Abstract
Summary
Supraglottic devices have changed the face of the airway management. These devices have contributed in a big way in airway management especially, in the difficult airway scenario significantly decreasing the pharyngolaryngeal morbidity. There is a plethora of these devices, which has been well matched by their wider acceptance in clinical practice. ProSeal laryngeal mask airway (PLMA) is one such frequently used device employed for spontaneous as well as controlled ventilation. However, the use of PLMA at times maybe associated with certain problems. Some of the problems related with its use are unique while others are akin to the classic laryngeal mask airway (cLMA). However, expertise is needed for its safe and judicious use, correct placement, recognition and management of its various malpositions and complications. The present article describes the tests employed for proper confirmation of placement to assess the ventilatory and the drain tube functions of the mask, diagnosis of various malpositions and the management of these aspects. All these areas have been highlighted under the heading of troubleshooting PLMA. Many problems can be solved by proper patient and procedure selection, maintaining adequate depth of anaesthesia, diagnosis and management of malpositions. Proper fixation of the device and monitoring cuff pressure intraoperatively may bring down the incidence of airway morbidity.
Keywords: Airway management, Equipment, ProSeal laryngeal mask airway, Classic laryngeal mask airway, Troubleshooting
Introduction
The ProSeal laryngealmask airway (PLMA) is the most complex and advanced version among all the laryngeal mask airways (LMAs).1,2 Some of the problems with its use are unique, such as oesophageal aspiration of air, gastric distension and airway obstruction which can occur even when the PLMA is correctly placed with a proper insertion technique3‐5. The other problems encountered are akin to the classic laryngeal mask airway (cLMA), with varying degrees of frequency and intensity. As a routine after insertion and inflation of the PLMA cuff to 60 cm H2O, the correct placement of the device is confirmed by several observations and certain specific tests designated to assess PLMA positioning and evaluate the ventilatory and drain tube functions of the mask. These diagnostic tests are simple and quick to perform and the first five of the following are more popular.
Visual assessment of depth of insertion
Unobstructed inspiratory and expiratory flow
Suprasternal notch tap test
Gel displacement test
Passage of gastric tube/ polyvinyl chloride (PVC) catheter through drain tube
Soap bubble test
Thread test
Self-inflating bulb technique
Trachlight™ test
Maximum minute ventilation (MMV) test
After confirming correct positioning, the PLMA is properly secured to avoid dislodgement as its cuff is bulkier than that of the cLMA.
1. Visual assessment of depth of insertion
Assess for adequate depth of insertion by examining the relation of the integral bite block to the incisors. Ideally the bite block lies between the teeth but protrudes in case the PLMA is inadequately inserted. Stix and O'Connor in a study of 274 adults, found that when the ProSeal LMA was correctly positioned, the midway point of the bite block was proximal to the incisors in 78% of women and 92% of men. A PLMA with its bite block lying entirely outside the mouth is almost unquestionably malpositioned6
2. Unobstructed inspiratory and expiratory flow
This is assessed by manually ventilating the patient, observing chest movements, capnography, expired tidal volume (VT) of > 8m1/kg, and evaluating the compliance by feel of the bag. The reported incidence of airway obstruction with PLMA has been found to vary from 2-10%.7,8. Increased resistance is suspected with partial obstruction resulting from infolding of the PLMA cuff or downfolding of epiglottis.3 The PLMA, with its large drain tube and cuff, may produce respiratory obstruction by displacing the cricoid cartilage anteriorly thereby exerting direct pressure on the arytenoid bodies and muscular processes.9
3. Suprasternal notch tap test or Brimacombe bounce
The suprasternal notch tap test or the “Brimacombe bounce” confirms the location of the PLMA tip in the oesophagus behind the cricoid cartilage. The test was first described by O'Connor etal in 2002.10 It involves tapping the suprasternal notch or cricoid cartilage, and observing simultaneous movement of a column of lubricant, or a soap bubble membrane at the proximal end of the drain tube Both the structures lie in close proximity to the hypopharynx, where the correctly placed distal cuff sits. The drain tube must be patent for the test to be positive. The test works by cuff compression causing drain tube compression within the drain tube, which in turn moves the lubricantor soap bubble. O'Connor etal10 reported a low false-negative rate for the suprasternal notch tap test in 50 adults, but false positives and negatives can occur. False positives can occur if the last 1-2 cm of the drain tube is folded over but some of the drain tube is still patent within the distal cuff.11 False negatives can occur if the oesophagus is open, since this can weaken the pressure wave.
4. Gel Displacement Test
Water-soluble gel (0.5-1 ml) is placed at the proximal end of the drain tube so that it forms a column of about 2-3 cm. Minimal movement or gentle up and down movements indicates a normal position. However, gel ejection with gentle positive pressure ventilation (PPV), indicates a leak from the drain tube, signifying improper seal of device with the hypopharynx (Fig 1). Thus, when positive, the test indicates airway leak through the drain tube.1,2
Fig 1.
Gel displacement test leaking drain tube
5. Passage of gastric tube/ PVC catheter through drain tube to verify the patency of drain tube
The posterior folding of the mask tip is ruled out by the successful passage of a gastric tube or a PVC catheter through the drain tube.1,2,12
6. Soap Bubble Test
In this test, soap bubble solution is placed over the tip of the drain tube and following observations may be made. When the tip of the PLMA is in the laryn-gopharynx, soap bubble solution column bubbles or the soap membrane bursts during positive pressure ventilation. When the PLMA tip enters the glottis, the tracheobronchial tree communicates directly to the drain tube. The drain tube transmits the airway pressures unless it is obstructed. The PLMA insertion into the glott is is diagnosed by watching either the formation of a spontaneous bubble which is blown away from drain tube port or the soap membrane oscillations seen with cardiac rhythm of the patient.13,14
7. Thread test
A gauze thread or small piece of cotton held over the proximal end of a leaking drain tube can also be used to detect air leak from the drain tube.13
8. Self-inflating bulb technique
This technique has been used for verification of proper placement of the oesophageal tracheal combitube®.15 A self-inflating bag is attached to the drain tube, the bulb injects easily and then remains collapsed with normal positioning of the PLMA. However, during glottic insertion, the self-inflating bulb injects easily and then re-inflates.16
9. Trachlight™
The Trachlight™ helps in quickly distinguishing glottic from oesophageal location of the tip of the PLMA mask. Trachlight™ (Laerdal Medical, Wappingers Falls, NY, USA) after removing its stylet is passed through the drain tube just as for blind endotracheal intubation.16 This is a simple and reliable means of detecting a PLMA tip fold over.17 A dull glow in the anterior neck with passage of the Trachlight™ wand beyond the drain tube tip indicates correct alignment of the PLMA with the upper esophageal sphincter.
10. Maximum Minute Volume Ventilation (MMV)
The MMV test consists of manually hyperventilating an anaesthetized and paralyzed patient with a PLMA for 15 seconds and extrapolating the total exhaled volume to one minute which can be graded as follows.
| Basal value | 5–7 L/min |
| Critical value | 6-12 L/min, threshold for removal of |
| PLMA | |
| Mean value | 26-29 L/min |
The test is easy to perform and can be completed with equipment that is readily accessible to almost every anaesthesiologist.
Anaesthesiologists should be alerted to the potential for significant airway obstruction in any patient with a MMV less than 12 L/min. It is advisable to remove the PLMA and use an alternative device before the initiation of surgery.9 In this scenario, one should not have a false sense of security due to the normal oxygen saturation as the latter does not guarantee the satisfactory elimination of CO2.18 However, the decision to remove the PLMA should be based depending on the patient's physical status, nature, site and duration of surgery.
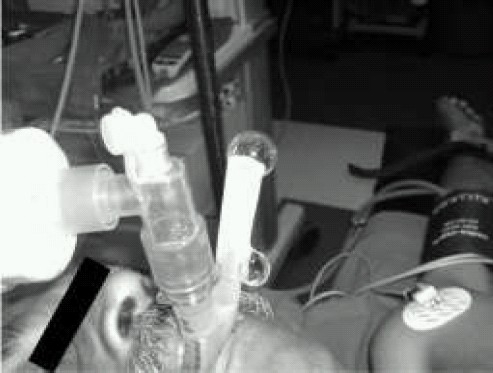
Trouble Shooting
Problems related to the PLMA might occur during: i) insertion of the device ii)maintenance/ emergence phases of anaesthesia iii) recovery phase; in the post anaesthesia care unit or in the ward. Most of the problems are detected in the perioperative period but some airway morbidity and nerve injuries might continue even after the patient has been discharged from the hospital. Various tools required for the purpose of trouble shooting are the PLMA itself with its cuff, drain tube and bite block, pressure gauge to monitor the oropharyngeal seal pressure, cuff pressure monitor, cotton, gauze thread, water soluble gel, and soap solution. Availability of respiratory module and fiberoptic scope can be very helpful in diagnosis and management of various malpositions. Common problems associated with PLMA use are:
I. Functional failure
This may result from several factors. The etiology could vary from failure to negotiate the cuff through the oral cavity, various malpositions to mechanical and dynamic causes contributing to airway obstruction inspite of a correctly placed device.19
A. Device Insertion failure
The first-time and overall insertion failure rate is 14% and 1% respectively.19 This phase may be associated with problems such as difficulty in insertion due to the following reasons:
-
Disproportionate oral aperture
Small oral aperture, inability to open mouth fully such as TM joint ankylosis, inappropriate size of the mask and mask not properly deflated before attempting insertion
Small oral cavity, small pharynx
Resistance encountered at posteriorpharyngeal wall during insertion
Short neck
Light plane of anaesthesia such as coughing, gagging, retching, stridor, hiccup, or biting of device.
Diagnosis
Inability to negotiate the mask through oral aperture
Corrective measures 1,2,12,19‐21
Proper selection of mask
Lateral approach where the cuff enters the oropharynx from the side of the hard palate.
Opening the patient's mouth with a laryngoscope followed by insertion of the device
Gum elastic bougie /fiberoptic insertion, PVC / gastric tube as stents to stiffen the drain tube12
Deepening level of anaesthesia
Jaw thrust
B. Gastric tube insertion failure and gastric insufflation
The failure rate for gastric tube insertion is 4%. The most common causes of failure of gastric tube placement are:19
Inadequate lubrication
Selection of improper size
Posterior folding of the mask
Cooled gastric tube22
The failure rate for prevention of gastric insufflation during PPV is 0.1% which is similar to the incidence seen with the tracheal tube.19
C. Dislodgement with loss of airway during maintenance phase
The PLMA gets dislodged resulting in loss of airway during the maintenance phase due to light plane of anaesthesia, improper fixation and changes in position e.g. extreme head down position during gynaecologic surgery and laparoscopic procedures. This can be avoided by proper fixation of the device. In the event of intraoperative displacement of the device, a gastric tube left in situ may be very helpful in reinsertion of the device by simply railroading the drain tube over the gastric tube.23
D. Malposition
One of the many advantages of PLMA over other LMA family members is that its malposition can be diagnosed and managed.20,21 Slight malrotation is more common with the PLMA as compared to the cLMA probably because of residual rotation in the sagittal plane or distortion of glottic geometry.24 Several malpositions have been described and the reported incidence is 5-15% at the first attempt.19‐21 The instruction manual describes three malpositions;1,2 (i) insufficient insertion depth, (ii) PLMA insertion into the glottis, (iii) PLMA tip folded backwards behind the bowl against the posterior pharyngeal wall.
Presently six malpositions (with approximate incidence) have been described.25‐27
1. Distal cuff in laryngopharynx
When the PLMA is not inserted to the desired depth, the distal cuff sits in the laryngopharaynx resulting in protrusion of the bite block.2,6,19,21
Diagnosis
Bite block protruding
Soap bubble test positive
Corrective measure
Further pushing in of the PLMA without colliding with the glottic inlet.19,21
2. Distal cuff in glottic inlet/PLMA insertion into the glottis
When the PLMA takes an anterior path during insertion, the distal cuff collides with the glottic inlet and either remains there or falls back in the laryngopharynx. PLMA entry into the glottis is not uncommon during insertion attempts because of the bulky and flexible mask tip. When the PLMA enters the glottis then the drain tube acts as an extension of the tracheobronchial tree, airway pressures are therefore transmitted through the drain tube and notthe airway tube.2,16
Diagnosis
Thread test
Gel displacement
Soap bubble test
Self-inflating bulb technique
Trachlight™
Corrective measures
Correction usually requires reinsertion using a lateral approach, of the gum elastic bougie (GEB) technique. In majority of cases, the reinsertion of the mask is to a noticeably increased depth of insertion. Location of the PLMA tip in the oesophagus behind the cricoid cartilage can be confirmed using the “suprasternalnotch tap test.”10 To distinguish between inadequate depth of insertion and glottic impaction, the PLMA can be pushed further inwards: the former will usually be corrected while the latter made worse, with increased airway obstruction or airway protective reflex activation.19 O'Connor and Stix have suggested that these malpositions can be distinguished using the soap bubble test.13,14
3. Distal cuff folded over
The advancing distal cuff of the PLMA gets folded (Fig 2) when it impacts against the posterior oropharyngeal wall thereby obliterating the lumen of the drain tube.19,20 Thus the distal cuff folds up beneath the advancing cuff until the unfolded proximal cuff is redirected inferiorly into the laryngopharynx by the build up of the folded cuff in the oropharynx. The folded distal cuff cannot easily unfold as it gets wedged into the laryngopharynx. Folding over has also been reported with the cLMA,28 but is probably more common with the PLMA due to its soft backplate.26 This malposition may occur with both finger / introducer insertion and be associated with a better seal and higher mucosal pressures than the correctly placed PLMA.
Fig 2.

Posterior folding of mask
Brimacom be et al, in a study of 95 patients with the fold over malpositions, found that in 92% resistance was encountered at the back of the mouth, in 83% the bite block protruded from the mouth, and in 98% ventilation was unaffected and the seal was normal.27 The main danger of unrecognised fold over phenomenon is that it predisposes the patient to gastric insufflation, regurgitation and pulmonary aspiration as ventilation is unhindered due to easily achieved high airway pressures.19 The patency of the drain tube must be assessed in all patients with the PLMA to exclude this malposition. In situations where passage of a gastric tube is not required, the patency can be tested by non-invasively passing the gastric tube or a PVC suction catheter only till the end of the drain tube.
Diagnosis
Resistance encountered at the back of the mouth
Bite block lying outside
Inability to pass a gastric tube/PVC catheter through the drain tube
Unaffected ventilation and seal pressure
Corrective measures19‐21
Reinsertion using a lateral approach
Reinsertion with the drain tube stiffened using a stylet
Guided insertion with a gum elastic bougie (GEB)
Digital correction by sweeping a finger behind the cuff
Of these, digital correction appears to be the least effective. Folding over cannot occur with the GEB insertion and gastric tube guided techniques.
4. Severe epiglottic downfolding
A well known cause of mechanical airway obstruction is severe epiglottic downfolding which occurs when the epiglottis is dragged inferiorly by the cuff and completely covers the laryngeal inlet (Fig 3). It is diagnosed when the anterior surface of the epiglottis is visible from the airway tube on fiberscope examination.7 Although a degree of downfolding of epiglottis has been reported in 17% of cases,29 critical airway obstruction seldom occurs from a downfolded epiglottis due to the design feature as the drain tube always suspends the epiglottis off the floor of the bowl. However, with cuff infolding (the two outside cuffs meet in the midline and the epiglottis cannot enter the bowl), a downfolded epiglottis becomes a risk factor for airway obstruction because it is now forced directly on the arytenoids.9 It may occur as a result of pre-insertion inflation of cuff, compression of pharynx and enlarged or floppy epiglottis.
Fig 3.
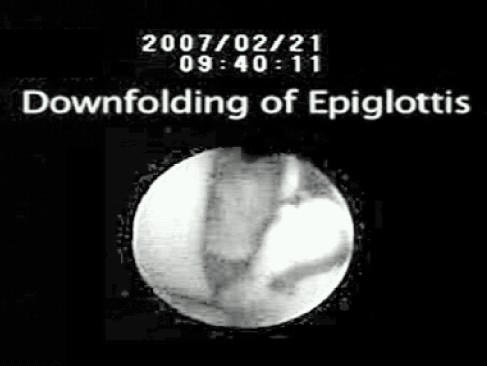
Severe epiglottic downfolding
Diagnosis
High airway pressures
Airway obstruction
MMV test
Fiberoptic examination
Corrective measures 19‐21
Reinsertion with the head/neck in a more extreme sniffing position
Jaw thrust
Laryngoscope guided placement of PLMA
5. Supraglottic and Glottis Compression
Glottic compression occurs when the glottic inlet is mechanically compressed by the distal cuff reducing the tension of the vocal cords.5 It is more likely to occur with a small pharynx, over inflated cuff and when the distal cuff is pressed into the hypopharynx with extra force.19 Compression of supraglottic and glottic structures may occasionally contribute to significant upper airway obstruction with a correctly placed tip of the cuff lying behind the cricoid cartilage.9
Diagnosis
High airway pressures
Airway obstruction
MMV test
Fiberoptic examination
Corrective measures 5,20,21
Reinsertion does not usually solve the problem.
Air should be withdrawn from the cuff
Anteroposterior diameter of the pharynx increased by adopting the sniffing position
Applying jaw thrust
6. Cuff infolding
Cuffinfolding refers to inward rotation of the large cuffs in front of the bowl so that they contact each other in the midline and obstruct gas flow (Fig 4). It is relatively uncommon and Stix reported 2 cases of cuff in-folding out of 317 cases.9,20 It is clinically indistinguishable from severe downfolding of epiglottis and both conditions may coexist at times. There is increased risk of cuff infolding with PLMA due to its deeper bowl and a more compliant cuff than that of the cLMA.2,3
Fig 4.
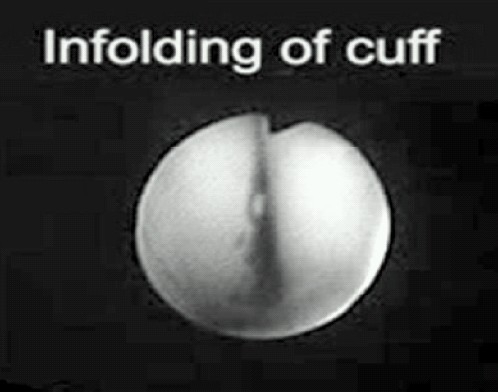
Cuff infolding
Diagnosis
High airway pressures
Airway obstruction
MMV test
Fiberoptic examination
Corrective measures20,21
Sniffing position which increases the anteroposterior diameter of the pharynx
Applying jaw thrust
Consider insertion of one size smaller LMA-ProSeal™
Ensure correct cuff inflation pressures
Air withdrawal from the cuff may be helpful
Table 1 shows Troubleshooting to various problems, causes, the required confirmatory test and their solutions.
Table 1.
Troubleshooting ProSeal Laryngeal Mask Airway
| Problem | Cause | Confirmatory tests, if any | Solution |
|---|---|---|---|
| (1) • Difficultyin negotiating the cuff at the oral aperture |
|
• Visual inspection |
|
| (2) • Insufficient depth of insertion |
|
||
| (3) • Migration/rotation/ bite block protruding |
|
|
|
| (4) • Difficultyin passing a gastric tube |
|
||
(5)
|
|
|
|
(6)
|
|
||
| (7) • High PAP without apparent cause (Obesity, COPD) |
|
||
| (8) • Singing patient |
|
||
| (9) • Abdominal distension |
|
||
| (10) • Regurgitation through drain tube |
|
|
|
| (11) • Laryngospasm |
|
|
|
| (12) • Bronchospasm |
|
||
| 1 – 6 Malposition, Gum elastic bougie (GEB), Peak airway pressure (PAP) | |||
| 1* – 6* Specific Solutions, Positive pressure ventilation (PPV) | |||
| COPD = Chronic obstructive pulmonary disease | |||
II. Regurgitation and aspiration
Regurgitation of gastric contents may result in supracuff soiling of the mask and pulmonary aspiration with catastrophic results.19,29 This may be precipitated by activation of protective reflexes due to light plane of anaesthesia as greater depth of anaesthesia is required for insertion of PLMA as compared to cLMA.30
Diagnosis
Fluid seen in the airway /drain tube
Intraoral examination
Fiberoptic examination of the tracheo bronchial tree
Sudden bronchospasm
Haemodynamic instability
Supracuff soiling of the mask on removal
Management of Regurgitation31
Leave the PLMA in situ
Suction of the gastric tube and the drain tube
Head down position and 100% oxygen should be administered
Fiberoptic evaluation and suction
Consider deepening level of anaesthesia and intubation of the patient fiberoptically via the PLMA
III. Airway morbidity and Trauma
Airway morbidity and trauma may result from difficulty and multiple attempts at insertion, prolonged surgery without intracuff monitoring and improper size selection of the PLMA.19
Diagnosis
Coughing, gagging, retching stridor, hiccup, orbiting
Audible noise, or as subtle increases in airway pressure orreductions in tidal volume
Laryngospasm, bronchospasm, regurgitation, and aspiration
Management 19,31
Eliminating the source of stimulation
Deepening anaesthesia
Head down position and 100% oxygen should be administered
Bronchodilators or high concentration of volatileagent
Many problems can be solved by proper patient and procedure selection, diagnosis and management of malpositions. Strategies to facilitate insertion by lateral/guided insertion techniques and maintaining adequate plane of anaesthesia may be helpful in improving first time and overall insertion success rates, correcting malpositions, overcoming difficult airway scenarios and prevention of regurgitation and pulmonary aspiration. Proper fixation of the device and monitoring cuff pressure in traoperatively especially during nitrous oxide based anaesthesia may bring down the incidence of airway morbidity.
References
- 1.LMA-ProSeal Instruction Manual. San Diego: LMA North America; 2001. [Google Scholar]
- 2.Brain AIJ, Verghese C, Strube PJ. The LMA ‘ProSeal’—a laryngeal mask with an oesophageal vent. Br J Anaesth. 2000;84:650–4. doi: 10.1093/bja/84.5.650. [DOI] [PubMed] [Google Scholar]
- 3.Stix MS, Rodriguez-Sallaberry FE, Cameron EM, et al. Esophageal aspiration of air through the drain tube of the ProSeal laryngeal mask. Anesth Analg. 2001;93:1354–7. doi: 10.1097/00000539-200111000-00065. [DOI] [PubMed] [Google Scholar]
- 4.O'Connor CJ, Jr, Davies SR, Stix MS, Dolan RW. Gastric distention in a spontaneously ventilating patient with a ProSeal laryngeal mask airway. Anesth Analg. 2002;94:1656–8. doi: 10.1097/00000539-200206000-00055. [DOI] [PubMed] [Google Scholar]
- 5.Brimacombe J, Richardson C, Kelley C, Donald S. Mechanical closure of the vocal cords with the laryngeal mask airway ProSeal™. Br J Anaesth. 2002;88:296–7. doi: 10.1093/bja/88.2.296. [DOI] [PubMed] [Google Scholar]
- 6.Stix MS, O'Connor CJ., Jr Depth of insertion of the ProSeal™ laryngeal mask airway. Br J Anaesth. 2003;90:235–7. doi: 10.1093/bja/aeg041. [DOI] [PubMed] [Google Scholar]
- 7.Brimacombe J, Keller C, Fullekrug B, et al. Amulticenter study comparing the ProSeal with the Classic laryngeal mask airway in anesthetized, nonparalyzed patients. Anesthesiology. 2002;96:289–95. doi: 10.1097/00000542-200202000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Keller C, Brimacombe J, Kleinsasser A, Brimacombe L. The laryngeal mask airway ProSeal™ as a temporary ventilatory device in grossly and morbidly obese patients before laryngoscope-guided tracheal intubation. Anesth Analg. 2002;94:737–40. doi: 10.1097/00000539-200203000-00048. [DOI] [PubMed] [Google Scholar]
- 9.Stix MS, O'Connor CJ. Maximum Minute Ventilation Test for the ProSeal™ Laryngeal Mask Airway. Anesth Analg. 2002;95:1782–7. doi: 10.1097/00000539-200212000-00059. [DOI] [PubMed] [Google Scholar]
- 10.O'Connor CJ, Jr, Borromeo CJ, Stix MS. Assessing ProSeal laryngeal mask positioning: the suprasternal notch test. Anesth Analg. 2002;94:1374–5. doi: 10.1097/00000539-200205000-00082. [DOI] [PubMed] [Google Scholar]
- 11.Brimacombe J, Keller C, Berry A, Mitchell S. Assessing ProSeal laryngeal mask positioning: the suprasternal notch test. Anesth Analg. 2002;94:1375. doi: 10.1097/00000539-200205000-00082. [DOI] [PubMed] [Google Scholar]
- 12.Sharma B, Sood J, Sahai C, Kumra VP. Efficacy and Safety Performance of ProSeal™ Laryngeal Mask Airway in Laparoscopic Surgery. Experience of 1000 cases. IJA. 2008;52:288–96. [Google Scholar]
- 13.O'Connor CJ, Jr, Davies SR, Stix MS. “Soap bubbles” and “gauze thread” drain tube tests. Anesth Analg. 2001;93:1082. doi: 10.1097/00000539-200110000-00067. [DOI] [PubMed] [Google Scholar]
- 14.O'Connor CJ, Jr, Stix MS. Place the bubble solution with your fingertip. Anesth Analg. 2002;94:763–4. doi: 10.1097/00000539-200203000-00057. [DOI] [PubMed] [Google Scholar]
- 15.Wafai Y, Salem MR, Baraka A, Joseph NJ, Czinn EA, Paulissian R. Effectiveness of the self-inflating bulb for verification of proper placement of the esophageal tracheal Combitube®. Anesth Analg. 1995;80:122–6. doi: 10.1097/00000539-199501000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Cornelius J, O'Connor MD, Jr, Michael S, Stix MD, PhD, Dennis Valade R. Glottic insertion of the Pro Seal™ LMA occurs in 6% of cases: a review of 627 patients. Can J Anesth. 2005;52:199–204. doi: 10.1007/BF03027729. [DOI] [PubMed] [Google Scholar]
- 17.Christodoulou C. ProSeal laryngeal mask foldover detection. Anesth Analg. 2004;99:312. doi: 10.1213/01.ANE.0000127714.32845.7F. [DOI] [PubMed] [Google Scholar]
- 18.Lumb AB. Nunn's applied respiratory physiology. 5th ed. Oxford, UK: Butterworth Heinemann; 2000. pp. 222–48. [Google Scholar]
- 19.Brimacombe JR. ProSeal LMA for ventilation and airwayprotection. In: Brimacombe JR, editor. Laryngeal Mask Anesthesia Principles and Practice. Philadelphia USA: WB Saunders; 2005. pp. 505–37. [Google Scholar]
- 20.Brimacombe J, Keller C. A Proposed algorithm for the management of airway obstruction with the ProSeal laryngeal mask airway. Anesth Analg. 2005;100:289–301. doi: 10.1213/01.ANE.0000145377.15812.FA. [DOI] [PubMed] [Google Scholar]
- 21. http://www.vitaid.com/canada/lma/resource/LMA-Proseal-troubleshootingguide.pdf.
- 22.Wardle D. Failed gastric tube insertion in the LMA-ProSeal. Anaesthesia. 2004;59:827–8. [PubMed] [Google Scholar]
- 23.Brimacombe J, Judd Vasoba D, Tortely K, Baryon E, Branagan H. Gastric tube-guided reinsertion of the ProSeal™ laryngeal mask airway. Anesth Analg. 2002;94:1670. doi: 10.1097/00000539-200206000-00062. [DOI] [PubMed] [Google Scholar]
- 24.Brimacombe J, Keller C. Stability of the ProSeal and standard laryngeal mask airway in different head and neck positions. A randomised crossover study. Eur J Anaesthesiol. 2003;20:65–9. doi: 10.1017/s0265021503000127. [DOI] [PubMed] [Google Scholar]
- 25.O'Connor CJ, Stix MS. Bubble solution diagnoses ProSeal insertion into the glottis. Anesth Analg. 2002;94:1671–2. doi: 10.1097/00000539-200206000-00065. [DOI] [PubMed] [Google Scholar]
- 26.Brimacombe J, Keller C, Berry A. Gastric insufflation with the ProSeal laryngeal mask. Anesth Analg. 2001;92:1614–5. doi: 10.1097/00000539-200106000-00053. [DOI] [PubMed] [Google Scholar]
- 27.Brimacombe J, Kennaugh S, Berry A, Keller C. Malposition of the ProSeal™ laryngeal mask. Anesth Analg. 2002;94:1367. [Google Scholar]
- 28.Nandi PR, Nunn JF, Charlesworth CH, Taylor SJ. Radiological study of the laryngeal mask. Eur J Anaesthesiol. 1991;4:33–9. [PubMed] [Google Scholar]
- 29.Brimacombe J, Keller C. The ProSeal laryngeal mask airway. A randomized, crossover study with the standard laryngeal mask airway in paralyzed, anesthetized patients. Anesthesiology. 2000;93:104–9. doi: 10.1097/00000542-200007000-00019. [DOI] [PubMed] [Google Scholar]
- 30.Kodaka M, Okamoto Y, Koyama K, et al. Predicted values of propofol EC50 and sevoflurane concentration for insertion of laryngeal mask classic and ProSeal. Br J Anaesth. 2003;92:242–5. doi: 10.1093/bja/aeh032. [DOI] [PubMed] [Google Scholar]
- 31.Brimacombe JR. ProSeal LMA for ventilation and airway protection. In: Brimacombe JR, editor. Laryngeal Mask Anesthesia Principles and Practice. Philadelphia USA: WB Saunders; 2005. pp. 241–57. [Google Scholar]


