] [PubMed] [Google Scholar]
- 76.Rimm EB, Yjatsky A, Grobbee D, Stampfer MJ. Review of moderate alcohol consumption and reduced risk of coronary heart disease. BMJ. 1996;312(7033):731–736. doi: 10.1136/bmj.312.7033.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Renaud S, Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary artery disease. Lancet. 1992;339(8808):1523–1526. doi: 10.1016/0140-6736(92)91277-F. [DOI] [PubMed] [Google Scholar]
- 78.St Leger AS, Cochrane AL, Moore F. Factors associated with cardiac mortality in developed countries with reference to the consumption of wine. Lancet. 1979;1(8124):1017–1020. doi: 10.1016/S0140-6736(79)92765-X. [DOI] [PubMed] [Google Scholar]
- 79.Aviram M, Rosenblat M, Billeke S, Du B. Human serum PON is inactivated by oxidized LDL and preserved by antioxidants. Free Rad Biol Med. 1999;26:892–904. doi: 10.1016/S0891-5849(98)00272-X. [DOI] [PubMed] [Google Scholar]
- 80.Fuhrman B, Aviram M. Preservation of paraoxonase activity by wine flavonoids. Ann N Y Acad Sci. 2002;957:321–324. doi: 10.1111/j.1749-6632.2002.tb02933.x. [DOI] [PubMed] [Google Scholar]
- 81.Vigna GB, Costantini F, Aldini G, et al. Effect of grape seed extract on low-density lipoprotein susceptibility to oxidation in heavy smokers. Metabolism. 2003;52:1250–1257. doi: 10.1016/S0026-0495(03)00192-6. [DOI] [PubMed] [Google Scholar]
- 82.Primo-Parmo SL, Sorenson RC, Teiber J, Du BN. Human serum paraoxonase/arylesterase (PON1) is one member of a multigene family. Genomics. 1996;33:498–507. doi: 10.1006/geno.1996.0225. [DOI] [PubMed] [Google Scholar]
- 83.Du BN. Human serum paraoxonase/arylesterase. In: Kalow W, editor. Pharmacogenetics of drug metabolism. New York: Pergamon Press; 1992. pp. 51–91. [Google Scholar]
- 84.Chemnitius JM, Losch H, Losch K, Zech R. Organophosphate detoxicating hydrolases in different vertebrate species. Comp Biochem Physiol C. 1983;76(1):85–93. doi: 10.1016/0742-8413(83)90048-8. [DOI] [PubMed] [Google Scholar]
- 85.Saha N, Roy AC, Teo SH, Tay JS, Ratnam SS. Influence of serum paraoxonase polymorphism on serum lipids and apolipoproteins. Clin Genet. 1991;40:277–282. doi: 10.1111/j.1399-0004.1991.tb03096.x. [DOI] [PubMed] [Google Scholar]
- 86.Mackness MI, Arrol S, Abbott CA, Durrington PN. Is paraoxanase related to atherosclerosis. Chem Biol Interac. 1993;87:161–171. doi: 10.1016/0009-2797(93)90038-Z. [DOI] [PubMed] [Google Scholar]
- 87.Mackness MI, Walker CH, Carlson LA. Low A-esterase activity in serum of patients with fish-eye disease. Clin Chem. 1987;33:587–588. [PubMed] [Google Scholar]
- 88.Mackness MI (1989) In: Reiner E, Aldridge WN, Hoskins FCG (eds) Enzymes hydrolysing organophosphorus compounds, pp 202–213
- 89.Jaichander P, Selvarajan K, Garelnabi M, Parthasartahy S. Induction of PON1 and apolipoprotein A-1 gene expression by asprin. J Lipid Res. 2008;49:2142–2148. doi: 10.1194/jlr.M800082-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mackness MI, Arrol S, Durrington PN. Paraoxonase prevents accumulation of lipoperoxides in low-density lipoprotein. FEBS Lett. 1991;286:152–154. doi: 10.1016/0014-5793(91)80962-3. [DOI] [PubMed] [Google Scholar]
- 91.Ng CJ, Wadleigh DJ, Gangopadhyay A. Paraoxonase 2 is capable of preventing cell-mediated oxidative modification of low density lipoprotein. J Biol Chem. 2001;276:44444–44449. doi: 10.1074/jbc.M105660200. [DOI] [PubMed] [Google Scholar]
- 92.Draganov DL, Stetson PL, Watson CE, Billecke SS, Du BN. Rabbit serum PON3 is a HDL associated lactonase and protects LDL against oxidation. J Biol Chem. 2000;275:33435–33442. doi: 10.1074/jbc.M004543200. [DOI] [PubMed] [Google Scholar]
- 93.Reddy ST, Wadleigh DJ, Grijalva V. Human PON3 is a HDL enzyme with biological activity similar to PON1 but not regulated by oxidized lipids. Arter Throm Vasc Biol. 2001;21:542–547. doi: 10.1161/01.atv.21.4.542. [DOI] [PubMed] [Google Scholar]
- 94.Navab M, Hama-Levy S, Lenten BJ, et al. Mildly oxidized LDL induces an increased apolipoprotein J/paraoxonase ratio. J Clin Invest. 1997;99:2005–2019. doi: 10.1172/JCI119369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Aviram M, Rosenbalt M, Bisgaier CL, Newton RS, Primo-Parmo SL, Du BN. Paraoxonase inhibits high-density lipoprotein oxidation and preserves its functions. A possible peroxidative role for paraoxonase. J Clin Invest. 1998;101:1581–1590. doi: 10.1172/JCI1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shih DM, Gu L, Xia YR, et al. Mice lacking serum paraoxonase are susceptible to organophosphate toxicity and atherosclerosis. Nature. 1998;394:284–287. doi: 10.1038/28406. [DOI] [PubMed] [Google Scholar]
- 97.Mackness B, Durrington P, McElduff P, Yarnell J, Azam N, Watt M, Mackness M. Low paraoxonase activity predicts coronary events in the Caerphilly Prospective Study. Circulation. 2003;107:2775–2779. doi: 10.1161/01.CIR.0000070954.00271.13. [DOI] [PubMed] [Google Scholar]
- 98.Aviram M, Rosenblat M. Paraoxonase 1, 2, 3, oxidative stress, and macrophage foam cell formation during atherosclerosis development. Free Radic Biol Med. 2004;37:1304–1316. doi: 10.1016/j.freeradbiomed.2004.06.030. [DOI] [PubMed] [Google Scholar]
- 99.Jakubowski H. Calcium-dependent human serum homocysteine thiolactone hydrolase. J Biol Chem. 2000;275:3957–3962. doi: 10.1074/jbc.275.6.3957. [DOI] [PubMed] [Google Scholar]
- 100.Sierksma A, Gaag MS, Tol A, James RW, Hendriks HF. Kinetics of HDL cholesterol and paraoxonase activity in moderate alcohol consumers. Alcohol Clin Exp Res. 2002;26(9):1430–1435. doi: 10.1097/01.ALC.0000030639.57507.60. [DOI] [PubMed] [Google Scholar]
- 101.Lakshman MR, Gottipati CS, Narasimhan SJ, Munoz J, Marmillot P, Nylon ES. Inverse correlation of serum paraoxonase and homocysteine thiolactonase activities and antioxidant capacity of high-density lipoprotein with the severity of cardiovascular disease in persons with type 2 diabetes mellitus. Metabolism. 2006;55:1201–1206. doi: 10.1016/j.metabol.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 102.Jakubowski H. The molecular basis of homocysteine thiolactone-mediated vascular disease. Clin Chem Lab Med. 2007;45:704–1716. doi: 10.1515/CCLM.2007.338. [DOI] [PubMed] [Google Scholar]
- 103.Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest. 2002;109:1125–1131. doi: 10.1172/JCI15593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Deakin S, Leviev I, Guernier S, James RW. Simvastatin modulates expression of the PON1 gene: a role for SREBP2. Arter Thromb Biol. 2003;23:2083–2089. doi: 10.1161/01.ATV.0000096207.01487.36. [DOI] [PubMed] [Google Scholar]
- 105.Gouedard C, Koum-Besson N, Barouki R, Morel Y. Opposite regulation of the human paraoxonase-1 gene PON-1 by fenofirate and statins. Mol Pharmacol. 2003;63(4):945–956. doi: 10.1124/mol.63.4.945. [DOI] [PubMed] [Google Scholar]
- 106.Gouedard C, Barouki R, Morel Y. Dietary polyphenols increase paraoxonase 1 gene expression by an aryl hydrocarbon receptor-dependent mechanism. Mol Cell Biol. 2004;24(12):5209–5222. doi: 10.1128/MCB.24.12.5209-5222.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Osaki F, Ikeda Y, Suehiro T, Ota K, Tsuzura S, Arii K, Kumon Y, Hashimoto K. Roles of Sp1 and protein kinase C in regulation of human serum paraoxonase 1 (PON1) gene transcription in HepG2 cells. Atherosclerosis. 2004;176(2):279–287. doi: 10.1016/j.atherosclerosis.2004.05.029. [DOI] [PubMed] [Google Scholar]
- 108.Rozenberg O, Shih DM, Aviram M. Human serum paraoxonase 1 decreases macrophage cholesterol biosynthesis: possible role for its phospholipase-A2-like activity and lysophosphatidylcholine formation. Arter Thromb Vasc Biol. 2003;23(3):461–467. doi: 10.1161/01.ATV.0000060462.35946.B3. [DOI] [PubMed] [Google Scholar]
- 109.Marmillot P, Rao MN, Liu QH, Chirtel SJ, Lakshman MR. Effect of dietary omega-3 fatty acids and chronic ethanol consumption on reverse cholesterol transport in rats. Metabolism. 2000;49(4):508–512. doi: 10.1016/S0026-0495(00)80017-7. [DOI] [PubMed] [Google Scholar]
- 110.Rosenblat M, Vaya J, Shih DM, Aviram M. Paraoxonase 1 (PON1) enhances HDL-mediated macrophage cholesterol efflux via the ABCA1 transporter in association with increased HDL binding to the cells: a possible role for lysophosphatidylcholine. Atherosclerosis. 2005;179(1):69–77. doi: 10.1016/j.atherosclerosis.2004.10.028. [DOI] [PubMed] [Google Scholar]
- 111.Rozenberg O, Shih DM, Aviram M. Paraoxonase 1 (PON1) attenuates macrophage oxidative status: studies in PON1 transfected cells and in PON1 transgenic mice. Atherosclerosis. 2005;181(1):9–18. doi: 10.1016/j.atherosclerosis.2004.12.030. [DOI] [PubMed] [Google Scholar]
- 112.Tol AA, Hendriks HFJB. Moderate alcohol consumption: effects on lipids and cardiovascular disease risk. Curr Opin Lipidol. 2001;12:19–23. doi: 10.1097/00041433-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 113.Agarwal DP. Cardioprotective effects of light-moderate consumption of alcohol: a review of putative mechanisms. Alcohol Alcohol. 2002;37:409. doi: 10.1093/alcalc/37.5.409. [DOI] [PubMed] [Google Scholar]
- 114.Gaag MS, Tol A, Scheek LM, James RW, Urgert R, Schaafsma G, Hendriks HF. Daily moderate alcohol consumption increases serum paraoxonase activity; a diet-controlled, randomized intervention study in middle-aged men. Atherosclerosis. 1999;147:405. doi: 10.1016/S0021-9150(99)00243-9. [DOI] [PubMed] [Google Scholar]
- 115.Prakash M, Shetty JK, Tripathy S, Verma M. Letter to the editor: serum paraoxonase in alcohol abusers associated with alcoholic liver disease. Clin Chim Acta. 2007;378:232–234. doi: 10.1016/j.cca.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 116.Gong M, Garige M, Varatharajalu R, Marmillot P, Gottipatti C, Leckey LC. Quercetin up-regulates paraoxonase 1 gene expression with concomitant protection against LDL oxidation. Biochem Biophys Res Commun. 2009;379:1001–1004. doi: 10.1016/j.bbrc.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 117.Penumathsa SV, Maulik N. Resveratrol: a promising agent in promoting cardioprotection against coronary heart disease. Can J Physiol Pharmacol. 2009;87:275–286. doi: 10.1139/Y09-013. [DOI] [PubMed] [Google Scholar]
- 118.Dudley JI, Lekli I, Mukherjee S, Das M, Bertelli AA, Das DK. Does white wine qualify for French paradox? Comparison of the cardioprotective effects of red and white wines and their constituents: resveratrol, tyrosol, and hydroxytyrosol. J Agric Food Chem. 2008;56:9362–9373. doi: 10.1021/jf801791d. [DOI] [PubMed] [Google Scholar]
- 119.Chan AY, Dolinsky VW, Soltys CM, Viollet B, Baksh S, Light PE, Dyck JRB. Resveratrol inhibits cardiac hypertrophy via AMP-activated protein kinase and Akt. J Biol Chem. 2008;283(35):24194–24201. doi: 10.1074/jbc.M802869200. [DOI] [PMC free article] [PubMed] [Google Scholar]