Abstract
The survival times of Caenorhabditis elegans worms infected with Legionella pneumophila from day 7.5 or later after hatching were shorter than those of uninfected worms. However, nematodes fed bifidobacteria prior to Legionella infection were resistant to Legionella. These nematodes may act as a unique alternative host for Legionella research.
Legionella pneumophila, an environmental bacterium naturally found in fresh water, is the major causative agent of Legionnaires' disease (7). Fresh water amoebas, a natural host of Legionella, have been used as an infection model to study invasion of Legionella into human macrophages and subsequent intracellular growth (15). However, analyses using these protozoa have inevitably concentrated on the intracellular lifestyle of L. pneumophila. The fate of Legionella organisms in nonmammalian metazoans had not been described (10) until a very recent report by Brassinga et al. (6).
Numerous authors have reported Caenorhabditis elegans to be a suitable model to investigate virulence-associated factors of human pathogens (2, 8, 11, 14, 16, 20, 23, 24, 30, 31, 33). In the present study, we examined whether C. elegans can serve as an alternative host for L. pneumophila. Although the nematocidal activity of Legionella has been described recently, the nematodes in the previous study were infected with the pathogen on buffered charcoal yeast extract (BCYE) agar plates, which can support Legionella growth (6). In contrast, our experiments were independently performed on simple agar plates to exclude the possibility that the inoculated pathogen would have proliferated regardless of whether it had successfully infected the nematodes and derived nutrition from the hosts. Garsin et al. showed that nutrition available in agar plates does influence the virulence of pathogens on the medium (9). Furthermore, some pathogens produce toxic metabolites on nutrient medium in situ (3), and thus, we also avoided this possibility. Moreover, we focused on the effects of worm age, since Legionella is prone to infect elderly people.
Age at infection is likely one of the most important determinants of disease morbidity and mortality (18). Since Legionella organisms are prone to infect elderly people opportunistically, infections in young and older nematodes were compared. Furthermore, survival curves were compared between worms fed Escherichia coli OP50 (OP), an international standard food for these organisms, and those fed bifidobacteria prior to infection with Legionella organisms, since lactic acid bacteria exert beneficial effects on human and animal health (21).
Nematocidal assays.
As a standard strain of C. elegans, Bristol N2 was maintained and propagated on nematode growth medium (NGM) according to standard techniques using OP (25). Tryptone soya agar (Oxoid, Basingstoke, United Kingdom) was used to culture OP at 37°C. The virulent and attenuated L. pneumophila strains used in this study are listed in Table 1. All attenuated strains were produced by transposon insertion into the Icm/Dot (intracellular multiplication/defect in organelle trafficking) type IV secretion system genes, which have been shown previously to be essential for virulence (5, 22). Legionella strains were cultured using BCYE agar plates (Oxoid) at 37°C for 2 days. Bifidobacterium infantis ATCC 15697 was also used to feed the worms, being one of five lactic acid bacteria that we previously found to have a longevity effect on nematodes (13). Transoligosaccharide (TOS) propionate agar (Eiken Chemical Co., Tochigi, Japan) was used to grow B. infantis anaerobically at 37°C (32). Bacteria were recovered from the agar plates, and each 10 mg (wet weight) of the bacteria suspended in 50 μl of M9 buffer (25) was spread onto peptone-free modified NGM (mNGM) in 5.0-cm-diameter petri dishes for feeding or infecting of C. elegans.
TABLE 1.
L. pneumophila strains used in this study
| Strain | Description | Reference or source |
|---|---|---|
| Philadelphia-1 (ATCC 33152) | Virulent, serogroup 1 | ATCC |
| AM511 | Philadelphia-1 Smr r− m+ | 17 |
| JR32 | Salt-sensitive derivative of AM511 | 22 |
| LELA2883 | JR32 dotB2883::Tn903dIIlacZ (insertion in icm/dot region I) | 22 |
| LELA3118 | JR32 dotA3118::Tn903dIIlacZ (insertion in icm/dot region I) | 22 |
| LELA3473 | JR32 icmR3473::Tn903dIIlacZ (insertion in icm/dot region II) | 22 |
| LELA4432 | JR32 icmE4432::Tn903dIIlacZ (insertion in icm/dot region II) | 22 |
| LELA3244 | JR32 icmD3244::Tn903dIIlacZ (insertion in icm/dot region II) | 22 |
| LELA3393 | JR32 icmB3393::Tn903dIIlacZ (insertion in icm/dot region II) | 22 |
| LELA1718 | JR32 icmF1718::Tn903dIIlacZ (insertion in icm/dot region II) | 22 |
Worms were generated from eggs released after exposure of adult hermaphrodites to a sodium hypochlorite-sodium hydroxide solution as described previously (28). The fertilized egg suspension was incubated overnight at 25°C to allow hatching, and the suspension of larval stage 1 (L1 stage) worms was centrifuged at 156 × g for 1 min. The supernatant was removed, and the remaining larvae were transferred onto fresh mNGM plates covered with OP and incubated at 25°C. Because the reproductive system regulates aging in C. elegans (12), in order not to disturb natural pubescence, worms were fed on OP until the start of Legionella infection.
Nematocidal assays were begun with adult worms, which were allocated at 30 each onto mNGM plates covered with suspensions of each Legionella strain. Once the feeding bacteria were switched from OP to Legionella, worms were given the pathogen during the entire assay time until death. The plates were incubated at 25°C, and live and dead worms were counted at least every 24 h. Worms produce progeny that develop into adults in 3 days, rendering it difficult to identify the original worms. Therefore, the original worms were transferred onto fresh plates at approximately 2-day intervals. A worm was considered dead when it failed to respond to a gentle touch with a worm picker. Worms that died as a result of getting stuck to the wall of the plate were excluded from the analysis. All nematode survival studies were conducted by a researcher with no prior knowledge of the bacterial strains fed to the worms. Nematode survival was calculated by the Kaplan-Meier method, and survival differences were tested for significance using the log rank test.
Influence of age of C. elegans on L. pneumophila infections.
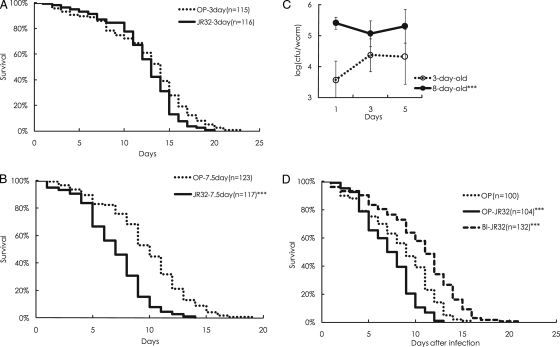
No significant differences in survival between 3-day-old worms fed OP and 3-day-old worms infected with virulent Legionella strains were seen (Fig. 1 A). However, when the worms were infected from 7.5 days after hatching, the virulent Legionella strains were obviously nematocidal (Fig. 1B).
FIG. 1.
Survival of nematodes infected with L. pneumophila. (A and B) At 3 days (A) or 7.5 days (B) of age, nematodes were transferred onto agar plates covered with the virulent L. pneumophila strain JR32. The survival curves were compared with those of worms fed on OP. (C) The number of Legionella cells recovered from the nematodes that started ingesting Legionella at 3 days of age was significantly lower than the number recovered from worms infected at 8 days of age. The results are presented as the means ± the standard errors, and the data were analyzed by two-factor factorial analysis of variance (ANOVA). (D) Adult worms fed a diet of bifidobacteria from 3 days of age for 5 days were transferred onto Legionella plates for infection, and survival curves were drawn. Nematodes fed bifidobacteria (BI) were significantly more resistant than controls to the pathogen (JR). All experiments were performed twice in duplicate or triplicate. *** indicates statistical significance at a P value of <0.001.
The present study is the first to show that L. pneumophila is virulent to elderly worms. Our previous study showed that Salmonella enterica is clearly virulent to both older and younger worms, although more so to elderly worms (13). These findings appear to be consistent with the epidemiological characteristics of both pathogens in humans: Legionella tends to infect older people in an opportunistic manner, while Salmonella can cause enteritis irrespective of host age.
To examine whether the virulence of Legionella correlates with its ability to accumulate in the nematodes, the number of organisms in the nematodes was determined according to the method of Garsin et al. (9) with some modifications. Each nematode was mechanically disrupted using a microtube pestle (Scientific Specialties Inc., Lodi, CA). The number of Legionella cells was determined using BCYE agar plates supplemented with polymyxin B at 80 IU/ml. The number of Legionella cells recovered from worms infected from 3 days after hatching was smaller than the number recovered from worms infected from 8 days after hatching (Fig. 1C); this logarithmic difference cannot be explained by the difference in body size (the area of the worm's projection) between elderly and young worms since the bodies of the 8-day-old worms were 20% larger than those of the 3-day-old worms.
Although there are no data to explain the vulnerability of the older worms, the ability of the older worms to adapt to microbes might have deteriorated, a possibility consistent with the finding that the level of heat shock protein 16 in 16-day-old worms responding to heat stress had declined to about 50% of that in 4-day-old young adults (34). Since nematodes have to switch distinct genes on and off to defend against and digest different species of ingested pathogens (35), it is likely that the worms that first encountered the Legionella cells when they were young were able to respond effectively to Legionella and that the 8-day-old worms were not.
Virulence of transposon insertion mutants in nematodes.
On the basis of these findings, 7.5- to 8-day-old nematodes were used as the hosts to examine the virulence of the Legionella strains. Although the parent strain JR32 showed significant nematocidal activity, all the genetically attenuated mutants, having been demonstrated to be less virulent in the lungs of guinea pigs (19) or in human macrophages (22), were considered nonpathogenic, similar to OP (Table 2). Interestingly, the attenuated mutant LELA1718, which is reportedly cytolethal in contrast to the other attenuated mutants in a cytotoxicity assay with HL-60-derived human macrophages (22), showed modest virulence in the nematodes compared to other avirulent mutants.
TABLE 2.
Mean and maximum survival days of worms infected with L. pneumophila strains
| Bacterial strain | Nematode age (days) at start of infection | Mean survival timea (days) ± SE | Maximum survival time (days) | No. of nematodes (no. of experiments)b |
|---|---|---|---|---|
| E. coli OP (control) | 3.0 | 13.20 ± 0.45 | 23 | 115 (2) |
| L. pneumophila JR32 | 3.0 | 12.80 ± 0.34 | 20 | 116 (2) |
| E. coli OP (control) | 7.5 | 10.20 ± 0.33 | 19 | 123 (2) |
| L. pneumophila JR32 | 7.5 | 7.40 ± 0.26*** | 14 | 117 (2) |
| E. coli OP (control) | 7.5 | 10.17 ± 0.44 | 17 | 70 (1) |
| L. pneumophila LELA2883 | 7.5 | 10.50 ± 0.54 | 20 | 69 (1) |
| L. pneumophila LELA3118 | 7.5 | 10.00 ± 0.53 | 21 | 72 (1) |
| L. pneumophila LELA3473 | 7.5 | 9.76 ± 0.49 | 19 | 72 (1) |
| L. pneumophila LELA4432 | 7.5 | 9.62 ± 0.49 | 18 | 74 (1) |
| L. pneumophila LELA3244 | 7.5 | 11.12 ± 0.51 | 18 | 60 (1) |
| L. pneumophila LELA3393 | 7.5 | 9.64 ± 0.44 | 16 | 65 (1) |
| L. pneumophila LELA1718c | 7.5 | 8.74 ± 0.43* | 15 | 66 (1) |
| E. coli OP (control) | 7.5 | 9.14 ± 0.38 | 17 | 78 (1) |
| L. pneumophila LELA1718c | 7.5 | 9.49 ± 0.38 | 15 | 70 (1) |
| E. coli OP (control) | 8.0 | 9.13 ± 0.45 | 14 | 48 (1) |
| L. pneumophila LELA1718c | 8.0 | 7.33 ± 0.42** | 13 | 48 (1) |
| L. pneumophila LELA4432 | 8.0 | 10.00 ± 0.52 | 18 | 46 (1) |
*, **, and *** indicate a statistically significant difference from the control at P values of <0.05, <0.01, and <0.001, respectively.
Each experiment was performed in duplicate or triplicate.
When worms were infected with LELA1718 at 7.5 days after hatching, the strain showed weak virulence in one of two experiments. The 8-day-old worms seemed to be more vulnerable to the strain.
The pathogenicity of L. pneumophila in C. elegans seems to correlate well with that in macrophages, and the nematode could serve as a unique host of Legionella spp. Indeed, several genes of human pathogens have been recently discovered to be involved in virulence in C. elegans, and some of these are also required for virulence in mammalian systems (4, 16, 26, 29). However, the pathogenesis of infections with Legionella spp. in nematodes remains to be elucidated. The numbers of organisms recovered from the worms were not significantly different among the three Legionella strains (JR32, LELA1718, and LELA4432) that showed different levels of pathogenicity. Since the nematodes actively take in bacteria, the differences in virulence would not result in a difference in bacterial number as long as the levels of bacterial resistance to antimicrobial peptides in the worms did not differ among the bacterial strains. Functional defects in the Icm/Dot type IV secretion system could have decreased the secretion of toxic effectors from the attenuated mutants and consequently increased worm survival. Programmed cell death in C. elegans appears to be an important defense response against pathogen attack and stress (1). Since Icm/Dot plays a role to inhibit programmed cell death (6), the attenuated mutants appeared not to reduce worm survival.
Influence of bifidobacteria on resistance against Legionella infection.
Three-day-old worms were assigned to either a control group that continued to be fed OP or to a group that was fed bifidobacteria for 5 days. The 8-day-old worms were then transferred onto mNGM covered with Legionella. Nematodes fed bifidobacteria were clearly resistant to subsequent Legionella infection, in contrast to nematodes fed OP before the Legionella infection, and nematodes fed bifidobacteria survived longer than the control worms fed OP throughout the experiment (Fig. 1D); however, the numbers of Legionella organisms recovered from the worms showed no significant difference between groups fed with bifidobacteria or OP. These results are similar to our previous findings that lactic acid bacteria are effective in increasing both the longevity of C. elegans and the host defense against Salmonella (13). Our ongoing experiments using mutated nematodes suggest that bifidobacteria enhance the worms' host defense via the PMK-1/p38 mitogen-activated protein kinase signaling pathway (unpublished results), which plays an important role in the innate immunity of C. elegans (27).
In conclusion, we found that L. pneumophila significantly reduced the life span of C. elegans via icm/dot-associated pathogenicity when the pathogen infected older worms. Since the worms died over the course of several days, the pathogen is considered to have caused what is known as slow killing (30). C. elegans can be an additional unique model to study opportunistic infection with Legionella spp.
Acknowledgments
We are grateful to Howard A. Shuman for kindly providing the L. pneumophila AM511, JR32, and LELA strains. The nematodes used in this work were kindly provided by T. Stiernagle at the Caenorhabditis Genetics Center, which is funded by the NIH National Center for Research Resources (NCRR).
This study was supported in part by a grant-in-aid from the Graduate School of Human Life Science, Osaka City University.
Footnotes
Published ahead of print on 23 April 2010.
REFERENCES
- 1.Aballay, A., and F. M. Ausubel. 2001. Programmed cell death mediated by ced-3 and ced-4 protects Caenorhabditis elegans from Salmonella typhimurium-mediated killing. Proc. Natl. Acad. Sci. U. S. A. 98:2735-2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aballay, A., P. Yorgey, and F. M. Ausubel. 2000. Salmonella typhimurium proliferates and establishes a persistent infection in the intestine of Caenorhabditis elegans. Curr. Biol. 10:1539-1542. [DOI] [PubMed] [Google Scholar]
- 3.Anyanful, A., J. M. Dolan-Livengood, T. Lewis, S. Sheth, M. N. Dezalia, M. A. Sherman, L. V. Kalman, G. M. Benian, and D. Kalman. 2005. Paralysis and killing of Caenorhabditis elegans by enteropathogenic Escherichia coli requires the bacterial tryptophanase gene. Mol. Microbiol. 57:988-1007. [DOI] [PubMed] [Google Scholar]
- 4.Begun, J., C. D. Sifri, S. Goldman, S. B. Calderwood, and F. M. Ausubel. 2005. Staphylococcus aureus virulence factors identified by using a high-throughput Caenorhabditis elegans-killing model. Infect. Immun. 73:872-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berger, K. H., and R. R. Isberg. 1993. Two distinct defects in intracellular growth complemented by a single genetic locus in Legionella pneumophila. Mol. Microbiol. 7:7-19. [DOI] [PubMed] [Google Scholar]
- 6.Brassinga, A. K., J. M. Kinchen, M. E. Cupp, S. R. Day, P. S. Hoffman, and C. D. Sifri. 2010. Caenorhabditis is a metazoan host for Legionella. Cell. Microbiol. 12:343-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fields, B. S., R. F. Benson, and R. E. Besser. 2002. Legionella and Legionnaires' disease: 25 years of investigation. Clin. Microbiol. Rev. 15:506-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gan, Y. H., K. L. Chua, H. H. Chua, B. Liu, C. S. Hii, H. L. Chong, and P. Tan. 2002. Characterization of Burkholderia pseudomallei infection and identification of novel virulence factors using a Caenorhabditis elegans host system. Mol. Microbiol. 44:1185-1197. [DOI] [PubMed] [Google Scholar]
- 9.Garsin, D. A., C. D. Sifri, E. Mylonakis, X. Qin, K. V. Singh, B. E. Murray, S. B. Calderwood, and F. M. Ausubel. 2001. A simple model host for identifying Gram-positive virulence factors. Proc. Natl. Acad. Sci. U. S. A. 98:10892-10897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hilbi, H., S. S. Weber, C. Ragaz, Y. Nyfeler, and S. Urwyler. 2007. Environmental predators as models for bacterial pathogenesis. Environ. Microbiol. 9:563-575. [DOI] [PubMed] [Google Scholar]
- 11.Hoshino, K., C. Yasui, T. Ikeda, K. Arikawa, H. Toshima, and Y. Nishikawa. 2008. Evaluation of Caenorhabditis elegans as the host in an infection model for food-borne pathogens. Jpn. J. Food Microbiol. 25:137-147. [Google Scholar]
- 12.Hsin, H., and C. Kenyon. 1999. Signals from the reproductive system regulate the lifespan of C. elegans. Nature 399:362-366. [DOI] [PubMed] [Google Scholar]
- 13.Ikeda, T., C. Yasui, K. Hoshino, K. Arikawa, and Y. Nishikawa. 2007. Influence of lactic acid bacteria on longevity of Caenorhabditis elegans and host defense against Salmonella enterica serovar Enteritidis. Appl. Environ. Microbiol. 73:6404-6409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joshua, G. W., A. V. Karlyshev, M. P. Smith, K. E. Isherwood, R. W. Titball, and B. W. Wren. 2003. A Caenorhabditis elegans model of Yersinia infection: biofilm formation on a biotic surface. Microbiology 149:3221-3229. [DOI] [PubMed] [Google Scholar]
- 15.Jules, M., and C. Buchrieser. 2007. Legionella pneumophila adaptation to intracellular life and the host response: clues from genomics and transcriptomics. FEBS Lett. 581:2829-2838. [DOI] [PubMed] [Google Scholar]
- 16.Kurz, C. L., S. Chauvet, E. Andres, M. Aurouze, I. Vallet, G. P. Michel, M. Uh, J. Celli, A. Filloux, S. De Bentzmann, I. Steinmetz, J. A. Hoffmann, B. B. Finlay, J. P. Gorvel, D. Ferrandon, and J. J. Ewbank. 2003. Virulence factors of the human opportunistic pathogen Serratia marcescens identified by in vivo screening. EMBO J. 22:1451-1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKinney, R. M., H. W. Wilkinson, H. M. Sommers, B. J. Fikes, K. R. Sasseville, M. M. Yungbluth, and J. S. Wolf. 1980. Legionella pneumophila serogroup six: isolation from cases of legionellosis, identification by immunofluorescence staining, and immunological response to infection. J. Clin. Microbiol. 12:395-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller, E., and N. Gay. 1997. Effect of age on outcome and epidemiology of infectious diseases. Biologicals 25:137-142. [DOI] [PubMed] [Google Scholar]
- 19.Miyamoto, H., S. Yoshida, H. Taniguchi, and H. A. Shuman. 2003. Virulence conversion of Legionella pneumophila by conjugal transfer of chromosomal DNA. J. Bacteriol. 185:6712-6718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mylonakis, E., A. Idnurm, R. Moreno, J. El Khoury, J. B. Rottman, F. M. Ausubel, J. Heitman, and S. B. Calderwood. 2004. Cryptococcus neoformans Kin1 protein kinase homologue, identified through a Caenorhabditis elegans screen, promotes virulence in mammals. Mol. Microbiol. 54:407-419. [DOI] [PubMed] [Google Scholar]
- 21.Naidu, A. S., W. R. Bidlack, and R. A. Clemens. 1999. Probiotic spectra of lactic acid bacteria (LAB). Crit. Rev. Food Sci. Nutr. 39:13-126. [DOI] [PubMed] [Google Scholar]
- 22.Sadosky, A. B., L. A. Wiater, and H. A. Shuman. 1993. Identification of Legionella pneumophila genes required for growth within and killing of human macrophages. Infect. Immun. 61:5361-5373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sifri, C. D., J. Begun, F. M. Ausubel, and S. B. Calderwood. 2003. Caenorhabditis elegans as a model host for Staphylococcus aureus pathogenesis. Infect. Immun. 71:2208-2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sifri, C. D., E. Mylonakis, K. V. Singh, X. Qin, D. A. Garsin, B. E. Murray, F. M. Ausubel, and S. B. Calderwood. 2002. Virulence effect of Enterococcus faecalis protease genes and the quorum-sensing locus fsr in Caenorhabditis elegans and mice. Infect. Immun. 70:5647-5650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stiernagle, T. 1999. Maintenance of C. elegans, p. 51-67. In I. A. Hope (ed.), C. elegans: a practical approach. Oxford University Press, New York, NY.
- 26.Styer, K. L., G. W. Hopkins, S. S. Bartra, G. V. Plano, R. Frothingham, and A. Aballay. 2005. Yersinia pestis kills Caenorhabditis elegans by a biofilm-independent process that involves novel virulence factors. EMBO Rep. 6:992-997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Styer, K. L., V. Singh, E. Macosko, S. E. Steele, C. I. Bargmann, and A. Aballay. 2008. Innate immunity in Caenorhabditis elegans is regulated by neurons expressing NPR-1/GPCR. Science 322:460-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sulston, J., and J. Hodgkin. 1988. Methods, p. 587-606. In W. B. Wood (ed.), The nematode Caenorhabditis elegans. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY.
- 29.Tan, M. W., and F. M. Ausubel. 2000. Caenorhabditis elegans: a model genetic host to study Pseudomonas aeruginosa pathogenesis. Curr. Opin. Microbiol. 3:29-34. [DOI] [PubMed] [Google Scholar]
- 30.Tan, M. W., S. Mahajan-Miklos, and F. M. Ausubel. 1999. Killing of Caenorhabditis elegans by Pseudomonas aeruginosa used to model mammalian bacterial pathogenesis. Proc. Natl. Acad. Sci. U. S. A. 96:715-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tan, M. W., L. G. Rahme, J. A. Sternberg, R. G. Tompkins, and F. M. Ausubel. 1999. Pseudomonas aeruginosa killing of Caenorhabditis elegans used to identify P. aeruginosa virulence factors. Proc. Natl. Acad. Sci. U. S. A. 96:2408-2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thitaram, S. N., G. R. Siragusa, and A. Hinton, Jr. 2005. Bifidobacterium-selective isolation and enumeration from chicken caeca by a modified oligosaccharide antibiotic-selective agar medium. Lett. Appl. Microbiol. 41:355-360. [DOI] [PubMed] [Google Scholar]
- 33.Thomsen, L. E., S. S. Slutz, M. W. Tan, and H. Ingmer. 2006. Caenorhabditis elegans is a model host for Listeria monocytogenes. Appl. Environ. Microbiol. 72:1700-1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walker, G. A., T. M. White, G. McColl, N. L. Jenkins, S. Babich, E. P. Candido, T. E. Johnson, and G. J. Lithgow. 2001. Heat shock protein accumulation is upregulated in a long-lived mutant of Caenorhabditis elegans. J. Gerontol. A Biol. Sci. Med. Sci. 56:B281-B287. [DOI] [PubMed] [Google Scholar]
- 35.Wong, D., D. Bazopoulou, N. Pujol, N. Tavernarakis, and J. J. Ewbank. 2007. Genome-wide investigation reveals pathogen-specific and shared signatures in the response of Caenorhabditis elegans to infection. Genome Biol. 8:R194. [DOI] [PMC free article] [PubMed] [Google Scholar]