Abstract
Summary: Staphylococcus aureus is an important cause of skin and soft-tissue infections (SSTIs), endovascular infections, pneumonia, septic arthritis, endocarditis, osteomyelitis, foreign-body infections, and sepsis. Methicillin-resistant S. aureus (MRSA) isolates were once confined largely to hospitals, other health care environments, and patients frequenting these facilities. Since the mid-1990s, however, there has been an explosion in the number of MRSA infections reported in populations lacking risk factors for exposure to the health care system. This increase in the incidence of MRSA infection has been associated with the recognition of new MRSA clones known as community-associated MRSA (CA-MRSA). CA-MRSA strains differ from the older, health care-associated MRSA strains; they infect a different group of patients, they cause different clinical syndromes, they differ in antimicrobial susceptibility patterns, they spread rapidly among healthy people in the community, and they frequently cause infections in health care environments as well. This review details what is known about the epidemiology of CA-MRSA strains and the clinical spectrum of infectious syndromes associated with them that ranges from a commensal state to severe, overwhelming infection. It also addresses the therapy of these infections and strategies for their prevention.
INTRODUCTION
Staphylococcus aureus is the most commonly isolated human bacterial pathogen and is an important cause of skin and soft-tissue infections (SSTIs), endovascular infections, pneumonia, septic arthritis, endocarditis, osteomyelitis, foreign-body infections, and sepsis (559). Methicillin-resistant S. aureus (MRSA) isolates are resistant to all available penicillins and other β-lactam antimicrobial drugs. They were once confined largely to hospitals, other health care environments, and patients frequenting these facilities. Since the mid-1990s, however, there has been an explosion in the number of MRSA infections reported for populations lacking risk factors for exposure to the health care system (4, 37, 105, 133, 140, 153, 158, 192, 237, 247, 259, 284, 300, 304, 306, 349, 383, 393, 456, 460, 654, 762, 802, 816, 972, 1020, 1029). This increase has been associated with the recognition of new MRSA strains, often called community-associated MRSA (CA-MRSA) strains, that have been responsible for a large proportion of the increased disease burden observed in the last decade. These CA-MRSA strains appear to have rapidly disseminated among the general population in most areas of the United States and affect patients with and without exposure to the health care environment.
The purpose of this review is to detail what is known about the epidemiology of CA-MRSA strains and the clinical spectrum of infectious syndromes associated with them, which ranges from a commensal state to severe, overwhelming infection. We will also discuss the therapy of these infections and strategies for their prevention.
CA-MRSA strains have been distinguished from their health care-associated MRSA (HA-MRSA) counterparts by molecular means. HA-MRSA strains carry a relatively large staphylococcal chromosomal cassette mec (SCCmec) belonging to type I, II, or III. These cassettes all contain the signature mecA gene, which is nearly universal among MRSA isolates. They are often resistant to many classes of non-β-lactam antimicrobials. HA-MRSA strains seldom carry the genes for the Panton-Valentine leukocidin (PVL). In contrast, CA-MRSA isolates carry smaller SCCmec elements, most commonly SCCmec type IV or type V. These smaller elements also carry the mecA gene and are presumably more mobile, although few explicit data support this notion (61). They are resistant to fewer non-β-lactam classes of antimicrobials and frequently carry PVL genes.
In addition to these genotypic characteristics, CA-MRSA strains affect a population distinct from those affected by HA-MRSA and cause distinct clinical syndromes. CA-MRSA infections tend to occur in previously healthy younger patients. They have been associated predominantly with SSTIs (105, 642, 654) but have also been linked to several severe clinical syndromes such as necrotizing pneumonia and severe sepsis. In contrast, HA-MRSA strains have been isolated largely from people who are exposed to the health care setting; the patients are older and have one or more comorbid conditions. HA-MRSA strains tend to cause pneumonia, bacteremia, and invasive infections.
CA-MRSA infections, far from being the clinical curiosity that they were in the mid-1990s, have become commonplace and have created a public health crisis in U.S. emergency departments (EDs) and other clinical settings. A population-based study of MRSA infections in San Francisco, CA, in 2004 to 2005 demonstrated that 90% of MRSA infections had onset in the community, with an incidence rate of 316 cases/100,000 population; excluding those with a history of hospitalization in the previous year, the incidence rate was 243 cases/100,000 population. There were many fewer hospital-onset infections, with an incidence of 31 cases/100,000 population (543). Furthermore, a U.S. Centers for Disease Control and Prevention (CDC) study estimated that in 2005, there were 31.8 culture-confirmed invasive MRSA infections in the United States per 100,000 population, amounting to 94,360 cases in that year. Because an estimated 7% of culture-confirmed CA-MRSA infections were invasive (481), it is likely that greater than 1,300,000 MRSA infections, in total, occurred in that year in the United States. Annual outpatient and ED visits for abscesses or cellulitis in the United States were estimated to have nearly doubled from 17.3 to 32.5 cases per 1,000 population between 1997 and 2005 (384), and CA-MRSA isolates are believed to be largely responsible for this rise. In some regions, CA-MRSA isolates account for 75% of community-associated S. aureus infections in children (460).
Complicating the epidemiological framework, some community-onset MRSA (CO-MRSA) infections are caused by HA-MRSA strains, perhaps related to the increasingly common management of complex HA-MRSA infections at home. Thus, MRSA in the community has a complex epidemiology arising from the circulation of “escaped,” or so-called feral, HA-MRSA strains in the general population (115, 117, 154, 437, 529, 852) and the newly recognized CA-MRSA strains (654).
The emergence of new CA-MRSA strains has important implications. Large reservoirs of MRSA isolates now exist outside health care facilities (188, 277, 385). Obviously, this implies that attempts in the United States to contain MRSA using currently accepted methods of infection control based in health care facilities are unlikely to succeed without a similar effort to control spread in the community (154, 186, 217, 543). Additionally, MRSA infections may be more expensive and difficult to treat than infections caused by methicillin-susceptible S. aureus (MSSA) (741). There are relatively few antibiotic agents available to treat MRSA infections (210). Moreover, the available agents have important limitations, and the development of new antibiotic classes has slowed (882, 994). S. aureus isolates that are resistant to each of the few antibacterial drug classes effective against MRSA have been reported (242, 562, 586, 599, 776), raising the theoretical possibility of untreatable multidrug-resistant (MDR) S. aureus infections.
With the antibiotic pressure exerted by the increasing use of vancomycin to treat MRSA infections, nine vancomycin-resistant S. aureus (VRSA) isolates have now been reported in the United States (142, 145, 146, 151, 286, 996). Vancomycin-intermediate S. aureus (VISA) strains, first reported in Japan in 1996 (389, 391), have been identified more commonly in many countries, including the United States (143, 542). The recognition of these strains represents an ominous threat (210). Perhaps a more important concern comes from the observed slow but steady increase in the level of resistance to vancomycin among unselected S. aureus strains that can occur with vancomycin therapy (327, 795, 892, 973). Therefore, clinical reliance on vancomycin—the centerpiece of our armamentarium against invasive MRSA infections—may no longer be possible (229).
EMERGENCE AND HISTORY OF MRSA
In 1961, soon after the introduction of methicillin, the first β-lactamase-resistant penicillin, strains of S. aureus that were resistant to methicillin were identified in the United Kingdom (438). From the 1960s into the early 1970s, MRSA infections in Europe were limited largely to hospital outbreaks caused predominantly by S. aureus phage type 83A (subsequently identified to be sequence type 250 [ST250]); this so-called “archaic clone” gradually became infrequent and was replaced in the 1970s and 1980s by five prevalent clonal lineages (10, 267, 771), although many MRSA backgrounds existed between the 1960s and 2000 (999). In the United Kingdom, MRSA was rare until the early 1990s and has since gradually increased in frequency as a nosocomial pathogen (347). The first case of MRSA infection recorded in Australia was in Sydney in 1965. Thereafter, nosocomial MRSA infections occurred sporadically in Melbourne and Sydney (323) and later appeared in other cities. Most Australian nosocomial MRSA isolates had a distinctive antibiogram, with resistance to trimethoprim-sulfamethoxazole (TMP-SMX), erythromycin, clindamycin, tetracycline, and gentamicin (919). Western Australia remained relatively free of MRSA until the late 1980s, when a distinctive non-MDR (gentamicin-susceptible) MRSA strain appeared in a remote northern region and quickly spread to the rest of Western Australia (908). In Queensland, Eastern Australia, in 2000 to 2006, population-based surveillance of antibiotic resistance patterns of MRSA strains causing infections among inpatients demonstrated an increase from 71 to 315 cases/1 million accrued patient-days for non-MDR (i.e., resistant to at least one non-β-lactam antibiotic and susceptible to ciprofloxacin)-resistant strains. A similar large increase was documented among outpatients during this period, from 52 to 490 cases/1 million outpatient visits, suggesting a rapid dissemination of the non-MDR MRSA strains. At the same time, the rates of inpatient bloodstream infection and other sites of infection caused by any MRSA strain decreased by 35% and 26%, respectively, while among outpatients, the rates increased by 31% and 224%, respectively (671). In Japan, MRSA isolates have been prevalent in academic hospitals since the late 1980s and spread into community hospitals in the 1990s (465), and while community-associated MRSA infections have been reported (465, 723, 881), the first clinical isolate known to carry the PVL genes in the CA-MRSA era was reported in 2003 (429, 881).
In contrast, in Finland, Norway, Sweden, the Netherlands, and Denmark, MRSA infections have remained rare even in the health care setting, which has been attributed by many to strict surveillance programs that have been the norm for decades in each of these nations (18, 469, 843, 860, 899).
In 1968, the first hospital outbreak of MRSA in the United States was reported from Boston, MA (45). In the 1960s to the 1990s, MRSA gradually became entrenched as an endemic pathogen in large, urban, university hospitals in the United States, particularly in intensive care units (ICUs). Subsequently, the percentage of S. aureus isolates from hospitalized patients in the United States that were resistant to methicillin increased from 2.4% in 1975 to 29% in 1991 (704). A diagnosis of MRSA infection was made for approximately 125,969 hospitalizations per year in the United States in 1999 to 2000 (493). Between January 1998 and June 2003, the annual average percentage of S. aureus isolates that were MRSA increased further to 51.6% of ICU and 42% of inpatient non-ICU S. aureus isolates (240). Similar persistently high or increasing rates of MRSA among S. aureus isolates have also been observed for health care settings in many other regions of the world (11, 32, 181, 253, 278, 291, 394, 539, 579, 692, 899).
Prior to the mid-1990s, investigation into the epidemiology of MRSA was limited largely to the health care setting because it was rare that MRSA strains would infect otherwise healthy people. The recognized risk factors then identified for MRSA infection and colonization included recent hospitalization; other exposures to the health care system; residence in a long-term care facility (91, 95, 245, 246, 524, 637, 638, 649, 864, 867, 897) or an acute-rehabilitation unit (578); the presence of an indwelling line or catheter; surgical wounds; chronic liver, lung, or vascular disease; malignancy; recent exposure to antibiotics; intravenous drug use (130); ICU admission; and exposure to a patient with any of these risk factors for MRSA (148, 383, 559, 914).
WHAT IS COMMUNITY-ASSOCIATED MRSA?
The terms CA-MRSA and HA-MRSA have been used to call attention both to the genotypic differences of certain MRSA isolates as well as to the epidemiological and clinical features of the infections that they cause. This sometimes loose interchange of terms has created confusion (216, 606, 796, 878). An essential component of epidemiological studies has been to define the clinical burden of CA-MRSA and HA-MRSA isolates, both of which circulate in the community. Important concepts bearing on these definitions are (i) the setting in which the MRSA infection begins; (ii) current or prior patient exposure to health care settings; (iii) poorly defined CA-MRSA patient risk factors, including prior MRSA infection; (iv) genetic characteristics and antibiotic susceptibilities of the causative MRSA isolate; and (v) the clinical syndrome manifested by the patient.
In 2000, the CDC created a case definition for a CA-MRSA infection: any MRSA infection diagnosed for an outpatient or within 48 h of hospitalization if the patient lacks the following health care-associated MRSA risk factors: hemodialysis, surgery, residence in a long-term care facility or hospitalization during the previous year, the presence of an indwelling catheter or a percutaneous device at the time of culture, or previous isolation of MRSA from the patient (132, 635). All other MRSA infections were considered to be HA-MRSA. This case definition was initially used to demonstrate that MRSA infections were occurring among healthy people in the community without health care exposure (306, 654). The case definition has been modified for the purposes of the CDC's Active Bacterial Core Surveillance Program for invasive MRSA infections to exclude the previous isolation of MRSA as a criterion for HA-MRSA (481).
A simpler, temporal definition is often used to designate CA-MRSA. By this criterion, all infections occurring among outpatients or among inpatients with an MRSA isolate obtained earlier than 48 h after hospitalization would be considered CA-MRSA. Infections meeting either of these temporal criteria are sometimes referred to as “community-onset” MRSA (CO-MRSA) infections.
Other criteria used to define CA-MRSA infections relate to relevant isolate characteristics. CA-MRSA isolates have been pedigreed by their antimicrobial susceptibility profiles, their DNA fragment patterns upon pulsed-field gel electrophoresis (PFGE) (587, 595, 894), protein A (spa) gene typing (486, 866, 868), carriage of PVL genes (540), multilocus sequence typing (MLST) (266, 268), and the type of SCCmec element carried (427). Definitions based on one or more of these isolate characteristics have been used to quantify the MRSA disease burden inside and outside the health care setting, but each one actually provides a different perspective. Importantly, none of the genotypic isolate characteristics are helpful to a clinician caring for an acutely ill patient because assessing them requires molecular strain testing that is not routinely or rapidly available (216).
When the CDC case definition is used to define the burden of disease caused by CA-MRSA isolates, two interesting phenomena can be demonstrated. The application of the definition to cases of infection with MRSA with onset in the community accurately identifies patients with infections caused by CA-MRSA isolates. However, if one uses the case definition to identify patients with infection caused by CA-MRSA isolates, the burden of disease caused by CA-MRSA isolates will be greatly underestimated (216, 217), and this analysis yields a reciprocal overestimation of health care-associated MRSA disease.
If the CDC case definition of CA-MRSA were used in the acute-care setting to aid in the selection of empiric antibiotic therapy, many people who could be managed with clindamycin, for example, would be unnecessarily treated with intravenous antimicrobial drugs because they have an illness caused by a CA-MRSA isolate and not a multiply resistant HA-MRSA isolate (217). The CDC case definition applied to patients with an MRSA infection is not a reliable proxy for the genetic characteristics or phenotype of the MRSA strain causing the infection. For example, at the University of Chicago in 2004 to 2005, the CDC definition would have classified 65.6% (404/616) of MRSA patients as having an HA-MRSA infection. However, among these “HA-MRSA” patients, 47% of the isolates carried SCCmec type IV, 35.9% were PVL positive (PVL+), and 40.1% were ST8 (Table 1) (216), traits attributed to CA-MRSA isolates. These data may have relevance to a large, recent study that estimated that only 8 to 20% of MRSA infections in three communities in the United States were CA-MRSA infections (306) when the CDC definition was applied. It is probable that many more than 8 to 20% of these infections were caused by novel CA-MRSA strains.
TABLE 1.
Characteristics associated with CA-MRSA among consecutive MRSA isolates obtained from patients at the University of Chicago Medical Center in 2004 to 2005a
| Strain characteristic | % of strains with indicated characteristic (n = 616) |
|---|---|
| Panton-Valentine leukocidin gene carriage | 54.6 |
| SCCmec type IV or V carriage | 62.8 |
| MLST-8 or MLST-1 | 59.7 |
| Clindamycin susceptibility | 56.3 |
| Non-multidrug-resistant susceptibility pattern | 62.5 |
Adapted from reference 216 with permission of the publisher. © 2008 by the Infectious Diseases Society of America.
Since about 2003, the distinctions between CA-MRSA and HA-MRSA isolates have become increasingly blurred. As mentioned above, HA-MRSA isolates do circulate in the community, especially among adults. Additionally, many reports have demonstrated that MRSA clones bearing SCCmec type IV, and particularly USA300, the predominant U.S. CA-MRSA PFGE type, now cause nosocomial MRSA outbreaks and infections among patients with chronic illnesses (Table 2). For example, among bloodstream infections in Atlanta, GA, in 2004, 34% of nosocomially transmitted isolates belonged to the USA300 CA-MRSA genotype (820), and in a Detroit, MI, hospital in 2005 to 2007, USA300 accounted for 20% (9/45) of tested nosocomial bloodstream infections (171). A study of surgical skin site infections in Birmingham, AL, from 2004 to 2005 demonstrated that USA300 was a common nosocomial pathogen (716) that first appeared in this setting in 2004 (715). The appearance of CA-MRSA strains in hospitals in the United States is likely responsible for the decreasing non-β-lactam antimicrobial resistance rates noted for MRSA isolates in ICUs between 1992 and 2003 (479). The presence of USA300 increased among MRSA isolates from a 1,000-bed long-term care facility in San Francisco, CA, from 11.3% in 2002 to 64% in 2006 (889).
TABLE 2.
Reports of CA-MRSA strains likely acquired in the health care setting in 1995 to 2008
| Location | Setting/source | Yr | Description | Reference |
|---|---|---|---|---|
| North America | ||||
| Los Angeles, CA | Hospital | 2004 | Breast milk transmission of MRSA in neonatal intensive care unit | 313 |
| Los Angeles, CA | Hospital | 1999-2004 | SCCmec type IV MRSA infections | 580 |
| Atlanta, GA | Hospital | 2003-2004 | 2 prosthetic joint infections caused by USA300 strains | 487 |
| Atlanta, GA | Hospital | 2004 | 34% of nosocomial MRSA bloodstream infections were USA300 | 820 |
| Iowa City, IA | Hospital | 2002-2006 | USA300 in burn trauma unit | 998 |
| Chicago, IL | Hospital | 2000-2006 | Non-MDR MRSA strains | 732 |
| Chicago, IL | Hospital | 2005-2007 | USA300 strains in kidney transplant recipients | 7; T. Stosor, personal communication |
| Denver, CO | Hospitals | 2003-2007 | USA300 bacteremia | 436 |
| Detroit, MI | Hospital | 2000-2005 | SCCmec type IV and PVL+ MRSA in end-stage renal disease patients | 444 |
| Detroit, MI | Hospital | 2005-2007 | USA300 bloodstream infections | 171 |
| Detroit, MI | Hospital | 2006 | SCCmec type IV and PVL+ MRSA in end-stage renal disease patients | 445 |
| Detroit, MI | Hospital | 2005-2006 | 36 USA300 infections with onset >48 h after hospital admission | 626 |
| New York City | Hospital | 2002 | USA400 infection in nursery | 93 |
| New York City | Hospital | 2002 | Non-multidrug-resistant MRSA-caused postpartum infections | 794 |
| Houston, TX | Veteran's hospital | 2003-2004 | USA300 bloodstream infections | 329 |
| San Antonio, TX | Hospital | Not stated | Pneumonia in neonate and colonization of other patients with USA300 strain | 590 |
| United States | Population-based national estimate | 2005-2006 | 12.1% of HA-MRSA (by CDC criteria) invasive infections caused by USA300 strains | 537 |
| Toronto, Ontario, Canada | Maternal-newborn unit, hospital | 2004 | Colonization or infection of 38 babies and 7 mothers by USA300 | 803 |
| 7 Canadian cities | Pathogens from ICU patients | 2005-2006 | 18/193 MRSA isolates were USA300 or USA400 reported from ICU surveillance project from 19 medical centers in Canada; all USA300 and USA400 strains were from 7 cities | 1026 |
| Asia | ||||
| Taiwan | Hospital | 1999-2005 | SCCmec type IV MRSA | 414 |
| Taiwan | Hospital | 1995-2006 | ST59 PVL+, SCCmec type IV or VT MRSA accounted for 18.7% of 257 MRSA bloodstream infections | 160 |
| Australia | ||||
| Western Australia | Hospital | 1995-1996 | Outbreak of MRSA infections caused by a strain commonly isolated in the community | 681 |
| Europe | ||||
| Paris, France | University hospital | 2001-2003 | PVL+, SCCmec type IV MRSA infections | 650 |
| Centre Region, France | Hospitals | 2004-2006 | Non-MDR MRSA strains | 934 |
| Poland | Hemodialysis patient | 2004 | ST80 SCCmec type IV, PVL+ colonizing strain | 80; A. Bogut, personal communication |
| Birmingham, United Kingdom | Hospital | 2004 | CA-MRSA in neonatal care unit | 214 |
| West Midlands, United Kingdom | Hospital | 2006 | PVL+, likely ST30 strain caused fatal pneumonia, sepsis, and shock in a health care worker | 376 |
| South America | ||||
| São Paulo, Brazil | Hospital | 2002-2003 | SCCmec type IV MRSA infection | 912; A. Levin, personal communication |
| Uruguay | Hospitals | 2003-2004 | USA1100 MRSA strains | 58 |
Given the complex epidemiology of CA-MRSA strains in health care settings and the circulation of HA-MRSA strains that occurs in the community, establishing a clear delineation between CA-MRSA and HA-MRSA strains has not been possible. CDC investigators have used a third category of MRSA infections, “health care-associated, community-onset” MRSA (HACO-MRSA) infection (480); this category includes cases that would be HA-MRSA infections by history of health care exposure but have onset in the community. This tripartite classification scheme, HA-, CA-, and HACO-MRSA, still has limitations because a history of exposure to a health care setting does not exclude the possibility of MRSA acquisition and infection in the community (217, 481).
The complex system of nomenclature now in use for MRSA infections in the United States is based on the historical limitation of MRSA infections to the health care system and among those with exposure to it. A revision of the nomenclature is warranted; to better reflect the contemporary epidemiology of MRSA, a paradigm shift is required.
CA-MRSA: an Epidemic and Its Origins
Scattered case reports describing patients with none of the known health care-associated risk factors for MRSA that had MRSA colonization or a clinical infection were published in the 1980s and the mid-1990s (29, 64, 205, 339, 359, 530, 711, 748, 801), including several outbreaks caused by different MRSA strain types in remote regions in Western Australia and then in the Northern Territory of Australia (670). Subsequently, beginning in 1993, case series of MRSA infection and colonization of patients lacking health care-associated risk factors were reported from six continents, in diverse states, nations, and regions (Table 3).
TABLE 3.
Cities, states, regions, and countries with reports of CA-MRSA infections and/or colonization in 1993 to 2009
| Location | Reference(s) |
|---|---|
| Africa | |
| Algeria | 56 |
| Egypt | 264 |
| Nigeria | 317 |
| Tunisia | 57 |
| Asia | |
| Cambodia | 164 |
| China | |
| Mainland | 1028 |
| Hong Kong | 395, 398 |
| India | 652 |
| Japan | 429, 465, 697, 723, 828, 881 |
| Kuwait | 920 |
| Malaysia | 799 |
| Saudi Arabia | 13, 16, 106, 107 |
| Singapore | 1001 |
| South Korea | 437, 474, 522, 563, 708, 710 |
| Taiwan | 90, 159, 160, 165, 166, 275, 410, 411, |
| 412, 414, 415, 525, 547, 548, 879, | |
| 880, 915, 934, 971, 972, 974, 975, | |
| 977, 1012 | |
| Australia/Oceania | |
| Australia | 178, 184, 185, 296, 337, 338, 340, 352, |
| 572, 573, 594, 641, 643, 644, 645, | |
| 647, 670, 672, 680, 681, 761, 861, | |
| 919, 921 | |
| New Zealand | 8, 354, 605 |
| Europe | |
| Austria | 348 |
| Belgium | 227 |
| Bulgaria | 657 |
| Denmark | 46, 77, 508, 509, 510, 923 |
| Finland | 459, 462, 469, 798, 924 |
| France | 225, 247, 312, 533, 555, 934, 955 |
| Germany | 199, 574, 1005 |
| Greece | 168, 461, 467, 571, 673, 814, 815, 909, |
| 962 | |
| Ireland | 778 |
| Italy | 40, 701, 728, 858, 901, 926, 956 |
| Latvia | 604 |
| Netherlands | 419, 856, 946, 1013, 1016 |
| Norway | 366, 379 |
| Russia | 42, 43 |
| Spain | 208, 579 |
| Sweden | 62, 274, 378, 847, 848 |
| Switzerland | 283, 289, 299, 534, 554, 865 |
| United Kingdom | 257, 262, 381, 439, 556, 693, 694 |
| North America | |
| Canada | 120, 144, 344, 395, 404, 443, 496, 541, |
| 585, 586, 690, 794, 812, 813, 817, | |
| 832, 885, 960, 1027 | |
| Mexico | 938 |
| United States | |
| Alaska | 36, 37, 125, 218, 504 |
| Alabama | 189, 373, 714 |
| Arkansas | 784 |
| California | |
| Loma Linda | 426 |
| Los Angeles | 140, 432, 607, 608, 609, 850 |
| Sacramento | 405, 406 |
| San Diego | 137, 193, 195, 589 |
| San Francisco | 153, 235, 303, 481, 543, 703, 744, 788, |
| 888, 1020 | |
| Colorado | 173, 436, 481 |
| Connecticut | 481, 695 |
| Georgia | 306, 385, 475, 481, 820, 821, 1000 |
| Hawaii | 85, 131, 270, 333 |
| Illinois | 19, 215, 216, 300, 301, 383, 403, 422, |
| 423, 733 | |
| Iowa | 846 |
| Kentucky | 446, 811 |
| Maryland | 158, 277, 306, 481 |
| Michigan | 1, 434, 445, 506, 626 |
| Midwestern rural Native | |
| American community | 349 |
| Minnesota | 104, 180, 481, 653, 654, 893 |
| Missouri | 308, 596, 691, 810 |
| Nebraska | 359 |
| New England | 235, 237, 279, 515, 541, 876 |
| New York | 94, 481, 743, 827, 891 |
| North Carolina | 100, 570, 824 |
| Ohio | 433 |
| Pennsylvania | 353, 476, 527, 690, 911, 1023 |
| South Dakota | 30 |
| Tennessee | 28, 72, 105, 188, 450, 473, 481, 655, |
| 688, 883 | |
| Texas | 12, 156, 175, 248, 261, 284, 293, 421, |
| 442, 460, 499, 630, 739, 740, 791, | |
| 841, 842, 855, 898, 993 | |
| Virginia | 1545, 863 |
| Washington and Oregon | 123, 223, 481 |
| West Virginia | 356 |
| Wisconsin | 833 |
| South America | |
| Argentina | 310, 852, 903 |
| Brazil | 292, 656, 757, 758, 813, 960 |
| Chile | 675 |
| Colombia | 17, 26 |
| Uruguay | 58, 564 |
In many countries, MRSA cases among patients without health care risk factors were reported for only small outbreaks or case series, while in the United States, Taiwan, Canada, and Australia, such MRSA infections in patients lacking health care exposure became common. CA-MRSA strains, often responsible for these infections, became endemic pathogens in certain population groups in each of these countries. Within the United States, the incidence of invasive CA-MRSA infections has not been geographically homogeneous (481), and the reasons for this are not understood. The highest prevalence of MRSA colonization recorded (with testing of several anatomical sites) was 42% (18/43 people tested) in a village in Western Australia (681). The impact of globalization has been felt in Scandinavia and other parts of Europe that have a low prevalence of MRSA, where many reported cases of CA-MRSA infection are suspected to have been imported from regions where the disease is endemic (40, 77, 147, 257, 262, 381, 459, 508, 509, 554, 828, 900, 956).
In other regions where the prevalence of CA-MRSA isolates has remained low, community-onset MRSA infections are still more likely to be caused by HA-MRSA strains. For example, HA-MRSA strains were responsible for community-onset bacteremia among military veterans in Taipei, Taiwan, in 1999 to 2002 (165); for community-onset MRSA infections in children in Birmingham, United Kingdom, in 2004 (5); and for SSTIs in outpatients in one region of the United Kingdom in 2005 (774). Few data that describe the epidemiology of MRSA in developing countries are available, but there is concern that CA-MRSA may have devastating consequences if it becomes epidemic in resource-poor regions (666).
An unanswered question is whether CA-MRSA strains are replacing other S. aureus strains causing colonization and infection or if they are instead adding to the burden of S. aureus infections and colonization in the United States and elsewhere. Evidence to support the latter contention is provided by several studies. For example, a study demonstrated that the number of SSTIs treated in U.S. ERs rose dramatically in 1997 to 2005; the increase was probably driven by CA-MRSA isolate infections (384), the predominant cause of SSTIs in ERs according to a recent study (628). At a children's hospital in St. Louis, MO, the number of abscesses with MSSA isolated in 1999 to 2007 increased 5-fold, while during the same period, the number of isolates with MRSA increased 250-fold. The increase in numbers of MSSA infections was not due to an increase in the number of cultures sent, and the USA300 PFGE pattern was found for six MSSA isolates tested (691). In a long-term care facility in San Francisco, CA, as USA300 became the predominant MRSA strain to cause infections, the incidence of MRSA infections doubled from 1997 to 2006 (889). In contrast, in other geographic locales, there is little evidence that the overall incidence of invasive S. aureus infections is increasing as rapidly; instead, it appears that as the number of invasive CA-MRSA infections rise, the number of invasive infections caused by HA-MRSA is decreasing. For example, in Chicago at Cook County Hospital, the incidence density, that is, the person-time incidence rate, of bloodstream infections caused by MRSA diagnosed >72 h after admission in January 2000 to June 2003 did not differ compared with that in July 2003 to December 2006. However, the proportion caused by CA-MRSA strains (defined by a specific antibiotic susceptibility pattern) doubled from 24% to 49% (732). In Denver, CO, at a city-owned hospital and its affiliated clinics, the number of community-acquired (i.e., a culture obtained from an ED or clinic or within 48 h after a hospital admission) S. aureus SSTIs did not increase overall, but the percentage caused by MRSA increased from 6% in the first quarter of 2002 to 45% in the second quarter of 2004 (P < 0.001) (173). Similarly, in the Calgary Health Region of Canada, as MRSA became a more common cause of S. aureus bacteremia in 2000 to 2006, the total incidence of S. aureus bacteremia did not rise (512).
A similar trend has been demonstrated for the prevalence of asymptomatic MRSA carriage. For example, there is evidence from population-based surveillance in the United States that as the prevalence of MRSA nasal colonization increased, the overall prevalence of any S. aureus nasal colonization decreased (895).
The emergence of CA-MRSA isolates and associated increases in methicillin resistance among S. aureus isolates may be recapitulating the epidemiological pattern that marked the increase in the prevalence of penicillin resistance among S. aureus isolates circulating in the community that had occurred years earlier. Resistance to penicillin, mediated by the production of β-lactamase, was identified among strains of S. aureus almost immediately after the introduction of penicillin in 1944 (477). By the late 1970s more than 80% of these isolates were penicillin resistant, and rates of penicillin resistance have remained in this range since. If the emergence of MRSA is following this pattern (148), the percentage of community-associated S. aureus infections caused by MRSA strains may continue to rise in the coming decades and may approach 100%.
Abundant molecular evidence supports the hypothesis that CA-MRSA clones have arisen in the community by the horizontal transfer of SCCmec elements and PVL genes, molecular features commonly associated with CA-MRSA isolates as well as perhaps other virulence and resistance factors, to the genomes of MSSA strains (212, 252, 281, 285, 388, 392, 536, 621, 687). However, a comparative study of CA-MRSA isolates from sentinel surveillance health care facilities in Minnesota, North Dakota, and Nebraska showed that locally prevalent CA-MRSA and MSSA strains were related and that the identified CA-MRSA strains differed from HA-MRSA isolates collected at the same facilities (285). Some researchers have proposed that an ST30 MSSA strain first acquired the PVL genes and then the SCCmec type IV element to become a PVL+ MRSA strain now uncommon in the United States (234). However, in Wisconsin, an ST30 strain isolated in the 1980s carrying the SCCmec type IV element but lacking PVL genes was identified, possibly representing a precursor to a later PVL+ CA-MRSA strain (92). These observations suggest that the currently prevalent CA-MRSA strains may have developed over several decades of complex evolution.
In Australia, it was hypothesized that new clones of CA-MRSA arose on several occasions in remote aboriginal communities after the introduction SCCmec type IV into already prevalent and virulent MSSA background strains (905). In a study of MRSA infections in 2004 to 2005 in the Northern Territory, clonal cluster 75 (CC75) strains (a clonal cluster not described for any other region) represented 25% of S. aureus isolates; MRSA and MSSA CC75 strains were both found among these isolates in a ratio of 2:1 (594), suggesting the local transmission of SCCmec to an MSSA CC75 clone with subsequent clonal expansion. In contrast, in other remote communities in Australia, such transfers did not occur in the most prevalent MSSA clones colonizing the population (680).
Why Did CA-MRSA Strains Appear and Succeed?
Several hypotheses to explain the emergence and entrenchment of CA-MRSA isolates have been proposed. None of these hypotheses definitively explain the observed epidemiological data. They are reviewed briefly here.
Because the emergence of new CA-MRSA isolates occurred in the late 1990s in tandem with the increasing use of fluoroquinolones (FQs), some have suggested that the relationship between the phenomena might be more than a coincidence. However, there is no known mechanism to link these phenomena. If they are related, the mechanism must be complex because most CA-MRSA isolates in the United States and Australia have been susceptible to FQs. Circumstantial evidence for an FQ-MRSA association in the health care setting is limited. The increased use of FQ has been associated with the elimination of MSSA strains from the colonization of the nasal mucosa (517), which might predispose one to colonization by MRSA strains. Other ideas have been proposed to link FQ exposure to epidemic CA-MRSA disease. For example, in an in vitro study, CA-MRSA strains obtained from subjects with nasal colonization were exposed to a subinhibitory concentration of FQ. In a microarray analysis, this resulted in the increased expression of 53 open reading frames of the exposed CA-MRSA isolates, including mecA, suggesting that β-lactam resistance may be increased by FQ exposure (890). Moreover, the restriction of FQ use in the health care setting has been shown to decrease the rate of MRSA isolation (121, 152), and FQ use has been identified as a risk factor for MRSA infection of hospitalized patients (254). Patients with a nosocomial MRSA infection at one medical center in 1997 to 1999 were more likely than patients with a nosocomial MSSA infection to have been previously treated with the FQ levofloxacin (odds ratio [OR], 8.01; 95% confidence interval [CI], 3.13 to 20.3) (345). A study in Hong Kong demonstrated that when MRSA nasal carriers were treated with an FQ or a β-lactam, they had a significantly increased MRSA nasal bacterial burden demonstrated by quantitative nasal culture and an increased likelihood of MRSA contamination of fomites in their environment (163), suggesting that FQ exposure may be associated with the dissemination of MRSA strains. Further circumstantial evidence of a relationship between FQ use and MRSA infection comes from an administrative health database in the United Kingdom, where in 2000 to 2004, 1,981 adults with an MRSA infection and no known health care exposure had a higher risk (OR, 3.37; 95% CI, 2.80 to 4.09) of having an FQ prescribed within the year prior to their MRSA infection than did 19,779 matched controls (809).
Other researchers have noted that the introduction of a routine childhood conjugate pneumococcal vaccination (Prevnar) in the United States in February 2000 coincided with the increase in the CA-MRSA infection rate and suggested that there may be a causal, and not just a temporal, link between the two phenomena. The United States, which has uniquely experienced epidemic CA-MRSA infections, was the only country recommending the vaccine for routine use for several years. Moreover, the recommendation for the routine use of Prevnar in 2002 in Canada may have retrospectively correlated with a rise in CA-MRSA infections there. Conversely, CA-MRSA was already commonly reported from Australia in January 2005 at the time of the addition of Prevnar to the National Immunization Program Schedule for the routine vaccination of children younger than 2 years of age. Prevnar was introduced as a recommended routine childhood vaccine in September 2006 in the United Kingdom, where CA-MRSA has continued to be rare. Only occasional case reports of MRSA infection in the community in the United Kingdom have been published to date. By August 2008, Prevnar was introduced as a routine childhood vaccine in 26 nations, introduced in 18 nations since 2006 (139). If the use of Prevnar is related to CA-MRSA incidence, more countries may experience CA-MRSA epidemics, but it should be noted that the predominant CA-MRSA genetic background differs in much of the world from those in the United States and Canada, and this may affect the association.
Biological plausibility for this relationship has been suggested by the observation that Prevnar vaccinees have decreased asymptomatic carriage of the seven vaccine serotypes of Streptococcus pneumoniae. Some researchers have postulated that decreased pneumococcal colonization may provide a new ecological niche for colonization with CA-MRSA strains; this is supported by evidence that the cocarriage of S. pneumoniae and S. aureus was found rarely among 790 healthy children in Israel in 2002 (753), a country with few CA-MRSA infections. In the Netherlands, a negative correlation was found between colonization by the vaccine serotypes of S. pneumoniae and S. aureus in children who had recurrent otitis media; S. aureus became a more common cause of otitis media in children after Prevnar vaccination (78). One mechanistic hypothesis suggested that S. aureus is inhibited by H2O2 produced by S. pneumoniae strains, an effect demonstrated in vitro (752, 754), which theoretically may decrease the likelihood of cocolonization in the nasal mucosa or elsewhere. Hypothetically, if Prevnar vaccination opened an ecological niche and if CA-MRSA strains were prevalent in the community and more fit than other S. aureus strains, CA-MRSA strains would occupy the niche.
Brook and Gober demonstrated an increase in the recovery of MRSA from acute otitis media with otorrhea. Among 50 children in suburban Washington, DC, in 1993 to 1998, prior to the licensure of Prevnar, 0/61 bacterial isolates recovered were MRSA isolates, compared with 5/63 (10%) MRSA isolates recovered in 2001 to 2006 (P < 0.05). During the second period, 92% of the patients had received Prevnar (97). Because otitis media is an infection of the middle ear caused by pharyngeal flora, this increase in MRSA otorrhea may reflect an increased pharyngeal colonization with MRSA with the elimination of vaccine serotypes of S. pneumoniae.
Controversy still surrounds the notion that Prevnar is associated with increasing MRSA colonization in a given population; some authors have not found evidence to support the contention that cocolonization with S. aureus and S. pneumoniae is uncommon (79, 597). One study showed no difference in the rates of S. aureus nasal carriage in children with otitis media who had received Prevnar and those who had not (176). Another study demonstrated no increase in the prevalence of S. aureus (neither MSSA nor MRSA) nasal colonization in a large group of children seen in Massachusetts primary care offices from November 2003 to April 2004, before the widespread use of Prevnar, compared with the prevalence from October 2006 to April 2007, after its introduction. However, that study was limited in that only children 3 months to 7 years of age were included, enrichment broth was not used to enhance the detection of S. aureus, and New England was among the last regions of the United States to report widespread CA-MRSA infections (518).
In a similar vein, group B Streptococcus and CA-MRSA isolates may compete for colonization in the vagina. In a study of vaginal colonization among pregnant women in New York City, NY, only 1/13 (7.7%) patients vaginally or rectally colonized with CA-MRSA (i.e., the isolates carried the SCCmec type IV or V element) were also colonized with group B Streptococcus; in contrast, 26/52 (50%) group B Streptococcus-colonized women had MSSA vaginal colonization, possibly suggesting increased competitive fitness among CA-MRSA strains relative to that of MSSA with respect to group B streptococcal colonization (161).
SCCmec ELEMENTS AND CA-MRSA
Nearly all MRSA strains contain the SCCmec element, which is uniformly integrated into a specific S. aureus chromosomal site known as orfx. SCCmec, which was likely acquired from a coagulase-negative staphylococcus species (622, 1004), carries the mecA gene, which encodes penicillin binding protein 2a (PBP2a), a cell wall transpeptidase, which, in conjunction with native PBP2, allows continued cell wall synthesis in the presence of β-lactams (726). In addition, SCCmec elements variably carry the mecR1 and mecI genes, which regulate the expression of mecA, with increased mecA translation induced by β-lactam antibiotic exposure. The mecA gene and its regulatory elements, taken together, comprise the mec complex (463). Different complex types have evolved, giving rise to MRSA strains with the class B mec complex, which express PBP2a constitutively, and strains with the class A mec complex, which express PBP2a only when induced by β-lactams. Two additional mec complexes, called classes C and D, have also been identified (390), although the class D complex has been found only in coagulase-negative Staphylococcus species.
Main Types of SCCmec Elements
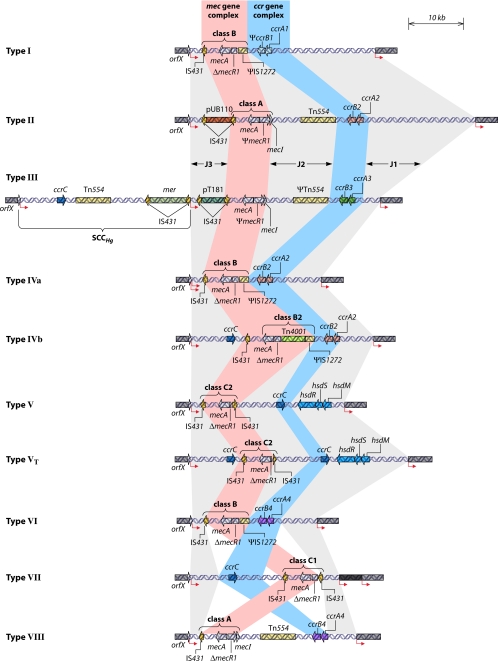
To date, nine types of SCCmec (types I to VIII and VT) have been defined, which can be distinguished by the type of ccr gene complex that mediates the site-specific excision and insertion of the SCCmec cassette out of or into the bacterial genome and the class of mec complex that they bear (428, 430, 431) (Fig. 1). The large SCCmec types I to III are present in HA-MRSA strains and were likely transferred to S. aureus from a commensal staphylococcal species on a few occasions (565). Among U.S. HA-MRSA isolates, SCCmec type II elements are usually carried, whereas SCCmec type III elements are more commonly identified in HA-MRSA isolates in other countries. The smaller SCCmec types IV and V, however, are believed to have been transferred to methicillin-susceptible backgrounds frequently, with the resultant emergence of novel, fit MRSA strains bearing the type IV or V elements (61, 207, 357). One study suggested that the type IV SCCmec element has been transferred to an MSSA strain >20 times (771). Although it was initially thought that SCCmec type IV first integrated into pathogenic S. aureus backgrounds in the mid-1990s, it is now known that this integration first occurred much earlier. For example, in Taiwan, SCCmec type IV elements were identified in PVL-negative ST59 MRSA isolates from 1992 (978).
FIG. 1.
Classification scheme for SCCmec type by ccr complex and mec complex type. (Adapted from reference 427.)
The type IV SCCmec element has been strongly associated with strains causing MRSA infections in patients with no HA-MRSA risk factors (212, 565) in the United States and elsewhere. The type II and III SCCmec elements include sites, called by some the junkyard regions, for the insertion of genes conferring non-β-lactam resistance phenotypes to S. aureus strains and, therefore, are more commonly associated with MDR phenotypes (392, 430). The presence of the SCCmec type IV element, which lacks genes conferring non-β-lactam antimicrobial resistance, may account for the decreased likelihood that CA-MRSA strains are MDR. Several subtypes of SCCmec type IV that vary depending on the typing system used have been described. An international committee of experts in 2009 formulated a consensus nomenclature for SCCmec types (427).
SCCmec Types IV and V in CA-MRSA Isolates
Children may be at a higher risk of infection by SCCmec type IV-bearing isolates than adults. In a study of MRSA infections at the University of Chicago Hospitals in 2004 to 2005, children were more likely than adults to be infected by strains that carried SCCmec type IV and the PVL genes and by strains that were susceptible to many non-β-lactam antibiotics (216, 219). Although no clinical data were available to assess the rate of community-onset infections, surveillance at a South Korean hospital in 2003 to 2005 demonstrated that children were more likely to be infected by SCCmec type IV-bearing strains (68% ST72 strains bearing SCCmec type IV and 6.8% ST5 strains bearing SCCmec type II), while adults were more likely to be infected by SCCmec type II-bearing strains (12% ST72 and 58% ST5 strains). Pediatric strains were also more likely to be susceptible to gentamicin, clindamycin, ciprofloxacin, and rifampin (709). These studies suggested that children are differentially exposed or differentially susceptible to SCCmec type IV-bearing strains or perhaps reflect more common exposure to the health care setting among adults. The reasons are not known, and this area requires further research.
SCCmec type V is similar to type IV in that it is small and presumably similarly mobile. It has been found in CA-MRSA isolates predominantly in Australia (670) and Taiwan (411, 414, 975). SCCmec type V is rare in Europe and the United States. However, in 2004 an ST377 strain of PVL+ MRSA with SCCmec type V was reported from Greece (168, 316) and elsewhere (312). More research is needed to determine why SCCmec type IV is associated with prevalent CA-MRSA strains, including USA300, and why strains bearing SCCmec type V remain limited largely to Asia and are relatively uncommon.
Because SCCmec types IV and V appear to be highly mobile, the dissemination of MRSA in a community population has probably been accomplished most commonly by transfers of MRSA strains from carriers to other individuals and also by the transfer of the smaller SCCmec elements that can be passed from MRSA strains to MSSA strains or even from a coagulase-negative staphylococcal strain to an MSSA strain (269). All these processes are probably facilitated in the presence of antibiotic receipt (84, 831).
In the countries of northern Europe that have accurate population-based reporting of MRSA infections, there has been an increase in numbers of reports of polyclonal CA-MRSA colonization and infection by SCCmec type IV-bearing, PVL+ MRSA strains. This presumably resulted from the easy and rapid transmissibility of the SCCmec type IV element from MRSA backgrounds to methicillin-susceptible S. aureus backgrounds. For example, in Denmark, the first ST80, PVL+, SCCmec type IV isolate was identified in 1993, although by 2004, only 88 cases were recorded (510). Among the few known MRSA isolates from infections of outpatients in Denmark in 2004, 82% (28/34 isolates) carried SCCmec type IV, and 47% were PVL+ (77). Another study from Copenhagen, Denmark, demonstrated the initial spread of PVL+ SCCmec type IV and V strains and showed that many genetic background types bearing these SCCmec elements were present there in 2003 to 2004 (46). SCCmec type IV became the most common SCCmec type carried by MRSA strains isolated from inpatients at a hospital in Basel, Switzerland. SCCmec type IV carriage increased from 33.3% among MRSA strains isolated in 2000 to 57.9% in 2004. Most of the SCCmec type IV-bearing MRSA strains were MDR and were isolated from patients who had CA- or HA-MRSA infections by the CDC definition (865).
VIRULENCE FACTORS IN CA-MRSA
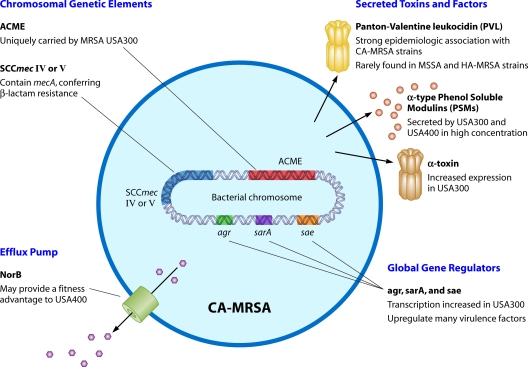
A number of putative virulence factors have been identified by experimental and epidemiological studies of CA-MRSA strains, particularly in USA300 (Fig. 2). They are reviewed here.
FIG. 2.
Hypothetical virulence factors in USA300 and other CA-MRSA strains. For details, see the text.
PVL and CA-MRSA
PVL is a two-component S. aureus pore-forming protein encoded by the lukF-PV and lukS-PV genes. It was first described in 1894 by Van de Velde (935) and was associated with SSTIs in 1932 by Panton et al. (707). The genes encoding PVL, which can spread from strain to strain by bacteriophages, were previously believed to be present in fewer than 5% of unselected clinical S. aureus isolates (540, 707) before the advent of CA-MRSA strains in the mid-1990s, although the genes were transiently found in a circulating ST30 clone in Japan in 1979 to 1985 (566).
PVL and CA-MRSA infections.
In the United States, after the mid-1990s, carriage of the PVL genes has been closely linked to infections caused by CA-MRSA strains in numerous epidemiological studies. Approximately 60 to 100% of CA-MRSA strains (by various definitions) have been shown to carry PVL genes. For example, in 2000, a large study from Minnesota found that 77% of patients with infections caused by CA-MRSA isolates (by the CDC case definition) were PVL+, but only 4% of HA-MRSA isolates were PVL+ (654). Among 812 military recruits in Texas in 2003, 66% of 45 MRSA strains colonizing the nares of recruits or causing infections among them were PVL+ (259). PVL genes were found in 33.5% of 671 banked MRSA isolates obtained in 1997 to 2002 from four clinical sites in the San Francisco area. Among MRSA isolates from detainees in the San Francisco County Jail, more than 70% were PVL+; of MRSA isolates from a clinic specializing in the treatment of SSTIs (all collected in 2000), 69% were PVL+. All PVL+ MRSA strains also carried the SCCmec type IV element (232).
While PVL has been strongly linked epidemiologically to prevalent CA-MRSA strains, it is not known with certainty how they contribute to their fitness and/or virulence or if they are merely a marker for other fitness or virulence determinants. PVL+ strains carrying SCCmec type IV, V, or VT (90, 411) with varied background genotypes in many geographic settings have now been identified, although the chromosomal site of PVL gene integration lacks any known genetic linkage to the insertion site of SCCmec elements. Moreover, no other S. aureus toxin genes have been associated as strongly with CA-MRSA strains as PVL (234, 609, 933). PVL genes are rarely found in MRSA strains carrying SCCmec types I, II, and III.
PVL genes may be more common among S. aureus isolates causing clinically apparent infection than among isolates causing asymptomatic colonization, although there are conflicting data. For example, among 13 SCCmec type IV-bearing MRSA strains colonizing New York State Prison detainees in 2005, 8 (61.5%) were PVL+. S. aureus strains causing infection, however, were more likely to be PVL+ than those causing asymptomatic colonization (24/60 strains [40%] versus 32/124 strains [25.8%]; P = 0.0498) (560). In contrast, among clinical USA400 MRSA isolates (see below) in the Calgary Health Region in Canada in 2000 to 2005, PVL+ and PVL-negative strains were as likely to cause mild or severe disease, and both were equally likely to asymptomatically colonize (1027).
In the United States, PVL genes have been almost universally detected among CA-MRSA strains causing SSTIs and S. aureus invasive diseases such as community-acquired necrotizing pneumonia (86, 190, 312, 321, 540, 618, 720, 917), severe sepsis, and other sometimes fatal infections (6, 33, 76, 133, 192, 584, 636, 719, 907, 917). Among patients with S. aureus pneumonia, higher mortality and an increased likelihood of sepsis, hemoptysis, and pleural effusion were documented for cases caused by a PVL+ strain (321).
In Australia, the first reports of community-onset MRSA infections in 1993 were caused by strains that lacked PVL genes. Subsequently, however, a polyclonal surge of largely PVL+ MRSA infections occurred among previously healthy, young adults and children; each newly described PVL+ SCCmec type IV-bearing community strain identified in that country had a distinct geographic distribution (670). Furthermore, the clinical syndromes among SSTIs in Australia caused by PVL+ MRSA strains differed from syndromes caused by PVL-negative strains. For example, in Queensland, Australia, in 2004 to 2005, 59% of SSTIs caused by PVL+ S. aureus strains were designated “furunculosis,” compared with only 10% of SSTIs caused by PVL-negative strains; the remainder of the SSTIs were described as “cellulitis” (34% versus 58%, respectively) or “surgical-wound infection” (7% versus 32%, respectively). Patients with PVL+ strains were younger, less likely to have SSTIs as a complication of surgery, and more likely to have been hospitalized for the management of SSTIs (642).
Studies from many countries in Europe also documented the emergence of PVL+ SCCmec type IV-bearing CA-MRSA strains in multiple S. aureus backgrounds, although CA-MRSA infections occur far less commonly there than in the United States (Table 4). For example, only 22.2% (12/54) of isolates from CA-MRSA patients (by the CDC case definition) submitted to an Irish reference laboratory from 1999 to 2005 were PVL+ (778) (Table 4).
TABLE 4.
Case series and surveillance studies of PVL+ SCCmec type IV- or V-bearing community MRSA infections reported in Europe indicating the genetic backgrounds identified
| Country and/or city | Collection details | Yr | No. of MRSA isolates tested | No. (%) of PVL+ isolates | Molecular typing results for PVL+ isolates | Reference |
|---|---|---|---|---|---|---|
| Finland | CA-MRSA from national reporting system | 2004-2006 | 298 | 90 (30) | ST80-IV/t044, ST8-IV/t008, ST30-IV/t019, ST1-IV/t127, miscellaneous types | 459 |
| Ireland | MRSA from national reference collection | 1999-2005 | 1,389 | 25 (1.8)a | ST5, ST8, ST22, ST30, ST80, ST154 | 778 |
| Denmark | Sample of isolates from CA-MRSA patientsb in Denmark collected by the Statens Serum Institut | 1999-2006 | 244 | 163 (66.8) | MLST clonal clusters CC1, CC5, CC8, CC22, CC30, CC59, CC80, CC88, CC152/377, CC398, miscellaneous CCs | 509 |
| Lyon, France | CA-MRSA and CA-MSSA infections; case series | 1999-2001 | 14 | 14 | 13 shared PFGE type; 1 differed by 1 band | 247 |
| Fréjus-Saint Raphaël, France | Community-onset MRSA disease at 1 hospital | 1999-2003 | 21c | 6c (28.6) | 5 same PFGE type as dominant strain in reference 247; 1 differed by 1 band; all agr type 3 | 225 |
| Geneva, Switzerland | SSTI patients with no health care exposure from private physicians' offices in city | 2002 | 10 | 7 (70) | 6 PFGE pulsotypes | 534 |
| Geneva, Switzerland | CA-MRSA isolates (i.e., from patients with no hospitalization in past 12 mo and nonstandard antibiogram) from 1 hospital | 2002-2005 | 151 | 60 (39.7) | ST1, ST5, ST8, ST30, ST59, ST80, ST152 | 299 |
| London, England | Ciprofloxacin-susceptible MRSA strains from 2 hospitals | 2000-2006 | 194 | 49 (25.3) | 24 spa types, ST1, ST8, ST59, ST80 | 694 |
| England and Wales | S. aureus isolates from clinical infections; reference collection | 2002-2003 | 470d | 23 (4.9); 12 were MRSA | 11 MRSA isolates, ST8 (n = 1), ST22 (n = 1), ST30 (n = 1), ST80 (n = 10) | 401 |
| England and Wales | Ciprofloxacin-susceptible strains isolated from boils, abscesses, and pneumonia from centers across England and Wales | 2005-2006 | 1,087 | 275 (25.3) | CC1 (n = 13), CC5 (n = 10), CC8 (n = 70), CC22 (n = 33), CC30 (n = 49), CC59 (n = 4), CC80 (n = 88), ST93 (n = 1) | 257 |
| Austria | Large reference collection | 2001-2006 | 1,150 | 94 (8.2) | ST5, ST8 (32%), ST22, ST30, ST80, ST152 (17%), ST777 | 490 |
| Vienna, Austria | MRSA isolates obtained at 1 hospital from patients with colonization or infection resistant only to β-lactams or β-lactams and fusidic acid | 1999-2007 | 41 | 16 (39) | 9 spa types (t021, t975, t3140, t3150, t044, t376, t3149, t3256, t1028) | 48 |
| Madrid, Spain | PVL+ MRSA infections in an emergency department (9 SSTIs, 1 bacteremia, 2 asymptomatic colonization, and 1 otitis media) | 2004-2007 | 13 | 13 | ST5, ST8, ST80 | 147 |
| Dresden, Germany | SSTIs with PVL+ strains | 2004-2005 | 3 | 3 | ST8, ST80 | 619; S. Monecke, personal communication |
| Örebro County, Sweden | Clinical PVL+ isolates (4 SSTIs, 1 joint, 1 pleural effusion) | 2001-2005 | 6 | 6 | ST8, ST36, ST80, ST152, ST154, ST256 | 62 |
All PVL+ isolates were from 2002 to 2005.
CA-MRSA infections had their onset in the community or were cultured <48 h after hospital admission, and the patients had no stay in a hospital or long-term care facility for 12 months.
Six patients with SSTI and no health care exposure had infections with PVL+ MRSA strains among 21 patients with community-onset MRSA infections.
This is the number of S. aureus isolates; the authors did not report how many were MRSA isolates.
In Asia, the reported occurrence of MRSA infections that have onset in the community and the rate of PVL gene carriage have varied by country. In Taiwan, PVL+ CA-MRSA strains of a single background type commonly cause infections. PVL genes were identified in all 17 isolates in one study of CA-MRSA infections in children, the majority of whom had SSTIs (972). Of 204 MRSA isolates colonizing the nares of healthy Taiwanese children in 2005 to 2006, 28% were PVL+; all PVL+ MRSA strains had one of two PFGE types, and all tested isolates were ST59 isolates or single-locus variants of ST59 (411).
In South Korea and China, PVL+ strains remain rare among reported community-onset MRSA infections. Only 1 of 138 MRSA isolates from patients in South Korea with CA-MRSA infections (by CDC criteria) in 2004 to 2005 was PVL+ (708). Among 3,096 healthy people in Seoul, South Korea, in 2003, the MRSA colonization prevalence was 0.97%; 30% of MRSA isolates carried SCCmec type IV. Of the 30 MRSA isolates identified, 70% (21) were PVL+; these were polyclonal, representing four STs, ST1, ST5, ST72, and ST83 (437). In Wenzhou, China, of 195 S. aureus isolates from clinical specimens at a single medical center in 2005 to 2006, 25 (12.8%) were PVL+; these belonged to six MLSTs. Of the 25 PVL+ S. aureus isolates, 19 were MRSA isolates. Six of the 25 PVL+ S. aureus isolates, including 2 of 19 MRSA isolates, were from “community-acquired” infections, although the criteria for this designation were not provided (1022). At pediatric hospitals in five Chinese cities in 2005 to 2006, 73 MRSA isolates were identified among 4,254 clinical S. aureus isolates. Of the 73 MRSA isolates, 30% (22/73) were PVL+, and these included the ST1, ST910, ST88, ST59, and ST338 genetic backgrounds. Among the 22 PVL+ MRSA strains, 16 (73%) were CA-MRSA infections according to the CDC case definition (1028).
The prevalence of the PVL genes was less common among MSSA isolates than among MRSA isolates from infections and colonization in several studies. For example, in a case-control study in rural Alaska in 2000 following an outbreak of MRSA SSTIs, no MSSA isolates causing colonization (n = 49) or clinical infection (n = 34) carried PVL genes, compared with 92% (73/79) of MRSA isolates causing colonization or infection (36). Among S. aureus isolates causing musculoskeletal infections in 59 children in Houston, TX, in 2000 to 2002, causative MRSA isolates were more likely to carry PVL genes than were causative MSSA isolates (27/31 versus 6/24; P = 0.00001) (584). PVL+ MSSA strains can cause serious infections (321, 765, 797, 851, 902), although such outbreaks appear to be relatively rare.
Role of PVL in the pathogenesis of MRSA infections.
PVL is a leukocidin that can lyse the cell membrane of human neutrophils, although its importance in pathogenesis is controversial. Recent evidence suggests that PVL may also inactivate mitochondria (315) and culminate in apoptosis. In animal models, PVL has been shown to be dermonecrotic (190, 981), perhaps explaining the pathobiology of the characteristic skin lesions associated with CA-MRSA SSTIs. These lesions often resemble an injury produced by a spider bite (241, 954), although common house spiders were not found to be carriers of CA-MRSA (50), and a correlation between the geographic distribution of recluse spiders and these typical lesions associated with MRSA infection has been lacking.
Recently, the importance of PVL in the pathogenesis of SSTIs and necrotizing pneumonia has come into question. Voyich et al. found that the presence or absence of PVL genes in MRSA strains did not affect strain virulence in mouse models of sepsis and SSTI, and their presence did not decrease neutrophil survival in in vitro assays (963). Wardenburg et al. found that the presence or absence of PVL did not affect the mortality rate of S. aureus pneumonia in a mouse model. Also, the absence of the PVL gene locus in deletion mutants did not alter the cytotoxic effect of wild-type USA300 (LAC) and USA400 (MW2) strains in vitro in human alveolar epithelial cells (983). That same group also found no difference in pneumonia and skin abscess rodent models after inoculation with a USA300 strain or its isogenic PVL knockout (982). In contrast, Labandeira-Rey et al. demonstrated that both the purified PVL protein and an RN6390 derivative with the PVL genes overexpressed on an introduced phage caused necrotizing pneumonia in a mouse model (498). In a model of rat pneumonia, in contrast, USA400 and USA300 clones and their respective isogenic PVL knockout strains did not differ in virulence (624). Diep et al. compared wild-type and isogenic PVL knockout strains of two USA300 isolates and demonstrated no differences in the isogenic mutants in their proteomes or in their global gene expression patterns irrespective of the presence of PVL genes (230). That same group challenged rabbits intravenously with a 1:1 mixture of a wild-type USA300 strain and an isogenic PVL knockout mutant and demonstrated that 24 and 48 h, but not 72 h, later, the PVL-containing wild-type strain was present in a greater density in homogenized kidneys of sacrificed rabbits, suggesting that PVL may provide an early survival benefit to MRSA strains in this model (230). Tseng et al. found that PVL was responsible for increased tissue damage in a myositis model in young, but not older, mice by comparing an MRSA isolate obtained from a patient with necrotizing fasciitis with its isogenic PVL knockout mutant (916). Those authors hypothesized that the younger mice had a more robust neutrophil response to PVL, resulting in more severe injury to muscle (916).
Hongo et al. found that PVL toxin did not produce a lysis of neutrophils from BALB/c mice, but the lytic activities against human neutrophils of supernatants from USA300 and USA400 strains were abrogated in the presence of monoclonal anti-PVL antibodies (402). Löffler et al. found that PVL did not lyse neutrophils from monkeys or mice, but it did lyse rabbit and human neutrophils (553). These findings support the importance of PVL in the pathogenesis of CA-MRSA infections in humans, while mouse models may not be appropriate to assess the contribution of PVL.
The conflicting results for the role of PVL in the pathogenesis of CA-MRSA infections may relate to the amount of PVL produced by individual strains. For example, Varshney et al. demonstrated that in a variety of clinical MRSA and MSSA strains, PVL production varied. When used in a murine skin infection model, strains with more PVL production produced larger skin lesions and higher bacterial burdens in the lesions at 7 days (947).
The PVL gene DNA sequences have allelic variation that may help to explain the conflicting results seen in animal studies. Among 28 S. aureus strains that underwent PVL gene sequencing, 7 nucleotide polymorphisms were found, but only 1 resulted in an amino acid substitution. The strains included representatives of the CA-MRSA ST80, USA300, and USA400 clones as well as a phage type 80/81 strain (ST30). The PVL gene sequence in the phage type 80/81 strain was hypothesized to contain the progenitor of the PVL gene sequences carried by the other isolates in the collection (1007). The PVL lukSF-PV gene sequences found in an international collection of isolates had two predominant variants; the two variants differed by a single amino acid substitution. The R variant was found only in USA300 and USA400 MRSA isolates from the United States, while the H variant was common in MSSA strains obtained elsewhere (685). In a separate study of a different group of S. aureus isolates, the R variant was found in USA300 and USA400 strains and in a CC93 clinical isolate from Australia; in contrast, the H variant was present in MSSA and MRSA strains from around the world and nearly all PVL+ CA-MRSA clones outside the United States (249). It is possible that the polymorphisms distinguishing the R and H variants may result in changes in the function of the PVL protein, potentially explaining the apparently contradictory results demonstrated in animal studies of the virulence of PVL+ MRSA strains (498, 983). The importance of these polymorphisms, if any, requires further research (441).
Other Virulence Factors in CA-MRSA Strains
Other candidate genes have been proposed to be important virulence factors driving the dominance of USA300 and other CA-MRSA clones in the community (679). It is estimated that 22% of the genome of S. aureus varies among strains, and these variable regions may include structural genes and regulatory apparatus that may influence fitness, pathogenicity, and virulence (287). Several examples that have received recent attention are discussed in this section.
ACME.
The arginine catabolic mobile element (ACME) is a 30.9-kb DNA element that contains 33 expressed reading frames and is present in many USA300 strains. It is integrated into orfx, the same site on the S. aureus chromosome into which SCCmec integrates, and it is frequently found in coagulase-negative staphylococcal species (236). It has been postulated that ACME may play a role in pathogenesis by conferring an enhanced ability of CA-MRSA strains to colonize the skin of healthy people and, thus, more easily disseminate in the community, although no experimental data exist to substantiate this hypothesis. ACME contains the structural gene arcA, encoding arginine deiminase, which in Streptococcus pyogenes inhibits the proliferation of peripheral blood monocytes and enhances bacterial survival at a low pH, such as that found on normal skin, in intracellular compartments of phagocytic cells (236), and in abscess cavities. In addition, arginine deiminase may deplete l-arginine, which is a substrate for nitric oxide production; nitric oxide is a toxic metabolite generated by human macrophages and other leukocytes to control microbial pathogens. While arcA is found in nearly all staphylococcal strains, the arcA gene contained in ACME has a distinctive nucleotide sequence. The consequences of carriage of the distinct arcA gene are unknown (236). Other open reading frames within ACME may also be relevant virulence factors; further research is necessary to investigate this possibility.
Of 214 S. aureus isolates from a reference collection, arcA was identified only in USA300 MRSA backgrounds containing SCCmec type IVa. It was not found in other successful CA-MRSA background types (e.g., USA400 or ST80 strains). Thus, like PVL, ACME is not necessary for the broad dissemination of an MRSA clone (326). Diep et al. found that all but 1 of 1,248 USA300 isolates tested from a reference collection carried the ACME element (233), although Montgomery et al. found that 8/90 (9%) tested USA300 isolates lacked arcA, a proxy marker for the ACME element (623). In an assay for competitive fitness, USA300 had superior fitness, as measured by the differential bacterial burden in tissues at autopsy compared with an isogenic mutant that had ACME and the SCCmec element deleted. Those authors concluded that the absence of the ACME element significantly decreased the in vivo fitness of USA300; ACME may therefore be central to the pathogenesis of USA300 infections (233). In contrast, Montgomery et al. found no difference between the virulence of USA300 strains and that of an isogenic ACME knockout in a rat model of necrotizing pneumonia or skin infection; furthermore, no difference was found in the expressions of global regulators of virulence determinants in these two strains (623).
The α-type PSMs.
The α-type phenol-soluble modulins (PSMs) and β-type PSMs, two groups of cytolytic peptides that are produced in higher concentrations in vitro by two U.S. CA-MRSA clones, USA400 (MW2) and USA300 (LAC), than by HA-MRSA strains tested have recently received attention as candidate virulence factors. PSMs are also found in coagulase-negative staphylococcus species (980). Delta-toxin is produced by S. aureus and is similar in structure to α-type PSMs. Isogenic clones of USA400 MW2 and USA300 LAC were created, in which the genetic loci PSMα and PSMβ were deleted and the start codon of the gene encoding delta-toxin (hld) was altered, abolishing the production of PSMs and delta-toxin in the mutants. These two deletion mutants were less lethal in a mouse model of bacteremia and less likely to cause skin lesions in infected mice than the corresponding wild-type strains. In vitro studies demonstrated that synthetic PSM-activated human neutrophils and that certain PSMs, especially PSMα3, caused neutrophil lysis in vitro. The in vitro lytic activities of the MW2 and LAC strains were increased compared with those of the corresponding mutant strains. This activity was restored by complementation using a plasmid expressing all α-type PSMs and partially complemented by a plasmid expressing PSMα3 alone. Strains lacking delta-toxin did not demonstrate any change in their abilities to lyse human neutrophils. These experiments suggested that PSMs may be in part responsible for the virulence of successful CA-MRSA clones (231, 980). Hongo et al. demonstrated that PSMα3, while it did not lyse human neutrophils at low concentrations, may be a cofactor that enhances the ability of PVL to lyse human neutrophils (402).
Protein A.
The species signature gene spa encodes protein A, which is expressed on the surface of nearly all S. aureus strains. Protein A contributes to the prevention of opsonization and subsequent phagocytosis by ineffectually binding the Fc region of IgG (295, 922). It also initiates a proinflammatory cascade in the airway by activating tumor necrosis factor receptor 1 (TNFR1) (328) and B cells in concert with other ligands (55). Protein A was also shown to enhance the activity of alpha-toxin in a murine model of skin infection (712). MRSA strains with certain spa types have a decreased ability to invade human cells in vitro (995), suggesting an association with certain spa types and virulence. This observation has not been confirmed by experiments using isogenic bacterial mutants with different spa types, and further research is needed to assess the importance of protein A as a virulence factor in CA-MRSA strains.
Other candidate virulence factors and mechanisms.
It has been proposed that MRSA strains lacking the pls gene, coding for the surface protein Pls, which decreases adhesion to human cell ligands and invasiveness, have decreased pathogenicity (995), but further research is needed to determine if this effect has clinical importance.
One group demonstrated with a mouse abscess model that the efflux pump norB, responsible for resistance to fluoroquinolones and other antimicrobial compounds, may provide a fitness advantage to wild-type MW2 (USA400) strains (239).
Recently, Montgomery et al. demonstrated increased levels of transcription of the PVL and alpha-toxin (hla) genes and of the global regulators agr, sarA, and saeRS in three USA300 MRSA strains compared with two USA400 strains. agr, sarA, and saeRS regulate the increased expression of many toxin and other proteins associated with virulence (624). This increased transcription was correlated with increased virulence in several rodent models of CA-MRSA pneumonia. These observations suggested that a difference in the quantitative expression of key virulence genes rather than their presence alone might account for the increased virulence or fitness of USA300. In further support of this, in a global assessment of exoprotein abundance, Burlak et al. found that 11 virulence factors, including Cna and Hla, had increased production in a USA300 (LAC) strain compared with a USA400 (MW2) strain. These virulence factors included proteases, molecules involved in adhesion to host cells, and toxins; the PVL protein was not detected in the supernatant from either strain (110).
NON-β-LACTAM ANTIBIOTIC SUSCEPTIBILITY AND CA-MRSA
CA-MRSA isolates have typically been susceptible to most non-β-lactam antimicrobial drugs (383, 654), including several orally available agents. This enables clinicians to have a number of options when selecting empiric treatments of putative CA-MRSA infections. CA-MRSA isolates are usually susceptible to clindamycin in the United States (300, 301), gentamicin in Australia (672), and ciprofloxacin in England (262, 375, 694). Indeed, susceptibility to more than two non-β-lactam antimicrobials (642) has been used as a proxy defining criterion to identify CA-MRSA. The treatment of CA-MRSA infections is discussed below; here we focus on the generally broad susceptibility and trends for increasing resistance among CA-MRSA strains (235, 779).
Mupirocin Resistance
Mupirocin, a topical antimicrobial, is often used as an intranasal agent in MRSA decolonization protocols and for the topical therapy of impetigo. It acts by binding bacterial isoleucyl tRNA synthetase, thereby inhibiting protein synthesis. Low-level mupirocin resistance results from point mutations in the ileS gene, while high-level resistance is associated with the presence of the mupA gene, which is carried on a plasmid and codes for a mutant isoleucyl tRNA synthetase that does not bind mupirocin (398).
Few centers routinely test MRSA isolates for susceptibility to mupirocin, but there is evidence that when it is used in decolonization regimens, resistance emerges rapidly (713). Among 14,840 patients admitted to a medical center in Chicago, 591 patients had a positive PCR assay and a positive culture for nasal MRSA. Of the 591 MRSA isolates, 17 (2.9%) had low-level mupirocin resistance, and 3 (0.5%) had high-level resistance (34), although the use of mupirocin at the center was not quantified. Similarly, among 4,980 MRSA isolates from 32 Canadian hospitals, high-level mupirocin resistance increased from 1.6% in 1995 to 1999 to 7.0% in 2000 to 2004. Mupirocin resistance mediated by the mupA gene was more common for isolates obtained from aboriginal populations than from others, from those with asymptomatic MRSA colonization than from those with a MRSA infection, and from those with CA-MRSA infection (as defined by a lack of risk factors for exposure to health care facilities) than from those with HA-MRSA infection (838); the use of mupirocin was not quantified for these hospitals.
In other centers, mupirocin use was quantified and correlated with increasing rates of resistance among MRSA isolates. In a study of MRSA nasal colonization among ICU patients in St. Louis in 2002 to 2004, where mupirocin was routinely administered to carriers for a mean of 6.08 days/1,000 patient-days, resistance was common: 13.2% of 302 isolates were resistant to mupirocin (MIC ≥ 8). Of these, 4.6% had low-level resistance and 8.6% had high-level resistance (449). At three hospitals in suburban Chicago, a mupirocin-based decolonization protocol was used routinely for 3 years for any patient found by active screening at admission to have nasal colonization with MRSA. In August 2005 to 2008, 4,934 MRSA isolates were obtained. Mupirocin resistance was detected for 4.1%, 5.5%, and 7.2% of the isolates during the first, second, and third years of the program, respectively (717).
In contrast, not all centers have noted frequent mupirocin resistance among MRSA isolates. Among 409 clinical MRSA isolates obtained in 2006 to 2007 at the Madigan Army Medical Center in Fort Lewis, WA, only 1.7% had high-level resistance to mupirocin (MIC > 1,024 μg/ml) and 2.4% had intermediate resistance (MIC, 1 to 32 μg/ml) by Etest. Those authors found no trend toward an increased prevalence of resistance over time despite the extensive usage of mupirocin-based topical creams in the Western Regional Command (96,968 g prescribed between March 2006 and February 2007) (721). Further studies are necessary to define the impact of mupirocin use on the development of resistance.
Clindamycin Resistance
Increasing non-β-lactam antimicrobial resistance among CA-MRSA clones, particularly to clindamycin, may complicate efforts to manage infections in the community. A study in Boston and San Francisco showed the emergence of a multidrug-resistant strain of MRSA carrying plasmid pUSA03, predominantly among isolates from men who have sex with men (MSM) in the community. This plasmid codes for resistance to clindamycin and mupirocin (235) and may be responsible for a high rate of failure in mupirocin decolonization attempts among MSM patients in New York City (343). At a health center in Boston serving a patient population in which >50% of the patients reported being MSM, among 123 first-patient MRSA isolates obtained in 2004 to 2005, 83% belonged to one of two subclones of USA300. Among the 102 isolates that had antimicrobial susceptibility testing, 98 (96%) were resistant to erythromycin, 87 (85%) were resistant to levofloxacin, 58 (57%) were resistant to clindamycin, and 31 (30%) were resistant to tetracycline. Twelve of the MDR isolates were tested, and all carried the mupA gene. All were susceptible to doxycycline and TMP-SMX (361). Similarly, in a study of CA-MRSA SSTIs among MSM patients in New York, only 37% were susceptible to clindamycin and 9% were susceptible to ciprofloxacin (825). Of 21 MRSA isolates obtained from the axillae or nares of otherwise healthy HIV-infected patients in New York City in 2005 to 2006, 8/21 (38%) carried the mupA gene, and 7/8 of these strains had constitutive resistance to clindamycin; all 8 isolates were USA300 strains. Ciprofloxacin resistance was found for 14/15 USA300 colonization isolates in the study (827).
Reduced Susceptibility to Vancomycin and Daptomycin
Rare cases of resistance of USA300 strains to intravenous non-β-lactam antibiotics have been reported. For example, a USA300 MRSA isolate that had low-level resistance to vancomycin and reduced susceptibility to daptomycin was isolated from a patient in San Francisco who died of MRSA lumbar discitis (344).
MOLECULAR EPIDEMIOLOGY OF CA-MRSA
USA300 Strains
In the 1990s, several S. aureus genetic backgrounds were responsible for initiating the CA-MRSA epidemic, but by the first years of the 21st century (309, 888), one well-characterized genetic background, USA300, emerged as the most prevalent strain in the contiguous 48 states in the United States (403, 475, 543, 702, 893, 895). Elsewhere in the world, including rural southwestern Alaska (218), other PVL+ genetic MRSA backgrounds have predominated (Table 5). USA300 has been isolated from patients on all continents except Antarctica, but its role as the dominant genetic background of CA-MRSA has not been duplicated outside the United States.
TABLE 5.
PVL+ strains of MRSA reported to cause infections among healthy populations in different regions of the world
| MLST | Predominant SCCmec type(s) | spa type(s) | Strain(s) | Regions where strain is common | References |
|---|---|---|---|---|---|
| ST1 | IV | t125, t127,t128, t175, t558, t1272, t1274 | USA400, CMRSA-7 | United States, Canada, Europe, Australia | 133, 184, 203, 218, 309, 509, 640, 913, 924, 956, 1017, 1027 |
| ST8 | IV | t008 | USA300, CMRSA-10, WA-MRSA-12 | United States, Canada, Europe | 171, 208, 216, 234, 309, 385, 403, 419, 443, 475, 481, 509, 543, 628, 702, 845, 875, 893, 895, 924 |
| ST30 | IV | t012, t018, t019, t021, t030, t043, t318 | SWP clone, WA MRSA, USA1100 | Australia, United States, Japan, Latin America, Turkey, Egypt, Middle East, Europe | 58, 92, 184, 252, 264, 276, 294, 352, 376, 429, 472, 509, 604, 644, 670, 682, 757, 778, 886, 905, 913, 920, 924 |
| ST59 | IV, V, VT | t216, t437 | USA1000 | Australia, Europe, Taiwan, United States | 68, 90, 92, 160, 184, 294, 411, 418, 509, 595, 694, 879, 913, 975, 977 |
| ST80 | IV | t042, t044, t070, t131, t237, t376, t455 | European clone | Australia, Europe, Kuwait, Algeria, Tunisia, Egypt, Malaysia | 56, 57, 184, 213, 264, 274, 299, 379, 490, 509, 510, 548, 555, 673, 693, 694, 814, 823, 913, 920, 924, 962 |
| ST93 | IV | t202 | Queensland clone | Australia, England | 184, 257, 258, 352, 641, 643, 670, 763, 913 |
Relevant characteristics of USA300 include the carriage of SCCmec type IV, PVL genes, and, in most strains, the ACME element. USA300 is classified as ST8 by MLST and is usually classified as t008 by spa typing. It is frequently susceptible to many non-β-lactam antimicrobials. USA300 is not the sole ST8, spa type t008, and SCCmec type IV-bearing MRSA strain (213), but other genetic backgrounds have not been as widely distributed.
USA300 became the dominant CA-MRSA strains in the United States in a remarkably brief period of time. Its predominance has been documented in a number of disparate settings. For example, in a population-based study of MRSA infections in San Francisco in 2004 to 2005, 78.5% of community-onset MRSA infections were caused by USA300 clones (543). At the Baltimore, MD, Veterans Affairs Medical Center in 2001 to 2005, the incidence of MRSA infections increased among patients with no history of MRSA colonization or infection from 0.2 (6 infections) to 5.9 (180 infections) per 1,000 outpatient visits; USA300 caused no MRSA SSTIs in 2000 but caused 84% of MRSA SSTIs in 2005. In this 5-year period the proportion of SSTI cultures that yielded MRSA increased from 4% to 42%. This increase was accompanied by an increase in the number of visits for SSTIs from 20 to 61 per 1,000 outpatient visits, an increase that was accounted for by the rising number of USA300 MRSA infections (443). USA300 was responsible for an estimated 29% of invasive MRSA disease in the United States in 2005 (481) and for 31.4% in 2005 to 2006 (537). In EDs in 11 U.S. cities in August 2004, USA300 was identified among 97% of MRSA isolates obtained from SSTI cultures (628). In Chicago, ST8 strains, corresponding to USA300, made up 55.4% of MRSA strains from individual inpatients and outpatients in 2004 to 2005 at a large tertiary care medical center and 82.8% of all MRSA isolates obtained from patients seen in the ED but not admitted (216). USA300 caused 35% (74/210) of MRSA bloodstream infections at the Henry Ford Hospital in Detroit, MI, in July 2005 to February 2007; 88% (65/74) had onset in the community (171). Among 53 patients admitted to Grady Memorial Hospital in Atlanta, GA, in 2003 and found to be nasally colonized with MRSA, a population presumably having a great chance of health care exposure, 16 (30%) carried USA300 strains (385).
In addition to infection-causing strains, USA300 has become increasingly common as a cause of asymptomatic colonization in the general population. In a nationally representative study of the noninstitutionalized U.S. population, the percentage of MRSA isolates recovered from nasal colonization that were USA300 strains doubled from 8.0% in 2001 to 2002 to 17.2% in 2003 to 2004 (P = 0.03) (895).
USA300 strains have been isolated disproportionately from certain high-risk groups in the United States. For example, of MRSA strains obtained in an international study of therapy of endocarditis, all 23 patients with USA300 strains were from North America; these patients were younger, more likely to be black, more likely to be intravenous drug users (IVDUs), and more likely to have right-sided endocarditis than were the 65 patients with non-USA300 strains (500).
USA300 emerged later in Canada than in the United States; limited evidence suggests that it may be following the same pattern of rapid dissemination in similar populations. USA300 was first reported by a large surveillance program in Canada in 2004, when it caused an outbreak of SSTIs in Alberta (170, 318). It was also isolated in 2004 to 2005 from SSTIs in MSM patients in Toronto (875) and from the nares of an Ontario schoolteacher in 2006 (363). First noted as a cause of bacteremia in the Calgary Health Region in 2004, USA300 quickly became the most common strain causing MRSA bacteremia, accounting for 26 of 88 (30%) reported cases in 2004 to 2006 (512). In 2005, 271 people in Calgary participating in a needle exchange program, a jail, a homeless shelter, or a substance abuse program were tested for colonization or infection with MRSA; 5.5% carried USA300 (319). USA300 was found to be the most common cause of skin infections in an emergency department in Vancouver, Canada, in 2003 to 2005 (14), although it was isolated only once (among 36 MRSA infections) among patients in the intensive care unit of a hospital in Edmonton, Alberta, in 1997 to 2005 (845).
USA300 has more recently been identified in Western Europe (40, 283, 299, 381, 419, 469, 508, 579, 786, 900), Japan (828), and Australia, where it has been called WA-MRSA-12 (184, 340, 620), but it remains an uncommon cause of SSTIs in the community in those regions.
The origin of USA300 has been uncertain, but O'Hara et al. analyzed the lukSF-PV DNA sequences encoding the PVL toxin in a sample of international clinical MRSA isolates and hypothesized that USA300 emerged after a CC8 MRSA strain acquired the PVL genes from a preexisting USA400 strain (685). If this is true, and if USA300, endowed with the PVL genes, became more fit than USA400, the acquisition of PVL might account for USA300 becoming the predominant MRSA genetic background circulating since 2001 (156, 309). As noted above, genes carried by the ACME element, specifically associated with USA300, may be virulence factors (233, 623). However, more research is needed to assess their importance. Particularly needed is an evaluation of the many open reading frames in the element that have not been adequately examined.
A prototype USA300 clone, USA300-0114, defined by the CDC by a PFGE pattern (595), has been sequenced (236), as has another USA300 clone isolated from Houston, TX. The two USA300 strains showed little difference in gene content, but they did have many polymorphisms in shared genes (386). Kennedy et al. sequenced the genomes of 10 USA300 patient isolates from diverse geographical locations in the United States to assess genetic variation. Those authors concluded from the relatively few single-nucleotide polymorphisms in the genomes that there has been a recent clonal diversification of a USA300 progenitor strain rather than an evolutionary convergence. Two of the 10 isolates, while genotypically closely related to the others, were associated with decreased virulence in a mouse sepsis model. These two isolates showed a decreased in vitro secretion of LukF-PV and the absence of alpha-hemolysin. One of these two isolates had a missense mutation in the agrA gene (a regulator of many secreted exoproteins) that may have been the critical reason for its decreased virulence, but the other isolate did not share this missense mutation (468).
USA300 may also be a common pulsotype among clinical MSSA isolates, suggesting that the genetic background, rather than the carriage of the SCCmec element, may underlie the fitness of USA300 (691). USA300 was the most common genotype among S. aureus strains causing nasal colonization among New York State Prison detainees in 2005 to 2006 and accounted for 16% (20/124) of S. aureus isolates. Seventy percent of the USA300 isolates were MSSA. In the same prison system, USA300 strains accounted for 48% (29/60) of S. aureus isolates from infections (560). Of invasive MSSA infections in children at a Houston, TX, hospital, 60% (77/128) were from patients with osteomyelitis; 14% (2/14) of invasive infections were caused by USA300 in 2001, and the percentage increased to 35% (11/31) in 2006. Of the 35 PVL+ MSSA isolates in that study, 25 (71%) were USA300 strains. This suggests that USA300 MSSA may also be increasingly common as a cause of invasive infections in the community (593).
Other Prominent CA-MRSA Genetic Backgrounds
Since the 1990s, MRSA strains with different genetic backgrounds carrying SCCmec type IV or V elements have been identified as etiological agents of infections among previously healthy people in different parts of the world (913, 933). These clones, like USA300, tend to be susceptible to most non-β-lactam antimicrobial drugs, tend to be PVL+, and have been associated with distinctive SSTIs resembling spider bites and necrotizing pneumonia.
It is likely that few countries have experienced epidemic community MRSA disease or frequent asymptomatic MRSA colonization among the general population as described for the United States. Indeed, reported rates of asymptomatic MRSA colonization in the developing world, Turkey, and northern Europe suggest that rates are low. For example, in 2005 the prevalence of nasal colonization with MRSA was 0.2% among hospitalized patients in Mali (785) and was similarly low in Malaysia (169). In Brazil in 2000 to 2001 the prevalence of MRSA nasopharyngeal colonization in children younger than 5 years of age with respiratory tract infections or meningitis within 6 h of hospitalization was 1.02% (7/686). All seven MRSA isolates obtained carried SCCmec type III (502), typical of HA-MRSA strains. In Switzerland in 2006, only 1 of 1,337 pediatric patients admitted to a group of hospitals had MRSA colonization (380). In England, colonization with MRSA in the community is rare, despite an estimated 3-fold increase in the rate of hospitalizations for abscesses, carbuncles, furuncles, and cellulitis between 1989 to 1990 and 2003 to 2004 and a greater-than-5-fold increase in the rate staphylococcal pneumonia (374). Similarly, in Ankara, Turkey, 4,050 schoolchildren were assayed for nasal colonization with MRSA in 2007: 24.7% carried S. aureus, but only 0.07% (3 children) carried MRSA (472).
The principal background genotypes of CA-MRSA strains other than USA300 are as follows.
ST1.
USA400 is the pulsotype of the strain of ST1 CA-MRSA that predominated among CA-MRSA clones in the United States when first recognized in the late 1990s. The genome of a prototype strain, MW2, has been sequenced (33). Curiously, there were scarcely any transposons or insertion sequence (IS) elements in the sequence, and many toxins were identified that were absent from other S. aureus genomic sequences, as were multiple superantigen genes. Moreover, the sequence was highly similar to that of MSSA476, also a cause of severe invasive disease in an immunocompetent child (399). MW2 was the CA-MRSA strain responsible for a fatal infection in a child from North Dakota in 1999 (133). USA400 was also identified in the community in 1999 to 2002 in Saskatchewan, Canada (640), and in 1995 to 2000 in Manitoba, Canada (1017). USA400 remained the predominant genotypic background of CA-MRSA strains in rural southwestern Alaska in 2004 to 2006 (218). Despite the ability of USA400 to cause severe, invasive disease, soon after 2000 it was replaced by USA300 as the predominant CA-MRSA strain in most regions of the United States (309) and later in parts of Canada (1027).
An ST1 strain carrying SCCmec type IV that has been usually susceptible to most non-β-lactam antimicrobial drugs and has been found most commonly to cause SSTIs has been described. This strain lacked PVL genes and circulates in the community in Australia, particularly in Western and South Australia (184, 352, 642), and England (693, 694); in Australia, it is designated WA-MRSA-1.
ST80.
CA-MRSA infections have remained infrequent in Western Europe relative to the United States. In Europe, ST80 is likely the most common PVL+, SCCmec type IV-bearing MRSA strain causing such infections. PVL+ ST80 MRSA strains bearing SCCmec type IV have been reported by many Western European nations as an increasingly common cause of skin infections in the community (913) in Austria (490), Norway (379), Denmark (509, 510), Sweden (274), England (693, 694), Switzerland (299), and Greece (673, 814). ST80 was a rare cause of sporadic invasive infections in France in 2006 to 2007 and accounted for 3.6% of 111 MRSA isolates collected during a national survey of patients with invasive disease (213). It is not known why ST80 strains have not spread to North America or why USA300 strains have not spread widely to Western Europe.
Less commonly, ST80 MRSA strains have also been reported for other parts of the world. In a nationwide surveillance of MRSA isolates from outpatients in Australia in 2004 to 2006, 2/462 (0.43%) isolates were ST80 (184). SCCmec type IV-bearing, PVL+, ST80 strains were also found to be the etiology of 10 CA-MRSA infections in Kuwait and comprised 39% of MRSA isolates collected by a reference laboratory from five hospitals in that country in 2001 to 2003. These ST80 isolates were isolated from inpatients and outpatients from skin, wounds, or groin (920). In Tunisia in 2003 to 2005, ST80 was the dominant genetic background identified among CA-MRSA isolates (i.e., isolated either from outpatients or from inpatients within 48 h of hospital admission) (57); ST80 was also obtained from CA-MRSA (CDC criteria) infections in Egypt (264). In Malaysia in late 2005, a person was identified with MRSA nasal colonization by a PVL+, ST80 strain that carried SCCmec type IV (823; V. Neela, personal communication).
ST30.
ST30 corresponds to phage type 80/81 strains of S. aureus that were virulent nosocomial pathogens in the United States during the 1950s and 1960s. These strains were MSSA strains and often carried the PVL genes (770). An ST30 MRSA clone, known as the Southwest Pacific (SWP) clone, is likely a direct descendant of the older 80/81 clones and has long been a common human pathogen in Australia (184, 352, 770, 905). Since the mid-1990s, MRSA ST30 clones with different pulsotypes and genetic characteristics have been reported from many parts of the world, including the United States, Japan, Latin America, Turkey, the Middle East, Egypt, and many countries in Western Europe (58, 264, 429, 472, 604, 670, 757, 778, 913, 920). ST30 isolates reported from many regions, including PFGE type USA1100 in the United States, carry the genetic determinants of PVL and the SCCmec type IV element (58), but these clones have many spa types, suggesting continued evolution (92, 252, 276, 294, 429, 682, 886). Such CA-MRSA-type ST30 MRSA strains have been reported more commonly than USA300 in certain countries, notably in Australia in 2004 to 2006 (184); it is not known why they persist as causes of community-associated infection in some regions and not in others.
ST59.
ST59 isolates are prevalent in Taiwan. Strains that are PVL+ have diverse spa types and several SCCmec types. PVL+ ST59 isolates have also been recovered from patients in Australia, Taiwan, the Netherlands, Denmark, England, the United States (92, 160, 184, 294, 418, 509, 694, 913, 977), and elsewhere. In Taiwan, ST59 clones with a distinctive SCCmec DNA sequence, type VT, and a multidrug-resistant phenotype are common (880). For example, PVL+ ST59 isolates bearing SCCmec type VT accounted for 25% (53/212) of MRSA strains colonizing healthy children in 2005 to 2006 at medical centers in three Taiwanese cities. However, ST59 strains that were PVL negative and carried SCCmec type IV accounted for 59% (129/212) of MRSA strains from tested children (411). Among 3,098 adult workers in Taiwan attending mandatory health screening in 2007, 3.8% (119/3,098) had nasal MRSA carriage. Of 119 MRSA isolates, 100 were ST59. Among these, 65/100 (65%) carried SCCmec type IV, of which 10/65 (15%) were PVL+; 35/100 (35%) carried SCCmec type V, of which 35/35 (100%) were PVL+ (977). In Taiwan, PVL+ ST59 strains tend to be resistant to more non-β-lactam antimicrobials than strains sharing this ST background in other parts of the world (879). In a study at the 2,500-bed National Taiwan University Hospital in Taipei in 2001 to 2006, 92% of the 30 available CA-MRSA isolates (by CDC criteria) from patients with bacteremia were ST59 strains (975). ST59 strains are currently rare in the United States, although an ST59 clone called USA1000 in the CDC classification has been identified sporadically (68, 595); the reasons for the high prevalence of ST59 in Taiwan, in contrast to its rarity in the United States, are not understood.
ST93.
The ST93 Queensland MRSA strain was first identified in 2000 in Queensland and New South Wales, Australia. It spread rapidly to become the predominant PVL+ MRSA clone isolated from infections in those regions. For example, in 2004 to 2005, in a national surveillance program in Australia, 87/462 (18.8%) MRSA isolates obtained from outpatients were ST93 strains, and all were PVL+. Among PVL+ MRSA isolates, 87/136 (63.9%) were ST93 strains, and they were isolated in all regions of the country (184). Despite the high prevalence of this strain in Australia (670), it has rarely been identified on other continents (258). It has been associated with severe infections, including necrotizing pneumonia (763), as well as SSTIs (352). A study of nasal colonization among healthy Queensland residents in 2005 to 2006 demonstrated a 0.7% (5/699) MRSA carriage rate; 20% (1/5) of the MRSA isolates were ST93 strains (643). As with ST59 in Taiwan, ST80 in Western Europe, and USA300 in North America, the proclivity of ST93 strains to colonize and infect Australians from certain regions with limited spread elsewhere (258) is not understood.
STAPHYLOCOCCUS AUREUS AS A COMMENSAL ORGANISM: ROLE OF ASYMPTOMATIC COLONIZATION
The epidemiology of CA-MRSA strains remains incompletely studied, but it must be considered in the context of what is known about asymptomatic colonization dynamics of other S. aureus strains. Most available information predates the emergence of CA-MRSA, and much of it is from Europe, where CA-MRSA infections remain relatively uncommon. Thus, the applicability of knowledge gained in that setting to the CA-MRSA strains epidemic in the United States is uncertain.
The asymptomatic carriage of S. aureus by humans is the primary natural reservoir, although domestic animals, livestock, and fomites may serve as adjunctive reservoirs. The anterior nasal mucosa has traditionally been thought to be the most frequent site for the detection of colonization of healthy carriers with S. aureus (91, 482, 773, 1002). The site sampled in the nasal mucosa may affect the demonstrable prevalence of colonization; for example, in one study, 22% of 412 patients carried S. aureus in the cavitas nasi but not in the more distal vestibulum nasi (325). Also, certain rapid PCR-based laboratory detection systems sometimes used in studies lack the sensitivity of culture and lack adequate sensitivity to detect small numbers of organisms (929).
A widely prevalent view was promulgated by Kluytmans et al., who distinguished three patterns of asymptomatic S. aureus carriage in the general population. Those authors estimated that 20% are persistent carriers, 60% are intermittent carriers, and 20% are noncarriers who rarely harbor the bacterium (482). It is not known if CA-MRSA strains colonize people in this fashion.
Recent studies have suggested that other anatomical sites may be asymptomatically colonized with S. aureus in the absence of nasal colonization. For example, among patients, health care workers, and blood donors in Basel, Switzerland, in 2000 to 2005, S. aureus carriage was underestimated by 25.7% when nasal cultures were not accompanied by throat cultures (600). In a study of 3,464 people in Switzerland in 2000 to 2006, including inpatients, health care workers, healthy blood donors, and dental patients, throat carriage of S. aureus with no concomitant carriage in the nares was found for 428 subjects (12.4%). This was associated with an age of <30 years (OR, 1.66; P < 0.001) and a lack of exposure to the health care setting (OR, 0.67; P = 0.001) (601). S. aureus colonization was found in the throat among orthopedic inpatients and staff more commonly than was colonization of the anterior nares (668). Among 89 tested health care workers at a hospital in Singapore, 18 (20%) carried MRSA in the throat, in the nares, or in both. Two (11%) were carriers in the throat and not the nose (150).
Similarly, for MRSA colonization among European inpatients, assessments of nasal carriage may not be adequate to test for asymptomatic carriage. At an English hospital that practiced routine MRSA screening at multiple body sites in 2008, MRSA colonization was identified slightly more often in the throat (72/635; 11.3%) than in the nose (59/635; 9.3%) or perineum (55/635; 8.7%); importantly, 23/72 (32%) patients with positive throat swabs did not have an isolate from another body site (71). Although these findings were not supported by a study of 150 adult ICU patients in Switzerland in 2005 where throat culture uniquely identified only 1 of 13 MRSA-colonized patients (368), the preponderance of evidence suggests that the human oropharynx may be an important reservoir for MRSA colonization. The same may be true for CA-MRSA strains in Europe or the United States, but data are lacking.
In a study of SSTI patients in Los Angeles, CA, 37% of 65 CA-MRSA patients (CDC criteria) were colonized with MRSA in at least one of four tested anatomical sites: 25% were colonized in the nares, 6% were colonized in the axilla, 11% were colonized in the inguinal region, and 13% were colonized in the rectum. Nonnasal colonization was identified for 25% of the patients, and 96% of colonized patients would have been identified by testing of nasal and inguinal swabs. In contrast to CA-MRSA, nonnasal S. aureus colonization was rare among CA-MSSA, HA-MSSA, and HA-MRSA patients (1018).
The asymptomatic carriage of S. aureus can be dynamic. For example, in 2001 to 2003 at an Australian hospital, half of 224 patients found to be colonized with MRSA carried more than one strain, and only 15.3% of colonized patients had persistent colonization at the same anatomical sites (535). Evidence from studies prior to the emergence of MRSA in the health care setting suggested that an individual with persistent nasal carriage of S. aureus is generally protected against the acquisition of new S. aureus strains. Intermittent S. aureus carriers, in contrast, may be at risk of acquiring MRSA colonization (482, 674), although persistence and strain variability of S. aureus carriage have not been well studied in the CA-MRSA era.
The reported duration of asymptomatic carriage of S. aureus has varied. In one study the half-life of MRSA nasal carriage was 40 months (800), and in another, nasal carriage of CA-MRSA isolates could be demonstrated for 2 years or longer (907). In a Swiss hospital, even in the setting of a study of routinely attempted decolonization of MRSA carriers, the median time to clearance was 226 days, and the maximum was 3.3 years. Risk factors for a longer duration of carriage were antibiotic use, the presence of an SSTI, the presence of an indwelling device, receipt of immunosuppressive therapy, and hemodialysis (582). At three suburban Chicago hospitals, hospitalized patients were routinely screened for nasal colonization with MRSA. From these data and chart records of any history of MRSA infection or previous MRSA colonization, it was estimated that 48.8% of patients (95% CI, 45.8% to 51.7%) continued to have MRSA carriage after 1 year and that 21.2% (95% CI, 13.1% to 31.4%) continued to have MRSA carriage after 4 years (769).
MRSA colonization of the nares is believed to be a risk factor for a clinically apparent infection with MRSA (191, 413, 561, 637), although the magnitude of the risk is not known. Ellis et al. demonstrated that 24 of 812 (3%) U.S. soldiers tested at a Texas Army base carried MRSA in the nares, and 9 of the 24 soldiers (38%) developed an SSTI in the course of 10 weeks, while only 8/229 (3%) soldiers carrying an MSSA strain developed an SSTI in the same period (259). Among 1,195 pediatric patients presenting for an outpatient physician's office visit in St. Louis tested for S. aureus nasal colonization, an SSTI was self-reported for 31.8% of those colonized with MRSA, 9.9% of those colonized with MSSA, and 8.9% of those with no S. aureus colonization during a 1-year follow-up. For all three groups combined, SSTI in the child during follow-up was associated with a history of SSTI in the child during the year prior to initial enrollment and also with an SSTI in a household member during the year of follow-up (307).
CA-MRSA infections often occur in people lacking simultaneous nasal MRSA carriage (466, 760). Among 64 pediatric patients with MRSA SSTIs at a Baltimore medical center, only 20 (31%) had MRSA nasal carriage, and only 23/39 (59%) patients with S. aureus recovered from an SSTI and a nasal swab culture had a concordance of both S. aureus PFGE type and susceptibility to methicillin in the two isolates (157).
Most data relating MRSA colonization risk to risk for subsequent disease are derived from settings where HA-MRSA is endemic and may not apply to CA-MRSA strains. For example, MRSA nasal carriage among adult ICU patients (220) and nasal or stool carriage among patients with cirrhosis (121) were a risk factor for subsequent infection.
Evidence that S. aureus nasal carriage predisposes one to infection with the same strain, which may or may not be applicable to CA-MRSA strains, comes from a study in Germany. Among 219 patients with S. aureus bacteremia, 180 (82.2%) had S. aureus in the nares of an identical PFGE type. Moreover, among 14 patients with S. aureus bacteremia, 12 had previous nasal carriage of the same strain as assessed by PFGE (959).
It is believed that hand carriage of MRSA is the major means of nosocomial MRSA transmission, but its role in the transmission of CA-MRSA backgrounds like USA300 and USA400 outside the health care setting has not been defined. Hand carriage of S. aureus was more likely for nurses with irritated skin (511). Furthermore, MRSA in the health care setting can be isolated from skin surfaces, such as the hands, even in the absence of nasal carriage (800), and transient hand carriage has been repeatedly demonstrated among health care workers (183, 592, 885) and may be more common among those wearing rings (910). Several studies from outside the United States have demonstrated the same phenomenon of MRSA transmission from health care workers to patients in the household setting. For example, a French study demonstrated that prior nursing home care was independently associated with infection by prevalent HA-MRSA strains when controlled for prior hospitalization, age of >65 years, and transfer from another institution (529), suggesting transmission from health care workers to patients in their homes. A Brazilian study demonstrated the transmission of MRSA from patients to their home-visiting health care workers (780). These data may not be applicable to an understanding of the transmission of CA-MRSA strains in households; if CA-MRSA is similarly transmitted from person to person by hand carriage, specific hand washing interventions may be appropriate to prevent its spread.
RISK FACTORS AND HIGH-RISK GROUPS FOR CA-MRSA CARRIAGE OR INFECTION IN THE UNITED STATES
Prior to the late 1990s, MRSA infections were confined largely to patients and others who had known exposures to the health care setting, but the epidemic of CA-MRSA infections in the United States has required a redefinition of the risk factors for MRSA disease. CA-MRSA infections have been reported for diverse populations, including adults and children, residents of inner city neighborhoods, Native American (NA) and Pacific Islander populations, incarcerated and military populations, and athletes, who lack risk factors for exposure to the health care setting. Low socioeconomic status may be one common link among many of the identified high-risk groups, although many patients with CA-MRSA infections have no apparent risk factor (596). Environmental, behavioral, or other as-yet-unidentified social risk factors for CA-MRSA colonization await systematic study.
New MRSA risk factors for infection or colonization with MRSA in the community have been identified since 1998. Groups thought to be at high risk for MRSA infection based on anecdotal occurrences are listed in Table 6. Each will be discussed in detail in this section; people in close contact with individuals in these groups may also be at an increased risk. Further research is needed to assess how these risk groups interact and what risk factors or exposure they may have in common.
TABLE 6.
Groups presumed to be at risk for CA-MRSA infections in the United States
| At-risk group |
|---|
| Neonates |
| Children beyond the neonatal period |
| Athletes |
| Household contacts of MRSA SSTI patients |
| Emergency department patients |
| Urban undeserved communities |
| Indigenous populations |
| Detainees in jail or prison |
| Cystic fibrosis patients |
| Military personnel |
| Men who have sex with men |
| HIV patients |
| Veterinarians, livestock handlers, and pet owners |
In addition to the putative high-risk groups for CA-MRSA infection listed in Table 6, there has been evidence of CA-MRSA strain transmission among children in day care centers (4, 822) and outbreaks of MRSA SSTIs within families (193, 237, 271, 272, 350, 381, 395, 533, 967), among children on a camping trip (180), among IVDUs (406), and in individuals exposed to another person with an SSTI by skin-to-skin contact during sexual activity (767). Inhalation drug use has also been shown to be a means of S. aureus transmission (742) and may play a role in CA-MRSA transmission, although this has not been well studied. Recent use of antibiotics has been associated with MRSA colonization (385) and infection (215, 841), but it is not known if this is an independent risk factor for MRSA or an association that may have confounding variables. Patients with atopic dermatitis have long been known to be predisposed to S. aureus and, by extension, MRSA infections and colonization; of 54 children with atopic dermatitis in Philadelphia, PA, in 2004, 80% (43/54) had skin or nare colonization with S. aureus, and 13% (7/54) carried MRSA (872).
While many studies have demonstrated that the prevalence of CA-MRSA infections has increased rapidly among certain populations in the United States, the prevalence of nasal colonization in the general population has increased less rapidly and remains relatively low (188, 385). For example, among 100 healthy students and faculty members at a community college in Hawaii, an area with a high rate of MRSA infection, 3% were colonized with MRSA (632), similar to the rate among 200 health care workers at Johns Hopkins University Hospital in 2004 to 2005, in the midst of epidemic CA-MRSA invasive infections in Baltimore (481), where only 2% were colonized with MRSA (447). In the National Health and Nutrition Survey (NHANES), which is administered to a demographically and geographically representative sample of the noninstitutionalized U.S. population, an estimated 2.3 million Americans carried MRSA in the nares in 2001 to 2002, or 0.8% of the population (346, 492). In 2003 to 2004 the prevalence of MRSA nasal colonization nearly doubled to 1.5% of the population despite an overall decrease in the percentage of the population colonized with any S. aureus strain between 2001 to 2002 and 2003 to 2004 (32.4% versus 28.6%; P < 0.05) (336, 895). The relatively low rates of colonization determined from the NHANES survey and other studies may reflect, in part, geographic variability, a characteristic of the CA-MRSA epidemic to date, or an anatomical site of MRSA carriage other than the nose.
The epidemiology of CA-MRSA is complex, and several studies suggested that there is no obvious boundary dividing the populations at risk for MSSA and MRSA infections in the community, even in high-risk settings such as a jail (215). A study in Los Angeles demonstrated that adult patients with community-onset MRSA could not be distinguished from adult patients with community-onset MSSA infections by characteristics such as age, race, comorbidities, site of infection, antibiotic use, duration of symptoms, bathing habits, level of education, level of crowding at home, substance use, history of homelessness, sexual behavior, or use of a public shower, spa, pool, or gym (608). Thus, it is difficult to determine which patients with suspected S. aureus infections require specific therapy for MRSA.
Neonatal MRSA Infections and Maternal Colonization and Infection
S. aureus, whether susceptible or resistant to methicillin, has long been known to be a cause of epidemic and endemic disease and a cause of infection in the first days of life among newborns in neonatal intensive care units (NICUs) and other settings. Since 2000, there has been an increasing number of reported outbreaks and cases caused by CA-MRSA strains. Several neonatal MRSA outbreaks have been linked to CA-MRSA strains (377, 435, 629), including USA300 (590, 591, 664, 777, 803) and USA400 (93) strains, and have been associated with visiting fathers (15), maternal mastitis (750, 807), expressed breast milk (313), peripartum maternal MRSA infection (255), and health care workers colonized or infected with MRSA, implying a community source (65, 214, 598, 803).
Case reports and case series have described a variety of clinical syndromes and means of introduction of MRSA into neonatal units. In 2001 to 2006 in Texas, neonatal MRSA infection in healthy term and near-term newborns was associated with a history of maternal MRSA skin infection (293). Among 23 MRSA SSTIs in mothers and newborn infants at a Toronto, Canada, hospital in 2004, the source was linked to a health care worker with eczema. The majority of the isolates were USA300 MRSA strains but were resistant to clindamycin and ciprofloxacin (803). Cases of severe, fatal neonatal MRSA pneumonia caused by USA300 have also been reported among neonates (590, 1019), as has necrotizing fasciitis (224).
What is the source of neonatal S. aureus acquisition? Vertical transmission undoubtedly plays a role. There is evidence that vaginal colonization with S. aureus is common (949), but vaginal MRSA colonization is unusual and has rarely been linked to neonatal infection. Neonatal dacrocystitis, lung abscess, and empyema were believed to result from vertical transmission from the mother of a 12-day-old infant in Los Angeles in 2007 (788; T. Ruter, personal communication). However, among 5,732 pregnant women in Alabama in 2003 to 2006, 3.5% were vaginally colonized with MRSA, but no neonatal MRSA infection was documented. Women with MRSA vaginal colonization in that study were more likely to be black, unmarried, and intravenous drug abusers and to have a lower level of education (21). A study in Cleveland, OH, demonstrated a 2.1% prevalence of nasal or vaginal colonization with MRSA among 96 women admitted to a labor and delivery unit; one woman had MRSA colonization at both sites. There was no association between neonatal infection and maternal colonization with S. aureus (54).
In New York City in 2005, 0.47% (14) of 2,963 pregnant women undergoing culture for group B streptococcal vaginal colonization had vaginal MRSA colonization (162). In a case-control study of that same population, women with any S. aureus vaginal colonization (8/65) were more likely than those without S. aureus colonization (1/52) to have a postpartum fever (161), suggesting that S. aureus vaginal colonization may be a risk factor for infection. In another study from New York City, 34/304 (11.2%) women in labor at term had nasal or vaginal colonization with MSSA, and 9/304 (3.0%) had MRSA. Infants born to these women underwent skin and nasal cultures after birth and again at 48 h; 16/252 (6.4%) infants were colonized with MSSA, and 9/252 (3.6%) infants were colonized with MRSA. A total of 5/252 (2.0%) infant-maternal pairs both carried MSSA, and 1/252 (0.4%) pairs both carried MRSA (i.e., the maternal vaginal colonization and the infant 48-h cultures were positive for MRSA). The infant and maternal MRSA strains in the concordant pair were identical by PFGE. At a 4-week follow-up, the single infant colonized at 48 h with MRSA and four infants not colonized with any S. aureus at birth or at 48 h developed S. aureus infections. That study suggested that MRSA colonization of neonates was not common and that most S. aureus infections of newborns were not due to vertical transmission (727).
Colonization in the hospital by means other than vertical transmission likely plays a major role in neonatal colonization. For example, in a hospital in Florida, 288 mother-neonatal pairs were assessed for MRSA colonization by nasal swabs of mothers and neonates, umbilicus cultures of the newborns within 24 h after birth, and a vaginal culture of the mother within 24 h prior to delivery. Only vaginal births were included. Six (2.1%) mothers and two (0.7%) newborns were colonized with MRSA; no mother-infant pair shared the same SCCmec type. Colonization of mothers was associated with black race, antibiotic use during pregnancy or intrapartum, and attendance by another child of the mother at a day care or an after-school program (756).
Outside the United States, MRSA vaginal colonization has been studied less well. In Japan, oropharyngeal MRSA colonization in the first week of life in extremely low-birth weight infants in an intensive care unit in 1997 to 2003 was associated with an increased risk of MRSA sepsis and with MRSA colonization during week 6 of life. Those authors hypothesized that colonization of the oropharynx in the first week of life with other, nonpathogenic bacteria may protect against colonization with MRSA (829). This suggests that colonization of the maternal vagina may not be implicated in neonatal MRSA infections.
In an Israeli NICU in 1993 to 2003, among 43 cases of MRSA bacteremia, 11 were caused by SCCmec type IV-bearing, PVL-negative strains susceptible to all non-β-lactam antimicrobial drugs tested, suggesting a CA-MRSA strain. Infants with infections caused by CA-MRSA strains did not differ in risk factors or outcomes compared to MSSA infections or MDR MRSA infections (494). Those authors concluded that it was difficult to judge the likelihood of MRSA infection in a hospitalized neonate with a suspected S. aureus infection; they recommended in such cases that initial treatment include an agent effective against MRSA (guided by the local S. aureus antibiogram).
Thus, it appears that neonates in both the United States and some foreign hospitals face the risk of early MRSA infections that may be related to vertical transmission but that neonates frequently acquire MRSA from other sources as well. More research is necessary to enact effective measures to curtail potentially fatal MRSA infections among neonates.
Children beyond the Neonatal Period
CA-MRSA in the United States was first identified in the 1990s among children in the Midwest (383). Since that time many areas in the United States have experienced a steep rise in the prevalence of colonization and the incidence of infection with MRSA among healthy children. In contrast, few other countries have experienced a comparable burden of pediatric CA-MRSA infections.
Early reports.
The emergence of community-based MRSA disease in the United States was heralded by the observation that children with MRSA SSTIs and no known exposure to health care environments presented with increasing frequency to the University of Chicago Hospitals between 1988 to 1989 and 1993 to 1995 (383). A follow-up study in 1998 to 1999 demonstrated a continued high rate of hospitalization for CA-MRSA disease at that institution (423). Those same investigators demonstrated asymptomatic carriage of MRSA in otherwise healthy children in the community in Chicago (422, 871). At the nearby University of Illinois at Chicago, a similar phenomenon was documented during the late 1990s through the surveillance of infections of children caused by MRSA strains susceptible to clindamycin (300, 301, 302). The early CA-MRSA isolates from the University of Illinois and those from the University of Chicago were genotypically similar (2); they were subsequently shown to be predominantly USA400 strains (309). In addition, in 1999, cases of fatal severe sepsis from MRSA were reported among previously healthy children in Chicago and elsewhere in the Midwest (133, 621), also caused by MRSA USA400.
MRSA colonization prevalence in U.S. children is increasing.
Nationally representative data showed that the prevalence of nasal carriage of MRSA in noninstitutionalized children aged 1 to 19 years more than doubled from 0.6% in 2001 to 2002 to 1.3% in 2002 to 2004 (336). However, studies from several cities in the United States have demonstrated an even more rapid rise in the prevalence of asymptomatic MRSA colonization of children. In Nashville, TN, in 2004, 9.2% of children attending two clinics for health maintenance visits were colonized by MRSA (188), an increase of more than 10-fold from 2001, when a similar study showed that 0.8% of children were colonized (655). Among 1,300 children presenting to 11 pediatric practices in St. Louis, MO, in 2005 to 2006, 2.4% had nasal colonization with MRSA. Risk factors for colonization included pet ownership, participation in sports, and fingernail biting. Of the MRSA isolates obtained, 66% carried SCCmec type IV and were therefore considered CA-MRSA strains (7/21 USA300, 3/21 USA800, and 3/21 USA1000 strains); black race and Medicaid enrollment were disproportionally represented among carriers of CA-MRSA compared with HA-MRSA genotypes (308). Within 48 h of admission to a children's hospital in Corpus Christi, TX, in 2005, a convenience sample of 76/350 (22%) pediatric patients had MRSA nasal colonization, one of the highest prevalence rates reported for any U.S. population (12).
Increasing burden of CA-MRSA infections among U.S. children.
Many medical centers in the United States have documented an increasing burden of CA-MRSA infections in children as a percentage of S. aureus infections, an absolute increase, or both (120, 353, 1023). Children in Texas cities experienced CA-MRSA earlier than in many parts of the United States. For example, in a children's hospital in Corpus Christi, 147 MRSA infections were identified in outpatients and inpatients in 1990 to 2000. Among these patients, 60 (47%) had CA-MRSA infections (by the 1988 CDC criteria for nosocomial infections [311]), and in 88% of patients (53/60), no HA-MRSA risk factors (i.e., no chronic disease; no day care attendance; no household contact with a known risk factor; no hospitalization, antibiotic use, or surgery in the previous 6 months; no indwelling catheter; and no history of intravenous drug use) were identified. A rapid rise in the number of cases in each subsequent year was noted: 35 of the 60 (58%) cases occurred in 2000, the final year of the study (284). In follow-up studies examining trends from 1990 to 2004 at the same hospital, it was reported that the number of CA-MRSA infections increased rapidly, from 0 to 9 per year in 1990 to 1999 to 459 per year in 2003 (739) and to 589 per year in 2004 (741).
In a prospective study in 2000 at Texas Children's Hospital in Houston, 44% of 144 community-acquired S. aureus infections were CA-MRSA (i.e., children lacked risk factors for health care exposure). There was a high monthly proportion of CA-MRSA among community-onset S. aureus disease isolates that increased from 60% in August 2001 to 67% in January 2002 (802) and to 76.4% in 2004 (460). At another hospital in Houston, among children hospitalized in 2000 to 2003, CA-MRSA (i.e., isolates from lesions cultured <72 h after hospitalization) accounted for 67% of community-associated S. aureus infections (683).
At a pediatric hospital in Memphis, TN, in 2000 to 2002, 52% of patients with MRSA isolates from clinical infections were CA-MRSA (by CDC criteria). This percentage of MRSA isolates that were from CA-MRSA infections increased from 38% in the first 18 months of the study to 67% in the last 12 months. Fifteen of the 16 CA-MRSA isolates tested shared the USA300 pulsotype (105). Children who presented in 2002 to 2003 to Johns Hopkins University Hospital with a skin infection caused by S. aureus were more likely to have an MRSA infection if they were African American or if they lived in a zip code near the hospital, an area with a high rate of poverty (158). Of S. aureus SSTIs in children at the Johns Hopkins ED in 2003 to 2005, 73% (217/296) were caused by MRSA; 81% were CA-MRSA infections (by the CDC criteria) in 2003, and this percentage increased to 85% in the second year (874).
CA-MRSA pediatric infections outside the United States.
Asymptomatic CA-MRSA colonization has not been reported for children in other countries, with a few exceptions. In Asia, reports that identified isolates that were predominantly ST59 and PVL+ and carried SCCmec type V or VT have come from Taiwan, South Korea, and Japan. A single colonizing MRSA genotype was identified among several schoolchildren in one class in Taiwan (415). In Taiwan in 2004, 9 of 69 (13.2%) kindergarteners in Taipei had nasal MRSA colonization (547; W. T. Lo, personal communication). In 2004 to 2006, 8.1% of 1,615 children <14 years of age in kindergartens or presenting to a physician for a health maintenance visit in Taipei, Taiwan, had MRSA nasal colonization, and 1.5% (25) were colonized by PVL+ strains. Of the PVL+ strains, 92% were resistant to clindamycin, and 68% carried SCCmec type VT (548). In a separate study, 6.7% of 3,046 children in Taiwan attending well-child visits had MRSA nasal colonization in 2005 to 2006 (411), an increase compared with 1.9% (5/262) of schoolchildren in 2001 to 2002 (412). In Seoul, South Korea, at an outpatient clinic at a tertiary care hospital, 6.1% (18/296) of children presenting for care had MRSA nasal colonization in 2005 to 2006; of these, 14/18 isolates were CA-MRSA (by the CDC definition), and 7/14 CA-MRSA isolates belonged to ST72 bearing SCCmec type IVa (484). In Niigata, Japan, in 2006 to 2007, 3/426 (0.7%) children attending outpatient physician's office visits had MRSA nasal carriage; in 2007 to 2008, 5/136 (3.7%) healthy children living with their families in eight prefectures had MRSA nasal carriage. None of the children in that study had been hospitalized in the previous year, and the MRSA isolates had a variety of genetic backgrounds, with none carrying the genes for PVL (697). In Narketpally, Andra Pradesh, India, in 2006, 12/392 (3.1%) children aged 5 to 15 years had nasal carriage of MRSA, but genotyping studies were not conducted (745; K. V. Ramana, personal communication).
MRSA infections have also been reported for children in a few regions of Asia. At a hospital in Taiwan, 210 MRSA isolates were obtained from clinical infections of 173 children in 2004 to 2005. Of the 210 isolates, 56% (102) were CA-MRSA by the CDC case definition; of these, 69% were ST59, 79% were PVL+, 70% carried SCCmec type VT, and 21% carried SCCmec type IV. In contrast, among isolates from health care-associated MRSA infections, only 20% were ST59 and carried the PVL genes, 21% carried SCCmec type VT, and 28% carried type IV (410). MRSA infections in nine children in Vietnam, including one fatal case of severe sepsis, were believed to result from exposure to a community vaccinator who was colonized with an ST59 strain bearing SCCmec type V (887). In Cambodia, 17 children in 2006 to 2007 had CA-MRSA infections by CDC criteria identified by surveillance at a clinical microbiology laboratory at a single children's hospital. The causative strains were ST834 with SCCmec type IV and were PVL negative or ST121 with SCCmec type V and were PVL+ (164). At pediatric hospitals in five Chinese cities, 29 CA-MRSA (by CDC criteria) infections in 2005 to 2006 were reviewed retrospectively. Several MLSTs were represented, including ST59, ST910, ST1, and ST88 (1028).
In Latin America, Europe, and Australia, case series have documented the presence of CA-MRSA in children. In 2002 to 2003, 22/2,345 (0.93%) children attending day care centers in 14 Mexican cities had nasal carriage of MRSA; however, only 10.1% of the children were identified as being S. aureus carriers, a rate lower than that found by most studies (950). In Buenos Aires, Argentina, in 2005, five SSTIs in children without exposure to the health care system were caused by PVL+ MRSA strains carrying SCCmec type IV (903). At a clinic in Athens, Greece, 88 CA-MRSA infections (by CDC criteria) among children younger than 14 years old were recorded in 2003 to 2005; 68% (28/41) of the strains belonged to one PFGE clonotype (similar to the PFGE type of ST80 strains) that was PVL+ and SCCmec type IV. Twenty of the 28 strains (71%) belonging to this clonotype were isolated from patients with SSTIs (673). In New South Wales, Australia, a retrospective review of gentamicin-susceptible MRSA infections in 2001 to 2002 at a children's hospital showed that 87 of 100 MRSA infections were caused by CA-MRSA (i.e., no health care exposure in the previous 12 months and a culture obtained <48 h after admission). Of the 87 infections, 67% caused SSTIs, and the majority were ST30 strains carrying SCCmec type IV (352).
Thus, CA-MRSA infections and colonization of children have been reported outside the United States; as it was in the United States, pediatric infections may be a harbinger of an epidemic to come in the general population of these countries.
Athletes
MRSA infections have been reported for members of athletic teams in a variety of sports and related activities such as dance (83), at levels from high school to professional in a variety of sports (Table 7). The frequency of these reports has suggested that athletes constitute a population at risk for MRSA infections and that athletic facilities constitute a new environment for the transmission of MRSA outside the health care system.
TABLE 7.
Athletic activities in which participants were reported to have MRSA infections
| Sport | Yr | Location | Level of competition | Reference(s) |
|---|---|---|---|---|
| Football | 2002-2003 | California | College | 135, 665 |
| 2000 | Pennsylvania | College | 135 | |
| 2004 | Illinois | High school | 83 | |
| 2007 | New York | High school | 134 | |
| 2006 | West Virginia | College | 356 | |
| Not stated | California | College | 792 | |
| 2006 | Pennsylvania | College | 87 | |
| 2005 | Florida | College | 25 | |
| 2003-2004 | Texas | High school | 44 | |
| 2002-2004 | Texas | College | 174 | |
| 2003 | Connecticut | College | 53 | |
| 2003 | Missouri | Professional | 466 | |
| Badminton | 2006 | Vladivostok, Russia | Unknown | 43 |
| Basketball | Not stated | Virginia | College | 863 |
| 2002-2004 | Texas | College | 174 | |
| Cross-country running | 2003-2004 | Texas | High school | 44 |
| Fencing | 2002-2003 | Colorado | Unknown | 135 |
| Rugby | 1996 | United Kingdom | Unknown | 854 |
| Saturation diving | Unknown | Texas | Unknown | 976 |
| Soccer | 2005-2006 | Netherlands | Unknown | 416 |
| 2004 | Slovenia | Unknown | 639 | |
| Volleyball | 2002-2004 | Texas | College | 174 |
| 2003-2004 | Texas | High school | 44 | |
| Weight lifting | 2002-2004 | Texas | College | 174 |
| Wrestling | 1993-1994 | Vermont | High school | 541 |
| 2003 | Indiana | High school | 135 | |
| 2003-2004 | Texas | High school | 44 |
Causative isolates obtained from athletes have usually shared characteristics with CA-MRSA strains, and USA300 has been identified as a frequent cause (665). Risk factors identified among athletes have included sharing personal items, such as soap, towels (134), razors, athletic training equipment, and clothing, in addition to poor hygiene habits (356, 665). In one case-control investigation of a USA300 SSTI outbreak on a high school football team, higher body mass index was a risk factor for MRSA infection (134). Data from Texas and Nebraska suggest that MRSA infections among high school athletes are very common and increasing in incidence. Among 186 athletic trainers at Texas high schools responding to a survey, 60 (32.3%) reported that they were aware of at least one case of MRSA infection in their athletic department in 2003 to 2004 (44). Among 271 Nebraska high schools surveyed, 4.4% reported having at least one athlete with an MRSA infection in 2006 to 2007, while 14.4% reported at least one infection in 2007 to 2008 (114).
While MRSA SSTIs have afflicted participants in many sports, football teams have been most frequently implicated. An outbreak in a college football team resulted in MRSA SSTIs in 1.8% (2/107) of players in 2002 and 15.8% (17/107) of players in 2003. The rate decreased to 1.0% (1/104) of players in 2004 with the introduction of an educational campaign, hexachlorophene-containing soap, disposable towels, showering before use of the athletic training room, improved decontamination of athletic training and weight room equipment, and increased availability of hand sanitizers (775). Unfortunately, it is not known which of these interventions, if any, contributed to the decreased rate of infection. A case-control study after an SSTI outbreak in 2005 in a Florida college football team identified previous skin abscess as the only independent risk factor for an MRSA SSTI among 13 patients (25). An outbreak of 6 confirmed and 19 suspected (cellulitis during the outbreak period with two or more of the following: swelling, fever, heat, or purulence) cases occurred in a college football team in August to September 2006; the three MRSA isolates tested belonged to USA300 or USA800, and risk factors for infection included the use of hydrocollator packs and other athletic training equipment as well as being a lineman or a tight end (356). In a meta-analysis of four previously published studies (53, 135, 665, 775) of players from three division I college football teams in 2003 to 2006, MRSA infections occurred in 6.7% (33/491) players, primarily on the extremities, with no relationship to position played (87).
Household Contacts of MRSA Patients
Transmission of S. aureus in the household setting was documented prior to the CA-MRSA epidemic (706), but new attention has been focused on the issue, with anecdotal suggestions that such transmission may be common. Reports of household contact transmission of CA-MRSA have been documented among health care workers (613) and, more recently, among non-health care workers in the community (193, 237, 272, 350, 400) in the United States, but the subject has not been studied rigorously. The role of fomites in household transmission is not known (see below).
Household transmission of CA-MRSA strains in the United States, Europe, and elsewhere (3, 271, 376, 378, 381, 395, 522, 533, 672, 697, 967, 977) has been reported. For example, among MRSA infections of families of military personnel in San Diego, CA, 10% of the 632 isolates in 2004 were from patients who had a family member who also had an MRSA infection in the same year (193). In Europe, where contact tracing of index MRSA cases is commonly performed, several case reports demonstrated household transmission (847). In Greece in 2003 to 2005, among 88 CA-MRSA infections of children, 15.9% had suspected transmission of MRSA from family members (673). In Lund, Sweden, in 2000 to 2005, household contacts were tested routinely for MRSA colonization when a hospitalized patient was identified with an MRSA infection. In 22 of 51 cases with contact tracing, 42 colonized household contacts were identified. In the 22 households with colonized contacts, 70% of the contacts were colonized with MRSA in the anterior nares, throat, or perineum or at the site of a skin lesion. With a single exception, all MRSA isolates from household contacts shared the spa type of the isolate from the corresponding index patient (440).
Sexual activity or other skin-to-skin contact may be a means of household CA-MRSA transmission (766), as was suggested by the apparent heterosexual transmission of USA300 among members of three households in New York City in 2004 to 2006 (182). More research is needed to assess the role of MRSA transmission within households and by sexual contact.
Emergency Department Patients
U.S. ED visits for SSTIs increased from an estimated 1.2 million in 1993 to 3.4 million in 2005, an increase from 1.35% to 2.98% of all ED visits (699), likely reflecting the impact of CA-MRSA. EDs serve as a safety net that provides health care for uninsured populations in the United States, and thus, the number of SSTIs treated may reflect the prevalence of these infections in communities with a low socioeconomic status (SES). The higher SES of patients in private physicians' offices, in contrast, may explain why a similar study of U.S. physicians' offices in 1993 to 2005, using data from the National Ambulatory Medical Care Survey, did not show an increase in the percentage of all office visits due to dermatitis or SSTI during this period (700).
Several studies of EDs support the finding that there is an increase in MRSA disease among ED patients. In August 2004, among 11 university-affiliated EDs in U.S. cities, MRSA accounted for 59% of 320 S. aureus SSTIs; 97% of the MRSA isolates were USA300 strains (628). Cultured skin lesions among adults presenting to an ED in Cincinnati, OH, with an SSTI in 3 months during 2005 yielded MRSA at a rate of 58%. Risk factors for MRSA infection included in a best-fit multivariable regression model were young age, sexual contact in the past month, the presence of an abscess cavity, and residence in a group home (433). In a Nashville, TN, ED, MRSA was isolated from 67.6% (255/367) of adult and 79.7% (145/182) of pediatric SSTI cultures in 2004 to 2005 (883). Of a convenience sample of 68 children who presented to an urban North Carolina emergency department with abscesses in 2005 to 2006 and underwent drainage, 88% (60/68) of isolates grew S. aureus; 85% (51/60) were MRSA (570). Among 195 children with SSTIs presenting to a suburban New Jersey ED in 2003 to 2007, 27% of isolates grew MRSA (453). In Philadelphia in 2007, 47/85 (55%) community-associated (by CDC criteria), culture-proven hand infections of adults presenting to an ED were caused by MRSA; MRSA was associated with intravenous nonmedical drug use and a high white blood cell (WBC) count of >8,700 cells/ml (690). In a Chicago, IL, ED, surveillance in 2004 to 2005 demonstrated that among 128 MRSA isolates recovered from ambulatory patients, 84.4% were susceptible to clindamycin, 94.5% carried SCCmec type IV, 89.1% were PVL+, 82.8% were ST8, and 91.4% were SSTIs, all characteristics of CA-MRSA strains and the SSTIs that they cause (216). At two military hospitals in Texas in 2004 to 2005, 68% of 220 abscesses cultured yielded MRSA (248). MRSA was the most common etiology of septic arthritis identified among 109 synovial fluid cultures sent from two EDs in California in 2006 to 2007; 6/12 (50%) cases diagnosed as septic arthritis were caused by MRSA, and 4/12 (33%) were caused by MSSA (303).
There are fewer studies from EDs outside the United States. At a French ED in 2004 to 2005, patients with MSSA and MRSA were compared. Of 93 MRSA patients, 9 were younger than 40 years of age and had no known health care exposure (955), documenting the existence CA-MRSA patients served by an ED in France. In a surveillance study of EDs in 2006 to 2007 in Hong Kong, MRSA was responsible for a minority, 19/298, of SSTI cultures and 19/126 S. aureus SSTI cultures. CA-MRSA (CDC criteria) accounted for 13/241 abscess cultures, 12 of which were PVL+; all carried SCCmec type IV or V. Six were ST30 strains and were susceptible to all non-β-lactams tested. Five were ST59 strains with variable susceptibility to tetracycline, clindamycin, and erythromycin. Of the 12 CA-MRSA SSTIs, 4 were infections of foreign workers from the Philippines (397). In an ED in Madrid, Spain, in 2007, seven CA-MRSA (by CDC criteria) SSTIs were diagnosed in children: 6/7 isolates obtained were ST8 isolates bearing SCCmec type IV, and 5/6 of these were PVL+ (208).
CA-MRSA infections are often treated in EDs, which provide care to an underserved and underinsured population in the United States; more research is needed to determine why they are a focus of the CA-MRSA epidemic.
Urban Underserved Communities
Studies of medically underserved communities in U.S. cities have revealed foci of CA-MRSA SSTIs and frequent asymptomatic MRSA nasal colonization. In San Francisco, CA-MRSA has been well documented to have targeted certain adult populations. For example, in 1999 to 2000, 2.7% of 833 homeless or poor adults harbored MRSA (153), a rate higher than that found in 2001 to 2002 in the general U.S. population (492). Among IVDUs in that city in 1999, 6.1% carried MRSA. Of the 35 MRSA isolates genotyped, 28 carried SCCmec type IV (154). Of isolates from adult patients at a clinic opened to treat SSTIs in an underserved community in 2000 to 2003, 91% were S. aureus, and 59% of the S. aureus isolates were MRSA isolates. Many of these patients were IVDUs (1020). At an urban public hospital in that same city, among 137 patients from a population skewed to the homeless and IVDUs in 2003 to 2004, 51% of cultures from SSTIs grew MRSA. Of cultures obtained from the nose or an SSTI in this population, 75% were MRSA isolates; 99% carried SCCmec type IV, and 94.1% were PVL+ (304). Among homeless and runaway youths (12 to 24 years old) in San Francisco in 2002, 6.2% of 308 subjects had nasal MRSA colonization. Of the 19 MRSA isolates identified, 84% were strains of USA300 or USA1000 (702), well-known CA-MRSA clones. Among 215 homeless men and women in Cleveland, OH, 25.6% (55/215) had nasal carriage of MRSA; MRSA carriage was associated with antibiotic use in the previous 30 days (P < 0.04), a history of alcoholism (P < 0.08), current smoking (P < 0.06), and a lower frequency of staying with a friend for at least 1 night in the previous 30 days (P < 0.03) than non-MRSA carriers. All of these associations remained significant upon multivariate analysis except cigarette smoking (dates of the study were not provided) (505).
It is likely that USA300 is more widespread in populations affected by poverty. MRSA isolates causing community-onset SSTIs in 2000 to 2002 from Stanford University Hospital (SUH), located in a suburban area that serves a population largely covered by private insurance, were compared with those from San Francisco General Hospital (SFGH), a hospital serving an inner-city community. At SUH, MRSA isolates were less likely to carry SCCmec type IV (29% versus 90%) and less likely to be PVL+ (16% versus 55%). Furthermore, 69% of SSTIs at SUH had their onset in the community, compared with 93% at SFGH. USA300 was the dominant clone causing SSTIs at SFGH in 2002 but was not at SUH. Being nonwhite and younger than 60 years of age were associated with infection caused by SCCmec type IV-bearing and PVL+ strains of MRSA (68).
Similarly, in Chicago, contrasting the experiences of a large public hospital and a large private hospital demonstrated different epidemiological patterns. At Cook County Hospital and its associated clinics, an increase in the incidence of CA-MRSA SSTIs from 24 cases/100,000 population in 2000 to 164.2 cases/100,000 population in 2005 was documented. In January 2000 to August 2005, 971 CA-MRSA SSTIs were recorded (using criteria similar to the CDC case definition). Risk factors for CA-MRSA infection, compared with CA-MSSA infection, included recent incarceration, African American race, and residence in a public housing complex (403, 731). In contrast, among adults hospitalized in 1998 to 1999 at Northwestern Memorial Hospital in Chicago, located near the more-affluent Loop region, only 1.9% (n = 20) of MRSA isolates cultured from 1,071 patients within 72 h of hospital admission were clindamycin susceptible (a frequently used proxy for CA-MRSA isolates) (873), suggesting that CA-MRSA disease had remained infrequent during that period in that population.
In other cities, including Dallas and Atlanta, racial and socioeconomic disparities predisposing one to MRSA infection risk were similarly documented. For example, during 5 months in 2003 at a Dallas hospital, among inpatient adults with S. aureus infections with isolates cultured within 72 h of admission, 63% had MRSA infections. The patients with MRSA were more likely than patients with MSSA to have a history of homelessness, to be African American, to have an SSTI, and/or to have used antibiotics in the previous 6 months (841). In Atlanta in 2003 at a large public hospital serving the inner city, 7.3% of 726 hospitalized patients had nasal colonization with MRSA at admission. Risk factors included HIV infection, SSTI, recent use of antibiotics, or admission to the hospital in the previous 12 months (385). A study in Atlanta in 2003 at a 1,000-bed public hospital and its affiliated clinics found that the USA300 strain was the predominant cause of S. aureus SSTIs diagnosed in outpatients or within 72 h of hospital admission and that African American race, female sex, and hospitalization within the previous 12 months were independently associated with infection by a CA-MRSA strain (475).
By 2007, most major urban centers in the United States had reported CA-MRSA case series. However, geographic variation continued. For example, CA-MRSA was recognized later on the East Coast than in the Midwest, Texas, Tennessee, and California. In 1999 to 2000, among 500 patients enrolled in a methadone program in New York City who were not current i.v. heroin users, only 10 (2% of all tested) had nasal colonization with MRSA. These MRSA isolates were genetically distinct from locally prevalent HA-MRSA strains; 9 of the 10 MRSA colonization isolates carried SCCmec type IV (611), suggesting a community origin. Since 2000, however, USA300 has become more common in New York City, and infections with USA300 have been associated with a higher incidence in neighborhoods with lower SES. In a study from Brooklyn, NY, in 2005 to 2006, hospitals in areas with a low SES (by several measures) were reported to have a higher rate of USA300 infections than hospitals in areas with a higher SES (94).
Outside the United States, few studies have documented similar associations between CA-MRSA and low SES. An exception was in Alberta, Canada, where CA-MRSA infection was associated with homelessness (318).
Indigenous Populations
Multiple indigenous populations, including Native American (NA), First Nation (Manitoba and Nunavut, Canada), Australian Aboriginal, Pacific Islander, and Alaska Native ethnicities, have been associated with a high risk of infection with CA-MRSA strains (Table 8 ). Many of these groups are disadvantaged in their societies, and their association with lower SES may be responsible for the increased risk of CA-MRSA infection (905). In Australia, CA-MRSA was first noted for aboriginal communities, a socially disadvantaged group with crowded living conditions and frequent use of antimicrobial drugs (905). In a small indigenous community in Australia, 15% of tested children had either infections or colonization by MRSA (958). In the United States, at hospitals administered by the Indian Health Service, MRSA-associated hospitalizations increased from 4.6 per 100,000 American Indians/Alaska Natives in 1996 to 1998 to 50.6 per 100,000 in 2003 to 2005. Among these patients, 59% had a diagnosis of SSTI (116).
TABLE 8.
Indigenous populations and CA-MRSAa
| Ethnicity | Yr | Study summary | Setting | Reference(s) |
|---|---|---|---|---|
| Native Americans (United States) | 1997 | 74% (46/62) of isolates identified in a review of MRSA infections at an Indian Health Service facility were CA-MRSA (i.e., obtained from an outpatient or <48 h after admission from an inpatient, no history of hospitalization, renal dialysis, or residence in an LTCF in the previous yr, and no documentation of i.v. drug use); the percentage of S. aureus isolates that were MRSA in this community increased from 4% in 1989 to 10% in 1993, 25% in 1994, and 57% in 1997 | Rural Midwestern Native American community | 349 |
| 2001 | 1.9% (9/468) of patients had asymptomatic carriage of MRSA; 56% (5/9) were CA-MRSA (i.e., taken from a patient without inpatient health care exposure, hemodialysis, or occupation in a health care facility in the previous year); 5 of the 9 (56%) MRSA isolates were closely related by PFGE typing; 8/9 (89%) isolates were susceptible to all non-β-lactam antibiotics tested with the exception of erythromycin (3/9 were resistant to erythromycin) | Predominantly Native American community, Washington State | 526 | |
| Native Alaskans (United States) | 1996, 2000 | Outbreaks of MRSA SSTIs; causative isolates were predominantly ST1, ST30, or ST59, all were PVL+, and all carried SCCmec type IV | Remote Native Alaskan villages, southwestern Alaska | 36, 37, 504 |
| Australian Aboriginal people and PIs | 2004 | MRSA colonization in 14 of 92 (15%) children in nose, throat, or skin wounds; 6/14 (43%) carried PVL+ ST93 strains, and 2/14 (14%) carried PVL+ ST30 strains; 5/14 (36%) carried PVL-negative ST5 strains; 14/15 (93%) were susceptible to all tested non-β-lactam antibiotics | Indigenous community, schoolchildren in grades 1-7, Queensland, Australia | 958 |
| 2000-2003 | 8 cases (4 pediatric and 4 adults) of severe invasive infections with either ST93 or ST30 PVL+ MRSA isolates obtained <48 h after admission, with no health care exposure or antibiotics in previous 12 months; 5/8 (63%) patients were PIs or of Aboriginal ethnicity | 3 large hospitals, Southeast Queensland, Australia | 720 | |
| 1991-1995 | Community-acquired WA-MRSA (i.e., Western Australian strain, defined by antibiotic susceptibilities) infections were more likely to occur in Aboriginals than in non-Aboriginals (RR, 25.9; 95% CI, 12.51-53.47) | Royal Darwin Hospital, Northern Territory, Australia | 573 | |
| 1997-1998 | 35 gentamicin-susceptible MRSA isolates from infections; 23 were community acquired; 17/23 (74%) patients had no health care exposure; 10/17 (59%) were PIs, and 1/17 (6%) was Aboriginal; all 11 isolates from PIs or Australian Aboriginal people were of the same pulsotypes | Clinical microbiology laboratory, 4 hospitals, Brisbane metropolitan area, Queensland, Australia | 672 | |
| 1998-2001 | Of 15 episodes of community-onset MRSA bacteremia (i.e., patients with isolates cultured <48 h after admission, with no indwelling catheter, and with no history of hospitalization or stay in an LTCF in previous 90 days) in 14 patients, 12/14 (86%) patients self-identified as being Aboriginal, while 25% of the population served by the hospital was Aborginal; 10 isolates carried SCCmec type IV | Royal Darwin Hospital, Northern Territory, Australia | 647 | |
| 2004-2005 | Case-cohort study of 100 non-MDR MRSA (i.e., resistant to ≤2 tested non-β-lactam antibiotics) infections compared with matched MSSA-infected patients (2:1) and MDR MRSA-infected patients (1:1); Aboriginal or Torres Strait Islanders had an odds ratio of non-MDR MRSA infection compared with MDR MRSA infection of 3.9 (95% CI, 1.16-16.92) upon univariate analysis; this was not significant upon multinomial logistic regression | 8 hospitals, southeast Queensland, Australia | 642 | |
| 2001-2002 | 100 gentamicin-susceptible MRSA infections of 98 patients; 20 patients were PIs (60% had ST30 SCCmec type IV isolates), and 10 were Aboriginal (80% had ST93 PVL+, SCCmec type IV isolates); all 3 episodes of bacteremia were in Aboriginal children with an ST93 strain; PIs and Aboriginals each accounted for <2% of the population of New South Wales | Pediatric teaching hospital, New South Wales, Australia | 352 | |
| 2005-2006 | 89% (98/104) of infections caused by non-MDR MRSA isolates (i.e., isolates resistant to <3 non-β-lactam antibiotics tested) were of Aboriginal people | Alice Springs Hospital, Alice Springs, Northern Territory, Australia | 861 | |
| Canadian FN | 1990-1992 | 259 MRSA infections of 135 inpatients in 36 mo; 85 patients had MRSA cultured <72 h after admission (community acquired); CA-MRSA patients were younger, more likely to have a rural residence, and more likely to be of FN ethnicity than HA-MRSA patients; 62% of CA-MRSA infections were in FN, and 14% of HA-MRSA infections were in FN (P < 0.001) | Five tertiary care hospitals in Winnipeg, Manitoba, Saskatoon, Saskatchewan, Calgary, Alberta, and Edmonton, Alberta, Canada | 263 |
| 2006-2007 | Outbreak of 43 CA-MRSA infections; 95% of isolates were USA400; for 5- to 9- and 20- to 29-yr-old populations, the cumulative incidence was 26/1,000; the outbreak accounted for 80% of reported MRSA cases in the province | Remote Inuit community with population of 2,000 in Nunavut, Canada | 203 | |
| 2003-2006 | Rising rates of MRSA cases reported from clinics serving FN communities, reaching an incidence of 8 to 16/10,000 in areas of 2 regional health authorities | Northern Manitoba, Canada | 507 | |
| 1995-2002 | 279 FN patients with MRSA infection or colonization; their isolates were more likely to be susceptible to erythromycin, clindamycin, TMP-SMX, and ciprofloxacin, more likely to be resistant to mupirocin, and more likely to have a pulsotype similar to USA300 (CMRSA-5) than MRSA isolates from non-FN patients; 61% of FN inpatients vs 33% of non-FN patients had a clinical MRSA infection; FN patients were 6-fold-more likely to have a CA-MRSA infection than non-FN patients | 38 hospitals, inpatients, Canada | 684 | |
| PIs | 2001-2003 | 51% of 346 CA-MRSA infections (CDC criteria) were of PIs, while only 24% of the state population was PIs in 2001; 92% of the infections studied were SSTIs | 4 health care facilities, Hawaii | 131, 270 |
| 1996-2000 | 80% of samples from Samoan or PI patients (4/5) vs 12% of non-Samoan/non-PI patients (4/34) with S. aureus SSTIs were MRSA | Surveillance, family practice clinic, Anchorage, AK | 125 | |
| 1997-1998 | Case series of 74 CA-MRSA infections (i.e., no previous contact with hospital or nursing home); disproportionate no. of cases in people from the South Pacific (e.g., Tonga and Western Samoa) | Hospitals in Brisbane, Canberra, Melbourne, and Sydney, Australia | 178 | |
| 1993-2004 | Review of 58 pediatric S. aureus sepsis cases; isolates from all 7 MRSA (12%) cases were cultured <48 h after admission, and all 7 patients were PIs or Maori | Hospital pediatric ICU in Auckland, New Zealand | 605 | |
| 1992-1996 | Case series of 10 MRSA infections in inpatients with onset in the community (excluding nursing home residents, those hospitalized in the previous 6 mo, or those with isolates cultured >48 h after admission); 2/10 (20%) patients were from American Samoa | Tripler Army Medical Center, Hawaii | 333 | |
| 1998 | Chart review of all 9 non-MDR MRSA isolates (susceptible to erythromycin, tetracycline, ciprofloxacin, gentamicin, rifampin, fusidic acid, and vancomycin) obtained in 2 months; all patients were Polynesians, and all had severe SSTIs | Clinical microbiology laboratory serving public hospitals, South Western Sydney Area Health Service, Australia | 337 | |
| 1998-1999 | 26 non-MDR MRSA infections; 29% (7/24) of non-MDR MRSA vs 0% (0/9) of MDR MRSA infections were in people born in Samoa, Tonga, or New Zealand; 44% of non-MDR MRSA vs 0% of MDR MRSA infections were CA-MRSA (i.e., no hospitalization, surgery, or residential care in previous 12 mo and no chronic disease) | Patients at emergency or dermatology departments at hospitals, South Western Sydney Area Health Service, Australia | 338 | |
| 2000-2001 | 39% (17/44) of infections with non-MDR MRSA occurred in patients from the Southwest Pacific Islands, while 3% of the general population was from these islands; 16/17 (94%) infections in PIs were community acquired (i.e., cultured <48 h after admission and in patients with no health care contact in the previous 12 mo and no chronic illness); 7 isolates were the “Pacific Island strain” by PFGE | Ipswich Hospital, Queensland, Australia | 645 |
Abbreviations: FN, First Nations; LTCF, long-term care facility; PI, Pacific Islander.
Pacific Islanders in many regions have been found to be a high-risk group for MRSA infection. Higher rates of all S. aureus infections have also been noted for Pacific Islanders by investigators in New Zealand and Australia (196, 387). The reasons for this association are not known. In Hawaii, a prospective study of all MRSA infections diagnosed at four health care facilities from July 2001 to June 2003 found that among 1,389 patients with MRSA infection, 28% were infected by CA-MRSA. These infections were disproportionately more common among self-described Pacific Islanders than among Asians. Those investigators did not collect markers for SES in this cohort. However, they did note that Pacific Islanders had a higher poverty rating, larger families, and a lower proportion of college graduates than did Asians (131).
More study is needed to determine why certain ethnic populations face a disproportionate risk of MRSA infection or asymptomatic colonization.
Incarcerated Populations
Incarcerated populations in the United States are at a high risk of MRSA infections. Many outbreaks have been reported in jails and prisons (136, 138, 918), and in many urban jails, MRSA has become an endemic pathogen and the predominant etiology of cultured SSTIs (39, 215, 703, 888). There have also been many case reports of detainees and recently released prisoners with MRSA infections (241, 299, 789, 832, 835, 941, 1021). Molecular evidence has linked the MRSA isolates from correctional facilities to local CA-MRSA strains (140, 215, 703, 918). In the only large-scale study of its kind, in 1999 to 2001, the Texas Department of Criminal Justice found that 12 MRSA infections occurred per 1,000 prisoner-years, a very high rate; among the risk factors identified were female gender, white race, jail (as opposed to prison) incarceration, and young age (39). The higher risk demonstrated for younger inmates suggests an epidemiological pattern consistent with CA-MRSA (136) in other populations.
Many detainees in urban jails are held for only brief periods of time and are often recidivists; this revolving door is potentially an amplifier of epidemic MRSA colonization in communities with a high prevalence of recently jailed individuals and their contacts. In the United States, the incarcerated population increased from 325,400 in 1970 (51) to 2,245,189 in June 2006 (793). Approximately 11.5 million inmates were released from incarceration facilities in 1998, most from local jails (660). In 2006, 1 in every 133 U.S. residents was incarcerated, but more than 1 in 9 (11.7%) African American men aged 25 to 29 years were detained (793). If jails are a common site of MRSA colonization, as they appear to be, this population and their contacts may face a high risk of MRSA colonization and infection.
MRSA has been shown to be the predominant pathogen causing SSTIs among detainees in jails in many U.S. cities. A study of MRSA isolates causing infections in five county jails near San Francisco demonstrated a dramatic rise in the percentage of S. aureus SSTIs caused by MRSA, from 29% in 1997 to 74% in 2002. There were two predominant MRSA clones, suggesting the spread of these clones in the jail or a common source of colonization among detainees (703). Among 502 MRSA isolates obtained in 2001 to 2007 from infections of detainees in the San Francisco County Jail, USA300 first appeared in 2001 and rapidly became the predominant strain after 2005. The number of MRSA infections rose each year, from 25 in 2000 to 60 in 2007, although there was little change in the numbers of MSSA infections each year. The majority of the strains were isolated from patients with SSTIs. Clindamycin resistance was found for 9.3% of MRSA isolates and did not significantly change over time (888). In an 18-month period in 2004 to 2005 in the Cook County Jail in Chicago, IL, the largest single-site pretrial detention facility in the United States, MRSA was identified as the etiology of 63.5% (240/378) of all cultured skin lesions and 85% (240/283) of all S. aureus skin infections (215). At Stroger Hospital of Cook County and its clinics in Chicago in 2000 to 2005, incarceration during the previous year was an independent risk factor for an MRSA SSTI (403). At the Whatcom County Jail in Washington, 50/74 (68%) SSTIs in 2005 were caused by MRSA (223).
In 2001 to 2002, an outbreak of MRSA SSTIs was recognized at the Los Angeles County Jail (LACJ), the largest county jail system in the United States. From January 2002 to June 2003, there were 1,697 MRSA skin infections reported; 79% were reviewed. The predominant isolates from the jail had CA-MRSA PFGE pulsotypes (140). The early diagnosis of some lesions (9% in 2002 and 14% in 2003 were diagnosed within 5 days of booking) (136, 140) may have reflected a high incidence of MRSA colonization in the community or, alternatively, rapid transmission in the jail setting. Further supporting the former position, a mathematical model of MRSA in the LACJ demonstrated that although >8,000 CA-MRSA SSTIs were recognized in 2002 to 2005, the inflow of infected detainees from the community may have fueled the epidemic (454).
The importance of fomite contamination with MRSA in jails is not known, but in a Texas jail, investigators in 2005 found that 8/132 (6.1%) fomites had recoverable MRSA; 4/6 tested MRSA isolates were USA300 isolates by PFGE (282).
There have been few studies of nasal MRSA colonization in a prison or jail. In 2000, 4.9% (86/1757) of inmates at a Mississippi prison were colonized with MRSA. There was a disproportionately high colonization rate for females (5.9%) compared with males (2.5%). The major risk factor identified for MRSA nasal colonization was residence in the prison for ≥60 days. Longer-term detainees had a 5.4% MRSA colonization rate, versus 0.7% for those incarcerated for a shorter time. Of 41 isolates cultured from infected detainees, the vast majority were susceptible to non-β-lactam antibiotics, and PFGE demonstrated three predominant clonotypes, suggesting a local focus of dissemination of MRSA among the detainees (138). In a study of detainees admitted to a correctional ward of a hospital in Maryland in 2003 to 2004, 13% had either a clinical MRSA infection or colonization; female detainees were more likely to be colonized (relative risk [RR], 2.46). Detainees from the Baltimore City Jail were more likely to be MRSA carriers than were detainees from other correctional institutions, with a very high carriage prevalence of 17%. The USA300 genotype constituted 36% of the 56 MRSA isolates tested and was the most common genotype recovered (1010). At the Baltimore City Jail in 2006, 15.8% (95/602) of newly arriving detainees had MRSA nasal colonization; 80% of the recovered strains were USA300 or related types. Surprisingly, only 13.1% (3/23) of SSTIs identified in this population were caused by MRSA (277).
Outbreaks in prisons have been studied less often, but they have provided insight into possible risk factors and means of MRSA transmission among incarcerated populations. For example, a CDC-sponsored case-control study after an outbreak of 59 cases of MRSA SSTI in a Mississippi prison in 1999 to 2000 demonstrated that 78% of the patients were female, while only 40% of the prison detainees were female. Detainee patients with an SSTI caused by MRSA were more likely than controls to have helped an inmate or to have been helped by another inmate with dressing changes of wounds, to have lanced their own or other detainees' boils, or to have shared personal items with other detainees (138). Poor personal hygiene, measured by using a composite hygiene score, was blamed for an outbreak of MRSA SSTIs in 2002 to 2003 in a prison in Missouri (918).
In 2001 to 2003, the CDC investigated MRSA outbreaks in Georgia prisons. A case-control study was performed for a 200-bed short-stay detention center, where 11 cases of MRSA SSTIs occurred in 2001. Risk factors for infection included incarceration for more than 36 days and outdoor work duty. Despite improvements to hygiene, after a 5-month hiatus with no infections, 19 more MRSA cases were detected in 2002 to 2003 (136). A second Georgia prison housed 1,500 inmates and had 11 cases of MRSA infection in 2002. A case-control study revealed the following risk factors: previous antibiotic use, self-draining of boils, skin laceration, washing clothes by hand, and arrival to the prison after 2001. Further surveillance revealed 73 additional infections in April 2002 to February 2003. Despite the isolation of inmates with MRSA infections and the provision of a 5-day supply of chlorhexidine-based soap for all inmates, 29 additional cases occurred in March to May 2003 (136). These studies demonstrate that while some risk factors are understood, the control of MRSA in places of incarceration may be a difficult task.
In 2005 to 2006, information on S. aureus infections and colonization was collected from the New York State prison system. In two prisons, MRSA nasal colonization was found for 0.8% (2/251) of men and 4.7% (11/236) of women; all 13 MRSA isolates carried SCCmec type IV, and 6/13 (46%) isolates were USA300 strains. Among 60 S. aureus isolates from infections of detainees occurring in January to June 2006, 48.3% (29/60) were MRSA isolates; of the 29 MRSA infection isolates, 48.2% (14/29) were PVL+, and 93.1% (27/29) carried SCCmec type IV, findings consistent with CA-MRSA strains. Associations between an increased length of stay and the likelihood of a PVL-positive MRSA infection were found for maximum-security prisoners. Among medium-security prisoners with S. aureus infections, both older age and longer length of stay were associated with a decreased likelihood of having an MRSA infection (560).
Most reports of incarceration-related MRSA disease have been from the United States. However, in Alberta, Canada, an outbreak of USA300 MRSA infections in 2004 demonstrated that a history of recent incarceration was a significant risk factor for infection (318). Two five-person outbreaks of MRSA SSTIs were recorded for a 500-person correctional facility in Hamilton, Ontario, in 2002 and 2004. All SSTIs were caused by USA300 strains that were PVL+, and there was proven contact among only some of the detainees, at least two of whom had shared a cell with a detainee who lanced the boils of others and one of whom had AIDS (575). A large outbreak of skin infections caused by CA-MRSA strains was reported for a prison in Uruguay, which was associated with a scabies infestation (564).
Overall, poor hygiene is likely a major contributor to the problem of MRSA infections in places of incarceration, but there may be other risk factors for incarcerated populations that put them at a specific risk for exposure to MRSA outside jails and prisons. Furthermore, if detainees are likely to become asymptomatic carriers of MRSA while incarcerated, with jail and prisons serving as a reservoir, released detainees may also spread MRSA to their families and other contacts.
Cystic Fibrosis
Cystic fibrosis (CF) is a chronic disease resulting from one of many mapped mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, which usually leads to progressive dysfunction in many organ systems, particularly the lung and respiratory tract. Patients with CF suffer from recurrent infections, bronchiectasis, and frequent respiratory tract colonization with antimicrobial-resistant bacterial pathogens, particularly Pseudomonas aeruginosa and S. aureus. MRSA respiratory carriage and infection are becoming increasingly common among CF patients according to data from the Cystic Fibrosis Foundation. In 1995, only 0.1% of CF patients had MRSA recovered from their respiratory tract; the prevalence increased to 7.3% in 2001 and 17.2% in 2005 (200, 201, 202). Some researchers have suggested that MRSA colonization is a poor prognostic sign in CF. During 2001, in an epidemiological study of 1,834 children from North America with CF and S. aureus in their respiratory tract cultures, CF patients with MRSA had a lower mean forced expiratory volume in 1 s (FEV1), were more likely to be treated with an antimicrobial drug, and were more likely to be hospitalized than those with MSSA infections. These children were likely colonized predominantly by HA-MRSA strains (755). A study from the Cystic Fibrosis Foundation registry from 1996 to 2005 including 17,357 CF patients aged 8 to 21 years, controlling for severity of disease at baseline, common coinfections, and common comorbidities, found that the FEV1 decline was 43% more rapid among the 1,732 patients who developed new and persistent MRSA infection than among the noncolonized patients with CF (206). Other researchers, using data for 5,090 patients in 2001 to 2003 from the Epidemiologic Study of CF, suggested that this association is not significant if one accounts for FEV1 prior to MRSA colonization (806). A prospective study is needed to definitively determine if there is a true association (805).
Several studies have examined the relative burden of CA- and HA-MRSA strain types among strains isolated from screening cultures and infections of CF patients to assess the impact of the CA-MRSA epidemic in this population. CF patients at Emory University in 2004 to 2005 were more likely to harbor an MRSA strain with inducible clindamycin resistance (68/143; 48%) than were non-CF patients (43/560; 8%) (P < 0.01) (627). At Washington University in St. Louis, 15% of children with CF newly colonized with MRSA in 2001 to 2004 had PVL+ MRSA strains. These children were more likely to have an active pulmonary infection than children colonized with PVL-negative strains (256). In Chapel Hill, NC, in 2005 to 2007, 19/707 (2.7%) CF patients were colonized by PVL+ MRSA strains that carried SCCmec type IV, while overall, 140/707 (19.8%) patients had at least one respiratory culture that grew MRSA in this period (332).
A study from Dallas and Chicago compared MRSA isolates obtained from 34 children with CF and 331 children without CF in 2004 to 2005. Of the CF patient isolates, 64.7% belonged to MLST clonal cluster 5 (CC5) and carried SCCmec type II, both markers for HA-MRSA strains, and 26.5% belonged to CC8 and carried SCCmec type IV, both markers for CA-MRSA strains. In contrast, among MRSA isolates from non-CF patients, 88.8% belonged to CC8 and carried SCCmec type IV, and only 4% had HA-MRSA markers. Isolates from CF patients were more likely to be resistant to clindamycin and ciprofloxacin. Isolates from screening cultures compared with isolates from active infections did not differ in the likelihood of carriage of PVL genes, suggesting that PVL+ isolates may not be more likely to cause disease in CF patients (324).
Although there are few data, MRSA colonization overall and PVL+ MRSA colonization in particular may be less common among CF patients in Europe than among CF patients in the United States. In Italy, 181/2,362 (7.6%) CF patients at nine centers were colonized with MRSA in 2004 to 2006. Of the 181 MRSA-colonized patients, 36% had isolates carrying SCCmec type IV. MRSA strains of a single, unstated PFGE type colonized 31 patients; 24 of these carried SCCmec type IV, and none of the 24 isolates carried PVL (119; S. Campana, personal communication). At nine centers in Belgium in 2001, 5% of 627 CF patients carried MRSA strains, and 67% were genotypically related by PFGE to “epidemic clones that are disseminated in Belgian hospitals” (952). In Madrid, 93 MRSA isolates from 18 CF patients were obtained in 1994 to 2006; all the isolates were MDR and polyclonal, but 44 of them were ST228 isolates bearing SCCmec type I and lacked the PVL genes (617). All CF patients in Northern Ireland are tested every 3 months for MRSA colonization; 17/250 were found to carry MRSA at some time during 1999 to 2004. By using a three-step protocol requiring 1 or 2 courses of oral fusidic acid and rifampin followed, if necessary, by intravenous teicoplanin, investigators were able to decolonize 16 of the 17 CF patients; they all remained free of MRSA sputum colonization 1 year later (567).
In summary, it appears that CF patients may be colonized with MRSA strains and that the rate is increasing. Some are CA-MRSA strains, but the patients remain at as great a risk or are at a greater risk for colonization and infection by the HA-MRSA strains that predominate in their geographical region. The importance of asymptomatic CA-MRSA colonization as a predictor of disease in this population remains unclear.
Military Populations
Healthy military populations and their families are another group who may be at risk for CA-MRSA infection and colonization (501). For example, among 812 new military recruits reporting for training in Texas in 2003, 24 (3%) carried MRSA in their nares; most had at least one risk factor for HA-MRSA. After 8 to 10 weeks of training, 9 of these 24 soldiers (35%) developed SSTIs, although 16 (66%) were no longer colonized with MRSA. Four recruits became newly colonized with MRSA while in training (259). This suggests that many recruits were transiently colonized and that colonization predisposes one to disease. In a follow-up study of 3,447 U.S. soldiers in Texas in 2005, 134 (3.9%) were colonized with MRSA (260). Of isolates from these soldiers, 53% were USA300 strains. Among the 3,066 soldiers who completed the study, 39 had an SSTI caused by MRSA, 97% of which were caused by USA300 strains (261). Among active military service members deployed to Iraq in March to July 2008, 66 were diagnosed with a carbuncle, furuncle, boil, or abscess, as determined by a retrospective review of administrative records. Of isolates from the 66 service members, 26 (39%) underwent culture; 22/26 (85%) grew S. aureus, and of these isolates, 15/22 (68%) grew MRSA (768).
Many other case series from various locations in the United States demonstrate how widespread CA-MRSA infections are among military populations. After a large outbreak of MRSA SSTIs in 2000 to 2002 among military recruits at a training facility in Virginia, of 874 healthy workers who had direct contact with the recruits, 2.7% (24/874) carried MRSA in their nares (1029). At a military facility in Washington State in 1994 to 1997, of 67 adult patients presenting with MRSA infections or carriage, 13% (9) were CA-MRSA infections (i.e., from patients presenting as outpatients or cultured <72 h after admission and with no hospitalization, surgery, or use of antibiotics in the previous 12 months and no cystic fibrosis, i.v. drug use, HIV infection, diabetes mellitus, cirrhosis, or hemodialysis) (49). Among patients hospitalized with MRSA infections on a military base in Honolulu, HI, in 1992 to 1996, 41% had a CA-MRSA infection (by the CDC case definition) (333). MRSA was the leading cause of cultured skin abscesses at EDs at two military hospitals in Texas in 2004 to 2005 (248).
The burden of CA-MRSA disease may be increasing among active-duty and retired military personnel and their dependents. At the Naval Medical Center in San Diego, in a retrospective analysis of MRSA disease isolates obtained in 1994 to 1997, the incidence of CA-MRSA (i.e., patients with no hospitalizations in the previous 6 months and if MRSA was cultured from an isolate from an outpatient or within 24 h of hospital admission) infections rose quickly, from 14% of all MRSA infections in 1994 to 1995 to 29% in 1996 to 1997 (456).
Military recruits, active-duty personnel, and their contacts may be exposed to a common reservoir of CA-MRSA (259). The risk factors for CA-MRSA colonization may be analogous to those in local jails, including crowded living conditions and suboptimal personal hygiene at times of intensive training.
In a review from a Veterans Affairs hospital in Houston in 2000 to 2001, investigators studied cultures from all SSTIs, which by patient self-report were related to “spider bites” and required surgical intervention. All 38 cultures meeting these two criteria grew S. aureus, and 87% (33/38) of the S. aureus isolates were MRSA isolates (273).
Outside the United States, few studies of MRSA colonization among military personnel have been published. Among 959 Greek Air Force employees in 2004 to 2005, 9 (0.94%) had nasal colonization with MRSA, and 2 of the 9 had no previous known exposure to the health care system (461).
HIV Infection/AIDS
HIV infection has been determined to be an independent risk factor for CA-MRSA infection and colonization in some settings, particularly after 2001 (109, 589, 911). For example, 41/44 (93%) isolates from SSTIs cultured at an HIV clinic in Dallas County, TX, in 2003 to 2004 grew MRSA (842). In 2002 to 2004, at a clinic in Houston serving 3,500 HIV-infected patients, 74% of 93 consecutive cultures of isolates from SSTIs with a recoverable organism grew MRSA (489; G. W. Krucke, personal communication). Of 146 HIV patients at a clinic in Dallas in 2005, 15 (10.3%) had MRSA nasal colonization, 8 of whom carried USA300 or USA400 strains. Independent risk factors for MRSA carriage were prior infection with MSSA or MRSA (OR, 32.4 and 9.71, respectively), no current or recent antimicrobial drug therapy (OR, 0.026), and a low mean CD4 cell count (374 versus 252 cells/mm3; OR, 0.996). Interestingly, none of the patients taking TMP-SMX prophylaxis for Pneumocystis jirovecii pneumonia were colonized with MRSA (128). In 2000 to 2003 at the Naval Medical Center in San Diego, 31/458 (6.8%) HIV-infected patients had an SSTI caused by CA-MRSA (by CDC criteria), and patients with a CA-MRSA SSTI did not differ significantly in age, gender, or race from the overall cohort of HIV-infected patients. CA-MRSA patients did not have advanced HIV disease. They had a mean CD4+ cell count of 445 cells/mm3, and the HIV viral load was <1,000 copies/ml in 48% of the patients; 71% of the patients were receiving antiretroviral therapy at the time of their infections (195). A study performed in 2000 to 2003 demonstrated a steady rise in the incidence of MRSA infections among patients at an adult HIV clinic in San Diego from 2 to 5 per 100 patients in a 6-month period (589). At a clinic in Maryland, the incidence of CA-MRSA infections among HIV patients was 40.3 cases per 1,000 person-years in 2005. MRSA infection was associated with a low CD4+ count, a high HIV viral load, recent use of systemic antibiotics, and a history of syphilis. As in Texas, no CA-MRSA infections occurred among the patients taking TMP-SMX prophylaxis (194). HIV infection was a risk factor for MRSA colonization among S. aureus-colonized individuals admitted to a hospital in Atlanta, GA, in 2003 (385). In 2004 to 2006 at a clinic in Philadelphia, 43 CA-MRSA SSTIs (by the CDC definition except that a previous isolation of MRSA was not considered to be an HA-MRSA infection) were identified among HIV-infected patients, with the number increasing from 5 in 2004 to 22 in 2006; 58.5% had a CD4 cell count of >200 cells/mm3, and 17% had an HIV viral load of >100,000 copies/ml (911). At the Cook County Hospital and its associated clinics in Chicago, CA-MRSA and CA-MSSA (criteria for community-associated infections were not provided) SSTIs were retrospectively reviewed for 2000 to 2007, and population-based incidence estimates were calculated. HIV-infected patients were more likely to have CA-MRSA SSTIs than were non-HIV-infected patients (incidence of 952 versus 156/100,000 population; RR, 6.1; P < 0.001) (733).
HIV-infected patients are at an increased risk not just for MRSA colonization but also for any S. aureus colonization; the reasons for this association are not known. Among 282 recreational drug users in New York City in 1999 to 2000, 46% of HIV-infected subjects and 29% of uninfected subjects were colonized with S. aureus. When isolates from subjects were cultured at 6-month intervals, the likelihood of new S. aureus nasal colonization was twice as great among HIV-infected subjects as that among non-HIV-infected subjects (hazard ratio, 2.2; 95% CI, 1.1 to 4.6). Furthermore, among the nine subjects with MRSA colonization in the first 18 months, seven were HIV infected (610).
Further research is needed to determine which HIV-infected patients are at the greatest risk for CA-MRSA colonization and infection. In New York City in 2005 to 2006, 107 HIV-infected patients and 52 matched non-HIV-infected patients (including close contacts of the HIV-infected subjects) with no hospitalization in the previous year were tested for nasal or axillary MRSA carriage during at least one of three monthly assessments and prospectively monitored. HIV-infected patients who had a mean CD4+ cells count of 559 cells per mm3 were more likely than controls to have MRSA carriage (16.8% versus 5.8%; P = 0.04) and were more likely to develop an MRSA infection (10 versus 0). HIV-infected patients were more likely than controls to have any S. aureus colonization (58.9% versus 34.6%; P = 0.004). MRSA infections were associated with previous antibiotic use (P = 0.04) (827).
The association of CA-MRSA and HIV may be greater in certain regions of the United States than in parts of the world where CA-MRSA colonization is less common. For example, among HIV patients in Rome, Italy, the risk for a severe MRSA infection was independently associated with exposure to the health care system; among 27 HIV-infected patients with a severe MRSA infection in 2002 to 2005, only 1 infection was caused by CA-MRSA (by the CDC definition) (244). In Omaha, NE, 2/100 tested HIV-infected patients at a single clinic had nasal or perigenital MRSA colonization; these cultures were processed without enrichment broth, and this may have decreased the sensitivity of the cultures (569). The finding of predominantly HA-MRSA infections among HIV-infected patients in Italy and in Nebraska contrasts with data from studies in many parts of the United States. This difference may indicate variable susceptibility to MRSA or, more likely, the geographic variation in CA-MRSA infections and colonization.
Men Who Have Sex with Men
Some researchers have suggested that MSM in the United States and Canada face an increased risk of MRSA colonization and infections (361, 521, 825, 840, 875). For example, among the MRSA isolates obtained from patients with infections in San Francisco in 2004 to 2006, infection caused by a USA300 strain carrying resistance plasmid pUSA03 (see discussion above) was most common among patients residing in eight zip code regions with a high proportion of same-sex male couples. Among patients who had an MRSA infection, self-identification as a man who has sex with men was associated with an MDR USA300 infection. The authors of that study speculated that the MDR USA300 strain may be sexually transmitted (235). At a clinic in Boston where approximately 70% of patients were MSM by self-report, 3.8% (30/795) of patients in 2005 to 2007 had MRSA recovered from the nares, the perianal region, or a skin infection, and 73% (22/30) of the isolates were USA300 strains. Among enrollees, 3.7% (29/795) had an SSTI at enrollment, and 9.2% (73/795) of patients had an SSTI during a 16-month period in 2005 to 2007. Any SSTI, whether caused by MRSA or not, was strongly associated with previous perianal carriage of MRSA (OR, 10.34; 95% CI, 2.84 to 37.60), prior skin infection (OR, 4.08; 95% CI, 2.31 to 7.22), and crystal methamphetamine use (OR, 4.98; 95% CI, 2.60 to 9.55). The authors of that study suggested that skin-to-skin contact and multiple sexual partners may predispose one to SSTIs caused by MRSA (877).
Outside the United States, studies have not shown an elevated rate of MRSA carriage in MSM. In Toronto, for example, only 1.6% (8/500) of MSM had asymptomatic carriage of MRSA in the nares or rectum in 2007 (23). No enrichment broth culture was utilized in the processing of culture swabs, which may have decreased their sensitivity compared with that of studies of many other populations. Furthermore, the MRSA epidemic may not have been as widespread in Canada in 2007. More research is needed to assess the reasons for the spread of CA-MRSA in the MSM population.
Veterinarians, Livestock Handlers, and Pet Owners
Domestic pets, livestock, wild birds, and other animals have recently been identified as carriers of MRSA in several countries and settings (Tables 9 and 10). The role of animals as vectors for human MRSA infection and colonization has not yet been fully characterized. It has been suggested that MRSA in animals may be a “humanosis”; this implies that MRSA generally originates from people and puts animals at risk for carriage and infection. Further research is necessary to assess this hypothesis. MRSA isolates obtained from domestic animals often belong to common human MRSA clonotypes (759); in contrast, MRSA isolates obtained from livestock are often genetically distinct.
TABLE 9.
Studies of MRSA carriage and infection in livestock animals and human contacts, 1993 to 2008
| Animals | Yr of study | Location(s) | Major finding(s) | Genotype(s) identifieda | Reference(s) |
|---|---|---|---|---|---|
| Chickens | 2006 | Belgium | Chickens on farms with cloacal or nasal MRSA colonization | ST398-IVa or -V or nontypeable SCCmec/t011, ST398-III/t567 | 663 |
| 2007 | Belgium | MRSA isolated from cloaca or nasal cavity of broiler chicken | spa type t1456, ST398 | 722 | |
| Cows | 2002-2004 | Hungary | Milk samples from cows with subclinical mastitis and tonsillar swab culture of milk industry worker grew MRSA identical by PFGE | ST1-IVa/t127, PVL negative | 451 |
| Horses | 1993-1994 | Michigan | Horses with MRSA wound infections after procedures; 3 health care workers had nasal colonization with MRSA strains related by PFGE | Not stated | 817 |
| 2000-2002 | Ontario, Canada | At a veterinary college and on 10 horse farms, MRSA isolates were obtained from screening cultures of the nares of horses and personnel as well as from sites of clinical infection; this yielded MRSA isolates from 79 horses and 27 personnel; a horse farm worker had the sole human infection; he had an MRSA SSTI complicating a tattoo wound; CMRSA-5 was isolated from him, and MRSA isolates identical by PFGE were recovered from 2 horses under his care | CMRSA-5 by PFGE (related to USA500, carrying SCCmec type IV, spa type t007, PVL negative) accounted for 26/27 (93%) isolates from people and 76/79 (96%) of isolates from horses | 991 | |
| 2004 | Ontario, Canada | A foal with MRSA arthritis and omphalophlebitis and its dam with MRSA nasal colonization were admitted to a veterinary hospital; health care workers who cared for the foal developed MRSA SSTIs, and 10/103 (9.7%) personnel had either nasal or groin colonization with MRSA | PVL negative and identical by PFGE, CMRSA-5 (related to USA500) | 988 | |
| 2004 | Liverpool, United Kingdom | 11/67 (16%) horses at a hospital had MRSA nasal or skin carriage; 3 others had clinical MRSA infections | 12 isolates from 7 horses had 5 PFGE types, all were PVL negative | 41 | |
| 2008 | Hertfordshire, United Kingdom | 2 MRSA infections in horses at a veterinary college hospital | ST398-IVa/t011, PVL negative | 552; A. Loeffler, personal communication | |
| 2003-2004 | Ireland | Horses at 7 veterinary clinics and a hospital with MRSA wound infections or “abdominal granuloma”; horse strains related to those recovered from the nares of attendant veterinary personnel | Unrelated to known clinical isolates held by a large Irish reference laboratory, all with identical or closely related PFGE types | 689 | |
| 2002-2003 | Ontario, Canada, and New York | Farm in Ontario with MRSA colonization in 9/53 (17%) horses and 1/10 (10%) personnel; farm in New York with MRSA colonization of 29/67 (43%) horses and 3/18 (17%) personnel | No information | 986 | |
| Not stated | Vienna, Austria | 2 horses with MRSA wound infections | ST398-IVa/t011 | 1006 | |
| Not stated | Lower Saxony, Germany | Foal with MRSA sinusitis | ST398-V/t1197 | 1006 | |
| 2002-2005 | Ontario, Canada | 69/3,372 (2.0%) horses upon admission to a teaching hospital had nasal MRSA colonization | No information | 987 | |
| 2007 | Belgium | 12/110 (10.9%) horses from Belgium, the Netherlands, France, and Luxemburg seen at a clinic had MRSA nasal colonization | ST398-IVa/t011 (n = 10), ST398-V/t011 (n = 2), and ST398-IVa/t1451 (n = 1) | 932 | |
| 2006-2007 | Vienna, Austria | MRSA infections among 25 horses at a university veterinary hospital; 18/131 (13.7%) personnel had MRSA colonization | Horse strains were ST1-IVa/t127 (n = 3), ST254-IVd/t036 (n = 15), and ST398-IVa/t011 (n = 7), and all were PVL negative; personnel strains were ST1-IVa/t127 (n = 2), ST254-IVd/t036 (n = 13), ST398-IVa/t011 (n = 2), and ST8-IVh/t008, and all were PVL negative | 198 | |
| 2003-2004 | United Kingdom | 9 MRSA isolates from clinical infections of horses | spa-CC8 (n = 8) or related to EMRSA-15 (n = 1); spa types included t020, t036, t064, and t451 | 625 | |
| Pigs | Not stated | France | 5/112 (4.5%) pig farmers carried MRSA in the nasopharynx; none of 27 nonfarmer controls matched by age, sex, and county of residence carried MRSA | ST8 (n = 2), ST5 (n = 1), ST438 (n = 1), and ST398 (n = 1) | 27, 31 |
| 2008 | China | MRSA isolated from dust samples on 5/9 (56%) pig farms in Sichuan Province | ST9/t899 or ST1376/t899, all PVL negative | 965 | |
| 2008 | China | MRSA isolated from nares of 58/509 (11.4%) pigs and 2/13 (15%) pig farm workers in 4 Chinese provinces; none of 276 cattle, 47 cattle workers, or 107 slaughterhouse workers had nasal MRSA carriage | ST9/t899 (n = 46), ST912/t899 (n = 13), and ST1297/t899 (n = 1), all PVL negative | 197 | |
| 2004-2005 | Netherlands | 3 family members on a pig farm (farm A) colonized with identical MRSA strains; at a university medical center, another farmer, a veterinarian, his son, and his son's nurse carried the same strain as above-described family; 1/30 (3.3%) pigs on farm A had perineal carriage of the same MRSA strain; at a meeting of regional pig farmers, 6/26 (23%) were colonized with MRSA in the throat and/or nose | None typeable by PFGE; spa type t108, t567, or t943 | 961 | |
| 2005 | Netherlands | A woman with MRSA mastitis and her daughter had MRSA nasal colonization; 3 family members and 3 coworkers on her pig farm had MRSA throat or nasal colonization, and 8/10 (80%) pigs on the farm had throat, nasal, or perineal colonization | All isolates were ST398-V/spa t108, agr type 1, and PVL and TSST negative | 417 | |
| Not stated | Lower Saxony, Germany | MRSA colonization in 1 pig from a veterinary medical school | ST398-V/t034 | 1006 | |
| 2005-2006 | Netherlands | 209/540 (39%) pigs in 9 slaughterhouses had MRSA nasal colonization; transmission of MRSA both prior to arrival and at slaughterhouses was likely | ST398 with SCCmec type III (n = 4), IVa (n = 41), or V (n = 59); spa types included t011, t108, t1254, t1255, t567, t034, and t943 | 226 | |
| 2005 | Singapore | 1/64 (1.5%) pigs used in exptl research, 1/50 (2%) pigs in a slaughterhouse, and 1/32 (3%) staff workers at an academic hospital's research facilities had MRSA nasal colonization | 2 isolates from pigs were ST398-V; 1 from a pig and 1 from a scientist were ST22-IV | 819 | |
| 2006 | Netherlands | 35/310 (11%) pigs on 7/31 (23%) farms had MRSA nasal colonization; 11 MRSA-colonized personnel had strains with the same genotype as those of pigs on their respective farms | ST398-IV or -V/t011, t108, t567, t899, and t1939, all PVL negative | 940 | |
| 2005 | Denmark | S. aureus nasal carriage in 10/100 (10%) pigs; 1/10 (10%) were MRSA, and 9/10 (90%) were MSSA | All nontypeable by PFGE; spa type t034 (n = 9) or related t1793 (n = 1) | 35, 351 | |
| 2004-2007 | Denmark | Pigs tested after a person working or living on the farm presented with CC398 MRSA (i.e., spa type t034, t108, or t1793) infection or carriage; 23/50 (46%) pigs had nasal carriage of CC398 MRSA | Pigs carried CC398, spa type t034 | 532 | |
| 2007 | Netherlands | On 50 farms, 33/232 (14%) pig farmers and their families had nasal colonization with MRSA, and either pigs had nasal carriage or fomites near pigs were contaminated with MRSA on 28/50 (56%) farms; on 15 farms with nasal colonization in people, animals and people had the same spa type | No information | 931 | |
| 2007-2008 | Iowa and Illinois | In 2 farm systems, 49% (147/299) of swine and 45% (9/20) of farm workers had MRSA nasal carriage | 15 MRSA isolates from animals and workers were all ST398-V, PVL negative | 846; T. Smith, personal communication | |
| Not stated | Ontario, Canada | 71/285 (24.9%) pigs on 20 farms had MRSA nasal or rectal colonization; 5/25 (20%) pig farmers had MRSA nasal carriage; on 5 farms with human colonization, concordant strain types were found in farmers and pigs | 59.2% of pig and human isolates had spa type t034 and could not be typed by PFGE; 10% of pig and 20% of human isolates were USA100 | 471 | |
| 2006 | Netherlands | MRSA SSTIs in 4 piglets on a breeding farm and 20 pigs on a supplier farm; MRSA nasal colonization in 2 farm workers | ST398-IV/t011 | 937 | |
| 2008 | Portugal | 4 pigs and 1 veterinarian from a pig farm had MRSA nasal carriage, and at a second farm, 3 pigs had MRSA nasal carriage | First farm had ST398-V/t011, PVL negative; second farm had ST30-V/t021, PVL negative | 730 | |
| Rabbits | 2002-2003 | Pennsylvania | 1 rabbit with an ear infection | PVL+ | 747 |
| 2003 | Ireland | At a clinic, MRSA wound culture from rabbit and MRSA nasal carriage in veterinary worker | Both isolates had the same PFGE type | 689 | |
| 2003-2004 | Berlin, Germany | Wound infection in a rabbit at a hospital | ST22-IV, PVL negative | 969 | |
| Rats | 2008 | Belgium and Netherlands | 5/40 (12.5%) black rats (Rattus rattus) trapped at pig farms had MRSA throat colonization | ST398/t011 (n = 4) and ST97/t1236 (n = 1), all PVL negative | 930 |
MRSA composite strain genotypes are presented in the following format: MLST type-SCCmec type/spa type. For example, ST398-IVa/t011 indicates a MRSA strain that was ST398 by MLST, carried the SCCmec type IVa element, and was type t011 by spa typing.
TABLE 10.
Studies of MRSA carriage and infection in domesticated and wild animals and human contacts, 1993 to 2008a
| Animals | Yr of study | Location(s) | Major finding(s) | Isolate characteristic(s)b | Reference(s) |
|---|---|---|---|---|---|
| Birds | 2002-2003 | Pennsylvania | Parrot with chronic MRSA sinusitis | PVL+ | 747 |
| 2003-2004 | Berlin, Germany | Parrot with MRSA osteomyelitis | ST22-IV, PVL negative | 969 | |
| Cats | 2003 | Ireland | Cat with MRSA UTI | No information | 689 |
| 2003-2004 | Germany | At a school of veterinary medicine, 2 cats with UTIs and 1 cat with an ear swab that grew MRSA | ST22-IV/t032, PVL negative | 869 | |
| 2002-2003 | Pennsylvania | Cat with an MRSA tooth abscess | PVL+ isolate | 747 | |
| 2000-2004 | Washington State and Quebec, Canada | 2 kittens at a rescue center with rhinitis and an employee there had MRSA nasal colonization; a cat had MRSA UTI, and the genotypically same strain colonized the owner's nose | CMRSA-2 by PFGE, SCCmec type II, PVL negative | 989 | |
| 2003-2004 | Berlin, Germany | 4 cats at a hospital, 1 with MRSA otitis and 3 with MRSA wound infections | ST22-IV, PVL negative (n = 3); Barnim strain by PFGE, SCCmec type IV, PVL negative (n = 1) | 969 | |
| 2002-2005 | Pennsylvania | Clinical syndromes did not differ when 33 MSSA and 13 MRSA isolates from cats (among 11,149 cats treated) at a veterinary medical center were compared | 15 tested isolates had related PFGE types; all carried SCCmec type II | 633 | |
| Not stated | Germany | Pet cat with pharyngeal MRSA colonization; genotypically identical strain caused recurrent SSTIs in its owner | ST80-IV/spa t131 | 839 | |
| 2003-2004 | Ireland and United Kingdom | 6 cats with MRSA infections | EMRSA-15 strain by PFGE; spa types included t022, t032, t379, and t628 | 625 | |
| Dogs | Not stated | United Kingdom, various locations | 210 dogs and cats with MRSA isolated from them | 29/31 isolates tested were EMRSA-15 (n = 25) or EMRSA-16 (n = 4), common pulsotypes in human infections | 759 |
| 1998 | South Korea | MRSA isolates obtained from 12 dogs at a veterinary hospital, with 3 from catheters, 6 from nares, 1 from conjunctiva, 1 from recurrent pyoderma, and 1 from a surgical wound infection | All isolates were MDR; none were susceptible to quinolones, gentamicin, or tobramycin | 698 | |
| 2003-2004 | Pennsylvania | Among 20,366 dogs and 8,026 cats admitted to a university veterinary hospital, 137 animals had S. aureus isolated from them; 39/137 were MRSA isolates obtained from 28 dogs, 8 cats, and 3 unknown animals; isolates were from the skin (n = 11), ear canal (n = 2), genitourinary tract (n = 5), respiratory tract (n = 4), or another site (n = 17) | Minority of isolates susceptible to clindamycin (28%), erythromycin (15%), or fluoroquinolones (10%) | 634 | |
| 2004 | Liverpool, United Kingdom | 3 dogs with MRSA infections, including joint infection, wound infection, and pleuropneumonia; 1 of the 3 had MRSA nasal and fecal carriage; a veterinary student who cared for 1 dog also carried MRSA | All isolates were EMRSA-15 by PFGE and PVL negative | 41 | |
| 2003-2004 | Ireland | 14 dogs at 25 veterinary clinics or a hospital with MRSA isolation, wound (n = 13) and nares (n = 1); veterinary personnel were also tested for nasal colonization | PFGE types of isolates from animals and personnel were common in an Irish reference collection of isolates from human infections | 689 | |
| 2004 | London, United Kingdom | 4/45 (9%) dogs at a veterinary hospital had nostril (n = 2) or buccal mucosa (n = 3) MRSA colonization; 13/78 personnel had MRSA colonization when tested at the same anatomical sites | 4 animal isolates and 7/18 human isolates were EMRSA-15 by PFGE | 551; A. Loeffler, personal communication | |
| 2003-2004 | Germany | 13 dogs with MRSA isolated from them at a school of veterinary medicine; sources were fistula (n = 1), urine (n = 2), implant (n = 1), wound swab (n = 5), joint puncture (n = 2), and skin swab (n = 2) | All isolates were ST22-IV/t032, PVL negative | 869 | |
| 2001 | Missouri | A pet dog carried a strain identical by PFGE to that found in recurrent surgical wound infections of a man and cellulitis in a woman, his owners; the dog was likely a reservoir after colonization from his owners | No further information | 577 | |
| 2003 | Netherlands | A dog and its owner, a health care worker, carried MRSA with a PFGE type identical to that of isolates from a nursing home MRSA outbreak and identified in a dog | No further information | 939 | |
| 1993-2002 | Utrecht, Netherlands | 2 dogs with MRSA infections, wound infection (n = 1) and flank fistula (n = 1) | 2 PFGE pulsotypes | 936 | |
| 2002-2003 | Pennsylvania | 8 dogs with MRSA infections | 5 different PFGE types, all PVL+ | 869 | |
| Not stated | United Kingdom | Pet therapy dog with MRSA colonization in pooled culture of nose, scalp, and interdigital folds of paws; likely acquired colonization during visit to human health care facility; 2 other therapy dogs were not colonized | Related to EMRSA-15, a common PFGE type among hospitalized patients in the United Kingdom | 265 | |
| 2000-2004 | Pennsylvania, New York State, and Ontario, Canada | Reports of a dog with a postoperative MRSA SSTI, and 4/37 (11%) personnel were colonized with the same strain; a dog had an MRSA surgical wound infection, another dog was colonized in the same facility, and 2/22 (9%) clinic personnel carried the same strain; a dog had MRSA infection after ocular surgery and was colonized with the same strain as his owner; and a dog with an MRSA UTI had an owner who was colonized with same strain | All isolates were CMRSA-2, SCCmec type II, and PVL negative | 989 | |
| Not stated | Geesthacht, Germany | A dog with an MRSA SSTI | ST398-V/spa t034 | 1006 | |
| Not stated | Hong Kong, China | 0.72% (6/815) of dogs tested had MRSA nasal colonization | SCCmec type IV (n = 1), type IV new variant (n = 2), and type IIIB (n = 3), all PVL negative | 81, 82 | |
| 2003-2004 | Berlin, Germany | 18 dogs at a hospital with MRSA isolated from them; anatomical sites were wounds (n = 15), dermatitis (n = 1), otitis (n = 1), and cystitis (n = 1) | ST22-IV (n = 15), ST239 (n = 2) with “untypeable” SCCmec and “related to the Barnim clone” with SCCmec type IV (n = 1); all 18 isolates were PVL negative | 969 | |
| 2003-2004 | Adelaide, South Australia | MRSA was obtained from cultures of 2/141 skin lesions in dogs at a 2 veterinary clinics; 0/51 healthy dogs had skin colonization with MRSA | No information | 576; M. Barton, personal communication | |
| 2003-2004 | Ireland and United Kingdom | 27 MRSA isolates from clinical cultures taken from dogs | 96% identical or closely related to EMRSA-15 by PFGE; spa types included t020, t022, t025, t032, t749, t883, t1021, t1041, and t1042 (the t1042 isolates were ST72 by MLST) | 625, 689 | |
| Other | 2003 | Ireland | A seal with an MRSA culture from a lymph node | No information | 689 |
| 2008 | United States | A premature elephant calf with MRSA SSTI; 20/55 previously healthy caretakers in contact with the calf had probable or confirmed MRSA SSTIs | Isolates from the calf (n = 3) and from caretakers (n = 5) were USA300 | 137 | |
| 2003-2004 | Berlin, Germany | A turtle and a guinea pig with MRSA dermatitis at a hospital | Both isolates were ST22-IV, PVL negative | 969 |
UTI, urinary tract infection.
MRSA composite strain genotypes are presented in the following format: MLST type-SCCmec type/spa type. For example, ST398-IVa/t011 indicates a MRSA strain that was ST398 by MLST, carried the SCCmec type IVa element, and was type t011 by spa typing.
Livestock as a reservoir for human MRSA colonization and infection and the ST398 sequence type.
Mounting evidence suggests that livestock, particularly pigs, may represent an important reservoir for CA-MRSA strains that can colonize and infect humans in close contact with them (222, 528, 625, 968, 1013) (Table 9). ST398 is the most commonly reported MRSA sequence type among large livestock in Europe. ST398 MRSA strains often carry genes coding for non-β-lactam antimicrobial resistance, including a plasmid-borne trimethoprim resistance gene, dfrK, identified in an isolate from a pig in Germany (452). These ST398 isolates are often referred to as nontypeable by PFGE because their genome is resistant to SmaI digestion (59). The isolates carry SCCmec type IV or V and typically lack PVL genes; several common spa types have been associated with these isolates.
Studies of asymptomatic MRSA colonization of a variety of farm animals have suggested that carriage rates vary widely. Among 300 healthy horses in Slovenia in 2005, no MRSA carriage was identified (951); a similar finding was obtained for 497 horses on 50 farms in 2006 in the maritime provinces of Canada (112) and for 87 military horses in Austria (year of collection not indicated) (853). In contrast, among 110 horses attending a clinic in Belgium in 2007, 10.9% (12 horses) had nasal colonization with MRSA ST398 strains of two spa types (932). ST398 was also isolated from poultry in Belgium in 2006 (663). In the Netherlands in 2006, MRSA colonization of pigs was identified in 7/31 (23%) tested farms. The ST398 MRSA strains from this study also had a variety of spa types (940).
Several studies have suggested high rates of asymptomatic colonization by ST398 MRSA backgrounds among swine and their handlers, suggesting that frequent transmission occurs, although secondary human-to-human spread to close contacts appears to be rare (199). Moreover, clinical infections among exposed swine farm workers have been reported infrequently. In Iowa, 49% (147/299) of swine and 45% (9/20) of farm workers in 2007 to 2008 carried ST398 MRSA in the nares; no other MRSA genetic backgrounds were identified. Younger swine were more likely to be carriers (846; T. Smith, personal communication). In Austria in March 2008, 13/162 (8%) pig farmers who attended a conference had MRSA nasal carriage, and all eight isolates examined had spa type t034, a type associated with ST398 strains (853). Among 127 farm workers and their contacts on 50 pig farms in Belgium in 2007, 37.8% (48/127) had nasal or skin lesion colonization with MRSA. MRSA carriage was associated with close contact with pigs, dogs, and horses and, paradoxically, with the use of protective clothing. The 48 MRSA isolates belonged to three spa types (t011, t034, and t567), but 94% (n = 45) were t011 isolates. Representative isolates of each spa type were found to share the ST398 genotype (228). In the Netherlands in 2004, >20% of pig farmers were colonized with ST398 MRSA, as were 39% of pigs destined for slaughterhouses; seven spa types were represented, and four predominated (226, 1013). In Austria, 21 of the 1,098 MRSA isolates from humans submitted to a reference laboratory in January 2006 to May 2008 were ST398 isolates. Among these isolates, 5 were obtained from clinical infections, 15 were obtained from cultures to assess colonization status, and the source of 1 was unknown. Of the 19 isolates from patients with information regarding animal exposure, 10 were from pig farmers or their relatives, 6 were from farmers with other animal exposures, and 3 were from people who had no known animal contact. The percentage of ST398 isolates increased in each year of the study and peaked at 2.5% of submitted isolates in January to May 2008 (491).
Invasive infection caused by ST398 occurs but rarely. In Italy, a pig farm worker developed pyomyositis caused by an MRSA ST398 strain. A subsequent investigation of the farm employing the patient revealed colonization by ST398 strains among 1 of 11 other swine workers and family members; ST398 strains were isolated from seven dust samples from farrowing areas on the farm, suggesting a porcine origin of the strains (701).
Although PVL genes have been generally absent from ST398 strains, one report from Sweden described them for isolates from two SSTIs occurring in previously healthy patients in 2006 and 2007. The strains had the t034 spa type, which has been widely reported among PVL-negative ST398 strains (992). Another PVL+ ST398 MRSA isolate (spa type t034 and SCCmec type V) was submitted to the national reference collection of the Netherlands in 2007 (420).
ST398 MSSA strains were also identified by colonization studies of pigs and pig farmers in France but not in a sample of non-pig farmers (27), suggesting that MSSA ST398 strains, like MRSA ST398 strains, are also most closely associated with pigs and pig farm workers. Similarly, MSSA ST398 isolates colonized two pig farmers in Holland and were also isolated from the blood of three elderly hospitalized patients, suggesting again that it may be a virulent clone in humans (928), at least occasionally.
MRSA genetic backgrounds other than ST398 have likely also been transmitted between farm animal handlers and livestock (Table 9). For example, at meat markets and livestock farms in Taiwan in 2004 to 2005, 3 MRSA isolates were isolated from fomites and 27 were isolated from the nares of workers; the most common strain types were ST59, ST338, and a single-locus variant of ST338 (404).
Transmission among swine and swine farm workers of ST398 MRSA strains and the isolation of ST398 strains among MRSA disease isolates from other patients have been studied most carefully in the Netherlands. At a hospital in a region of the country with 7,000 pig farms, screening of health care workers and high-risk individuals who were hospitalized was routinely performed in 2002 to 2006. Seventy-three colonized individuals were identified, 31.5% of whom (23 individuals) carried “nontypeable” MRSA presumed to be ST398 (226, 1013); all of the nontypeable strains were identified in 2004 to 2006. In July to December 2006, a period when a history of direct exposure to pigs or veal calves triggered a screening nasal culture, 19 patients with PFGE-nontypeable MRSA carriage were identified, 87% of whom had previous exposure to pigs or calves. Among MRSA carriers with PFGE-nontypeable strains, clinical infection was less common (13%) than among carriers of PFGE-typeable strains (42%), again suggesting that ST398 may not be as virulent as other genetic backgrounds (945). Among 1,721 health care workers in the Netherlands, MRSA colonization was 10-fold higher (1.7%) among those reporting contact with pigs and veal calves than among those without such contact (0.15%), although this difference was not significant (the time when the study was performed was not stated) (1015). At a Dutch hospital in 2000 to 2006, 26% of 95 patients and health care workers from whom MRSA was isolated likely acquired their isolate from animals. Individuals with animal contact were responsible for the >3-fold annual increase in the rate of MRSA isolation during this period (946). In the 6 months after the introduction of more intensive surveillance programs in July 2006, >21% of all MRSA strains obtained by the national reference center for MRSA in the Netherlands were nontypeable and presumably ST398 strains (943). In 2007, the percentage of MRSA strains that were nontypeable increased to 30.3% (793/2619), with 80% of these isolates having spa type t011 or t108 (420).
In addition to the risk posed to farmers and others working with animals, the general population may be at risk for exposure to MRSA carried by livestock from poor hygienic practices at petting zoos (990). This suggestion requires further investigation.
Veterinary practice as a risk factor for the transmission of MRSA between animals and humans.
Reported rates of asymptomatic MRSA colonization have varied among animals tested at veterinary facilities (Tables 9 and 10). Among 3,372 horses admitted to a veterinary teaching hospital in Ontario, Canada, in 2002 to 2005, 69 (2%) were colonized with MRSA; risk factors for colonization included antimicrobial use in the previous 30 days, previous MRSA colonization or infection, known MRSA colonization or infection in the past on the farm of origin, admission to the hospital's surgery service, or being in a neonatal intensive care unit (987). Among dogs admitted to a Canadian veterinary teaching hospital in 2004, 1/193 (0.5%) carried MRSA recovered from the nares, axilla, and rectum (365).
Several studies suggested that MRSA strains may be transmitted between humans and animals in the veterinary setting (27, 817, 969, 988) (Table 9). The human and animal strains share common genetic backgrounds and were closely related; few differences were identified when comparing the DNA sequences of selected genes of MRSA isolates sharing genetic backgrounds from humans and horses (970). More data are needed to determine if there are genetic differences in MRSA isolates that may be responsible for specific adaptation for the colonization of animals or humans.
Veterinarians, particularly those caring for large animals, have been identified as a high-risk group for asymptomatic MRSA carriage, likely because of their close animal contact. Among 152 Dutch veterinary doctors and students with a history of contact with livestock, a high prevalence (4.6%) of MRSA colonization was documented (the time when the study was performed was not stated) (1014). At a veterinary conference in 2005 in Baltimore, MD, 6.5% (27/417) of tested attendees carried MRSA in the nares, including 15.6% (15/96) of personnel caring for large animals (364). At an international equine veterinary conference in 2006 in San Antonio, TX, 10.1% (26/257) of attendees tested carried one of three pulsotypes of MRSA (USA300, USA100, or USA500). Risk factors for MRSA carriage included a history of caring for a horse with an MRSA infection in the previous year, the attendee having had an MRSA infection in the past year, and self-reported failure to wash hands between farms or between handling of infected animals (20). At an international conference of veterinarians in Denmark in 2006, 12.5% (34/272) carried MRSA in the nares or the throat; 31 of the 34 recovered MRSA isolates were likely ST398 isolates. MRSA carriers came from nine countries (1016; M. Wulf, personal communication). This trend was not observed for the Czech Republic, where, at a veterinary conference in 2008, only 0.7% (2/280) of screened attendees carried MRSA (1024). Similarly, at a university small-animal veterinary clinic in Scotland, 2/64 (3.1%) personnel had nasal carriage of MRSA; both isolates were EMRSA-15 by PFGE analysis, a common strain among human nosocomial infections (382).
MRSA and meat or milk sold for human consumption.
In studies from three continents, MRSA has been isolated from retail meat products (676), from milk and meat samples (478, 497, 519, 538), and from meat industry workers. In the Netherlands, MRSA was isolated from 2 of 79 raw beef and pork samples from retail meat stores in 2006. One isolate was a USA300 strain, and the other was nontypeable by PFGE using SmaI digestion. This isolate may have been an ST398 strain, although sequence typing was not performed (942). In 2007 to 2008, 264/2,217 (11.9%) raw retail meat samples in the Netherlands had recoverable MRSA. Analysis of spa types suggested that 85% of the recovered isolates were ST398 isolates (221). In Austria, 1/82 raw meat products tested carried MRSA with spa type t011 (likely ST398) (the time when the study was performed was not stated) (853). The testing of 120 retail meat samples from grocery stores in Baton Rouge, LA, in 2008 revealed S. aureus on 45.6% of pork and 20% of beef samples. MRSA was isolated from 5% (6/120) of the meat samples. The MRSA strains belonged to the USA300 or USA100 pulsotype (738). There is no current indication that consumers face a risk of MRSA colonization or infection from this source, although studies have not been undertaken to assess this specifically. Further research is warranted to determine if contamination arises from the colonization of animals or of meat handlers.
Household pets.
Although some researchers have suggested that household pets may be an important reservoir for MRSA in the community, there have been few explicit data (Table 10). The transmission of HA-MRSA strains among pets and owners did occur in the pre-CA-MRSA era (126), and after 2000, CA-MRSA strain transmission (790, 938), including USA300 (957) and ST398 (667) strains, has been reported. Among 70 S. aureus isolates from 46 cats treated at a clinic in Philadelphia in 2002 to 2005, all 15 MRSA strains tested carried SCCmec type II, a molecular characteristic of HA-MRSA strains from people (633). This finding suggests that cats may serve as a reservoir of MRSA in humans. In Hong Kong, only 17 of 736 tested dog owners both were colonized with S. aureus and owned a colonized dog. MRSA strains were isolated from 8.2% of the dogs and from 2.3% of the dog owners, but only one dog-owner pair was concordant in MRSA colonization status. Furthermore, only 6/17 of the dog-owner S. aureus isolate pairs shared PFGE types (81), implying that the transmission of S. aureus between dogs and their owners was relatively infrequent despite the high MRSA carriage rate. Some studies have not found any colonization among surveyed pets, for example, among 200 healthy dogs in Europe (951).
Despite this, pets have been anecdotally implicated as a source of human infection caused by MRSA. One outbreak of MRSA in a family was linked to a pet cat. The clearance of ST80 MRSA colonization in a family member with furunculosis did not occur until systemic antimicrobial drug therapy was administered to the cat, which was colonized with the same strain (839).
More research is needed to assess the importance of pets as a reservoir of MRSA in the home and to what degree S. aureus is a zoonosis (853). Few data on the use of antimicrobial drugs among pets in the United States have been collected (544); the overuse of these drugs may increase the risk of MRSA carriage in pets.
CLINICAL MANIFESTATIONS OF CA-MRSA
Patients with SSTIs
Purulent SSTIs caused by CA-MRSA strains are the most common clinical manifestations of CA-MRSA (104, 216, 654). An uncomplicated CA-MRSA SSTI typically presents as an abscess that may resemble a spider bite filled with purulent material (241). Among adults with an abscess and surrounding erythema, the presence of a central black eschar had a positive predictive value of 94% and a negative predictive value of 45% for an MRSA isolate (113). CA-MRSA abscesses can be found in diverse anatomical locations, including the breast (615, 855, 1003), vulva (898), hand after clenched-fist injury (63), and neck (353, 426). However, SSTIs can vary in appearance and can also present as folliculitis, paronychia, furuncle, felon, cellulitis with drainage (628), or lymphadenitis (353). Except for the distinctive appearance noted above, MRSA SSTIs cannot be distinguished from SSTIs caused by other agents, including MSSA (215, 608), on clinical grounds.
Small studies have suggested that the recurrence of CA-MRSA SSTIs is common after treatment. In Dallas, a recurrent CA-MRSA SSTI was documented at a distinct anatomical site within 2 years of the index CA-MRSA infection in 11/41 (27%) HIV-infected patients (842). A recurrence of 1 to 3 CA-MRSA (i.e., onset outside the health care setting) SSTIs at a distinct anatomical site occurred among 5 of 11 adult HIV-infected patients in Chicago in 2003 to 2004; the intervals between index lesions and recurrences were not stated (19). Among 87 MSM in New York City who presented with a CA-MRSA (i.e., onset in the community) SSTI, 31% had a recurrence within 6 months after the resolution of the initial infection. Recurrence rates among those receiving MRSA-appropriate and MRSA-inappropriate initial antibiotic therapy (21/63 versus 6/20) were similar (825, 840). Among 61 patients with a CA-MRSA SSTI presenting to a New York City clinic in 2004 to 2006, 41% had one recurrence and 18% had more than one recurrence within 25 months; the median time to recurrence was 1 month. The likelihood of recurrence was not significantly different among HIV-infected patients, recipients of TMP-SMX prophylaxis, individuals with MRSA nasal colonization, or recipients of mupirocin for nasal decolonization (743). At a Boston clinic at which approximately 70% of patients self-identified as being MSM, in a 16-month period in 2005 to 2007, 9.2% (73/795) of patients developed an SSTI: 31/73 (43%) of the SSTIs were cellulitis, and 26/73 (36%) were furuncles. Of the SSTIs, 56% (41/73) were cultured, and 22/41 (54%) grew MRSA. Of those with an SSTI, 20% (16/73) developed a recurrence; culture data from recurrent lesions were not reported, so the proportion of recurrent lesions caused by MRSA was unknown. The authors of that study did not report whether antibiotics chosen for the treatment of the initial SSTIs were known to be active against the isolates obtained from the initial SSTIs (877).
SSTIs caused by MSSA also recur but less frequently than those caused by MRSA. Among detainees at the Cook County Jail in Chicago in 2004 to 2005, 14% of patients with an MRSA SSTI and 8.8% of patients with an MSSA SSTI had a recurrence within 6 months (215). Among 31 HIV-infected patients with a CA-MRSA (CDC criteria) SSTI in 2000 to 2007 at an HIV clinic in San Diego, 14 (41%) had a recurrent SSTI at a distinct anatomical location a median of 4 months after the index lesion. Culture results were available for only some recurrent lesions; of 14 patients with a CA-MRSA index SSTI and a recurrence, 7 (50%) had a culture-confirmed CA-MRSA SSTI recurrence. Recurrence was associated with an HIV viral load of >1,000 copies/ml (OR, 0.14; P = 0.03 for patients with a viral load of <1,000 copies/ml), and there was a trend for an increased risk of recurrence if an incision-and-drainage procedure was not performed for the index CA-MRSA SSTI (OR, 0.19; P = 0.07) (195).
Why recurrent CA-MRSA SSTIs are common is not known. Immunity after an initial MRSA SSTI would seem to be absent in patients with a recurrence. The mechanism by which recurrence occurs is unclear. Possibilities include reinfection from persistent asymptomatic CA-MRSA carriage or reinfection after acquisition from environmental MRSA contamination or after new MRSA acquisition from close human or animal contact.
Invasive Infections and Necrotizing Pneumonia
Severe, invasive CA-MRSA disease in previously healthy patients has been reported from many centers. “New” staphylococcal syndromes have been recognized in association with CA-MRSA isolates, suggesting that CA-MRSA genetic backgrounds and, possibly, the corresponding MSSA genetic background may carry novel virulence genes, a combination of virulence factors absent in many MSSA strains, or an upregulation of widely prevalent virulence factors (204) (Table 11).
TABLE 11.
Reported invasive CA-MRSA infections in 1998 to 2009
| Type of infection or syndrome | Reference(s) |
|---|---|
| Brain abscess | 470, 546, 835 |
| Cavernous sinus thrombosis | 641, 651, 789 |
| Diarrhea and shock | 9 |
| Endocarditis | 38, 292, 367, 522, 728 |
| Epidural abscess | 103 |
| Fournier's gangrene | 111, 457 |
| Iliopsoas abscess, postpartum or otherwise | 850, 993 |
| Lemierre's syndrome | 60, 72 |
| Mediastinitis, mediastinal abscess | 118, 1009 |
| Meningitis | 641, 808, 960, 971 |
| Orbital cellulitis | 789, 948 |
| Acute osteomyelitis | 159, 379, 439, 467, 513, 584, 677, 791, 815, 821, 971 |
| Necrotizing conjunctivitis | 100 |
| Necrotizing fasciitis | 7, 17, 87, 159, 224, 379, 523, 525, 609, 911, 1021 |
| Necrotizing pneumonia | 3, 86, 96, 99, 102, 124, 141, 159, 189, 190, 247, 305, 312, 320, 321, 322, 331, 355, 372, 396, 429, 540, 564, 583, 590, 602, 614, 618, 669, 677, 719, 720, 763, 781, 804, 848, 858, 870, 906, 907, 917, 925, 926, 1028 |
| Prostatic abscess | 724 |
| Purpura fulminans | 488 |
| Pyomyositis | 7, 296, 354, 415, 467, 527, 545, 584, 701, 705, 826, 971 |
| Retropharyngeal abscess | 288 |
| Septic arthritis | 415, 564, 584, 720, 736, 857 |
| Septic thrombophlebitis or so-called “pelvic syndrome” | 330, 467, 677, 870 |
| Sepsis, severe sepsis | 6, 30, 124, 133, 159, 179, 192, 262, 360, 571, 603, 621, 720, 857, 887, 917, 1011 |
Necrotizing fasciitis, necrotizing pneumonia, severe sepsis, and septic thrombophlebitis of large veins such as the iliac or femoral veins caused by S. aureus were rarely reported for healthy individuals prior to the emergence of CA-MRSA. However, there are now many reports of such infections (Table 11). For example, Miller et al. described 14 adults with necrotizing fasciitis caused by MRSA at the University of California at Los Angeles (UCLA) in 2003 to 2004, 4 of whom had no preexisting medical comorbidity. The five available isolates were USA300 and PVL+ and carried SCCmec type IV (609).
Severe, invasive CA-MRSA infections have a high mortality rate, even when optimal therapeutic regimens are used. For example, the mortality rate for eight children with CA-MRSA sepsis at Vanderbilt University Medical Center in Tennessee was 50% (124). While many invasive syndromes have been described (Table 11), this discussion will focus on necrotizing pneumonia.
CA-MRSA necrotizing pneumonia is a distinct syndrome of hemoptysis, leucopenia, high fever, and cavitary lung lesions upon radiography, often requiring mechanical ventilation. While infrequent, there is some evidence that the incidence of this condition may be increasing. Among inpatients at 59 U.S. hospitals in 2002 to 2003, MRSA was the etiology of 15.9% of pneumonias and 8.9% of community-acquired pneumonias; a case of pneumonia was defined by the presence of a billing code for pneumonia in administrative data and a concomitant positive respiratory bacterial culture (485). Cases of necrotizing MRSA pneumonia have often been linked to antecedent respiratory viral infection, particularly influenza (3, 96, 729, 906). The clinical presentation of CA-MRSA necrotizing pneumonia is reminiscent of rapidly progressive influenza cases during the 1918 influenza pandemic caused by S. aureus superinfection (167). Indeed, recent studies have suggested that most deaths related to the 1918 influenza pandemic were due to complicating bacterial pneumonia (101, 631). In 2009, in the first two waves of the worldwide pandemic of H1N1 2009 influenza A virus, several published series included cases of MRSA pneumonia complicating influenza in previously healthy people in the United States (129, 144, 320) and Australia (646). More data are needed to define the interaction of influenza virus and S. aureus in the human respiratory tract.
Necrotizing pneumonia often has a rapidly progressive, fatal course and occurs most often in children and young adult patients. Gillet et al. reported 16 cases of community-acquired S. aureus pneumonia caused by PVL+ strains in France in 1986 to 1998 with a mortality rate of 63% (321). In a statewide surveillance of severe CA-MRSA (CDC criteria, except that health care exposures were “not recent”) infections in 2005 to 2007 in Georgia, 101/1,670 (6.1%) patients had MRSA pneumonia, 29/101 (29%) of whom died. Controlling for age, patients with MRSA pneumonia had an odds ratio of dying of 11.34 (95% CI, 5.59 to 22.98; P < 0.001) (1000) relative to other patients with severe CA-MRSA infections. Among 50 cases of necrotizing community-acquired pneumonia caused by PVL+ S. aureus strains in 1986 to 2005, the mortality rate was 56%, and the median age was 14.5 years. Death was independently associated with “airway bleeding,” erythroderma, and leucopenia. A focal staphylococcal infection elsewhere, prior to the onset of pneumonia, was associated with decreased mortality (322). Anecdotal reports and series such as this report suggest that CA-MRSA lung infections resulting from hematogenous spread may have a lower case fatality rate than primary MRSA pneumonia.
During the 2003-2004 influenza season, 248 cases of secondary bacterial infection were reported among 13,560 laboratory-confirmed cases of influenza in the United States. S. aureus was the most commonly identified pathogen in these cases (44/248 [17.7%] S. aureus versus 32/248 [12.9%] S. pneumoniae isolates), and the majority of the S. aureus isolates were MRSA for both adults (24/31) and children (7/13) (729). Among children, 40 state health departments reported 153 deaths from influenza in 2003 to 2004. Among the 102 cases with adequate data, 24 (24%) had a coinfecting bacterium; nearly half (11 cases; 46%) were S. aureus. Six of the 10 S. aureus isolates for which data were available were methicillin resistant (67). In the largest series to date, 51 cases of S. aureus pneumonia were reported to a U.S. Emerging Infections Network survey in 2006 to 2007. Of the 47 isolates with known susceptibility, 37 (78%) were MRSA isolates, and the median patient age was 16 years. Thirty-three percent of those tested had concomitant influenza virus infection, and 51% (24/47) of the patients died a median of 4 days after the onset of symptoms. Leucopenia was independently associated with death. Of the 17 MRSA isolates available, 16 were USA300, and 1 was a PVL-negative USA100 isolate (455). In Atlanta in 2006 to 2007, 7/65 (11%) children admitted to hospitals with influenza had a simultaneous S. aureus infection, most of which were MRSA (5/7) and most of which were pneumonia (5/7). An additional seven children had simultaneous respiratory syncytial virus (RSV) and S. aureus infections (751).
The pathogenesis of these severe CA-MRSA infections, such as pneumonia, sepsis, and septic thrombophlebitis, requires further research to define high-risk populations, to identify host genetic characteristics that increase susceptibility to infection, to assess the importance of antecedent colonization with MRSA as a risk factor, and to devise methods to prevent these devastating clinical syndromes.
TREATMENT OF CA-MRSA INFECTIONS
Uncomplicated SSTIs
Reviews and guidelines of therapy for CA-MRSA SSTIs abound (209, 335, 341, 516, 616, 735), although there have been few controlled studies. The choice of empiric therapy for CA-MRSA SSTIs requires the clinician to distinguish between uncomplicated SSTIs and severe or complicated SSTIs (209). Uncomplicated SSTIs are not accompanied by systemic signs that indicate a potential for rapidly progressive clinical decline and a lack clinical features of complicated SSTIs, including a large or rapidly growing lesion or a lesion with deep tissue penetration. A systemic inflammatory response syndrome and leucopenia are absent. Host characteristics such as immunocompromise, age younger than 6 months, lack of a reliable site for outpatient follow-up care, or poorly controlled comorbid conditions may dictate the need for hospitalization (209).
In a region or a population with a high prevalence of CA-MRSA, e.g., where >10% of clinical S. aureus isolates are MRSA isolates, β-lactam antibiotics are no longer reliable for empiric therapy. For small, uncomplicated CA-MRSA skin abscesses (i.e., those <5 cm in diameter), when reliable follow-up is available, incision and drainage may be adequate without antimicrobial drug therapy (362). This contention is supported by studies in which patients received MRSA-inappropriate antimicrobials for MRSA SSTIs and, nevertheless, did well. In 2002 to 2003 in Dallas, 58/62 (94%) children with SSTIs treated with an MRSA-inappropriate antimicrobial (i.e., antimicrobial drugs to which the cultured isolate was not susceptible in vitro) had improvement at a 1- to 6-day follow-up: 37/62 (60%) patients continued on the original drug regimen, while 21/62 (34%) patients were changed to an MRSA-appropriate agent; no difference in outcome was observed (520). Similar results were found by uncontrolled studies conducted with adults treated with MRSA-inappropriate antimicrobials in 11 geographically diverse U.S. emergency departments in 2004 (628) and among patients treated at a clinic for SSTIs in San Francisco in both 2000 to 2001 (718) and 2004 to 2005 (744). In 2004 to 2005, a subset of 166 outpatients attending a San Francisco wound clinic were randomized after incision, drainage, and packing of a skin abscess >2 cm in diameter to receive cephalexin or placebo. Although 87.8% of isolates from the study subjects were MRSA isolates, high cure rates did not differ significantly at 7 days for those treated with cephalexin (84.1%) and those treated with placebo (90.5%) (744).
MRSA-appropriate antimicrobial therapy appears to be important, however, for the treatment of at least some SSTIs caused by CA-MRSA strains, as suggested by a retrospective study of two hospitals in Arkansas. Treatment failure occurred for 5% of 312 patients with a CA-MRSA SSTI in 2003 to 2006 when MRSA-appropriate therapy was used within 48 h of presentation but occurred for 13% of 219 patients with SSTIs when MRSA-inappropriate therapy was used (P = 0.001). Incision and drainage were performed for 80% of the patients at the index visit. The difference in the rate of treatment failure was significant even when included in a logistic regression model with many other potential predictors. It is not clear if patients received therapy with a single antimicrobial or multiple agents (784).
Although some researchers have reported worse outcomes for CA-MRSA than for CA-MSSA infections, SSTIs caused by MRSA with onset in the community did not have worse outcomes than those caused by MSSA in Los Angeles in 2004 (607).
There is no consensus as to which patients can be treated with incision and drainage alone and which patients require adjunctive antimicrobial therapy (334). Readers of the New England Journal of Medicine demonstrated that U.S. providers polled to recommend treatment for a college athlete with a 5- by 3-cm buttock SSTI differed in their preferred initial management: among the 11,205 respondents, 41% advocated drainage and an antimicrobial agent active against MRSA, 31% advocated drainage alone, and 28% advocated drainage and an agent active against MSSA (149, 358).
Initial empiric antimicrobial therapy, when given, must be chosen in accordance with local institutional antibiotic susceptibility data. In geographic regions with a high prevalence of CA-MRSA, a sample of the purulent material should be sent for culture and susceptibility testing. Antimicrobials such as clindamycin, doxycycline, minocycline, and trimethoprim-sulfamethoxazole (TMP-SMX) are often recommended for empiric treatment, although randomized clinical trials have not been conducted to evaluate or compare these therapies for CA-MRSA; such trials were, however, initiated in 2009 under the sponsorship of the NIH. As always, therapy should be adjusted to target the culture and antimicrobial susceptibility results when available.
Clindamycin remains a mainstay of therapy for uncomplicated CA-MRSA SSTIs in much of the United States, although some researchers have suggested that resistance may be increasing among CA-MRSA strains (235, 361). Despite heavy use, however, the rate of clindamycin resistance changed little at a Baltimore pediatric ED: 96% of 217 MRSA isolates in 2003 to 2005 were susceptible to clindamycin, similar to the percent found in 2002 to 2003 (874). A group from Baylor University in 2000 to 2002 found in an uncontrolled study that clindamycin was effective for invasive community-onset MRSA infections of children (585). Although it is often associated with a successful outcome in therapy for SSTIs, concern has also been raised about the risk of Clostridium difficile-associated diarrhea (696) with clindamycin therapy. When an S. aureus isolate is susceptible to clindamycin but resistant to erythromycin, inducible resistance to clindamycin should be assessed by the D test, as recommended by the Clinical and Laboratory Standards Institute (661).
TMP-SMX is also favored by many experts for the treatment of CA-MRSA SSTIs. However, it may be ineffective against cellulitis or other SSTIs caused by group A streptococci, and therefore, treatment failure may occur in this situation, although few explicit data are available. Allergy to sulfa drugs or renal failure can preclude its use. Furthermore, there is a theoretical risk of treatment failure of antifolate drugs in the presence of pus because the presence of large amounts of released thymidine from tissue damage may abrogate the effect of these agents (737). A randomized, placebo-controlled study of pediatric patients with an SSTI in an ED in St. Louis, MO, in 2006 to 2008 demonstrated that incision and drainage with subsequent oral placebo (4/76; 5.26%) were noninferior to incision and drainage with a 10-day course of TMP-SMX (3/73; 4.11%). Eighty percent of the lesions grew MRSA, and 100% of the isolates were susceptible to TMP-SMX (251). Investigators at Fenway Clinic in Boston reported that TMP-SMX was used to treat more than 76% of MRSA SSTIs in 2005. In a retrospective study, in 1998 to 2005, they found that therapy using an agent to which causative MRSA strains were susceptible (commonly TMP-SMX) was associated with a higher odds of clinical resolution of MRSA SSTIs in a multivariate logistic regression model (876). A retrospective study of children admitted to Texas Children's Hospital in Houston in 2004 to 2005 for CA-MRSA SSTIs (no hospitalization in the previous year, no indwelling catheters or percutaneous devices, and no chronic medical conditions that predispose one “to hospitalization or frequent medical visits”) compared outcomes among those who received oral TMP-SMX and those who received clindamycin therapy prescribed at discharge. Patients with concurrent, invasive MRSA infection were excluded. Among 215 and 200 children receiving TMP-SMX and clindamycin, respectively, there was no difference in the percentages of patients returning to the hospital for a worsening of the index lesions. However, more patients treated with clindamycin had undergone surgical drainage prior to discharge (93.5% versus 86%; P = 0.0003), potentially biasing the outcome in favor of clindamycin treatment (424).
Limited data are available to document the efficacy of doxycycline or minocycline in the treatment of an MRSA SSTI after incision and drainage (783); like TMP-SMX, these agents are unlikely to be useful when there is a high suspicion for group A streptococcal infection. In an underpowered, small, open-label study of outpatients in 2005 to 2006 at an ED in Dallas, TX, 34 patients with an SSTI (23 with MRSA, 4 with MSSA, 2 culture negative, and the remaining 5 with coagulase-negative staphylococcus, Corynebacterium species, Streptococcus milleri, or “gastrointestinal flora”) were randomized to receive TMP-SMX or doxycycline. Fourteen patients with an SSTI (8 of whom had MRSA) were randomized to receive TMP-SMX, and 20 patients (15 of whom had MRSA) were randomized to receive doxycycline; one patient in the TMP-SMX group was lost to follow-up. In an intention-to-treat analysis, no significant difference in the failure rate was found (3/14 [21%] in the doxycycline group and 0/19 [0%] in the TMP-SMX group; reported as a P value of 0.28) (127).
Oral therapy with linezolid, a bacteriostatic oxazolidinone, is effective in treating patients with an SSTI; resistance to linezolid among MRSA isolates has been reported with prolonged use (66) but is rare with short-term use. The use of linezolid is limited by high cost, limited availability of the suspension, the occurrence of thrombocytopenia with prolonged use, and the availability of less-expensive, effective oral antimicrobial drugs.
Certain antimicrobial drugs should be avoided as therapy for MRSA SSTIs despite susceptibility documented by laboratory testing. FQs are an important example. Resistance to FQs is common (628), and the rate of resistance of S. aureus increases rapidly with exposure. Resistance emerging during FQ therapy was related to the duration of therapy and dosing in an in vitro model (884). Rifampin should also not be used as a sole agent in the therapy of CA-MRSA infections because of the high rate of emergence of resistance (335).
Severe Infections
Invasive CA-MRSA infections, such as bacteremia, pneumonia, and osteomyelitis, when suspected, usually require hospitalization and therapy with intravenous antibiotics (209). Although guidelines and reviews have been reported (47, 341, 658, 677), evidence to guide therapy remains scarce. Appropriate cultures are essential and should be obtained prior to the initiation of empiric antibiotic therapy. Antimicrobial therapy for such severe CA-MRSA infections is generally the same as that for invasive HA-MRSA infections (781). Vancomycin is still the primary agent used for suspected invasive CA-MRSA infections; it is generally well tolerated and has few adverse effects. Concerns have been raised about its poor penetration into lung tissue, underdosing, reported treatment failure in cases of necrotizing pneumonia caused by PVL+ CA-MRSA strains (984), increasing low-level (intermediate) resistance (389, 542), and “MIC creep” (549, 795, 892). It is not known if alternative initial antibiotic choices would improve the often fatal outcome of severe, invasive CA-MRSA infections with their rapid, progressive clinical tempo (209, 298).
The efficacy of parenteral TMP-SMX for the therapy of invasive CA-MRSA infections has received little study. Among 100 IVDUs with severe S. aureus infections randomized to receive intravenous vancomycin or TMP-SMX, the cure rates, 57/58 (98%) for vancomycin and 37/43 (86%) for TMP-SMX, differed insignificantly; 47% of the patients had MRSA infections (581). That study was performed before the CA-MRSA infection era. Also, the study may have lacked adequate power to demonstrate a difference, as the authors themselves admitted, but the data suggest that intravenous TMP-SMX deserves additional evaluation.
The adjunctive use of an antimicrobial agent interfering with bacterial protein synthesis, such as clindamycin or linezolid, is sometimes advocated for a CA-MRSA infection in which toxin-mediated pathogenesis is suspected, although there is limited evidence to support this approach (250, 602). Such adjunctive therapy may be particularly valuable for intravascular infections when viable organisms are expected for several days despite therapy. The theoretical basis for this approach rests on the hypothesis that ribosomally active antibiotics decrease toxin production more rapidly than other antibiotics. The in vitro exposure of MRSA isolates to a subinhibitory concentration of β-lactam antibiotics increased the expression of toxin genes, including those for PVL, alpha-toxin, and toxic shock syndrome toxin 1 (TSST-1). In contrast, the use of clindamycin or linezolid decreased the production of these toxins (862).
Several newer antistaphylococcal agents are available for parenteral therapy, including daptomycin, linezolid, tigecycline, and quinupristin-dalfopristin. Daptomycin, which is bactericidal and can be administered once daily to patients with normal renal function, has been shown to be effective against MRSA SSTIs (24) and has been used in adults with bacteremic infections. In a randomized, controlled trial with adults, daptomycin was noninferior to vancomycin for the therapy of right-sided S. aureus endocarditis, although treatment failures occurred due to the emergence of daptomycin resistance during therapy (297). Daptomycin is not useful for pneumonia because it is inactivated by pulmonary surfactant (836). Although it is generally well tolerated, patients require weekly creatinine kinase testing to monitor for rhabdomyolysis, a rare but potentially serious adverse reaction (122). Safety and efficacy data are lacking for pediatric patients.
Tigecycline, a glycylcycline antibiotic chemically related to minocycline, has been approved for use in patients with intra-abdominal infections and MRSA SSTIs (776, 859) and is safe and effective for the therapy of complicated MRSA SSTIs in hospitalized patients, with a cure rate similar to that of vancomycin (78.6% versus 87.0% in a microbiologically modified intention-to-treat analysis) (290). This static agent is dosed twice daily intravenously; common adverse reactions include nausea, vomiting, and abdominal pain (290, 859). Tigecycline is not appropriate for children younger than 8 years of age.
Linezolid is well suited for the therapy of MRSA respiratory infection because of its excellent penetration into the lung, and it may be an appropriate choice especially in cases in which the MIC of vancomycin is high (844). Reports of linezolid resistance with prolonged use have occurred (599).
The use of the streptogramin antibiotic combination quinupristin-dalfopristin is sometimes limited by severe, reversible arthralgias as well as nausea, diarrhea, vomiting, conjugated bilirubinemia, and rash that occurs with prolonged use (782). Resistance of S. aureus has been reported (242, 562).
Two newly developed cephalosporins, ceftobiprole and ceftaroline, which differ from other β-lactam antimicrobials in their high affinity for PBP2a, show promise as agents effective against MRSA (172, 725, 1025). They have not been licensed for use in the United States. The novel glycopeptides dalbavancin (772), telavancin (155), and oritavancin (734) inhibit cell wall synthesis like vancomycin. Telavancin, which was approved by the U.S. Food and Drug Administration (FDA) in September 2009, also causes a depolarization of the bacterial cell membrane, theoretically enhancing its bactericidal effect (155). The main advantages of dalbavancin and oritavancin over vancomycin may be their long half-lives, which allow for infrequent dosing (927). No data for efficacy or safety in children are available for these novel agents.
One case report (360) and one in vitro study (314) suggested that intravenous immunoglobulin (IVIG) may be an effective adjunctive therapy for sepsis caused by PVL+ CA-MRSA, but further study is needed to validate this observation (658). Infectious foci should be drained, and necrotic tissue should be debrided when feasible (7, 87, 159, 224, 379, 523, 525, 609, 1021).
PREVENTION OF CA-MRSA INFECTIONS
Infection control practice in the health care setting relies on guidelines from professional and governmental bodies (177, 341, 834). The standard hospital guidelines regarding MRSA prevention stress that “antibiotic-resistant pathogens are sensitive to routinely used hospital disinfectants, but it is essential that correct and meticulous cleaning and use of disinfectants be performed” (648). With few exceptions (408), however, most specific interventions, including the isolation or cohorting of colonized individuals, active identification of MRSA carriage by surveillance cultures of high-risk populations, decolonization of MRSA carriers, environmental disinfection by chemical means or even light (568), or some combination of the above-described interventions, have failed to reliably limit transmission or spread (557). Even with this uncertainty, in community and other institutional settings, there is far less evidence to support the use of these approaches, and as the CA-MRSA epidemic continues, the need for effective interventions has become more acute.
MRSA Recovery from Fomites
Many researchers have found MRSA in the environment outside the health care setting, but the relevance of its presence on fomites to human colonization and infection is not clear. A variety of MRSA genotypes has been isolated from seawater at recreational beaches in Hawaii (818) and beaches in California and Washington State (849); it has been recovered from coins in the presence of pus and blood, although MRSA could not be recovered from clean coins within 4 h of initial contamination (904). In Boston, S. aureus was recovered from fomites in 34/35 homes of healthy individuals with a child in diapers and a cat or dog in the home; MRSA was recovered from fomites in 9/35 homes. MRSA was recovered from sinks, countertops, faucet handles, dish sponges, pet food dishes, infant high-chair trays, and others (812). Efforts to eradicate the colonization of health care workers in Germany in 1995 to 2001 succeeded only when household contacts and heavily contaminated fomites in the homes of the health care workers were disinfected (483), suggesting that fomites may constitute important environmental reservoirs. Specific fomite materials have not been tested extensively for the survival of MRSA. Evidence from one study suggests that MRSA survives poorly on copper surfaces compared with stainless steel (678), but there are no studies available on the replacement of metal surfaces with copper in the community.
It is clear that MRSA environmental contamination is common, at least in the hospital (370) and, from case reports, in the community as well. MRSA can spread from person to person via direct casual contact or from the contamination of inanimate objects (88, 588). However, the importance of environmental contamination in MRSA transmission remains uncertain. Spread between patients and environmental surfaces may occur rapidly. Environmental contamination with MRSA occurred within 24 h of admission of two ICU patients with an MRSA infection in a hospital in England; the rooms had been cleaned with a hydrogen peroxide aerosol prior to the admissions (371). MRSA can survive on objects such as dry mops for up to 4 weeks (686); paper and foil wrappings of sterile hospital goods for more than 38 weeks (238); plastic charts, a laminated table, and polyester cloth curtains for more than 1 week (407); and mattresses for months (662). MRSA can also be recovered from hospital ventilation systems (187, 495), chiropractic adjusting tables (70), computer keyboards, pagers (52), and faucet handles (108). In a Japanese hospital, MRSA was isolated from sinks, floors, bed sheets, and the air in a surgery ward. The number of CFU of MRSA detected from air samples increased more than 50 times during the changing of bed linens, although the significance of airborne MRSA in transmission is not known (830).
Even reportedly rigorous cleaning may not be effective in eradicating MRSA contamination of fomites. At a hospital in the United Kingdom, in 46% of rooms formerly housing MRSA-infected patients, cultures of mattresses, pillows, chairs, lockers, bed wheels, commodes, bed frames, nurse call buttons, a television set, floors, window sills, or door handles still grew MRSA despite “terminal” cleaning (75).
Limited evidence from studies in the health care setting indicates that environmental contamination can lead to human colonization and disease with MRSA (370), although much of the data are only suggestive. At a Baltimore, MD, outpatient infectious disease clinic in 2004, two health care workers developed MRSA SSTIs. Seven of 36 environmental cultures tested grew MRSA. All seven isolates carried the SCCmec type IV element and the genes for the PVL toxin (448). After a pediatric ICU MRSA outbreak in Taiwan, investigation revealed that 26.2% of health care workers were colonized with MRSA. Some of the health care workers carried the same MRSA clone that was isolated from patient infections and from a fomite; other health care workers carried different MRSA clones (539). In a dermatology ward, it was deemed likely that the contamination of hospital equipment with MRSA and borderline methicillin-resistant S. aureus led to 13 infections (514). Dutch investigators isolated a strain of MRSA from a physician's office floor that may have been the source of his nasal recolonization (966). A hospital outbreak of MRSA in a general surgical ward in the United Kingdom was contained only after an aggressive environmental cleaning program was instituted. This included the formation of a new infection control team that met monthly, sequential closure of each part of the ward for thorough cleaning, dust traps being removed from around radiators, ventilation ducts being cleaned, the hours of weekly person-cleaning time being increased from 66.5 to 123.5 h, curtains being laundered every 6 months at a minimum, and several other interventions. Of 673 environmental cultures obtained from hospital rooms before and after an intervention, 10.7% grew MRSA. Among MRSA isolates from male patients housed in these rooms, 55 had an identical PFGE type, the same type shared by all but 1 of 58 environmental isolates tested (746). A study of an ICU showed that the attributable risk for the acquisition of MRSA infections from occupying a bed previously occupied by a patient who was colonized by or infected with MRSA accounted for only 5.1% of MRSA cases in the ICU (409).
MRSA SSTIs and MRSA gastrointestinal colonization (89) in the health care setting may be more likely to produce environmental contamination than either other MRSA infections or colonization. In a study from a Rhode Island hospital, 36% of tested surfaces (including patient gowns, nurses uniforms, beds, blood pressure cuffs, over-bed tables, floors, linens, and door handles) were contaminated in rooms of patients with skin or urine infections with MRSA, whereas only 6% of surfaces were contaminated in rooms of patients with MRSA infections at other sites (88). A study of a nursing home showed rare environmental contamination by MRSA, despite a high prevalence of nasal colonization among its patients and despite the fact that 10% of patients newly acquired MRSA asymptomatic colonization while at the nursing home (91). This finding suggests that when active infections are rare, even in the presence of a high prevalence of asymptomatic colonization, environmental contamination may be uncommon.
Chlorhexidine Gluconate and MRSA Decolonization
Chlorhexidine gluconate (CHG) is a skin antiseptic in use in the health care setting since the 1950s with many potential applications for infection control, as discussed in a recent review (612). CHG is bactericidal for several pathogenic bacteria (787), including MRSA (74, 458, 503). However, bacteria, particularly Gram-negative bacteria, can develop resistance to CHG (98) that may increase with increased CHG use (979). It has not been used widely or studied rigorously in community settings, although it is often recommended by decolonization protocols for patients with recurrent MRSA infections. It is also commonly used for preoperative bathing for surgical procedures, although a systematic review of randomized trials in the literature in 2006 showed no decrease in surgical-site infections in the hospital after preoperative antiseptic bathing; all six trials compared CHG with no intervention or bar soap (985).
In the health care arena, CHG is safe (464) and provides a “residual effect” that continues to kill pathogens for up to 48 h after application to the skin (558). CHG has been used successfully to limit the spread of vancomycin-resistant enterococci (VRE) in an medical intensive care unit (953), to prevent catheter infections (73, 531), and for hand disinfection (964). Universal CHG baths as part of a multifaceted intervention, including the screening of all admitted patients for nasal colonization, isolation of colonized patients, and rotating universal use of three intranasal antimicrobial ointments, was successful in decreasing MRSA infections in one ICU in the United Kingdom; the independent effect of CHG is not known (342). In one hospital study, the use of CHG baths alone was associated with a loss of MRSA colonization in 9 of 50 patients (369). An aggressive decolonization regimen applied to 87 patients in a randomized trial of CHG washes, mupirocin nasal ointment, and oral rifampin and doxycycline for 7 days yielded 74% decolonization 3 months later, compared with 32% among 25 untreated patients. At 8 months, 54% of the treated group remained free of MRSA colonization; again, however, the independent effect of CHG is not known (837).
It is not certain that evidence derived from the health care setting can be applied to CA-MRSA isolates in other arenas. One study of chlorhexidine skin cleaning in a large cohort of soldiers did not show an effect on decreasing the incidence of SSTIs (997).
Mupirocin
Inside and outside the health care setting, mupirocin has long been used for the attempted decolonization of patients colonized by S. aureus, but the efficacy data are conflicting (713, 749) A 2008 review of four randomized, controlled trials showed a significant decrease in rates of postsurgical infections among S. aureus-colonized patients receiving mupirocin compared with either placebo or no treatment (3.6% versus 6.7%; RR, 0.55; CI, 0.34 to 0.89) (944). Another review in 2003 found no evidence to support the general practice of using topical or systemic antimicrobial therapy to decolonize people with MRSA in the nose or elsewhere on the body (550).
Few systematic studies of mupirocin to decolonize MRSA carriers have been attempted in the community. At a Texas Army base in 2005, 3,447 soldiers attending classes were randomized into two groups. All were screened for MRSA colonization. Those colonized with MRSA received mupirocin or placebo. A cotton-tipped applicator was used to apply 2% mupirocin ointment or placebo twice daily into the nasal vestibule for 5 days. Although mupirocin was effective at decolonizing 58 of 66 (87.9%) colonized soldiers compared with 42 of 65 (64.6%) colonized soldiers receiving placebo in a 16-week follow-up period, the incidence rates of MRSA skin infections were similar for the two groups (19 versus 20 confirmed MRSA skin abscesses). Also, the incidence of new CA-MRSA colonization in the group of soldiers decolonized with mupirocin (23/1,607; 1.4%) did not differ significantly from new colonization in the placebo-treated group (24/1,459; 1.6%) (260). In another community-based trial, mupirocin failed to produce lasting decolonization among MRSA carriers (343). Thus, there is no evidence that mupirocin or any other intranasal antimicrobial agent should be used in any community setting for MRSA decolonization.
Retapamulin
Retapamulin is a topical antibiotic, the first in a class known as the pleuromutilins to be approved by the U.S. FDA for the treatment of impetigo. In part because cross-resistance to other antimicrobials is thought to be unlikely and because it is effective against tested MRSA strains, this drug may be useful in decolonization regimens for MRSA. The drug acts by inhibiting the 50S subunit of the ribosome. Clinical trials are needed to assess the value of retapamulin for this indication (211, 764).
Specific Populations
Athletes.
Among athletes, there are several published guidelines for the prevention of MRSA transmission, although few provide evidence. For example, a general guideline for the control of MRSA in the community, prepared in 2004 and updated in December 2007, has been released by the Washington State Department of Health in collaboration with other government bodies in the state. Guidelines for the control of MRSA in the athletic setting (425) were included. The National Collegiate Athletic Association (NCAA) has published guidelines specifically for wrestlers, recommending that wrestlers with an SSTI be excluded from play until 72 h after the initiation of therapy if there is marked clinical improvement and no new lesions appearing for 48 h. An intact occlusive dressing must be in place before and during competition or practice (659).
Jails and prisons.
Although there are few relevant published data, the U.S. Federal Bureau of Prisons has released guidelines for the prevention and treatment of MRSA infections among incarcerated populations. These guidelines do not recommend routine attempts to decolonize detainees. Decolonization is recommended in the case of “recurrent MRSA infections or in the context of a MRSA outbreak” with intranasal mupirocin applied twice daily for 5 days. The guidelines call for detainee education that stresses the importance of regular hand washing, exclusion of infected detainees with draining wounds from certain activities, special procedures for the transfer of inmates, and early intervention for skin infections. Enhanced surveillance is recommended after a single case of MRSA is diagnosed. Detainees with infections are placed in individual cells only if they have uncontained drainage, whereas those with small skin infections that can be “easily contained by [a] simple dressing” can remain among the general population. In an outbreak setting, the cohorting of infected inmates, increased attention to hand hygiene, the use of antimicrobial soaps, more stringent infection control measures in clinics, and targeted examination of close contacts of infected inmates are recommended (280). Such a comprehensive program may not be practical in all jails and prisons, and more research is needed to evaluate the contribution of the individual interventions.
The Texas Department of State Health Services has prepared similar guidelines for MRSA prevention among incarcerated individuals (896).
Some researchers have advocated improved hygiene with better access to soap, showers, and clean clothing; educational campaigns; round-the-clock urgent care; and dedicated wound clinics as potential interventions to prevent the spread of MRSA in incarceration settings (69). For example, after an outbreak of MRSA SSTIs in a Georgia prison facility housing 197 detainees, administrators implemented several interventions, including skin examinations upon arrival, liquid soap near all bathroom sinks, CHG body washes for 5 days for all detainees at the start of the intervention, an educational program on skin hygiene, and waiving of the sick visit fee for skin complaints; all detainees were urged to visit the clinic if they had skin lesions. For detainees with MRSA skin lesions, a standardized antimicrobial regimen was prescribed, intranasal mupirocin and/or oral rifampin was given for decolonization, and careful attention was paid to dressing changes. With these interventions, the incidence of MRSA SSTIs decreased from 11.6 to 0 per 10,000 detainee-days (1008). The introduction of such a multiplicity of interventions, while apparently effective at curtailing an outbreak, may not be universally practical in jails and prisons. In other settings, alcohol-based hand sanitizers have been used to improve hand hygiene, but as demonstrated by a case of severe intoxication of a prison inmate who ingested hand sanitizer (243) and given their flammability, these agents are not typically allowed in places of incarceration.
Biography
 Michael Z. David, MD (Yale University), Ph.D. (History, University of Chicago), MS (Health Studies, University of Chicago), completed the Robert Wood Johnson Clinical Scholars Program and clinical infectious diseases fellowship at the University of Chicago. He is now Instructor in the Departments of Medicine, Pediatrics, and Health Studies at the University of Chicago. He is interested in the determinants of the fitness of successful methicillin-resistant Staphylococcus aureus (MRSA) strains as well as specific populations at high risk for asymptomatic carriage of MRSA. He has evaluated the criteria used to define MRSA as being community associated and studied the molecular epidemiology of MRSA infection for the past 5 years, including studies of cystic fibrosis patients, Alaska Natives, incarcerated populations, and patients at academic medical centers. He also studies the history of infectious diseases and their control.
Michael Z. David, MD (Yale University), Ph.D. (History, University of Chicago), MS (Health Studies, University of Chicago), completed the Robert Wood Johnson Clinical Scholars Program and clinical infectious diseases fellowship at the University of Chicago. He is now Instructor in the Departments of Medicine, Pediatrics, and Health Studies at the University of Chicago. He is interested in the determinants of the fitness of successful methicillin-resistant Staphylococcus aureus (MRSA) strains as well as specific populations at high risk for asymptomatic carriage of MRSA. He has evaluated the criteria used to define MRSA as being community associated and studied the molecular epidemiology of MRSA infection for the past 5 years, including studies of cystic fibrosis patients, Alaska Natives, incarcerated populations, and patients at academic medical centers. He also studies the history of infectious diseases and their control.
 Robert S. Daum, MD, CM (McGill University), Professor of Pediatrics, heads the University of Chicago MRSA Research Center. His projects include a Household Contacts Study to prospectively define colonization and infection rates among household contacts of index patients with CA-MRSA infection and the rates of environmental contamination in these households, a Treatment Study to determine the optimal management of uncomplicated skin and soft-tissue infections, and a Jail Study to determine the frequency of environmental contamination in the Dallas County Jail and the effectiveness of bathing with chlorhexidine wipes in decreasing the prevalence of MRSA. He also studies staphylococcal signal transduction mechanisms to gain insight into antibiotic resistance mechanisms among MRSA strains. His laboratory focuses on molecular pathophysiology to investigate the reasons for the dominance of the USA300 CA-MRSA clone. A newly initiated immunological study is an attempt to understand why people are differentially susceptible to CA-MRSA infections.
Robert S. Daum, MD, CM (McGill University), Professor of Pediatrics, heads the University of Chicago MRSA Research Center. His projects include a Household Contacts Study to prospectively define colonization and infection rates among household contacts of index patients with CA-MRSA infection and the rates of environmental contamination in these households, a Treatment Study to determine the optimal management of uncomplicated skin and soft-tissue infections, and a Jail Study to determine the frequency of environmental contamination in the Dallas County Jail and the effectiveness of bathing with chlorhexidine wipes in decreasing the prevalence of MRSA. He also studies staphylococcal signal transduction mechanisms to gain insight into antibiotic resistance mechanisms among MRSA strains. His laboratory focuses on molecular pathophysiology to investigate the reasons for the dominance of the USA300 CA-MRSA clone. A newly initiated immunological study is an attempt to understand why people are differentially susceptible to CA-MRSA infections.
REFERENCES
- 1.Abdel-Haq, N., H. Al-Tatari, P. Chearskul, H. Salimnia, B. I. Asmar, M. R. Fairfax, and M. Amjad. 2009. Methicillin-resistant Staphylococcus aureus (MRSA) in hospitalized children: correlation of molecular analysis with clinical presentation and antibiotic susceptibility testing (ABST) results. Eur. J. Clin. Microbiol. Infect. 28:547-551. [DOI] [PubMed] [Google Scholar]
- 2.Abi-Hanna, P., A. L. Frank, J. P. Quinn, S. Kelkar, P. C. Schreckenberger, M. K. Hayden, and J. F. Marcinak. 2000. Clonal features of community-acquired methicillin-resistant Staphylococcus aureus in children. Clin. Infect. Dis. 30:630-631. [DOI] [PubMed] [Google Scholar]
- 3.Adam, H., A. McGeer, and A. Simor. 2007. Fatal case of post-influenza community-associated MRSA pneumonia in an Ontario teenager with subsequent familial transmission. Can. Commun. Dis. Rep. 33:45-48. [PubMed] [Google Scholar]
- 4.Adcock, P., P. Pastor, F. Medley, J. Patterson, and T. Murphy. 1998. Methicillin-resistant Staphylococcus aureus in two childcare centers. J. Infect. Dis. 178:577-580. [DOI] [PubMed] [Google Scholar]
- 5.Adedeji, A., T. M. A. Weller, and J. W. Gray. 2007. MRSA in children presenting to hospitals in Birmingham, UK. J. Hosp. Infect. 65:29-34. [DOI] [PubMed] [Google Scholar]
- 6.Adem, P. V., C. P. Montgomery, A. N. Husain, T. K. Koogler, V. Arangelovich, M. Humilier, S. Boyle-Vavra, and R. S. Daum. 2005. Staphylococcus aureus sepsis and the Waterhouse-Friderichsen syndrome in children. N. Engl. J. Med. 353:1245-1251. [DOI] [PubMed] [Google Scholar]
- 7.Adeyemi, O. A., C. Qi, T. R. Zembower, M. G. Ison, T. H. Grant, B. J. Hartigan, M. Malczynski, and V. Stosor. 2008. Invasive infections with community-associated methicillin-resistant Staphylococcus aureus after kidney transplantation. J. Clin. Microbiol. 46:2809-2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adhikari, R. P., G. M. Cook, I. Lamont, S. Lang, H. Heffernan, and J. M. B. Smith. 2002. Phenotypic and molecular characterization of community occurring, Western Samoan phage pattern methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother. 50:825-831. [DOI] [PubMed] [Google Scholar]
- 9.Agwu, A., K. M. Brady, T. Ross, K. C. Carroll, and N. A. Halsey. 2007. Cholera-like diarrhea and shock associated with community-acquired methicillin-resistant Staphylococcus aureus (USA400 clone) pneumonia. Pediatr. Infect. Dis. J. 26:271-273. [DOI] [PubMed] [Google Scholar]
- 10.Aires de Sousa, M., and H. De Lencastre. 2003. Evolution of sporadic isolates of methicillin-resistant Staphylococcus aureus (MRSA) in hospitals and their similarities to isolates of community-acquired MRSA. J. Clin. Microbiol. 41:3806-3815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alcoceba, E., A. Mena, M. Cruz Pérez, E. R. de Gopegui, J. Gil, A. Ramírez, C. Gallegos, A. Serra, J. L. Pérez, and A. Oliver. 2007. Molecular epidemiology of methicillin-resistant Staphylococcus aureus in Majorcan hospitals: high prevalence of the epidemic clone EMRSA-15. Clin. Microbiol. Infect. 13:599-605. [DOI] [PubMed] [Google Scholar]
- 12.Alfaro, C., M. Mascher-Denen, J. Fergie, and K. Purcell. 2006. Prevalence of methicillin-resistant Staphylococcus aureus nasal carriage in patients admitted to Driscoll Children's Hospital. Pediatr. Infect. Dis. J. 25:459-461. [DOI] [PubMed] [Google Scholar]
- 13.Alghaithy, A. A., N. E. Bilal, M. Gedebou, and A. H. Weily. 2000. Nasal carriage and antibiotic resistance of Staphylococcus aureus isolates from hospital and non-hospital personnel in Abha, Saudi Arabia. Trans. R. Soc. Trop. Med. Hyg. 94:504-507. [DOI] [PubMed] [Google Scholar]
- 14.Al-Rawahi, G. N., S. Reynolds, S. D. Porter, L. Forrester, L. Kishi, T. Chong, W. R. Bowie, and P. W. Doyle. 2010. Community-associated CMRSA-10 (USA300) is the predominant strain among methicillin-resistant Staphylococcus aureus strains causing skin and soft tissue infections in patients presenting to the emergency department of a Canadian tertiary care hospital. J. Emerg. Med. 38:6-11. [DOI] [PubMed] [Google Scholar]
- 15.Al-Tawfiq, J. A. 2006. Father-to-infant transmission of community-associated, methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Infect. Control Hosp. Epidemiol. 27:636-637. [DOI] [PubMed] [Google Scholar]
- 16.Al-Tawfiq, J. A. 2006. Incidence and epidemiology of methicillin-resistant Staphylococcus aureus infection in a Saudi Arabian hospital, 1999-2003. Infect. Control Hosp. Epidemiol. 27:1137-1139. [DOI] [PubMed] [Google Scholar]
- 17.Alvarez, C. A., O. J. Barrientes, A. L. Leal, G. A. Contreras, L. Barrero, S. Rincón, L. Diaz, N. Vanegas, and C. A. Arias. 2006. Community-associated methicillin-resistant Staphylococcus aureus, Colombia. Emerg. Infect. Dis. 12:2000-2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andersen, B. M., M. Rasch, and G. Syversen. 2007. Is an increase of MRSA in Oslo, Norway, associated with changed infection control policy? J. Infect. 55:531-538. [DOI] [PubMed] [Google Scholar]
- 19.Anderson, E. J., C. Hawkins, M. K. Bolon, and F. J. Palella. 2006. A series of skin and soft tissue infections due to methicillin-resistant Staphylococcus aureus in HIV-infected patients. J. Acquir. Immune Defic. Syndr. 41:125-127. [DOI] [PubMed] [Google Scholar]
- 20.Anderson, M. E. C., S. L. Lefebvre, and J. S. Weese. 2008. Evaluation of prevalence and risk factors for methicillin-resistant Staphylococcus aureus colonization in veterinary personnel attending an international equine veterinary conference. Vet. Microbiol. 129:410-417. [DOI] [PubMed] [Google Scholar]
- 21.Andrews, W. W., R. Schelonka, K. Waites, A. Stamm, S. P. Cliver, and S. Moser. 2008. Genital tract methicillin-resistant Staphylococcus aureus: risk of vertical transmission in pregnant women. Obstet. Gynecol. 111:113-118. [DOI] [PubMed] [Google Scholar]
- 22.Anonymous. 1994. Tentative final monograph for health care antiseptic products: proposed rule. Fed. Regist. 59:31402-31452. [Google Scholar]
- 23.Antoniou, T., R. Devlin, K. Gough, M. Mulvey, K. C. Katz, M. Zehtabchi, J. Polsky, D. Tilley, J. Brunetta, G. Arbess, C. Guiang, B. Chang, C. Kovacs, A. Ghavam-Rassoul, C. Cavacuiti, B. Corneslon, P. Berger, and M. R. Loutfy. 2009. Prevalence of community-associated methicillin-resistant Staphylococcus aureus colonization in men who have sex with men. Int. J. STD AIDS 20:180-183. [DOI] [PubMed] [Google Scholar]
- 24.Arbeit, R. D., D. Maki, F. P. Tally, E. Campanaro, B. I. Eisenstein, and Daptomycin 90-01 and 99-01 Investigators. 2004. The safety and efficacy of daptomycin for the treatment of complicated skin and skin-structure infections. Clin. Infect. Dis. 38:1673-1681. [DOI] [PubMed] [Google Scholar]
- 25.Archibald, L. K., J. Shapiro, A. Pass, K. Rand, and F. Southwick. 2008. Methicillin-resistant Staphylococcus aureus infection in a college football team: risk factors outside the locker room and playing field. Infect. Control Hosp. Epidemiol. 29:450-453. [DOI] [PubMed] [Google Scholar]
- 26.Arias, C. A., S. Rincon, S. Chowdhury, E. Martínez, W. Coronell, J. Reyes, S. R. Nallapareddy, and B. E. Murray. 2008. MRSA USA300 clone and VREF—a U.S.-Columbian connection? N. Engl. J. Med. 359:2177-2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Armand-Lefevre, L., R. Ruimy, and A. Andremont. 2005. Clonal comparison of Staphylococcus aureus from healthy pig farmers, human controls, and pigs. Emerg. Infect. Dis. 11:711-714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arnold, S. R., D. Elias, S. C. Buckingham, E. D. Thomas, E. Novais, A. Arkader, and C. Howard. 2006. Changing patterns of acute hematogenous osteomyelitis and septic arthritis: emergence of community-associated methicillin-resistant Staphylococcus aureus. J. Pediatr. Orthop. 26:703-708. [DOI] [PubMed] [Google Scholar]
- 29.Ash, N., and M. Salai. 1995. Primary psoas abscess due to methicillin-resistant Staphylococcus aureus concurrent with septic arthritis of the hip. South. Med. J. 88:863. [DOI] [PubMed] [Google Scholar]
- 30.Assimacopoulos, A. P., K. L. Strandberg, J. H. Rotschafer, and P. M. Schlievert. 2009. Extreme pyrexia and rapid death due to Staphylococcus aureus infection: analysis of 2 cases. Clin. Infect. Dis. 48:612-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aubry-Damon, H., K. Grenet, P. Sall-Ndiaye, D. Che, E. Cordeiro, M. E. Bougnoux, E. Rigaud, Y. Le Strat, V. Lemanissier, L. Armand-Lefèvre, D. Delzescaux, J. C. Desenclos, M. Liénard, and A. Andremont. 2004. Antimicrobial resistance in commensal flora of pig farmers. Emerg. Infect. Dis. 10:873-879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ayliffe, G. A. J. 1997. The progressive intercontinental spread of methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 24(Suppl. 1):S74-S79. [DOI] [PubMed] [Google Scholar]
- 33.Baba, T., F. Takeuchi, M. Kuroda, H. Yuzawa, K. Aoki, A. Oguchi, Y. Nagai, N. Iwama, K. Asano, T. Naimi, H. Kuroda, L. Cui, K. Yamamoto, and K. Hiramatsu. 2002. Genome and virulence determinants of high virulence community-acquired MRSA. Lancet 359:1819-1827. [DOI] [PubMed] [Google Scholar]
- 34.Babu, T., V. Rekasius, J. P. Parada, P. Schreckenberger, and M. Challapalli. 2009. Mupirocin resistance among methicillin-resistant Staphylococcus aureus colonized patients at admission to a tertiary care medical center. J. Clin. Microbiol. 47:2279-2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bagcigil, F. A., A. Moodley, K. E. Baptiste, V. F. Jensen, and L. Guardabassi. 2007. Occurrence, species distribution, antimicrobial resistance and clonality of methicillin- and erythromycin-resistant staphylococci in the nasal cavity of domestic animals. Vet. Microbiol. 121:307-315. [DOI] [PubMed] [Google Scholar]
- 36.Baggett, H. C., T. W. Hennessy, K. Rudolph, D. Bruden, A. Reasonover, A. Parkinson, R. Sparks, R. M. Donlan, P. Martinez, K. Mongkolrattanothai, and J. C. Butler. 2004. Community-onset methicillin-resistant Staphylococcus aureus associated with antibiotic use and the cytotoxin Panton-Valentine leukocidin during a furunculosis outbreak in rural Alaska. J. Infect. Dis. 189:1565-1573. [DOI] [PubMed] [Google Scholar]
- 37.Baggett, H. C., T. W. Hennessy, R. Leman, C. Hamlin, D. Bruden, A. Reasonover, P. Martinez, and A. C. Butler. 2003. An outbreak of community-onset methicillin-resistant Staphylococcus aureus skin infections in southwestern Alaska. Infect. Control Hosp. Epidemiol. 24:397-402. [DOI] [PubMed] [Google Scholar]
- 38.Bahrain, M., M. Vasiliades, M. Wolff, and F. Younus. 2006. Five cases of bacterial endocarditis after furunculosis and the ongoing saga of community-acquired methicillin-resistant Staphylococcus aureus infections. Scand. J. Infect. Dis. 38:702-707. [DOI] [PubMed] [Google Scholar]
- 39.Baillargeon, J., M. F. Kelley, C. T. Leach, G. Baillargeon, and B. H. Pollack. 2004. Methicillin-resistant Staphylococcus aureus infection in the Texas prison system. Clin. Infect. Dis. 38:e92-e95. [DOI] [PubMed] [Google Scholar]
- 40.Baldan, R., C. T. Din, G. Semeraro, C. Costa, P. Cichero, P. Scarpellini, M. Moro, and D. M. Cirillo. 2009. Severe community-onset infections in healthy individuals caused by community-acquired MRSA in an Italian teaching hospital. J. Hosp. Infect. 72:271-273. [DOI] [PubMed] [Google Scholar]
- 41.Baptiste, K. E., K. Williams, N. J. Williams, A. Wattret, P. D. Clegg, S. Dawson, J. E. Corkill, T. O'Neill, and C. A. Hart. 2005. Methicillin-resistant staphylococci in companion animals. Emerg. Infect. Dis. 11:1942-1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baranovich, T., H. Zaraket, I. I. Shabana, V. Nevzorova, V. Turcyuicov, and H. Suzuki. 4 August 2009. Molecular characterization and susceptibility of methicillin-resistant and methicillin-susceptible Staphylococcus aureus isolates from hospitals and the community in Vladivostok, Russia. Clin. Microbiol. Infect. doi: 10.1111/j.1469-0691.2009.02891.x. [DOI] [PubMed]
- 43.Baranovich, T., V. Potapov, and T. Yamamoto. 2007. The first isolation of Panton-Valentine-leukocidin (PVL) positive community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) in Russia. Euro Surveill. 12(11):pii=3157. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=3157. [DOI] [PubMed] [Google Scholar]
- 44.Barr, B., and M. Felkner. 2006. High school athletic departments as sentinal surveillance sites for community-associated methicillin-resistant staphylococcal infections. Texas Med. 102:56-61. [PubMed] [Google Scholar]
- 45.Barrett, F. F., R. F. McGehee, and M. Finland. 1968. Methicillin-resistant Staphylococcus aureus at Boston City Hospital: bacteriologic and epidemiologic observations. N. Engl. J. Med. 279:441-448. [DOI] [PubMed] [Google Scholar]
- 46.Bartels, M. D., K. Boye, A. R. Larsen, R. Skov, and H. Westh. 2007. Rapid increase of genetically diverse methicillin-resistant Staphylococcus aureus, Copenhagen, Denmark. Emerg. Infect. Dis. 13:1533-1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barton, M., M. Hawkes, D. Moore, J. Conly, L. Nicolle, U. Allen, N. Boyd, J. Embree, L. V. Horne, N. Le Saux, S. Richardson, A. Moore, D. Tran, V. Waters, M. Vearcombe, K. Katz, J. S. Weese, J. Embil, M. Ofner-Agnostini, and E. L. Ford-Jones. 2006. Guidelines for the prevention and management of community-associated methicillin-resistant Staphylococcus aureus: a perspective for Canadian health care practitioners. Can. J. Infect. Dis. Med. Microbiol. 17(Suppl. C):4C-24C. [PMC free article] [PubMed] [Google Scholar]
- 48.Bauer, C. C., P. Apfalter, F. Daxboeck, N. Bachhofner, M. Stadler, A. Blacky, M. Diab-Elschahawi, and O. Assadian. 2009. Prevalence of Panton-Valentine leukocidin genes in methicillin-resistant Staphylococcus aureus isolates phenotypically consistent with community-acquired MRSA, 1999-2007, Vienna General Hospital. Eur. J. Clin. Microbiol. Infect. Dis. 28:909-912. [DOI] [PubMed] [Google Scholar]
- 49.Baum, S. E., J. T. Morris, D. P. Dooley, and R. Watson. 2003. Methicillin-resistant Staphylococcus aureus in an adult military beneficiary population lacking risk factors: susceptibility to orally available agents. Mil. Med. 168:126-130. [PubMed] [Google Scholar]
- 50.Baxtrom, C., T. Mongkolpradit, J. N. Kasiomos, L. M. Braune, R. D. Wise, P. Sierwald, and K. H. Ramsey. 2006. Common house spiders are not likely vectors of community-acquired methicillin-resistant Staphylococcus aureus infections. J. Med. Entomol. 43:962-965. [DOI] [PubMed] [Google Scholar]
- 51.Beck, A. J. 2000. Prisoners in 1999, bulletin. NCJ 183476. Bureau of Justice Statistics, Office of Justice Programs, Department of Justice, Washington, DC.
- 52.Beer, D., B. Vanddermeer, C. Brosnikoff, S. Shokoples, R. Rennie, and S. Forgie. 2006. Bacterial contamination of health care workers' pagers and the efficacy of various disinfecting agents. Pediatr. Infect. Dis. J. 25:1074-1075. [DOI] [PubMed] [Google Scholar]
- 53.Begier, E. M., K. Frenette, N. L. Barrett, P. Mshar, S. Petit, D. J. Boxrud, K. Watkins-Colwell, S. Wheeler, E. A. Cebelinski, A. Glennen, D. Nguyen, J. L. Hadler, and the Connecticut Bioterrorism Field Epidemiology Response Team. 2004. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns. Clin. Infect. Dis. 39:1446-1453. [DOI] [PubMed] [Google Scholar]
- 54.Beigi, R., and J. Hanrahan. 2007. Staphylococcus aureus and MRSA colonization rates among gravidas admitted to labor and delivery: a pilot study. Infect. Dis. Obstet. Gynecol. 2007:70876. doi: 10.1155/2007/70876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bekeredjian-Ding, I., S. Inamura, T. Giese, H. Moll, S. Endres, A. Sing, U. Zähringer, and G. Hartmann. 2007. Staphylococcus aureus protein A triggers T cell-independent B cell proliferation by sensitizing B cells for TLR2 ligands. J. Immunol. 178:2803-2812. [DOI] [PubMed] [Google Scholar]
- 56.Bekkhoucha, S. N., A. Cady, P. Gautier, F. Itim, and P. Y. Donnio. 2009. A portrait of Staphylococcus aureus from the other side of the Mediterranean Sea: molecular characteristics of isolates from Western Algeria. Eur. J. Clin. Microbiol. Infect. Dis. 28:553-555. [DOI] [PubMed] [Google Scholar]
- 57.Ben Nejma, M., M. Mastouri, B. B. H. Jrad, and M. Nour. 2 April 2008. Characterization of ST80 Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus clone in Tunisia. Diagn. Microbiol. Infect. Dis. doi: 10.1016/j.diagmicrobio.2008.02.010. [DOI] [PubMed]
- 58.Benoit, S. R., C. Estivariz, C. Mogdasy, W. Pedreira, A. Galiana, A. Galiana, H. Bagnulo, R. Gorwitz, G. E. Fosheim, L. K. McDougal, and D. Jernigan. 2008. Community strains of methicillin-resistant Staphylococcus aureus as potential cause of healthcare-associated infections, Uruguay, 2002-2004. Emerg. Infect. Dis. 14:1216-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bens, C. C. P. M., A. Voss, and C. H. W. Klassen. 2006. Presence of a novel DNA methylation enzyme in methicillin-resistant Staphylococcus aureus isolates associated with pig farming leads to uninterpretable results in standard pulsed-field gel electrophoresis analysis. J. Clin. Microbiol. 44:1875-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bentley, T. P., and D. F. Brennan. 2008. Lemierre's syndrome: methicillin-resistant Staphylococcus aureus (MRSA) finds a new home. J. Emerg. Med. 37:131-134. [DOI] [PubMed] [Google Scholar]
- 61.Berglund, C., and B. Söderquist. 2008. The origin of a methicillin-resistant Staphylococcus aureus isolate at a neonatal ward in Sweden—possible horizontal transfer of a staphylococcal cassette chromosome mec between methicillin-resistant Staphylococcus haemolyticus and Staphylococcus aureus. Clin. Microbiol. Infect. 14:1048-1056. [DOI] [PubMed] [Google Scholar]
- 62.Berglund, C., G. Prévost, B. J. Laventie, D. Keller, and B. Söderquist. 2008. The genes for Panton-Valentine leukocidin (PVL) are conserved in diverse lines of methicillin-resistant and methicillin-susceptible Staphylococcus aureus. Microbes Infect. 10:878-884. [DOI] [PubMed] [Google Scholar]
- 63.Berlet, G., R. S. Richards, and J. H. Roth. 1997. Clenched-fist injury complicated by methicillin-resistant Staphylococcus aureus. Can. J. Surg. 40:313-314. [PMC free article] [PubMed] [Google Scholar]
- 64.Berman, D. S., W. Eisner, and B. Kreiswirth. 1993. Community-acquired methicillin-resistant Staphylococcus aureus infection. N. Engl. J. Med. 329:1896. [DOI] [PubMed] [Google Scholar]
- 65.Bertin, M. L., J. Vinski, S. Schmitt, C. Sabella, L. Danziger-Isakov, M. McHugh, G. W. Procop, G. Hall, S. M. Gorson, and J. Goldfarb. 2006. Outbreak of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit epidemiologically linked to a healthcare worker with chronic otitis. Infect. Control Hosp. Epidemiol. 27:581-585. [DOI] [PubMed] [Google Scholar]
- 66.Besier, S., A. Ludwig, J. Zander, V. Brade, and T. A. Wichelhaus. 2008. Linezolid resistance in Staphylococcus aureus: gene dosage effect, stability, fitness costs, and cross-resistances. Antimicrob. Agents Chemother. 52:1570-1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bhat, N., J. G. Wright, K. R. Broder, E. L. Murray, M. E. Greenburg, M. J. Glover, A. M. Likos, D. L. Posey, A. Klimov, S. E. Lindstrom, A. Balish, M. J. Medina, T. R. Wallis, J. Guarner, C. D. Paddock, W. J. Shieh, S. R. Zaki, J. J. Sejvar, D. K. Shay, S. A. Harper, N. J. Cox, K. Fukuda, T. M. Uyeki, and Influenza Special Investigations Team. 2005. Influenza-associated deaths among children in the United States. N. Engl. J. Med. 353:2559-2567. [DOI] [PubMed] [Google Scholar]
- 68.Bhattacharya, D., H. Carleton, C. J. Tsai, E. J. Baron, and F. Perdreau-Remington. 2007. Differences in clinical and molecular characteristics of skin and soft tissue methicillin-resistant Staphylococcus aureus isolates between two hospitals in northern California. J. Clin. Microbiol. 45:1798-1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bick, J. A. 2007. Infection control in jails and prisons. Clin. Infect. Dis. 45:1047-1055. [DOI] [PubMed] [Google Scholar]
- 70.Bifero, A. E., J. Prakash, and J. Bergin. 2006. The role of chiropractic adjusting tables as reservoirs for microbial diseases. Am. J. Infect. Control 34:155-157. [DOI] [PubMed] [Google Scholar]
- 71.Bignardi, G. E., and S. Lowes. 2009. MRSA screening: throat swabs are better than nose swabs. J. Hosp. Infect. 71:373-374. [DOI] [PubMed] [Google Scholar]
- 72.Bilal, M., K. O. Cleveland, and M. S. Gelfand. 2009. Community-acquired methicillin-resistant Staphylococcus aureus and Lemierre syndrome. Am. J. Med. 338:326-327. [DOI] [PubMed] [Google Scholar]
- 73.Bleasdale, S. C., R. A. Hayes, W. E. Trick, M. K. Hayden, D. W. Blom, M. O. Vernon, and R. A. Weinstein. 2005. Does chlorhexidine gluconate bathing of medical intensive care unit patients prevent blood stream infections?, abstr. LB2-28. Abstr. 45th Intersci. Conf. Antimicrob. Agents Chemother., Washington, DC.
- 74.Block, C., E. Robenshtok, A. Simhon, and M. Shapiro. 2000. Evaluation of CHX and povidone iodine activity against methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus faecalis using a surface test. J. Hosp. Infect. 46:147-152. [DOI] [PubMed] [Google Scholar]
- 75.Blythe, D., D. Keenlyside, S. J. Dawson, and A. Galloway. 1998. Environmental contamination due to methicillin-resistant Staphylococcus aureus (MRSA). J. Hosp. Infect. 38:67-70. [DOI] [PubMed] [Google Scholar]
- 76.Bocchini, C. E., K. G. Hulten, E. O. Mason, B. E. Gonzalez, W. A. Hammerman, and S. L. Kaplan. 2006. Panton-Valentine leukocidin genes are associated with enhanced inflammatory response and local disease in acute hematogenous Staphylococcus aureus osteomyelitis in children. Pediatrics 117:433-440. [DOI] [PubMed] [Google Scholar]
- 77.Böcher, S., A. Gervelmeyer, D. L. Monnet, K. Mølbak, R. L. Skov, and the Danish CA-MRSA Study Group. 2008. Methicillin-resistant Staphylococcus aureus: risk factors associated with community-onset infections in Denmark. Clin. Microbiol. Infect. 14:942-948. [DOI] [PubMed] [Google Scholar]
- 78.Bogaert, D., A. van Belkum, M. Sluijter, A. Luijendijk, R. de Groot, H. C. Rümke, H. A. Verbruge, and P. W. Hermans. 2004. Colonisation by Streptococcus pneumoniae and Staphylococcus aureus in healthy children. Lancet 363:1871-1872. [DOI] [PubMed] [Google Scholar]
- 79.Bogaert, D., J. Nouwn, W. M. Hermans, and A. van Belkum. 2006. Lack of interference between Streptococcus pneumoniae and Staphylococcus aureus in HIV-infected individuals. J. Infect. Dis. 194:1617-1618. [DOI] [PubMed] [Google Scholar]
- 80.Bogut, A., M. Kozioł-Montewka, I. Baranowicz, L. Józwiak, Z. Al-Doori, D. Morrison, D. Kaczor, and A. Ksiazek. 2008. Community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) in Poland: further evidence for the changing epidemiology of MRSA. New Microbiol. 31:229-234. [PubMed] [Google Scholar]
- 81.Boost, M. V., M. M. O'Donoghue, and A. James. 2008. Prevalence of Staphylococcus aureus carriage among dogs and their owners. Epidemiol. Infect. 136:953-964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Boost, M. V., M. M. O'Donoghue, and K. H. G. Siu. 2007. Characterisation of methicillin-resistant Staphylococcus aureus isolates from dogs and from their owners. Clin. Microbiol. Infect. 13:731-733. [DOI] [PubMed] [Google Scholar]
- 83.Borchardt, S. M., J. S. Yoder, and M. S. Dworkin. 2005. Is the recent emergence of community-associated methicillin-resistant Staphylococcus aureus among participants in competitive sports limited to participants? Clin. Infect. Dis. 40:906-907. [DOI] [PubMed] [Google Scholar]
- 84.Borer, A., J. Gilad, P. Yagupsky, N. Peled, N. Porat, R. Trefler, H. Shprecher-Levy, K. Riesenberg, M. Shipman, and F. Schlaeffer. 2002. Community-acquired methicillin-resistant Staphylococcus aureus in institutionalized adults with developmental disabilities. Emerg. Infect. Dis. 8:966-970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bothwell, N. E., J. Shvidler, and B. B. Cable. 2007. Acute rise in methicillin-resistant Staphylococcus aureus infections in a coastal community. Otolaryngol. Head Neck Surg. 137:942-946. [DOI] [PubMed] [Google Scholar]
- 86.Boussaud, V., A. Parrot, C. Mayaud, M. Wislez, M. Antoine, C. Picard, F. Delisle, J. Etienne, and J. Cadranel. 2003. Life-threatening hemoptysis in adults with community-acquired pneumonia due to Panton-Valentine leukocidin-secreting Staphylococcus aureus. Intensive Care Med. 29:1840-1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bowers, A. L., G. R. Huffman, and B. J. Sennett. 2008. Methicillin-resistant Staphylococcus aureus infections in collegiate football players. Med. Sci. Sports Exerc. 40:1362-1367. [DOI] [PubMed] [Google Scholar]
- 88.Boyce, J. M., G. Potter-Bynoe, C. Chenevert, and T. King. 1997. Environmental contamination due to methicillin-resistant Staphylococcus aureus: possible infection control implications. Infect. Control Hosp. Epidemiol. 18:622-627. [PubMed] [Google Scholar]
- 89.Boyce, J. M., N. L. Havill, J. A. Otter, and N. M. T. Adams. 2007. Widespread environmental contamination associated with patients with diarrhea and methicillin-resistant Staphylococcus aureus colonization of the gastrointestinal tract. Infect. Control Hosp. Epidemiol. 28:1142-1147. [DOI] [PubMed] [Google Scholar]
- 90.Boyle-Vavra, S., B. Ereshefsky, C. C. Wang, and R. S. Daum. 2005. Successful multiresistant community-associated methicillin-resistant Staphylococcus aureus lineage from Taipei, Taiwan, that carries either the novel staphylococcal chromosome cassette mec (SCCmec) type VT or SCCmec type IV. J. Clin. Microbiol. 43:4719-4730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bradley, S. F., M. S. Terpenning, M. A. Ramsey, L. T. Zarins, K. A. Jorgensen, W. S. Sottile, D. R. Schaberg, and C. A. Kauffman. 1991. Methicillin-resistant Staphylococcus aureus: colonization in a long-term care facility. Ann. Intern. Med. 115:417-422. [DOI] [PubMed] [Google Scholar]
- 92.Brady, J. M., M. E. Stemper, A. Weigel, P. H. Chyou, K. D. Reed, and S. K. Shukla. 2007. Sporadic “transitional” community-associated methicillin-resistant Staphylococcus aureus strains from health care facilities in the United States. J. Clin. Microbiol. 45:2654-2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bratu, S., A. Eramo, R. Kopec, E. Coughlin, M. Ghitan, R. Yost, E. K. Chapnick, D. Landman, and J. Quale. 2005. Community-associated methicillin-resistant Staphylococcus aureus in hospital nursery and maternity units. Emerg. Infect. Dis. 11:808-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bratu, S., D. Landman, J. Gupta, M. Trehan, M. Panwar, and J. Quale. 2006. A population-based study examining the emergence of community-associated methicillin-resistant Staphylococcus aureus USA300 in New York City. Ann. Clin. Microbiol. Antimicrob. 5:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Briggs, S., C. McGuiness, M. Foster, and S. Roberts. 2002. A reservoir for methicillin-resistant Staphylococcus aureus in the Auckland community? N. Z. Med. J. 115(1162):U182. [PubMed] [Google Scholar]
- 96.Broadfield, E., N. Doshi, P. D. G. Alexander, M. Greaves, and A. Woodcock. 2009. Cunning and community-acquired pneumonia. Lancet 373:270. [DOI] [PubMed] [Google Scholar]
- 97.Brook, I., and A. E. Gober. 2009. Bacteriology of spontaneously draining acute otitis media in children before and after the introduction of pneumococcal vaccination. Pediatr. Infect. Dis. J. 28:640-642. [DOI] [PubMed] [Google Scholar]
- 98.Brooks, S. E., M. A. Walczak, R. Hameed, and P. Coonan. 2002. Chlorhexidine resistance in antibiotic-resistant bacteria isolated from the surfaces of dispensers of soap containing chlorhexidine. Infect. Control Hosp. Epidemiol. 23:692-695. [DOI] [PubMed] [Google Scholar]
- 99.Brophy, J., Y. Yau, P. Cox, K. Katz, and A. Bitnun. 2007. A sentinel case of community-associated methicillin-resistant Staphylococcus aureus in Canada. Paediatr. Child Health 12:319-322. [PMC free article] [PubMed] [Google Scholar]
- 100.Brown, S. M., G. T. Raflo, and W. L. Fanning. 2009. Transconjunctival orbital invasion by methicillin-resistant Staphylococcus aureus. Arch. Ophthalmol. 127:941-942. [DOI] [PubMed] [Google Scholar]
- 101.Brundage, J. F., and G. D. Shanks. 2009. Deaths from bacterial pneumonia during 1918-19 influenza pandemic. Emerg. Infect. Dis. 15:346-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bruno, G., J. M. Bruno, and A. A. Miyake. 2007. Community-acquired methicillin-resistant Staphylococcus aureus infection with fatal necrotizing pneumonia from lip abscess: a case report. J. Oral Maxillifac. Surg. 65:2350-2353. [DOI] [PubMed] [Google Scholar]
- 103.Bruns, A. S., and N. Sood. 2009. Community-acquired methicillin-resistant Staphylococcus aureus epidural abscess with bacteremia and multiple lung abscesses: case report. Am. J. Crit. Care 18:86-88. [DOI] [PubMed] [Google Scholar]
- 104.Buck, J. M., K. Como-Sabetti, K. H. Harriman, R. N. Danila, D. J. Boxrud, A. Glennen, and R. Lynfield. 2005. Community-associated methicillin-resistant Staphylococcus aureus, Minnesota, 2000-2003. Emerg. Infect. Dis. 11:1532-1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Buckingham, S. C., L. K. McDougal, L. D. Cathey, K. Comeaux, A. S. Craig, S. K. Fridkin, and F. C. Tenover. 2004. Emergence of community-acquired methicillin-resistant Staphylococcus aureus at a Memphis, Tennessee children's hospital. Pediatr. Infect. Dis. J. 23:619-624. [DOI] [PubMed] [Google Scholar]
- 106.Bukharie, H. A., and M. S. Abdelhadi. 2001. The epidemiology of methicillin-resistant Staphylococcus aureus at a Saudi university hospital. Microb. Drug Resist. 7:413-416. [DOI] [PubMed] [Google Scholar]
- 107.Bukharie, H. A., M. S. Abdelhadi, I. A. Saeed, A. M. Rubaish, and E. B. Larbi. 2001. Emergence of methicillin-resistant Staphylococcus aureus as a community pathogen. Diagn. Microbiol. Infect. Dis. 40:1-4. [DOI] [PubMed] [Google Scholar]
- 108.Bures, S., J. T. Fishbain, C. F. T. Uyehara, J. M. Parker, and B. W. Berg. 2000. Computer keyboards and faucet handles as reservoirs of nosocomial pathogens in the intensive care unit. Am. J. Infect. Control 28:465-470. [DOI] [PubMed] [Google Scholar]
- 109.Burkey, M. D., L. E. Wilson, R. D. Moore, G. M. Lucas, J. Francis, and K. A. Gebo. 2008. The incidence of and risk factors for MRSA bacteraemia in an HIV-infected cohort in the HAART era. HIV Med. 9:858-862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Burlak, C., C. H. Hammer, M. A. Robinson, A. R. Whitney, M. J. McGavin, B. N. Kreiswirth, and F. R. Deleo. 2007. Global analysis of community-associated methicillin-resistant Staphylococcus aureus exoproteins reveals molecules produced in vitro and during infection. Cell. Microbiol. 9:1172-1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Burton, M. J., P. Shah, and E. Swiatlo. 2008. Community-acquired methicillin-resistant Staphylococcus aureus as a cause of Fournier's gangrene. Am. J. Med. Sci. 335:327-328. [DOI] [PubMed] [Google Scholar]
- 112.Burton, S., R. Reid-Smith, J. T. McClure, and J. S. Weese. 2008. Staphylococcus aureus in healthy horses in Atlantic Canada. Can. Vet. J. 49:797-799. [PMC free article] [PubMed] [Google Scholar]
- 113.Busch, B. A., M. T. Ahern, M. Topinka, J. J. Jenkins, and M. A. Weiser. 8 July 2008. Eschar with cellulitis as a clinical predictor in community-acquired MRSA skin abscess. J. Emerg. Med. doi: 10.1016/j.jemermed.2007.11.072. [DOI] [PubMed]
- 114.Buss, B. F., S. W. Mueller, M. Theis, A. Keyser, and T. J. Safranek. 2009. Population-based estimates of methicillin-resistant Staphylococcus aureus (MRSA) infections among high school athletes—Nebraska, 2006-2008. J. Sch. Nurs. 25:282-291. [DOI] [PubMed] [Google Scholar]
- 115.Bygott, J., D. A. Enoch, R. P. M. Carson, and J. A. Karas. 2008. Presumed community-acquired methicillin-resistant Staphylococcus aureus (MRSA) isolates reflect spillover of healthcare-associated MRSA. J. Hosp. Infect. 69:197-198. [DOI] [PubMed] [Google Scholar]
- 116.Byrd, K. K., R. C. Holman, M. G. Bruce, T. W. Hennessy, J. D. Wenger, D. L. Bruden, D. L. Haberling, C. Steiner, and J. E. Cheek. 2009. Methicillin-resistant Staphylococcus aureus-associated hospitalizations among the American Indian and Alaska Native population. Clin. Infect. Dis. 49:1009-1015. [DOI] [PubMed] [Google Scholar]
- 117.Calfee, D. P., L. J. Durbin, T. P. Germanson, D. M. Toney, E. B. Smith, and B. M. Farr. 2003. Spread of methicillin-resistant Staphylococcus aureus (MRSA) among household contacts of individuals with nosocomially acquired MRSA. Infect. Control Hosp. Epidemiol. 24:422-426. [DOI] [PubMed] [Google Scholar]
- 118.Calvano, T. P., D. M. Ferraro, V. Prakash, K. Mende, and D. R. Hospenthal. 2009. Community-associated methicillin-resistant Staphylococcus aureus mediastinitis. J. Clin. Microbiol. 47:3367-3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Campana, S., P. Cocchi, G. Döring, and G. Taccetti. 2007. Emergence of an epidemic clone of community-associated methicillin-resistant Panton-Valentine leukocidin-negative Staphylococcus aureus in cystic fibrosis patients. J. Clin. Microbiol. 45:3146-3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Campbell, A. L., K. A. Bryant, B. Stover, and G. S. Marshall. 2003. Epidemiology of methicillin-resistant Staphylococcus aureus at a children's hospital. Infect. Control Hosp. Epidemiol. 24:427-430. [DOI] [PubMed] [Google Scholar]
- 121.Campillo, B., C. Dupeyron, and J. P. Richardet. 2001. Epidemiology of hospital-acquired infections in cirrhotic patients: effect of carriage of methicillin-resistant Staphylococcus aureus and influence of previous antibiotic therapy and norfloxacin prophylaxis. Epidemiol. Infect. 127:443-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Carpenter, C. F., and H. F. Chambers. 2004. Daptomycin: another novel agent for treating infections due to drug-resistant Gram-positive pathogens. Clin. Infect. Dis. 38:994-1000. [DOI] [PubMed] [Google Scholar]
- 123.Carter, T. G., E. J. Dierks, R. Bracis, and O. R. Beirne. 2005. Community acquired methicillin-resistant Staphylococcus aureus facial abscesses: case reports. J. Oral Maxillofac. Surg. 63:1021-1025. [DOI] [PubMed] [Google Scholar]
- 124.Castaldo, E. T., and E. Y. Yang. 2007. Severe sepsis attributable to community-associated methicillin-resistant Staphylococcus aureus: an emerging fatal problem. Am. Surg. 73:684-687. [PubMed] [Google Scholar]
- 125.Castrodale, L. J., M. Beller, and B. D. Gessner. 2004. Over-representation of Samoan/Pacific Islanders among patients with methicillin-resistant Staphylococcus aureus (MRSA) infections at a large family practice clinic in Anchorage, Alaska 1996-2000. Alaska Med. 46:88-91. [PubMed] [Google Scholar]
- 126.Cefai, C., S. Ashurst, and C. Owens. 1994. Human carriage of methicillin resistant Staphylococcus aureus linked with a pet dog. Lancet 344:539-540. [DOI] [PubMed] [Google Scholar]
- 127.Cenizal, M. J., D. Skiest, S. Luber, R. Bedimo, P. Davis, P. Fox, K. Delaney, and R. D. Hardy. 2007. Prospective randomized trial of empiric therapy with trimethoprim-sulfamethoxazole or doxycycline for outpatient skin and soft tissue infections in an area of high prevalence of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 51:2628-2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cenizal, M. J., R. D. Hardy, M. Anderson, K. Katz, and D. J. Skiest. 2008. Prevalence of and risk factors for methicillin-resistant Staphylococcus aureus (MRSA) nasal colonization in HIV-infected ambulatory patients. J. Acquir. Immune Defic. Syndr. 48:567-571. [DOI] [PubMed] [Google Scholar]
- 129.Centers for Disease Control and Prevention. 2009. Bacterial coinfections in lung tissue specimens from fatal cases of 2009 pandemic influenza A (H1N1)—United States, May-August 2009. MMWR Morb. Mortal. Wkly. Rep. 58:1071-1074. [PubMed] [Google Scholar]
- 130.Centers for Disease Control and Prevention. 1981. Community-acquired methicillin-resistant Staphylococcus aureus infections—Michigan. MMWR Morb. Mortal. Wkly. Rep. 30:185-187. [PubMed] [Google Scholar]
- 131.Centers for Disease Control and Prevention. 2004. Community-associated methicillin-resistant Staphylococcus aureus infections in Pacific Islanders—Hawaii, 2001-2003. MMWR Morb. Mortal. Wkly. Rep. 53:767-770. [PubMed] [Google Scholar]
- 132.Centers for Disease Control and Prevention. 3 February 2005. Community associated MRSA information for clinicians. Infection control topics. Centers for Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca_clinicians.html#4.
- 133.Centers for Disease Control and Prevention. 1999. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus—Minnesota and North Dakota, 1997-1999. MMWR Morb. Mortal. Wkly. Rep. 48:707-710. [PubMed] [Google Scholar]
- 134.Centers for Disease Control and Prevention. 2009. Methicillin-resistant Staphylococcus aureus among players on a high school football team—New York City, 2007. MMWR Morb. Mortal. Wkly. Rep. 58:52-55. [PubMed] [Google Scholar]
- 135.Centers for Disease Control and Prevention. 2003. Methicillin-resistant Staphylococcus aureus infections among competitive sports participants—Colorado, Indiana, Pennsylvania, and Los Angeles County, 2000-2003. MMWR Morb. Mortal. Wkly. Rep. 52:793-795. [PubMed] [Google Scholar]
- 136.Centers for Disease Control and Prevention. 2003. Methicillin-resistant Staphylococcus aureus infections in correctional facilities—Georgia, California, and Texas, 2001-2003. MMWR Morb. Mortal. Wkly. Rep. 52:992-996. [PubMed] [Google Scholar]
- 137.Centers for Disease Control and Prevention. 2009. Methicillin resistant Staphylococcus aureus skin infections from an elephant calf—San Diego, California, 2008. MMWR Morb. Mort. Wkly. Rep. 58:194-198. [PubMed] [Google Scholar]
- 138.Centers for Disease Control and Prevention. 2001. Methicillin-resistant Staphylococcus aureus skin or soft tissue infections in a state prison—Mississippi, 2000. MMWR Morb. Mortal. Wkly. Rep. 50:919-922. [PubMed] [Google Scholar]
- 139.Centers for Disease Control and Prevention. 2008. Progress in introduction of pneumococcal conjugate vaccine—worldwide, 2000-2008. MMWR Morb. Mortal. Wkly. Rep. 57:1148-1151. [PubMed] [Google Scholar]
- 140.Centers for Disease Control and Prevention. 2003. Public health dispatch: outbreaks of community-associated methicillin-resistant Staphylococcus aureus skin infections—Los Angeles County, California, 2002-2003. MMWR Morb. Mortal. Wkly. Rep. 52:88. [PubMed] [Google Scholar]
- 141.Centers for Disease Control and Prevention. 2007. Severe methicillin-resistant Staphylococcus aureus community-acquired pneumonia associated with influenza—Louisiana and Georgia, December 2006-January 2007. MMWR Morb. Mortal. Wkly. Rep. 54:325-329. [PubMed] [Google Scholar]
- 142.Centers for Disease Control and Prevention. 2002. Staphylococcus aureus resistant to vancomycin—United States, 2002. MMWR Morb. Mortal. Wkly. Rep. 51:565-567. [PubMed] [Google Scholar]
- 143.Centers for Disease Control and Prevention. 1997. Staphylococcus aureus with reduced susceptibility to vancomycin—United States, 1997. MMWR Morb. Mortal. Wkly. Rep. 46:765-766. [PubMed] [Google Scholar]
- 144.Centers for Disease Control and Prevention. 2009. Surveillance for pediatric deaths associated with 2009 pandemic influenza A (H1N1) virus infection—United States, April-August 2009. MMWR Morb. Mortal. Wkly. Rep. 58:941-947. [PubMed] [Google Scholar]
- 145.Centers for Disease Control and Prevention. 2004. Vancomycin-resistant Staphylococcus aureus—New York, 2004. MMWR Morb. Mortal. Wkly. Rep. 53:22-23. [PubMed] [Google Scholar]
- 146.Centers for Disease Control and Prevention. 2002. Vancomycin-resistant Staphylococcus aureus—Pennsylvania, 2002. MMWR Morb. Mortal. Wkly. Rep. 51:902. [PubMed] [Google Scholar]
- 147.Cercenado, E., O. Cuevas, M. Marín, E. Bouza, P. Trincado, T. Boquete, B. Padilla, and A. Vindel. 2008. Community-acquired methicillin-resistant Staphylococcus aureus in Madrid, Spain: transcontinental importation and polyclonal emergence of Panton-Valentine leukocidin-positive isolates. Diagn. Microbiol. Infect. Dis. 61:143-149. [DOI] [PubMed] [Google Scholar]
- 148.Chambers, H. F. 2001. The changing epidemiology of Staphylococcus aureus? Emerg. Infect. Dis. 7:178-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Chambers, H. F., R. C. Moellering, and P. Kamitsuka. 2008. Management of skin and soft-tissue infection. N. Engl. J. Med. 359:1063-1067. [DOI] [PubMed] [Google Scholar]
- 150.Chan, K. S., M. L. Ling, L. Y. Hsu, and A. L. Tan. 2009. Methicillin resistant Staphylococcus aureus throat colonization among healthcare workers during an outbreak in Singapore General Hospital. Infect. Control Hosp. Epidemiol. 30:95-97. [DOI] [PubMed] [Google Scholar]
- 151.Chang, S., D. M. Sievert, J. C. Hageman, M. L. Boulton, F. C. Tenover, F. P. Downes, S. Shah, J. T. Rudrik, G. R. Pupp, W. J. Brown, D. Cardo, and S. Fridkin. 2003. Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. N. Engl. J. Med. 348:1342-1347. [DOI] [PubMed] [Google Scholar]
- 152.Charbonneau, P., J. J. Parienti, P. Thibon, M. Ramakers, C. Daubin, D. du Cheyron, G. Lebouvier, X. Le Coutour, and R. Leclercq for the French Fluoroquinolone Free (3F) Study Group. 2006. Fluoroquinolone use and methicillin-resistant Staphylococcus aureus isolation rates in hospitalized patients: a quasi experimental study. Clin. Infect. Dis. 42:778-784. [DOI] [PubMed] [Google Scholar]
- 153.Charlebois, E. D., D. R. Bangsberg, N. J. Moss, M. R. Moore, A. R. Moss, H. F. Chambers, and F. Perdreau-Remington. 2002. Population-based community prevalence of methicillin-resistant Staphylococcus aureus in the urban poor of San Francisco. Clin. Infect. Dis. 34:425-433. [DOI] [PubMed] [Google Scholar]
- 154.Charlebois, E. D., F. Perdreau-Remington, B. Kreiswirth, D. R. Bangsberg, D. Ciccarone, B. A. Diep, V. L. Ng, K. Chansky, B. Edlin, and H. F. Chambers. 2004. Origins of community strains of methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 39:47-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Charneski, L., P. N. Patel, and D. Sym. 2009. Telavancin: a novel lipoglycopeptide antibiotic. Ann. Pharmacother. 43:928-938. [DOI] [PubMed] [Google Scholar]
- 156.Chavez-Bueno, S., B. Bozdogan, K. Katz, K. L. Bowlware, N. Cushion, D. Cavuoti, N. Ahmad, G. H. McCracken, and P. C. Appelbaum. 2005. Inducible clindamycin resistance and molecular epidemiologic trends of pediatric community-acquired methicillin-resistant Staphylococcus aureus in Dallas, Texas. Antimicrob. Agents Chemother. 49:2283-2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Chen, A. E., J. B. Cantey, K. C. Carroll, T. Ross, S. Speser, and G. K. Siberry. 2009. Discordance between Staphylococcus aureus nasal colonization and skin infections in children. Pediatr. Infect. Dis. J. 28:244-246. [DOI] [PubMed] [Google Scholar]
- 158.Chen, A. E., M. Goldstein, K. Carroll, X. Song, T. M. Perl, and G. K. Siberry. 2006. Evolving epidemiology of pediatric Staphylococcus aureus cutaneous infections in a Baltimore hospital. Pediatr. Emerg. Care 22:717-723. [DOI] [PubMed] [Google Scholar]
- 159.Chen, C. J., L. H. Su, C. H. Chiu, T. Y. Lin, K. S. Wong, Y. Y. M. Chen, and Y. C. Huang. 2007. Clinical features and molecular characteristics of invasive community-acquired methicillin-resistant Staphylococcus aureus infections in Taiwanese children. Diagn. Microbiol. Infect. Dis. 59:287-293. [DOI] [PubMed] [Google Scholar]
- 160.Chen, C. J., P. R. Hsueh, L. H. Su, C. H. Chiu, T. Y. Lin, and Y. C. Huang. 2009. Change in the molecular epidemiology of methicillin-resistant Staphylococcus aureus bloodstream infections in Taiwan. Diagn. Microbiol. Infect. Dis. 65:199-201. [DOI] [PubMed] [Google Scholar]
- 161.Chen, K. T., H. Campbell, L. N. Borrell, R. C. Huard, L. Saiman, and P. Della-Latta. 2007. Predictors and outcomes for pregnant women with vaginal-rectal carriage of community-associated methicillin-resistant Staphylococcus aureus. Am. J. Perinatol. 24:235-240. [DOI] [PubMed] [Google Scholar]
- 162.Chen, K. T., R. C. Huard, P. Della-Latta, and L. Saiman. 2006. Prevalence of methicillin-sensitive and methicillin-resistant Staphylococcus aureus in pregnant women. Obstet. Gynecol. 108:482-487. [DOI] [PubMed] [Google Scholar]
- 163.Cheng, V. C. C., I. W. S. Li, A. K. L. Wu, B. S. F. Tang, K. H. L. Ng, K. K. W. To, H. Tse, T. L. Que, P. L. Ho, and K. Y. Yuen. 2008. Effect of antibiotics on the bacterial load of meticillin-resistant Staphylococcus aureus colonization in anterior nares. J. Hosp. Infect. 70:27-34. [DOI] [PubMed] [Google Scholar]
- 164.Chheng, K., S. Tarquinio, V. Wuthiekanun, L. Sin, J. Thaipadungpanit, P. Amornchai, N. Chanpheaktra, S. Tumapa, H. Putchhat, N. P. J. Day, and S. J. Peacock. 2009. Emergence of community-associated methicillin-resistant Staphylococcus aureus associated with pediatric infection in Cambodia. PLoS One 4:e6630. doi: 10.1371/journal.pone.0006630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Chi, C. Y., M. W. Ho, C. M. Ho, P. C. Lin, J. H. Wang, and C. P. Fung. 2007. Molecular epidemiology of community-acquired methicillin-resistant Staphylococcus aureus bacteremia in a teaching hospital. J. Microbiol. Immunol. Infect. 40:310-316. [PubMed] [Google Scholar]
- 166.Chi, C. Y., W. W. Wong, C. P. Fung, K. W. Yu, and C. Y. Liu. 2004. Epidemiology of community-acquired Staphylococcus aureus bacteremia. J. Microbiol. Immunol. Infect. 37:16-23. [PubMed] [Google Scholar]
- 167.Chickering, H. T., and J. H. Park. 1919. Staphylococcus aureus pneumonia. JAMA 72:617-626. [Google Scholar]
- 168.Chini, V., E. Petinaki, H. Meugnier, A. Foka, M. Bes, J. Etienne, G. Dimitracopoulos, and I. Spiliopoulou. 2008. Emergence of a new clone carrying Panton-Valentine leukocidin genes and staphylococcal cassette chromosome mec type V among methicillin-resistant Staphylococcus aureus in Greece. Scand. J. Infect. Dis. 40:368-372. [DOI] [PubMed] [Google Scholar]
- 169.Choi, C. S., C. S. Yin, A. A. Bakar, Z. Saweki, N. N. Naing, F. Jamal, and N. Othman. 2006. Nasal carriage of Staphylococcus aureus among healthy adults. J. Microbiol. Immunol. Infect. 39:458-464. [PubMed] [Google Scholar]
- 170.Christianson, S., G. R. Golding, J. Campbell, the Canadian Nosocomial Infection Surveillance Program, and M. R. Mulvey. 2007. Comparative genomics of Canadian epidemic lineages of methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 45:1904-1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Chua, T., C. L. Moore, M. B. Perri, S. M. Donebedian, W. Masch, D. Vager, S. L. Davis, K. Lulek, B. Zimnicki, and M. J. Zervos. 2008. Molecular epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) bloodstream isolates in Detroit. J. Clin. Microbiol. 46:2345-2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Chung, M., A. Antignac, C. Kim, and A. Tomasz. 2008. Comparative study of the susceptibilities of major epidemic clones of methicillin-resistant Staphylococcus aureus to oxacillin and to the new broad-spectrum cephalosporin ceftobiprole. Antimicrob. Agents Chemother. 52:2709-2717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Clancy, M. J., A. Graepler, P. E. Breese, C. S. Price, and W. J. Burman. 2005. Widespread emergence of methicillin-resistant Staphylococcus aureus infections in Denver. South. Med. J. 98:1069-1075. [DOI] [PubMed] [Google Scholar]
- 174.Cohen, P. R. 2005. Cutaneous community-acquired methicillin-resistant Staphylococcus aureus infection in participants of athletic activities. South. Med. J. 98:596-602. [DOI] [PubMed] [Google Scholar]
- 175.Cohen, P. R., and R. Kurzrock. 2004. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: an emerging clinical problem. J. Am. Acad. Dermatol. 50:277-280. [DOI] [PubMed] [Google Scholar]
- 176.Cohen, R., C. Levy, F. Thollot, F. de la Rocque, M. Koskas, M. Bonnet, B. Fritzell, and E. Varon. 2007. Pneumococcal conjugate vaccine does not influence Staphylococcus aureus carriage in young children with acute otitis media. Clin. Infect. Dis. 45:1583-1587. (Erratum, 46: 489, 2008.) [DOI] [PubMed] [Google Scholar]
- 177.Coia, J. E., G. J. Duckworth, D. I. Edwards, M. Farrington, C. Fry, H. Humphreys, C. Mallaghan, and D. R. Tucker for the Joint Working Party of the British Society of Antimicrobial Chemotherapy, the Hospital Infection Society, and the Infection Control Nurses Association. 2006. Guidelines for the control of methicillin-resistant Staphylococcus aureus (MRSA) in healthcare facilities. J. Hosp. Infect. 63S:S1-S44. [DOI] [PubMed] [Google Scholar]
- 178.Collignon, P., I. Gosbell, A. Vickery, G. Nimmo, T. Stylianopoulos, and T. Gottlieb. 1998. Community-acquired methicillin-resistant Staphylococcus aureus in Australia. Lancet 352:146-147. [DOI] [PubMed] [Google Scholar]
- 179.Collins, J. J., J. K. Takeyasu, E. S. Nadel, and D. F. M. Brown. 2006. Septic shock and community-acquired MRSA. J. Emerg. Med. 31:211-214. [DOI] [PubMed] [Google Scholar]
- 180.Como-Sabetti, K., K. Harriman, B. Juni, A. Westbrook, E. Cebelinski, D. Boxrud, and R. Lynfield. 2006. Methicillin-resistant Staphylococcus aureus at canoe camp. Emerg. Infect. Dis. 12:1759-1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Conceição, T., M. Aires-de-Sousa, M. Füzi, Á. Tóth, J. Pászti, E. Ungvári, W. B. van Leeuwen, A. van Belkum, H. Grundmann, and H. de Lencastre. 2007. Replacement of methicillin-resistant Staphylococcus aureus clones in Hungary over time: a 10-year surveillance study. Clin. Microbiol. Infect. 13:971-979. [DOI] [PubMed] [Google Scholar]
- 182.Cook, H. A., E. Y. Furuya, E. Larson, G. Vasquez, and F. D. Lowy. 2007. Heterosexual transmission of community-associated methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 44:410-413. [DOI] [PubMed] [Google Scholar]
- 183.Cookson, B., B. Peters, M. Webster, I. Phillips, M. Rahman, and W. Noble. 1989. Staff carriage of epidemic methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 27:1471-1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Coombs, G. W., G. R. Nimmo, J. C. Pearson, K. J. Christiansen, J. M. Bell, P. J. Collignon, M. L. McLaws, and the Australian Group for Antimicrobial Resistance. 2009. Prevalence of MRSA strains among Staphylococcus aureus isolated from outpatients, 2006. Commun. Dis. Intell. 33:10-20. [PubMed] [Google Scholar]
- 185.Coombs, G. W., G. R. Nimmo, J. M. Bell, F. Huygens, F. G. O'Brien, M. J. Malkowski, J. C. Pearson, A. J. Stephens, P. M. Giffard, and the Australian Group for Antimicrobial Resistance. 2004. Genetic diversity among community-acquired methicillin-resistant Staphylococcus aureus strains causing outpatient infections in Australia. J. Clin. Microbiol. 42:4735-4743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Cooper, B. S., G. F. Medley, S. P. Stone, C. C. Kibber, B. D. Cookson, J. A. Roberts, G. Duckworth, R. Lai, and S. Ebrahim. 2004. Methicillin-resistant Staphylococcus aureus in hospitals and the community: stealth dynamics and control catastrophes. Proc. Natl. Acad. Sci. U. S. A. 101:10223-10228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Cotterill, S., R. Evans, and A. P. Fraise. 1996. An unusual source for an outbreak of methicillin-resistant Staphylococcus aureus on an intensive therapy unit. J. Hosp. Infect. 32:207-216. [DOI] [PubMed] [Google Scholar]
- 188.Creech, C. B., D. S. Kernodle, A. Alsentzer, C. Wilson, and K. M. Edwards. 2005. Increasing rates of nasal carriage of methicillin-resistant Staphylococcus aureus in healthy children. Pediatr. Infect. Dis. J. 24:617-621. [DOI] [PubMed] [Google Scholar]
- 189.Creel, A. M., S. H. Durham, K. W. Benner, J. A. Alten, and M. K. Winkler. 2009. Severe invasive community-associated methicillin-resistant Staphylococcus aureus infections in previously healthy children. Pediatr. Crit. Care Med. 10:323-327. [DOI] [PubMed] [Google Scholar]
- 190.Cribier, B., G. Prévost, P. Couppie, V. Finck-Barbançon, E. Grosshans, and Y. Piémont. 1992. Staphylococcus aureus leukocidin: a new virulence factor in cutaneous infections? An epidemiological and experimental study. Dermatology 185:175-180. [DOI] [PubMed] [Google Scholar]
- 191.Croft, C. A., V. A. Mejia, D. E. Barker, R. A. Maxwell, B. W. Dart, P. W. Smith, and R. P. Burns. 2009. Methicillin-resistant Staphylococcus aureus in a trauma population: does colonization predict infection? Am. Surg. 75:458-461. [PubMed] [Google Scholar]
- 192.Crum, N. F. 2005. The emergence of severe, community-acquired methicillin-resistant Staphylococcus aureus infections. Scand. J. Infect. Dis. 37:651-656. [DOI] [PubMed] [Google Scholar]
- 193.Crum, N. F., R. U. Lee, M. S. Thornton, O. C. Stine, M. R. Wallace, C. Barrozo, A. Keefer-Norris, S. Judd, and K. L. Russell. 2006. Fifteen-year study of the changing epidemiology of methicillin-resistant Staphylococcus aureus. Am. J. Med. 119:943-951. [DOI] [PubMed] [Google Scholar]
- 194.Crum-Cianflone, N. F., A. A. Burgi, and B. R. Hale. 2007. Increasing rates of methicillin-resistant Staphylococcus aureus infections among HIV-infected persons. Int. J. STD AIDS 18:521-526. [DOI] [PubMed] [Google Scholar]
- 195.Crum-Cianflone, N., J. Weekes, and M. Bavaro. 2009. Recurrent community-associated methicillin-resistant Staphylococcus aureus infections among HIV-infected persons: incidence and risk factors. AIDS Patient Care STDs 23:499-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Crump, J. A., D. R. Murdoch, and M. G. Baker. 2001. Emerging infectious diseases in an island ecosystem: the New Zealand perspective. Emerg. Infect. Dis. 7:767-772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Cui, S., J. Li, C. Hu, S. Jin, F. Li, Y. Guo, L. Ran, and Y. Ma. 2009. Isolation and characterization of methicillin-resistant Staphylococcus aureus from swine and workers in China. J. Antimicrob. Chemother. 64:680-683. [DOI] [PubMed] [Google Scholar]
- 198.Cuny, C., B. Strommenger, W. Witte, and C. Stanek. 2008. Clusters of infections in horses with MRSA ST1, ST254, and ST398 in a veterinary hospital. Microb. Drug Resist. 14:307-310. [DOI] [PubMed] [Google Scholar]
- 199.Cuny, C., R. Nathaus, F. Layer, B. Strommenger, D. Altmann, and W. Witte. 2009. Nasal colonization of humans with methicillin-resistant Staphylococcus aureus (MRSA) CC398 with and without exposure to pigs. PLoS One 4:e6800. doi: 10.1371/journal.pone.0006800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Cystic Fibrosis Foundation. 1995. Patient registry. Cystic Fibrosis Foundation, Bethesda, MD.
- 201.Cystic Fibrosis Foundation. 2001. Patient registry. Cystic Fibrosis Foundation, Bethesda, MD.
- 202.Cystic Fibrosis Foundation. 2005. Patient registry. Cystic Fibrosis Foundation, Bethesda, MD.
- 203.Dalloo, A., I. Sobol, C. Palacios, M. Mulvey, D. Gravel, and L. Panaro. 2008. Investigation of community-associated methicillin-resistant Staphylococcus aureus in a remote northern community, Nunavut, Canada. Can. Commun. Dis. Rep. 34:1-7. [PubMed] [Google Scholar]
- 204.Dalton, H. J. 2007. Community-acquired methicillin-resistant Staphylococcus aureus: a new scourge so virulent even extracorporeal membrane oxygenation may not help? Pediatr. Crit. Care Med. 8:294-296. [DOI] [PubMed] [Google Scholar]
- 205.Dammann, T. A., R. M. Wiens, and G. D. Taylor. 1988. Methicillin-resistant Staphylococcus aureus: identification of a community outbreak by monitoring of hospital isolates. Can. J. Public Health 79:312-314. [PubMed] [Google Scholar]
- 206.Dasenbrook, E. C., C. A. Merlo, M. Diener-West, N. Lechtzin, and M. P. Boyle. 2008. Persistent methicillin-resistant Staphylococcus aureus and rate of FEV1 decline in cystic fibrosis. Am. J. Respir. Crit. Care Med. 178:814-821. [DOI] [PubMed] [Google Scholar]
- 207.Daskalaki, M., J. R. Otero, F. Sanz, and F. Chaves. 2007. Bacteremia due to clonally derived methicillin-resistant, gentamicin-susceptible isolates and methicillin-susceptible, gentamicin-resistant isolates of Staphylococcus aureus. J. Clin. Microbiol. 45:3446-3448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Daskalaki, M., P. Rojo, M. Marin-Ferrer, M. Barrios, J. R. Otero, and F. Chaves. 2010. Panton-Valentine leukocidin-positive Staphylococcus aureus skin and soft tissue infections among children in an emergency department in Madrid, Spain. Clin. Microbiol. Infect. 16:74-77. [DOI] [PubMed] [Google Scholar]
- 209.Daum, R. S. 2007. Clinical practice: skin and soft tissue infections caused by methicillin-resistant Staphylococcus aureus. N. Engl. J. Med. 387:380-390. [DOI] [PubMed] [Google Scholar]
- 210.Daum, R. S., and J. B. Seal. 2001. Evolving antimicrobial chemotherapy for Staphylococcus aureus infections: our backs to the wall. Crit. Care Med. 29:N92-N96. [DOI] [PubMed] [Google Scholar]
- 211.Daum, R. S., S. Kar, and P. Kirkpatrick. 2007. Retapamulin. Nat. Rev. Drug Discov. 6:865-866. [Google Scholar]
- 212.Daum, R. S., T. Ito, K. Hiramatsu, F. Hussain, K. Mongkolrattanothai, M. Jamklang, and S. Boyle-Vavra. 2002. A novel methicillin-resistance cassette in community-associated methicillin-resistant Staphylococcus aureus isolates of diverse genetic backgrounds. J. Infect. Dis. 186:1344-1347. [DOI] [PubMed] [Google Scholar]
- 213.Dauwalder, O., G. Lina, G. Durand, M. Bes, H. Meugnier, V. Jarlier, B. Coignard, F. Vandensch, J. Etienne, and F. Laurent. 2008. Epidemiology of invasive MRSA clones in France, 2006-2007. J. Clin. Microbiol. 46:3454-3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.David, M. D., A. M. Kearns, S. Gossain, M. Ganner, and A. Holmes. 2006. Community-associated methicillin-resistant Staphylococcus aureus: nosocomial transmission in a neonatal care unit. J. Hosp. Infect. 64:244-250. [DOI] [PubMed] [Google Scholar]
- 215.David, M. Z., C. Mennella, M. Mansour, S. Boyle-Vavra, and R. S. Daum. 2008. Predominance of methicillin-resistant Staphylococcus aureus among pathogens causing skin and soft tissue infections in a large urban jail: risk factors and recurrence rates. J. Clin. Microbiol. 46:3222-3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.David, M. Z., D. Glikman, S. E. Crawford, J. Peng, K. J. King, M. A. Hostetler, S. Boyle-Vavra, and R. S. Daum. 2008. What is community associated methicillin-resistant Staphylococcus aureus? J. Infect. Dis. 197:1235-1243. [DOI] [PubMed] [Google Scholar]
- 217.David, M. Z., J. D. Siegel, H. F. Chambers, and R. S. Daum. 2008. Determining whether methicillin-resistant Staphylococcus aureus is associated with health care. JAMA 299:519. [DOI] [PubMed] [Google Scholar]
- 218.David, M. Z., K. M. Rudolph, T. W. Hennessey, S. Boyle-Vavra, and R. S. Daum. 2008. Molecular epidemiology of methicillin-resistant Staphylococcus aureus, rural southwestern Alaska. Emerg. Infect. Dis. 14:1693-1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.David, M. Z., S. E. Crawford, S. Boyle-Vavra, M. A. Hostetler, D. C. Kim, and R. S. Daum. 2006. Contrasting pediatric and adult methicillin-resistant Staphylococcus aureus isolates. Emerg. Infect. Dis. 12:631-637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Davis, K. A., J. J. Stewart, H. K. Crouch, C. E. Florez, and D. R. Hospenthal. 2004. Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin. Infect. Dis. 39:776-782. [DOI] [PubMed] [Google Scholar]
- 221.de Boer, E., J. T. M. Zwartkruis-Nahuis, B. Wit, X. W. Huijsdens, A. J. de Neeling, T. Bosch, R. A. A. van Oosterom, A. Vila, and A. E. Heuvelink. 2009. Prevalence of methicillin resistant Staphylococcus aureus in meat. Int. J. Food Microbiol. 134:52-56. [DOI] [PubMed] [Google Scholar]
- 222.Declercq, P., D. Petré, B. Gordts, and A. Voss. 2008. Complicated community-acquired soft tissue infection by MRSA from porcine origin. Infection 36:590-592. [DOI] [PubMed] [Google Scholar]
- 223.Deger, G. E., and D. W. Quick. 2009. The enduring menace of MRSA: incidence, treatment, and prevention in a county jail. J. Correct. Health Care 15:174-178. [DOI] [PubMed] [Google Scholar]
- 224.Dehority, W., E. Wang, P. S. Vernon, C. Lee, F. Perdreau-Remington, and J. Bradley. 2006. Community-associated methicillin-resistant Staphylococcus aureus necrotizing fasciitis in a neonate. Pediatr. Infect. Dis. J. 25:1080-1081. [DOI] [PubMed] [Google Scholar]
- 225.Del Giudice, P., V. Blanc, F. Durupt, M. Bes, J.-P. Martinez, E. Counillon, G. Lina, F. Vandenesch, and J. Etienne. 2006. Emergence of two populations of methicillin-resistant Staphylococcus aureus with distinct epidemiological, clinical and biological features, isolated from patients with community-acquired skin infections. Br. J. Dermatol. 154:118-124. [DOI] [PubMed] [Google Scholar]
- 226.de Neeling, A. J., M. J. M. van den Broek, E. C. Spalburg, M. G. van Santen-Verheuvel, W. D. C. Dam-Deisz, H. C. Boshuizen, A. W. van de Giessen, E. van Duijkeren, and X. W. Huijsdens. 2007. High prevalence of methicillin-resistant Staphylococcus aureus in pigs. Vet. Microbiol. 122:366-372. [DOI] [PubMed] [Google Scholar]
- 227.Denis, O., A. Deplano, H. De Beenhouwer, M. Hallin, G. Huysmans, M. G. Garrino, Y. Glupczynski, X. Malaviolle, A. Vergison, and M. J. Struelens. 2005. Polyclonal emergence and importation of community-acquired methicillin-resistant Staphylococcus aureus strains harbouring Panton-Valentine leucocidin genes in Belgium. J. Antimicrob. Chemother. 56:1103-1106. [DOI] [PubMed] [Google Scholar]
- 228.Denis, O., C. Suetens, M. Hallin, B. Catry, I. Ramboer, M. Dispas, G. Willems, B. Gordts, P. Butaye, and M. J. Struelens. 2009. Methicillin-resistant Staphylococcus aureus ST398 in swine farm personnel, Belgium. Emerg. Infect. Dis. 15:1098-1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Deresinski, S. 2007. Vancomycin and Staphylococcus aureus—an antibiotic enters obsolescence. Clin. Infect. Dis. 44:1536-1542. [DOI] [PubMed] [Google Scholar]
- 230.Diep, B. A., A. M. Palazzolo, P. Tattevin, L. Basuino, K. R. Braughton, A. R. Whitney, L. Chen, B. N. Kreiswirth, M. Otto, F. R. Deleo, and H. F. Chambers. 2008. Contribution of Panton-Valentine leukocidin in community-associated methicillin-resistant Staphylococcus aureus pathogenesis. PLoS One 3:e3198. doi: 10.1371/journal.pone.0003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Diep, B. A., and M. Otto. 2008. The role of virulence determinants in community-associated MRSA pathogenesis. Trends Microbiol. 16:361-369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Diep, B. A., G. F. Sensabaugh, N. A. Somboona, H. A. Carleton, and F. Perdreau-Remington. 2004. Widespread skin and soft-tissue infections due to two methicillin-resistant Staphylococcus aureus strains harboring the genes for Panton-Valentine leucocidin. J. Clin. Microbiol. 42:2080-2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Diep, B. A., G. S. Stone, L. Basuino, C. J. Graber, A. Miller, S. A. des Etages, A. Jones, A. M. Palazzolo-Balance, F. Perdreau-Remington, G. F. Sensabaugh, F. R. DeLeo, and H. F. Chambers. 2008. The arginine catabolic mobile element and staphylococcal chromosomal cassette mec linkage: convergence of virulence and resistance in the USA300 clone of methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 197:1523-1530. [DOI] [PubMed] [Google Scholar]
- 234.Diep, B. A., H. A. Carleton, R. F. Chang, G. F. Sensabaugh, and F. Perdreau-Remington. 2006. Roles of 34 virulence genes in the evolution of hospital- and community-associated strains of methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 193:1495-1503. [DOI] [PubMed] [Google Scholar]
- 235.Diep, B. A., H. F. Chambers, C. J. Graber, J. D. Szumowski, L. G. Miller, L. L. Han, J. H. Chen, J. L. Lin, T. H. Phan, H. A. Carleton, L. K. McDougal, F. C. Tenover, D. E. Cohen, K. H. Mayer, G. F. Sensabaugh, and F. Perdreau-Remington. 2008. Emergence of multidrug-resistant, community associated methicillin-resistant Staphylococcus aureus clone USA300 in men who have sex with men. Ann. Intern. Med. 148:249-258. [DOI] [PubMed] [Google Scholar]
- 236.Diep, B. A., S. R. Gill, R. F. Chang, T. F. Phan, J. H. Chen, M. G. Davidson, F. Lin, J. Lin, H. A. Carleton, E. F. Mongodin, G. F. Sensabaugh, and F. Perdreau-Remington. 2006. Complete genome sequence of USA300, an epidemic clone of community-acquired meticillin-resistant Staphylococcus aureus. Lancet 367:731-739. [DOI] [PubMed] [Google Scholar]
- 237.Dietrich, D. W., D. B. Auld, and L. A. Mermel. 2004. Community-acquired methicillin-resistant Staphylococcus aureus in southern New England children. Pediatrics 133:e347-e352. [DOI] [PubMed] [Google Scholar]
- 238.Dietze, B., A. Rath, C. Wendt, and H. Martiny. 2001. Survival of MRSA on sterile goods packaging. J. Hosp. Infect. 49:255-261. [DOI] [PubMed] [Google Scholar]
- 239.Ding, Y., Y. Onodera, J. C. Lee, and D. C. Hooper. 2008. NorB, an efflux pump in Staphylococcus aureus MW2, contributes to bacterial fitness in abscesses. J. Bacteriol. 190:7123-7129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Division of Healthcare Quality Promotion, National Center for Infectious Diseases, Centers for Disease Control and Prevention, Public Health Service, U.S. Department of Health and Human Services. 2003. National Nosocomial Infections Surveillance (NNIS) system report, data summary from January 1992 through June 2003, issued August 2003. Am. J. Infect. Control 31:481-498. [DOI] [PubMed] [Google Scholar]
- 241.Dominguez, T. J. 2004. It's not a spider bite, it's community-acquired methicillin-resistant Staphylococcus aureus. J. Am. Board Fam. Pract. 17:220-226. [DOI] [PubMed] [Google Scholar]
- 242.Dowzicky, M., G. H. Talbot, C. Feger, P. Prokocimer, J. Etienne, and R. Leclerq. 2000. Characterization of isolates associated with emerging resistance to quinupristin/dalfopristin (Synercid) during a worldwide clinical program. Diagn. Microbiol. Infect. Dis. 37:57-62. [DOI] [PubMed] [Google Scholar]
- 243.Doyon, S., and C. Welsh. 2007. Intoxication of a prison inmate with an ethyl alcohol-based hand sanitizer. N. Engl. J. Med. 356:529-530. [DOI] [PubMed] [Google Scholar]
- 244.Drapeau, C. M. J., C. Angeletti, A. Festa, and N. Petrosillo. 2007. Role of previous hospitalization in clinically-significant MRSA infection among HIV-infected inpatients: results of a case-control study. BMC Infect. Dis. 7:36. doi: 10.1186/1471-2334-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Drinka, P. J., M. E. Stemper, C. D. Gauerke, J. E. Miller, and K. D. Reed. 2004. Screening for methicillin-resistant Staphylococcus aureus in a nursing home. Infect. Control Hosp. Epidemiol. 25:95-96. [DOI] [PubMed] [Google Scholar]
- 246.Drinka, P., J. T. Faulks, C. Gauerke, B. Goodman, M. Stemper, and K. Reed. 2001. Adverse events associated with methicillin-resistant Staphylococcus aureus in a nursing home. Arch. Intern. Med. 161:2371-2377. [DOI] [PubMed] [Google Scholar]
- 247.Dufour, P., Y. Gillet, M. Bes, G. Lina, F. Vandenesch, D. Floret, J. Etienne, and H. Richet. 2002. Community-acquired methicillin-resistant Staphylococcus aureus infections in France: emergence of a single clone that produces Panton-Valentine leukocidin. Clin. Infect. Dis. 35:819-824. [DOI] [PubMed] [Google Scholar]
- 248.Dufresne, G. W., R. D. Wells, and J. A. Pfaff. 2008. The retrospective prevalence of community-acquired methicillin-resistant Staphylococcus aureus in soft tissue abscesses at two military level I trauma centers. Mil. Med. 173:945-948. [DOI] [PubMed] [Google Scholar]
- 249.Dumitrescu, O., A. Tristan, H. Meugnier, M. Bes, M. Gouy, J. Etienne, G. Lina, and F. Vandenesch. 2008. Polymorphism of the Staphylococcus aureus Panton-Valentine leukocidin genes and its possible link with the fitness of community-associated methicillin-resistant S. aureus. J. Infect. Dis. 198:792-794. [DOI] [PubMed] [Google Scholar]
- 250.Dumitrescu, O., S. Boisset, M. Bes, Y. Benito, M. E. Reverdy, F. Vandenesch, J. Etienne, and G. Lina. 2007. Effect of antibiotics on Staphylococcus aureus producing Panton-Valentine leukocidin. Antimicrob. Agents Chemother. 51:1515-1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Duong, M., S. Markwell, J. Peter, and S. Barenkamp. 29 April 2009. Randomized, controlled trial of antibiotics in the management of community-acquired skin abscesses in the pediatric patient. Ann. Emerg. Med. doi: 10.1016/j.annemergmed.2009.03.014. [DOI] [PubMed]
- 252.Durand, G., M. Bes, H. Meugnier, M. C. Enright, F. Forey, N. Liassine, A. Wenger, K. Kikuchi, G. Lina, F. Vandenesch, and J. Etienne. 2006. Detection of new methicillin-resistant Staphylococcus aureus clones containing toxic-shock syndrome toxin 1 gene responsible for hospital- and community-acquired infections in France. J. Clin. Microbiol. 44:847-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Durmaz, B., R. Durmaz, and K. Şahin. 1997. Methicillin resistance among Turkish isolates of Staphylococcus aureus strains from nosocomial and community infections and their resistance patterns using various antimicrobial agents. J. Hosp. Infect. 37:325-329. [DOI] [PubMed] [Google Scholar]
- 254.Dziekan, G., A. Hahn, K. Thüne, G. Schwarzer, K. Schäfer, F. D. Daschner, and H. Grundmann. 2000. Methicillin-resistant Staphylococcus aureus in a teaching hospital: investigation of nosocomial transmission using a matched case-control study. J. Hosp. Infect. 46:263-270. [DOI] [PubMed] [Google Scholar]
- 255.Eckhardt, C., J. S. Halvosa, S. M. Ray, and H. M. Blumberg. 2003. Transmission of methicillin-resistant Staphylococcus aureus in the neonatal intensive care unit from a patient with community-acquired disease. Infect. Control Hosp. Epidemiol. 24:460-461. [DOI] [PubMed] [Google Scholar]
- 256.Elizur, A., R. C. Orscheln, T. W. Ferkol, J. J. Atkinson, W. M. Dunne, R. S. Buller, J. R. Armstrong, E. R. Mardis, G. A. Storch, and C. L. Cannon. 2007. Panton-Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus lung infections in patients with cystic fibrosis. Chest 131:1718-1725. [DOI] [PubMed] [Google Scholar]
- 257.Ellington, M. J., C. Perry, M. Ganner, M. Warner, I. M. Smith, R. L. Hill, L. Shallcross, S. Sabersheikh, A. Holmes, B. D. Cookson, and A. M. Kearns. 2009. Clinical and molecular epidemiology of ciprofloxacin-susceptible MRSA encoding PVL in England and Wales. Eur. J. Clin. Microbiol. Infect. Dis. 28:1113-1121. [DOI] [PubMed] [Google Scholar]
- 258.Ellington, M. J., M. Ganner, M. Warner, E. Boakes, B. D. Cookson, R. L. Hill, and A. M. Kearns. 15 July 2009. First international spread and dissemination of the virulent Queensland community associated-MRSA strain. Clin. Microbiol. Infect. doi: 10.1111/j.1469-0691.2009.02994.x. [DOI] [PubMed]
- 259.Ellis, M. W., D. R. Hospenthal, D. P. Dooley, P. J. Gray, and C. K. Murray. 2004. Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers. Clin. Infect. Dis. 39:971-979. [DOI] [PubMed] [Google Scholar]
- 260.Ellis, M. W., M. E. Griffith, D. P. Dooley, J. C. McLean, J. H. Jorgensen, J. E. Patterson, K. A. David, J. S. Hawley, J. A. Regules, R. G. Rivard, P. J. Gray, J. M. Ceremuga, M. A. DeJoseph, and D. R. Hospenthal. 2007. Targeted intranasal mupirocin to prevent colonization and infection by community-associated methicillin-resistant Staphylococcus aureus strains in soldiers: a cluster randomized controlled trial. Antimicrob. Agents Chemother. 51:3591-3598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Ellis, M. W., M. E. Griffith, J. H. Jorgensen, D. R. Hospenthal, K. Mende, and J. E. Patterson. 2009. Presence and molecular epidemiology of virulence factors in methicillin-resistant Staphylococcus aureus strains colonizing and infecting soldiers. J. Clin. Microbiol. 47:940-947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Elston, J. W. T., J. Meigh, A. M. Kearns, N. Jordan-Owers, A. Newton, R. E. Meigh, and G. Barlow. 2009. Community-associated meticillin-resistant Staphylococcus aureus: epidemiology, microbiology and clinical impact in East Yorkshire, UK. J. Hosp. Infect. 72:307-313. [DOI] [PubMed] [Google Scholar]
- 263.Embil, J., K. Ramotar, L. Romance, M. Alfa, J. Conly, S. Cronk, G. Taylor, B. Sutherland, T. Louie, H. Henderson, and L. E. Nicolle. 1994. Methicillin-resistant Staphylococcus aureus in tertiary care institutions on the Canadian prairie. Infect. Control Hosp. Epidemiol. 15:646-651. [DOI] [PubMed] [Google Scholar]
- 264.Enany, S., E. Yaoita, Y. Yoshida, M. Enany, and T. Yamamoto. 2010. Molecular characterization of Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus isolates in Egypt. Microbiol. Res. 165:152-162. [DOI] [PubMed] [Google Scholar]
- 265.Enoch, D. A., J. A. Karas, J. D. Slater, M. M. Emery, K. M. Kearns, and M. Farrington. 2005. MRSA carriage in a pet therapy dog. J. Hosp. Infect. 60:186-188. [DOI] [PubMed] [Google Scholar]
- 266.Enright, M. C., and B. G. Spratt. 1999. Multilocus sequence typing. Trends Microbiol. 7:482-487. [DOI] [PubMed] [Google Scholar]
- 267.Enright, M. C., D. A. Robinson, G. Randle, E. J. Feil, H. Grundmann, and B. G. Spratt. 2002. The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA). Proc. Natl. Acad. Sci. U. S. A. 99:7687-7692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Enright, M. C., N. P. Day, C. E. Davies, S. J. Peacock, and B. G. Spratt. 2000. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J. Clin. Microbiol. 38:1008-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Epstein, C. R., W. C. Yam, J. S. M. Peiris, and R. J. Epstein. 2009. Methicillin-resistant commensal staphylococci in healthy dogs as a potential zoonotic reservoir for community-acquired antibiotic resistance. Infect. Genet. Evol. 9:283-285. [DOI] [PubMed] [Google Scholar]
- 270.Estivariz, C. F., S. Y. Park, J. C. Hageman, J. Dvorin, M. M. Melish, R. Arpon, P. Coon, S. Slavish, M. Kim, L. K. McDougal, B. Jensen, S. McAllister, D. Lonsway, G. Killgore, P. E. Effler, and D. B. Jernigan. 2007. Emergence of community-associated methicillin-resistant Staphylococcus aureus in Hawaii, 2001-2003. J. Infect. 54:349-357. [DOI] [PubMed] [Google Scholar]
- 271.Eveillard, M., Y. Martin, N. Hidri, Y. Boussougant, and M. Joly-Guillou. 2004. Carriage of methicillin-resistant Staphylococcus aureus among hospital employees: prevalence, duration, and transmission to households. Infect. Control Hosp. Epidemiol. 25:114-120. [DOI] [PubMed] [Google Scholar]
- 272.Faden, H., and S. Ferguson. 2001. Community-acquired methicillin-resistant Staphylococcus aureus and intrafamily spread of pustular disease. Pediatr. Infect. Dis. J. 20:554-555. [DOI] [PubMed] [Google Scholar]
- 273.Fagan, S. P., D. H. Berger, K. Rahwan, and S. S. Awad. 2003. Spider bites presenting with methicillin-resistant Staphylococcus aureus soft tissue infection require early aggressive treatment. Surg. Infect. (Larchmt.) 4:311-315. [DOI] [PubMed] [Google Scholar]
- 274.Fang, H., G. Hedin, G. Li, and C. E. Nord. 2008. Genetic diversity of community-associated methicillin-resistant Staphylococcus aureus in southern Stockholm. Clin. Microbiol. Infect. 14:370-376. [DOI] [PubMed] [Google Scholar]
- 275.Fang, Y. H., P. R. Hsueh, J. J. Hu, P. I. Lee, J. M. Chen, C. Y. Lee, and L. M. Huang. 2004. Community-acquired methicillin-resistant Staphylococcus aureus in children in northern Taiwan. J. Microbiol. Immunol. Infect. 37:29-34. [PubMed] [Google Scholar]
- 276.Faria, N. A., D. C. Oliviera, H. Westh, D. L. Monnet, A. R. Larsen, R. Skov, and H. de Lencastre. 2005. Epidemiology of emerging methicillin-resistant Staphylococcus aureus (MRSA) in Denmark: a nationwide study in a country with low prevalence of MRSA infection. J. Clin. Microbiol. 43:1836-1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Farley, J. E., T. Ross, P. Stamper, S. Baucom, E. Larson, and K. C. Carroll. 2008. Prevalence, risk factors, and molecular epidemiology of methicillin-resistant Staphylococcus aureus among newly arrested men in Baltimore, Maryland. Am. J. Infect. Control 36:644-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Fatholazadeh, B., M. Emaneini, G. Gilbert, E. Udo, M. Aigholi, M. H. Modarressi, K. Nouri, H. Sedaghat, and M. M. Feizabadi. 2008. Staphylococcal cassette chromosome mec (SCCmec) analysis and antimicrobial susceptibility patterns of methicillin-resistant Staphylococcus aureus (MRSA) isolates in Tehran, Iran. Microb. Drug Resist. 14:217-220. [DOI] [PubMed] [Google Scholar]
- 279.Feder, H. M. 2000. Methicillin-resistant Staphylococcus aureus infections in 2 pediatric outpatients. Arch. Fam. Med. 9:560-562. [DOI] [PubMed] [Google Scholar]
- 280.Federal Bureau of Prisons, U.S. Department of Justice. 2005. Management of methicillin-resistant Staphylococcus aureus infections (clinical practice guideline). Federal Bureau of Prisons, U. S. Department of Justice, Washington, DC. http://www.bop.gov/news/PDFs/mrsa.pdf.
- 281.Feil, E. J., J. E. Cooper, H. Grundmann, D. A. Robinson, M. C. Enright, T. Berendt, S. J. Peacock, J. M. Smith, M. Murphy, B. G. Spratt, C. E. Moore, and P. J. Day. 2003. How clonal is Staphylococcus aureus? J. Bacteriol. 185:3307-3316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Felkner, M., K. Andrews, L. H. Field, J. P. Taylor, T. Baldwin, A. M. Valle-Rivera, J. Presley, S. Newsome, and E. Casey. 2009. Detection of Staphylococcus aureus including MRSA on environmental surfaces in a jail setting. J. Correct. Health Care 15:310-317. [DOI] [PubMed] [Google Scholar]
- 283.Fenner, L., A. F. Widmer, M. Dangel, and R. Frei. 2008. Distribution of spa types among methicillin-resistant Staphylococcus aureus isolates during a 6 year period at a low-prevalence university hospital. J. Med. Microbiol. 57:612-616. [DOI] [PubMed] [Google Scholar]
- 284.Fergie, J. E., and K. Purcell. 2001. Community-acquired methicillin-resistant Staphylococcus aureus infections in south Texas children. Pediatr. Infect. Dis. J. 20:860-863. [DOI] [PubMed] [Google Scholar]
- 285.Fey, P. D., M. E. Saïd-Salim, S. H. Hinrichs, D. J. Boxrud, C. C. David, B. N. Kreiswirth, and P. M. Schlievert. 2003. Comparative molecular analysis of community- or hospital-acquired methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 47:196-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Finks, J., E. Wells, T. L. Dyke, N. Husain, L. Plizga, R. Heddurshetti, M. Wilkins, J. Rudrik, J. Hageman, J. Patel, and C. Miller. 2009. Vancomycin-resistant Staphylococcus aureus, Michigan, USA, 2007. Emerg. Infect. Dis. 15:943-945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Fitzgerald, J. R., D. E. Sturdevant, S. M. Mackie, S. R. Gill, and J. M. Musser. 2001. Evolutionary genomics of Staphylococcus aureus: insights into the origin of methicillin-resistant strains and the toxic shock syndrome epidemic. Proc. Natl. Acad. Sci. U. S. A. 98:8821-8826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Fleisch, A. F., S. Nolan, J. Gerber, and S. E. Coffin. 2007. Methicillin-resistant Staphylococcus aureus as a cause of extensive retropharyngeal abscess in two infants. Pediatr. Infect. Dis. J. 26:1161-1163. [DOI] [PubMed] [Google Scholar]
- 289.Fleisch, F., E. C. Oechslin, A. R. Gujer, E. Ritzler, A. Imhof, C. Ruef, and W. H. Reinhart. 2005. Transregional spread of a single clone of methicillin-resistant Staphylococcus aureus between groups of drug users in Switzerland. Infection 33:273-277. [DOI] [PubMed] [Google Scholar]
- 290.Florescu, I., M. Beuran, R. Dimov, A. Razbaduskas, M. Bochan, G. Fishev, G. Durkart, T. Babinchak, C. A. Cooper, E. J. Ellis-Grosse, N. Dartois, and H. Gandjini on behalf of the 307 Study Group. 2008. Efficacy and safety of tigecycline compared with vancomycin or linezolid for treatment of serious infections with methicillin-resistant Staphylococcus aureus or vancomycin-resistant entrococci: a phase 3, multicentre, double-blind, randomized study. J. Antimicrob. Chermother. 62(Suppl. 1):i17-i28. [DOI] [PubMed] [Google Scholar]
- 291.Fluit, A. C., C. L. C. Wielders, J. Verhoef, and F. J. Schmitz. 2001. Epidemiology and susceptibility of 3,051 Staphylococcus aureus isolates from 25 university hospitals participating in the European SENTRY study. J. Clin. Microbiol. 39:3727-3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Fortes, C. Q., C. A. Espanha, F. P. Bustorff, B. C. Zappa, A. L. P. Ferreira, R. B. Moreira, N. G. Pereira, V. F. Fowler, and H. Deshmukh. 2008. First reported case of infective endocarditis caused by community-acquired methicillin-resistant Staphylococcus aureus not associated with healthcare contact in Brazil. Braz. J. Infect. Dis. 12:541-543. [DOI] [PubMed] [Google Scholar]
- 293.Fortunov, R. M., K. G. Hulten, W. A. Hammerman, E. O. Mason, and S. L. Kaplan. 2006. Community-acquired Staphylococcus aureus infections in term and near-term previously healthy neonates. Pediatrics 118:874-881. [DOI] [PubMed] [Google Scholar]
- 294.Fossum, A. E., and G. Bukholm. 2006. Increased incidence of methicillin-resistant Staphylococcus aureus ST80, novel ST125 and SCCmec IV in the south-eastern part of Norway during a 12-year period. Clin. Microbiol. Infect. 12:627-633. [DOI] [PubMed] [Google Scholar]
- 295.Foster, T. J. 2005. Immune evasion by staphylococci. Nat. Rev. Microbiol. 3:948-958. [DOI] [PubMed] [Google Scholar]
- 296.Fowler, A., and A. Mackay. 2006. Community-acquired methicillin-resistant Staphylococcus aureus pyomyositis in an intravenous drug user. J. Med. Microbiol. 55:123-125. [DOI] [PubMed] [Google Scholar]
- 297.Fowler, V. G., H. W. Boucher, G. R. Corey, E. Abrutyn, A. W. Karchmer, M. E. Rupp, D. P. Levine, H. F. Chambers, F. P. Tally, G. A. Vigliani, C. H. Cabell, A. S. Link, I. DeMeyer, S. G. Filler, M. Zervos, P. Cook, J. Parsonnet, J. M. Bernstein, C. S. Price, G. N. Forrest, G. Fätkenheuer, M. Gareca, S. J. Rehm, H. R. Brodt, A. Tice, S. E. Cosgrove, and the S. aureus Endocarditis and Bacteremia Study Group. 2006. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N. Engl. J. Med. 355:653-665. [DOI] [PubMed] [Google Scholar]
- 298.Francis, J. S., K. Carroll, E. Nuermberger, and J. G. Bartlett. 2005. Reply to Wargo and Eiland. Clin. Infect. Dis. 40:1378-1379. [Google Scholar]
- 299.Francois, P., S. Harbarth, A. Huyghe, G. Renzi, M. Bento, A. Gervaix, D. Pittet, and J. Schrenzel. 2008. Methicillin-resistant Staphylococcus aureus, Geneva, Switzerland, 1993-2005. Emerg. Infect. Dis. 14:304-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Frank, A. L., J. F. Marcinak, P. D. Mangat, and P. C. Schreckenberger. 1999. Community-acquired and clindamycin-susceptible methicillin-resistant Staphylococcus aureus in children. Pediatr. Infect. Dis. J. 18:993-1000. [DOI] [PubMed] [Google Scholar]
- 301.Frank, A. L., J. F. Marcinak, P. D. Mangat, and P. C. Schreckenberger. 1999. Increase in community-acquired methicillin-resistant Staphylococcus aureus in children. Clin. Infect. Dis. 29:935-936. [DOI] [PubMed] [Google Scholar]
- 302.Frank, A. L., J. F. Marcinak, P. D. Mangat, J. T. Tjhio, S. Kalkar, P. C. Schreckenberger, and J. P. Quinn. 2002. Clindamycin treatment of methicillin-resistant Staphylococcus aureus infections in children. Pediatr. Infect. Dis. J. 21:530-534. [DOI] [PubMed] [Google Scholar]
- 303.Frazee, B. W., C. Fee, and L. Lambert. 2009. How common is MRSA in adult septic arthritis? Ann. Emerg. Med. 54:695-700. [DOI] [PubMed] [Google Scholar]
- 304.Frazee, B. W., J. Lynn, E. D. Charlebois, L. Lambert, D. Lowery, and F. Perdreau-Remington. 2005. High prevalence of methicillin-resistant Staphylococcus aureus in emergency department skin and soft tissue infections. Ann. Emerg. Med. 45:311-320. [DOI] [PubMed] [Google Scholar]
- 305.Frazee, B. W., T. O. Salz, L. Lambert, and F. Perdreau-Remington. 2005. Fatal community-associated methicillin-resistant Staphylococcus aureus pneumonia in an immunocompetent young adult. Ann. Emerg. Med. 46:401-404. [DOI] [PubMed] [Google Scholar]
- 306.Fridkin, S. K., J. C. Hageman, M. Morrison, L. T. Sanza, K. Como-Sabetti, J. A. Jernigan, K. Harriman, L. H. Harrison, R. Lynfield, and M. M. Farley. 2005. Methicillin-resistant Staphylococcus aureus in three communities. N. Engl. J. Med. 352:1436-1444. [DOI] [PubMed] [Google Scholar]
- 307.Fritz, S. A., E. K. Epplin, J. Garbutt, and G. A. Storch. 2009. Skin infection in children colonized with community-associated methicillin-resistant Staphylococcus aureus. J. Infect. 59:394-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Fritz, S. A., J. Garbutt, A. Elward, W. Shannon, and G. A. Storch. 2008. Prevalence of risk factors for community-acquired methicillin-resistant and methicillin-sensitive Staphylococcus aureus colonization in children seen in a practice-based research network. Pediatrics 121:1090-1098. [DOI] [PubMed] [Google Scholar]
- 309.Furtado, N., P. D. Mangat, A. L. Frank, W. Janda, S. Boyle, and R. S. Daum. 2006. Two clindamycin susceptible (community associated) MRSA epidemics in Chicago, abstr. 378. Abstr. 46th Annu. Meet. Infect. Dis. Soc. Am. (IDSA), Toronto, Canada.
- 310.Gardella, N., M. von Specht, A. Cuirolo, A. Rosato, G. Gutkind, and M. Mollerach. 2008. Community-associated methicillin-resistant Staphylococcus aureus, eastern Argentina. Diagn. Microbiol. Infect. Dis. 62:343-347. [DOI] [PubMed] [Google Scholar]
- 311.Garner, J. S., W. R. Jarvis, T. G. Emori, T. C. Horan, and J. M. Hughes. 1988. CDC definitions for nosocomial infections. Am. J. Infect. Control 16:128-140. [DOI] [PubMed] [Google Scholar]
- 312.Garnier, F., A. Tristan, B. Francois, J. Etienne, M. Delage-Corre, C. Martin, F. Denis, and M. C. Ploy. 2006. Pneumonia and new methicillin-resistant Staphylococcus aureus clone. Emerg. Infect. Dis. 12:498-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Gastelum, D. T., D. Dassey, L. Mascola, and L. M. Yasuda. 2005. Transmission of community-associated methicillin-resistant Staphylococcus aureus from breast milk in the neonatal intensive care unit. Pediatr. Infect. Dis. J. 24:1122-1124. [DOI] [PubMed] [Google Scholar]
- 314.Gauduchon, V., G. Cozon, F. Vandenesch, A. L. Genestier, N. Eyssade, S. Peyrol, J. Etienne, and G. Lina. 2004. Neutralization of Staphylococcus aureus Panton Valentine leukocidin by intravenous immunoglobulin in vitro. J. Infect. Dis. 189:346-353. [DOI] [PubMed] [Google Scholar]
- 315.Genestier, A. L., M. C. Michallet, G. Prévost, G. Bellot, L. Chalabreysse, S. Peyrol, F. Thivolet, J. Etienne, G. Lina, F. M. Vallette, F. Vandensch, and L. Genestier. 2005. Staphylococcus aureus Panton-Valentine leukocidin directly targets mitochondria and induces Bax-independent apoptosis of human neutrophils. J. Clin. Invest. 115:3117-3127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Gerogianni, I., G. Mpatavanis, K. Gourgoulianis, A. Maniatis, I. Spiliopoulou, and E. Petinaki. 2006. Combination of staphylococcal chromosome cassette SCCmec type V and Panton-Valentine leukocidin genes in a methicillin-resistant Staphylococcus aureus that caused necrotizing pneumonia in Greece. Diagn. Microbiol. Infect. Dis. 56:213-216. [DOI] [PubMed] [Google Scholar]
- 317.Ghebremedhin, B., M. O. Olugbosi, A. M. Raji, R. A. Bakare, B. König, and W. König. 2009. Emergence of a community-associated methicillin-resistant Staphylococcus aureus with a unique reistance profile in southwest Nigeria. J. Clin. Microbiol. 47:2975-2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Gilbert, M., J. MacDonald, D. Gregson, J. Siushansian, K. Zhang, S. Elsayed, K. Laupland, T. Louie, K. Hope, M. Mulvey, J. Gillespie, D. Nielsen, V. Wheeler, M. Louie, A. Honish, G. Keays, and J. Conly. 2006. Outbreak in Alberta of community-acquired (USA300) methicillin-resistant Staphylococcus aureus in people with a history of drug use, homelessness or incarceration. CMAJ 175:149-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Gilbert, M., J. MacDonald, M. Louie, D. Gregson, K. Zhang, S. Alsayed, K. Laupland, D. Nelson, V. Wheeler, T. Lye, and J. Conly. 2007. Prevalence of USA300 colonization or infection and associated variables during an outbreak of community-associated methicillin-resistant Staphylococcus aureus in a marginalized urban population. Can. J. Infect. Dis. Med. Microbiol. 18:357-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Gill, J. R., Z. M. Sheng, S. F. Ely, D. G. Guinee, M. B. Beasley, J. Suh, C. Deshpande, D. J. Mollura, D. M. Morens, M. Bray, W. D. Travis, and J. K. Taubenberger. 2010. Pulmonary pathologic findings of fatal 2009 pandemic influenza A/H1N1 viral infections. Arch. Pathol. Lab. Med. 134:235-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Gillet, Y., B. Issartel, P. Vanhems, J. Fournet, G. Lina, M. Bes, F. Vandenesch, Y. Piémont, N. Brousse, D. Floret, and J. Etienne. 2002. Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet 359:753-759. [DOI] [PubMed] [Google Scholar]
- 322.Gillet, Y., P. Vanhems, G. Lina, M. Bes, F. Vandenesch, D. Floret, and J. Etienne. 2007. Factors predicting mortality in necrotizing community-acquired pneumonia caused by Staphylococcus aureus containing Panton-Valentine leukocidin. Clin. Infect. Dis. 45:315-321. [DOI] [PubMed] [Google Scholar]
- 323.Givney, R., A. Vickery, A. Holliday, M. Pegler, and R. Benn. 1998. Evolution of an endemic methicillin-resistant Staphylococcus aureus population in an Australian hospital from 1967 to 1996. J. Clin. Microbiol. 36:552-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Glikman, D., J. D. Siegel, M. Z. David, N. M. Okoro, S. Boyle-Vavra, M. L. Dowell, and R. S. Daum. 2008. Complex molecular epidemiology of methicillin-resistant Staphylococcus aureus isolates from children with cystic fibrosis in the era of epidemic community-associated methicillin-resistant S. aureus. Chest 133:1381-1387. [DOI] [PubMed] [Google Scholar]
- 325.Gluck, U. 2001. Nasal carriage of Staphylococcus aureus. N. Engl. J. Med. 344:1399. [PubMed] [Google Scholar]
- 326.Goering, R. V., L. K. McDougal, G. E. Fosheim, K. K. Bonnstetter, D. J. Wolter, and F. C. Tenover. 2007. Epidemiologic distribution of catabolic mobile element among selected methicillin-resistant Staphylococcus aureus isolates. J. Clin. Microbiol. 45:1981-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Golan, Y., C. Baiez-Giangreco, C. O'Sullivan, and D. R. Snyder. 2006. Trends in vancomycin susceptibility among consecutive MRSA bacteremic isolates, abstr. LB11. Abstr. 44th Annu. Meet. Infect. Dis. Soc. Am., Arlington, VA.
- 328.Gómez, M. I., A. Lee, B. Reddy, A. Muir, G. Soong, A. Pitt, A. Cheung, and A. Prince. 2004. Staphylococcus aureus protein A induces airway epithelial inflammatory responses by activating TNFR1. Nat. Med. 10:842-848. [DOI] [PubMed] [Google Scholar]
- 329.Gonzalez, B. E., A. M. Rueda, S. A. Shelburne, D. M. Musher, R. J. Hamill, and K. G. Hultén. 2006. Community-associated strains of methicillin-resistant Staphylococcus aureus as a cause of healthcare-associated infection. Infect. Control Hosp. Epidemiol. 27:1051-1056. [DOI] [PubMed] [Google Scholar]
- 330.Gonzalez, B. E., J. Teruya, D. H. Mahoney, K. G. Hulten, R. Edwards, L. B. Lamberth, W. A. Hammerman, E. O. Mason, and S. L. Kaplan. 2006. Venous thrombosis associated with staphylococcal osteomyelitis in children. Pediatrics 117:1673-1679. [DOI] [PubMed] [Google Scholar]
- 331.Gonzalez, B. E., K. G. Hulten, M. K. Dishop, L. B. Lamberth, W. A. Hammerman, E. O. Mason, Jr., and S. L. Kaplan. 2005. Pulmonary manifestations in children with invasive community-acquired Staphylococcus aureus infection. Clin. Infect. Dis. 41:583-590. [DOI] [PubMed] [Google Scholar]
- 332.Goodrich, J. S., T. N. Sutton-Shields, A. Kerr, J. P. Wedd, M. B. Miller, and P. H. Gilligan. 2009. Prevalence of community-associated methicillin-resistant Staphylococcus aureus in patients with cystic fibrosis. J. Clin. Microbiol. 47:1231-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Gorak, E. J., S. M. Yamada, and J. D. Brown. 1999. Community-acquired methicillin-resistant Staphylococcus aureus in hospitalized adults and children without known risk factors. Clin. Infect. Dis. 29:797-800. [DOI] [PubMed] [Google Scholar]
- 334.Gorwitz, R. J. 2007. The role of ancillary antimicrobial therapy for treatment of uncomplicated skin infections in the era of community-associated methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 44:785-787. [DOI] [PubMed] [Google Scholar]
- 335.Gorwitz, R. J., D. B. Jernigan, J. H. Jernigan, and Participants in the CDC-Convened Experts' Meeting on Management of MRSA in the Community. 2006. Strategies for clinical management of MRSA in the community: summary of an experts' meeting convened by the Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca.html.
- 336.Gorwitz, R. J., D. Kruszon-Moran, S. K. McAllister, G. M. McQuillan, L. K. McDougal, G. E. Fosheim, B. J. Jensen, G. Killgore, F. C. Tenover, and M. J. Kuehnert. 2008. Changes in the prevalence of Staphylococcus aureus nasal colonization in the United States, 2001-2004. J. Infect. Dis. 197:1226-1234. [DOI] [PubMed] [Google Scholar]
- 337.Gosbell, I. B., J. L. Mercer, S. A. Neville, K. G. Chant, B. B. Jalaludin, and R. Munro. 2001. Community-acquired, non-multiresistant oxacillin-resistant Staphylococcus aureus (NORSA) in south western Sydney. Pathology 33:206-210. [PubMed] [Google Scholar]
- 338.Gosbell, I. B., J. L. Mercer, S. A. Neville, S. A. Crone, K. G. Chant, B. B. Jalaludin, and R. Munro. 2001. Non-multiresistant and multiresistant methicillin-resistant Staphylococcus aureus in community-acquired infections. Med. J. Aust. 174:627-630. [DOI] [PubMed] [Google Scholar]
- 339.Gottlieb, R. D., M. K. Shah, D. C. Perlman, and C. P. Kimmelman. 1992. Community-acquired methicillin-resistant Staphylococcus aureus infections in otolaryngology. Otolaryngol. Head Neck Surg. 107:434-437. [DOI] [PubMed] [Google Scholar]
- 340.Gottlieb, T., W. Y. Su, J. Merlino, and E. Y. L. Cheong. 2008. Recognition of USA300 isolates of community-acquired methicillin-resistant Staphylococcus aureus in Australia. Med. J. Aust. 189:179-180. [DOI] [PubMed] [Google Scholar]
- 341.Gould, F. K., R. Brindle, P. R. Chadwick, A. P. Fraise, S. Hill, D. Nathwani, G. L. Ridgway, M. J. Spry, and R. E. Warren on behalf of the MRSA Working Party of the British Society for Antimicrobial Therapy. 2009. Guidelines (2008) for the prophylaxis and treatment of methicillin-resistant Staphylococcus aureus infections in the United Kingdom. J. Antimicrob. Chemother. 63:849-861. [DOI] [PubMed] [Google Scholar]
- 342.Gould, I. M., F. M. MacKenzie, G. MacLennan, D. Pacitti, E. J. Watson, and D. W. Noble. 2007. Topical antimicrobials in combination with admission screening and barrier precautions to control endemic methicillin-resistant Staphylococcus aureus in an intensive care unit. Int. J. Antimicrob. Agents 29:536-543. [DOI] [PubMed] [Google Scholar]
- 343.Graber, C. J., and B. S. Schwartz. 2008. Failure of decolonization in patients with infections due to mupirocin-resistant strains of community-associated methicillin-resistant Staphylococcus aureus. Infect. Control Hosp. Epidemiol. 29:284. [DOI] [PubMed] [Google Scholar]
- 344.Graber, C. J., M. K. Wong, H. A. Carleton, F. Perdreau-Remington, B. L. Haller, and H. F. Chambers. 2007. Intermediate vancomycin susceptibility in a community-associated MRSA clone. Emerg. Infect. Dis. 13:491-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Graffunder, E. M., and R. A. Venezia. 2002. Risk factors associated with nosocomial methicillin-resistant Staphylococcus aureus (MRSA) infection including previous use of antimicrobials. J. Antimicrob. Chemother. 49:999-1005. [DOI] [PubMed] [Google Scholar]
- 346.Graham, P. L., S. X. Lin, and E. L. Larson. 2006. A U.S. population-based survey of Staphylococcus aureus colonization. Ann. Intern. Med. 144:318-325. [DOI] [PubMed] [Google Scholar]
- 347.Griffiths, C., T. L. Lamagni, N. S. Crowcroft, G. Duckworth, and C. Rooney. 2004. Trends in MRSA in England and Wales: analysis of morbidity and mortality data for 1993-2002. Health Stat. Q. 21:15-22. [PubMed] [Google Scholar]
- 348.Grisold, A. J., G. Zarfel, A. Stoeger, G. Feierl, R. B. Raggam, and E. Marth. 2009. Emergence of community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) in southeast Austria. J. Infect. 58:168-170. [DOI] [PubMed] [Google Scholar]
- 349.Groom, A. V., D. H. Wolsey, T. S. Naimi, K. Smith, S. Johnson, D. Boxrud, K. A. Moore, and J. E. Cheek. 2001. Community-acquired methicillin-resistant Staphylococcus aureus in a rural American Indian community. JAMA 286:1201-1205. [DOI] [PubMed] [Google Scholar]
- 350.Gross-Schulman, S., D. Dassey, L. Mascola, and C. Anaya. 1998. Community-acquired methicillin-resistant Staphylococcus aureus. JAMA 280:421-422. [PubMed] [Google Scholar]
- 351.Guardabassi, L., M. Stegger, and R. Skov. 2007. Retrospective detection of methicillin-resistant and susceptible Staphylococcus aureus ST398 in Danish slaughter pigs. Vet. Microbiol. 122:384-386. [DOI] [PubMed] [Google Scholar]
- 352.Gubbay, J. B., I. B. Gosbell, T. Barbagiannakos, A. M. Vickery, J. L. Mercer, and M. Watson. 2008. Clinical features, epidemiology, antimicrobial resistance, and exotoxin genes (including that of Panton-Valentine leukocidin) of gentamicin-susceptible methicillin-resistant Staphylococcus aureus (GS-MRSA) isolated at a paediatric teaching hospital in New South Wales, Australia. Pathology 40:64-71. [DOI] [PubMed] [Google Scholar]
- 353.Guss, J., and K. Kazahaya. 2007. Antibiotic-resistant Staphylococcus aureus in community-acquired pediatric neck abscesses. Int. J. Pediatr. Otorhinolaryngol. 71:943-948. [DOI] [PubMed] [Google Scholar]
- 354.Gwynne-Jones, D. P., and N. S. Stott. 1999. Community-acquired methicillin-resistant Staphylococcus aureus: a cause of musculoskeletal sepsis in children. J. Pediatr. Orthop. 19:413-416. [PubMed] [Google Scholar]
- 355.Hageman, J. C., T. M. Uyeki, J. S. Francis, D. B. Jernigan, J. G. Wheeler, C. B. Bridges, S. J. Barenkamp, D. M. Sievert, A. Srinivasan, M. C. Doherty, L. K. McDougal, G. E. Killgore, U. A. Lopatin, R. Coffman, J. K. MacDonald, S. K. McAllister, G. E. Fosheim, J. B. Patel, and L. C. McDonald. 2006. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003-04 influenza season. Emerg. Infect. Dis. 12:894-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Hall, A. J., D. Bixler, and L. E. Haddy. 2008. Multiclonal outbreak of methicillin-resistant Staphylococcus aureus on a collegiate football team. Epidemiol. Infect. 137:85-93. [DOI] [PubMed] [Google Scholar]
- 357.Hallin, M., O. Denis, A. Deplano, R. De Mendonça, R. De Ryck, S. Rottiers, and M. J. Struelens. 2007. Genetic relatedness between methicillin-susceptible and methicillin-resistant Staphylococcus aureus: results of a national survey. J. Antimicrob. Chemother. 59:465-472. [DOI] [PubMed] [Google Scholar]
- 358.Hammond, S. P., and L. R. Baden. 2008. Management of skin and soft-tissue infection—polling results. N. Engl. J. Med. 359:e20. [DOI] [PubMed] [Google Scholar]
- 359.Hamoudi, A. C., R. N. Palmer, and T. L. King. 1983. Nafcillin resistant Staphylococcus aureus: a possible community origin. Infect. Control 4:153-157. [DOI] [PubMed] [Google Scholar]
- 360.Hampson, F. G., S. W. Hancock, and R. A. Primhak. 2006. Disseminated sepsis due to a Panton-Valentine leukocidin producing strain of community acquired meticillin resistant Staphylococcus aureus and use of intravenous immunoglobulin therapy. Arch. Dis. Child. 91:201-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Han, L. L., L. K. McDougal, R. J. Gorwitz, K. H. Mayer, J. B. Patel, J. M. Sennott, and J. L. Fontana. 2007. High frequencies of clindamycin and tetracycline resistance in methicillin-resistant Staphylococcus aureus pulsed-field type USA300 isolates collected at a Boston ambulatory health center. J. Clin. Microbiol. 45:1350-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Hankin, A., and W. W. Everett. 2007. Are antibiotics necessary after incision and drainage of a cutaneous abscess? Ann. Emerg. Med. 50:49-51. [DOI] [PubMed] [Google Scholar]
- 363.Hanselman, B. A., S. A. Kruth, J. Rouseau, and J. S. Weese. 2008. Methicillin-resistant Staphylococcus aureus colonization in schoolteachers in Ontario. Can. J. Infect. Dis. Med. Microbiol. 19:405-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Hanselman, B. A., S. A. Kruth, J. Rousseau, D. E. Low, B. M. Willey, A. McGeer, and S. Weese. 2006. Methicillin-resistant Staphylococcus aureus colonization in veterinary personnel. Emerg. Infect. Dis. 12:1933-1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Hanselman, B. A., S. Kruth, and J. S. Weese. 2008. Methicillin-resistant staphylococcal colonization in dogs entering a veterinary teaching hospital. Vet. Microbiol. 126:277-281. [DOI] [PubMed] [Google Scholar]
- 366.Hanssen, A. M., A. Fossum, J. Mikalsen, D. S. Halvorsen, G. Bukholm, and J. U. E. Sollid. 2005. Dissemination of community-acquired methicillin-resistant Staphylococcus aureus clones in northern Norway: sequence types 8 and 80 predominate. J. Clin. Microbiol. 43:2118-2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Haque, N. Z., S. L. David, C. L. Manieski, D. Vager, S. M. Donabedian, M. B. Perri, R. Sabbagh, F. Cheema, and M. J. Zervos. 2007. Infective endocarditis caused by USA300 methicillin-resistant Staphylococcus aureus (MRSA). Int. J. Antimicrob. Agents 30:72-77. [DOI] [PubMed] [Google Scholar]
- 368.Harbarth, S., J. Schrenzel, C. Akakpo, G. Renzi, and B. Ricou. 2007. Is throat screening necessary to detect MRSA colonization upon admission to an intensive care unit? J. Clin. Microbiol. 45:1072-1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Harbarth, S., S. Dharan, N. Liassine, P. Herrault, R. Auckenthaler, and D. Pittet. 1999. Randomized, placebo-controlled, double-blind trial to evaluate the efficacy of mupirocin for eradicating carriage of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 43:1412-1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Hardy, K. J., B. A. Oppenheim, S. Gossain, F. Gao, and P. M. Hawkey. 2006. A study of the relationship between environmental contamination with methicillin-resistant Staphylococcus aureus (MRSA) and patients' acquisition of MRSA. Infect. Control Hosp. Epidemiol. 27:127-132. [DOI] [PubMed] [Google Scholar]
- 371.Hardy, K. J., S. Gossain, N. Henderson, C. Drugan, B. A. Oppenheim, F. Gao, and P. M. Hawkey. 2007. Rapid recontamination with MRSA of the environment of an intensive care unit after decontamination with hydrogen peroxide vapour. J. Hosp. Infect. 66:360-368. [DOI] [PubMed] [Google Scholar]
- 372.Hasan, S. I., and H. B. Hale. 2008. Community-acquired methicillin-resistant Staphylococcus aureus necrotizing pneumonia: a report of three cases. Hosp. Physician 44:37-41. [Google Scholar]
- 373.Hasty, M., A. Klasner, S. Kness, T. K. Denmark, D. Ellis, M. I. Herman, and L. Brown. 2007. Cutaneous community-associated methicillin-resistant Staphylococcus aureus among all skin and soft-tissue infections in two geographically distant pediatric emergency departments. Acad. Emerg. Med. 14:35-40. [DOI] [PubMed] [Google Scholar]
- 374.Hayward, A., F. Knott, I. Petersen, D. M. Livermore, G. Duckworth, A. Islam, and A. M. Johnson. 2008. Increasing hospitalizations and general practice prescriptions for community-onset staphylococcal disease, England. Emerg. Infect. Dis. 14:720-726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Health Protection Agency. 2005. Community MRSA in England and Wales: definition through strain characterisation. Commun. Dis. Rep. Wkly. 15:11. http://www.hpa.org.uk/cdr/archives/2005/cdr1105.pdf. [Google Scholar]
- 376.Health Protection Agency. 2006. Hospital-associated transmission of Panton-Valentine leukocidin (PVL) positive community-associated MRSA in the West Midlands. Commun. Dis. Rep. Wkly. 16:50. http://www.hpa.org.uk/cdr/archives/2006/cdr5006.pdf. [Google Scholar]
- 377.Healy, C. M., K. G. Hulten, D. L. Palazzi, J. R. Campbell, and C. J. Baker. 2004. Emergence of new strains of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Clin. Infect. Dis. 39:1460-1466. [DOI] [PubMed] [Google Scholar]
- 378.Hedin, G., and H. Fang. 2007. Epidemiology of methicillin-resistant Staphylococcus aureus in southern Stockholm, 2000-2003. Microb. Drug Resist. 13:241-250. [DOI] [PubMed] [Google Scholar]
- 379.Heggelund, L., H. H. Samdal, R. Eggum, T. Jacobsen, T. Bruun, and P. Elstrøm. 2007. Severe case of invasive community-acquired methicillin-resistant Staphylococcus aureus in Norway. Euro Surveill. 12(45):pii=3304. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=3304. [DOI] [PubMed] [Google Scholar]
- 380.Heininger, U., F. Datta, A. Gervaix, U. B. Schaad, C. Berger, B. Vaudaux, C. Aebi, M. Hitzler, C. Kind, H. E. Gnehm, R. Frei, and the PIGS/MRSA Study Group. 2007. Prevalence of nasal colonization with methicillin-resistant Staphylococcus aureus in children: a multicenter cross-sectional study. Pediatr. Infect. Dis. J. 26:544-546. [DOI] [PubMed] [Google Scholar]
- 381.Helgason, K. O., M. E. Jones, and G. Edwards. 2007. Panton-Valentine leukocidin positive Staphylococcus aureus and foreign travel. J. Clin. Microbiol. 46:832-833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Heller, J., S. K. Armstrong, E. K. Girvan, S. W. J. Reid, A. Moodley, and D. J. Mellor. 2009. Prevalence and distribution of meticillin-resistant Staphylococcus aureus within the environment and staff of a university veterinary clinic. J. Small Anim. Pract. 50:168-173. [DOI] [PubMed] [Google Scholar]
- 383.Herold, B. C., L. C. Immergluck, M. C. Maranan, D. S. Lauderdale, R. E. Gaskin, S. Boyle-Vavra, C. D. Leitch, and R. S. Daum. 1998. Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA 279:593-598. [DOI] [PubMed] [Google Scholar]
- 384.Hersh, A. L., H. F. Chambers, J. H. Maselli, and R. Gonzales. 2008. National trends in ambulatory visits and antibiotic prescribing for skin and soft tissue infections. Arch. Intern. Med. 168:1585-1591. [DOI] [PubMed] [Google Scholar]
- 385.Hidron, A. I., E. V. Kourbatova, J. S. Halvosa, B. J. Terrell, L. K. McDougal, F. C. Tenover, H. M. Blumberg, and M. D. King. 2005. Risk factors for colonization with methicillin-resistant Staphylococcus aureus (MRSA) in patients admitted to an urban hospital: emergence of community-associated MRSA nasal carriage. Clin. Infect. Dis. 41:159-166. [DOI] [PubMed] [Google Scholar]
- 386.Highlander, S. K., K. G. Hultén, X. Qin, H. Jiang, S. Yerrapragada, E. O. Mason, Y. Shang, T. M. Williams, R. M. Fortunov, Y. Liu, O. Igboeli, J. Petrosino, M. Tirumalai, A. Uzman, G. E. Fox, A. M. Cardenas, D. M. Muzny, L. Hemphill, Y. Ding, S. Dugan, P. R. Blyth, C. J. Buhay, H. H. Dinh, A. C. Hawes, M. Holder, C. L. Kovar, S. L. Lee, W. Liu, L. V. Nazareth, Q. Wang, J. Zhou, S. L. Kaplan, and G. M. Weinstock. 2007. Subtle genetic changes enhance virulence of methicillin resistant and sensitive Staphylococcus aureus. BMC Microbiol. 7:99. doi: 10.1186/1471-2180-7-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Hill, P. C., M. Birch, S. Chambers, D. Drinkovic, R. B. Ellis-Pegler, R. Everts, D. Murdoch, S. Pottumarthy, S. A. Roberts, C. Swager, S. L. Taylor, M. G. Thomas, C. G. Wong, and A. J. Morris. 2001. Prospective study of 424 cases of Staphylococcus aureus bacteraemia: determination of factors affecting incidence and mortality. Int. Med. J. 31:97-103. [PubMed] [Google Scholar]
- 388.Hiramatsu, K. 1995. Molecular evolution of MRSA. Microbiol. Immunol. 39:531-543. [DOI] [PubMed] [Google Scholar]
- 389.Hiramatsu, K. 1998. The emergence of Staphylococcus aureus with reduced susceptibility to vancomycin in Japan. Am. J. Med. 104:75-105. [DOI] [PubMed] [Google Scholar]
- 390.Hiramatsu, K., L. Cui, M. Kuroda, and T. Ito. 2001. The emergence and evolution of methicillin-resistant Staphylococcus aureus. Trends Microbiol. 9:486-493. [DOI] [PubMed] [Google Scholar]
- 391.Hiramatsu, K., N. Aviaka, H. Hanaki, S. Kawasaki, Y. Hosoda, S. Hori, Y. Fukuchi, and I. Kobayashi. 1997. Dissemination in Japanese hospitals of strains of Staphylococcus aureus heterogeneously resistant to vancomycin. Lancet 350:1670-1673. [DOI] [PubMed] [Google Scholar]
- 392.Hiramatsu, K., Y. Katayama, H. Yuzawa, and T. Ito. 2002. Molecular genetics of methicillin-resistant Staphylococcus aureus. Int. J. Med. Microbiol. 292:67-74. [DOI] [PubMed] [Google Scholar]
- 393.Hisata, K., K. Kuwahara-Arai, M. Yamanoto, T. Ito, Y. Nakatomi, L. Cui, T. Baba, M. Terasawa, C. Sotozono, S. Kinoshita, Y. Yamashiro, and K. Hiramatsu. 2005. Dissemination of methicillin-resistant staphylococci among healthy Japanese children. J. Clin. Microbiol. 43:3364-3372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Ho, M., L. McDonald, T. L. Lauderdale, L. L. Yeh, P. C. Chen, and Y. R. Shiau. 1999. Surveillance of antibiotic resistance in Taiwan, 1998. J. Microbiol. Immunol. Infect. 32:239-249. [PubMed] [Google Scholar]
- 395.Ho, P. L., C. Cheung, G. C. Mak, C. W. Tse, T. K. Ng, C. H. Cheung, T. L. Que, R. Lam, W. M. Lai, R. W. Yung, and K. Y. Yuen. 2006. Molecular epidemiology and household transmission of community-associated methicillin-resistant Staphylococcus aureus in Hong Kong. Diagn. Microbiol. Infect. Dis. 57:145-151. [DOI] [PubMed] [Google Scholar]
- 396.Ho, P. L., M. P. Wong, E. L. Lai, K. H. Chan, and S. S. Chiu. 2008. DNA typing of cytological samples for retrospective identification of an early case of Panton-Valentine leukocidin positive, community-associated methicillin-resistant Staphylococcus aureus pneumonia. J. Clin. Microbiol. 46:2457-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Ho, P. L., S. K. Chuang, Y. F. Choi, R. A. Lee, A. C. H. Lit, T. K. Ng, T. L. Que, K. C. Shek, H. K. Tong, C. W. S. Tse, W. K. Tung, and R. W. H. Yung for the Hong Kong CA-MRSA Surveillance Network. 2008. Community-associated methicillin-resistant and methicillin-sensitive Staphylococcus aureus: skin and soft tissue infections in Hong Kong. Diagn. Microbiol. Infect. Dis. 61:245-250. [DOI] [PubMed] [Google Scholar]
- 398.Hodgeson, J. E., S. P. Curnock, K. G. Dyke, R. Morris, D. R. Sylvester, and M. S. Gross. 1994. Molecular characterization of the gene encoding high-level mupirocin resistance in Staphylyococcus aureus J2870. Antimicrob. Agents Chemother. 38:1205-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Holden, M. T., E. J. Feil, J. A. Lindsay, S. J. Peacock, N. P. Day, M. C. Enright, T. J. Foster, C. E. Moore, L. Hurst, R. Atkin, A. Barron, N. Bason, S. D. Bentley, C. Chillingworth, T. Chillingworth, C. Churcher, L. Clark, C. Corton, A. Cronin, J. Doggett, L. Dowd, T. Feltwell, Z. Hance, B. Harris, H. Hauser, S. Holroyd, K. Jagels, K. D. James, N. Lennard, A. Line, R. Mayes, S. Moule, K. Mungall, D. Ormond, M. A. Quail, E. Rabbinowitsch, K. Rutherford, M. Sanders, S. Sharp, M. Simmonds, K. Stevens, S. Whitehead, B. G. Barrell, B. G. Spratt, and J. Parkhill. 2004. Complete genomes of two clinical Staphylococcus aureus strains: evidence for the rapid evolution of virulence and drug resistance. Proc. Natl. Acad. Sci. U. S. A. 101:9786-9791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Hollis, R. J., J. L. Barr, B. N. Doebbeling, M. A. Pfaller, and R. P. Wenzel. 1995. Familial carriage of methicillin-resistant Staphylococcus aureus and subsequent infection in a premature neonate. Clin. Infect. Dis. 21:328-332. [DOI] [PubMed] [Google Scholar]
- 401.Holmes, A., M. Ganner, S. McGuane, T. L. Pitt, B. D. Cookson, and A. M. Kearns. 2005. Staphylococcus aureus isolates carrying Panton-Valentine leukocidin genes in England and Wales: frequency, characterization, and association with clinical disease. J. Clin. Microbiol. 43:2384-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Hongo, I., T. Baba, K. Oishi, Y. Morimoto, T. Ito, and K. Hiramatsu. 2009. Phenol-soluble modulin α3 enhances the human neutrophil lysis mediated by Panton-Valentine leukocidin. Clin. Infect. Dis. 200:715-723. [DOI] [PubMed] [Google Scholar]
- 403.Hota, B., C. Ellenbogen, M. K. Hayden, A. Aroutcheva, T. W. Rice, and R. A. Weinstein. 2007. Community associated methicillin-resistant Staphylococcus aureus skin and soft infections at a public hospital: do public housing and incarceration amplify transmission? Arch. Intern. Med. 167:1026-1033. [DOI] [PubMed] [Google Scholar]
- 404.Hsieh, J. M., R. S. Chen, T. Y. Tsai, T. M. Pan, and C. C. Chou. 2008. Phylogenetic analysis of livestock oxacillin-resistant Staphylococcus aureus. Vet. Microbiol. 126:234-242. [DOI] [PubMed] [Google Scholar]
- 405.Huang, H., N. M. Flynn, J. H. King, C. Monchaud, M. Morita, and S. H. Cohen. 2006. Comparisons of community associated methicillin-resistant Staphylococcus aureus (MRSA) and hospital-associated MRSA infections in Sacramento, California. J. Clin. Microbiol. 44:2423-2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Huang, H., S. H. Cohen, J. H. King, C. Monchaud, H. Nguyen, and N. M. Flynn. 2008. Injecting drug use and community-associated methicillin-resistant Staphylococcus aureus infection. Diagn. Microbiol. Infect. Dis. 60:347-350. [DOI] [PubMed] [Google Scholar]
- 407.Huang, R., S. Mehta, D. Weed, and C. S. Price. 2006. Methicillin-resistant Staphylococcus aureus survival on hospital fomites. Infect. Control Hosp. Epidemiol. 27:1267-1269. [DOI] [PubMed] [Google Scholar]
- 408.Huang, S. S., D. S. Yokoe, V. L. Hinrichsen, L. S. Spurchise, R. Datta, I. Miroshnik, and R. Platt. 2006. Impact of routine intensive care unit surveillance cultures and resultant barrier precautions on hospital-wide methicillin-resistant Staphylococcus aureus bacteremia. Clin. Infect. Dis. 43:971-978. [DOI] [PubMed] [Google Scholar]
- 409.Huang, S. S., R. Datta, and R. Platt. 2006. Risk of acquiring antibiotic-resistant bacteria from prior room occupants. Arch. Intern. Med. 166:1945-1951. [DOI] [PubMed] [Google Scholar]
- 410.Huang, Y. C., C. F. Ho, C. J. Chen, L. H. Su, and T. Y. Lin. 2008. Comparative molecular analysis of community-associated and healthcare-associated methicillin-resistant Staphylococcus aureus isolates from children in northern Taiwan. Clin. Microbiol. Infect. 14:1167-1172. [DOI] [PubMed] [Google Scholar]
- 411.Huang, Y. C., K. P. Hwang, P. Y. Chen, C. J. Chen, and T. Y. Lin. 2007. Prevalence of methicillin-resistant Staphylococcus aureus nasal colonization among Taiwanese children in 2005 and 2006. J. Clin. Microbiol. 45:3992-3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Huang, Y. C., L. H. Lin, C. J. Chen, and T. Y. Lin. 2005. Nasal carriage of methicillin-resistant Staphylococcus aureus in school children without identifiable risk factors in northern Taiwan. Pediatr. Infect. Dis. J. 24:276-278. [DOI] [PubMed] [Google Scholar]
- 413.Huang, Y. C., Y. H. Chou, L. H. Su, R. I. Lien, and T. Y. Lin. 2006. Methicillin-resistant Staphylococcus aureus colonization and its association with infection among infants hospitalized in neonatal intensive care units. Pediatrics 118:469-474. [DOI] [PubMed] [Google Scholar]
- 414.Huang, Y. H., S. P. Tseng, J. M. Hu, J. C. Tsai, P. R. Hsueh, and L. J. Teng. 2007. Clonal spread of SCCmec type IV methicillin-resistant Staphylococcus aureus between community and hospital. Clin. Microbiol. Infect. 13:717-724. [DOI] [PubMed] [Google Scholar]
- 415.Huang, Y., L. Su, and T. Lin. 2004. Nasal carriage of methicillin-resistant Staphylococcus aureus in contacts of an adolescent with community-acquired disseminated disease. Pediatr. Infect. Dis. J. 23:919-922. [DOI] [PubMed] [Google Scholar]
- 416.Huijsdens, X. W., A. M. C. van Lier, E. van Kregten, L. Verhoef, M. G. van Santen-Verheuvel, E. Spalburg, and W. J. B. Wannet. 2006. Methicillin-resistant Staphylococcus aureus in Dutch soccer team. Emerg. Infect. Dis. 12:1584-1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Huijsdens, X. W., B. J. van Kijke, E. Spalburg, M. G. van Santen-Verheuvel, M. E. O. C. Heck, G. N. Pluister, A. Voss, W. J. B. Wannet, and A. J. de Neeling. 2006. Community-acquired MRSA and pig-farming. Ann. Clin. Microbiol. Antimicrob. 5:26. doi: 10.1186/1476-0711-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Huijsdens, X. W., M. G. van Santen-Verheuvel, E. Spalburg, M. E. Heck, G. N. Pluister, B. A. Eijkelkamp, A. J. de Neeling, and W. J. Wannet. 2006. Multiple cases of familial transmission of community-acquired methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 44:2994-2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Huijsdens, X. W., M. Janssen, N. H. M. Renders, A. Leenders, P. van Wijk, M. G. van Santen-Verheuvel, J. K. van-Driel, and G. Morroy. 2008. Methicillin-resistant Staphylococcus aureus in a beauty salon, the Netherlands. Emerg. Infect. Dis. 14:1197-1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Huijdens, X. W., T. Bosch, M. G. van Santen-Verheuvel, E. Spalburg, G. N. Pluister, M. van Luit, M. E. O. C. Heck, A. Haenen, and A. J. de Neeling. 2009. Molecular characterisation of PFGE non-typable methicillin-resistant Staphylococcus aureus in the Netherlands, 2007. Euro Surveill. 14(38):pii=19335. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19335. [DOI] [PubMed] [Google Scholar]
- 421.Hulten, K. G., S. L. Kaplan, B. E. Gonzalez, W. A. Hammerman, L. B. Lamberth, J. Veralovic, and E. O. Mason. 2006. Three-year surveillance of community onset health care-associated Staphylococcus aureus infections in children. Pediatr. Infect. Dis. J. 25:349-353. [DOI] [PubMed] [Google Scholar]
- 422.Hussain, F. M., S. Boyle-Vavra, and R. S. Daum. 2001. Community-acquired methicillin-resistant Staphylococcus aureus in healthy children attending an outpatient pediatric clinic. Pediatr. Infect. Dis. J. 20:763-767. [DOI] [PubMed] [Google Scholar]
- 423.Hussain, F. M., S. Boyle-Vavra, C. D. Bethel, and R. S. Daum. 2000. Current trends in community-acquired methicillin-resistant Staphylococcus aureus at a tertiary care pediatric facility. Pediatr. Infect. Dis. J. 19:1163-1166. [DOI] [PubMed] [Google Scholar]
- 424.Hyun, D. Y., E. O. Mason, A. Forbes, and S. L. Kaplan. 2009. Trimethoprim-sulfamethoxazole or clindamycin for treatment of community-acquired methicillin resistant Staphylococcus aureus skin and soft tissue infections. Pediatr. Infect. Dis. J. 28:57-59. [DOI] [PubMed] [Google Scholar]
- 425.Infectious Diseases Society of Washington, Public Health, Seattle and King County, Tacoma-Pierce County Department of Health, and Washington State Department of Health. 2007. Guidelines for the evaluation and management of community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections. Washington State Department of Health, Olympia, WA. http://www.doh.wa.gov/topics/antibiotics /MRSAguidelines.htm.
- 426.Inman, J. C., M. Rowe, M. Ghostine, and T. Fleck. 2008. Pediatric neck abscesses—changing organisms and empiric therapies. Laryngoscope 118:2111-2114. [DOI] [PubMed] [Google Scholar]
- 427.International Working Group on the Classification of Staphylococcal Cassette Chromosome Elements (IWG-SCC). 2009. Classification of staphylococcal cassette chromosome mec (SCCmec): guidelines for reporting novel SCCmec elements. Antimicrob. Agents Chemother. 53:4961-4967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Ito, T., K. Okuma, X. X. Ma, H. Yuzawa, and K. Hiramatsu. 2003. Insights on antibiotic resistance of Staphylococcus aureus from its whole genome: genomic island SCC. Drug Resist. Updat. 6:41-52. [DOI] [PubMed] [Google Scholar]
- 429.Ito, T., M. Iijima, T. Fukushima, M. Nonoyama, M. Ishii, T. Baranovich, T. Otsuka, T. Takano, and T. Yamamoto. 2008. Pediatric pneumonia death caused by community-acquired methicillin-resistant Staphylococcus aureus, Japan. Emerg. Infect. Dis. 14:1312-1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Ito, T., X. X. Ma, F. Takeuchi, K. Okuma, H. Yuzawa, and K. Hiramatsu. 2004. Novel type V staphylococcal cassette chromosome mec driven by a novel cassette chromosome recombinase, ccrC. Antimicrob. Agents Chemother. 48:2637-2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Ito, T., Y. Katayama, K. Asada, N. Mori, K. Tsutsumimoto, C. Tiensasitorn, and K. Hiramatsu. 2001. Structural comparison of three types of staphylococcal cassette chromosome mec integrated in the chromosome in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 45:1323-1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Iyer, S., and D. H. Jones. 2004. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: a retrospective analysis of clinical presentation and treatment of a local outbreak. J. Am. Acad. Dermatol. 50:854-858. [DOI] [PubMed] [Google Scholar]
- 433.Jacobus, C. H., C. J. Lindsell, S. D. Leach, G. J. Fermann, A. B. Kressel, and L. E. Rue. 2007. Prevalence and demographics of methicillin-resistant Staphylococcus aureus in culturable skin and soft tissue infections in an urban emergency department. BMC Emerg. Med. 7:19. doi: 10.1186/1471-227X-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Jahamy, H., R. Ganga, B. Al Raiy, S. Shemes, V. Nagappan, M. Sharma, K. Riederer, and R. Khatib. 2008. Staphylococcus aureus skin/soft tissue infections: the impact of SCCmec type and Panton-Valentine leukocidin. Scand. J. Infect. Dis. 40:601-606. [DOI] [PubMed] [Google Scholar]
- 435.James, L., R. J. Gorwitz, R. C. Jones, J. T. Watson, J. C. Hageman, D. B. Jernigan, Y. Lord, N. Cabelles, C. Cortes, R. G. Golash, J. S. Price, and S. I. Gerber. 2008. Methicillin-resistant Staphylococcus aureus infections among healthy full-term newborns. Arch. Dis. Child. Fetal Neonatal Ed. 93:F40-F44. [DOI] [PubMed] [Google Scholar]
- 436.Jenkins, T. C., B. D. McCollister, R. Sharma, K. K. McFann, N. E. Madinger, M. Barron, M. Bessesen, C. S. Price, and W. J. Burman. 2009. Epidemiology of healthcare-associated bloodstream infection caused by USA300 strains of methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Infect. Control Hosp. Epidemiol. 30:233-241. [DOI] [PubMed] [Google Scholar]
- 437.Jeong, H. Y., J. E. Lee, B. K. Choi, K. W. Seo, S. H. Park, Y. L. Kim, K. M. Baek, K. Lee, and D. K. Rhee. 2007. Molecular epidemiology of community-associated methicillin-resistant Staphylococcus aureus in Seoul, Korea (2003): pervasiveness of multidrug-resistant SCCmec type II methicillin-resistant S. aureus. Microb. Drug Resist. 13:178-185. [DOI] [PubMed] [Google Scholar]
- 438.Jevons, M. P. 1961. “Celbenin”-resistant staphylococci. BMJ 1:124-125. [Google Scholar]
- 439.Jeyaratnam, D., C. Reid, A. Kearns, and J. Klein. 2006. Community associated MRSA: an alert to paediatricians. Arch. Dis. Child. 91:511-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Johansson, P. J. H., E. B. Gustafsson, and H. Ringberg. 2007. High prevalence of MRSA in household contacts. Scand. J. Infect. Dis. 39:764-768. [DOI] [PubMed] [Google Scholar]
- 441.John, F. J., and J. A. Lindsay. 2008. Clones and drones: do variants of Panton-Valentine leukocidin extend the reach of community-associated methicillin-resistant Staphylococcus aureus? J. Infect. Dis. 197:175-178. [DOI] [PubMed] [Google Scholar]
- 442.Johnigan, R. H., K. D. Pereira, and M. D. Poole. 2003. Community-acquired methicillin-resistant Staphylococcus aureus in children and adolescents: changing trends. Arch. Otolaryngol. Head Neck Surg. 129:1049-1052. [DOI] [PubMed] [Google Scholar]
- 443.Johnson, J. K., T. Khoie, S. Shurland, K. Kreisel, O. C. Stine, and M. C. Roghmann. 2007. Skin and soft tissue infections caused by methicillin-resistant Staphylococcus aureus USA300 clone. Emerg. Infect. Dis. 13:1195-1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Johnson, L. B., A. A. Venugopal, J. Pawlak, and L. D. Saravolatz. 2006. Emergence of community-associated methicillin-resistant Staphylococcus aureus infection among patients with end-stage renal disease. Infect. Control Hosp. Epidemiol. 27:1057-1062. [DOI] [PubMed] [Google Scholar]
- 445.Johnson, L. B., J. Jose, F. Yousif, J. Pawlak, and L. D. Saravolatz. 2009. Prevalence of colonization with community-associated methicillin-resistant Staphylococcus aureus among end-stage renal disease patients and healthcare workers. Infect. Control Hosp. Epidemiol. 30:4-8. [DOI] [PubMed] [Google Scholar]
- 446.Johnson, P. N., R. P. Rapp, C. T. Nelson, J. S. Butler, S. Overman, and R. J. Kuhn. 2007. Characterization of community-acquired methicillin-resistant Staphylococcus aureus infections in children. Ann. Pharmacother. 41:1361-1367. [DOI] [PubMed] [Google Scholar]
- 447.Johnston, C. P., A. K. Stokes, T. Ross, M. Cai, K. C. Carroll, S. E. Cosgrove, and T. M. Perl. 2007. Staphylococcus aureus colonization among healthcare workers at a tertiary care hospital. Infect. Control Hosp. Epidemiol. 28:1404-1407. [DOI] [PubMed] [Google Scholar]
- 448.Johnston, C. P., L. Cooper, W. Ruby, K. C. Carroll, S. E. Cosgrove, and T. M. Perl. 2006. Epidemiology of community-acquired methicillin-resistant Staphylococcus aureus skin infections among healthcare workers in an outpatient clinic. Infect. Control Hosp. Epidemiol. 27:1133-1136. [DOI] [PubMed] [Google Scholar]
- 449.Jones, J. C., T. J. Rogers, P. Brookmeyer, W. M. Dunne, G. A. Storch, C. M. Coopersmith, V. J. Fraser, and D. K. Warren. 2007. Mupirocin resistance in patients colonized with methicillin-resistant Staphylococcus aureus in a surgical intensive care unit. Clin. Infect. Dis. 45:541-547. [DOI] [PubMed] [Google Scholar]
- 450.Jones, T. F., M. E. Kellum, S. S. Porter, M. Bell, and W. Schaffner. 2002. An outbreak of community-acquired foodborne illness caused by methicillin-resistant Staphylococcus aureus. Emerg. Infect. Dis. 8:82-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Juhász-Kaszanyitzky, E., S. Jánosi, P. Somogyi, A. Dán, L. van der Graaf-van Bloois, E. van Duijkeren, and J. A. Wagenaar. 2007. MRSA transmission between cows and humans. Emerg. Infect. Dis. 13:630-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Kadlec, K., and S. Schwarz. 2009. Identification of a novel trimethoprim resistance gene, dfrK, in a methicillin-resistant Staphylococcus aureus ST398 and its physical linkage to the tetracycline resistance gene tet(L). Antimicrob. Agents Chemother. 53:776-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.Kairam, N., M. E. Silverman, D. F. Salo, E. Baorto, B. Lee, and C. S. Amato. 8 July 2009. Cutaneous methicillin-resistant Staphylococcus aureus in a suburban community hospital pediatric emergency department. J. Emerg. Med. doi: 10.1016/j/jemermed.2009.05.015. [DOI] [PubMed]
- 454.Kajita, E., J. T. Okano, E. N. Bodine, S. P. Layne, and S. Blower. 2007. Modelling an outbreak of an emerging pathogen. Nat. Rev. Microbiol. 5:700-709. [DOI] [PubMed] [Google Scholar]
- 455.Kallen, A. J., J. Brunkard, Z. Moore, P. Budge, K. E. Arnold, G. Fosheim, L. Finelli, S. E. Beekmann, P. M. Polgreen, R. Gorwitz, and J. Hageman. 2009. Staphylococcus aureus community-acquired pneumonia during the 2006 to 2007 influenza season. Ann. Emerg. Med. 53:358-365. [DOI] [PubMed] [Google Scholar]
- 456.Kallen, A. J., T. J. Driscoll, S. Thornton, P. E. Olson, and M. R. Wallace. 2000. Increase in community-acquired methicillin-resistant Staphylococcus aureus at a naval medical center. Infect. Control Hosp. Epidemiol. 21:223-226. [DOI] [PubMed] [Google Scholar]
- 457.Kalorin, C. M., and E. H. Tobin. 2007. Community-associated methicillin-resistant Staphylococcus aureus causing Fournier's gangrene and genital infections. J. Urol. 177:967-971. [DOI] [PubMed] [Google Scholar]
- 458.Kampf, G., R. Jarosch, and H. Ruden. 1998. Limited effectiveness of CHX based hand disinfectants against methicillin-resistant Staphylococcus aureus (MRSA). J. Hosp. Infect. 38:297-303. [DOI] [PubMed] [Google Scholar]
- 459.Kanerva, M., S. Salmenlinna, J. Vuopio-Varkila, P. Lehtinen, T. Möttönen, M. J. Virtanen, and O. Lyytikäinen. 2009. Community-associated methicillin-resistant Staphylococcus aureus isolated in Finland in 2004 to 2006. J. Clin. Microbiol. 47:2655-2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Kaplan, S. L., K. G. Hulten, B. E. Gonzalez, W. A. Hammerman, L. Lamberth, J. Versalovic, and E. O. Mason. 2005. Three-year surveillance of community-acquired methicillin-resistant Staphylococcus aureus in children. Clin. Infect. Dis. 40:1785-1791. [DOI] [PubMed] [Google Scholar]
- 461.Karapsias, S., E. T. Piperaki, I. Spiliopoulou, G. Katsanis, and A. Tseleni-Kotsovili. 2008. Methicillin-resistant Staphylococcus aureus nasal carriage among healthy employees of the Hellenic Air Force. Euro Surveill. 13(40):pi=18999. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleID=18999. [DOI] [PubMed] [Google Scholar]
- 462.Kardén-Lilja, M., S. Ibrahim, J. Vuopio-Varkila, S. Salmenlinna, O. Lyytikäinen, L. Siira, and A. Virolainen. 2007. Panton-Valentine leukocidin genes and staphylococcal chromosomal cassette mec types amongst Finnish community-acquired methicillin-resistant Staphylococcus aureus strains, 1997-1999. Eur. J. Clin. Microbiol. Infect. Dis. 26:729-733. [DOI] [PubMed] [Google Scholar]
- 463.Katayama, Y., T. Ito, and K. Hiramatsu. 2000. A new class of genetic element, staphylococcus cassette chromosome mec, encodes methicillin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 44:1549-1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464.Kaul, A. F., and J. F. Jewett. 1981. Agents and techniques for disinfection of the skin. Surg. Gynecol. Obstet. 152:677-685. [PubMed] [Google Scholar]
- 465.Kayaba, H., K. Kodama, H. Tamura, and Y. Fujiwara. 1997. The spread of methicillin-resistant Staphylococcus aureus in a rural community: will it become a common microorganism colonizing among the general population? Jpn. J. Surg. 27:217-219. [DOI] [PubMed] [Google Scholar]
- 466.Kazakova, S. V., J. C. Hageman, M. Matava, A. Srinivasan, L. Phelan, B. Garfinkel, T. Boo, S. McAllister, J. Anderson, B. Jensen, D. Dodson, D. Lonsway, L. K. McDougal, M. Arduino, V. J. Fraser, G. Killgore, F. C. Tenover, S. Cody, and D. B. Jernigan. 2005. A clone of methicillin-resistant Staphylococcus aureus among professional football players. N. Engl. J. Med. 352:468-475. [DOI] [PubMed] [Google Scholar]
- 467.Kefala-Agoropoulou, K., E. Protonotarious, D. Vitti, S. Sarafidou, A. Anastasiou, K. Kollios, and E. Roilides. 2010. Life-threatening infection due to community-acquired methicillin-resistant Staphylococcus aureus: case report and review of the literature. Eur. J. Pediatr. 169:47-53. [DOI] [PubMed] [Google Scholar]
- 468.Kennedy, A. D., M. Otto, K. R. Braughton, A. R. Whitney, L. Chen, B. Mathema, J. R. Mediavilla, K. A. Byrne, L. D. Parkins, F. C. Tenover, B. N. Kreiswirth, J. M. Musser, and F. R. DeLeo. 2008. Epidemic community-associated methicillin-resistant Staphylococcus aureus: recent clonal expansion and diversification. Proc. Natl. Acad. Sci. U. S. A. 105:1327-1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Kerttula, A. M., O. Lyytikäinen, M. Kardén-Lilja, S. Ibrahem, S. Salmenlinna, A. Virolainen, and J. Vuopio-Varkila. 2007. Nationwide trends in molecular epidemiology of methicillin-resistant Staphylococcus aureus, Finland, 1997-2004. BMC Infect. Dis. 7:94. doi: 10.1186/1471-2334-7-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Khan, M. A., J. R. Greig, and J. Jayamohan. 2000. Community-acquired methicillin-resistant Staphylococcus aureus brain abscess in an immunocompetent individual. Scand. J. Infect. Dis. 32:423-424. [DOI] [PubMed] [Google Scholar]
- 471.Khanna, T., R. Friendship, C. Dewey, and J. S. Weese. 2008. Methicillin-resistant Staphylococcus aureus colonization in pigs and pig farmers. Vet. Microbiol. 128:298-303. [DOI] [PubMed] [Google Scholar]
- 472.Kilic, A., G. Mert, Z. Senses, O. Bedir, H. Aydogan, A. C. Basustaoglu, and P. C. Appelbaum. 2008. Molecular characterization of methicillin-resistant Staphylococcus aureus nasal isolates from Turkey. Antonie Van Leeuwenhoek 94:615-619. [DOI] [PubMed] [Google Scholar]
- 473.Kilic, A., H. Li, C. W. Stratton, and Y. W. Tang. 2006. Antimicrobial susceptibility patterns and and staphylococcal cassette chromosome mec types of, as well as Panton-Valentine leukocidin occurrence among, methicillin-resistant Staphylococcus aureus isolates from children and adults in middle Tennessee. J. Clin. Microbiol. 44:4436-4440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Kim, E. S., J. S. Song, H. J. Lee, P. G. Choe, K. H. Park, J. H. Cho, W. B. Park, S. H. Kim, J. H. Bang, D. M. Kim, K. U. Park, S. Shin, M. S. Lee, H. J. Choi, N. J. Kim, E. C. Kim, M. Oh, H. B. Kim, and K. W. Choe. 2007. A survey of community-associated strains of methicillin-resistant Staphylococcus aureus in Korea. J. Antimicrob. Chemother. 60:1108-1114. [DOI] [PubMed] [Google Scholar]
- 475.King, M. D., B. J. Humphrey, Y. F. Wang, E. V. Kourbatova, S. M. Ray, and H. M. Blumberg. 2006. Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. Ann. Intern. Med. 144:309-317. [DOI] [PubMed] [Google Scholar]
- 476.Kiran, R. V., B. McCampbell, A. P. Angeles, R. D. Montilla, C. Medina, A. Mitra, J. Gaughn, J. Spears, and A. Mitra. 2006. Increased prevalence of community-acquired methicillin-resistant Staphylococcus aureus in hand infections at an urban medical center. Plast. Reconstr. Surg. 118:161-166. [DOI] [PubMed] [Google Scholar]
- 477.Kirby, W. M. M. 1944. Extraction of a highly potent penicillin inactivator from penicillin resistant staphylococci. Science 99:452-453. [DOI] [PubMed] [Google Scholar]
- 478.Kitai, S., A. Shimizu, J. Kawano, E. Sato, C. Nakano, T. Uji, and H. Kitagawa. 2005. Characterization of Staphylococcus aureus isolated from retail raw chicken meat in Japan. J. Vet. Med. Sci. 67:107-110. [DOI] [PubMed] [Google Scholar]
- 479.Klevens, R. M., J. R. Edwards, F. C. Tenover, L. C. McDonald, T. Horan, R. Gaynes, and the National Nosocomial Infections Surveillance System. 2006. Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992-2003. Clin. Infect. Dis. 42:389-391. [DOI] [PubMed] [Google Scholar]
- 480.Klevens, R. M., M. A. Morrison, S. K. Fridkin, A. Reingold, S. Petit, K. Gershman, S. Ray, L. H. Harrison, R. Lynfield, G. Dumyati, J. M. Townes, A. S. Craig, G. Fosheim, L. K. McDougal, F. C. Tenover, and Active Bacterial Core Surveillance of the Emerging Infections Program Network. 2006. Community-associated methicillin-resistant Staphylococcus aureus and healthcare risk factors. Emerg. Infect. Dis. 12:1991-1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 481.Klevens, R. M., M. A. Morrison, and J. Nadle. 2007. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 298:1763-1771. [DOI] [PubMed] [Google Scholar]
- 482.Kluytmans, J., A. Van Belkum, and H. Verbrugh. 1997. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin. Microbiol. Rev. 10:505-520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 483.Kniehl, E., A. Becker, and D. H. Forster. 2005. Bed, bath and beyond: pitfalls in the prompt eradication of methicillin-resistant Staphylococcus aureus carrier status in healthcare workers. J. Hosp. Infect. 59:180-187. [DOI] [PubMed] [Google Scholar]
- 484.Ko, K. S., J. Y. Lee, J. Y. Baek, K. R. Peck, J. Y. Rhee, K. T. Kwon, S. T. Heo, K. M. Ahn, and J. H. Song. 2008. Characterization of Staphylococcus aureus nasal carriage from children attending an outpatient clinic in Seoul, Korea. Microb. Drug Resist. 14:37-44. [DOI] [PubMed] [Google Scholar]
- 485.Kollef, M. H., A. Shorr, Y. P. Tabak, V. Gupta, L. Z. Liu, and R. S. Johannes. 2005. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest 128:3854-3862. [DOI] [PubMed] [Google Scholar]
- 486.Koreen, L., S. V. Ramaswamy, E. A. Graviss, S. Naidich, J. M. Musser, and B. N. Kreiswirth. 2004. spa typing method for discriminating among Staphylococcus aureus isolates: implications for use of a single marker to detect genetic micro- and macrovariation. J. Clin. Microbiol. 42:792-799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 487.Kourbatova, E. V., J. S. Halvosa, M. D. King, S. M. Ray, N. White, and H. M. Blumberg. 2005. Emergence of community-associated methicillin-resistant Staphylococcus aureus USA 300 clone as a cause of health care-associated infections among patients with prosthetic joint infections. Am. J. Infect. Control 33:385-391. [DOI] [PubMed] [Google Scholar]
- 488.Kravitz, G. R., D. J. Dries, M. L. Peterson, and P. M. Schlievert. 2005. Pupura fulminans due to Staphylococcus aureus. Clin. Infect. Dis. 40:941-947. [DOI] [PubMed] [Google Scholar]
- 489.Krueke, G. W., D. E. Grimes, R. M. Grimes, and T. D. Dang. 2009. Antibiotic resistance in Staphylococcus aureus-containing cutaneous abscesses of patients with HIV. Am. J. Emerg. Med. 27:344-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 490.Krziwanek, K., C. Luger, B. Sammer, S. Stumvoll, M. Stammler, S. Metz-Gercek, and H. Mittermayer. 2007. PVL-positive MRSA in Austria. Eur. J. Clin. Microbiol. Infect. Dis. 26:931-935. [DOI] [PubMed] [Google Scholar]
- 491.Krziwanek, K., S. Metz-Gercek, and H. Mittermayer. 2009. Methicillin-resistant Staphylococcus aureus ST398 from human patients, Upper Austria. Emerg. Infect. Dis. 15:766-769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 492.Kuehnert, M. J., D. Kruszon-Moran, H. A. Hill, G. McQuillan, S. K. McAllister, G. Fosheim, L. K. McDougal, J. Chaitram, B. Jensen, S. K. Fridkin, G. Killgore, and F. C. Tenover. 2006. Prevalence of Staphylococcus aureus nasal colonization in the United States. J. Infect. Dis. 193:172-179. [DOI] [PubMed] [Google Scholar]
- 493.Kuehnert, M. J., H. A. Hill, B. A. Kupronis, J. I. Tokars, S. L. Solomon, and D. B. Jernigan. 2005. Methicillin-resistant Staphylococcus aureus hospitalizations, United States. Emerg. Infect. Dis. 11:868-872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 494.Kuint, J., A. Barzilai, G. Regev-Yochay, E. Rubinstein, N. Keller, and A. Maayan-Metzger. 2007. Comparison of community-acquired methicillin-resistant Staphylococcus aureus to other staphylococcal species in a neonatal intensive care unit. Eur. J. Pediatr. 166:319-325. [DOI] [PubMed] [Google Scholar]
- 495.Kumari, D. N. P., T. C. Haji, V. Keep, P. M. Hawkey, V. Duncanson, and E. Flower. 1998. Ventilation grilles as a potential source of methicillin-resistant Staphylococcus aureus causing an outbreak in an orthopaedic ward at a district general hospital. J. Hosp. Infect. 39:127-133. [DOI] [PubMed] [Google Scholar]
- 496.Kurbis, C. A., and J. L. Wylie. 2001. Community-based cluster of methicillin-resistant Staphylococcus aureus in Manitoba. Can. J. Infect. Dis. 12:149-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 497.Kwon, N. H., K. T. Park, J. S. Moon, W. K. Jung, S. H. Kim, J. M. Kim, S. K. Hong, H. C. Koo, Y. S. Joo, and Y. H. Park. 2005. Staphylococcal cassette chromosome mec (SCCmec) characterization and molecular analysis for methicillin-resistant Staphylococcus aureus and novel SCCmec subtype IVg isolated from bovine milk in Korea. J. Antimicrob. Chemother. 56:624-632. [DOI] [PubMed] [Google Scholar]
- 498.Labandeira-Rey, M., F. Couzon, S. Boisset, E. L. Brown, M. Bes, Y. Benito, E. M. Barbu, V. Vazquez, M. Höök, J. Etienne, F. Vandenesch, and M. G. Bowden. 2007. Staphylococcus aureus Panton-Valentine leukocidin causes necrotizing pneumonia. Science 315:1130-1133. [DOI] [PubMed] [Google Scholar]
- 499.Laibl, V. R., J. S. Sheffield, S. Roberts, D. D. McIntire, S. Trevino, and G. D. Wendel. 2005. Clinical presentation of community-acquired methicillin-resistant Staphylococcus aureus in pregnancy. Obstet. Gynecol. 106:461-465. [DOI] [PubMed] [Google Scholar]
- 500.Lalani, T., J. J. Federspiel, H. W. Boucher, T. H. Rude, I. G. Bae, M. J. Rybak, G. T. Tonthat, G. R. Corey, M. E. Stryjewski, G. Sakoulas, V. H. Chu, J. Alder, J. N. Steenbergen, S. A. Luperchio, M. Campion, C. W. Woods, and V. G. Fowler. 2008. Associations between the genotype of Staphylococcus aureus bloodstream isolates and the clinical characteristics and outcomes of bacteremic patients. J. Clin. Microbiol. 46:2890-2896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 501.LaMar, J. E., R. B. Carr, C. Zinderman, and K. McDonald. 2003. Sentinel cases of community-acquired methicillin-resistant Staphylococcus aureus onboard a naval ship. Mil. Med. 168:135-138. [PubMed] [Google Scholar]
- 502.Lamaro-Cardoso, J., M. Castanheira, R. M. de Oliviera, S. A. Silva, A. C. C. Pignatari, R. E. Mendes, F. C. Pimenta, and A. L. S. S. Andrade. 2007. Carriage of methicillin-resistant Staphylococcus aureus in children in Brazil. Diagn. Microbiol. Infect. Dis. 57:467-470. [DOI] [PubMed] [Google Scholar]
- 503.Lambert, R. J. W. 2004. Comparative analysis of antibiotic and antimicrobicidal biocide susceptibility data in clinical isolates of methicillin-sensitive Staphylococcus aureus, methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa between 1989 and 2000. J. Appl. Microbiol. 97:699-711. [DOI] [PubMed] [Google Scholar]
- 504.Landen, M. G. 1997. An outbreak of boils associated with steambathing. State of Alaska epidemiology bulletin, no. 27. Alaska Department of Health and Social Services, Division of Public Health, Anchorage, AK.
- 505.Landers, T. F., R. E. Harris, T. E. Wittum, and K. B. Stevenson. 2009. Colonization with Staphylococcus aureus and methicillin-resistant S. aureus among a sample of homeless individuals, Ohio. Infect. Control Hosp. Epidemiol. 30:801-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 506.LaPlant, K. L., M. J. Rybak, M. Amjad, and G. W. Kaatz. 2007. Antimicrobial susceptibility and staphylococcal chromosome cassette mec type in community- and hospital-associated methicillin-resistant Staphylococcus aureus. Pharmacotherapy 27:3-10. [DOI] [PubMed] [Google Scholar]
- 507.Larcombe, L., J. Waruk, J. Schellenberg, and M. Ormond. 2007. Rapid emergence of methicillin-resistant Staphylococcus aureus among children and adolescents in northern Manitoba, 2003-2006. Can. Commun. Dis. Rep. 33:9-14. [PubMed] [Google Scholar]
- 508.Larsen, A. R., M. Stegger, R. V. Goering, M. Sørum, and R. Skov. 2007. Emergence and dissemination of the methicillin-resistant Staphylococcus aureus USA300 clone in Denmark (2000-2005). Euro Surveill. 12(2):pii=682. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=682. [Google Scholar]
- 509.Larsen, A. R., M. Stegger, S. Böcher, M. Sørum, D. L. Monnet, and R. L. Skov. 2009. Emergence and characterization of community-associated methicillin-resistant Staphylococcus aureus infections in Denmark, 1999 to 2006. J. Clin. Microbiol. 47:73-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 510.Larsen, A. R., S. Bocher, M. Stegger, R. Goering, L. V. Pallesen, and R. Skov. 2008. Epidemiology of European community-associated methicillin-resistant Staphylococcus aureus clonal complex 80 type IV strains isolated in Denmark from 1993 to 2004. J. Clin. Microbiol. 46:62-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Larson, E. L., H. Norton, A. Carrie, J. D. Pyrek, S. M. Sparks, E. U. Cagatay, and J. M. Bartkus. 1998. Changes in bacterial flora associated with skin damage on hands of health care personnel. Am. J. Infect. Control 26:513-521. [DOI] [PubMed] [Google Scholar]
- 512.Laupland, K. B., T. Ross, and D. B. Gregson. 2008. Staphylococcus aureus bloodstream infections: risk factors, outcomes, and the influence of methicillin-resistance in Calgary, Canada, 2000-2006. Clin. Infect. Dis. 198:336-343. [DOI] [PubMed] [Google Scholar]
- 513.Laurens, M. B., R. M. Becker, J. K. Johnson, J. S. Wolf, and K. L. Kotloff. 2008. MRSA with progression from otitis media and sphenoid sinusitis to clival osteomyelitis, pachymeningitis and abducens nerve palsy in an immunocompetent 10-year-old patient. Int. J. Pediatr. Otorhinolaryngol. 72:945-951. [DOI] [PubMed] [Google Scholar]
- 514.Layton, M. C., M. Perez, P. Heald, and J. E. Patterson. 1993. An outbreak of mupirocin-resistant Staphylococcus aureus on a dermatology ward associated with an environmental reservoir. Infect. Control Hosp. Epidemiol. 14:369-375. [DOI] [PubMed] [Google Scholar]
- 515.Layton, M. C., W. J. Hierholzer, and J. E. Patterson. 1995. The evolving epidemiology of methicillin-resistant Staphylococcus aureus at a university hospital. Infect. Control Hosp. Epidemiol. 16:12-17. [DOI] [PubMed] [Google Scholar]
- 516.Le, J., and J. M. Lieberman. 2006. Management of community-associated methicillin-resistant Staphylococcus aureus infections in children. Pharmacotherapy 26:1758-1770. [DOI] [PubMed] [Google Scholar]
- 517.LeBlanc, L., J. Pepin, K. Toulouse, M. F. Oullette, M. A. Coulombe, M. P. Corriveau, and M. E. Alary. 2006. Fluoroquinolones and risk for methicillin-resistant Staphylococcus aureus, Canada. Emerg. Infect. Dis. 12:1398-1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 518.Lee, G. M., S. S. Huang, S. L. Rifas-Shiman, V. L. Hinrichsen, S. I. Pelton, K. Kleinman, W. P. Hanage, M. Lipsitch, A. J. McAdam, and J. A. Finkelstein. 2009. Epidemiology and risk factors for Staphylococcus aureus colonization in children in the post-PVC7 era. BMC Infect. Dis. 9:110. doi: 10.1186/1471-2334-9-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Lee, J. H. 2003. Methicillin (oxacillin)-resistant Staphylococcus aureus strains isolated from major food animals and their potential transmission to humans. Appl. Environ. Microbiol. 69:6489-6494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 520.Lee, M. C., A. M. Rios, M. F. Aten, A. A. Mejias, A. Cavuoti, G. H. McCracken, and R. D. Hardy. 2004. Management and outcome of children with skin and soft tissue abscesses caused by community-acquired methicillin-resistant Staphylococcus aureus. Pediatr. Infect. Dis. J. 23:123-127. [DOI] [PubMed] [Google Scholar]
- 521.Lee, N. E., M. M. Taylor, E. Bancroft, P. J. Ruane, M. Morgan, L. McCoy, and P. A. Simon. 2005. Risk factors for community-associated methicillin-resistant Staphylococcus aureus skin infections among HIV-positive men who have sex with men. Clin. Infect. Dis. 40:1529-1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 522.Lee, S. Y., J. Y. Kim, J. H. Kim, S. Y. Kim, C. Park, Y. S. Park, Y. H. Seo, and Y. K. Cho. 2009. A case of primary infective endocarditis caused by community-associated methicillin-resistant Staphylococcus aureus in a healthy individual and colonization in the family. Yonsei Med. J. 50:152-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 523.Lee, T. C., M. M. Carrick, B. G. Scott, J. C. Hodges, and H. Q. Pham. 2007. Incidence and clinical characteristics of methicillin-resistant Staphylococcus aureus necrotizing fasciitis in a large urban hospital. Am. J. Surg. 194:809-813. [DOI] [PubMed] [Google Scholar]
- 524.Lee, Y. L., T. Cesario, G. Gupta, L. Flionis, C. Tran, M. Decker, and L. Thrupp. 1997. Surveillance of colonization and infection with Staphylococcus aureus susceptible or resistant to methicillin in a community skilled-nursing facility. Am. J. Infect. Control 25:312-321. [DOI] [PubMed] [Google Scholar]
- 525.Lee, Y. T., J. C. Lin, N. C. Wang, M. Y. Peng, and F. Y. Chang. 2007. Necrotizing fasciitis in a medical center in northern Taiwan: emergence of methicillin-resistant Staphylococcus aureus in the community. J. Microbiol. Immunol. Infect. 40:335-341. [PubMed] [Google Scholar]
- 526.Leman, R., F. Alvarado-Ramy, S. Pocock, N. Barg, M. Kellum, S. McAllister, J. Cheek, and M. Kuehnert. 2004. Nasal carriage of methicillin-resistant Staphylococcus aureus in an American Indian population. Infect. Control Hosp. Epidemiol. 25:121-125. [DOI] [PubMed] [Google Scholar]
- 527.Lemonick, D. M. 26 March 2009. Non-tropical pyomyositis caused by methicillin-resistant Staphylococcus aureus: an unusual cause of bilateral leg pain. J. Emerg. Med. doi: 10.1016/j.jemermed.2008.12.020. [DOI] [PubMed]
- 528.Leonard, F. C., and B. K. Markey. 2008. Meticillin-resistant Staphylococcus aureus in animals: a review. Vet. J. 175:27-36. [DOI] [PubMed] [Google Scholar]
- 529.Lescure, F. X., G. Locher, M. Eveillard, M. Biendo, S. V. Agt, G. Le Loup, Y. Douadi, O. Ganry, F. Vandenesch, F. Eb, J. L. Schmidt, and J. Etienne. 2006. Community-acquired infection with healthcare-associated methicillin-resistant Staphylococcus aureus: the role of nursing care. Infect. Control Hosp. Epidemiol. 27:1213-1218. [DOI] [PubMed] [Google Scholar]
- 530.Levine, D. P., R. D. Cushing, J. Jui, and W. J. Brown. 1982. Community-acquired methicillin-resistant Staphylococcus aureus endocarditis in the Detroit Medical Center. Ann. Intern. Med. 97:330-338. [DOI] [PubMed] [Google Scholar]
- 531.Levy, I., J. Katz, E. Solter, Z. Samra, B. Vidne, E. Birk, S. Ashkenazi, and O. Dagan. 2005. Chlorhexidine-impregnated dressing for the prevention of colonization of central venous catheters in infants and children. Pediatr. Infect. Dis. J. 24:676-679. [DOI] [PubMed] [Google Scholar]
- 532.Lewis, H. C., K. Mølbak, C. Reese, F. M. Aarestrup, M. Selchau, M. Sørum, and R. L. Skov. 2008. Pigs as a source of methicillin-resistant Staphylococcus aureus CC398 infections in humans, Denmark. Emerg. Infect. Dis. 14:1383-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 533.L'Hériteau, F., J. Lucet, A. Scanvic, and E. Bouvet. 1999. Community-acquired methicillin-resistant Staphylococcus aureus and familial transmission. JAMA 282:1038-1039. [DOI] [PubMed] [Google Scholar]
- 534.Liassine, N., R. Auckenthaler, M. Descombes, M. Bes, F. Vandenesch, and J. Etienne. 2004. Community-acquired methicillin-resistant Staphylococcus aureus isolated in Switzerland contains the Panton-Valentine leukocidin or exfoliative toxin genes. J. Clin. Microbiol. 42:825-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 535.Lim, M. S. C., C. L. Marshall, and D. Spelman. 2006. Carriage of multiple subtypes of methicillin-resistant Staphylococcus aureus by intensive care unit patients. Infect. Control Hosp. Epidemiol. 27:1063-1067. [DOI] [PubMed] [Google Scholar]
- 536.Lim, T. T., F. N. Chong, F. G. O'Brien, and W. B. Grubb. 2003. Are all community methicillin-resistant Staphylococcus aureus related? A comparison of their mec regions. Pathology 35:336-343. [PubMed] [Google Scholar]
- 537.Limbago, B., G. E. Fosheim, V. Schoonover, C. E. Crane, J. Nadle, S. Petit, D. Heltzel, S. M. Ray, L. H. Harrison, R. Lynfield, G. Dumyali, J. M. Townes, W. Schaffner, Y. Mu, and S. K. Fridkin for the Active Bacterial Core Surveillance (ABCs) MRSA Investigators. 2009. Characterization of methicillin-resistant Staphylococcus aureus isolates collected in 2005 and 2006 with invasive disease: a population-based analysis. J. Clin. Microbiol. 47:1344-1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 538.Lin, J., K. S. Yeh, H. T. Liu, and J. H. Lin. 2009. Staphylococcus aureus isolated from pork and chicken carcasses in Taiwan: prevalence and antimicrobial susceptibility. J. Food Prot. 72:608-611. [DOI] [PubMed] [Google Scholar]
- 539.Lin, Y. C., T. L. Lauderdale, H. M. Lin, P. C. Chen, M. F. Cheng, K. S. Hsieh, and Y. C. Liu. 2007. An outbreak of methicillin-resistant Staphylococcus aureus infection in patients of a pediatric intensive care unit and high carriage rate among health care workers. J. Microbiol. Immunol. Infect. 40:325-334. [PubMed] [Google Scholar]
- 540.Lina, G., Y. Piémont, F. Godail-Gamot, M. Bes, M. Peter, V. Gauduchon, F. Vadenesch, and J. Etienne. 1999. Involvement of Panton-Valentine-leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin. Infect. Dis. 29:1128-1132. [DOI] [PubMed] [Google Scholar]
- 541.Lindenmayer, J., S. Schoenfeld, R. O'Grady, and J. Carney. 1998. Methicillin-resistant Staphylococcus aureus in a high-school wrestling team and in the surrounding community. Arch. Intern. Med. 158:895-899. [DOI] [PubMed] [Google Scholar]
- 542.Liu, C., and H. F. Chambers. 2003. Staphylococcus aureus with heterogeneous resistance to vancomycin: epidemiology, clinical significance, and critical assessment of diagnostic methods. Antimicrob. Agents Chemother. 47:3040-3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 543.Liu, C., C. J. Graber, M. Karr, B. A. Diep, L. Basuino, B. S. Schwartz, M. C. Enright, J. O'Hanlon, J. C. Thomas, F. Perdreau-Remington, S. Gordon, H. Gunthorpe, R. Jacobs, P. Jensen, G. Leoung, J. S. Rumack, and H. F. Chambers. 2008. A population-based study of the incidence and molecular epidemiology of methicillin-resistant Staphylococcus aureus disease in San Francisco, 2004-2005. Clin. Infect. Dis. 46:1637-1646. [DOI] [PubMed] [Google Scholar]
- 544.Lloyd, D. H. 2007. Reservoirs of antimicrobial resistance in pet animals. Clin. Infect. Dis. 45:S148-S152. [DOI] [PubMed] [Google Scholar]
- 545.Lo, B. M., and B. A. Fickenscher. 2008. Primary pyomyositis caused by CA-MRSA. Int. J. Emerg. Med. 1:331-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 546.Lo, B. M., and E. A. Erwin. 2008. Missed epidural brain abscess after furunculosis. Am. J. Emerg. Med. 26:522.e3-522.e4. [DOI] [PubMed] [Google Scholar]
- 547.Lo, W. T., W. J. Lin, M. H. Tseng, J. J. Lu, S. Y. Lee, M. L. Chu, and C. C. Wang. 2007. Nasal carriage of a single clone of community-acquired methicillin-resistant Staphylococcus aureus among kindergarten attendees in northern Taiwan. BMC Infect. Dis. 7:51. doi: 10.1186/1471-2334-7-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 548.Lo, W. T., W. J. Lin, M. H. Tseng, S. R. Wang, M. L. Chu, and C. C. Wang. 2008. Risk factors and molecular analysis of Panton-Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus colonization in healthy children. Pediatr. Infect. Dis. J. 27:713-718. [DOI] [PubMed] [Google Scholar]
- 549.Lodise, T. P., C. D. Miller, J. Graves, A. Evans, E. Graffunder, M. Helmecke, and K. Stellerecht. 2008. Predictors of high vancomycin MIC values among patients with methicillin-resistant Staphylococcus aureus bacteremia. J. Antimicrob. Chemother. 62:1138-1141. [DOI] [PubMed] [Google Scholar]
- 550.Loeb, M., C. Main, C. Walker-Dilks, and A. Eady. 2003. Antimicrobial drugs for treating methicillin-resistant Staphylococcus aureus colonization. Cochrane Database Syst. Rev. 4:CD003340. doi: 10.1002/14651858.CD003340. [DOI] [PubMed] [Google Scholar]
- 551.Loeffler, A., A. K. Boag, J. Sung, J. A. Lindsay, L. Guardabassi, A. Dalsgaard, H. Smith, K. B. Steven, and D. H. Lloyd. 2005. Prevalence of methicillin-resistant Staphylococcus aureus among staff and pets in a small animal referral hospital in the UK. J. Antimicrob. Chemother. 56:692-697. [DOI] [PubMed] [Google Scholar]
- 552.Loeffler, A., A. M. Kearns, M. J. Ellington, L. J. Smith, V. E. Unt, J. A. Lindsay, D. U. Pfeiffer, and D. H. Lloyd. 2009. First isolation of MRSA ST398 from UK animals: a new challenge for infection control teams? J. Hosp. Infect. 72:269-271. [DOI] [PubMed] [Google Scholar]
- 553.Löffler, B., M. Hussain, M. Grundmeier, M. Brück, D. Holzinger, G. Varga, J. Roth, B. C. Kahl, R. A. Proctor, and G. Peters. 2010. Staphylococcus aureus Panton-Valentine leukocidin is a very potent cytotoxic factor for human neutrophils. PLoS Pathog. 6:e1000715. doi: 10.1371/journal.ppat.1000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 554.Longtin, Y., P. Sudre, P. François, J. Schrenzel, C. Aramburu, R. Pastore, A. Gervaix, G. Renzi, D. Pittet, and S. Harbarth. 2009. Community-associated methicillin-resistant Staphylococcus aureus: risk factors for infection, and long-term follow-up. Clin. Microbiol. Infect. 15:552-559. [DOI] [PubMed] [Google Scholar]
- 555.Lorette, G., P. Beaulieu, F. A. Allaert, A. Mahmoudi, and V. Jarlier. 2009. Superficial community-acquired skin infections: prevalence of bacteria and antibiotic susceptibility in France. J. Eur. Acad. Dermatol. Venereol. 23:1423-1426. [DOI] [PubMed] [Google Scholar]
- 556.Loughrey, A., B. C. Millar, C. E. Goldsmith, P. J. Rooney, and J. E. Moore. 2007. Emergence of community-associated MRSA (CA-MRSA) in Northern Ireland. Ulster Med. J. 76:68-71. [PMC free article] [PubMed] [Google Scholar]
- 557.Loveday, H. P., C. M. Pellowe, S. R. L. J. Jones, and R. J. Pratt. 2006. A systematic review of the evidence for interventions for the prevention and control of meticillin-resistant Staphylococcus aureus (1996-2004): report to the Joint MRSA Working Party (subgroup A). J. Hosp. Infect. 63S:S45-S70. [DOI] [PubMed] [Google Scholar]
- 558.Lowbury, E. J., and H. A. Lilly. 1973. Use of 4 per cent chlorhexidine detergent solution (Hibiscrub) and other methods of skin disinfection. Br. Med. J. i:510-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 559.Lowy, F. D. 1998. Staphylococcus aureus infections. N. Engl. J. Med. 339:520-532. [DOI] [PubMed] [Google Scholar]
- 560.Lowy, F. D., A. E. Aiello, M. Bhat, V. D. Johnson-Lawrence, M. H. Lee, E. Burrell, L. N. Wright, G. Vasquez, and E. L. Larsen. 2007. Staphylococcus aureus colonization and infection in New York state prisons. J. Infect. Dis. 196:911-918. [DOI] [PubMed] [Google Scholar]
- 561.Lu, P. L., J. C. Tsai, Y. W. Chiu, F. Y. Chang, Y. W. Chen, C. F. Hsiao, and L. K. Siu. 2007. Methicillin-resistant Staphylococcus aureus carriage, infection and transmission in dialysis patients, healthcare workers and their family members. Nephrol. Dial. Transplant. 23:1659-1665. [DOI] [PubMed] [Google Scholar]
- 562.Luh, K. T., P. R. Hsueh, L. J. Teng, H. J. Pan, Y. C. Chen, J. J. Lu, J. J. Wu, and S. W. Ho. 2000. Quinupristin-dalfopristin resistance among Gram-positive bacteria in Taiwan. Antimicrob. Agents Chemother. 44:3374-3380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 563.Ma, S. H., Y. S. Lee, S. H. Lee, H. K. Kim, J. S. Jin, E. K. Shin, and J. C. Lee. 2007. Meticillin-resistant Staphylococcus aureus clones with distinct clinical and microbiological features in a Korean community. J. Med. Microbiol. 56:866-868. [DOI] [PubMed] [Google Scholar]
- 564.Ma, X. X., A. Galiana, W. Pedreira, M. Mowszowicz, I. Christophersen, S. Machiavello, L. Lope, S. Benaderet, F. Buela, W. Vincento, M. Albini, O. Bertaux, I. Constenla, H. Bagnulo, L. Llosa, T. Ito, and K. Hiramatsu. 2005. Community-acquired methicillin-resistant Staphylococcus aureus, Uruguay. Emerg. Infect. Dis. 11:973-976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 565.Ma, X. X., T. Ito, C. Tiensasitorn, M. Jamklang, P. Chongtrakool, S. Boyle-Vavra, R. S. Daum, and K. Hiramatsu. 2002. Novel type of staphylococcal cassette chromosome mec identified in community-acquired methicillin-resistant Staphylococcus aureus strains. Antimicrob. Agents Chemother. 46:1147-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 566.Ma, X. X., T. Ito, P. Chongtrakool, and K. Hiramatsu. 2006. Predominace of clones carrying Panton-Valentine leukocidin genes among methicillin-resistant Staphylococcus aureus strains isolated in Japansese hospitals from 1979 to 1985. J. Clin. Microbiol. 44:4515-4527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 567.Macfarlane, M., A. Leavy, J. McCaughan, R. Fair, and A. J. M. Reid. 2007. Successful decolonization of meticillin-resistant Staphylococcus aureus in pediatric patients with cystic fibrosis (CF) using a three-step protocol. J. Hosp. Infect. 65:231-236. [DOI] [PubMed] [Google Scholar]
- 568.Maclean, M., S. J. MacGregor, J. G. Anderson, and G. Woolsey. 2008. High-intensity narrow-spectrum light inactivation and wavelength sensitivity of Staphylococcus aureus. FEMS Microbiol. Lett. 285:227-232. [DOI] [PubMed] [Google Scholar]
- 569.Madariaga, M. G., F. Ullrich, and S. Swindells. 2009. Low prevalence of community-acquired methicillin-resistant Staphylococcus aureus colonization and apparent lack of correlation with sexual behavior among HIV-infected patients in Nebraska. Clin. Infect. Dis. 48:1485-1487. [DOI] [PubMed] [Google Scholar]
- 570.Magilner, D., M. M. Byerly, and D. M. Cline. 2008. The prevalence of methicillin resistant Staphylococcus aureus (CA-MRSA) in skin abscesses presenting to the pediatric emergency department. N. C. Med. J. 69:351-354. [PubMed] [Google Scholar]
- 571.Magira, E. E., D. Zervakis, C. Routsi, M. Kontogiori, C. Roussos, S. Nanas, and S. Mentzelopoulos. 2007. Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton-Valentine leukocidin genes: a lethal cause of pneumonia in an adult immunocompetent patient. Scand. J. Infect. Dis. 39:466-469. [DOI] [PubMed] [Google Scholar]
- 572.Maguire, G. P., A. D. Arthur, P. J. Boustead, B. Dwyer, and B. J. Currie. 1998. Clinical experience and outcomes of community-acquired and nosocomial methicillin-resistant Staphylococcus aureus in a northern Australian hospital. J. Hosp. Infect. 38:273-281. [DOI] [PubMed] [Google Scholar]
- 573.Maguire, G. P., A. D. Arthur, P. J. Boustead, B. Dwyer, and B. J. Currie. 1996. Emerging epidemic of community-acquired methicillin-resistant Staphylococcus aureus infection in the Northern Territory. Med. J. Aust. 164:721-723. [DOI] [PubMed] [Google Scholar]
- 574.Maier, J., H. Melzl, U. Reischl, I. Drubel, W. Witte, N. Lehn, and H. Linde. 2005. Panton-Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus in Germany associated with travel or foreign family origin. Eur. J. Clin. Microbiol. Infect. Dis. 24:637-639. [DOI] [PubMed] [Google Scholar]
- 575.Main, C. L., P. Jayaratne, A. Haley, C. Rutherford, F. Smaill, and D. N. Fisman. 2005. Outbreaks of infection caused by community-acquired methicillin-resistant Staphylococcus aureus in a Canadian correctional facility. Can. J. Infect. Dis. Med. Microbiol. 16:343-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 576.Malik, S., H. Peng, and M. D. Barton. 2006. Partial nucleotide sequencing of the mecA genes of Staphylococcus aureus isolates from cats and dogs. J. Clin. Microbiol. 44:413-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 577.Manian, F. A. 2003. Asymptomatic nasal carriage of mupirocin-resistant, methicillin-resistant Staphylococcus aureus (MRSA) in a pet dog associated with MRSA infection in household contacts. Clin. Infect. Dis. 36:e26-e28. [DOI] [PubMed] [Google Scholar]
- 578.Manian, F. A., D. Senkel, J. Zack, and L. Meyer. 2002. Routine screening for methicillin-resistant Staphylococcus aureus among patients newly admitted to an acute rehabilitation unit. Infect. Control Hosp. Epidemiol. 23:516-519. [DOI] [PubMed] [Google Scholar]
- 579.Manzur, A., A. M. Dominguez, M. Pujol, M. P. M. González, E. Limon, A. Hornero, R. Martín, F. Gudiol, and J. Ariza. 2008. Community-acquired methicillin-resistant Staphylococcus aureus infections: an emerging threat in Spain. Clin. Microbiol. Infect. 14:377-380. [DOI] [PubMed] [Google Scholar]
- 580.Maree, C. M., R. S. Daum, S. Boyle-Vavra, K. Matayoshi, and L. G. Miller. 2007. Community-associated methicillin-resistant Staphylococcus aureus isolates causing healthcare-associated infections. Emerg. Infect. Dis. 13:236-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 581.Markowitz, N., E. L. Quinn, and L. D. Saravolatz. 1992. Trimethoprim-sulfamethoxazole compared with vancomycin for the treatment of Staphylococcus aureus infection. Ann. Intern. Med. 117:390-398. [DOI] [PubMed] [Google Scholar]
- 582.Marschall, J., and K. Muhlemann. 2006. Duration of methicillin-resistant Staphylococcus aureus carriage, according to risk factors for acquisition. Infect. Control Hosp. Epidemiol. 27:1206-1212. [DOI] [PubMed] [Google Scholar]
- 583.Martin, B. T., P. Palasanthiran, I. B. Gosbell, T. Barbagiannakos, E. J. Best, and R. L. Henry. 2005. Severe childhood pneumonitis caused by the Queensland strain of community acquired methicillin-resistant Staphylococcus aureus. Med. J. Aust. 182:249. [DOI] [PubMed] [Google Scholar]
- 584.Martínez-Aguilar, G., A. Avalos-Mishaan, K. Hulten, W. Hammerman, E. O. Mason, and S. L. Kaplan. 2004. Community-acquired, methicillin-resistant and methicillin-susceptible Staphylococcus aureus musculoskeletal infections in children. Pediatr. Infect. Dis. J. 23:701-706. [DOI] [PubMed] [Google Scholar]
- 585.Martinez-Aguilar, G., W. A. Hammerman, E. O. Mason, and S. L. Kaplan. 2003. Clindamycin treatment of invasive infections caused by community-acquired, methicillin-resistant and methicillin-susceptible Staphylococcus aureus in children. Pediatr. Infect. Dis. J. 22:593-598. [DOI] [PubMed] [Google Scholar]
- 586.Marty, F. M., W. W. Yeh, C. B. Wennersten, L. Venkataraman, E. Albano, E. P. Alyea, H. S. Gold, L. R. Baden, and S. K. Pillai. 2006. Emergence of a clinical daptomycin-resistant Staphylococcus aureus isolate during treatment of methicillin-resistant Staphylococcus aureus bacteremia and osteomyelitis. J. Clin. Microbiol. 44:595-597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 587.Maslow, J., A. Slutsky, and R. Arbeit. 1993. The application of pulsed field gel electrophoresis to molecular epidemiology, p. 563-572. In H. Persing, T. Smith, F. Tenover, and T. White (ed.), Diagnostic molecular microbiology: principles and applications. American Society for Microbiology, Washington, DC.
- 588.Masterton, R. G., J. E. Coia, A. W. Notman, L. Kempton-Smith, and B. D. Cookson. 1995. Refractory methicillin-resistant Staphylococcus aureus carriage associated with contamination of the home environment. J. Hosp. Infect. 29:318-319. [DOI] [PubMed] [Google Scholar]
- 589.Matthews, W. C., J. C. Caperna, R. E. Barber, F. J. Torriani, L. G. Miller, S. May, and J. A. McCutchan. 2005. Incidence of and risk factors for clinically significant methicillin-resistant Staphylococcus aureus infection in a cohort of HIV-infected adults. J. Acquir. Immune Defic. Syndr. 40:155-160. [DOI] [PubMed] [Google Scholar]
- 590.McAdams, R. M., E. Mazuchowski, M. W. Ellis, and M. Rajnik. 2005. Necrotizing staphylococcal pneumonia in a neonate. J. Perinatol. 25:677-679. [DOI] [PubMed] [Google Scholar]
- 591.McAdams, R. M., M. W. Ellis, S. Trevino, and M. Rajnik. 2008. Spread of methicillin resistant Staphylococcus aureus USA300 in a neonatal intensive care unit. Pediatr. Int. 50:810-815. [DOI] [PubMed] [Google Scholar]
- 592.McBryde, E. S., L. C. Bradley, M. Whitby, and D. L. S. McElwain. 2004. An investigation of methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 58:104-108. [DOI] [PubMed] [Google Scholar]
- 593.McCaskill, M. L., E. O. Mason, S. L. Kaplan, W. Hammerman, L. B. Lamberth, and K. G. Hultén. 2007. Increase of the USA300 clone among community-acquired methicillin-susceptible Staphylococcus aureus causing invasive infections. Pediatr. Infect. Dis. J. 26:1122-1127. [DOI] [PubMed] [Google Scholar]
- 594.McDonald, M., A. Dougall, D. Holt, F. Huygens, F. Oppedisano, P. M. Giffard, J. Inman-Bamber, A. J. Stephens, R. Towers, J. R. Carapetis, and B. J. Currie. 2006. Use of single-nucleotide polymorphism genotyping system to demonstrate the unique epidemiology of methicillin-resistant Staphylococcus aureus in remote aboriginal communities. J. Clin. Microbiol. 44:3720-3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 595.McDougal, L. K., C. D. Steward, G. E. Killgore, J. M. Chaitram, S. K. McAllister, and F. C. Tenover. 2003. Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: establishing a national database. J. Clin. Microbiol. 41:5113-5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 596.McMullen, K. M., D. K. Warren, and K. F. Woeltje. 2008. The changing susceptibilities of methicillin-resistant Staphylococcus aureus at a Midwestern hospital: the emergence of “community-associated” MRSA. Am. J. Infect. Control 37:454-457. [DOI] [PubMed] [Google Scholar]
- 597.McNally, L. M., P. M. Jeena, K. Gajee, A. W. Sturm, A. M. Tomkins, H. M. Coovadia, and D. Goldblatt. 2006. Reply to Bogaert et al. J. Infect. Dis. 194:1618-1619. [DOI] [PubMed] [Google Scholar]
- 598.Méan, M., M. R. Mallaret, P. Andrini, C. Recule, T. Debuuon, P. Pavese, and J. Croizé. 2007. A neonatal specialist with recurrent methicillin-resistant Staphylococcus aureus (MRSA) carriage implicated in the transmission of MRSA to newborns. Infect. Control Hosp. Epidemiol. 28:625-628. [DOI] [PubMed] [Google Scholar]
- 599.Meka, V. G., S. K. Pillai, G. Sakoulas, C. Wennersten, L. Venkataraman, P. C. DeGiroami, G. M. Eliopoulos, R. C. Moellering, and H. S. Gold. 2004. Linezolid resistance in sequential Staphylococcus aureus isolates associated with a T2500A mutation in the 23S rRNA gene and loss of a single copy of rRNA. J. Infect. Dis. 190:311-317. [DOI] [PubMed] [Google Scholar]
- 600.Mertz, D., R. Frei, B. Jaussi, A. Tietz, C. Stebler, U. Flückiger, and A. F. Widmer. 2007. Throat swabs are necessary to reliably detect carriers of Staphylococcus aureus. Clin. Infect. Dis. 45:475-477. [DOI] [PubMed] [Google Scholar]
- 601.Mertz, D., R. Frei, N. Periat, M. Zimmerli, M. Battegay, U. Flückiger, and A. F. Widmer. 2009. Exclusive Staphylococcus aureus throat carriage: at risk populations. Arch. Intern. Med. 169:172-178. [DOI] [PubMed] [Google Scholar]
- 602.Micek, S. T., M. Dunne, and M. H. Kollef. 2005. Pleuropulmonary complications of Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus: importance of treatment with antimicrobials inhibiting exotoxin production. Chest 128:2732-2738. [DOI] [PubMed] [Google Scholar]
- 603.Michalopoulos, A., and M. E. Falagas. 2006. Multi-systemic methicillin-resistant Staphylococcus aureus (MRSA) community-acquired infection. Med. Sci. Monit. 12:CS39-CS43. [PubMed] [Google Scholar]
- 604.Miklaševics, E., S. Hæggman, A. Balode, B. Sanchez, A. Martinsons, O. Olsson-Liljequist, and U. Dumpis. 2004. Report on the first PVL-positive community-acquired MRSA strain in Latvia. Euro Surveill. 9(11):pii=485. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=485. [PubMed] [Google Scholar]
- 605.Miles, F., L. Voss, E. Segedin, and B. J. Anderson. 2005. Review of Staphylococcus aureus infections requiring admission to a pediatric intensive care unit. Arch. Dis. Child. 90:1274-1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 606.Millar, B. C., A. Loughrey, J. S. Elborn, and J. E. Moore. 2007. Proposed definitions of community-associated meticillin-resistant Staphylococcus aureus (CA-MRSA). J. Hosp. Infect. 67:109-113. [DOI] [PubMed] [Google Scholar]
- 607.Miller, L. G., C. Quan, A. Shay, K. Mostafaie, K. Bharadwa, N. Tan, K. Matayoshi, J. Cronin, J. Tan, G. Tagudar, and A. S. Bayer. 2007. A prospective investigation of outcomes after hospital discharge for endemic community-acquired methicillin-resistant and -susceptible Staphylococcus aureus skin infection. Clin. Infect. Dis. 44:483-492. [DOI] [PubMed] [Google Scholar]
- 608.Miller, L. G., F. Perdreau-Remington, A. S. Bayer, B. Diep, N. Tan, K. Bharadwa, J. Tsui, J. Perlroth, A. Shay, G. Tagudar, U. Ibebuogu, and B. Spellberg. 2007. Clinical and epidemiologic characteristics cannot distinguish community associated methicillin-resistant Staphylococcus aureus infection from methicillin-susceptible S. aureus infection: a prospective investigation. Clin. Infect. Dis. 44:471-482. [DOI] [PubMed] [Google Scholar]
- 609.Miller, L. G., F. Perdreau-Remington, G. Rieg, S. Mehdi, J. Perlroth, A. S. Bayer, A. W. Tang, T. O. Phung, and B. Spellberg. 2005. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N. Engl. J. Med. 352:1445-1453. [DOI] [PubMed] [Google Scholar]
- 610.Miller, M., C. Cespedes, M. Bhat, P. Vavagiakis, R. S. Klein, and F. D. Lowy. 2007. Incidence and persistence of Staphylococcus aureus nasal colonization in a community sample of HIV-infected and -uninfected drug users. Clin. Infect. Dis. 45:343-346. [DOI] [PubMed] [Google Scholar]
- 611.Miller, M., C. Cespedes, P. Vavagiakis, R. S. Klein, and F. D. Lowy. 2003. Staphylococcus aureus colonization in a community sample of HIV-infected and HIV-uninfected drug users. Eur. J. Clin. Microbiol. Infect. Dis. 22:463-469. [DOI] [PubMed] [Google Scholar]
- 612.Milstone, A. M., C. L. Passaretti, and T. M. Perl. 2008. Chlorhexidine: expanding the armamentarium for infection control and prevention. Clin. Infect. Dis. 46:274-281. [DOI] [PubMed] [Google Scholar]
- 613.Mitsuda, T., K. Arai, M. Ibe, T. Imagawa, N. Tonomo, and S. Yokota. 1999. The influence of methicillin-resistant Staphylococcus aureus (MRSA) carriers in a nursery and transmission of MRSA to their households. J. Hosp. Infect. 42:45-51. [DOI] [PubMed] [Google Scholar]
- 614.Miyashita, T., Y. Shimamoto, H. Nishiya, Y. Koshibu, H. Sugiyama, Y. Ono, T. Stoh, H. Haraoka, J. Nakano, K. Ohta, T. Sato, N. Morinaga, and M. Noda. 2002. Destructive pulmonary embolism in a patient with community-acquired staphylococcal bacteremia. J. Infect. Chemother. 8:99-102. [DOI] [PubMed] [Google Scholar]
- 615.Moazzez, A., R. L. Kelso, S. Towfigh, H. Sohn, T. V. Berne, and R. J. Mason. 2007. Breast abscess bacteriologic features in the era of community-acquired methicillin-resistant Staphylococcus aureus epidemics. Arch. Surg. 142:881-884. [DOI] [PubMed] [Google Scholar]
- 616.Moellering, R. C. 2008. Current treatment options for community-acquired methicillin-resistant Staphylococcus aureus infection. Clin. Infect. Dis. 46:1032-1037. [DOI] [PubMed] [Google Scholar]
- 617.Molina, A., R. Del Campo, L. Máiz, M. I. Morosini, A. Lamas, F. Baquero, and R. Cantón. 2008. High prevalence in cystic fibrosis patients of multiresistant hospital-acquired methicillin-resistant Staphylococcus aureus ST228-SCCmecI capable of biofilm formation. J. Antimicrob. Chemother. 62:961-967. [DOI] [PubMed] [Google Scholar]
- 618.Monaco, M., R. Antonucci, P. Palange, M. Venditti, and A. Pantosi. 2005. Methicillin-resistant Staphylococcus aureus necrotizing pneumonia. Emerg. Infect. Dis. 11:1647-1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 619.Monecke, S., P. Slickers, M. J. Ellington, A. M. Kearns, and R. Ehricht. 2007. High diversity of Panton-Valentine leukocidin-positive, methicillin-susceptible isolates of Staphylococcus aureus and implications for the evolution of community-associated methicillin-resistant S. aureus. Clin. Microbiol. Infect. 13:1157-1164. [DOI] [PubMed] [Google Scholar]
- 620.Monecke, S., R. Ehricht, P. Slickers, H. L. Tan, and G. Coombs. 2009. The molecular epidemiology and evolution of Panton-Valentine leukocidin-positive, methicillin resistant Staphylococcus aureus strain USA300 in Western Australia. Clin. Microbiol. Infect. 15:770-776. [DOI] [PubMed] [Google Scholar]
- 621.Mongkolrattanothai, K., S. Boyle, M. D. Kahana, and R. S. Daum. 2003. Severe Staphylococcus aureus infections caused by clonally related community-acquired methicillin-susceptible and methicillin-resistant isolates. Clin. Infect. Dis. 37:1050-1058. [DOI] [PubMed] [Google Scholar]
- 622.Mongkolrattanothai, K., S. Boyle, T. V. Murphy, and R. S. Daum. 2004. Novel non-mecA-containing staphylococcal chromosomal cassette composite island containing pbp4 and tagF genes in a commensal staphylococcal species: a possible reservoir for antibiotic resistance islands in Staphylococcus aureus. Antimicrob. Agents Chemother. 48:1823-1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 623.Montgomery, C. P., S. Boyle-Vavra, and R. S. Daum. 2009. The arginine catabolic mobile element is not associated with enhanced virulence in experimental invasive disease caused by the community-associated methicillin-resistant Staphylococcus aureus USA300 genetic background. Infect. Immun. 77:2650-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 624.Montgomery, C. P., S. Boyle-Vavra, P. V. Adem, J. C. Lee, A. N. Husain, J. Clasen, and R. S. Daum. 2008. Comparison of virulence in community-associated methicillin-resistant Staphylococcus aureus pulsotypes USA300 and USA400 in a rat model of pneumonia. J. Infect. Dis. 198:561-570. [DOI] [PubMed] [Google Scholar]
- 625.Moodley, A., M. Stegger, A. F. Bagcigil, K. E. Batiste, A. Loeffler, D. H. Lloyd, N. J. Williams, N. Leonard, Y. Abbott, R. Skov, and L. Guardabassi. 2006. spa typing of methicillin-resistant Staphylococcus aureus isolated from domestic animals and veterinary staff in the UK and Ireland. J. Antimicrob. Chemother. 58:1118-1123. [DOI] [PubMed] [Google Scholar]
- 626.Moore, C. L., A. Hingwe, S. M. Donabedian, M. B. Perri, S. L. Davis, N. Z. Haque, K. Reyes, D. Vager, and M. J. Zervos. 2009. Comparative evaluation of epidemiology and outcomes of methicillin-resistant Staphylococcus aureus (MRSA) USA300 infections causing community- and healthcare-associated infections. Int. J. Antimicrob. Agents 34:148-155. [DOI] [PubMed] [Google Scholar]
- 627.Moore, Z. S., R. C. Jerris, and J. A. Hilinski. 2008. High prevalence of inducible clindamycin resistance among Staphylococcus aureus isolates from patients with cystic fibrosis. J. Cyst. Fibros. 7:206-209. [DOI] [PubMed] [Google Scholar]
- 628.Moran, G. J., A. Krishnadasan, R. J. Gorwitz, G. E. Fosheim, L. K. McDougal, R. B. Carey, and D. A. Talan for the EMERGEncy ID Net Study Group. 2006. Methicillin-resistant S. aureus infections among patients in the emergency department. N. Engl. J. Med. 355:666-674. [DOI] [PubMed] [Google Scholar]
- 629.Morel, A. S., F. Wu, P. Della-Latta, A. Cronquist, D. Rubinstein, and L. Saiman. 2002. Nosocomial transmission of methicillin-resistant Staphylococcus aureus from a mother to her preterm quadruplet infants. Am. J. Infect. Control 30:170-173. [DOI] [PubMed] [Google Scholar]
- 630.Moreno, F., C. Crisp, J. H. Jorgensen, and J. E. Patterson. 1995. Staphylococcus aureus as a community organism. Clin. Infect. Dis. 21:1308-1312. [DOI] [PubMed] [Google Scholar]
- 631.Morens, D. M., J. K. Taubenberger, and A. S. Fauci. 2008. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J. Infect. Dis. 198:962-970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 632.Morita, J. E., R. S. Fujioka, A. D. Tice, J. Berestecky, D. Sato, S. E. Seifried, and A. R. Katz. 2007. Survey of methicillin-resistant Staphylococcus aureus (MRSA) carriage in healthy college students, Hawai'i. Hawaii Med. J. 66:213-215. [PubMed] [Google Scholar]
- 633.Morris, D. O., E. A. Maudlin, K. O'Shea, F. S. Shofer, and S. C. Rankin. 2006. Clinical, microbiological, and molecular characterization of methicillin-resistant Staphylococcus aureus infections in cats. Am. J. Vet. Res. 67:1421-1425. [DOI] [PubMed] [Google Scholar]
- 634.Morris, D. O., K. A. Rook, F. S. Shofer, and S. C. Rankin. 2006. Screening of Staphylococcus aureus, Staphylococcus intermedius, and Staphylococcus schleiferi isolates obtained from small companion animals for antimicrobial resistance: a retrospective review of 749 isolates (2003-4). Vet. Dermatol. 17:332-337. [DOI] [PubMed] [Google Scholar]
- 635.Morrison, M. A., J. C. Hageman, and R. M. Klevens. 2006. Case definition for community-associated methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 62:241. [DOI] [PubMed] [Google Scholar]
- 636.Moumile, K., C. Cadilhac, G. Lina, P. Berche, C. Glorion, and A. Ferroni. 2006. Severe osteoarticular infection associated with Panton-Valentine leukocidin-producing Staphylococcus aureus. Diagn. Microbiol. Infect. Dis. 56:95-97. [DOI] [PubMed] [Google Scholar]
- 637.Muder, R. R., C. Brennan, M. M. Wagener, R. M. Vickers, J. D. Rihs, G. A. Hancock, Y. C. Yee, J. M. Miller, and V. L. Yu. 1991. Methicillin-resistant staphylococcal colonization and infection in a long-term care facility. Ann. Intern. Med. 114:107-112. [DOI] [PubMed] [Google Scholar]
- 638.Mulhausen, P. L., L. J. Harrell, M. Weinberger, G. G. Kochersberger, and J. R. Feussner. 1996. Contrasting methicillin-resistant Staphylococcus aureus colonization in Veterans Affairs and community nursing homes. Am. J. Med. 100:24-31. [DOI] [PubMed] [Google Scholar]
- 639.Müller-Premru, M., B. Strommenger, N. Alikadic, W. Witte, A. W. Friedrich, K. Seme, N. S. Kucina, D. Smrke, V. Spik, and M. Gubina. 2005. New strains of community-acquired methicillin-resistant Staphylococcus aureus with Panton-Valentine leukocidin causing an outbreak of severe soft tissue infection in a football team. Eur. J. Clin. Microbiol. Infect. Dis. 24:848-850. [DOI] [PubMed] [Google Scholar]
- 640.Mulvey, M. R., L. MacDougall, B. Cholin, G. Horsman, M. Fidyk, and S. Woods. 2005. Community-associated methicillin-resistant Staphylococcus aureus, Canada. Emerg. Infect. Dis. 11:844-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 641.Munckhof, W. J., A. Krishnan, P. Kruger, and D. Looke. 2008. Cavernous sinus thrombosis and meningitis from community-acquired methicillin-resistant Staphylococcus aureus infection. Intern. Med. J. 38:283-287. [DOI] [PubMed] [Google Scholar]
- 642.Munckhof, W. J., G. R. Nimmo, J. Carney, J. M. Schooneveldt, F. Huygens, J. Inman-Bamber, E. Tong, A. Morton, and P. Giffard. 2008. Methicillin-susceptible, non-multidrug resistant and multidrug resistant methicillin-resistant Staphylococcus aureus infections: a clinical, epidemiological and microbiological comparative study. Eur. J. Clin. Microbiol. Infect. Dis. 27:355-364. [DOI] [PubMed] [Google Scholar]
- 643.Munckhof, W. J., G. R. Nimmo, J. M. Schooneveldt, S. Schlebusch, A. J. Stephens, G. Williams, F. Huygens, and P. Giffard. 2009. Nasal carriage of Staphylococcus aureus, including community-associated methicillin-resistant strains, in Queensland adults. Clin. Microbiol. Infect. 15:149-155. [DOI] [PubMed] [Google Scholar]
- 644.Munckhof, W. J., J. Harper, J. Schooneveldt, and G. R. Nimmo. 2002. Recent appearance of clindamycin resistance in community-acquired methicillin-resistant Staphylococcus aureus (MRSA) in south-east Queensland. Med. J. Aust. 176:243-244. [DOI] [PubMed] [Google Scholar]
- 645.Munckhof, W. J., J. Schoonveldt, G. W. Coombs, J. Hoare, and G. R. Nimmo. 2003. Emergence of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infection in Queensland, Australia. Int. J. Infect. Dis. 7:259-267. [DOI] [PubMed] [Google Scholar]
- 646.Murray, R. J., J. O. Robinson, J. N. White, F. Hughes, G. W. Coombs, J. C. Pearson, H. L. Tan, G. Chidlow, S. Williams, K. J. Christiansen, and D. W. Smith. 2010. Community-acquired pneumonia due to pandemic A(H1N1)2009 influenzavirus and methicillin resistant Staphylococcus aureus co-infection. PLoS One 5:e8705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 647.Murray, R. J., T. T. Lim, J. C. Pearson, W. B. Grubb, and G. D. Lum. 2004. Community-onset methicillin-resistant Staphylococcus aureus bacteremia in northern Australia. Int. J. Infect. Dis. 8:275-283. [DOI] [PubMed] [Google Scholar]
- 648.Muto, C. A., J. A. Jernigan, B. E. Ostrowsky, H. M. Richet, W. R. Jarvis, J. M. Boyce, and B. M. Farr. 2003. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and Enterococcus. Infect. Control Hosp. Epidemiol. 24:362-386. [DOI] [PubMed] [Google Scholar]
- 649.Mylotte, J. M., S. Goodnough, and A. Tayara. 2001. Antibiotic-resistant organisms among long-term care facility residents on admission to an inpatient geriatrics unit: retrospective and prospective surveillance. Am. J. Infect. Control 29:139-144. [DOI] [PubMed] [Google Scholar]
- 650.Naas, T., N. Fortineau, C. Spicq, J. Robert, V. Jarlier, and P. Nordmann. 2005. Three-year survey of community-acquired methicillin-resistant Staphylococcus aureus producing Panton-Valentine leukocidin in a French university hospital. J. Hosp. Infect. 61:321-329. [DOI] [PubMed] [Google Scholar]
- 651.Naesens, R., M. Ronsyn, P. Druwe, M. Ieven, and A. Jeurissen. 2009. Central nervous system invasion by community-acquired methicillin-resistant Staphylococcus aureus: case report and review of the literature. J. Med. Microbiol. 58:1247-1251. [DOI] [PubMed] [Google Scholar]
- 652.Nagaraju, U., G. Bhat, M. Kuruvila, G. S. Pai, Jayalakshmi, and R. P. Babu. 2004. Methicillin-resistant Staphylococcus aureus in community-acquired pyoderma. Int. J. Dermatol. 43:412-414. [DOI] [PubMed] [Google Scholar]
- 653.Naimi, T., K. LeDell, D. Boxrud, A. Groom, C. Steward, S. Johnson, J. M. Besser, C. O'Boyle, R. N. Danila, J. E. Cheek, M. T. Osterholm, K. A. Moore, and K. E. Smith. 2001. Epidemiology and clonality of community-acquired methicillin-resistant Staphylococcus aureus in Minnesota, 1996-1998. Clin. Infect. Dis. 33:990-996. [DOI] [PubMed] [Google Scholar]
- 654.Naimi, T. S., K. H. LeDell, K. Como-Sabetti, S. M. Borchardt, D. J. Boxrud, J. Etienne, S. K. Johnson, F. Vadenesch, S. Fridkin, C. O'Boyle, R. N. Danila, and R. Lynfield. 2003. Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA 290:2976-2984. [DOI] [PubMed] [Google Scholar]
- 655.Nakamura, M. M., K. L. Rohling, M. Shashaty, H. Lu, Y. Tang, and K. M. Edwards. 2002. Prevalence of methicillin-resistant Staphylococcus aureus nasal carriage in the community pediatric population. Pediatr. Infect. Dis. J. 21:917-921. [DOI] [PubMed] [Google Scholar]
- 656.Nascimento-Carvalho, C. M., T. G. Lyra, N. N. Alves, R. M. Caldas, and M. G. Barberino. 2008. Resistance to methicillin and other antimicrobials among community-acquired and nosocomial Staphylococcus aureus strains in a pediatric teaching hospital in Salvador, Northeast Brazil. Microb. Drug Resist. 14:129-131. [DOI] [PubMed] [Google Scholar]
- 657.Nashev, D., L. Bizeva, and K. Toshkova. 2007. First cases of infections caused by Panton-Valentine leukocidin positive community-acquired methicillin-resistant Staphylococcus aureus in Bulgaria. Euro Surveill. 12(26):pii=3225. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=3225. [DOI] [PubMed] [Google Scholar]
- 658.Nathwani, D., M. Morgan, R. G. Masterson, M. Dryden, B. D. Cookson, G. French, and D. Lewis on behalf of the British Society for Antimicrobial Chemotherapy Working Party on Community-Onset MRSA Infections. 2008. Guidelines for UK practice for the diagnosis and management of methicillin-resistant Staphylococcus aureus (MRSA) infections preenting in the community. J. Antimicrob. Chemother. 61:976-994. [DOI] [PubMed] [Google Scholar]
- 659.National College Athletic Association. 2005. Wrestling rules and interpretations, appendix D. National College Athletic Association, Indianapolis, IN.
- 660.National Commission on Correctional Health Care. 2002. The health status of soon-to-be-released inmates: a report to Congress, March 2002. National Commission on Correctional Health Care, Chicago, IL. http://www.ncchc.org/pubs/pubs_stbr.html.
- 661.National Committee for Clinical Laboratory Standards. 2004. Performance standards for antimicrobial disk susceptibility testing: 14th informational supplement, M100-S14. NCCLS, Wayne, PA.
- 662.Ndawula, E. M., and L. Brown. 1991. Mattresses as reservoirs of epidemic methicillin-resistant Staphylococcus aureus. Lancet 337:488. [DOI] [PubMed] [Google Scholar]
- 663.Nemati, M., K. Hermans, U. Lipinska, O. Denis, A. Deplano, M. Struelens, L. A. Devrise, F. Pasmans, and F. Haesebrouck. 2008. Antimicrobial resistance of old and recent Staphylococcus aureus isolates from poultry: first detection of livestock-associated methicillin-resistant strain ST398. Antimicrob. Agents Chermother. 52:3817-3819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 664.Nguyen, D. M., E. Bancroft, L. Mascola, R. Guevara, and L. Yasuda. 2007. Risk factors for neonatal methicillin-resistant Staphylococcus aureus infection in a well-infant nursery. Infect. Control Hosp. Epidemiol. 28:406-411. [DOI] [PubMed] [Google Scholar]
- 665.Nguyen, D. M., L. Mascola, and E. Bancroft. 2005. Recurring methicillin-resistant Staphylococcus aureus infections in a football team. Emerg. Infect. Dis. 11:526-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 666.Nickerson, E. K., V. Wuthiekanun, N. P. Day, W. Chaowagul, and S. J. Peacock. 2006. Meticillin-resistant Staphylococcus aureus in rural Asia. Lancet Infect. Dis. 6:70-71. [DOI] [PubMed] [Google Scholar]
- 667.Nienhoff, U., K. Kadlec, I. F. Chanberny, J. Verspohl, G. F. Gerlach, S. Schwarz, D. Simon, and I. Nolte. 2009. Transmission of methicillin-resistant Staphylococcus aureus strains between humans and dogs: two case reports. J. Antimicrob. Chemother. 64:660-662. [DOI] [PubMed] [Google Scholar]
- 668.Nilsson, P., and T. Ripa. 2006. Staphylococcus aureus throat colonization is more frequent than colonization in the anterior nares. J. Clin. Microbiol. 44:3334-3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 669.Nimmo, G. R., and E. G. Playford. 2003. Community-acquired MRSA bacteraemia: four additional cases including one associated with severe pneumonia. Med. J. Aust. 178:245-246. [DOI] [PubMed] [Google Scholar]
- 670.Nimmo, G. R., and G. W. Coombs. 2008. Community-associated methicillin-resistant Staphylococcus aureus (MRSA) in Australia. Int. J. Antimicrob. Agents 31:401-410. [DOI] [PubMed] [Google Scholar]
- 671.Nimmo, G. R., J. Fong, D. L. Patterson, and M. L. McLaws. 2008. Changing epidemiology of meticillin-resistant S. aureus in Queensland, Australia, 2000-2006: use of passive surveillance of susceptibility phenotypes. J. Hosp. Infect. 70:305-313. [DOI] [PubMed] [Google Scholar]
- 672.Nimmo, G. R., J. Schooneveldt, G. O'Kane, B. McCall, and A. Vickery. 2000. Community acquisition of gentamicin-sensitive methicillin-resistant Staphylococcus aureus in southeast Queensland, Australia. J. Clin. Microbiol. 38:3926-3931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 673.Niniou, I., S. Vourli, E. Lebessi, M. Fonustoukou, A. Vatopoulos, D. G. Pasparakis, D. A. Kafetzis, and M. N. Tsolia. 2008. Clinical and molecular epidemiology of community-acquired methicillin-resistant Staphylococcus aureus infections in children in central Greece. Eur. J. Clin. Microbiol. Infect. Dis. 27:831-837. [DOI] [PubMed] [Google Scholar]
- 674.Noble, W. C., R. E. O. Williams, M. P. Jevons, and R. A. Shooter. 1964. Some aspects of nasal carriage of staphylococci. J. Clin. Pathol. 17:79-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 675.Noriega, L. M., P. González, J. C. Hormazábal, C. Pinto, M. Canals, J. M. Munita, L. Thompson, A. Marcotti, J. Pérez, D. Ibáñez, P. Araya, C. Canals, and P. Vial. 2008. Staphylococcus aureus communitario resistente a cloxacilina: comunicación de los primeros cinco casos descritos en Chile. Rev. Med. Chile 136:885-891. [PubMed] [Google Scholar]
- 676.Normanno, G., M. Corrente, G. La Salandra, A. Dambrosio, N. C. Quaglia, A. Parisi, G. Greco, A. L. Bellaciccio, S. Virgilio, and G. V. Celano. 2007. Methicillin-resistant Staphylococcus aureus (MRSA) in foods of animal origin product in Italy. Int. J. Food Microbiol. 117:219-222. [DOI] [PubMed] [Google Scholar]
- 677.Nourse, C., M. Starr, and W. Munckhof. 2007. Community-acquired methicillin-resistant Staphylococcus aureus causes severe disseminated infection and deep venous thrombosis in children: literature review and recommendations for management. J. Paediatr. Child Health 43:656-661. [DOI] [PubMed] [Google Scholar]
- 678.Noyce, J. O., H. Michels, and C. W. Keevil. 2006. Potential use of copper surfaces to reduce survival of epidemic meticillin-resistant Staphylococcus aureus in the healthcare environment. J. Hosp. Infect. 63:289-297. [DOI] [PubMed] [Google Scholar]
- 679.Nygaard, T. K., F. R. DeLeo, and J. M. Voyich. 2008. Community-associated methicillin-resistant Staphylococcus aureus skin infections: advances toward identifying the key virulence factors. Curr. Opin. Infect. Dis. 21:147-152. [DOI] [PubMed] [Google Scholar]
- 680.O'Brien, F. G., G. W. Coombs, J. W. Pearman, M. Gracey, M. Moss, K. J. Christiansen, and W. B. Grubb. 2009. Population dynamics of methicillin-susceptible and -resistant Staphylococcus aureus in remote communities. J. Antimicrob. Chemother. 64:684-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 681.O'Brien, F. G., J. W. Pearman, M. Gracey, T. V. Riley, and W. B. Grubb. 1999. Community strain of methicillin-resistant Staphylococcus aureus involved in a hospital outbreak. J. Clin. Microbiol. 37:2858-2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 682.O'Brien, F. G., T. T. Lim, F. N. Chong, G. W. Coombs, M. C. Enright, D. A. Robinson, A. Monk, B. Saïd, B. N. Kreiswirth, and W. B. Grubb. 2004. Diversity among community isolates of methicillin-resistant Staphylococcus aureus in Australia. J. Clin. Microbiol. 42:3185-3190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 683.Ochoa, T. J., J. R. Mohr, A. Wanger, J. R. Murphy, and G. P. Heresi. 2005. Community-associated methicillin-resistant Staphylococcus aureus in pediatric patients. Emerg. Infect. Dis. 11:966-968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 684.Ofner-Agostini, M., A. E. Simor, M. Mulvey, E. Bryce, M. Loeb, A. McGreer, A. Kiss, S. Paton, and Canadian Nosocomial Infection Surveillance Program, Health Canada. 2006. Methicillin-resistant Staphylococcus aureus in Canadian aboriginal people. Infect. Control Hosp. Epidemiol. 27:204-207. [DOI] [PubMed] [Google Scholar]
- 685.O'Hara, F. P., N. Guex, J. M. Word, L. A. Miller, J. A. Becker, S. L. Walsh, N. E. Scangarella, J. M. West, R. M. Shawar, and H. Amrine-Madsen. 2008. A geographic variant of the Staphylococcus aureus Panton-Valentine leukocidin toxin and the origin of community-associated methicillin-resistant S. aureus USA300. J. Infect. Dis. 197:187-194. [DOI] [PubMed] [Google Scholar]
- 686.Oie, S., and A. Kamiya. 1996. Survival of methicillin-resistant Staphylococcus aureus on naturally contaminated dry mops. J. Hosp. Infect. 34:145-149. [DOI] [PubMed] [Google Scholar]
- 687.Okuma, K., K. Iwakawa, J. D. Turnidge, W. B. Grubb, J. M. Bell, F. G. O'Brien, G. W. Coombs, J. W. Pearman, F. C. Tenover, M. Kapi, C. Tiensasitorn, T. Ito, and K. Hiramatsu. 2002. Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community. J. Clin. Microbiol. 40:4289-4294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 688.Olesevich, M., and A. Kennedy. 2007. Emergence of community-acquired methicillin-resistant Staphylococcus aureus soft tissue infections. J. Pediatr. Surg. 42:765-768. [DOI] [PubMed] [Google Scholar]
- 689.O'Mahoney, R., Y. Abbott, F. C. Leonard, B. K. Markey, P. J. Quinn, P. J. Pollack, S. Fanning, and A. S. Rossney. 2005. Methicillin-resistant Staphylococcus aureus (MRSA) isolated from animals and veterinary personnel in Ireland. Vet. Microbiol. 109:285-296. [DOI] [PubMed] [Google Scholar]
- 690.O'Malley, M., J. Fowler, and A. M. Ilyas. 2009. Community-acquired methicillin-resistant Staphylococcus aureus infections of the hand: prevalence and timeliness of treatment. J. Hand Surg. 34A:504-508. [DOI] [PubMed] [Google Scholar]
- 691.Orscheln, R. C., D. A. Hunstad, S. A. Fritz, J. A. Loughman, K. Mitchell, E. K. Storch, M. Gaudreault, P. L. Sellenriek, J. R. Armstrong, E. R. Mardis, and G. A. Storch. 2009. Contribution of genetically restricted, methicillin-susceptible strains to the ongoing epidemic of community-acquired Staphylococcus aureus infections. Clin. Infect. Dis. 49:536-542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 692.Oteo, J., F. Baquero, A. Vindel, and J. Campos. 2004. Antibiotic resistance in 3113 blood isolates of Staphylococcus aureus in 40 Spanish hospitals participating in the European Antimicrobial Resistance Surveillance System (2000-2002). J. Antimicrob. Chemother. 53:1033-1038. [DOI] [PubMed] [Google Scholar]
- 693.Otter, J. A., and G. L. French. 2008. Community-associated methicillin-resistant Staphylococcus aureus in injecting drug users and the homeless in south London. J. Hosp. Infect. 69:198-200. [DOI] [PubMed] [Google Scholar]
- 694.Otter, J. A., and G. L. French. 2008. The emergence of community-associated methicillin-resistant Staphylococcus aureus at a London teaching hospital, 2000-2006. Clin. Microbiol. Infect. 14:670-676. [DOI] [PubMed] [Google Scholar]
- 695.Otter, J. A., N. L. Havill, J. M. Boyce, and G. L. French. 2009. Comparison of community-associated methicillin-resistant Staphylococcus aureus from teaching hospitals in London and the USA, 2004-2006: where is USA300 in the UK? Eur. J. Clin. Microbiol. Infect. Dis. 28:835-839. [DOI] [PubMed] [Google Scholar]
- 696.Owens, R. C., C. J. Donskey, R. P. Gaynes, V. G. Loo, and C. A. Muto. 2008. Antimicrobial-associated risk factors for Clostridium difficile infection. Clin. Infect. Dis. 46:S19-S31. [DOI] [PubMed] [Google Scholar]
- 697.Ozaki, K., M. Takano, W. Higuchi, T. Takano, S. Yabe, Y. Nitahara, A. Nishiyama, and T. Yamamoto. 2009. Genotypes, intrafamilial transmission, and virulence potential of nasal methicillin-resistant Staphylococcus aureus from children in the community. J. Infect. Chermother. 15:84-91. [DOI] [PubMed] [Google Scholar]
- 698.Pak, S. I., H. R. Han, and A. Shimizu. 1999. Characterization of methicillin-resistant Staphylococcus aureus isolated from dogs in Korea. J. Vet. Med. Sci. 61:1013-1018. [DOI] [PubMed] [Google Scholar]
- 699.Pallin, D. J., D. J. Egan, A. J. Pelletier, J. A. Espinola, D. C. Hooper, and C. A. Camargo. 2007. Increased emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann. Emerg. Med. 51:291-298. [DOI] [PubMed] [Google Scholar]
- 700.Pallin, D. J., J. A. Espinola, D. Y. Leung, D. C. Hooper, and C. A. Camargo, Jr. 2009. Epidemiology of dermatitis and skin infections in United States physicians' offices, 1993-2005. Clin. Infect. Dis. 49:901-907. [DOI] [PubMed] [Google Scholar]
- 701.Pan, A., A. Battisti, A. Zoncada, F. Bernieri, M. Boldini, A. Franco, M. Giorgi, M. Iurescia, S. Lorenzotti, M. Martinotti, M. Monaci, and A. Pantosti. 2009. Community-acquired methicillin-resistant Staphylococcus aureus ST398 infection, Italy. Emerg. Infect. Dis. 15:845-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 702.Pan, E. S., B. A. Diep, E. D. Charlebois, C. Auerswald, H. A. Carleton, G. F. Sensabaugh, and F. Perdreau-Remington. 2005. Population dynamics of methicillin-resistant Staphylococcus aureus—and their relation to community-associated disease activity. J. Infect. Dis. 192:811-818. [DOI] [PubMed] [Google Scholar]
- 703.Pan, E. S., B. A. Diep, H. A. Carleton, E. D. Charlebois, G. F. Sensabaugh, B. L. Haller, and F. Perdreau-Remington. 2003. Increasing prevalence of methicillin-resistant Staphylococcus aureus infection in California jails. Clin. Infect. Dis. 37:1384-1388. [DOI] [PubMed] [Google Scholar]
- 704.Panlilio, A. L., D. H. Culver, R. P. Gaynes, S. Banerjee, B. S. Henderson, J. S. Tolson, W. J. Martone, and the National Nosocomial Infections Surveillance System. 1992. Methicillin-resistant Staphylococcus aureus in U.S. hospitals 1975-1991. Infect. Control Hosp. Epidemiol. 13:582-586. [DOI] [PubMed] [Google Scholar]
- 705.Pannaraj, P. S., K. G. Hulten, B. E. Gonzalez, E. O. Mason, and S. L. Kaplan. 2006. Infective pyomyositis and myositis in children in the era of community-acquired, methicillin-resistant Staphylococcus aureus infection. Clin. Infect. Dis. 43:953-960. [DOI] [PubMed] [Google Scholar]
- 706.Panton, P. N. 1932. Staphylococcal infection. Lancet 220:1019-1020. [Google Scholar]
- 707.Panton, P. N., M. B. Came, F. C. O. Valentine, and M. R. C. P. Lond. 1932. Staphylococcal toxin. Lancet i:506-508. [Google Scholar]
- 708.Park, C., D. G. Lee, S. W. Kim, S. M. Choi, S. H. Park, H. S. Chun, J. H. Choi, J. H. Yoo, W. S. Shin, J. H. Kang, J. H. Kim, S. Y. Lee, S. M. Kim, and B. Y. Pyun. 2007. Predominance of community-associated methicillin-resistant Staphylococcus aureus strains carrying chromosome cassette mec type IVA in South Korea. J. Clin. Microbiol. 45:4021-4026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 709.Park, J. Y., J. S. Jin, H. Y. Kang, E. H. Jeong, J. C. Lee, Y. C. Lee, S. Y. Seol, D. T. Cho, and J. Kim. 2007. A comparison of adult and pediatric methicillin-resistant Staphylococcus aureus isolates collected from patients at a university hospital in Korea. J. Microbiol. 45:447-452. [PubMed] [Google Scholar]
- 710.Park, M. K., M. H. Jung, H. J. Kang, J. S. Woo, H. M. Lee, H. H. Jung, S. J. Hwang, and S. W. Chae. 2008. The changes of MRSA infection in chronic suppurative otitis media. Otolaryngol. Head Neck Surg. 139:395-398. [DOI] [PubMed] [Google Scholar]
- 711.Pate, K. R., R. L. Nolan, T. L. Bannerman, and S. Feldman. 1995. Methicillin-resistant Staphylococcus aureus in the community. Lancet 346:978. [DOI] [PubMed] [Google Scholar]
- 712.Patel, A. H., P. Nowlan, E. D. Weavers, and T. Foster. 1987. Virulence of protein A-deficient and alpha-toxin-deficient mutants of Staphylococcus aureus isolated by allele replacement. Infect. Immun. 55:3103-3110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 713.Patel, J. B., R. J. Gorwitz, and J. A. Jernigan. 2009. Mupirocin resistance. Clin. Infect. Dis. 49:935-941. [DOI] [PubMed] [Google Scholar]
- 714.Patel, M., C. J. Hoesley, S. A. Moser, A. M. Stamm, J. W. Bradley, and K. B. Waites. 2008. Dissemination of community-associated methicillin-resistant Staphylococcus aureus in a tertiary care hospital. South. Med. J. 101:40-45. [DOI] [PubMed] [Google Scholar]
- 715.Patel, M., K. B. Waites, C. J. Hoesley, A. M. Stamm, K. C. Canupp, and S. A. Moser. 2008. Emergence of USA300 MRSA in a tertiary medical centre: implications for epidemiological studies. J. Hosp. Infect. 68:208-213. [DOI] [PubMed] [Google Scholar]
- 716.Patel, M., R. A. Kumar, A. M. Stamm, C. J. Hoesley, S. A. Moser, and K. B. Waites. 2007. USA300 genotype community-associated methicillin-resistant Staphylococcus aureus as a cause of surgical site infections. J. Clin. Microbiol. 45:3431-3433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 717.Paule, S. M., A. Robicsek, R. Thompson, K. Kaul, and L. R. Peterson. 2008. Three years of universal surveillance and decolonization: the effect on mupirocin resistance, abstr. C2-1069. Abstr. 48th Annu. Intersci. Conf. Antimicrob. Agents Chemother. (ICAAC)-Infect. Dis. Soc. Am. (IDSA) 46th Annu. Meet. American Society for Microbiology and Infectious Diseases Society of America, Washington, DC.
- 718.Paydar, K. Z., S. L. Hansen, E. D. Charlebois, H. W. Harris, and D. M. Young. 2006. Inappropriate antibiotic use in soft tissue infections. Arch. Surg. 141:850-854. [DOI] [PubMed] [Google Scholar]
- 719.Peleg, A. Y., and W. J. Munckhof. 2004. Fatal necrotising pneumonia due to community-acquired methicillin-resistant Staphylococcus aureus (MRSA). Med. J. Aust. 181:228-229. [DOI] [PubMed] [Google Scholar]
- 720.Peleg, A. Y., W. J. Munckhof, S. L. Kleinschmidt, A. J. Stephens, and F. Huygens. 2005. Life-threatening community-acquired methicillin-resistant Staphylococcus aureus infection in Australia. Eur. J. Clin. Microbiol. Infect. Dis. 24:384-387. [DOI] [PubMed] [Google Scholar]
- 721.Perkins, D., J. S. Hogue, M. Fairchok, L. Braun, and H. B. Viscount. 2008. Mupirocin resistance screening of methicillin-resistant Staphylococcus aureus isolates at the Madigan Army Medical Center. Mil. Med. 173:604-608. [DOI] [PubMed] [Google Scholar]
- 722.Persoons, D., S. Van Hoorebeke, K. Hermans, P. Butaye, A. de Kruif, F. Haesebrouke, and J. Dewulf. 2009. Methicillin-resistant Staphylococcus aureus in poultry. Emerg. Infect. Dis. 15:452-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 723.Piao, C., T. Karasawa, K. Totsuka, T. Uchiyama, and K. Kikuchi. 2005. Prospective surveillance of community-onset and healthcare-associated methicillin-resistant Staphylococcus aureus isolated from a university-affiliated hospital in Japan. Microbiol. Immunol. 49:959-970. [DOI] [PubMed] [Google Scholar]
- 724.Pierce, J. R., Q. Saeed, and W. R. Davis. 2008. Prostatic abscess due to community-acquired methicillin-resistant Staphylococcus aureus. Am. J. Med. Sci. 335:154-156. [DOI] [PubMed] [Google Scholar]
- 725.Pillar, C., M. K. Aranza, D. Shah, and D. F. Sahm. 2008. In vitro activity profile of ceftobiprole, an anti-MRSA cephalosporin, against recent Gram-positive and Gram-negative isolates of European origin. J. Antimicrob. Chemother. 61:595-602. [DOI] [PubMed] [Google Scholar]
- 726.Pinho, M. G., H. de Lencastre, and A. Tomasz. 2001. An acquired and a native penicillin-binding protein cooperate in building the cell wall of drug-resistant staphylococci. Proc. Natl. Acad. Sci. U. S. A. 98:10886-10891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 727.Pinter, D. M., J. Mandel, K. G. Hulten, H. Minkoff, and M. F. Tosi. 2009. Maternal-infant perinatal transmisson of methicillin-resistant and methicillin-sensitive Staphylococcus aureus. Am. J. Perinatol. 26:145-151. [DOI] [PubMed] [Google Scholar]
- 728.Pistella, E., F. Campanile, D. Bongiorno, S. Stefani, G. D. Di Nucci, P. Serra, and M. Venditti. 2004. Successful treatment of disseminated cerebritis complicating methicillin-resistant Staphylococcus aureus endocarditis unresponsive to vancomycin therapy with linezolid. Scand. J. Infect. Dis. 36:222-225. [DOI] [PubMed] [Google Scholar]
- 729.Podewils, L. J., L. A. Liedtke, L. C. McDonald, J. C. Hageman, L. S. Strausbaugh, T. K. Fischer, D. B. Jernigan, T. M. Uyeki, M. J. Kuehnert, and Infectious Diseases Society of America Emerging Infections Network. 2005. A national survey of severe influenza-associated complications among children and adults, 2003-2004. Clin. Infect. Dis. 40:1693-1696. [DOI] [PubMed] [Google Scholar]
- 730.Pomba, C., H. Hasman, L. M. Cavaco, J. D. de Fonseca, and F. M. Aarestrup. 2009. First description of meticillin-resistant Staphylococcus aureus (MRSA) CC30 and CC398 from swine in Portugal. Int. J. Antimicrob. Agents 34:193-194. [DOI] [PubMed] [Google Scholar]
- 731.Popovich, K., B. Hota, A. Aroutcheva, and R. A. Weinstein. 2007. A phenotypic prediction rule for community-associated methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 45:2293-2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 732.Popovich, K. J., R. A. Weinstein, and B. Hota. 2008. Are community-associated methicillin-resistant Staphylococcus aureus (MRSA) strains replacing traditional nosocomial strains? Clin. Infect. Dis. 46:787-894. [DOI] [PubMed] [Google Scholar]
- 733.Popovich, K., R. A. Weinstein, A. Aroutcheva, T. Rice, and B. Hota for CDC Prevention Epicenters. 2008. Community-associated methicillin-resistant Staphylococcus aureus and HIV—intersecting epidemics, abstr. L-776. Abstr. 48th Annu. Intersci. Conf. Antimicrob. Agents Chemother. (ICAAC)-Infect. Dis. Soc. Am. (IDSA) 46th Annu. Meet. American Society for Microbiology and Infectious Diseases Society of America, Washington, DC. [DOI] [PubMed]
- 734.Poulakou, G., and H. Giamarellou. 2008. Oritavancin: a new promising agent in the treatment of infections due to Gram-positive pathogens. Expert Opin. Invest. Drugs 17:225-243. [DOI] [PubMed] [Google Scholar]
- 735.Powell, J. P., and R. P. Wenzel. 2008. Antibiotic options for community-acquired MRSA. Expert Rev. Anti Infect. Ther. 6:299-307. [DOI] [PubMed] [Google Scholar]
- 736.Proctor, R. A. 2006. Community acquired methicillin-resistant Staphylococcus aureus: a Wisconsin perspective. Wisconsin Med. J. 105:40-45. [PubMed] [Google Scholar]
- 737.Proctor, R. A. 2008. Role of folate antagonists in the treatment of methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 46:584-593. [DOI] [PubMed] [Google Scholar]
- 738.Pu, S., F. Han, and B. Ge. 2009. Isolation and characterization of methicillin-resistant Staphylococcus aureus from Louisiana retail meats. Appl. Environ. Microbiol. 75:265-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 739.Purcell, K., and J. Fergie. 2005. Epidemic of community-acquired methicillin-resistant Staphylococcus aureus infections. Arch. Pediatr. Adolesc. Med. 159:980-985. [DOI] [PubMed] [Google Scholar]
- 740.Purcell, K., and J. E. Fergie. 2002. Exponential increase in community-acquired methicillin-resistant Staphylococcus aureus infections in south Texas children. Pediatr. Infect. Dis. J. 21:988-989. [DOI] [PubMed] [Google Scholar]
- 741.Purcell, K., J. Fergie, and M. D. Peterson. 2006. Economic impact of the community-acquired methicillin-resistant Staphylococcus aureus epidemic on the Driscoll Children's Health Plan. Pediatr. Infect. Dis. J. 25:178-180. [DOI] [PubMed] [Google Scholar]
- 742.Quagliarello, B., C. Cespedes, M. Miller, A. Toro, P. Vavagiakis, R. S. Klein, and F. D. Lowy. 2002. Strains of Staphylococcus aureus obtained from drug-use networks are closely linked. Clin. Infect. Dis. 35:671-677. [DOI] [PubMed] [Google Scholar]
- 743.Rahimian, J., R. Khan, and K. A. LaScalea. 2007. Does nasal colonization or mupirocin treatment affect recurrence of methicillin-resistant Staphylococcus aureus skin and skin structure infections? Infect. Control Hosp. Epidemiol. 28:1415-1416. [DOI] [PubMed] [Google Scholar]
- 744.Rajendran, P. M., D. Young, T. Maurer, H. Chambers, F. Perdreau-Remington, P. Ro, and H. Harris. 2007. Randomized, double-blind, placebo-controlled trial of cephalexin for treatment of uncomplicated skin abscesses in a population at risk for community methicillin-resistant Staphylococcus aureus infection. Antimicrob. Agents Chemother. 51:4044-4048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 745.Ramana, K. V., S. K. Mohanty, and C. G. Wilson. 2009. Staphylococcus aureus of anterior nares of school going children. Indian J. Pediatr. 76:813-816. [DOI] [PubMed] [Google Scholar]
- 746.Rampling, A., S. Wiseman, L. Davis, A. P. Hyett, A. N. Walbridge, G. C. Payne, and A. J. Cornaby. 2001. Evidence that hospital hygiene is important in the control of methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 49:109-116. [DOI] [PubMed] [Google Scholar]
- 747.Rankin, S., S. Roberts, K. O'Shea, D. Maloney, M. Lorenzo, and C. E. Benson. 2005. Panton Valentine leukocidin (PVL) toxin positive MRSA strains isolated from companion animals. Vet. Microbiol. 108:145-148. [DOI] [PubMed] [Google Scholar]
- 748.Rathore, M. H., and M. W. Kline. 1989. Community-acquired methicillin-resistant Staphylococcus aureus infections in children. Pediatr. Infect. Dis. J. 8:645-647. [DOI] [PubMed] [Google Scholar]
- 749.Raz, R., D. Miron, R. Colodner, Z. Staler, Z. Samara, and Y. Keness. 1996. A 1-year trial of nasal mupirocin in the prevention of recurrent staphylococcal nasal colonization and skin infection. Arch. Intern. Med. 156:1109-1112. [PubMed] [Google Scholar]
- 750.Reddy, P., C. Qi, T. Zembower, G. A. Noskin, and M. Bolon. 2007. Postpartum mastitis and community-acquired methicillin-resistant Staphylococcus aureus. Emerg. Infect. Dis. 13:298-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 751.Reed, C., A. J. Kallen, M. Patton, K. E. Arnold, M. M. Farley, J. Hageman, and L. Finelli. 2009. Infection with community-onset Staphylococcus aureus and influenza virus in hospitalized children. Pediatr. Infect. Dis. J. 28:572-576. [DOI] [PubMed] [Google Scholar]
- 752.Regev-Yochay, G., K. Trzciński, C. M. Thompson, R. Malley, and M. Lipsitch. 2006. Interference between Streptococcus pneumoniae and Staphylococcus aureus: in vitro hydrogen peroxide-mediated killing by Streptococcus pneumoniae. J. Bacteriol. 188:4996-5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 753.Regev-Yochay, G., R. Dagan, M. Raz, Y. Carmeli, B. Shainberg, E. Derazne, G. Rahav, and E. Rubinstein. 2004. Association between carriage of Streptococcus pneumoniae and Staphylococcus aureus in children. JAMA 292:716-720. [DOI] [PubMed] [Google Scholar]
- 754.Regev-Yochay, G., R. Malley, E. Rubinstein, M. Raz, R. Dagan, and M. Lipsitch. 2008. In vitro bactericidal activity of Streptococcus pneumoniae and bactericidal susceptibility of Staphylococcus aureus strains isolated from cocolonized versus noncocolonized children. J. Clin. Microbiol. 46:747-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 755.Ren, C. L., W. J. Morgan, M. W. Konstan, M. S. Schechter, J. S. Wagener, K. A. Fisher, and W. E. Regelmann for the Investigators and Coordinators of the Epidemiologic Study of Cystic Fibrosis. 2007. Presence of methicillin-resistant Staphylococcus aureus in respiratory cultures from cystic fibrosis patients is associated with lower lung function. Pediatr. Pulmonol. 42:513-518. [DOI] [PubMed] [Google Scholar]
- 756.Reusch, M., P. Ghosh, C. Ham, A. Klotchko, S. Singapuri, and G. Everett. 2008. Prevalence of MRSA colonization in peripartum mothers and their newborn infants. Scand. J. Infect. Dis. 40:667-671. [DOI] [PubMed] [Google Scholar]
- 757.Ribeiro, A., A. Z. Coronado, M. C. Silva-Carvalho, B. T. Ferreira-Carvalho, C. Dias, R. Rozenbaum, P. F. Del Peloso, C. F. Leite, L. A. Teixeira, and A. M. Sá Figueirdo. 2007. Detection and characterization of international community-acquired infections by methicillin-resistant Staphylococcus aureus clones in Rio de Janeiro and Porto Alegre cities causing both community- and hospital-associated diseases. Diagn. Microbiol. Infect. Dis. 59:339-345. [DOI] [PubMed] [Google Scholar]
- 758.Ribeiro, A., C. Dias, M. C. Silva-Carvalho, L. Berquó, F. A. Ferreira, R. N. S. Santos, B. T. Ferreira-Carvalho, and A. M. Figueiredo. 2005. First report of infection with community-acquired methicillin-resistant Staphylococcus aureus in South America. J. Clin. Microbiol. 43:1985-1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 759.Rich, M., L. Roberts, and A. Kearns. 2005. Methicillin-resistant staphylococci isolated from animals. Vet. Microbiol. 105:313-314. [DOI] [PubMed] [Google Scholar]
- 760.Rihn, J. A., K. Posfay-Barbe, C. D. Harner, A. Macurak, A. Farley, K. Greenawalt, and M. G. Michaels. 2005. Community-acquired methicillin-resistant Staphylococcus aureus outbreaks in a local high school football team unsuccessful interventions. Pediatr. Infect. Dis. J. 24:841-843. [DOI] [PubMed] [Google Scholar]
- 761.Riley, T. V., and I. L. Rouse. 1995. Methicillin-resistant Staphylococcus aureus in Western Australia, 1983-1992. J. Hosp. Infect. 29:177-188. [DOI] [PubMed] [Google Scholar]
- 762.Rim, J. Y., and A. E. Bacon. 2007. Prevalence of community-acquired methicillin-resistant Staphylococcus aureus colonization in a random sample of healthy individuals. Infect. Control Hosp. Epidemiol. 28:1044-1046. [DOI] [PubMed] [Google Scholar]
- 763.Risson, D. C., E. D. O'Connor, R. W. Guard, J. M. Schooneveldt, and G. R. Nimmo. 2007. A fatal case of necrotising pneumonia due to community-associated methicillin-resistant Staphylococcus aureus. Med. J. Aust. 186:479-480. [DOI] [PubMed] [Google Scholar]
- 764.Rittenhouse, S., S. Biswas, J. Broskey, L. McCloskey, T. Moore, S. Vasey, J. West, M. Zalacain, R. Zonis, and D. Payne. 2006. Selection of retapamulin, a novel pleuromutilin for topical use. Antimicrob. Agents Chemother. 50:3882-3885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 765.Roberts, J. C., S. P. Gulino, K. K. Peak, V. A. Luna, and R. Sanderson. 2008. Fatal necrotizing pneumonia due to a Panton-Valentine leukocidin positive community-associated methicillin-sensitive Staphylococcus aureus and influenza coinfection: a case report. Ann. Clin. Microbiol. Antimicrob. 7:5. doi: 10.1186/1476-0711-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 766.Roberts, J. R. 2007. Lap dancer's lament: an occupational hazard related to community associated methicillin-resistant Staphylococcus aureus. Ann. Emerg. Med. 49:116-117. [DOI] [PubMed] [Google Scholar]
- 767.Roberts, J. R., L. McCawley, M. Laxton, and H. Trumbo. 2007. Genital community associated methicillin-resistant Staphylococcus aureus infection can be a sexually transmitted disease. Ann. Emerg. Med. 50:93-94. [DOI] [PubMed] [Google Scholar]
- 768.Roberts, S. S., and R. J. Kazragis. 2009. Methicillin resistant Staphylococcus aureus infections in U.S. service members deployed to Iraq. Mil. Med. 174:408-411. [DOI] [PubMed] [Google Scholar]
- 769.Robicsek, A., J. L. Beaumont, and L. R. Peterson. 2009. Duration of colonization with methicillin resistant Staphylococcus aureus. Clin. Infect. Dis. 48:910-913. [DOI] [PubMed] [Google Scholar]
- 770.Robinson, D. A., A. M. Kearns, A. Holmes, D. Morrison, H. Grundmann, G. Edwards, F. G. O'Brien, F. C. Tenover, L. K. McDougal, A. B. Monk, and M. C. Enright. 2005. Re-emergence of early pandemic Staphylococcus aureus as a community-acquired meticillin-resistant clone. Lancet 365:1256-1258. [DOI] [PubMed] [Google Scholar]
- 771.Robinson, D. A., and M. C. Enright. 2003. Evolutionary models of the emergence of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 47:3926-3934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 772.Roecker, A. M., and S. D. Pope. 2008. Dalbavancin: a lipoglycopeptide antibacterial for Gram-positive infections. Expert Opin. Pharmacother. 9:1745-1754. [DOI] [PubMed] [Google Scholar]
- 773.Rohr, U., M. Wilhelm, G. Muhr, and S. Gatermann. 2004. Qualitative and (semi)quantitative characterization of nasal and skin methicillin-resistant Staphylococcus aureus carriage of hospitalized patients. Int. J. Hyg. Environ. Health 207:51-55. [DOI] [PubMed] [Google Scholar]
- 774.Rollason, J., L. Bastin, A. C. Hilton, D. G. Pillay, T. Worthington, C. McKeon, P. De, K. Burrows, and P. A. Lambert. 2008. Epidemiology of community-acquired meticillin-resistant Staphylococcus aureus obtained from the UK West Midlands region. J. Hosp. Infect. 70:314-320. [DOI] [PubMed] [Google Scholar]
- 775.Romano, R., D. Lu, and P. Holtom. 2006. Outbreak of community-acquired methicillin-resistant Staphylococcus aureus skin infections among a collegiate football team. J. Athl. Train. 41:141-145. [PMC free article] [PubMed] [Google Scholar]
- 776.Rose, W. E., and M. J. Rybak. 2006. Tigecycline: first of a new class of antimicrobial agents. Pharmacotherapy 26:1099-1110. [DOI] [PubMed] [Google Scholar]
- 777.Rosenthal, A., D. White, S. Churilla, S. Brodie, and K. C. Katz. 2006. Optimal surveillance culture sites for detection of methicillin-resistant Staphylococcus aureus in newborns. J. Clin. Microbiol. 44:4234-4236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 778.Rossney, A. S., A. C. Shore, P. M. Morgan, M. M. Fitzgibbon, B. O'Connell, and D. C. Coleman. 2007. The emergence and importation of diverse genotypes of MRSA harboring the Panton-Valentine leukocidin gene (pvl) reveal that pvl is a poor marker for community-acquired MRSA in Ireland. J. Clin. Microbiol. 45:2554-2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 779.Rossney, A., and S. O'Connell. 2008. Emerging high-level mupirocin resistance among MRSA isolates in Ireland. Euro Surveill. 13(14):pii=8084. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=8084. [PubMed] [Google Scholar]
- 780.Rozenbaum, R., M. C. Silva-Carvalho, R. R. Souza, M. C. N. Melo, C. N. Gobbi, L. R. Coelho, R. L. Ferreira, B. T. Ferreira-Carvalho, A. L. Schuenck, F. M. C. S. Neves, L. R. P. O. F. Silva, and A. M. S. Figueiredo. 2006. Molecular characterization of methicillin-resistant Staphylococcus aureus disseminated in a home care system. Infect. Control Hosp. Epidemiol. 27:1041-1050. [DOI] [PubMed] [Google Scholar]
- 781.Rubinstein, E., M. H. Kollef, and D. Nathwani. 2008. Pneumonia caused by methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 46(Suppl. 5):S378-S385. [DOI] [PubMed] [Google Scholar]
- 782.Rubinstein, E., P. Prokocimer, and G. H. Talbot. 1999. Safety and tolerability of quinupristin/dalfopristin: administration guidelines. J. Antimicrob. Chemother. 44(Topic A):37-46. [DOI] [PubMed] [Google Scholar]
- 783.Ruhe, J. J., and A. Menon. 2007. Tetracyclines as an oral treatment option for patients with community-onset methicillin-resistant Staphylococcus aureus skin and soft-tissue infections. Antimicrob. Agents Chermother. 51:3298-3303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 784.Ruhe, J. J., N. Smith, R. W. Bradsher, and A. Menon. 2007. Community-onset methicillin-resistant Staphylococcus aureus skin and soft tissue infections: impact of antimicrobial therapy on outcome. Clin. Infect. Dis. 44:777-784. [DOI] [PubMed] [Google Scholar]
- 785.Ruimy, R., A. Maiga, L. Armand-Lefevre, I. Maiga, A. Diallo, A. K. Koumaré, K. Ouattara, S. Soumaré, K. Gaillard, J. C. Lucet, A. Andrement, and E. J. Feil. 2008. The carriage population of Staphylococcus aureus from Mali is composed of a combination of pandemic clones and the divergent Panton-Valentine leukocidin-positive genotype ST152. J. Bacteriol. 190:3962-3968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 786.Ruppitsch, W., A. Stoger, D. Schmid, R. Fretz, A. Indra, F. Allerberger, and W. Witte. 2007. Occurrence of the USA300 community-acquired Staphylococcus aureus clone in Austria. Euro Surveill. 12(43):pii=3294. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=3294. [DOI] [PubMed] [Google Scholar]
- 787.Russell, A. D., and M. J. Day. 1993. Antibacterial efficacy of chlorhexidine. J. Hosp. Infect. 25:229-238. [DOI] [PubMed] [Google Scholar]
- 788.Rutar, T. 2009. Vertically acquired community methicillin-resistant Staphylococcus aureus dacrocystitis in a neonate. J. AAPOS 13:79-81. [DOI] [PubMed] [Google Scholar]
- 789.Rutar, T., O. M. Zwick, K. P. Cockerham, and J. C. Horton. 2005. Bilateral blindness from orbital cellulitis caused by community-acquired methicillin-resistant Staphylococcus aureus. Am. J. Ophthalmol. 140:740-742. [DOI] [PubMed] [Google Scholar]
- 790.Rutland, B. E., J. S. Weese, C. Bolin, J. Au, and A. N. Malani. 2009. Human-to-dog transmission of methicillin-resistant Staphylococcus aureus. Emerg. Infect. Dis. 15:1328-1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 791.Saavedra-Lozano, J., A. Mejías, N. Ahmad, E. Peromingo, M. I. Ardura, S. Guillen, A. Syed, D. Cavuoti, and O. Ramilo. 2008. Changing trends in acute osteomyelitis in children: impact of methicillin-resistant Staphylococcus aureus infections. J. Pediatr. Orthop. 28:569-575. [DOI] [PubMed] [Google Scholar]
- 792.Saben, B. 2004. Community-acquired methicillin-resistant Staphylococcus aureus skin infection in a football player. Curr. Sports Med. Rep. 3:269-271. [DOI] [PubMed] [Google Scholar]
- 793.Sabol, W. J., T. D. Minton, and P. M. Harrison. 2008. Prison and jail inmates at midyear 2006, bulletin. NCJ 217675. Bureau of Justice Statistics, Office of Justice Programs, Department of Justice, Washington, DC. http://www.ojp.usdoj.gov/bjs/pub/pdf/pjim06.pdf.
- 794.Saiman, L., M. O'Keefe, P. L. Graham, F. Wu, B. Saïd-Salim, B. Kreiswirth, A. LaSala, P. M. Schlievert, and P. Della-Latta. 2003. Hospital transmission of community-acquired methicillin-resistant Staphylococcus aureus among postpartum women. Clin. Infect. Dis. 37:1313-1319. [DOI] [PubMed] [Google Scholar]
- 795.Sakoulas, G., R. C. Moellering, and G. M. Eliopoulos. 2006. Adaptation of methicillin-resistant Staphylococcus aureus in the face of vancomycin therapy. Clin. Infect. Dis. 42(Suppl. 1):S40-S50. [DOI] [PubMed] [Google Scholar]
- 796.Salgado, C. D., B. M. Farr, and D. P. Calfee. 2003. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin. Infect. Dis. 36:131-139. [DOI] [PubMed] [Google Scholar]
- 797.Salliot, C., V. Zeller, X. Puechal, V. Manceron, S. Sire, N. Varache, J. Etienne, N. Desplaces, and J. M. Ziza. 2006. Panton-Valentine leukocidin-producing Staphylococcus aureus infections: report of 4 French cases. Scand. J. Infect. Dis. 38:192-195. [DOI] [PubMed] [Google Scholar]
- 798.Salmenlinna, S., O. Lyytikäinen, and J. Vuopio-Varkila. 2002. Community-acquired methicillin-resistant Staphylococcus aureus, Finland. Emerg. Infect. Dis. 8:602-607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 799.Sam, I. C., M. Kahar-Bador, Y. F. Chan, S. K. Loong, and F. M. N. Ghazali. 2008. Multisensitive community-acquired methicillin-resistant Staphylococcus aureus infections in Malaysia. Diagn. Microbiol. Infect. Dis. 62:437-439. [DOI] [PubMed] [Google Scholar]
- 800.Sanford, M. D., A. F. Widmer, M. J. Bale, R. N. Jones, and R. P. Wenzel. 1994. Efficient detection and long-term persistence of the carriage of methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 19:1123-1128. [DOI] [PubMed] [Google Scholar]
- 801.Saravolatz, L. D., N. Markowitz, L. Arking, D. Pohlod, and E. Fisher. 1982. Methicillin-resistant Staphylococcus aureus: epidemiologic observations during a community-acquired outbreak. Ann. Intern. Med. 96:11-16. [DOI] [PubMed] [Google Scholar]
- 802.Sattler, C. A., E. O. Mason, and S. L. Kaplan. 2002. Prospective comparison of risk factors and demographic and clinical characteristics of community-acquired, methicillin-resistant versus methicillin-susceptible Staphylococcus aureus infection in children. Pediatr. Infect. Dis. J. 21:910-916. [DOI] [PubMed] [Google Scholar]
- 803.Saunders, A., L. Panaro, A. McGeer, A. Rosenthal, D. White, B. M. Willey, D. Gravel, E. Bontovics, B. Yaffe, and K. Katz. 2007. A nosocomial outbreak of community-associated methicillin-resistant Staphylococcus aureus among healthy newborns and postpartum mothers. Can. J. Infect. Dis. Med. Microbiol. 18:128-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 804.Sawicki, G. S., F. L. Lu, C. Valim, R. H. Cleveland, and A. A. Colin. 2008. Necrotising pneumonia is an increasingly detected complication of pneumonia in children. Eur. Respir. J. 31:1285-1291. [DOI] [PubMed] [Google Scholar]
- 805.Sawicki, G. S., L. Rasouliyan, and C. L. Ren. 2009. The impact of MRSA on lung function in patients with cystic fibrosis. Am. J. Respir. Crit. Care Med. 179:734-735. [DOI] [PubMed] [Google Scholar]
- 806.Sawicki, G. S., L. Rasouliyan, D. J. Pasta, W. R. Regelmann, J. L. Wagener, D. A. Waltz, and C. L. Ren for the Investigators and Coordinators of the Epidemiologic Study of Cystic Fibrosis. 2008. The impact of incident methicillin-resistant Staphylococcus aureus detection on pulmonary function in cystic fibrosis. Pediatr. Pulmonol. 43:1117-1123. [DOI] [PubMed] [Google Scholar]
- 807.Sax, H., K. Posfay-Barbe, S. Harbarth, P. Francois, S. Touveneau, C. L. Pessoa-Silva, J. Schrenzel, S. Dharan, A. Gervaix, and D. Pittet. 2006. Control of a cluster of community-associated, methicillin-resistant Staphylococcus aureus in neonatology. J. Hosp. Infect. 63:93-100. [DOI] [PubMed] [Google Scholar]
- 808.Sayana, S., and H. Khanlou. 2008. Meningitis due to hematogenous dissemination of community-associated methicillin-resistant Staphylococcus aureus (MRSA) in a patient with AIDS. J. Int. Assoc. Physicians AIDS Care 7:289-291. [DOI] [PubMed] [Google Scholar]
- 809.Schneider-Lindner, V., J. A. Delaney, S. Dial, A. Dascal, and S. Suissa. 2007. Antimicrobial drugs and community-acquired methicillin-resistant Staphylococcus aureus, United Kingdom. Emerg. Infect. Dis. 13:994-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 810.Schramm, G. E., J. A. Johnson, J. A. Doherty, S. T. Micek, and M. H. Kollef. 2007. Increasing incidence of sterile-site infections due to non-multidrug-resistant oxacillin-resistant Staphylococcus aureus among hospitalized patients. Infect. Control Hosp. Epidemiol. 28:95-97. [DOI] [PubMed] [Google Scholar]
- 811.Schulz, P., M. Allen, Q. Murray, S. A. Smith, L. Goss, R. Carrico, and J. Ramirez. 2005. Infections due to community-acquired methicillin-resistant Staphylococcus aureus: an emergent epidemic in Kentucky. J. Ky. Med. Assoc. 103:194-203. [PubMed] [Google Scholar]
- 812.Scott, E., S. Duty, and M. Callahan. 2008. A pilot study to isolate Staphylococcus aureus and methicillin-resistant S. aureus from environmental surfaces in the home. Am. J. Infect. Control 36:458-460. [DOI] [PubMed] [Google Scholar]
- 813.Scribel, L. V., M. C. Silva-Carvalho, R. R. Souza, S. V. Superti, C. H. C. Kvitko, A. M. S. Figueiredo, and A. P. Zavascki. 2009. Clinical and molecular epidemiology of methicillin-resistant Staphylococcus aureus carrying SCCmecIV in a university hospital in Porto Alegre, Brazil. Diagn. Microbiol. Infect. Dis. 65:457-461. [DOI] [PubMed] [Google Scholar]
- 814.Sdougkos, G., V. Chini, D. A. Papanastasiou, G. Christodoulou, E. Stamatakis, A. Vris, I. Christodoulidi, G. Protopapadakis, and I. Spiliopoulou. 2008. Community-associated methicillin resistant Staphylococcus aureus infections and nasal carriage among children: molecular microbial data and clinical characteristics. Clin. Microbiol. Infect. 14:995-1001. [DOI] [PubMed] [Google Scholar]
- 815.Sdougkos, G., V. Chini, D. A. Papanastasiou, G. Christodoulou, G. Tagaris, G. Dimitracopoulos, and I. Spiliopoulou. 2007. Methicillin-resistant Staphylococcus aureus producing Panton-Valentine leukocidin as a cause of acute osteomyelitis in children. Clin. Microbiol. Infect. 13:651-654. [DOI] [PubMed] [Google Scholar]
- 816.Seal, J. B., B. Moreira, C. D. Bethel, and R. S. Daum. 2003. Antimicrobial resistance in Staphylococcus aureus at the University of Chicago Hospitals: a 15-year longitudinal assessment in a large university-based hospital. Infect. Control Hosp. Epidemiol. 24:403-408. [DOI] [PubMed] [Google Scholar]
- 817.Seguin, J. C., R. D. Walker, J. P. Caron, W. E. Kloos, C. G. George, R. J. Hollis, R. N. Jones, and M. A. Pfaller. 1999. Methicillin-resistant Staphylococcus aureus outbreak in a veterinary teaching hospital: potential human-to-animal transmission. J. Clin. Microbiol. 37:1459-1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 818.Seifried, S. E., A. D. Tice, and M. Eischen. 2007. Diversity of community-associated strains of methicillin-resistant Staphylococcus aureus in Hawaii. J. Infect. Dis. 195:305. [DOI] [PubMed] [Google Scholar]
- 819.Sergio, D. M. B. S., T. H. Koh, L. Y. Hsu, B. E. Ogden, A. L. H. Goh, and P. K. H. Chow. 2007. Investigation of meticillin-resistant Staphylococcus aureus in pigs used for research. J. Med. Microbiol. 56:1107-1109. [DOI] [PubMed] [Google Scholar]
- 820.Seybold, U., E. V. Kourbatova, J. G. Johnson, S. J. Halvosa, Y. F. Wang, M. D. King, S. M. Ray, and H. M. Blumberg. 2006. Emergence of community-associated methicillin-resistant Staphylococcus aureus USA300 genotype as a major cause of health care-associated blood stream infections. Clin. Infect. Dis. 42:647-656. [DOI] [PubMed] [Google Scholar]
- 821.Seybold, U., N. J. Talati, Q. Kizilbash, M. Shah, H. M. Blumberg, and C. Franco-Paredes. 2007. Hematogenous osteomyelitis mimicking osteosarcoma due to community associated methicillin-resistant Staphylococcus aureus. Infection 35:190-193. [DOI] [PubMed] [Google Scholar]
- 822.Shahin, R., I. L. Johnson, F. Jamieson, A. McGreer, J. Tolkin, and E. L. Ford-Jones. 1999. Methicillin-resistant Staphylococcus aureus carriage in a child care center following a case of the disease. Arch. Pediatr. Adolesc. Med. 153:864-868. [DOI] [PubMed] [Google Scholar]
- 823.Shamsudin, M. N., Z. Sekawi, A. van Belkum, and V. Neela. 2008. First community-acquired meticillin-resistant Staphylococcus aureus in Malaysia. J. Med. Microbiol. 57:1180-1181. [DOI] [PubMed] [Google Scholar]
- 824.Shapiro, A., S. Raman, M. Johnson, and M. Piehl. 2009. Community-acquired MRSA infection in North Carolina children: prevalence, antibiotic sensitivities, and risk factors. N. C. Med. J. 70:102-107. [PubMed] [Google Scholar]
- 825.Shastry, L., J. Rahimian, and S. Lascher. 2007. Community associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections in men who have sex with men in New York City. Arch. Intern. Med. 167:854-857. [DOI] [PubMed] [Google Scholar]
- 826.Shedek, B. K., and E. J. Nilles. 2008. Community-associated methicillin-resistant Staphylococcus aureus pyomyositis complicated by compartment syndrome in an immunocompetent young woman. Am. J. Emerg. Med. 26:737.e3-737.e4. [DOI] [PubMed] [Google Scholar]
- 827.Shet, A., B. Mathema, J. R. Mediavilla, K. Kishii, S. Mehandru, P. Jeane-Pierre, M. Laroche, B. M. Willey, N. Kreiswirth, M. Markowitz, and B. N. Kreiswirth. 2009. Colonization and subsequent skin and soft tissue infection due to methicillin-resistant Staphylococcus aureus in a cohort of otherwise healthy adults infected with HIV type 1. J. Infect. Dis. 200:88-93. [DOI] [PubMed] [Google Scholar]
- 828.Shibuya, Y., M. Hara, W. Higuchi, T. Takano, Y. Iwao, and T. Yamamoto. 2008. Emergence of the community-acquired methicillin-resistant Staphylococcus aureus USA300 clone in Japan. J. Infect. Chemother. 14:439-441. [DOI] [PubMed] [Google Scholar]
- 829.Shimizu, A., K. Shimizu, and T. Nakamura. 2008. Non-pathogenic bacterial flora may inhibit colonization by methicillin-resistant Staphylococcus aureus in extremely low birth weight infants. Neonatology 93:158-161. [DOI] [PubMed] [Google Scholar]
- 830.Shiomori, T., H. Miyamoto, and K. Makishima. 2001. Significance of airborne transmission of methicillin-resistant Staphylococcus aureus in an otolaryngology-head and neck surgery unit. Arch. Otolaryngol. Head Neck Surg. 127:644-648. [DOI] [PubMed] [Google Scholar]
- 831.Shopsin, B., B. Mathema, X. Zhao, J. Martinez, J. Kornblum, and B. N. Kreiswirth. 2000. Resistance rather than virulence selects for the clonal spread of methicillin-resistant Staphylococcus aureus: implications for MRSA transmission. Microb. Drug Resist. 6:239-244. [DOI] [PubMed] [Google Scholar]
- 832.Shopsin, B., S. Hering, and B. N. Kreiswirth. 2003. Hospital-acquired and community-derived: the future of MRSA? Clin. Infect. Dis. 37:151-153. [DOI] [PubMed] [Google Scholar]
- 833.Shukla, S. K., M. E. Stemper, S. V. Ramaswamy, J. M. Conradt, R. Reich, E. A. Graviss, and K. D. Reed. 2004. Molecular characteristics of nosocomial and Native American community-associated methicillin-resistant Staphylococcus aureus clones from rural Wisconsin. J. Clin. Microbiol. 42:3752-3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 834.Siegel, J. D., E. Rhinehart, M. Jackson, L. Chiarello, and the Healthcare Infection Control Practices Advisory Committee. 2006. Management of multidrug-resistant organisms in healthcare settings, 2006. Centers for Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/ncidod/dhqp/pdf/ar/mdroGuideline2006.pdf. [DOI] [PubMed]
- 835.Sifri, C. D., J. Park, G. A. Helm, M. E. Stemper, and S. K. Shukla. 2007. Fatal brain abscess due to community-associated methicillin-resistant Staphylococcus aureus strain USA300. Clin. Infect. Dis. 45:e113-e117. [DOI] [PubMed] [Google Scholar]
- 836.Silverman, J. A., L. I. Mortin, A. D. Vanpraagh, T. Li, and J. Alder. 2005. Inhibition of daptomycin by pulmonary surfactant. J. Infect. Dis. 191:2149-2152. [DOI] [PubMed] [Google Scholar]
- 837.Simor, A. E., E. Phillips, A. McGeer, A. Konvalinka, M. Loeb, H. R. Devlin, and A. Kiss. 2007. Randomized controlled trial of chlorhexidine gluconate for washing, intranasal mupirocin, and rifampin and doxycycline versus no treatment for the eradication of methicillin-resistant Staphylococcus aureus colonization. Clin. Infect. Dis. 44:178-185. [DOI] [PubMed] [Google Scholar]
- 838.Simor, A. E., T. L. Stuart, L. Louie, C. Watt, M. Ofner-Agostini, D. Gravel, M. Mulvey, M. Loeb, A. McGreer, E. Bryce, A. Matlow, and the Canadian Nosocomial Infection Surveillance Program. 2007. Mupirocin-resistant, methicillin-resistant Staphylococcus aureus strains in Canadian hospitals. Antimicrob. Agents Chemother. 51:3880-3886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 839.Sing, A., C. Tuschak, and S. Hörmansdorfer. 2008. Methicillin-resistant Staphylococcus aureus in a family and its pet cat. N. Engl. J. Med. 358:1200-1201. [DOI] [PubMed] [Google Scholar]
- 840.Skiest, D. J., and T. W. Cooper. 2007. High recurrence rate of CA-MRSA skin and soft tissue infections. Ann. Intern. Med. 167:2527. [DOI] [PubMed] [Google Scholar]
- 841.Skiest, D. J., K. Brown, T. W. Cooper, H. Hoffman-Roberts, H. R. Mussa, and A. C. Elliott. 2007. Prospective comparison of methicillin-suceptible and methicillin-resistant Staphylococcus aureus infections in hospitalized patients. J. Infect. 54:427-434. [DOI] [PubMed] [Google Scholar]
- 842.Skiest, D., K. Brown, J. Hester, T. Moore, C. Crosby, H. R. Mussa, H. Hoffman-Roberts, and T. Cooper. 2006. Community-onset methicillin-resistant Staphylococcus aureus in an urban HIV clinic. HIV Med. 7:361-368. [DOI] [PubMed] [Google Scholar]
- 843.Skov, R., O. Gudlaugsson, H. Hardardottir, S. Harthug, T. Jakobsen, H. J. Kolmos, B. Olsson-Liljequist, R. Peltonen, Y. Tventen, J. Vuopio-Varkila, and C. Åhrén. 2008. Proposal of common Nordic epidemiological terms and definitions for methicillin-resistant Staphylococcus aureus (MRSA). Scand. J. Infect. Dis. 40:495-502. [DOI] [PubMed] [Google Scholar]
- 844.Skrupky, L. P., S. T. Micek, and M. H. Kollef. 2007. Optimizing therapy for MRSA pneumonia. Semin. Respir. Crit. Care Med. 28:615-623. [DOI] [PubMed] [Google Scholar]
- 845.Sligl, W., G. Taylor, R. T. N. Gibney, R. Rennie, and L. Chui. 2007. Methicillin-resistant Staphylococcus aureus in a Canadian intensive care unit: delays in initiating effective therapy due to low prevalence of infection. Can. J. Infect. Dis. Med. Microbiol. 18:139-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 846.Smith, T. C., M. J. Male, A. L. Harper, J. S. Kroeger, G. P. Tinker, E. D. Moritz, A. W. Capuano, L. A. Herwaldt, and D. J. Diekema. 2009. Methicillin-resistant Staphylococcus aureus (MRSA) strain ST398 is present in Midwestern U.S. swine and swine workers. PLoS One 4:e4258. doi: 10.1371/journal.pone.0004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 847.Söderquist, B., and C. Berglund. 2008. Simultaneous presence of an invasive and a carrier strain of methicillin-resistant Staphylococcus aureus (MRSA) in a family. Scand. J. Infect. Dis. 40:987-989. [DOI] [PubMed] [Google Scholar]
- 848.Söderquist, B., C. Berglund, and K. Strålin. 2006. Community-acquired pneumonia and bacteremia caused by an unusual methicillin-resistant Staphylococcus aureus (MRSA) strain with sequence type 36, staphylococcal cassette chromosome mec type IV and Panton-Valentine leukocidin genes. Eur. J. Clin. Microbiol. Infect. Dis. 25:604-606. [DOI] [PubMed] [Google Scholar]
- 849.Soge, O. O., J. S. Meschke, and M. C. Roberts. 2009. Methicillin-resistant Staphylococcus aureus and methicillin-resistant coagulase-negative Staphylococcus spp. from West Coast public marine parks, abstr. C2-146. Abstr. 49th Intersci. Conf. Antimicrob. Agents Chemother., San Francisco, CA. [DOI] [PMC free article] [PubMed]
- 850.Sokolov, K. M., E. Kreye, L. G. Miller, C. Choi, and A. W. Tang. 2007. Postpartum iliopsoas pyomyositis due to community-acquired methicillin-resistant Staphylococcus aureus. Obstet. Gynecol. 110:535-538. [DOI] [PubMed] [Google Scholar]
- 851.Sola, C., H. A. Saka, A. Vindel, J. L. Bocco, and the Córdoba S. aureus Collaborative Study Group. 2007. High frequency of Panton-Valentine leukocidin genes in invasive methicillin-susceptible strains and the relationship with methicillin-resistant Staphylococcus aureus in Córdoba, Argentina. Eur. J. Clin. Microbiol. Infect. Dis. 26:281-286. [DOI] [PubMed] [Google Scholar]
- 852.Sola, C., H. A. Saka, the Cordoba MRSA Collaborative Study Group, A. Vindel, and J. L. Bocco. 2008. Emergence and dissemination of a community-associated methicillin-resistant Panton-Valentin leukocidin-positive Staphylococcus aureus clone sharing the sequence type 5 lineage with the most prevalent nosocomial clone in the same region of Argentina. J. Clin. Microbiol. 46:1826-1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 853.Springer, B., U. Orendi, P. Much, G. Höger, W. Ruppitsch, K. Krziwanek, S. Metz-Gercek, and H. Mittermayer. 2009. Methicillin-resistant Staphylococcus aureus: a new zoonotic agent? Wien. Klin. Wochenschr. 121:86-90. (In German.) [DOI] [PubMed] [Google Scholar]
- 854.Stacey, A. R., K. E. Endersby, P. C. Chan, and R. R. Marples. 1998. An outbreak of methicillin-resistant Staphylococcus aureus infection in a rugby football team. Br. J. Sports Med. 32:153-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 855.Stafford, I., J. Hernandez, V. Laibl, J. Sheffield, S. Roberts, and G. W. Wendel. 2008. Community-acquired methicillin-resistant Staphylococcus aureus among patients with puerperal mastitis requiring hospitalization. Obstet. Gynecol. 112:533-537. [DOI] [PubMed] [Google Scholar]
- 856.Stam-Bolink, E. M., D. Mithoe, W. H. Baas, J. P. Arends, and A. V. M. Möller. 2007. Spread of a methicillin-resistant Staphylococcus aureus ST80 strain in the community of the northern Netherlands. Eur. J. Clin. Microbiol. Infect. Dis. 26:723-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 857.Stankovic, C., and P. V. Mahajan. 2006. Healthy children with invasive community-acquired methicillin-resistant Staphylococcus aureus infections. Pediatr. Emerg. Care 22:361-363. [DOI] [PubMed] [Google Scholar]
- 858.Stefani, S., D. Bangiorno, V. Cafiso, F. Campanile, M. Crapis, F. Cristini, A. Sartor, S. Scarparo, D. Spina, and P. Viale. 2009. Pathotype and susceptibility profile of a community-acquired methicillin resistant Staphylococcus aureus strain responsible for a case of severe pneumonia. Diagn. Microbiol. Infect. Dis. 63:100-104. [DOI] [PubMed] [Google Scholar]
- 859.Stein, G. E., and W. A. Craig. 2006. Tigecycline: a critical analysis. Clin. Infect. Dis. 43:518-524. [DOI] [PubMed] [Google Scholar]
- 860.Stenhem, M., A. Örtqvist, H. Ringberg, L. Larsson, B. Olsson-Liljequist, S. Hæggman, K. Ekdahl, and the Swedish Study Group on MRSA Epidemiology. 2006. Epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) in Sweden 2000-2003, increasing incidence and regional differences. BMC Infect. Dis. 6:30. doi: 10.1186/1471-2334-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 861.Stevens, C. L., A. Ralph, J. E. McLeod, and M. I. McDonald. 2006. Community-acquired methicillin-resistant Staphylococcus aureus in central Australia. Commun. Dis. Intell. 30:462-466. [PubMed] [Google Scholar]
- 862.Stevens, D. L., Y. Ma, D. B. Salmi, E. McIndoo, R. J. Wallace, and A. Bryant. 2007. Impact of antibiotics on the expression of virulence-associated exotoxin genes in methicillin-sensitive and in methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 195:202-211. [DOI] [PubMed] [Google Scholar]
- 863.Stevens, M. P., G. Bearman, A. Rosato, and M. Edmond. 2008. Community-acquired methicillin resistant Staphylococcus aureus in a women's collegiate basketball team. South. Med. J. 101:1067-1068. [DOI] [PubMed] [Google Scholar]
- 864.Storch, G. A., J. L. Radcliff, P. L. Meyer, and J. H. Hinrichs. 1987. Methicillin-resistant Staphylococcus aureus in a nursing home. Infect. Control 8:24-29. [DOI] [PubMed] [Google Scholar]
- 865.Strandén, A. M., R. Frei, H. Adler, U. Flückiger, and A. F. Widmer. 2009. Emergence of SCCmec type IV as the most common type of methicillin-resistant Staphylococcus aureus in a university hospital. Infection 37:44-48. [DOI] [PubMed] [Google Scholar]
- 866.Strandén, A., R. Frei, and A. F. Widmer. 2003. Molecular typing of methicillin-resistant Staphylococcus aureus: can PCR replace pulsed-field gel electrophoresis? J. Clin. Microbiol. 41:3181-3186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 867.Strassbaugh, L. J., C. Jacobson, D. L. Sewell, S. Potter, and T. T. Ward. 1991. Methicillin-resistant Staphylococcus aureus in extended-care facilities: experiences in a Veterans' Affairs nursing home and a review of the literature. Infect. Control Hosp. Epidemiol. 12:36-45. [DOI] [PubMed] [Google Scholar]
- 868.Strommenger, B., C. Braulke, D. Heuck, C. Schmidt, B. Pasemann, U. Nübel, and W. Witte. 2007. Spa typing of Staphylococcus aureus as a frontline tool in epidemiological typing. J. Clin. Microbiol. 46:574-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 869.Strommenger, B., C. Kehrenberg, C. Kettlitz, C. Cuny, J. Verspohl, W. Witte, and S. Schwarz. 2006. Molecular characterization of methicillin-resistant Staphylococcus aureus strains from pet animals and their relationship to human isolates. J. Antimicrob. Chemother. 57:461-465. [DOI] [PubMed] [Google Scholar]
- 870.Stumpf, P. G., M. Flores, and J. Murillo. 2008. Serious postpartum infection due to MRSA in an asymptomatic carrier: case report and review. Am. J. Perinatol. 25:413-415. [DOI] [PubMed] [Google Scholar]
- 871.Suggs, A. H., M. C. Maranan, S. Boyle-Vavra, and R. S. Daum. 1999. Methicillin-resistant and borderline methicillin-resistant asymptomatic Staphylococcus aureus colonization in children without identifiable risk factors. Pediatr. Infect. Dis. J. 18:410-414. [DOI] [PubMed] [Google Scholar]
- 872.Suh, L., S. Coffin, K. H. Leckerman, J. M. Gelfand, P. J. Honig, and A. C. Yang. 2008. Methicillin-resistant Staphylococcus aureus colonization of children with atopic dermatitis. Ped. Dermatol. 25:528-534. [DOI] [PubMed] [Google Scholar]
- 873.Suntharam, N., D. Hacek, and L. R. Peterson. 2001. Low prevalence of community-acquired methicillin-resistant Staphylococcus aureus in adults at a university hospital in the central United States. J. Clin. Microbiol. 39:1669-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 874.Szczesiul, J. M., K. M. Shermock, U. I. Murtaza, and G. K. Siberry. 2007. No decrease in clindamycin susceptibility despite increased use of clindamycin for pediatric community-associated methicillin-resistant Staphylococcus aureus skin infections. Pediatr. Infect. Dis. J. 26:852-854. [DOI] [PubMed] [Google Scholar]
- 875.Sztramko, R., K. Katz, T. Antoniou, M. R. Mulvey, J. Brunetta, F. Crouzat, C. Kovacs, B. Merkley, D. Tilley, and M. R. Loutfy. 2007. Community-associated methicillin-resistant Staphylococcus aureus infections in men who have sex with men: a case series. Can. J. Infect. Dis. Med. Microbiol. 18:257-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 876.Szumowski, J. D., D. E. Cohen, F. Kanaya, and K. H. Mayer. 2007. Treatment and outcomes of MRSA at an ambulatory clinic. Antimicrob. Agents Chemother. 51:423-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 877.Szumowski, J. D., K. M. Wener, H. S. Gold, M. Wong, L. Venkataraman, C. A. Runde, D. E. Cohen, K. H. Mayer, and S. B. Wright. 2009. Methicillin-resistant Staphylococcus aureus colonization, behavioral risk factors, and skin and soft-tissue infection at an ambulatory clinic serving a large population of HIV-infected men who have sex with men. Clin. Infect. Dis. 49:118-121. [DOI] [PubMed] [Google Scholar]
- 878.Tacconelli, E., L. Venkataraman, P. C. De Girolami, and E. M. C. D'Agata. 2004. Methicillin-resistant Staphylococcus aureus bacteraemia diagnosed at hospital admission: distinguishing between community-acquired versus healthcare-associated strains. J. Antimicrob. Chemother. 53:474-479. [DOI] [PubMed] [Google Scholar]
- 879.Takano, T., K. Saito, L. J. Teng, and T. Yamamoto. 2007. Spread of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) in hospitals in Tapei, Taiwan in 2005, and comparison of its drug resistance with previous hospital-acquired MRSA. Microbiol. Immunol. 51:627-632. [DOI] [PubMed] [Google Scholar]
- 880.Takano, T., W. Higuchi, T. Otsuka, T. Baranovich, S. Enany, K. Saito, H. Isobe, S. Dohmae, K. Ozaki, M. Takano, Y. Iwao, M. Shibuya, T. Okubo, S. Yabe, D. Shi, I. Reva, L. J. Teng, and T. Yamamoto. 2008. Novel characteristics of community-acquired methicillin-resistant Staphylococcus aureus belonging to multilocus sequence type 59 in Taiwan. Antimicrob. Agents Chemother. 52:837-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 881.Takizawa, Y., I. Taneike, S. Nakagawa, T. Oishe, Y. Nitihara, N. Iwakura, K. Ozaki, M. Takano, T. Nakayama, and T. Yamamoto. 2005. A Panton-Valentine leukocidin (PVL)-positive community-acquired methicillin-resistant Staphylococcus aureus (MRSA) strain, another such strain carrying a multiple-drug resistance plasmid, and other more-typical PVL-negative MRSA strains found in Japan. J. Clin. Microbiol. 43:3356-3363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 882.Talbot, G. H., J. Bradley, J. E. Edwards, D. Gilbert, M. Scheld, and J. G. Bartlett. 2006. Bad bugs need drugs: an update on the development pipeline from the antimicrobial availability task force of the Infectious Diseases Society of America. Clin. Infect. Dis. 42:657-668. [DOI] [PubMed] [Google Scholar]
- 883.Talbot, T. R., J. J. Nania, P. W. Wright, I. Jones, and D. Aronsky. 2007. Evaluation of the microbiology of soft-tissue abscesses in the era of community-associated strains of methicillin-resistant Staphylococcus aureus: an argument for empirical contact precautions. Infect. Control Hosp. Epidemiol. 28:730-732. [DOI] [PubMed] [Google Scholar]
- 884.Tam, V. H., A. Louie, T. R. Frische, M. Desiel, W. Liu, D. L. Brown, L. Deshpande, R. Leary, R. N. Jones, and G. L. Drusano. 2007. Impact of drug-exposure intensity and duration of therapy on the emergence of Staphylococcus aureus resistance to a quinolone antimicrobial. J. Infect. Dis. 195:1818-1827. [DOI] [PubMed] [Google Scholar]
- 885.Tammelin, A., F. Klötz, A. Hambræus, E. Ståhle, and U. Ransjö. 2003. Nasal and hand carriage of Staphylococcus aureus in staff at a department for thoracic and cardiovascular surgery: endogenous or exogenous source? Infect. Control Hosp. Epidemiol. 24:686-689. [DOI] [PubMed] [Google Scholar]
- 886.Taneike, I., T. Otsuka, S. Dohmae, S. Saito, K. Ozaki, M. Takano, W. Higuchi, T. Takano, and T. Yamamoto. 2006. Molecular nature of methicillin-resistant Staphylococcus aureus derived from explosive nosocomial outbreaks of the 1980s in Japan. FEBS Lett. 580:2323-2334. [DOI] [PubMed] [Google Scholar]
- 887.Tang, C. T., N. D. Tho, N. T. Hoa, N. T. M. Phuong, L. V. Tuan, T. S. Diep, J. Lindsay, N. T. Dung, B. V. Cam, L. Q. Thinh, L. T. Hai, L. D. Linh, J. Campbell, N. T. K. Tien, N. V. V. Chau, J. Cockfield, L. T. Giang, P. V. Nghiem, L. H. Son, H. T. Son, L. V. Phung, M. Counahan, A. Bentsi-Enchill, R. Brown, J. Simmerman, N. T. Chinh, T. T. Hien, J. Farrar, and C. Shultsz. 2007. An outbreak of severe infection with community-acquired MRSA carrying Panton-Valentine leukocidin following vaccination. PLoS One 2:e822. doi: 10.1371/journal.pone.0000822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 888.Tattevin, P., B. A. Diep, M. Jula, and F. Perdreau-Remington. 2008. Long-term follow-up of methicillin-resistant Staphylococcus aureus molecular epidemiology after emergence of clone USA300 in San Francisco jail populations. J. Clin. Microbiol. 46:4056-4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 889.Tattevin, P., B. A. Diep, M. Jula, and F. Perdreau-Remington. 2009. Methicillin-resistant Staphylococcus aureus USA300 clone in a long-term care facility. Emerg. Infect. Dis. 15:953-955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 890.Tattevin, P., L. Basuino, and H. F. Chambers. 2009. Subinhibitory fluoroquinolone exposure selects for reduced beta-lactam susceptibility in methicillin-resistant Staphylococcus aureus and alterations in the SOS-mediated response. Res. Microbiol. 160:187-192. [DOI] [PubMed] [Google Scholar]
- 891.Tejeda-Ramirez, E., M. Behani, and R. J. Leggiadro. 2009. Community-associated methicillin-resistant Staphylococcus aureus infection in an inner city hospital pediatric inpatient population. South. Med. J. 102:135-138. [DOI] [PubMed] [Google Scholar]
- 892.Tenover, F. C., and R. C. Moellering. 2007. The rationale for revising the Clinical and Laboratory Standards Institute vancomycin minimal inhibitory concentration interpretive criteria for Staphylococcus aureus. Clin. Infect. Dis. 44:1208-1215. [DOI] [PubMed] [Google Scholar]
- 893.Tenover, F. C., L. K. McDougal, G. V. Goering, G. Killgore, S. J. Projan, J. B. Patel, and P. M. Dunman. 2006. Characterization of a strain of community-associated methicillin-resistant Staphylococcus aureus widely disseminated in the United States. J. Clin. Microbiol. 44:108-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 894.Tenover, F. C., R. D. Arbeit, R. V. Goering, P. A. Mickelsen, B. E. Murray, D. H. Persing, and B. Swaminathan. 1995. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol. 33:2233-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 895.Tenover, F. C., S. McAllister, G. Fosheim, L. K. McDougal, R. B. Carey, B. Limbago, D. Lonsway, J. B. Patel, M. J. Kuehnert, and R. Gorwitz. 2008. Characterization of Staphylococcus aureus isolates from nasal cultures collected from individuals in the United States in 2001 to 2004. J. Clin. Microbiol. 46:2837-2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 896.Texas Department of State Health Services and Correctional Facilities Workgroup. 2006. Prevention, treatment and containment of methicillin-resistant Staphylococcus aureus infections. Texas Department of State Health Services, Austin, TX. http://www.dshs.state.tx.us/idcu/health/antibiotic_resistance/mrsa/prevention_treatment.pdf.
- 897.Thomas, J. C., J. Bridge, S. Waterman, J. Vogt, L. Kilman, and G. Hancock. 1989. Transmission and control of methicillin-resistant Staphylococcus aureus in a skilled nursing facility. Infect. Control Hosp. Epidemiol. 10:106-110. [DOI] [PubMed] [Google Scholar]
- 898.Thurman, A. R., T. M. Satterfield, and D. E. Soper. 2008. Methicillin-resistant Staphylococcus aureus as a common cause of vulvar abscesses. Obstet. Gynecol. 112:538-544. [DOI] [PubMed] [Google Scholar]
- 899.Tiemersma, E. W., S. L. A. M. Bronzwaer, O. Lyytikäinen, J. E. Degner, P. Schrijnemakers, N. Bruinsma, J. Monen, W. Witte, H. Grundmann, and European Antimicrobial Resistance Surveillance System Participants. 2004. Methicillin-resistant Staphylococcus aureus in Europe, 1999-2002. Emerg. Infect. Dis. 10:1627-1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 900.Tietz, A., R. Frei, and A. F. Widmer. 2005. Transatlantic spread of USA300 clone MRSA. N. Engl. J. Med. 353:532-533. [DOI] [PubMed] [Google Scholar]
- 901.Tinelli, M., A. Pantosti, C. Lusardi, M. Vimercati, and M. Monaco. 2007. First detected case of community-acquired methicillin-resistant Staphylococcus aureus skin and soft tissue infection in Italy. Euro Surveill. 12(15):pii=3173. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=3173. [DOI] [PubMed] [Google Scholar]
- 902.Tinelli, M., M. Monaco, M. Vimercati, A. Ceraminiello, and A. Pantosti. 2009. Methicillin-susceptible Staphylococcus aureus in skin and soft tissue infections, Northern Italy. Emerg. Infect. Dis. 15:250-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 903.Tokumoto, M. B., V. Ybarra, M. Torreno, M. Rodríguez, M. S. Ramírez, L. Jordá-Vargas, and D. Centrón. 2007. Emergence of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) paediatric clone among skin and soft tissue infections in Buenos Aires. Int. J. Antimicrob. Agents 30:469-474. [DOI] [PubMed] [Google Scholar]
- 904.Tolba, O., A. Loughrey, C. E. Goldsmith, B. C. Millar, P. J. Rooney, and J. E. Moore. 2007. Survival of epidemic strains of nosocomial and community-acquired methicillin-resistant Staphylococcus aureus on coins. Am. J. Infect. Control 35:342-346. [DOI] [PubMed] [Google Scholar]
- 905.Tong, S. Y. C., M. I. McDonald, D. C. Holt, and B. J. Currie. 2008. Global implications of the emergence of community-associated methicillin-resistant Staphylococcus aureus in indigenous populations. Clin. Infect. Dis. 46:1871-1878. [DOI] [PubMed] [Google Scholar]
- 906.Tong, S. Y. C., N. M. Anstey, G. D. Lum, R. A. Lilliebridge, D. P. Stephens, and B. J. Currie. 2008. Fatal community-associated methicillin-resistant Staphylococcus aureus pneumonia after influenza. Med. J. Aust. 188:61. [DOI] [PubMed] [Google Scholar]
- 907.Torell, E., D. Molin, E. Tano, C. Ehrenborg, and C. Ryden. 2005. Community-acquired pneumonia and bacteraemia in a healthy young woman caused by methicillin-resistant Staphylococcus aureus (MRSA) carrying the genes encoding Panton-Valentine leukocidin (PVL). Scand. J. Infect. Dis. 37:902-904. [DOI] [PubMed] [Google Scholar]
- 908.Torvaldsen, S., C. Roberts, and T. V. Riley. 1999. The continuing evolution of methicillin-resistant Staphylococcus aureus in Western Australia. Infect. Control Hosp. Epidemiol. 20:133-135. [DOI] [PubMed] [Google Scholar]
- 909.Tragiannidis, A., G. Tzouvelekis, M. Eboriadou, L. Fidani, E. Pavlou, T. Papageorgiou, and F. Athanassiadou. 2008. Septic pulmonary embolism due to Staphylococcus aureus. Pediatr. Int. 50:717. [DOI] [PubMed] [Google Scholar]
- 910.Trick, W. E., M. O. Vernon, R. A. Hayes, C. Nathan, T. W. Rice, B. J. Peterson, J. Segreti, S. F. Welbel, S. L. Solomon, and R. A. Weinstein. 2003. Impact of ring wearing on hand contamination and comparison of hand hygiene agents in a hospital. Clin. Infect. Dis. 36:1383-1390. [DOI] [PubMed] [Google Scholar]
- 911.Trihn, T. T., W. R. Short, and L. A. Mermel. 2009. Community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infection in HIV-infected patients. J. Int. Assoc. Physicians AIDS Care 8:176-180. [DOI] [PubMed] [Google Scholar]
- 912.Trinidade, P., R. L. Pacheco, S. F. Costa, F. Rossi, A. A. Barone, E. M. Mamizuka, and A. S. Levin. 2005. Prevalence of SCCmec type IV in nosocomial isolates of methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 43:3435-3437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 913.Tristan, A., M. Bes, H. Meugnier, G. Lina, B. Bozdogan, P. Courvalin, M. E. Reverdy, M. C. Enright, F. Vandenesch, and J. Etienne. 2007. Global distribution of Panton-Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus, 2006. Emerg. Infect. Dis. 13:594-600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 914.Troillet, N., Y. Carmeli, M. H. Samore, J. Dakos, K. Eichelberger, P. C. DeGirolami, and A. W. Karchmer. 1998. Carriage of methicillin-resistant Staphylococcus aureus at hospital admission. Infect. Control Hosp. Epidemiol. 19:181-185. [DOI] [PubMed] [Google Scholar]
- 915.Tsai, H. C., P. J. Chao, C. L. Sy, S. S. Lee, Y. S. Chen, S. R. Wann, and Y. C. Liu. 2008. Community-associated methicillin-resistant Staphylococcus aureus infective endocarditis with Panton-Valentine leukocidin gene in an injection drug user with HIV infection. Intern. Med. 47:1485-1489. [DOI] [PubMed] [Google Scholar]
- 916.Tseng, C. W., P. Kyme, J. Low, M. A. Rocha, R. Alsabeh, L. G. Miller, M. Otto, M. Arditis, B. A. Diep, V. Nizet, T. M. Doherty, D. O. Beenhouer, and G. Y. Liu. 2009. Staphylococcus aureus Panton-Valentine leucocidin contributes to inflammation and muscle tissue injury. PLoS One 4:e6387. doi: 10.01371/journal.pone.0006387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 917.Tseng, M. H., B. H. Wei, W. J. Lin, J. J. Lu, S. Y. Lee, S. R. Wang, S. J. Chen, and C. C. Wang. 2005. Fatal sepsis and necrotizing pneumonia in a child due to community-acquired methicillin-resistant Staphylococcus aureus: case report and literature review. Scand. J. Infect. Dis. 37:504-507. [DOI] [PubMed] [Google Scholar]
- 918.Turabelidze, G., M. Lin, B. Wolkoff, D. Dodson, S. Gladbach, and B. Zhu. 2006. Personal hygiene and methicillin-resistant Staphylococcus aureus. Emerg. Infect. Dis. 12:422-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 919.Turnidge, J. D., and J. M. Bell. 2000. Methicillin-resistant Staphylococcal [sic] aureus evolution in Australia over 35 years. Microb. Drug Resist. 6:223-229. [DOI] [PubMed] [Google Scholar]
- 920.Udo, E. E., F. G. O'Brien, N. Al-Sweih, B. Noronha, B. Matthew, and W. B. Grubb. 2008. Genetic lineages of community-associated methicillin-resistant Staphylococcus aureus in Kuwait hospitals. J. Clin. Microbiol. 46:3514-3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 921.Udo, E. E., J. W. Pearman, and W. B. Grubb. 1993. Genetic analysis of community isolates of methicillin-resistant Staphylococcus aureus in Western Australia. J. Hosp. Infect. 25:97-108. [DOI] [PubMed] [Google Scholar]
- 922.Uhlén, M., B. Guss, B. Nilsson, S. Gatenbeck, L. Philipson, and M. Lindberg. 1984. Complete sequence of the staphylococcal gene encoding protein A. J. Biol. Chem. 259:1695-1702. [PubMed] [Google Scholar]
- 923.Urth, T., J. Gitte, R. Skov, and H. C. Schonheyder. 2005. Spread of a methicillin-resistant Staphylococcus aureus ST80-IV clone in a Danish community. Infect. Control Hosp. Epidemiol. 26:144-149. [DOI] [PubMed] [Google Scholar]
- 924.Vaino, A., M. Kardén-Lilja, S. Ibrahem, A. M. Kerttula, S. Salmenlinna, A. Virolainen, and J. Vuopio-Varkila. 2008. Clonality of epidemic methicillin-resistant Staphylococcus aureus strains in Finland as defined by several molecular methods. Eur. J. Clin. Microbiol. Infect. Dis. 27:545-555. [DOI] [PubMed] [Google Scholar]
- 925.Valalumkal, J. V., H. Whittingham, O. Vanderkooi, T. E. Stewart, D. E. Low, M. Mulvey, and A. McGeer. 2007. Necrotizing pneumonia and septic shock: suspecting CA-MRSA in patients presenting to Canadian emergency departments. Can. J. Emerg. Med. 9:300-303. [DOI] [PubMed] [Google Scholar]
- 926.Valentini, P., G. Parisi, M. Monaco, F. Crea, T. Spanu, O. Ranno, M. Tronci, and A. Pantosti. 2008. An uncommon presentation for a severe invasive infection due to methicillin-resistant Staphylococcus aureus clone USA300 in Italy: a case report. Ann. Clin. Microbiol. Antimicrob. 7:11. doi: 10.1186/1476-0711-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 927.Van Bambeke, F. 2006. Glycopeptides and glycodepsipeptides in clinical development: a comparative review of their antibacterial spectrum, pharmacokinetics and clinical efficacy. Curr. Opin. Invest. Drugs 7:740-749. [PubMed] [Google Scholar]
- 928.van Belkum, A., D. C. Melles, J. K. Peeters, W. B. van Leeuwen, E. van Duijkeren, X. W. Huijsdens, E. Spalburg, A. J. de Neeling, and H. A. Verbrugh on behalf of the Dutch Working Party on Surveillance and Research of MRSA (SOM). 2008. Methicillin-resistant and -susceptible Staphylococcus aureus sequence type 398 in pigs and humans. Emerg. Infect. Dis. 14:479-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 929.van Belkum, A., H. G. N. Niesters, W. G. MacKay, and W. B. van Leeuwen. 2007. Quality control of direct molecular diagnostics for methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 45:2698-2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 930.van de Gissen, A. W., M. G. van Santen-Verheuvel, P. D. Hengeveld, T. Bosch, E. M. Broens, and C. B. E. M. Reusken. 2009. Occurrence of methicillin-resistant Staphylococcus aureus in rats living on pig farms. Prev. Vet. Med. 91:270-273. [DOI] [PubMed] [Google Scholar]
- 931.van den Broek, I. V. F., B. A. G. L. van Cleef, A. Haenen, E. M. Broens, P. J. van der Wolf, M. J. M. van den Broek, X. W. Huijsdens, J. A. J. W. Kluytmans, A. W. van de Giessen, and E. W. Tiemersma. 2009. Methicillin-resistant Staphylococcus aureus in people living and working in pig farms. Epidemiol. Infect. 137:700-708. [DOI] [PubMed] [Google Scholar]
- 932.Van den Eede, A., A. Martens, U. Lipinska, M. Struelens, A. Deplano, O. Denis, F. Haesebrouke, F. Gasthuys, and K. Hermans. 2009. High occurance of methicillin-resistant Staphylococcus aureus ST398 in equine nasal samples. Vet. Microbiol. 133:138-144. [DOI] [PubMed] [Google Scholar]
- 933.Vandenesch, F., T. Naimi, M. C. Enright, G. Lina, G. R. Nimmo, H. Heffernan, N. Liassine, M. Bes, T. Greenland, M. Reverdy, and J. Etienne. 2003. Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton-Valentine leukocidin genes: worldwide emergence. Emerg. Infect. Dis. 9:978-984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 934.van der Mee-Marquet, N., C. Epinette, J. Loyau, L. Arnault, A. S. Domelier, B. Losfelt, N. Girard, R. Quentin, and the Bloodstream Infection Study Group of the Relais d'Hygiène du Centre. 2007. Staphylococcus aureus strains isolated from bloodstream infections changed significantly in 2006. J. Clin. Microbiol. 45:851-857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 935.Van de Velde, H. 1894. Étude sur la mécanisme de la virulence du staphylocoque pyogène. Cellule 10:402-460. [Google Scholar]
- 936.van Duijkeren, E., A. T. A. Box, M. E. O. C. Heck, W. J. B. Wannet, and A. C. Fluit. 2004. Methicillin-resistant staphylococci isolated from animals. Vet. Microbiol. 103:91-97. [DOI] [PubMed] [Google Scholar]
- 937.van Duijkeren, E., M. D. Jansen, S. C. Flemming, H. de Neeling, J. A. Waganaar, A. H. W. Schoormans, A. van Nes, and A. C. Fluit. 2007. Methicillin-resistant Staphylococcus aureus in pigs with exudative epidermitis. Emerg. Infect. Dis. 13:1408-1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 938.van Duijkeren, E., M. J. H. M. Wolfhagen, M. E. O. C. Heck, and W. J. B. Wannet. 2005. Transmission of a Panton-Valentine leucocidin-positive, methicillin-resistant Staphylococcus aureus strain between humans and a dog. J. Clin. Microbiol. 43:6209-6211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 939.van Duijkeren, E., M. J. Wolfhagen, A. T. Box, M. E. Heck, W. J. Wannet, and A. C. Fluit. 2004. Human-to-dog transmission of methicillin-resistant Staphylococcus aureus. Emerg. Infect. Dis. 10:2235-2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 940.van Duijkeren, E., R. Ikawaty, R. J. Broekhuizen-Stins, M. D. Jansen, E. C. Spalburg, A. J. de Neeling, J. G. Allart, A. van Nes, J. A. Wagenaar, and A. C. Fluit. 2008. Transmission of methicillin-resistant Staphylococcus aureus strains between different kinds of pig farms. Vet. Microbiol. 126:383-389. [DOI] [PubMed] [Google Scholar]
- 941.van Hal, S. J. M., and J. J. Post. 2004. Community-acquired MRSA epiduritis in an Australian prison inmate. Med. J. Aust. 180:650-651. [DOI] [PubMed] [Google Scholar]
- 942.van Loo, I. H. M., B. M. W. Diederen, P. H. M. Savelkoul, J. H. C. Woudenberg, R. Roosendaal, A. van Belkum, N. Lemmens-den Toom, C. Verhulst, P. H. J. van Keulen, and J. A. J. W. Kluytmans. 2007. Methicillin-resistant Staphylococcus aureus in meat products, the Netherlands. Emerg. Infect. Dis. 13:1753-1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 943.van Loo, I., X. Huijsdens, E. Tiemersma, A. de Neeling, N. van de Sande-Bruinsma, D. Beaujean, A. Voss, and J. Kluytmans. 2007. Emergence of methicillin-resistant Staphylococcus aureus of animal origin in humans. Emerg. Infect. Dis. 12:1834-1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 944.van Rijen, M. M. L., M. Bonten, R. P. Wenzel, and J. A. J. W. Kluytmans. 2008. Intranasal mupirocin for the reduction of Staphylococcus aureus infections in surgical patients with nasal carriage: a systematic review. J. Antimicrob. Chemother. 61:254-261. [DOI] [PubMed] [Google Scholar]
- 945.van Rijen, M. M. L., P. H. van Keulen, and J. A. Kluytmans. 2008. Increase in a Dutch hospital of methicillin-resistant Staphylococcus aureus related to animal farming. Clin. Infect. Dis. 46:261-263. [DOI] [PubMed] [Google Scholar]
- 946.van Rijen, M. M. L., T. Bosch, M. E. O. C. Heck, and J. A. J. W. Kluytmans. 2009. Meticillin-resistant Staphylococcus aureus epidemiology and transmission in a Dutch hospital. J. Hosp. Infect. 36:81-95. [DOI] [PubMed] [Google Scholar]
- 947.Varshney, A. K., L. R. Martinez, S. M. Hamilton, A. E. Bryant, M. H. Levi, P. Gialanella, D. L. Stevens, and B. C. Fries. 2010. Augmented production of Panton-Valentine leukocidin toxin in methicillin-resistant and methicillin-susceptible Staphylococcus aureus is associated with worse outcome in a murine skin infection model. J. Infect. Dis. 201:92-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 948.Vazan, D. F., and S. R. Kodsi. 2008. Community-acquired methicillin-resistant Staphylococcus aureus orbital cellulitis in a non-immunocompromised child. J. AAPOS 12:205-206. [DOI] [PubMed] [Google Scholar]
- 949.Veeh, R. H., M. E. Shirtliff, J. R. Petik, J. A. Flood, C. C. David, J. L. Seymour, M. A. Hansmann, K. M. Kerr, M. E. Pasmore, and J. W. Costerton. 2003. Detection of Staphylococcus aureus biofilm on tamps and menses components. J. Infect. Dis. 188:519-530. [DOI] [PubMed] [Google Scholar]
- 950.Vélazquez-Guadarrama, N., G. Martinez-Aguilar, J. A. Galindo, G. Zuñiga, and A. Arbo-Sosa. 2009. Methicillin resistant S. aureus colonization in Mexican children attending day care centres. Clin. Invest. Med. 32:E57-E63. [DOI] [PubMed] [Google Scholar]
- 951.Vengust, M., M. E. Anderson, J. Rousseau, and J. S. Weese. 2006. Methicillin-resistant staphylococcal colonization in clinically normal dogs and horses in the community. Lett. Appl. Microbiol. 43:602-606. [DOI] [PubMed] [Google Scholar]
- 952.Vergison, A., O. Denis, A. Deplano, G. Casimir, G. Claeys, F. DeBaets, K. DeBoeck, N. Douat, H. Franckx, J. Gigi, M. Ieven, C. Knoop, P. Lebeque, F. Lebrun, A. Malfroot, F. Paucquay, D. Pierard, J. Van Eldere, and M. J. Struelens. 2007. National survey of molecular epidemiology of Staphylococcus aureus colonization in Belgian cystic fibrosis patients. J. Antimicrob. Chemother. 59:893-899. [DOI] [PubMed] [Google Scholar]
- 953.Vernon, M. O., M. K. Hayden, W. E. Trick, R. A. Hayes, D. W. Blom, and R. A. Weinstein. 2006. Chlorhexidine gluconate to cleanse patients in a medical intensive care unit. Arch. Intern. Med. 166:306-312. [DOI] [PubMed] [Google Scholar]
- 954.Vetter, R. S., B. B. Pagac, R. W. Reiland, D. T. Bolesh, and D. L. Swanson. 2006. Skin lesions in barracks: consider community-associated methicillin-resistant Staphylococcus aureus infection instead of spider bites. Mil. Med. 171:830-832. [DOI] [PubMed] [Google Scholar]
- 955.Viallon, A., O. Marjollet, P. Berthelot, A. Carricajo, S. Guyomarćh, R. Florianne, F. Zeni, and J. C. Bertrand. 2007. Risk factors associated with methicillin-resistant Staphylococcus aureus infection in patients admitted to the ED. Am. J. Emerg. Med. 25:880-886. [DOI] [PubMed] [Google Scholar]
- 956.Vignaroli, C., P. E. Varaldo, and A. Camporese. 2009. Methicillin-resistant Staphylococcus aureus USA400 clone, Italy. Emerg. Infect. Dis. 15:995-996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 957.Vitale, C. B., T. L. Gross, and J. S. Weese. 2006. Methicillin-resistant Staphylococcus aureus in cat and owner. Emerg. Infect. Dis. 12:1998-2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 958.Vlack, S., L. Cox, A. Y. Peleg, C. Canuto, C. Stewart, A. Conlon, A. Stephens, P. Giffard, F. Huygens, A. Mollinger, R. Vohra, and J. S. McCarthy. 2006. Carriage of methicillin-resistant Staphylococcus aureus in a Queensland indigenous community. Med. J. Aust. 184:556-559. [DOI] [PubMed] [Google Scholar]
- 959.von Eiff, C., K. Becker, K. Machka, H. Stammer, and G. Peters. 2001. Nasal carriage as a source of Staphylococcus aureus bacteremia. N. Engl. J. Med. 344:11-16. [DOI] [PubMed] [Google Scholar]
- 960.von Specht, M., N. Gardella, P. Tagliaferri, G. Gutkind, and M. Mollerach. 2006. Methicillin-resistant Staphylococcus aureus in community-acquired meningitis. Eur. J. Clin. Microbiol. Infect. Dis. 25:267-269. [DOI] [PubMed] [Google Scholar]
- 961.Voss, A., F. Loeffen, J. Bakker, C. Klaassen, and M. Wulf. 2005. Methicillin-resistant Staphylococcus aureus in pig farming. Emerg. Infect. Dis. 11:1965-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 962.Vourli, S., H. Vagiakou, G. Ganteris, M. Orfanidou, M. Polemis, A. Vatapoulos, and H. Malamou-Ladas. 2009. High rates of community-acquired, Panton-Valentine leukocidin (PVL) positive methicillin-resistant S. aureus infections in adult outpatients in Greece. Euro Surveill. 14(2):pii=19089. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19089. [DOI] [PubMed] [Google Scholar]
- 963.Voyich, J. M., M. Otto, B. Mathema, K. R. Braughton, A. R. Whitney, D. Welty, R. D. Long, D. W. Dorward, D. J. Gardner, G. Lina, B. N. Kreiswirth, and F. R. DeLeo. 2006. Is Panton-Valentine leukocidin the major virulence determinant in community associated methicillin-resistant Staphylococcus aureus disease? J. Infect. Dis. 194:1761-1770. [DOI] [PubMed] [Google Scholar]
- 964.Wade, J. J., N. Desai, and M. W. Casewell. 1991. Hygenic hand disinfection for the removal of epidemic vancomycin-resistant Enterococcus faecium and gentamicin-resistant Enterobacter cloacae. J. Hosp. Infect. 18:211-218. [DOI] [PubMed] [Google Scholar]
- 965.Wagenaar, J. A., H. Yue, J. Pritchard, M. Broekhuizen-Stins, X. Huijsdens, D. J. Mevius, T. Bosch, and E. Van Duijkeren. 2009. Unexpected sequence types in livestock associated methicillin-resistant Staphylococcus aureus (MRSA): MRSA ST9 and a single-locus variant of ST9 in pig farming in China. Vet. Microbiol. 139:405-409. [DOI] [PubMed] [Google Scholar]
- 966.Wagenvoort, J. H. T., E. I. G. B. De Brauwer, and M. L. H. Sijstermans. 2002. MRSA decontamination of paper-containing objects. J. Hosp. Infect. 51:74-77. [DOI] [PubMed] [Google Scholar]
- 967.Wagenvoort, J. H. T., E. I. G. B. De Brauwer, M. L. H. Sijstermans, and H. M. J. Toenbreker. 2005. Risk of re-introduction of methicillin-resistant Staphylococcus aureus into the hospital by intrafamilial spread from and to healthcare workers. J. Hosp. Infect. 59:67-68. [DOI] [PubMed] [Google Scholar]
- 968.Waller, A. 2005. The creation of a new monster: MRSA and MRSI—important emerging veterinary and zoonotic diseases. Vet. J. 169:315-316. [DOI] [PubMed] [Google Scholar]
- 969.Walther, B., L. H. Wieler, A. W. Friedrich, A. M. Hanssen, B. Kohn, L. Brunnberg, and A. Lübke-Becker. 2008. Methicillin-resistant Staphylococcus aureus (MRSA) isolated from small and exotic animals at a university hospital during routine microbiological examinations. Vet. Microbiol. 127:171-178. [DOI] [PubMed] [Google Scholar]
- 970.Walther, B., S. Monecke, C. Ruscher, A. W. Friedrich, R. Ehricht, P. Slickers, A. Soba, C. G. Wleklinski, L. H. Wieler, and A. Lübke-Becker. 2009. Comparative molecular analysis substantiates zoonotic potential of equine methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 47:704-710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 971.Wang, C. C., C. H. Chuang, and C. H. Chiu. 2005. Community-acquired disseminated methicillin-resistant Staphylococcus aureus infection: case report and clinical implications. Ann. Trop. Paediatr. 25:53-57. [DOI] [PubMed] [Google Scholar]
- 972.Wang, C., W. Lo, M. Chu, and L. K. Siu. 2004. Epidemiological typing of community-acquired methicillin-resistant Staphylococcus aureus isolates from children in Taiwan. Clin. Infect. Dis. 39:481-487. [DOI] [PubMed] [Google Scholar]
- 973.Wang, G., J. F. Hindler, K. W. Ward, and D. A. Bruckner. 2006. Increasing vancomycin MICs for Staphylococcus aureus clinical isolates from a university hospital during a 5-year period. J. Clin. Microbiol. 44:3883-3886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 974.Wang, J. J., J. T. Wang, S. Y. Chen, P. R. Hsueh, H. C. Kung, Y. C. Chen, and S. C. Chang. 2007. Adult methicillin-resistant Staphylococcus aureus bacteremia in Taiwan: clinical significance of non-multi-resistant antibiograms and Panton-Valentine leukocidin gene. Diagn. Microbiol. Infect. Dis. 59:365-371. [DOI] [PubMed] [Google Scholar]
- 975.Wang, J. L., S. Y. Chen, J. T. Wang, G. H. Wu, W. C. Chiang, P. R. Hsueh, Y. C. Chen, and S. C. Chang. 2008. Comparison of both clinical features and mortality risk associated with bacteremia due to community-acquired methicillin-resistant Staphylococcus aureus and methicillin-susceptible S. aureus. Clin. Infect. Dis. 46:799-806. [DOI] [PubMed] [Google Scholar]
- 976.Wang, J., S. Barth, M. Richardson, K. Corson, and J. Mader. 2003. An outbreak of methicillin-resistant Staphylococcus aureus cutaneous infection in a saturation diving facility. Undersea Hyperb. Med. 30:277-284. [PubMed] [Google Scholar]
- 977.Wang, J. T., C. H. Liao, C. T. Fang, W. C. Chie, M. S. Lai, T. L. Lauderdale, W. S. Lee, J. H. Huang, and S. C. Chang. 2009. Prevalence and risk factors for colonization by methicillin-resistant Staphylococcus aureus among Taiwanese adults in the community. J. Clin. Microbiol. 47:2957-2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 978.Wang, J. T., C. T. Fang, Y. C. Chen, C. L. Wu, M. L. Chen, and S. C. Chang. 2007. Staphylococcal cassette chromosome mec in MRSA, Taiwan. Emerg. Infect. Dis. 13:494-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 979.Wang, J. T., W. H. Sheng, J. L. Wang, D. Chen, M. L. Chen, Y. C. Chen, and S. C. Chang. 2008. Longitudinal analysis of chlorhexidine susceptibilities of nosocomial methicillin-resistant Staphylococcus aureus isolates at a teaching hospital in Taiwan. J. Antimicrob. Chemother. 62:514-517. [DOI] [PubMed] [Google Scholar]
- 980.Wang, R., K. R. Braughton, D. Kretschmer, T. L. Bach, S. Y. Queck, M. Li, A. D. Kennedy, D. W. Dorward, S. J. Klebanoff, A. Peschel, F. R. Deleo, and M. Otto. 2008. Identification of novel cytolytic peptides as key virulence determinants for community-associated MRSA. Nat. Med. 13:1510-1514. [DOI] [PubMed] [Google Scholar]
- 981.Ward, P. D., and W. H. Turner. 1980. Identification of staphylococcal Panton-Valentine leukocidin as a potent dermonecrotic toxin. Infect. Immun. 28:393-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 982.Wardenburg, J. B., A. M. Palazzolo-Balance, M. Otto, O. Schneewind, and F. R. DeLeo. 2008. Panton-Valentine leukocidin is not a virulence determinant in murine models of community-associated methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 198:1166-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 983.Wardenburg, J. B., T. Bae, M. Otto, F. R. DeLeo, and O. Schneewind. 2007. Poring over pores: α-hemolysin and Panton-Valentine leukocidin in Staphylococcus aureus pneumonia. Nat. Med. 13:1405-1406. [DOI] [PubMed] [Google Scholar]
- 984.Wargo, K. A., and E. H. Eliand. 2005. Appropriate antimicrobial therapy for community-acquired methicillin-resistant Staphylococcus aureus carrying the Panton-Valentine leukocidin genes. Clin. Infect. Dis. 40:1376-1378. [DOI] [PubMed] [Google Scholar]
- 985.Webster, J., and S. Osborne. 2006. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst. Rev. 2:CD004985. doi: 10.1002/14651858.CD004985.pub2. [DOI] [PubMed]
- 986.Weese, J. S., and J. Rousseau. 2005. Attempted eradication of methicillin-resistant Staphylococcus aureus colonization in horses on two farms. Equine Vet. J. 37:510-514. [DOI] [PubMed] [Google Scholar]
- 987.Weese, J. S., and S. L. Lefebvre. 2007. Risk factors for methicillin-resistant Staphylococcus aureus colonization in horses admitted to a veterinary teaching hospital. Can. Vet. J. 48:921-926. [PMC free article] [PubMed] [Google Scholar]
- 988.Weese, J. S., F. Caldwell, B. M. Wiley, B. N. Kreiswirth, A. McGeer, J. Rousseau, and D. E. Low. 2006. An outbreak of methicillin-resistant Staphylococcus aureus skin infections resulting from horse to human transmission in a veterinary hospital. Vet. Microbiol. 114:160-164. [DOI] [PubMed] [Google Scholar]
- 989.Weese, J. S., H. Dick, B. M. Willey, A. McGreer, B. N. Kreiswirth, B. Innis, and D. E. Low. 2006. Suspected transmission of methicillin-resistant Staphylococcus aureus between domestic pets and humans in veterinary clinics and in the household. Vet. Microbiol. 115:148-155. [DOI] [PubMed] [Google Scholar]
- 990.Weese, J. S., L. McCarthy, M. Mossop, H. Martin, and S. Lefebvre. 2007. Observation of practices at petting zoos and the potential impact on zoonotic disease transmission. Clin. Infect. Dis. 45:10-15. [DOI] [PubMed] [Google Scholar]
- 991.Weese, J. S., M. Archambault, B. M. Willey, H. Dick, P. Hearn, B. N. Kreiswirth, B. Said-Salim, A. McGreer, Y. Likhoshvay, J. F. Prescott, and D. E. Low. 2005. Methicillin-resistant Staphylococcus aureus in horses and horse personnel, 2000-2002. Emerg. Infect. Dis. 11:430-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 992.Welinder-Olsson, C., K. Florén-Johansson, L. Larsson, S. Öberg, L. Karlsson, and C. Åhrén. 2008. Infection with Panton-Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus t034. Emerg. Infect. Dis. 14:1271-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 993.Wells, R. D., and V. S. Bebarta. 2006. Primary iliopsoas abscess caused by community-acquired methicillin-resistant Staphylococcus aureus. Am. J. Emerg. Med. 24:897-898. [DOI] [PubMed] [Google Scholar]
- 994.Wenzel, R. P. 2004. The antibiotic pipeline—challenges, costs, values. N. Engl. J. Med. 351:523-526. [DOI] [PubMed] [Google Scholar]
- 995.Werbick, C., K. Becker, A. Mellmann, K. M. Juuti, C. von Eiff, G. Peters, P. I. Kuusela, A. W. Friedrich, and B. Sinha. 2007. Staphylococcal chromosomal cassette mec type I, spa type, and expression of Pls are determinants of reduced cellular invasiveness of methicillin-resistant Staphylococcus aureus isolates. J. Infect. Dis. 195:1678-1685. [DOI] [PubMed] [Google Scholar]
- 996.Whitener, C. J., S. Y. Park, F. A. Browne, L. J. Parent, K. Julian, B. Bozdogan, P. C. Appelbaum, J. Chaitram, L. M. Weigel, J. Jernigan, L. K. McDougal, F. C. Tenover, and S. K. Fridkin. 2004. Vancomycin-resistant Staphylococcus aureus in the absence of vancomycin exposure. Clin. Infect. Dis. 38:1049-1055. [DOI] [PubMed] [Google Scholar]
- 997.Whitman, T. J., R. K. Herlihy, C. D. Schlett, P. R. Murray, G. A. Grandits, A. Ganesan, M. Brown, J. Mancuso, W. B. Adams, and D. R. Tribble. 2008. Chlorhexidine impregnated cloths to prevent skin and soft tissue infections in Marine officer candidates: a cluster-randomized, double-blind, controlled trial, abstr. L-774. Abstr. 48th Annu. Intersci. Conf. Antimicrob. Agents Chemother. (ICAAC)-Infect. Dis. Soc. Am. (IDSA) 46th Annu. Meet. American Society for Microbiology and Infectious Diseases Society of America, Washington, DC.
- 998.Wibbenmeyer, L. A., G. P. Kealey, B. A. Latenser, D. J. Diekman, I. M. Williams, S. L. Coffman, P. L. Winokur, J. S. Kroeger, R. W. Lewis, and L. A. Herwaldt. 2008. Emergence of the USA300 strain of methicillin-resistant Staphylococcus aureus in a burn-trauma unit. J. Burn Care Res. 29:790-797. [DOI] [PubMed] [Google Scholar]
- 999.Wielders, C. L. C., A. C. Fluit, S. Brisse, J. Verhoef, and F. J. Schmitz. 2002. mecA gene is widely distributed in Staphylococcus aureus population. J. Clin. Microbiol. 40:3970-3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1000.Wiersma, P., M. T. D'Angelo, W. R. Daley, J. Tuttle, K. E. Arnold, S. M. Ray, J. L. Ladson, S. N. Bulens, and C. L. Drenzek. 2009. Surveillance for severe community-associated methicillin-resistant Staphylococcus aureus infection. Epidemiol. Infect. 137:1674-1678. [DOI] [PubMed] [Google Scholar]
- 1001.Wijaya, L., L. Y. Hsu, and A. Kurup. 2006. Community-associated methicillin-resistant Staphylococcus aureus: overview and local situation. Ann. Acad. Med. Singapore 35:479-486. [PubMed] [Google Scholar]
- 1002.Williams, R. E. O. 1963. Healthy carriage of Staphylococcus aureus: its prevalence and importance. Bacteriol. Rev. 27:56-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1003.Wilson-Clay, B. 2008. Case report of methicillin-resistant Staphylococcus aureus (MRSA) mastitis with abscess formation in a breastfeeding woman. J. Hum. Lact. 24:326-329. [DOI] [PubMed] [Google Scholar]
- 1004.Wisplinghoff, H., A. E. Rosato, M. C. Enright, M. Noto, W. Craig, and G. L. Archer. 2003. Related clones containing SCCmec type IV predominate among clinically significant Staphylococcus epidermidis isolates. Antimicrob. Agents Chemother. 47:3574-3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1005.Witte, W., B. Strommenger, C. Cuny, D. Heuck, and U. Nuebel. 2007. Methicillin-resistant Staphylococcus aureus containing the Panton-Valentine leukocidin gene in Germany in 2005 and 2006. J. Antimicrob. Chermother. 60:1258-1263. [DOI] [PubMed] [Google Scholar]
- 1006.Witte, W., B. Strommenger, C. Stanek, and C. Cuny. 2007. Methicillin-resistant Staphylococcus aureus ST398 in humans and animals, central Europe. Emerg. Infect. Dis. 13:255-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1007.Wolter, D. J., F. C. Tenover, and R. V. Goering. 2007. Allelic variation in genes encoding Panton-Valentine leukocidin from community-associated methicillin-resistant Staphylococcus aureus. Clin. Microbiol. Infect. 13:827-830. [DOI] [PubMed] [Google Scholar]
- 1008.Wootton, S. H., K. Arnold, H. A. Hill, S. McAllister, M. Ray, M. Kellum, M. LaMarre, M. E. Lane, J. Chaitram, S. Lance-Parker, and M. J. Kuehnert. 2004. Intervention to reduce the incidence of methicillin-resistant Staphylococcus aureus skin infections in a correctional facility in Georgia. Infect. Control Hosp. Epidemiol. 25:402-407. [DOI] [PubMed] [Google Scholar]
- 1009.Wright, C. T., R. M. S. Stocks, D. L. Armstrong, S. R. Arnold, and H. J. Gould. 2008. Pediatric mediastinitis as a complication of methicillin-resistant Staphylococcus aureus retropharyngeal abscess. Arch. Otolaryngol. Head Neck Surg. 134:408-413. [DOI] [PubMed] [Google Scholar]
- 1010.Wright, M. O., J. P. Furuno, R. A. Venezia, J. K. Johnson, H. C. Standiford, J. N. Hebden, J. Hill, D. M. Hartley, A. D. Harris, and E. N. Perenevich. 2007. Methicillin-resistant Staphylococcus aureus infection and colonization among hospitalized prisoners. Infect. Control Hosp. Epidemiol. 28:877-879. [DOI] [PubMed] [Google Scholar]
- 1011.Wu, C. T., J. J. Lin, and S. H. Hsia. 2008. Cutaneous pustular manifestations associated with disseminated septic embolism due to Panton-Valentine leukocidin-producing strain of community-acquired methicillin-resistant Staphylococcus aureus. Int. J. Dermatol. 47:942-943. [DOI] [PubMed] [Google Scholar]
- 1012.Wu, K. C., H. H. Chiu, J. H. Wang, N. S. Lee, H. C. Lin, C. C. Hsieh, F. J. Tsai, C. T. Peng, and Y. C. Tseng. 2002. Characteristics of community-acquired methicillin-resistant Staphylococcus aureus in infants and children without known risk factors. J. Microbiol. Immunol. Infect. 35:53-56. [PubMed] [Google Scholar]
- 1013.Wulf, M., and A. Voss. 2008. MRSA in livestock animals—an epidemic waiting to happen? Clin. Microbiol. Infect. 14:519-521. [DOI] [PubMed] [Google Scholar]
- 1014.Wulf, M., A. van Nes, A. Eikelenboom-Boskamp, J. de Vries, W. Melchers, C. Klaasen, and A. Voss. 2006. Methicillin-resistant Staphylococcus aureus in veterinary doctors and students, the Netherlands. Emerg. Infect. Dis. 12:1939-1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1015.Wulf, M. W. H., E. Tiemersma, J. Kluytmans, B. Bogaers, A. C. A. P. Leenders, M. W. H. Jansen, J. Berkhout, E. Ruijters, D. Haverkate, M. Isken, and A. Voss. 2008. MRSA carriage in healthcare personnel in contact with farm animals. J. Hosp. Infect. 70:186-190. [DOI] [PubMed] [Google Scholar]
- 1016.Wulf, M. W. H., M. Sørum, A. van Nes, R. Skov, W. J. G. Melchers, C. H. W. Klaasen, and A. Voss. 2008. Prevalence of methicillin resistant Staphylococcus aureus among veterinarians: an international study. Clin. Microbiol. Infect. 14:29-34. [DOI] [PubMed] [Google Scholar]
- 1017.Wylie, J. L., and D. L. Nowicki. 2005. Molecular epidemiology of community- and health care-associated methicillin-resistant Staphylococcus aureus in Manitoba, Canada. J. Clin. Microbiol. 43:2830-2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1018.Yang, E. S., J. Tan, S. Eells, G. Rieg, G. Tagudar, and L. G. Miller. 18 August 2009. Body site colonization in patients with community-associated methicillin-resistant Staphylococcus aureus and other types of S. aureus skin infections. Clin. Microbiol. Infect. doi: 10.1111/j.1469-0691.2009.02836.x.x. [DOI] [PubMed]
- 1019.Yee-Guardino, S., D. Kumar, N. Abughali, M. Tuohy, G. S. Hall, and M. L. Kumar. 2008. Recognition and treatment of neonatal community-associated MRSA pneumonia and bacteremia. Pediatr. Pulmonol. 43:203-205. [DOI] [PubMed] [Google Scholar]
- 1020.Young, D. M., H. W. Harris, E. D. Charlebois, H. Chambers, A. Campbell, F. Perdreau-Remington, C. Lee, M. Mankani, R. Mackersie, and W. P. Schecter. 2004. An epidemic of methicillin-resistant Staphylococcus aureus soft tissue infections among medically underserved patients. Arch. Surg. 139:947-953. [DOI] [PubMed] [Google Scholar]
- 1021.Young, L. M., and C. S. Price. 2008. Community-associated methicillin-resistant Staphylococcus aureus emerging as important cause of necrotizing fasciitis. Surg. Infect. 9:469-474. [DOI] [PubMed] [Google Scholar]
- 1022.Yu, F., Z. Chen, C. Liu, X. Zhang, X. Lin, S. Chi, T. Zhou, Z. Chen, and X. Chen. 2007. Prevalence of Staphylococcus aureus carrying Panton-Valentine leukocidin genes among isolates from hospitalized patients in China. Clin. Microbiol. Infect. 14:381-384. [DOI] [PubMed] [Google Scholar]
- 1023.Zaoutis, T. E., P. Toltzos, J. Chu, T. Abrams, M. Dul, J. Kim, K. L. McGowan, and S. E. Coffin. 2006. Clinical and molecular epidemiology of community-acquired methicillin-resistant Staphylococcus aureus infections among children with risk factors for health care-associated infection. Pediatr. Infect. Dis. J. 25:343-348. [DOI] [PubMed] [Google Scholar]
- 1024.Zemlicková, H., M. Fridrichová, K. Tyllová, V. Jakubu, and I. Machová. 2009. Carriage of methicillin-resistant Staphylococcus aureus in veterinary personnel. Epidemiol. Infect. 137:1233-1236. [DOI] [PubMed] [Google Scholar]
- 1025.Zhanel, G. G., G. Sniezek, F. Schweizer, S. Zelenitsky, P. R. Lagacé-Wiens, E. Rubinstein, A. S. Gin, D. J. Hoban, and J. A. Karlowsky. 2009. Ceftaroline: a novel broad-spectrum cephalosporin with activity against meticillin-resistant Staphylococcus aureus. Drugs 69:809-831. [DOI] [PubMed] [Google Scholar]
- 1026.Zhanel, G. G., M. DeCorby, K. A. Nichol, P. J. Baudry, J. A. Karlowsky, P. R. S. Lagace-Wiens, M. McCracken, M. R. Mulvey, D. J. Hoban, and the Canadian Antimicrobial Resistance Alliance. 2008. Characterization of methicillin-resistant Staphylococcus aureus, vancomycin-resistant enterococci and extended-spectrum beta-lactamase-producing Escherichia coli in intensive care units in Canada: results of the Canadian National Intensive Care Unit (CA-ICU) study (2005-2006). Can. J. Infect. Dis. Med. Microbiol. 19:243-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1027.Zhang, K., J. A. McClure, S. Elsayed, J. Tan, and J. M. Conly. 2008. Coexistence of Panton-Valentine leukocidin positive and negative community-associated MRSA USA400 sibling strain in a large Canadian health-care region. J. Infect. Dis. 197:195-204. [DOI] [PubMed] [Google Scholar]
- 1028.Zhang, W., X. Shen, H. Zhang, C. Wang, Q. Deng, L. Liu, and Y. Yang. 2009. Molecular epidemiological analysis of methicillin-resistant Staphylococcus aureus isolates from Chinese pediatric patients. Eur. J. Clin. Microbiol. Infect. Dis. 28:861-864. [DOI] [PubMed] [Google Scholar]
- 1029.Zinderman, C. E. 2004. Community-acquired methicillin-resistant Staphylococcus aureus among military recruits. Emerg. Infect. Dis. 10:941-944. [DOI] [PMC free article] [PubMed] [Google Scholar]