Abstract
Background
The impact of active surveillance, comprising annual computed tomography scanning and bone marrow biopsies, in the follow-up of patients after high-dose therapy with autologous stem cell rescue for recurrent follicular lymphoma was analyzed.
Design and Methods
Seventy-one of 99 patients who received high-dose therapy commenced the surveillance program. Response duration, time to next treatment and overall survival were compared according to whether disease progression had been diagnosed on the basis of surveillance investigations or on clinical grounds.
Results
After a median follow-up of 16 years, progression was documented by surveillance in 16 patients and clinically in 18, the median response duration being 2.4 and 2.3 years, respectively (P=NS). Ten patients with a relapse detected clinically started treatment immediately, contrasting with one patient whose relapse was detected by surveillance investigations. Five patients with relapses detected by surveillance investigations have not required treatment after a median follow-up of 18 years, whereas all but two patients with a relapse detected clinically have been treated. The median time to next treatment was 7 years for patients with a relapse identified by surveillance investigations and 4 years for those whose relapse was manifested clinically (P=0.03). Overall survival was not significantly different between the two groups.
Conclusions
Surveillance investigations, consisting of annual computed tomography scanning and bone marrow biopsies, have no impact on the management of patients with recurrent follicular lymphoma and do not improve the outcome of these patients.
Keywords: active surveillance, clinical relapse, high-dose therapy, follicular lymphoma
Introduction
The clinical course of follicular lymphoma, the second most common histological subtype of non-Hodgkin’s lymphoma,1 is characterized by repeated responses to different treatments and almost inevitable recurrence.2 In most patients, the illness follows an indolent course and may not require treatment until symptoms or complications develop. However, recurrence can be associated with histological transformation to diffuse large B-cell lymphoma (DLBCL),3 which carries a dismal prognosis.
The optimal follow-up strategy for follicular lymphoma after the induction of a remission has not been defined and hence, clinical practice varies considerably. Many centers use surveillance strategies incorporating radiological investigations and bone marrow biopsies at regular, pre-specified intervals, but there is little consensus. The current North American guidelines suggest the use of surveillance scans at regular intervals ‘as clinically indicated’4,5 whereas the European Society of Medical Oncology Follicular Lymphoma guidelines do not recommend routine scans beyond 2 years after the end of treatment.6
High dose therapy (HDT) with autologous stem cell rescue as consolidation of second or subsequent remission was first used at St. Bartholomew’s hospital in patients with follicular lymphoma in 1985.7,8 At the time, HDT was experimental and was thus performed in the setting of a clinical trial, aiming at demonstrating, amongst other objectives, the relevance of a molecular remission during follow-up. In this context, an intensive surveillance program including annual computed tomographic (CT) scans and bone marrow biopsies was implemented to accurately assess the outcome of patients following this therapeutic strategy. The aim of the current study was to analyze the impact of this surveillance strategy on the detection of recurrence following HDT and on the management and outcome of such recurrences.
Design and Methods
Patients’ characteristics
Ninety-nine patients (median age, 45 years; range, 25–61) with follicular lymphoma in second or subsequent complete (38%) or ‘good partial’ (62%) remission received HDT between 1985 and 1995. The clinical characteristics of these patients have been previously reported.7,8
High-dose therapy and follow-up strategy
HDT comprised cyclophosphamide (60 mg/kg daily for 2 days) and fractionated total body irradiation (2 Gy twice daily for 3 days). Within 24 hours of the last dose of radiation, the autologous bone marrow which had been treated in vitro with anti-CD20 (or several antibodies) and complement was re-infused. Patients were followed-up monthly for the first 3 months, quarterly for 3 years, every 6 months for 2 years and annually thereafter, by history, physical examination, full blood count and serum biochemistry. Surveillance investigations comprised annual CT scans and unilateral bone marrow aspirates and trephine biopsies. At progression, lymph node and bone marrow biopsies were performed whenever possible. The diagnosis of histological transformation was defined by the presence of histological features of DLBCL.
Definitions and statistical analysis
Clinical relapse was defined as recurrence based on investigations (radiological imaging and, whenever possible, tissue biopsy) prompted by the presence of new symptoms, detection of new signs by either the patient or the doctor or by abnormal routine blood tests. Surveillance relapse was defined as recurrence detected in a patient without suspicious symptoms, clinically detectable signs and no suspicious results on the full blood count but with new pathological changes on a surveillance CT scan or a surveillance bone marrow biopsy.
New suspicious sites on imaging were biopsied if this was technically feasible. The date of relapse was defined as the date of the scan or bone marrow biopsy that identified a surveillance recurrence or the date of the radiological investigation or biopsy that confirmed a clinical relapse. Response duration was defined from the date of HDT to the date of relapse or progression. Time to next treatment and overall survival were calculated by the Kaplan-Meier method from the time of HDT to the next treatment or death from any cause, respectively. Statistical significance was calculated by the log-rank test where appropriate. Median follow-up was calculated for patients alive at last follow-up.
Results
Adherence to the surveillance strategy
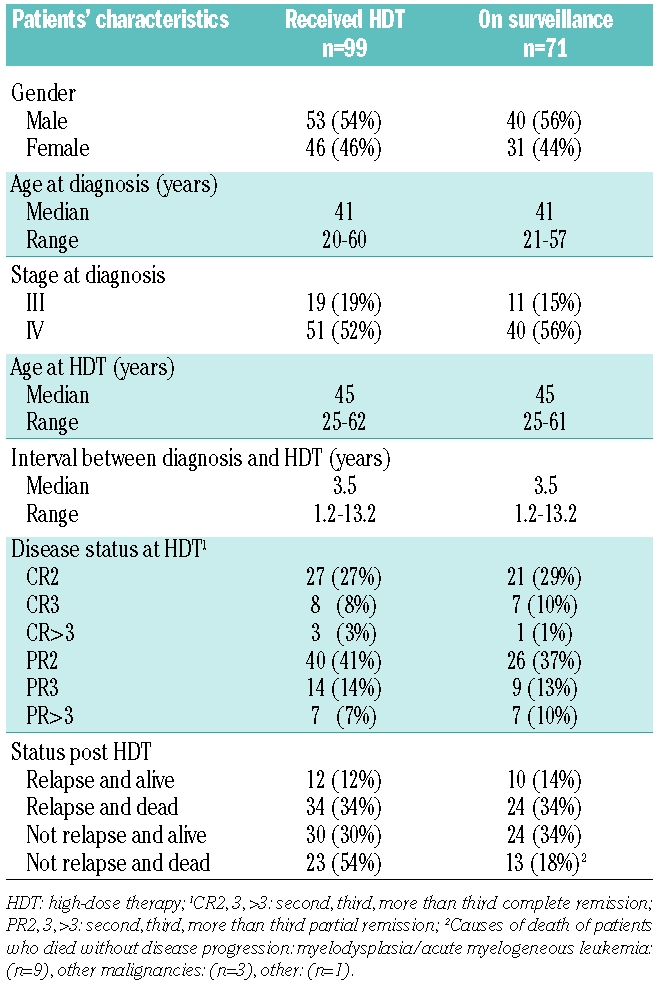
Seventy-one of the 99 patients who received HDT (72%) commenced annual surveillance investigations approximately 1 year after HDT. Their clinical characteristics are detailed in Table 1. The remaining 28 patients did not undergo surveillance investigations because of relapse within 1 year (20 patients, 71%), follow-up elsewhere (7 patients, 25%), or the patient’s wishes (1 patient, 4%). Eighty-six percent of the patients who commenced surveillance actually had annual CT scans and bone marrow biopsies until disease progression or death.
Table 1.
Patients’ characteristics.
Diagnosis of disease progression
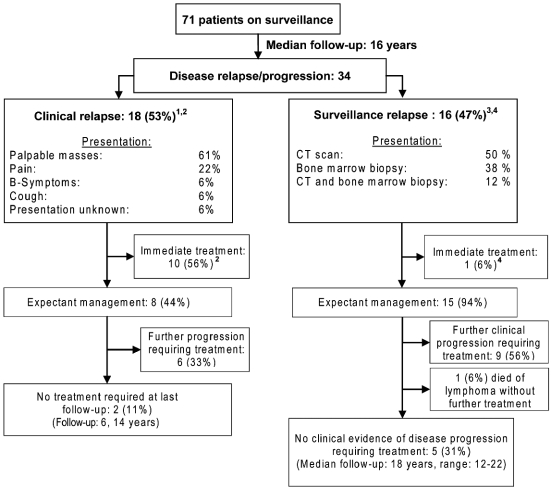
After a median follow-up of 16 years (range, 11–22 years), 34 of the 71 patients (48%) on annual surveillance developed recurrent or progressive disease. In 18 of these 34 patients (53%), the recurrence was detected clinically (clinical relapses) and in 16 (47%), on the basis of surveillance investigations in the absence of clinically detectable signs or symptoms (surveillance relapses) (Figure 1). There were no statistically significant differences in the percentage of surveillance relapses among patients who had achieved a partial remission before HDT [8/42 patients (19%)] in comparison with those who were in complete remission [8/29 patients (28%)]. Eleven of 18 patients (61%) with a clinical relapse presented with new palpable masses, first detected by the patient in five cases and by the doctor in two cases (this information was not recorded for the other four patients). Surveillance relapse was diagnosed by CT alone in 50% of cases, by bone marrow biopsy in 38% and on both synchronously in 12%. All patients with a surveillance relapse diagnosed by bone marrow biopsy had unremarkable blood counts. Transformation to DLBCL was diagnosed at first relapse/progression in 5/18 patients with a clinical relapse and in 1/16 patients with a surveillance relapse.
Figure 1.
Presentation and management at relapse/progression after HDT. 1Stage at relapse: I–II: (n=7), III–IV: (n=5), unknown: (n=6); 2Histological transformation to DLBCL: (n=5); 3Stage at relapse: I–II: (n=3), III–IV: (n=8), unknown: (n=5); 4Histological transformation to DLBCL: (n=1).
There was no statistically significant difference in the median response duration between clinically detected (2.3 years) and surveillance recurrences (2.4 years).
Management and outcome following recurrence/progression
Ten of the 18 patients (56%) with a clinical relapse started treatment immediately (Figure 1), including all five patients with histological transformation and five with symptomatic or rapidly progressing lymphadenopathy but no transformation. The remainder were observed closely, six requiring further treatment at a median time of 10 months (range, 4–21 months) after developing rapidly progressive or symptomatic lymphadenopathy. Two patients remain well without treatment at last follow-up.
In contrast, among patients with a surveillance relapse, only the patient with biopsy-proven histological transformation was treated immediately. Nine others from this group started treatment after a period of close observation (median time from relapse to treatment, 3 years; range, 5 months - 7 years) because of histological transformation in one further patient and rapidly progressive or symptomatic lymphadenopathy in all others. One patient in this group died with disease progression without receiving any further treatment, given other significant co-morbidities. Five patients remain well without treatment at last follow-up and have shown no evidence of clinical progression after a median follow-up of 18 years following HDT (Figure 1). In four of them evidence of disease has repeatedly been confirmed by CT or bone marrow biopsy. One patient had only a single positive bone marrow biopsy and subsequent biopsies were negative.
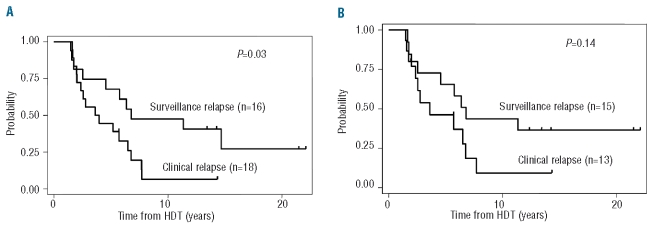
The median time to next treatment was significantly longer for patients with a surveillance relapse (median, 7 years; range, 1.5–15 years) than for those with a clinical relapse (median, 4 years; range, 1.6–8 years; P=0.03; Figure 2A). After excluding patients with histological transformation, the time to next treatment for the clinical relapse group was shorter than that for patients with a surveillance recurrence but the difference was no longer statistically significant (P=0.14, Figure 2B).
Figure 2.
(A) Time to next treatment for 34 patients with relapse/progression after HDT. (B) Time to next treatment for patients with relapse/progression after HDT, excluding transformation (n=28).
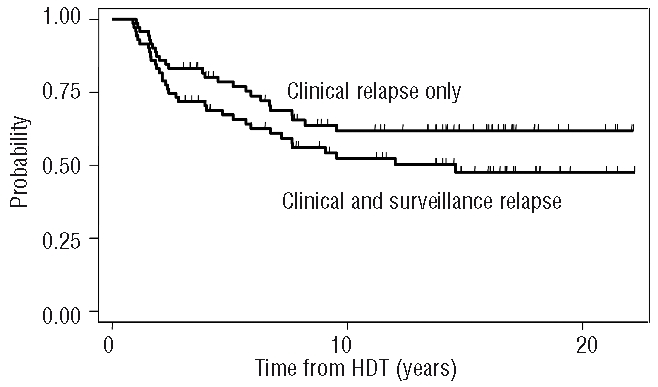
The median overall survival for patients with a clinical relapse was 8 years (range, 1.7–21 years), in comparison with 9 years (range, 1.9–22 years) for patients with a surveillance relapse (P=0.16, Figure 3).
Figure 3.
Overall survival for 34 patients with relapse/progression after HDT.
Discussion
This study reports the results of a surveillance program with annual CT scans and bone marrow biopsies in patients with follicular lymphoma treated with HDT. This exhaustive surveillance strategy was set up in the context of a clinical trial assessing the efficacy of HDT by analyzing the presence of molecular evidence of disease. HDT with stem cell rescue, an intensive treatment, resulted in a significantly longer freedom from recurrence in comparison with that achieved by conventional chemotherapy in a historical control group. Such a thorough follow-up made sense in the context of that study; however, the value of an intensive surveillance strategy for patients with follicular lymphoma outside a clinical trial is debatable. There is a lack of evidence regarding the potential benefits of routine surveillance investigations in follicular lymphoma and, consequently, recommendations in the published guidelines4–6 are empirically based on expert consensus only. The rationale for surveillance investigations lies in a simple hypothesis: the outcome of patients would improve if recurrences were detected earlier and treatment was initiated in less advanced stages of the disease. This strategy, which underlies cancer screening, might be appropriate for solid tumors or other more aggressive lymphomas, but it is more difficult to justify in a disease such as follicular lymphoma, in which patients are frequently asymptomatic with an excellent performance status in spite of being diagnosed in advanced stage and, thus, deferring initial therapy is an accepted therapeutic option.9 Additional disadvantages of surveillance strategies include increased resource utilization, radiation exposure, patients’ discomfort and, potentially, an increase in patients’ anxiety and in the number of false positive results.
The current study demonstrated that almost half of the recurrences could be detected by surveillance investigations before the disease became symptomatic or clinically detectable. This is in contrast to the use of CT surveillance in patients with DLBCL in which only 6% of recurrences are identified by CT scanning in asymptomatic patients.10 In the present study there were no differences in the median response duration according to whether recurrences were diagnosed clinically or based on surveillance investigations. In this sense, our surveillance strategy would not have fulfilled the objective of allowing early detection of the disease, had this been the purpose of the investigations. In the same line, surveillance investigations failed to identify patients with early-stage disease as almost three quarters of patients with a surveillance recurrence had stage III or IV at relapse. This contrasts with what was previously reported following an analysis of surveillance CT scans in patients with DLBCL, showing that surveillance investigations identified a group with a particularly indolent clinical course.11 However, the implications of having advanced stage disease are not the same in follicular lymphoma as in DLBCL. In fact, among those with a surveillance recurrence in the present study, only the patient with histological transformation required immediate treatment, contrasting with more than half the patients requiring treatment in the clinical relapse group. Thus, the median time to next treatment was almost double in patients with a surveillance relapse than in those with a clinical relapse, with one third of the patients in the former group not having needed any therapeutic intervention after a median follow-up of 18 years. The higher proportion of patients with histological transformation in the group with clinical recurrences (28% versus 6%) most likely did not account for their shorter time to next treatment, as, after excluding patients with histological transformation, those with clinical relapses still required treatment earlier than patients with surveillance relapses.
The results of this study re-enforce and reflect the natural history and the clinical course of follicular lymphoma: the majority of patients are asymptomatic with good performance status despite being diagnosed in advanced stage, so that frequently they do not need treatment straightaway after diagnosis and can be managed expectantly. A history of waxing and waning lymphadenopathy with spontaneous regressions before the diagnosis is made or before treatment is initiated is not unusual.9 Treatment at diagnosis in asymptomatic patients has not been shown to prolong survival in randomized trials comparing this approach to initial therapy.12–14
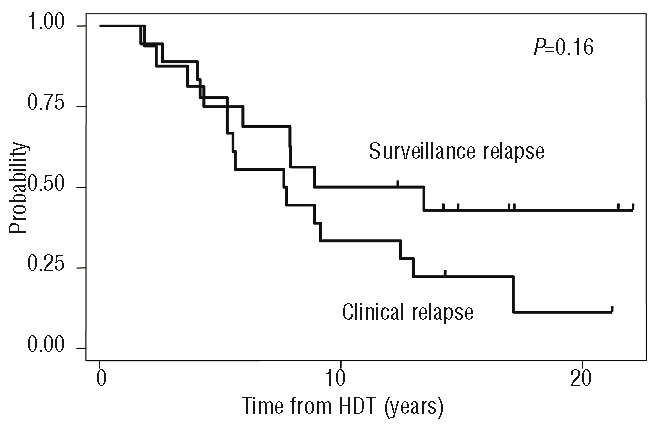
Thus, in the current study surveillance investigations did allow early detection of some recurrences but this did not lead to diagnoses in less advanced stages of the disease. More importantly, identification of recurrences by surveillance investigations had no impact on treatment initiation or the outcome of the patients. Notwithstanding, the impact that surveillance investigations had on ‘outcome measures’ must be recognized. The relapse rate for patients treated with HDT and stem cell rescue and submitted to an intensive surveillance program was 48% in comparison with a theoretical clinical relapse rate of 41% (including those with a clinical relapse, n=18, and those with a surveillance relapse not treated initially with a subsequent clinical relapse needing treatment, n=11). Similarly, the median response duration from HDT to any recurrence was 15 years and would have not yet been reached for clinical relapses only (Figure 4).
Figure 4.
Impact of the surveillance strategy on the response duration
In conclusion, this study demonstrates that annual surveillance CT scans and bone marrow biopsies following HDT for follicular lymphoma are futile from the patients’ point of view, as they fail to identify patients who need treatment urgently and have no impact on patients’ management, which is actually driven by the clinical course of the illness. Such surveillance investigations increase costs, radiation exposure and potentially create added anxiety. As mentioned, at the time that this study began, HDT for follicular lymphoma was a highly experimental procedure and it was, therefore, important to find out the real incidence of recurrence. In practice, the benefit of the clinical trial has been two-fold. The role of myelo-ablative therapy has been clarified. In addition, the lack of benefit to patients of (research-driven) surveillance has been demonstrated.
Acknowledgments
the authors would like to thank Professor J. Armitage for his helpful comments on the manuscript.
Footnotes
Funding: SM was kindly supported by grants from Olivia Walduck’s family and from the Mark Ridgwell Family trust.
Authorship and Disclosures
SM was the principal investigator and takes primary responsibility for the paper. AZSR and AD contributed vital data. JM performed the statistical analysis. MG, SM and TAL coordinated the research and analyzed data. MG wrote the paper.
Presented in abstract form at the 50th annual meeting of the American Society of Hematology, San Francisco, December 2008.
The authors reported no potential conflicts of interest.
References
- 1.The Non-Hodgkin’s Lymphoma Classification Project. A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin’s lymphoma. Blood. 1997;89(11):3909–18. [PubMed] [Google Scholar]
- 2.Johnson PW, Rohatiner AZ, Whelan JS, Price CG, Love S, Lim J, et al. Patterns of survival in patients with recurrent follicular lymphoma: a 20-year study from a single center. J Clin Oncol. 1995;13(1):140–7. doi: 10.1200/JCO.1995.13.1.140. [DOI] [PubMed] [Google Scholar]
- 3.Montoto S, Davies AJ, Matthews J, Calaminici M, Norton AJ, Amess J, et al. Risk and clinical implications of transformation of follicular lymphoma to diffuse large B-cell lymphoma. J Clin Oncol. 2007;25(17):2426–33. doi: 10.1200/JCO.2006.09.3260. [DOI] [PubMed] [Google Scholar]
- 4.Diagnostic Imaging in Lymphoma. Ontario: Cancer Care Ontario; 2006. Mar 8, [Google Scholar]
- 5.Non-Hodgkin’s Lymphoma. National Comprehensive Cancer Network; 2009. 27/01/2009. [Google Scholar]
- 6.Dreyling M. Newly diagnosed and relapsed follicular lymphoma: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2008;19(Suppl 2):ii77–8. doi: 10.1093/annonc/mdn096. [DOI] [PubMed] [Google Scholar]
- 7.Apostolidis J, Gupta RK, Grenzelias D, Johnson PW, Pappa VI, Summers KE, et al. High-dose therapy with autologous bone marrow support as consolidation of remission in follicular lymphoma: long-term clinical and molecular follow-up. J Clin Oncol. 2000;18(3):527–36. doi: 10.1200/JCO.2000.18.3.527. [DOI] [PubMed] [Google Scholar]
- 8.Rohatiner AZ, Nadler L, Davies AJ, Apostolidis J, Neuberg D, Matthews J, et al. Myeloablative therapy with autologous bone marrow transplantation for follicular lymphoma at the time of second or subsequent remission: long-term follow-up. J Clin Oncol. 2007;25(18):2554–9. doi: 10.1200/JCO.2006.09.8327. [DOI] [PubMed] [Google Scholar]
- 9.Horning SJ, Rosenberg SA. The natural history of initially untreated low-grade non-Hodgkin’s lymphomas. N Engl J Med. 1984;311(23):1471–5. doi: 10.1056/NEJM198412063112303. [DOI] [PubMed] [Google Scholar]
- 10.Guppy AE, Tebbutt NC, Norman A, Cunningham D. The role of surveillance CT scans in patients with diffuse large B-cell non-Hodgkin’s lymphoma. Leuk Lymphoma. 2003;44(1):123–5. doi: 10.1080/1042819021000040323. [DOI] [PubMed] [Google Scholar]
- 11.Liedtke M, Hamlin PA, Moskowitz CH, Zelenetz AD. Surveillance imaging during remission identifies a group of patients with more favorable aggressive NHL at time of relapse: a retrospective analysis of a uniformly-treated patient population. Ann Oncol. 2006;17(6):909–13. doi: 10.1093/annonc/mdl049. [DOI] [PubMed] [Google Scholar]
- 12.Young RC, Longo DL, Glatstein E, Ihde DC, Jaffe ES, DeVita VT., Jr The treatment of indolent lymphomas: watchful waiting v aggressive combined modality treatment. Semin Hematol. 1988;25(2 Suppl 2):11–6. [PubMed] [Google Scholar]
- 13.Ardeshna KM, Smith P, Norton A, Hancock BW, Hoskin PJ, MacLennan KA, et al. Long-term effect of a watch and wait policy versus immediate systemic treatment for asymptomatic advanced-stage non-Hodgkin lymphoma: a randomised controlled trial. Lancet. 2003;362(9383):516–22. doi: 10.1016/s0140-6736(03)14110-4. [DOI] [PubMed] [Google Scholar]
- 14.Brice P, Bastion Y, Lepage E, Brousse N, Haioun C, Moreau P, et al. Comparison in low-tumor-burden follicular lymphomas between an initial no-treatment policy, prednimustine, or interferon alfa: a randomized study from the Groupe d'Etude des Lymphomes Folliculaires. Groupe d'Etude des Lymphomes de l'Adulte. J Clin Oncol. 1997;15(3):1110–7. doi: 10.1200/JCO.1997.15.3.1110. [DOI] [PubMed] [Google Scholar]