Abstract
Background & Aim: Hyperhomocysteimemia is a cardiovascular risk factor even among children. Supplementation of oral folic acid may reduce homocysteine levels to normal. However, data is limited at this point for healthy children and adolescents.
Methods: Five hundre and twenty four children participated in the study; Twenty six of them were found to be hyperho mocysteinemic(>95th percentile for age). Twenty of them received 5 mg of folic acid twice per week for two consecutive months while the other six received a diet rich in dietary folate.
Results: Serum homocysteine levels were statistically significantly decreased from 13.1 (10-24.2 µmol/L ) to 7.7 (4.9- 15.2 µmol/L), p<0.001. Serum folate levels were significantly rose from 4.3 (3-20 ng/mL) to 16.8 (7-20 ng/mL), p<0.001. On the contrary, no important changes were observed in the above parameters in children to whom a diet rich in folic acid was recommended. Homocysteine levels were found to be positively associated with age (r=0.314, p<0.001), BMI (r=0.192, p<0.001), WC (r = 0.215, p<0.001), simple sugars (r= 0.182, p<0.001 ) and negatively associated with folic acid (r = -0.331, p<0.001), vitamin B12 (r = -0.214, p<0.001) and dietary folic acid (r= -0.228, p=0.003).
Conclusions: Oral folic acid 5 mg twice per week may efficiently reduce serum homocysteine levels and increase serum folic acid levels in healthy children with increased homocysteine levels (>95th percentile for age). Hyperhomocysteinemia in childhood may be a predictive factor of cardiovascular disease. In addition, these results may offer more help to health practioners in order to establish more prospective studies to elucidate the relationship between homocysteine, folic acid and heart disease in children.
Keywords: folic acid, hyperhomocysteinemia, children, cardiovascular disease
Hyperhomocysteinemia (HHCY) is emerging an independent predictor of stroke, atherosclerosis, and cardiovascular disease even among children1,2. In adults a 5 µmol/L increase in serum homocysteine (tHcy) levels was associated with an increase risk of stroke and ischemic heart disease by >50% and 30%, respectively3. Folate status is one of the most important determinants of tHcy concentrations and folic acid supplementation significantly and safely improves homocysteine levels4. Folic acid supplements are well tolerated and have been found to decrease homocysteine levels and also to improve vascular function in children5. Even a weekly single dose may be beneficial of increasing red blood cell folate levels and reducing serum tHcy levels6,7. Data is limited in children as far as concern supplementation of folic acid in healthy children. The purpose of our study was to examine the effects of 5 mg of oral folic acid twice per week on 1) serum homocysteine levels, 2) serum folate and vitamin B12 levels in healthy hyperhomocysteinemic children for 2 consecutive months.
Methods
The study was conducted in 8 public schools from different socioeconomic status in Northern Greece; Five hundred and twendy four children (aged 6-15y) participated in the study. Twenty six out of 524 children presented hyperhomocysteinemia (>95th percentile for age). All information about the children's history methods and percentile ranges are fully presented in a previous published paper8. Written informed consent was obtained from the parents of each child participating in the study. Permission was also obtained from the Ethical Committee of Aristotle University of Thessaloniki, Greece.
Subjects were divided in three age groups. The 1st one included 112 children aged 6-9y, the 2nd one included 144 children aged 10-12y and the 3rd one included 268 participants aged 13-15y.
Twenty out of 26 hyperhomocysteinemic children underwent a therapeutic intervention with oral folic acid, 5 mg, twice per week for 2 months, while the other 6 children received a diet rich with folic acid (500 mcg) for the same period of time. The dietary intervention included general information to the parents and children of foods high in dietary folate and how many servings of these foods each child must have every day in order to get 500 mcg of folate.
After the two month period, the subjects entered a washout phase of two weeks before the second measurement. The participants were also fasted 10-12h overnight before the two measurements.
Blood samples were drawn by venipuncture into 10-ml empty evacuated tubes without ethylenediaminetetraacetic acid (EDTA), heparin or clot activators. The tubes were centrifuged within the next 1/2 hour at 2000xg for 15 min. The serum then was separated and was analyzed for tHcy, folate and B12 measurements. Homocysteine was measured with Fluorescence Polarization Immunoassay method (FPIA) using Abbot IMx analyzer, while folate and vitamin B12 were measured by Electrochemiluminescence using the Elecsys of 2010 Roche analyzer. Albumin levels were also measured to ensure normal function of circulating protein since homocysteine is carried out bounded to albumin. Creatinine was also measured to ensure proper renal function.
All data work was analyzed using SPSS 13.0 software (Statistical Package for Social Sciences). Data skewed to the right and the geometric means with 95 CI were presented. Variables, which were found not normally distributed, were log-transformed. Analysis of variance, (ANOVA) was used to test for differences of variances in the three age groups. For post hoc comparisons of means, Bonferroni test was used. Correlation between variables was analyzed by Pearsons method. In statistical analysis, values of P<0.05 were regarded as statistically significant.
Results
Six (6) children presented with hyperhomocysteinemia (tHcy >9.98 µmol/L) in the first age group, seven (7) children (tHcy >10.62 mol/L) in the 2nd age group, and thirteen (13) children (tHcy >14.40 mol/L) in the 3rd age group.
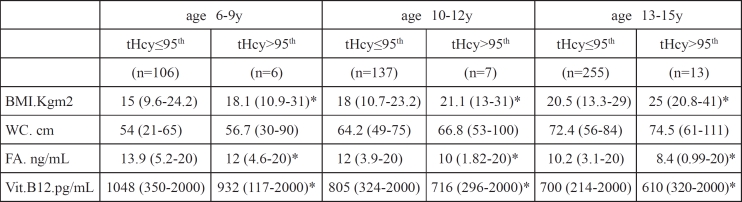
Table 1 shows the anthropometric and clinical parameters of children with tHcy levels >95th and ≤95th percentiles for all three age groups. Children with tHcy >95th percentile had higher BMI, WC and lower serum folic acid and vitamin B12 compared with the children having tHcy ≤95th percentile.
Table 1. Anthropometric and clinical parameters in children with tHcy levels >95th and ?95th percentiles for all three age groups.
Values are presented as geometric means-in parentheses (min-max) *Statistical significant difference between tHcy≤ 95th and > 95th in all three age groups (P<0.05) BMI: body mass index, WC: waist circumference, FA: folic acid
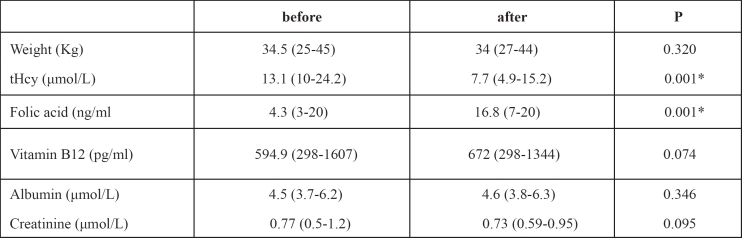
Serum homocysteine levels significantly decreased (P<0.001), while serum folic acid levels were statistically significantly improved (P<0.001) in the children who received oral folic acid for 2 months. No significant changes were observed for serum vitamin B12 levels, albumin and creatinine. (Table 2).
Table 2. Characteristics of subjects (n=20) before and after 2 months of therapy with folic acid.
Values are presented as geometric means. In parentheses (min -max). * Statistically significantly difference (p<0.05) tHcy, total serum homocysteine
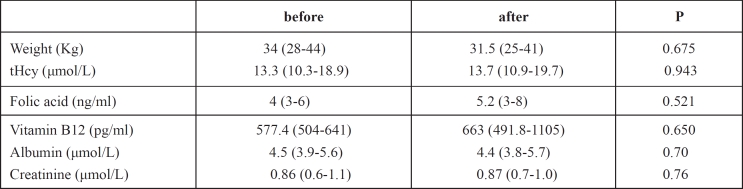
Table 3 shows information from children who received a diet rich in folic acid for the 2 month period. No significant changes were observed for serum homocysteine, folic acid and vitamin B12 and the other parameters.
Table 3. Characteristics of subjects (n=6) before and after 2 months with a diet rich in folic acid.
Values are presented as geometric means. In parentheses (min -max). *Statistically significantly difference (p<0.05) tHcy, total serum homocysteine
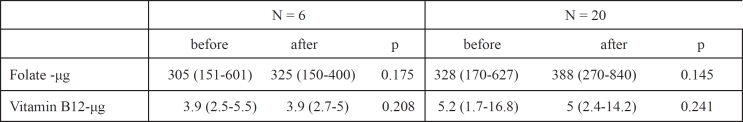
Table 4 shows data from dietary intake of folate and vitamin B12 in both groups after the 2 month period. No significant changes were observed in both groups.
Table 4. Dietary nutrient intake before and after 2 months for children receiving oral folic acid (n-=20) and diet rich in dietary folate (n=6).
Values are presented as geometric means. In parentheses (min -max). *Statistically significantly difference (p<0.05)
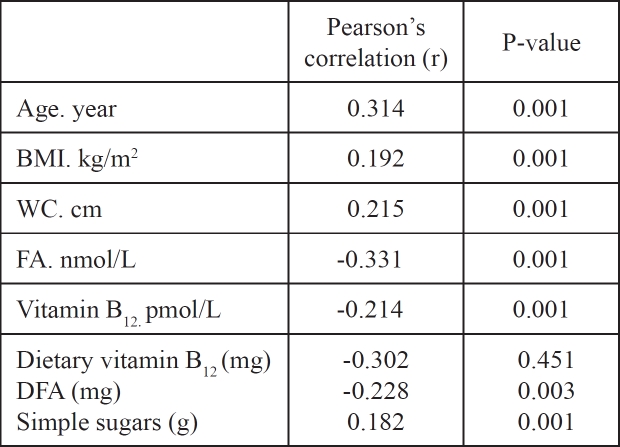
Homocysteine levels were found to be positively associated with age (r=0.314, P<0.001), BMI (r=0.192, p<0.001), WC (r = 0.215, p<0.001), simple sugars (r= 0.182, p<0.001 ) and negatively associated with folic acid (r = -0.331, p<0.001), vitamin B12 (r = -0.214, p<0.001) and dietary folic acid (r= -0.228, p=0.003) (table 5).
Table 5. Correlates of tHcy (N=524).
BMI: body mass index, WC: waist circumference, FA: folic acid, DFA: dietary folic acid
Discussion
The major finding of the study was that short-term dietary supplementation of folic acid reduces tHcy levels and increases serum folic acid in healthy hyperhomocysteinemic children. Previous data have shown that supplementation of folic acid once per week is enough to increase blood folate levels and reduce serum homocysteine concentrations6,7. Our study reported that oral folic acid of 5 mg two times per week may successfully reduces homocysteine concentrations to normal and increase serum folic acid levels.
At this time no studies have been looked on folic acid supplementation in healthy children. Folic acid supplementation has been reported by other experts to improve homocysteine levels of different type of diseases1,2,5,9–13. Folic acid supplementation has been reported1 to improve homocysteine levels in children with a thromboembolism event as well as in obese children with early atherosclerosis2. Bennett-Richards et al9 reported in his study that a 8 week supplementation with folic acid reduces homocysteine levels and improves endothelial function in children with chronic renal failure. In another study, Huemer et al10 concluded that oral folic acid supplementation reduces homocysteine and increase folic acid levels in children with epilepsy. Recently two other studies show the effects of folic acid on homocysteine levels. Di Rosa et al11 reported in 19 children with hyperhomocysteinemia who suffered from migraines that folic acid supplementation may be beneficial for these children. In another study, MacKenzie et al12 found that 5 mg of folic acid daily reduces homocysteine levels, increases folic acid levels and also normalizes endothelial function in children with type 1 diabetes. Folic acid supplementation may also improve antioxidant capacity as well as reducing homocysteine levels in young children with myocardial infarction13.
Also, our results showed that our therapeutic trial with foods rich in folic acid in hypehomocysteinemic children did not result in what was expected originally, possibly due to the fact that these children did not comply with our dietary advice.
Conclusion
Children with serum tHcy levels > 95th percentile for age should be recommended to take oral folic acid if diet is not working in order to reduce tHcy levels. A 5mg oral folic acid dose twice per week for two months seems to be efficient. Hyperhomocysteimemia is a cardiovascular risk factor even among children. HHCY may be a predictive risk factor of cardiovascular disease. In addition, to that these results may offer more help to health practioners in order to develop more observational and prospective studies to elucidate the relationship between homocysteine, folic acid and heart disease in children.
References
- 1.Kosch A, Koch HG, Heineke A, Kurnik K, Heller C, Nowak-Göttl U. Inreases fasting total homocysteine plasma levels as a risk factor for thromboembolism in children. Thromb Kaemost. 2004;91:308–314. doi: 10.1160/TH03-02-0038. [DOI] [PubMed] [Google Scholar]
- 2.Huang XM, Zang YY, Yu ZS, Zhu WH, Fu JF, He J, et al. Early arterial atherosclerosis and level of plasma homocysteine in simply obese children. Zhongua Er Ke Za Zhi. 2005;43:192–195. [PubMed] [Google Scholar]
- 3.Wald DS, Laws M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ. 2002;325:1202. doi: 10.1136/bmj.325.7374.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brattstrom L, Wilcken DE. Homocysteine and cardiovascular disease: cause or effect? Am J Clin Nutr. 2000;72:315–323. doi: 10.1093/ajcn/72.2.315. [DOI] [PubMed] [Google Scholar]
- 5.Pena AS, Wiltshire E, Gent R, Hirte C, Cooper J. Folic acid improves endothelial function in children and adolescents with type 1 diabetes. J Pediatr. 2004;144:500–504. doi: 10.1016/j.jpeds.2003.12.049. [DOI] [PubMed] [Google Scholar]
- 6.Norsworthy B, Skeaff CM, Adank C, Green TJ. Effects of oncea-week or daily folic acid supplementation on red blood cell folate concentrations in women. Eur J Clin Nutr. 2004;58:548–554. doi: 10.1038/sj.ejcn.1601843. [DOI] [PubMed] [Google Scholar]
- 7.Adank C, Green TJ, Skeaff CM, Briars B. Weekly high-dose folic acid supplementation is effective in lowering serum homocysteine concentrations in women. Ann Nutr Metab. 2003;47:55–59. doi: 10.1159/000069278. [DOI] [PubMed] [Google Scholar]
- 8.Papandreou D, Mavromichalis I, Makedou A, Rousso I, Arvanitidou M. Reference range of total serum homocysteine level and dietary indexes in healthy Greek schoolchildren aged 6-15 years. British J Nutr. 2006;96:719–724. [PubMed] [Google Scholar]
- 9.Bennett-Richards K, Kattenhorn M, Oakley G, Varghese Z, Rees L, Deanfield JE. Does oral folic lower Total Homocysteine Levels and Improve Endothelial Function in Children with Chronic Renal Failure? Circulation. 2002;105:1810. doi: 10.1161/01.cir.0000014417.95833.1d. [DOI] [PubMed] [Google Scholar]
- 10.Huemer M, Ausserer B, Graninger G. Hyperhomocysteinemia in children treated with antiepileptic drugs is normalized by folic acid supplementation. Epilepsia. 2005;46:1677–1683. doi: 10.1111/j.1528-1167.2005.00264.x. [DOI] [PubMed] [Google Scholar]
- 11.Di Rosa G, Attina S, Spano M. Efficacy of folic acid in children with migraine, hyperhomocysteinemia and MTHFR polymorphisms. Headache. 2007;47:1342–1344. doi: 10.1111/j.1526-4610.2007.00932.x. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie KE, Wiltshire EJ, Gent R, Hirte C, Piotto L, Cooper JJ. Folate and vitamin B6 rapidly normalize endothelial dysfunction in children with type 1 diabetes mellitus. Pediatrics. 2006;118:242–253. doi: 10.1542/peds.2005-2143. [DOI] [PubMed] [Google Scholar]
- 13.Assanelli D, Bonanome A, Pezzini A, Albertini F, Maccalli P, Grassi M. Folic acid and vitamin E supplementation effects on homocysteinemia, endothelial function and plasma antioxidant capacity in young myocardial-infarction patients. Pharmacol Res. 2004;49:79–84. doi: 10.1016/j.phrs.2003.07.009. [DOI] [PubMed] [Google Scholar]