Abstract
Objective
This study was conducted to evaluate a computer-imaging program called HAAIR (Help with Adjustment to Alopecia by Image Recovery) that was developed to provide educational support and reduce distress in women with hair loss following chemotherapy.
Methods
Forty-five women who had been diagnosed with cancer and anticipated alopecia following treatment were randomly assigned to either the Computer Imagining Intervention group (IG) or Standardized Care group (SCG). Patients in the IG used a computer imaging program that created the patient’s image on a screen to simulate baldness and use of wigs while patients in the SCG were directed to a resource room at the Cancer Center established for women with chemotherapy-related alopecia. Assessment data using the Brief Symptom Inventory, Importance of Hair Questionnaire, and the Brief Cope were completed at baseline (T1), before chemotherapy and hair loss, following hair loss (T2), and 3 months follow-up (T3).
Results
All women were able to successfully use the touch screen computerized imaging program and reported that using the computer was a positive, helpful experience, thus establishing acceptability and usability. Women in both the IG and the SCG group showed significantly lower Hair Loss Distress scores at T2 after hair loss than at T1 with T3 distress scores increasing in the SCG and decreasing in the IG. Those with avoidance coping reported more distress.
Conclusions
This evaluation demonstrates that the HAAIR program is a patient-endorsed educational and supportive complement to care for women facing chemotherapy-related alopecia.
Keywords: cancer, oncology, alopecia, NCI, computer imaging, education
INTRODUCTION
Alopecia, or hair loss, is a distressing side-effect of chemotherapy for patients who must use certain drugs or chemical agents to prevent cancer recurrence [1–4]. Among the various side effects of chemotherapy, (e.g., nausea, fatigue), alopecia continues to be rated as one of the top five most upsetting experiences for women who must endure it [5]. Some patients have refused treatment [6] and 8% of women in one study considered refusal because of this side effect [7].
Recognition of chemotherapy-related alopecia and related psychosocial problems has been noted in the literature for three decades [2,7–15]. A recent review has summarized a number of both qualitative and quantitative studies [5]. To date, scalp cooling [16–19] has been used to try to prevent hair loss with debatable success, and pharmaceutical solutions continue to be investigated [20,21]. Unfortunately, the extent of the hair loss, whether partial or total, does not appear to be directly related to how distressed the patient finds the experience [22,23]. This suggests that emotional adjustment to alopecia is as complex as it is for adjustment to a diagnosis of breast or other cancers [24,25]. For some women, chemotherapy-induced alopecia has been noted as a distressing stigmatizing experience [26] as well as a traumatic event separate from the diagnosis of cancer [27]. It can serve as a constant visual reminder of “I have cancer”.
Cancer patients who experienced alopecia have reported that they still felt “unprepared” although they sought information from other women who had been through chemotherapy and associated alopecia, or received written educational information from nurses and other health care professionals or from cancer support web sites suggesting that other strategies are needed to address this need [15]. Due to the high financial burden of cancer, interventions that are low-cost as well as effective are of the utmost importance. Moreover, many women diagnosed with cancer are indigent and carry no insurance. Cancer Centers and health care systems throughout the U.S. recognize a need for cost-effective strategies to provide psychosocial support to assist women coping with the side effects of cancer treatment, notably alopecia. The high costs associated with clinical space may be a barrier for the inclusion of dedicated space to be used to facilitate adjustment to alopecia patients. For most health systems physical space for life-saving medical treatments or the early detection of disease (e.g. breast cancer) will likely take precedence over space for psychosocial support if a choice must be made. As such, effective technological advances that address psychosocial needs that do not require high expenses associated with clinical space are needed that can be located in close proximity to cancer treatment clinics.
It may be difficult to prepare patients for chemotherapy-related alopecia because the experience may be different for each person, yet based upon data from a small qualitative study, it is argued that women do engage in some sort of anticipatory coping before hair loss [28]. For interventions aimed at reducing psychosocial distress in women with alopecia following treatment for cancer, more information is needed on the relationship between patient coping styles and adjustment to hair loss to inform better treatment strategies. Women with breast cancer who use more direct and confrontational coping strategies have been found to be less distressed than those using avoidance and denial [29]. Emotional control is related to higher disturbance of mood, anxiety and depression [30] while acceptance, use of humor, and positive re-framing are associated with better adjustment to breast cancer [31]. Less is known about coping specific to hair loss. One study found that how women adjusted to hair loss with regard to their body image was associated to some extent with their ability to cope [27]. A dermatology study using the Brief COPE found that avoidant coping and problem-focused, but not active emotional coping accounted for 7% of the variance in lower quality of life in a sample of people with alopecia not associated with cancer [32]; however, more research is needed in this area since there are few empirical studies on alopecia [33]. There is need for improved quality of care for cancer patients to address psychosocial needs and related distress from diagnosis through survivorship [34], and reducing distress associated with alopecia falls within this domain. The development of technologies that could be used to reduce alopecia distress is a step in this direction.
Computer-based approaches and imagery interventions, as well as patient education tailored to the individual, have been found to be effective for a number of conditions suggesting the potential benefits of similar applications for alopecia [35–40]. The success of computers to facilitate patient education and symptom reduction provides support for the proposed computer-assisted intervention to education patients about alopecia and reduce alopecia-related distress. In a review of 21 research-based studies, Lewis (1991) found that an effect size greater than 0.5 was achieved in 75% of cases resulting in improvement in condition for patients. Computers have been found useful for helping asthma patients control symptoms [41]; to improve self-assessment of symptom scores due to benign prostatic hyperplasia [42] among others.
In an effort to address the distress of alopecia, and to facilitate anticipatory coping, we were interested in discovering whether existing technology that was available in beauty salons might be applicable to help women prepare for chemotherapy-related hair loss. However, a review of existing programs found that there were no software programs that were user-friendly for patients or that simulated baldness. Therefore, a computer imaging system, called HAAIR (Help with Adjustment to Alopecia Image Recovery) was developed by a university-business partnership under a SBIR grant from the National Cancer Institute to determine the feasibility of using it to help cancer patients adjust to chemotherapy-related alopecia. Our first step in this pilot study, in anticipation of further research in this area, was to determine if a single session with a clinician would help prepare the patient in advance of the hair loss by use of the baldness feature of the HAAIR program to help desensitize the patient to the actual experience of baldness, in addition to education about alopecia in a supportive environment. In this paper, we discuss the outcome of an evaluation of the computer imaging system. The aims of the evaluation are: 1) to determine the acceptability and ease of use of the HAAIR system for patients, and 2) to compare the effects of the HAAIR system to those of an enhanced standard care program in reducing alopecia-related distress.
METHODS
Design
This evaluation study used both qualitative and quantitative methods. To determine the acceptability and ease of use of the HAAIR system for patients, qualitative feedback from participants was obtained at baseline following completion of the assessment measures and during or after use of the system. An experimental pretest-post test design was used to examine clinical effects [43]. Assessment data were collected at baseline (T1), following hair loss (T2), and 3 months follow-up (T3). The clinical objective was to determine if the use of the HAAIR system was associated with less distress following hair loss than Standard Care.
Sample
The study was explained verbally and in writing to each participant. All participants in the study provided signed informed consent documents that explained that they would be assigned to the intervention or treatment group randomly, like that of a “flip of a coin”. Using a simple randomization sequence [44], a total of 45 women patients were assigned to the HAAIR intervention group (IG) or a standardized control group (SCG). Patients were compensated $25 each time they completed the assessments. The study was approved by the University of Virginia’s Human Investigation Committee. All participants were informed that, if needed, crisis counseling and psychiatric services were available throughout the study.
Inclusion criteria included female cancer patient with a current diagnosis of breast, gynecological or other cancer and chemotherapy treatment that was associated with alopecia. Exclusion criteria were: (a) age less than 18 or more than 75 years, (b) failure to provide written informed consent, (c) significant incapacitating physical or mental illness, (d) medical staff consensus that the level of intellectual functioning was not commensurate with the tasks, and/or (e) prior experience of cancer and alopecia.
Procedures and Measures
Nurses of physicians with patients who were likely to be treated with agents known to cause alopecia were asked to provide informational flyers with the contact number of Drs. McGarvey and Baum to the patients. Any patient who contacted one of the study team and stated an interest in participation was approached as soon as possible for a comprehensive description of the study by the primary Interviewer (Bloomfield), usually within 48 hours. In addition, recruitment included brochures posted in various hospital locations and on the Cancer Center clinical trials website. A screening interview of the patient was conducted either on the phone or in person by the Interviewer to assess participant eligibility based on the inclusion/exclusion criteria.
The Interviewer was a cancer survivor who is also a clinical nurse specialist in adult psychiatric counseling. She obtained informed consent, collected assessment data from patients who responded in writing to a battery of questionnaires over the three time points of the study, as well as demonstrated the HAAIR system. She was available to provide support as patients processed feelings about upcoming chemotherapy-related hair loss in both the IG and SCG if they arose during contact time with her.
Qualitative data were obtained verbally by open-ended questions asked during or following use of HAAIR (e.g. “Did you enjoy using the system?, “Are you glad that you were able to try the system?”). In addition, observation of the patients using the system as well as direct questioning served to establish usability.
The quantitative measures for this study included: A Demographic Characteristics Questionnaire, which obtained information on age, race/ethnicity, education, employment, marital status, and self-reported type of cancer was used at baseline. In addition, the Interviewer assessed the degree of hair loss on a scale of 0=no loss, 1=slight hair loss, 2=some hair loss, 3=moderate hair loss, 4=almost all hair, 5=complete hair loss.
The Brief Symptom Inventory (BSI-18), with 18 items, measures general psychological distress to comprise an overall distress score, the Global Severity Index (GSI) and three subscale symptom scores (i.e., somatization, depression, anxiety) related to having cancer. Patients rate each item on a 5-point scale from 0 “not at all” to 4 “extremely”. Higher scores indicate greater intensity of symptoms or distress. Missing data and score calculations were done following the BSI 18 manual. Subscales and GSI ranged from 0–4. Clinically significant psychological distress was indicated if the GSI T-score was ≥ 63 [45]. The BSI-18 has been used in many studies of cancer in women [36].
The Importance of Hair Questionnaire (IHQ) was used specifically to assess hair loss distress [2,46]. The IHQ is a 20-item self-rating scale. Hair loss distress total scores ranged from 0 to 75 (Cronbach’s α=0.806) . As with the total score, a higher score reflects greater distress also on the five IHQ subscales: “hair difficult” (expecting hair loss to be emotionally difficult) range from 0 to 20 (Cronbach’s α=0.880), “hair desirable” (feeling more sexually desirable when one’s hair looks good) (Cronbach’s α=0.819) and “hair social” (expecting good social support from friends and family) (Cronbach’s α=0.795) range from 0 to 15, “hair others note” (others notice my hair) (Cronbach’s α=0.610) and “hair confidence” (confidence in ability to adjust to hair loss) (Cronbach’s α=0.146) each range from 0 to 10. The IHQ has been factor analyzed and shows a positive correlation with the BSI anxiety subscale score (McGarvey & Leon-Verdin, manuscript in preparation).
The Brief Cope, which was derived from the Cope, was used to assess the manner in which patients coped with having cancer [47]. It is a 24-item measure that lists various coping methods when the dealing with a stressor (e.g. mental disengagement, positive reframing). Each item is rated on a 4-point scale ranging from 1 “I have not done this at all” to 4 “I have been doing this a lot”. Items were recoded into two categories: active copying (Cronbach’s α=0.780), and avoidant coping (Cronbach’s α=0.586). Internal consistency was tested by calculating Cronbach’s Alphas. Patients were then classified into one of the categories, depending on their total scores on each coping style. Good psychometric properties have been shown for assessment of situational coping and dispositional coping efforts [48].
The HAAIR Intervention
The HAAIR computer imaging system took over three years to successfully develop and test with normal samples, recovered cancer patients and health care professionals prior to its use with newly diagnosed cancer patients for the evaluation study. The HAAIR system uses digital imaging processing and a graphical user-interface on a desktop or portable computer. For the evaluation, a desktop computer was physically located in a 4′×4′, attractively decorated alcove in the Breast Center on the first floor of Hospital West at the University of Virginia for patients’ convenience. IG patients met the Interviewer at this location and following T1 assessments, sat down in one of two comfortable, upholstered chairs positioned in front of the digital camera, which was installed above the computer screen. A mirror and related hair products were available for patient use, if desired. To use the HAAIR system, the patient placed a red scarf over her hair. With a push of a button on the computer screen that was easily located within reach, the patient was “walked” through the process using directions and touch screen virtual “buttons”. The Interviewer sat in the chair beside the patient to explain the procedure and to provide assistance if needed. The patient facilitated her own photograph being taken by the digital camera and four images of her face were displayed on the computer screen in real time. The patient was then able to select the image of herself that she preferred or to delete them all and repeat the process. Once the patient accepted a photo of herself, she could touch another virtual button that created optional images of seeing herself with a bald head and of her head wearing a variety of different wigs and hair styles. Each session lasted between 60 and 90 minutes. In addition, each patient was provided a no cost booklet published by the National Cancer Institute entitled Chemotherapy and You: A Guide to Self-Help During Cancer Treatment (NIH Publication No 03-1136, 2003) as well as information on where to purchase wigs. Patients were asked to comment on the ease of operating the system (i.e., “How user friendly was the HAAIR system?”), and if the HAAIR system was useful to them with regard to informing or showing them what to expect with their upcoming hair loss; participants were also invited to make suggestions to improve the system.
Standardized Care
The UVA Cancer Center is better equipped than many health care facilities around the U.S. where standard care includes no specific resources for women with cancer facing alopecia. At UVA, the Cancer Center has a special alopecia-specific resource room—identified as “Ramona’s room”—which is conveniently located near the infusion center. The approximately 16 by 14 foot room resembles a woman’s fashionable dressing room and is equipped with a mirror, comfortable chair, a case of wigs, patient education materials and other head coverings typically worn by women to cover their baldness following chemotherapy. The room is dedicated to helping women adjust to hair loss, and was originally funded by a charitable donation in memory of a woman who lost her life to breast cancer. Over the years, other charitable groups have continued to provide funds to purchase wigs and other supplies for women following hair loss after treatment for cancer. A nurse or the oncologist typically informs the patient that alopecia will be a temporary side effect of chemotherapy. Standard Care includes the patient’s oncology nurse telling the patient about the purpose and location of Ramona’s room, which is available for use whenever the clinic is open. For this study, the standard care was “standardized” to ensure that each woman received the same written NCI educational booklet about side effects of chemotherapy and the same list of places to purchase wigs. This information was provided by the Interviewer.
Statistical Analysis
Analyses were performed using SPSS 16 software. For BSI, missing data were handled as BSI manual instructions, for other questionnaires data were considered as missing completely at random (MCAR). The level of alpha required for determining statistical significance was set at p=.05.
This study was designed to test the hypothesis of a treatment effect on the outcome at the .05 alpha level, two-tailed. Since this is a pilot study with a relatively small sample, no corrections were made for conducting multiple statistical tests. As an effect size greater than a Cohen’s d of .5 was achieved in 75% of previous computer-based studies [49], this study was powered to assume this moderate effect size. Given these assumptions, and with 45 participants recruited for this study, statistical power was adequate but not optimal (.75) for testing the main hypothesis of a treatment effect on the outcome [50]. We had originally planned to recruit 100 participants, which given our other assumptions, would have yielded statistical power greater than .95 [50], but unfortunately, due to unforeseen time delays in development and in obtaining IRB approval, the recruitment period was by necessity shortened resulting in a final sample size that was not this large.
Descriptive statistics were calculated on all studied variables. Demographic characteristics were assessed using Student t-test, Fisher’s exact test, and Pearson’s chi-square tests as appropriate to determine differences between patients in the IG and SCG. Pearson’s correlations were conducted using a two-tailed test of significance to investigate the relationship between avoidance coping and distress. The effect of confounding variables was examined using multivariate analysis at baseline. If the effect was found to be significant, the variable in question was considered for the repeated measurement analysis.
Pre-intervention (T1) differences between groups on demographic characteristics and Post-intervention (T2) and (T3) on the outcome measures were analyzed using a general linear model analysis of variance for continuous variables. The Greenhouse-Geisser adjustment was used for the effect of treatment, time and the interaction of the effect and time of visit.
RESULTS
Technical Evaluation Results
Qualitative feedback from the patients who operated the HAAIR system confirmed its “ease-of-use” and educational usefulness. All patients in the intervention were able to use the touch screen system either with no assistance or minimal assistance from the Interviewer. The Interviewer assisted patients with the HAAIR system by verbal encouragement and a brief initial demonstration. Patients who did not use a computer at home or work were somewhat reluctant to try the system at first, but soon realized that it required very little computer knowledge and was as easy to use as touching the screen.
All patients (100%) stated that they “enjoyed” or “were glad” that they used the system to demonstrate to themselves or to learn what to expect with hair loss. Seeing themselves completely bald seemed to have the most dramatic effect on the patients based on their verbal feedback. In all cases, humor and use of the touch screen provided a relatively relaxed environment in which to discuss chemotherapy-related hair loss. One of the most positive features of the HAAIR system was related to the issue of fatigue. Patients stated that “virtually” trying on wigs and changing hair styles was not as difficult and exhausting as raising one’s arms to try on wigs in real life. In addition, patients stated that they liked having the Interviewer or a family member present during the process to provide feedback, support and to increase opportunities to share a measure of levity over an otherwise serious, frightening anticipated event. The opportunity to ask the Interviewer questions about alopecia was also reported as helpful.
Over half (60%) of the women volunteered suggestions to improve the system or commented on features that they did or did not like. Most patients wanted to see a greater number of wigs with more hair styles that they could virtually “try on”. Other comments were: a) to include a greater variety of wig colors so that patients could better match their virtual hair color to that of their real hair, b) to reword “Tease hair” on the screen instructions to “Move Up” for adjusting the wig upon the head image, c) to house the HAAIR system inside a private “photo booth” such as one might see in a shopping mall for snapping small photos, d) to reduce the size of the 8.5″ × 11″ photo, e) to add the loss of eyebrows in addition to head baldness as an option, and f) to incorporate simple, bullet-like written educational messages about what to expect into the program. In summary, the development of the HAAIR system was successful with regard to both ease of use and perceived usefulness. Improvements that were suggested by patients are likely to further increase patient satisfaction.
Cost Effectiveness
Costs of the physical space in the medical center that was used for the HAAIR system in the IG were compared to the costs of space of the resource room that was used for the SCG. Space to provide psychosocial support using HAAIR was about 14 times less expensive than the cost of Standard Care The current value of “Ramona’s Room” (14′ × 16′) is approximately $88,256, which is based on $394 per square foot costs for a 14reported by the hospital facilities manager while the value of the space needed for the HAAIR system (4′ × 4′) is $6,304 [51]. A cost effectiveness study was beyond the scope of the evaluation; however, the HAAIR system itself, as it currently exists, costs about $5,000. We did not calculate the costs of furniture, mirrors, wigs, wig stand, etc. that are in Ramona’s Room. Even if these costs are less, the overall costs remain higher for the resource room than the spaced needed for HAAIR.
Clinical Results
Sample Characteristics
At baseline (T1) and T2, 97.5% of the patients completed the study measures. At T3, one patient could not be reached to be assessed and did not return mailed assessment questionnaires. She was then dropped from the study. As such, 95% of the patients completed all three assessments for the study. From the total sample, data from five patients (11.1%) in the IG were excluded from the analyses because they did not meet inclusion criteria due to having previously had cancer and alopecia.
There were no significant differences in demographics characteristics between IG and the SCG patients. Mean age in the IG was comparable to that of the SCG (51.7 vs. 50.9). Most patients in this study identified themselves as White Non-Hispanic, 76% in IG and 83.3% in SCG. There were similar numbers of patients in each group for different education levels. Consistent percentages were reported for employment status in both groups. Most patients had breast cancer (60% in IG and 65% in SCG), which was followed by ovarian cancer (32% in IG and 15% in SCG). Patients had either “complete” (60% in IG and 65% in SCG) or “almost all” hair loss (40% in IG and 35% in SCG). See table 1 for more details.
Table 1.
Demographics characteristics.
| Intervention Group N = 25 (100%) | Standard Care Group N = 20 (100%) | p-value | |
|---|---|---|---|
| Age in years | 51.72 ± 10.55 | 50.85 ± 10.31 | 0.78 |
| Race | 0.71 | ||
| White/Caucasian | 19 (76) | 15 (83.3) | |
| Other | 6 (24) | 3 (16.7) | |
| Education | 0.18 | ||
| High School or less | 4 (20) | 7 (36.8) | |
| Bachelor’s Degree or less | 10 (40) | 9 (47.4) | |
| Some Graduate School or more | 10 (40) | 3 (15.8) | |
| Employment | 0.72 | ||
| Full time | 10 (40) | 6 (31.6) | |
| Part time | 5 (20) | 3 (15.8) | |
| Not employed | 10 (40) | 10 (52.6) | |
| Marital Status | 0.98 | ||
| Single | 8 (32) | 6 (31.6) | |
| Married | 17 (68) | 13 (68.4) | |
| Cancer type | 0.89 | ||
| Breast | 15 (60) | 13 (65) | |
| Ovarian | 8 (32) | 3 (15) | |
| Lung | 0 | 2 (10) | |
| Blood | 1 (4) | 1 (5) | |
| Melanoma | 1 (4) | 1 (5) | |
| Degree of Hair Loss | 0.73 | ||
| Complete Hair Loss | 15 (60) | 13 (65) | |
| Almost all Hair Loss | 10 (40) | 7 (35) |
Brief Symptom Inventory
Nineteen patients in each arm completed the BSI-18 questionnaire at T1, T2 and T3 assessments. At baseline, there were more patients in IG (75 %) than in SCG (47.4%) not expressing a clinical level of psychological distress; the T-scores for the three BSI subscales were all under 63. The others had a least one T-score over or equal the cut off score of 63. Using GSI criterion, 31.6% (n = 6) of the SCG and 20% (n = 4) of the IG were considered clinically distressed.
Table 2 shows results for subscale dimensions and GSI across time. IG subscale scores ranged from .61 (depression) to .96 (anxiety) while SCG scores ranged from .72 (depression) to 1.2 (anxiety). Means and standard deviations for the BSI subscale scores are provided in Table 2. Somatization (p = .011), anxiety (p = .005), and GSI (p = .005) were related to age with younger patients indicating more distress in these areas than older patients. Depression was associated with age (F(1,37) = 7.036, p = .012) and cancer type (F(3,35) = 3.795, p = .019). No significant interaction was found between time of visit and treatment group. No significant differences were found between groups. As such, the global and symptom experiences of distress related to cancer were reduced as much in the IG group as in the SCG.
Table 2.
Mean and standard deviation (SD) for the raw score and the mean of the T-transformation (Tscore*) on Brief Symptom Inventory dimensions (1) and global index score (2).
| Somatization1 | Depression1 | Anxiety1 | GSI2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Tscore* | Mean | SD | Tscore* | Mean | SD | Tscore* | Mean | SD | Tscore* | |
| TIME 1 | ||||||||||||
| IG | .63 | .70 | 51.9 | .61 | .76 | 52.9 | .96 | .88 | 53.7 | .73 | .67 | 53.2 |
| SCG | .72 | .82 | 52.5 | .80 | .83 | 55.3 | 1.2 | .72 | 57.0 | .90 | .70 | 56.1 |
| TIME 2 | ||||||||||||
| IG | .95 | .99 | 56.2 | .54 | .66 | 51.8 | .81 | .80 | 51.3 | .77 | .77 | 52.9 |
| SCG | .92 | .63 | 56.4 | .59 | .61 | 52.5 | .80 | .68 | 51.8 | .77 | .54 | 54.0 |
| TIME 3 | ||||||||||||
| IG | .97 | .90 | 56.9 | .76 | 1.0 | 53.3 | .86 | .95 | 51.4 | .87 | .85 | 54.4 |
| SCG | .93 | .56 | 57.2 | .87 | .71 | 56.4 | .89 | .64 | 53.1 | .90 | .57 | 56.3 |
Cut off for clinical disorders in the T-transformation is set a 63 for all dimensions and the global index score.
IG stands for Intervention Group.
SCG stands for Standard Care Group.
Importance of Hair
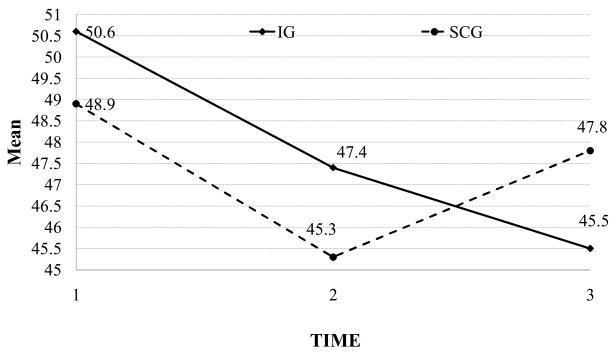
Complete data were available on 36 patients for the analyses on IHQ distress. At T1, patients did not have significant differences in hair loss distress between groups. At T2, both IG and SCG showed significant decline in distress from baseline, while at the end of follow-up (T3), the hair loss distress continues to decrease in the IG while there was an increase in the SCG. As such, the interaction of treatment and time (p = .079) while not meeting criterion set for statistical significance indicates a trend and 8.8% of the variation was explained by this factor (See Figure 1). In addition, a moderate effect size was seen in the IHQ subscale “hair desirable” score, 13.3% of the variation was explained by the interaction with p = .029. The results for other subscales of the IHQ are shown in Table 3.
Figure 1.
Changes in Hair Loss Distress Over Time
Table 3.
Mean and standard deviation (SD) of the Important of Hair Questionnaire subscales at each time visit and the comparison of the change between both arms.
| Group | Mean (SD) T1 | Mean (SD) T2 | Mean (SD) T3 | Effect tested at T1 vs T3 | p-value | Partial Eta2 |
|---|---|---|---|---|---|---|
| Hair loss distress | between-subjects | 0.939 | 0.000 | |||
| IG | 50.6 (11.0) | 47.4 (10.6) | 45.5 (11.8) | within-subjects | 0.008 | 0.189 |
| SCG | 48.9 (12.5) | 45.3 (14.9) | 47.8 (9.5) | interaction | 0.079 | 0.088 |
| Difficult | between-subjects | 0.504 | 0.013 | |||
| IG | 11.8 (5.1) | 9.3 (4.8) | 9.6 (6.0) | within-subjects | 0.002 | 0.240 |
| SCG | 10.4 (6.5) | 8.4 (6.2) | 8.6 (5.3) | interaction | 0.792 | 0.002 |
| Desirable | between-subjects | 0.542 | 0.011 | |||
| IG | 10.7 (3.8) | 10.1 (3.8) | 9.0 (3.9) | within-subjects | 0.009 | 0.184 |
| SCG | 10.6 (3.2) | 9.9 (3.7) | 10.4 (2.5) | interaction | 0.029 | 0.133 |
| Social | between-subjects | 0.424 | 0.019 | |||
| IG | 12.8 (2.1) | 13.1 (1.6) | 12.9 (1.8) | within-subjects | 0.033 | 0.126 |
| SC | 12.6 (2.4) | 13.6 (2.4) | 14.0 (1.4) | interaction | 0.091 | 0.082 |
| Others Note | between-subjects | 0.333 | 0.028 | |||
| IG | 6.7 (2.0) | 6.4 (1.5) | 5.8 (1.4) | within-subjects | 0.027 | 0.135 |
| SC | 6.2 (2.4) | 5.3 (2.4) | 5.3 (1.7) | interaction | 0.000 | 0.000 |
| Confidence | between-subjects | 0.379 | 0.034 | |||
| IG | 6.4 (1.6) | 6.3 (1.9) | 6.2 (1.9) | within-subjects | 0.823 | 0.001 |
| SC | 6.9 (2.1) | 6.4 (2.3) | 6.9 (1.6) | interaction | 0.505 | 0.013 |
The interaction is between the time visits and the treatment groups
IG stands for Intervention Group
SCG stands for Standard Care Group
Individual differences, including age, cancer type, and marital status were not significantly correlated with hair loss distress.
Coping with Cancer
Patients in this study tend to have higher active coping scores than avoidance coping scores (t-test = 15.77, df = 86, p < .001); and their coping styles were not found to change significantly over time. At T1, the active coping mean was 40.2 (SD = 6.1) while the avoidance coping mean was 22.3 (SD = 4.3). No significant differences were found between treatment groups. Avoidance coping score was positively correlated with hair loss distress (ρ=.328, p = .032) and GSI (ρ= .667, p < .001); patients with higher avoidance score tend to have higher distress levels.
Limitations
Several limitations should be mentioned in this evaluation study. A larger sample size would have permitted greater power to investigate group differences. The relative lack of ethnic diversity prevented the investigation of ethnic group differences. Finally, the Cancer Center does not currently formally evaluate the use of Ramona’s room. As such, the collection of information from the SCG patients regarding their reactions to using the resource room was not available from which to compare to the IG patients feedback on the HAAIR system. Only receipt of the NIH pamphlet and the availability of the Interviewer during data collection period to answer questions were assured.
DISCUSSION
The development of a computer imaging system that demonstrates baldness as well as interactively illustrates how women would look in a variety of wigs and hair styles was shown to be feasible and acceptable to patients in this evaluation study as well as being a cost effective resource. The HAAIR system can be operated on a desktop or portable computer requiring little physical space in a clinic. Female patients found this system to have high acceptability and experienced it to be user-friendly, particularly because of the use of a touch screen that required very little computer literacy. The system is a useful educational resource that creates a realistic experience of hair loss and confrontation with baldness that could be rehearsed prior to the actual event.
There were certain inherent advantages of the HAAIR system over a dedicated on-site resource specifically for hair loss in a clinical setting. First, the amount of physical space needed for the HAAIR system is much less than an entire resource room. While the lack of documentation of use of Ramona’s room was a limitation of the study, oncology nurses, cancer health educators and the clinical psychologist report that most of their patients probably visit the room at least once. Since women report that obtaining written material still left them feeling “unprepared” for alopecia, it seems likely that the Standard Care patients may have visited the resource room and that the combination of the educational NIH pamphlet and the use of the resource room showed similar effectiveness in reducing alopecia distress among patients by Time 2. Second, the HAAIR system has the potential to prevent or reduce fatigue among patient seeking to actively prepare for hair loss by viewing themselves bald and trying on various hair and wig images that might be used to disguise their baldness during recuperation. Third, the HAAIR system is portable. In this study, we choose to recruit only patients who could come to the IG site for the study. It is also possible to take the HAAIR system on a portable computer to patients who are confined to their home or living a distance from the hospital and who do not have the energy and/or funds to transport to the Breast Center to use the system. Fourth, the cost of the HAAIR system (approximately $5,000) is significantly less than the cost of building or dedicating and equipping an entire resource room.
The IG patients were as likely but not more likely to report reduced overall general psychological distress with regard to having cancer than were patients in the Standardized Care Group, as measured by the GSI and three subscale symptom scores of the BSI. It appears that the single-session exposure to the HAAIR system is not associated with a clinical effect any more than was a one-time exposure to the SCG resource room. This suggests that both the HAAIR system and cancer Center Resource room function in a patient education capacity and not specifically as a clinical resource to address overall general psychological distress associated with having cancer.
Based on the coping theory of Lazarus and Folkman [52], which defined coping as cognitive and behavioral efforts to manage stressful encounters, coping strategies were not defined as inherently adaptive nor maladaptive. However, prospective research aimed at delineating outcomes in coping with the stress of a breast cancer diagnosis [53] found that cognitive avoidance was the only unique variable that predicted negative affect. A more recent study of alopecia [34] distress in a sample of participants recruited for internet support groups with various causes for hair loss, found that avoidant coping was associated with poorer quality of life but not active coping. In our study, there were more patients with an active than avoidance style of coping who chose to take part in the HAAIR study. It is not surprising that coping style did not change in this study, as it is a rather stable variable and the intervention included only a single session with the patient. However, it may be that coping behavior could change, if more women with avoidant coping styles became exposed to the tool by having it available in the clinic or through its introduction as part of standard patient education about alopecia.
Future Research
This study to test the effectiveness of using computer imaging technology to facilitate coping and adjustment in patients with alopecia may contribute to future research associated with guided imagery within the structure of virtual reality technology for treating traumatic side effects related to alopecia experienced by many female cancer patients. Virtual Reality Exposure therapy has been effective for treating Vietnam Veterans for PTSD, [54] and patient’s with anxiety disorders (e.g. phobias) [55]. In addition, its use is being explored in Italy, where a virtual reality environment was recreated to treat a disturbed body image in a non-clinical sample with reported positive results [38]. To date, virtual reality has been explored as a distraction intervention to relieve symptoms of distress for cancer patients receiving chemotherapy with mixed results. In one study, patients reported a positive effect for distraction and perceived time of treatment but did not report a decrease in distress symptoms [56] while another study of older women with breast cancer using virtual reality distraction reported lower anxiety levels than controls [57] Since the HAAIR system was not envision as a distraction tool, future research and development might focus on desensitization through exposure within a clinical protocol that provided psychological support.
In the present study, when hair loss distress was investigated as the outcome, rather than general psychological distress not specific to alopecia, a time and group trend effect was found. Future studies on this topic would benefit from a larger sample size to further investigate this finding. Furthermore, the use of the HAAIR computer imaging system may have potential as an adjunct clinical tool using guided imagery techniques and interventions that have been found to be successful in improving quality of life in women recovering from cancer [36, 58–61] If the tool is used within a cancer center clinic, feedback forms and referrals to psychosocial support should be made available to users.
Table 4.
Means and standard deviation (SD) of the coping style across time by intervention group. Statistics for the intervention effect and the time effect.
| Intervention Group | Statistic | P-value | |||
|---|---|---|---|---|---|
| Time | Standard Care Group | Intervention Group | |||
| Active Cope | Baseline | 40.3 (6.27) | 40.2 (6.13) | Between subject effect | 0.188 |
| Mean (SD) | After Hair Loss | 37.4 (8.27) | 33.2 (15.08) | Within subject effect | 0.002 |
| After Hair Re-grow | 37.4 (7.83) | 30.6 (15.86) | |||
| Avoidance Cope | Baseline | 22.4 (4.85) | 21.6 (3.62) | Between subject effect | 0.268 |
| Mean (SD) | After Hair Loss | 22.5 (5.68) | 21.2 (3.82) | Within subject effect | 0.702 |
| After Hair Re-grow | 20.9 (4.67) | 21.5 (3.82) | |||
Acknowledgments
The development of the project began with charitable gift to the University of Virginia Cancer Center from Mr. Howard Melton in memory of his late wife. This project was completed with funding from the National Cancer Institute, Division of Cancer Control & Population Sciences, Grant # R44-CA099873-02 to Eugene Parker, Jr. PhD.
References
- 1.Carpenter JS, Brockopp DY. Evaluation of self-esteem of women with cancer receiving chemotherapy. Oncol Nurs Forum. 1994 May;21(4):751–7. [PubMed] [Google Scholar]
- 2.McGarvey EL, Baum LD, Pinkerton RC, Rogers LM. Psychological sequelae and intervention for treatment-induced alopecia among female cancer patients. Cancer Pract. 2001 Nov-Dec;9(6):283–9. doi: 10.1046/j.1523-5394.2001.96007.x. [DOI] [PubMed] [Google Scholar]
- 3.Munstedt K, Manthey N, Sachsse S, Vahrson H. Changes in self-concept and body image during alopecia induced cancer chemotherapy. Support Care Cancer. 1997 Mar;5(2):139–43. doi: 10.1007/BF01262572. [DOI] [PubMed] [Google Scholar]
- 4.Pickard-Holley S. The symptom experience of alopecia. Semin Oncol Nurs. 1995 Nov;11(4):235–8. doi: 10.1016/s0749-2081(05)80003-8. [DOI] [PubMed] [Google Scholar]
- 5.Lemieux J, Maunsell E, Provencher L. Chemotherapy-induced alopecia and effects on quality of life among women with breast cancer: A literature review. Psychooncology. 2008 Apr;17(4):317–28. doi: 10.1002/pon.1245. [DOI] [PubMed] [Google Scholar]
- 6.Tierney AJ, Taylor J, Closs SJ. Knowledge, expectations and experiences of patients receiving chemotherapy for breast cancer. Scand J Caring Sci. 1992;6(2):75–80. doi: 10.1111/j.1471-6712.1992.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 7.Freedman TG. Social and cultural dimensions of hair loss in women treated for breast cancer. Cancer Nurs. 1994 Aug;17(4):334–41. [PubMed] [Google Scholar]
- 8.Batchelor D. Hair and cancer chemotherapy: consequences and nursing care--a literature study. Eur J Cancer Care (Engl) 2001 Sep;10(3):147–63. doi: 10.1046/j.1365-2354.2001.00272.x. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher J. Women’s experience of hair loss associated with cancer chemotherapy: A qualitative study. Amherst: University of Massachusetts; 1992. Unpublished doctoral dissertation. [Google Scholar]
- 10.Ron IG, Kalmus Y, Kalmus Z, et al. Scalp cooling in the prevention of alopecia in patients receiving depilating chemotherapy. Support Care Cancer. 1997 Mar;5(2):136–8. doi: 10.1007/BF01262571. [DOI] [PubMed] [Google Scholar]
- 11.Keller JF, Blausey LA. Nursing issues and management in chemotherapy-induced alopecia. Oncol Nurs Forum. 1988 sep–Oct;15(5):603–7. [PubMed] [Google Scholar]
- 12.Nerenz DR, Love RR, Leventhal H, Easterling DV. Psychosocial consequences of cancer chemotherapy for elderly patients. Health Serv Res. 1986 Feb;20(6 Pt2):961–76. [PMC free article] [PubMed] [Google Scholar]
- 13.Smith FP, McCabe MS. Preventing chemotherapy-induced alopecia. Am Fam Physician. 1983 Jul;28(1):182–4. [PubMed] [Google Scholar]
- 14.Wagner L, Gorely M. Body image and patients experiencing alopecia as a result of cancer chemotherapy. Cancer Nurs. 1979 Oct;2(5):365–9. [PubMed] [Google Scholar]
- 15.Williams J, Wood C, Cunningham-Warburton P. A narrative study of chemotherapy-induced alopecia. Oncol Nurs Forum. 1999 Oct;26(9):1463–8. [PubMed] [Google Scholar]
- 16.Anderson JE, Hunt JM, Smith IE. Prevention of doxorubicin-induced alopecia by scalp cooling in patients with advanced breast cancer. Br Med J (Clin Res Ed) 1981 Feb 7;282(6262):423–4. doi: 10.1136/bmj.282.6262.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christodoulou C, Klouvas G, Efstathiou E, et al. Effectiveness of the MSC cold cap system in the prevention of chemotherapy-induced alopecia. Oncology. 2002;62(2):97–102. doi: 10.1159/000048253. [DOI] [PubMed] [Google Scholar]
- 18.Macduff C, Mackenzie T, Hutcheon A, et al. The effectiveness of scalp cooling in preventing alopecia for patients receiving epirubicin and docetaxel. Eur J Cancer Care (Engl) 2003 Jun;12(2):154–61. doi: 10.1046/j.1365-2354.2003.00382.x. [DOI] [PubMed] [Google Scholar]
- 19.Protière C, Evans K, Camerlo J, et al. Efficacy and tolerance of a scalp-cooling system for prevention of hair loss and the experience of breast cancer patients treated by adjuvant chemotherapy. Support Care Cancer. 2002 Oct;10(7):529–37. doi: 10.1007/s00520-002-0375-y. [DOI] [PubMed] [Google Scholar]
- 20.Duvic M, Lemak NA, Valero V, et al. A randomized trial of minoxidil in chemotherapy-induced alopecia. J Am Acad Dermatol. 1996 Jul;35(1):74–8. doi: 10.1016/S0190-9622(96)90500-9. [DOI] [PubMed] [Google Scholar]
- 21.Roy RK, Thakur M, Dixit VK. Development and evaluation of polyherbal formulation for hair growth-promoting activity. J Cosmet Dermatol. 2007 Jun;6(2):108–12. doi: 10.1111/j.1473-2165.2007.00305.x. [DOI] [PubMed] [Google Scholar]
- 22.Land SR, Koopec JA, Youthers G, et al. Health-related quality of life in axillary node-negative breast cancer patients undergoing AC versus CMF chemotherapy: Findings from the National Surgical Adjuvant Breast and Bowel Project B-23. Breast Cancer Res Treat. 2004 Jul;86(2):153–64. doi: 10.1023/B:BREA.0000032983.87966.4e. [DOI] [PubMed] [Google Scholar]
- 23.Sitzia J, Juggins L. Side effects of cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) chemotherapy for breast cancer. Cancer Pract. 1998 Jan–Feb;6(1):13–21. doi: 10.1046/j.1523-5394.1998.1998006013.x. [DOI] [PubMed] [Google Scholar]
- 24.Koopman C, Hermanson K, Diamond S, et al. Social support, life stress, pain and emotional adjustment to advance breast cancer. Psychooncology. 1998 Mar-Apr;7(2):107–11. doi: 10.1002/(SICI)1099-1611(199803/04)7:2<101::AID-PON299>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 25.McGarvey EL, Canterbury RJ, Koopman C, et al. Acute stress disorder following diagnosis of cancer. International Journal of Rehabilitation and Health. 1998 Jan;4(1):1–15. [Google Scholar]
- 26.Roseman S. Cancer and stigma: experience of patients with chemotherapy-induced alopecia. Patient Educ Couns. 2004 Mar;52(3):333–9. doi: 10.1016/S0738-3991(03)00040-5. [DOI] [PubMed] [Google Scholar]
- 27.Boehmke MM, Dickerson SS. Symptom, symptom experience and symptom distress encountered by women with breast cancer undergoing current treatment modalities. Cancer Nurs. 2005 Sep–Oct;28(5):382–9. doi: 10.1097/00002820-200509000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Frith H, Harcourt D, Fussell A. Anticipating an altered appearance: Women undergoing chemotherapy treatment for breast cancer. Eur J Oncol Nurs. 2007 Dec;11(5):385–91. doi: 10.1016/j.ejon.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Holland J, Rowland J. Handbook of psyhchooncology: Psychologic care of the patient with cancer. New: Oxford University Press; 1990. [Google Scholar]
- 30.Classen C, Koopman C, Angell KL, Spiegel D. Coping styles associated with psychological adjustment to metastatic breast cancer. Health Psycholgy. 1996 Nov;15(6):434–7. doi: 10.1037//0278-6133.15.6.434. [DOI] [PubMed] [Google Scholar]
- 31.Carver CS, Pozo C, Harris SD, et al. How coping mediates the effect of optimism on distress: A study of women with early stage breast cancer. J Pers Soc Psychology. 1993 Nov;65(2):375–390. doi: 10.1037//0022-3514.65.2.375. [DOI] [PubMed] [Google Scholar]
- 32.Cartwright T, Endean N, Porter A. Illness perceptions, coping and quality of life in patients with alopecia. Br J Dermatol. 2009 May;160(5):1034–1039. doi: 10.1111/j.1365-2133.2008.09014.x. [DOI] [PubMed] [Google Scholar]
- 33.Helms RL, O’Hea EL, Corso M. Body image issues in women with breast cancer. Psychol Health Med. 2008 May;13(3):313–325. doi: 10.1080/13548500701405509. [DOI] [PubMed] [Google Scholar]
- 34.Holland J, Weiss T. The new standard of quality cancer care: Integrating the psychosocial aspects in routine cancer from diagnosis through survivorship. Cancer J. 2008 Nov–Dec;14(6):425–428. doi: 10.1097/PPO.0b013e31818d8934. [DOI] [PubMed] [Google Scholar]
- 35.Bental DS, Cawsey A, Jones R. Patient information systems that tailor to the individual. Patient Educ Couns. 1999 Feb;36(2):171–80. doi: 10.1016/s0738-3991(98)00133-5. [DOI] [PubMed] [Google Scholar]
- 36.Freeman L, Cohen L, Stewart M, et al. Imagery intervention for recovering breast cancer patients: Clinical trial of safety and efficacy. J Soc Integr Oncol. 2008 Spring;6(2):67–75. [PubMed] [Google Scholar]
- 37.Lewis D. Computer-based approaches to patient education: A review of the literature. J Am Med Inform Assoc. 1999 Jul–Aug;6(4):272–82. doi: 10.1136/jamia.1999.0060272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Riva G. Modifications of body-image induced by virtual reality. Perceptual and Motor Skill. 1998;86(1):163–70. doi: 10.2466/pms.1998.86.1.163. [DOI] [PubMed] [Google Scholar]
- 39.Robinson TN, Patrick K, Eng TR, Gustafson D. An evidence-based approach to interactive health communication--A challenge to medicine in the information age. JAMA. 1998 Oct;280(14):1264–9. doi: 10.1001/jama.280.14.1264. [DOI] [PubMed] [Google Scholar]
- 40.Wofford JL, Smith ED, Miller DP. The multimedia computer for office-based patient education: A systematic review. Patient Educ Couns. 2005 Nov;59(2):148–57. doi: 10.1016/j.pec.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 41.Takabayashi K, Tomita M, Tsumoto S, et al. Computer-assisted instructions for patients with bronchial asthma. Patient Educ Couns. 1999 Nov;38(3):241–248. doi: 10.1016/s0738-3991(99)00015-4. [DOI] [PubMed] [Google Scholar]
- 42.van Schaik P, Ahmed T, Suvakovic N, et al. Effect of an educational multimedia prostate program on the International Prostate Symptom Score. Eur Urol. 1999;36(1):36–39. doi: 10.1159/000019924. [DOI] [PubMed] [Google Scholar]
- 43.Fitz-Gibbon CT, Morris LL. How to design a Program Evaluation. Sage Publications, Inc.; California: 1987. [Google Scholar]
- 44.Schulz KF, Grimes DA. Unequal group sized in randomized trials: guarding against guessing. Lancet. 2002 Mar;359(9310):966–970. doi: 10.1016/S0140-6736(02)08029-7. [DOI] [PubMed] [Google Scholar]
- 45.Derogatis LR. BSI-18: Brief Symptom Inventory 18: Administration, Scoring and Procedures Manual, NCS Pearson, Inc, P.O. Box 1416, Minneapolis, MN, 55440. 2001,
- 46.Baum L, McGarvey E. Importance of hair questionnaire A, 1999, copyright.
- 47.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. J Pers Soc Psychol. 1989 Feb;56(2):267–83. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 48.Carver CS. You want to measure coping but your portocol’s too long: Consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 49.Lewis D. Computer-based approaches to patient education: A review of the literature. J Am Med Inform Assoc. 1999 Jul–Aug;6(4):272–282. doi: 10.1136/jamia.1999.0060272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cohen J. Statistical power analysis for the behavioral sciences. 2. Lawrence Erlbaum Associates; New Jersey: 1988. [Google Scholar]
- 51.Fox K. Personal communication with Medical Center, Facilities Plan & Capital Development staff. University of Virginia; Charlottesville: 2009. [Google Scholar]
- 52.Lazarus RS, Folkman S. Stress, appraisal and coping. Springer; New York: 1984. [Google Scholar]
- 53.Stanton Al, Snider PR. Coping with a breast cancer diagnosis: a prospective study. Health Psychol. 1993 Jan;12(1):16–23. doi: 10.1037//0278-6133.12.1.16. [DOI] [PubMed] [Google Scholar]
- 54.Rothbaum BO, Hodges L, Alarcon R, et al. Virtual reality exposure therapy for PTSD Vietnam veterans: A case study. J Trauma Stress. 1999 Apr;12(2):263–271. doi: 10.1023/A:1024772308758. [DOI] [PubMed] [Google Scholar]
- 55.Rothbaum BO, Hodges LF. The use of virtual reality exposure in the treatment of anxiety disorder. Behav Modif. 1999 Oct;23(4):507–525. doi: 10.1177/0145445599234001. [DOI] [PubMed] [Google Scholar]
- 56.Schneider SM, Hood LE. Virtual reality: a distraction intervention for chemotherapy. Onclol Nurs Forum. 2007 Jan;34(1):39–46. doi: 10.1188/07.ONF.39-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schneider SM, Ellis M, Coombs WT, et al. Virtual reality intervention for older women with breast cancer. Cyberpsychol Behav. 2003 Jun;6(3):301–307. doi: 10.1089/109493103322011605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baider L, Uziely B, De-Nour AK. Progressive muscle relaxation and guided imagery in cancer patients. Gen Hosp Psychiatry. 1994 Sep;16(5):340–47. doi: 10.1016/0163-8343(94)90021-3. [DOI] [PubMed] [Google Scholar]
- 59.Edwards DJA. Cognitive restructuring through guided imagery: Lessons from Gestalt therapy. In: Freeman A, Simon KM, Neutler LE, Arkowitz H, editors. Comprehensive Handbook of Cognitive Therapy. Plenum Press; New York: 1989. [Google Scholar]
- 60.Kolcaba K, Fox C. The effects of guided imagery on comfort of women with early stage breast cancer undergoing radiation therapy. Oncol Nurs Forum. 1999 Jan–Feb;26(1):67–72. [PubMed] [Google Scholar]
- 61.Lazarus A. In the mind’s eye: The power of imagery for personal enrichment. New York: Guilford Press; 1977. [Google Scholar]