Abstract
Purpose: Guided by an explanatory matrix of family conflict at the end of life, the purpose of this article was to examine the correlates and predictors of family conflict reported by 155 spouses and adult children of persons with lung cancer. Design and Methods: A cross-sectional statewide survey of family members of persons who died from lung cancer was conducted as part of the larger study on the Assessment of Cancer CarE and SatiSfaction in Wisconsin. Results: Significant bivariate correlations were found between family conflict and family context variables (i.e., a history of conflict, younger respondent age, race, and specified end-of-life care wishes of the patient), conditions (i.e., greater physical and psychological clinical care needs of the patient), and contributing factors (i.e., communication constraints and family asserting control). In the multivariate model, significant predictors of family conflict included prior family conflict, race, communication constraints, and family members asserting control; the model explained 72% of the variance in conflict. Implications: Implications for routine assessment and screening to identify families at risk and recommendations for the development and testing of interventions to facilitate shared decision making and enhance open communication among at-risk families are highlighted.
Keywords: Palliative care, Family functioning, Family caregivers
Lung cancer is the leading cause of cancer mortality for both men and women in the United States (American Cancer Society, 2008), and nearly 70% of persons diagnosed with this disease are 65 years or older (Stöppler & Marks, 2008). Individuals with lung cancer are diagnosed later and die earlier than persons with other forms of cancer creating distinctive strains and decision-making challenges for patients and their families (Pearman, 2008). Families play an important role in diagnosis and treatment decision making and face many challenges in caring for patients with lung cancer; the symptoms associated with the disease and its treatments are especially difficult to endure and witness.
Given the pervasive difficulties associated with the poor lung cancer prognosis after a diagnosis and the high comorbidity of later life chronic conditions (Juan, Albert, Campos, Caranyana, & Alberola, 2007), the demands on families are many and the potential for conflict is high (Badr & Taylor, 2006). Family members report high stress (Cameron, Franche, Cheung, & Stewart, 2002), and as many as two thirds report family disagreements regarding treatment decisions, discontinuation of treatment, and use of hospice care (Zhang & Siminoff, 2003a, 2003b). National research agendas call for increased attention to understanding the experiences and difficulties that arise for family members at the end of life (Kramer, Christ, Bern-Klug, & Francoeur, 2005; National Institutes of Health State-of-the-Science Conference Statement, 2004). Understanding what contributes to family conflict at the end of life is vital to identifying families at risk and to planning services and interventions to support these families.
The purpose of this article was to examine the correlates and predictors of family conflict at the end of life reported by spouses and adult children of persons recently deceased from lung cancer.
Definition and Conceptual Framework
We define family conflict as “interpersonal tension or struggle among two or more persons whose opinions, values, needs, or expectations are opposing or incompatible” (Kramer, Boelk, & Auer, 2006, p. 794). Consistent with other definitions of family conflict as “recurrent, stressful differences and disagreements” (Davis, 1997, p. 85), “overt interpersonal disagreement” (Semple, 1992, p. 649), and a “strong feeling of resentment toward a relative” (Strawbridge & Wallhagen, 1991, p. 772), interpersonal tension or struggle experienced by families in conflict may be exemplified in overt behaviors, such as arguments, disagreements, name calling or yelling, and/or covert feelings of resentment or anger among family members.
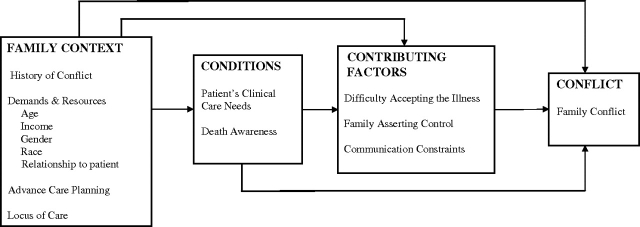
The conceptual framework for this study was based on an explanatory matrix of family conflict generated from a qualitative investigation (Kramer et al., 2006). According to this model, three primary domains explain the variability found in family conflict. These include the “family context,” “conditions” that shape interactions or actions, and “contributing factors.” Figure 1 outlines the components of the model.
Figure 1.
Explanatory matrix of family conflict at the end of life.
Family Context
Conflict derives meaning within the context of the family environment (Kramer et al., 2006). Families caring for patients with lung cancer come to that experience in the context of their prior relationships, their distinctive resources and demands, and they vary in terms of how they have approached advanced care planning. Qualitative research suggests that a history of unresolved conflict is likely to stimulate conflict at the end of life (Kramer et al.), and other evidence suggests that adult children report more family conflict than spouses (Clark, Shields, Aycock, & Wolf, 2003; Kissane, Bloch, Burns, McKenzie, & Posterino, 1994; Peisah, Brodaty, & Quadrio, 2006; Semple, 1992). Limited empirical attention has been given to documenting other contextual and demographic variables that are correlated with family conflict at the end of life, yet such information might help to identify families that are at greatest risk. Particular contextual variables such as respondent income, education, locus of care, race–ethnicity, age, and gender are of interest as potential indicators of the resources available to families and the demands family members face across the end-of-life continuum in which family conflict may arise (Kramer et al.). Results from the National Comorbidity Survey revealed higher rates of family conflict and violence among younger, less educated, poorer female respondents and lower rates among non-Hispanic Whites compared with African American and Hispanic respondents (Kessler, Molnar, Feurer, & Appelbaum, 2001). We are interested in determining the extent to which resources such as socioeconomic status (i.e., education and income), and access to hospice care that is patient and family centered (National Consensus Project for Quality Palliative Care, 2009), will be associated with less conflict and other sociodemographic variables such as race–ethnicity, age, and gender that have been correlated with conflict in the general population (Kessler et al.) are associated with more conflict at the end of life.
Difficult decisions about stopping or prolonging treatment falls upon family members who may disagree among themselves about appropriate care (Kramer et al., 2006). Advance care planning typically comprises three behaviors—completing a living will, appointing a durable power of attorney for health care (DPAHC), and holding discussions with others about one’s treatment preferences (Carr & Khodyakov, 2007). Advance care planning may reduce conflict arising from uncertainties regarding the patient’s wishes. One study investigating the impact of life-sustaining treatment decisions on families suggested that stress among relatives can be reduced when patients formulate an advance care plan (Tilden, Tolle, Garland, & Nelson, 1995).
Conditions
Conditions “are dimensions of a phenomenon that facilitate, block or in some way shape actions and/or interactions” (Kools, McCarthy, Durham, & Robrecht, 1996, p. 318). The primary conditions identified in prior qualitative research that underlie the processes of family conflict at the end of life include the patient’s clinical care needs arising from their declining health status (i.e., the illness) and an awareness of approaching death. In the context of a lung cancer diagnosis, distressing symptoms commonly include pain, shortness of breath, nausea or vomiting, fatigue, depression, and/or anxiety. Death awareness is curtailed when patient–physician communication is inadequate and when cancer is actively and aggressively treated (Valdimarsdóttir et al., 2007), which is the usual treatment of choice for lung cancer (American Cancer Society, 2008). A study of doctor–lung cancer patient communication found that physicians often failed to recognize patients’ misconceptions about the intent of treatment and prognosis, and most patients overestimated their probability of a cure (Quirt et al., 1997). According to the explanatory matrix, family members of patients with more distressing symptoms and who have been informed that the patient may die from lung cancer will likely experience greater difficulty accepting the illness, attempts at asserting control in the decision-making process, communication constraints, and ultimately higher family conflict.
Contributing Factors
Contributing factors are the “intended or unintended actions or interactions … impelled by … conditions” (Kools et al., 1996, p. 318) that contribute to family conflict. Primary contributing factors of conflict identified in the previous qualitative investigation included family member’s death anxiety or difficulty accepting the illness, family members “asserting control,” and communication constraints (Kramer et al., 2006). Death anxiety or the emotional difficulty of accepting the illness prompted family members to behave in insensitive ways that would stimulate conflict; for example, insisting or demanding that aggressive treatments be implemented regardless of what the patient or other family members desired (Kramer et al.). Emotionally accepting a progressive downward course of illness was reported as one of the most difficult tasks facing family caregivers of cancer patients (Chan & Chang, 1999). Family members asserted control and escalated family conflict by engaging in actions or enacting decisions that thwarted the needs or wishes of others, such as the example of a son of an older male patient, who used his medical degree to change the medications of his father, without consulting the patient’s wife or physician (Kramer et al.). We know from friendship studies that when an individual asserts control without considering the wishes of others, that conflict in the friendship is a natural outcome (Updegraff et al., 2004). Other evidence supports our prior findings documenting a relationship between family conflict and ineffective communication among family caregivers (Clark et al., 2003). Communication constraints often arise out of “genuine caring and desire to protect other family members” (Kramer et al., p. 797), from “avoidance of psychological distress,” and belief in “positive thinking” (Zhang & Siminoff, 2003a, p. 415). Communication constraints are commonly reported among families of patients with cancer (Chekryn, 1984; Cooper, 1984; Hilton, 1994) and may contribute to the development of conflict because it inhibits uniform understanding of health status, conditions and needs, prevents expression of genuine feelings, and diminishes opportunities to diffuse misunderstandings (Kramer et al.).
This study focused on the following primary research question: To what extent is family conflict at the end of life among family members of persons with lung cancer a function of the family context, conditions and contributing factors? This study will test the following research hypotheses, which were generated from the review of the literature and the conceptual framework described earlier.
Hypothesis 1: The “family context” will be associated with family conflict. More specifically, conflict at the end of life will be higher among families with a prior history of conflict, without advance care planning, and younger, female, African American and adult child respondents and will be lower among families with greater socioeconomic resources (i.e., higher income and education) and those who received hospice care.
Hypothesis 2: Patient clinical care needs and death awareness will be positively associated with “contributing factors” and “family conflict.”
Hypothesis 3: After controlling for the family context (i.e., history of family conflict, demands and resources, and advance care planning) and “conditions” (i.e., patients clinical care needs and death awareness), contributing factors will significantly predict family conflict.
Methods
Assessment of Cancer CarE and SatiSfaction Study
The results reported here are drawn from a larger study on the Assessment of Cancer CarE and SatiSfaction (ACCESS) in the state of Wisconsin in which persons diagnosed with four types of invasive cancer (breast, prostate, colorectal, and lung cancers), reported to the statewide tumor registry in 2004, were invited to complete a survey. Using the Wisconsin Comprehensive Cancer Control Plan (2005–2010) as a guide, the ACCESS planning committee designed the study to address barriers to care, patient satisfaction, and quality of life/symptom management among Wisconsin cancer patients. As will be described subsequently, because the prognosis for many lung cancer patients is poor, an ancillary study of family members was conducted that provides the basis for the analysis reported here.
Case Identification and Data Collection.—
Wisconsin residents newly diagnosed between July and December 2004 with lung cancer aged 18–79 years and reported to the Wisconsin Cancer Reporting System (WCRS) were eligible for the ACCESS study. Established in 1976, the WCRS collects cancer incidence data on Wisconsin residents as mandated by chapter 255.04, Wisconsin Statutes. In addition, cases were required to have a publicly available telephone number. A total of 1185 lung cancer cases were randomly selected from the WCRS database to determine eligibility into the ACCESS study. This database included a random sample of non-Hispanic Whites and, to increase minority representation, all non-White and/or Hispanic lung cancer cases. After merging the 1185 cases with the National Death Index, 795 (67%) were found to be deceased and 488 of the deceased cases (61%) had a publically available telephone number.
Of the 488 eligible deceased lung cancer patients, 358 family members with contact information were identified, representing 73%. The family member who was most involved in the care of the patient was invited to participate in this ancillary study of family members. Two hundred and five (57%) agreed to receive the study questionnaire and 169 returned surveys (82% of those who received the survey; 47% of total contacted). One hundred and fifty-eight (93%) respondents were spouses (n = 141) or adult children (n = 17). The analytic sample is confined to 155 of these respondents who had sufficient data on family conflict.
An introductory letter was mailed to the lung cancer patients between July 2006 and November 2007 to alert the households that they would be receiving a telephone call from an ACCESS study staff person. These letters were sent on average 26.4 months after the patient’s cancer diagnosis. Calls were made within 2 weeks of these mailings to verify lung cancer vital status and ask permission to send a study questionnaire. For deceased lung cancer patients, persons in the household were asked to identify the next of kin who had been most involved in the care of the patient and to provide contact information (i.e., name and address) for that individual. Mailed packets were then sent to the family member, which included a cover letter, the survey, a study participant information sheet, and a small incentive (i.e., U.S. postage stamp book; value: $7.80). Mailings and follow-up protocols for nonrespondents (i.e., postcard reminder at 1 week, full packet at 3 weeks, and telephone calls at 5 weeks) followed Dillman’s (1978) total design method. The time between death and completion of the surveys averaged 19 months (SD = 7.37) and ranged from 0.9 to 34 months.
Measures
Dependent Variable: Family Conflict.—
Scales have been developed to measure conflict in contexts of caregiving families for persons with Alzheimer’s disease (Semple, 1992) and stroke (Clark et al., 2003), interparental conflict (Kline, Wood, & Moore, 2003), conflict in Asian American Families (Lee, Choe, Kim, & Ngo, 2000), and general conflict in the family environment (Moos & Moos, 1994). Measures of family conflict salient to the end-of-life context have not been developed and tested. A brief four item “Family Conflict at the End-of Life” (FC-EOL) scale was developed for this study based on findings from a prior qualitative study (see Kramer et al., 2006), a literature review, and prior clinical experience. Consistent with our definition of family conflict, respondents were asked to use a 5-point scale (1 = not at all to 5 = very much) to answer the following four questions anchored in the end-of-life experience: “As you think about the decisions that your family member and the rest of the family faced near the end of life, how much did any family members: Disagree or argue with one another? Feel resentment toward one another? Feel anger toward one another? Insult or yell at one another?” A mean score for family conflict was calculated. Cronbach’s α for the FC-EOL scale was .93; item to total correlations ranged from .72 to .88. A square-root transformation of the family conflict scale was necessary to correct for positive skewness and kurtosis (Tabachnick & Fidell, 2000). Results will be reported using the transformed variable.
Family Context.—
Four domains of the family context were measured. We assessed “History of family conflict” prior to illness with a two-item scale developed by the first author (Kramer) to assess family disagreements and tensions. Respondents were asked “Prior to [the decedent’s] illness, how much did any of your family members: ‘have serious arguments with one another;’ and ‘insult or yell at one another’?” Response categories range from 0 = not at all to 4 = very much. Cronbach’s α was .94. “Respondent characteristics” included sociodemographic variables such as age (continuous variable that was dichotomized; 0 = younger than 65 years; 1 = 65 years or older), race (0 = non-Hispanic White; 1 = African American), education (three categories that include high school or less, some college, and college or advanced degree), income (four income categories included less than $15,000, $15,000–$29,999, $30,000–$49,999, and $50,000+), and relationship to the deceased (0 = adult child; 1 = spouse). “Advanced care planning” was ascertained by the presence of a DPAHC and living will, and respondents were asked “Did your family member have specific wishes or plans about the types of medical treatment he/she wanted while dying?” (0 = no; 1 = yes). In addition, “locus of care” was asked with two questions: “Was your family member hospitalized during his/her last month of life?” and “Was hospice involved in the medical care of your family member?” (0 = no; 1 = yes).
Conditions: Patients Clinical Care Needs.—
An index of four common “physical symptoms” associated with lung cancer was assessed by asking: “Did your family member have a) pain; b) shortness of breath; c) nausea or vomiting; or d) severe tiredness or fatigue during or after any of his/her cancer treatments?” Cronbach’s α was .66. A “psychological symptoms” index was assessed by asking “Did your family member experience a) loss of hope or depression; and/or b) anxiety during or after any of his/her cancer treatments?” Cronbach’s α was .57. “Death awareness” was assessed with a single item: “Did you or your family member ever talk to a doctor about the chance that he/she would die from lung cancer?” (0 = no; 1 = yes).
Contributing Factors.—
Contributing factors were assessed by the following three single-item indicators. “Difficulty accepting the illness”: “How much did any family members find it hard to accept the illness?” “Family asserting control”: “How much did family members make decisions about care that others did not want?” “Communication constraints”: “How much did any family members have trouble talking with one another?” For all items, respondents used a 5-point continuum to indicate the degree to which the contributing factor was present at the end of life (0 = not at all to 4 = very much).
Missing Data
There were several strategies used for handling missing data. Person mean substitution (Downey & King, 1998) was used for the two conflict study scales in which 50% or more of the data were available. This method has been found to be the optimal technique for imputing missing data when half of the items are present (Hawthorne & Elliott, 2005). This applied to one respondent on history of conflict and one respondent for family conflict at the end of life who answered 75% of the scale responses. Several missing data strategies were examined for contextual variables with similar results. Two respondents missing age data were spouses whose partners had Medicare; these women were place into the 65 years and older category. Because all respondents with children in the home were younger than 65 years, the third missing respondent with children in the home was placed into the younger than 65 years age category. Two respondents missing race data who indicated that they were non-Hispanic/Latino(a) were placed into the non-Hispanic/Latino(a) White category. A similar process was followed for education, advance care planning, and death awareness in which the few missing cases were placed into modal categories. For each of these variables that had missing data, we additionally created dummy variables for missing cases. Bivariate and multivariate analyses examining the relationship between the reduced categorical variables versus the created dummy variables with family conflict, as well as analysis using a listwise deletion approach in which no more than 3% of the analytic subsample was missing on any one of the measures, all lead to the same results. Given the small sample size, we report results for the reduced categorical variables. Imputations were not made for income or locus of care variables.
Results
Presence of Family Conflict
Thirty-five percent of families reported some type of family conflict. Twenty-nine percent reported that there were disagreements or arguments among family members at the end of life, 22% reported resentments among family members, 19% reported family members felt anger toward one another, and 12% reported that family members insulted or yelled at one another. Overall, levels of family conflict were relatively low in this sample as evidenced by the positively skewed mean score of 0.38 (SD = 0.76; range = 0–4). The square-root transformed family conflict scale used for the analysis ranged from 0–2, with the mean of 0.33 (SD = 0.52).
Sample Description and Family Conflict: Hypothesis 1
Sample characteristics and family conflict means for family context categorical variables are described in Table 1. The majority of respondents were female, of European ancestry, and spouses, with less than a college education. The sample fell fairly evenly into the younger than and older than 65 years age groupings; however, the mean age was 63 years for family members and 66 years for patients (SD = 8.82; range = 43–80), indicating that this was primarily an older sample. Most patients had engaged in advanced care planning in the form of completing a DPAHC and a living will (86% and 81%, respectively), but only 40% had expressed specific wishes for end-of-life care. More than half of the patients had been hospitalized prior to death, and the majority (68%) received hospice care.
Table 1.
Sample Characteristics and Family Conflict Means for Family Context Categorical Variables (N = 155)
| Family conflicta | ||
| M (SD) | M (SD) | |
| History of conflict | 0.38 (0.73) | |
| Age, years | 63 (12) | |
| N (%) | ||
| Less than 65 (b=1) | 76 (49.0) | 0.46 (0.56)* |
| 65+ (b=2) | 79 (51.0) | 0.20 (0.44) |
| Income, $ | ||
| Less than 15,000 | 18 (12.5) | 0.43 (0.58) |
| 15,000–29,999 | 33 (23.1) | 0.20 (0.46) |
| 30,000–49,999 | 56 (39.2) | 0.37 (0.51) |
| 50,000+ | 36 (25.2) | 0.42 (0.58) |
| Gender | ||
| Male | 32 (20.6) | 0.32 (0.51) |
| Female | 123 (79.4) | 0.37 (0.55) |
| Race | ||
| Non-Hispanic White (b=2) | 150 (96.8) | 0.32 (0.51)* |
| African American | 5 (3.2) | 0.77 (0.56) |
| Relationship to patient | ||
| Spouse | 139 (89.7) | 0.31 (0.31)† |
| Adult child | 16 (10.3) | 0.53 (0.56) |
| Education | ||
| High school grad or less (b=3) | 97 (62.6) | 0.29 (0.50) |
| Some college | 38 (24.5) | 0.41 (0.53) |
| College or advanced degree | 20 (12.9) | 0.36 (0.59) |
| Advanced care planning | ||
| Pt. had DPAHC | ||
| No | 22 (14) | 0.22 (0.46) |
| Yes (b=1) | 133 (86) | 0.34 (0.53) |
| Pt. had living will | ||
| No | 29 (18.7) | 0.30 (0.59) |
| Yes (b=5) | 126 (81.3) | 0.34 (0.50 |
| Pt. expressed end-of-life care wishes | ||
| No (b=4) | 95 (61.3) | 0.24 (0.44)** |
| Yes | 60 (38.7) | 0.47 (0.60) |
| Locus of care | ||
| Pt. hospitalized prior to death | ||
| No | 68 (44.4) | 0.40 (0.55) |
| Yes | 85 (55.6) | 0.28 (0.49) |
| Pt. received hospice care | ||
| No | 48 (31.8) | 0.35 (0.50) |
| Yes | 103 (68.2) | 0.33 (0.53) |
Notes: Pt = patient.
p Values reported for F test or t tests for significant difference in family conflict.
bRefers to the number of missing respondents who were included in this category.
†p ≤ .10. *p ≤ .05. **p ≤ .01.
We hypothesized that conflict at the end of life will be higher among families with a prior history of conflict, without advance care planning, and younger, female, African American and adult child respondents and will be lower among families with greater socioeconomic resources (i.e, higher income and education) and those who received hospice care. As shown in Table 1, bivariate relationships between the contextual variables and the dependent variables reveal that family conflict was higher among those who were younger (t = 3.28, p ≤ .01), African American (t = −1.96, p ≤ .05), and adult children at a trend level only (t = 1.65, p ≤ .10). Contrary to our expectation, no relationship was found for income, education, for having a DPAHC or a living will, and reports of conflict were higher in situations in which the patient had expressed their end-of-life care wishes (t = −2.66, p ≤ .01). Hypothesis 1 is partially supported.
Conditions, Contributing Factors, and Family Conflict: Hypothesis 2
We hypothesized that patient clinical care needs and death awareness will be positively associated with contributing factors and family conflict. Table 2 presents the means and standard deviations of the analytic variables as well as the zero-order correlations among them. All the conditions were positively associated with contributing factors and with family conflict, although some of these relationships were trend level only. Difficulty in accepting the illness was significantly higher among patients with more clinical care needs at trend level only (r = .14, p ≤ .10 and r = .13, p ≤ .10 for physical and psychological symptoms, respectively) and was significantly correlated with death awareness (r = .17, p ≤ .05). Physical and psychological symptoms were associated with family asserting control (r = .25, p ≤ .01 and r = .18, p ≤ .05, respectively) and communication constraints (r = .19, p ≤ .05 and r = .31, p ≤ .001). Death awareness was correlated with family asserting control (r = .20, p ≤ .05) and communication constraints at the trend level (r = .13, p ≤ .10). Family conflict was significantly higher among families with patients who had more physical (r = .27, p ≤ .01) and psychological symptoms (r = .34, p < .001), and there was a trend level effect with death awareness (r = .13, p ≤ .10). Hypothesis 2 is supported.
Table 2.
Correlations and Descriptives for Analytic Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| 1 | Family conflict at end of life | — | ||||||||||
| 2 | History of conflict | .58*** | — | |||||||||
| 3 | Respondent agea | −.25** | −.15† | — | ||||||||
| 4 | Respondent racea | .17* | .03 | −.04 | — | |||||||
| 5 | Advanced care planning: specified wishesa | .21** | .06 | −.17* | .01 | — | ||||||
| 6 | Patient physical symptoms | .27** | .26** | −.27** | .12 | .15† | — | |||||
| 7 | Patient psychological symptoms | .34*** | .28*** | −.37*** | .03 | .15† | .50*** | — | ||||
| 8 | Death awarenessa | .13† | .03 | −.07 | .00 | .07 | .08 | .11 | — | |||
| 9 | Difficulty accepting illnessa | .20* | .14† | .16† | .14† | .04 | .14† | .13† | .17* | — | ||
| 10 | Family asserting control | .56*** | .25** | −.22** | .16† | .21** | .25** | .18* | .20* | .05 | — | |
| 11 | Communication constraints | .71*** | .33*** | −.11 | .04 | .14† | .19* | .31*** | .13† | .22** | .41*** | — |
| M | 0.33 | 0.38 | 0.51 | 0.03 | 0.39 | 2.12 | 0.85 | 0.80 | 2.10 | 0.31 | 0.59 | |
| SD | 0.52 | 0.73 | 0.50 | 0.18 | 0.49 | 1.34 | 0.81 | 0.40 | 1.35 | 0.72 | 0.90 | |
| Range | 0–2 | 0–4 | 0–1 | 0–1 | 0–1 | 0–4 | 0–2 | 0–1 | 0–4 | 0–4 | 0–4 | |
Notes: aMeans for dichotomous variables are reported as proportions.
†p ≤ .10. *p ≤ .05. **p ≤ .01. ***p ≤ .001.
Contributing Factors and Family Conflict: Hypothesis 3
We hypothesized that after controlling for the family context and conditions, that contributing factors will significantly predict family conflict. To test this third hypothesis, hierarchical multiple regression analysis was conducted that controlled for the family context and conditions of the patient. Due to the number of independent variables and the limited sample size, only the contextual variables that were significantly associated with family conflict were entered into the regression equation. The first block of independent variables included four contextual variables (i.e., history of conflict, family member age and race, and patient specified wishes for end-of-life care). The second block included the two clinical care need variables and death awareness. The third block included the three contributing factors (i.e., difficulty accepting illness, family asserting control, and communication constraints).
Table 3 presents the results of the regression analysis which explained 72% of the total variance in family conflict. In the first step of the model, family contextual variables explained 41% of the variance in conflict, and all four of the variables were significant predictors. In the second step, conditional variables did not make a significant contribution to the prediction of family conflict as a set, explaining only 2% of the total variance. In the third step, contributing factors uniquely explained 29% of the variance in conflict, the most important two being communication constraints and asserting control. Significant main effects in the prediction of family conflict in the final model included prior family conflict (β = .34, p ≤ .001), race (β = .11, p ≤ .05), communication constraints (β = .47, p ≤ .001), and family members asserting control (β = .24, p ≤ .001). Hypothesis 3 is supported.
Table 3.
Hierarchical Regression Analysis for Family Conflict
| Variables | Betas | ||
| Step1 | Step 2 | Step 3 | |
| Family context | |||
| History of conflict | .55*** | .52*** | .34*** |
| Family member age | −.13* | −.09 | −.07 |
| Family member race | .17** | .17** | .11* |
| Advanced care planning: specified wishes | .15* | .13* | .06 |
| Conditions | |||
| Physical symptoms | −.00 | −.03 | |
| Psychological symptoms | .12 | .02 | |
| Death awareness | .09 | .00 | |
| Contributing factors | |||
| Difficulty accepting illness | .02 | ||
| Family asserting control | .24*** | ||
| Communication constraints | .47*** | ||
| Total R2 | .41 | .43 | .72 |
| R2 change | .41 | .02 | .29 |
| F for R2 change | 26.15*** | 1.80 | 50.01*** |
*p ≤ .05. **p ≤ .001. *** p ≤ .001 (two-tailed).
Discussion
Although support of families is a core function of palliative care (Hudson, Quinn, O’Hanlon, & Aranda, 2008), efforts to address family needs have been hampered by the lack of descriptive data “regarding the composition or dynamics of families who characteristically need the most support” and who present with conflict at the end of life (King & Quill, 2006, p. 713). This study provides insights into the correlates and predictors of family conflict reported by spouses and adult children of persons who have died with lung cancer. Results reveal that conflict is higher among younger and African American respondents, and race remained a significant predictor after controlling for all other variables. With only five African American families included in this analysis, we strongly caution against over interpretation of this finding. We do not know the distinctive stressors these families have experienced or how they compare with other African American families with lung cancer. These findings are consistent with some studies investigating family discord in the general population (Kessler et al., 2001; Sorenson, Upchurch, & Shen, 1996). However, other than research documenting that racial minorities have higher medical costs that may be attributed to greater use of life-sustaining interventions (Hanchate, Kronman, Young-Xu, Ash, & Emanuel, 2009), and findings that greater family discord tends to be associated with stronger preferences for life-prolonging treatments (Winter & Parks, 2008), little research has examined the experience of African American families at the end of life. Family conflict may be affected by many factors that are external to the family, such as the experience of societal oppression, stress, discrimination, and access to resources. Future research is needed to understand variability in the experience in family conflict across diverse cancer populations and the source and etiology of conflicts that arise.
Not surprisingly, this study documents that the family’s history of conflict is a strong predictor of end-of-life conflict. This supports prior qualitative research findings that a history of unresolved conflict is likely to stimulate conflict at the end of life (Kramer et al., 2006). Routine assessment and screening for prior conflict as well as general family functioning (e.g., see King & Quill, 2006) would allow service providers to identify families at risk. Screening strategies have been used successfully to identify at-risk families in palliative care for a family-focused grief therapy intervention (Kissane et al., 2006).
Even after controlling for prior family conflict and demographic variables, asserting control regarding decisions about care and communication constraints in the family were significant predictors of conflict at the end of life. These contributing factors reflect decision-making and communication styles that influence family member interactions. Some evidence suggests that asserting control is associated with higher levels of conflict in friendship situations (Updegraff et al., 2004), and more expressive forms of communication are associated with greater family cohesiveness (Schrodt, 2005). Given the increased incidence of communication constraints among families of cancer patients (Cooper, 1984), this is a particularly important area for future research. Our study suggests that these responses may be stimulated when patients have more distressing symptoms and the family is aware of death. The development and testing of interventions to provide greater emotional support to the family in these circumstances and to facilitate shared decision making and enhance open communication among at risk families may be a fruitful area for future research.
There were two unexpected findings from this study. First, although we expected that conflict would be lower among families of patients who had completed advanced directives and expressed their end-of-life care wishes, we found that conflict was not associated with advanced directives and was higher when wishes were specified. Prior research suggests that family stress associated with end-of-life decision making is high when advance directives are not completed (Tilden et al., 1995). It should be noted that the majority of our sample had completed advanced directives. Spouses of older patients who responded to the survey may have had more information about wishes than adult children who arrived on the seen when care needs escalated. In addition, prior research suggests that incongruence in perceptions of care preferences may contribute to conflict (Kramer et al., 2006), and we did not ascertain how many or the extent to which family members were informed about the patient’s end-of-life care wishes. It is possible that even if family members are aware of the patient’s wishes, that they may simply disagree with these wishes and have other motivations for contesting them (e.g., religious beliefs). Family-based interventions such as family conferencing have been proposed as one method to ensure greater understanding and collaboration regarding end-of-life care decision making (Hudson et al., 2008), but further research is needed to understand the relationship between conflict and various forms of care planning, so that these family-based interventions may be further developed and refined.
The second unexpected finding was the absence of relationship between socioeconomic status and family conflict. We expected that the limited resources available to poorer and less educated families might result in higher conflict but found no difference in conflict by income or education. As will be described subsequently, an important limitation of this study was the nonrepresentative nature of this sample. Few respondents were living in poverty and nearly half had some college or a college degree. A study of family fighting using several data sets revealed that the relationship between socioeconomic status and family conflict was significant in some but not in all the data sets (Flake & Forste, 2006). Additional research is needed to further examine the role that socioeconomic status may have in predicting conflict at the end of life.
The limitations of this study design and measurement limit the full interpretation of its results and the conclusions that may be drawn. First, the cross-sectional design does not answer the directional nature of the relationships between family context, conditions, contributing factors, and family conflict. Although our conceptual model proffers that the contributing factors may influence family conflict, it is equally plausible that family conflict may influence communications constraints and family member’s efforts to assert control. Family interactions and relationships are dynamic rather than static processes. Time-ordered data are necessary to test the directionality of these relationships. Second, we rely on retrospective reports of conflict at the end of life. Given that the time from death to the completion of the surveys ranged so widely, averaging 19 months, and that time may influence recall, this is an important limitation. Ethical and methodological considerations curtail the amount of information researchers may obtain from patients and their families during the dying process, making studies of family conflict at the end of life in “real time,” especially challenging. Third, some of our measures are limited. For example, the single-item “death awareness” indicator of whether or not a conversation with an MD occurred regarding the likelihood of death and the locus of care questions that did not specify location at time of death may have underestimated potential relationships. The clinical care needs of the patients were assessed in terms of the number of symptoms during or after cancer treatments. Although these symptoms are common throughout the trajectory of illness and are often actively treated in palliative care settings (Stöppler & Marks, 2008), given that the majority of our sample had received hospice care and were likely no longer receiving cancer treatments, it is possible that our results seriously underestimate the potential role that clinical care needs of the patient at end of life may influence family conflict. Another limitation that restricts the generalizability of study findings is the nonrepresentative nature of the sample. Although the ACCESS study sought a representative statewide sample and over sampled by race, less than half of the eligible families completed the survey, and the sample was primarily of European descent and female spouses. The overall rates of family conflict were fairly modest, and a high percentage of our sample had living wills or DPAHC. Other studies have found higher rates of family conflict among more diverse samples (Kramer et al., 2006; Scharlach, Li, & Dalvi, 2006) and among siblings and adult children compared with spouses (Kissane et al., 1994). Given these limitations, it is important that these findings be viewed as a beginning step in understanding the correlates and predictors of family conflict at the end of life and that they be replicated and extended in longitudinal investigations, using more representative and diverse samples, across sites of care.
There are a number of implications for working with later life families that we would suggest could be taken into consideration. First, routine assessment involving multiple family members to obtain a careful history of family functioning and relationship quality might help to identify families at risk for conflict. Attention to family communication, roles, prior experiences with death, unresolved conflicts, and perceptions of health status could be explored It is advisable to recognize that family conflict may not always be apparent to the health care team or even to the family member (particularly a spouse caregiver). Supporting other research, we found slightly higher reports of conflict among adult children caring for parents than spouses (Clark et al., 2003; Kissane et al., 1994; Peisah et al., 2006; Semple, 1992). Second, assessment of the resources and demands on later families will provide a better understanding of the constraints that families face that might contribute to family discord. Third, family meetings might help to build trust and facilitate the exchange of information across generations regarding patient care needs and provide an opportunity to foster shared decision making and enhance communication. Finally, given the high degree of social stigma associated with lung cancer, many of these families face the end-of-life process with a great deal of loneliness and isolation that is likely exacerbated by conflict. Providing spouses and adult children an opportunity to openly grieve the losses associated with family discord and the disease itself may help to ease this distress.
In conclusion, we really know very little about the phenomenon of family conflict at the end of life and yet this is a major challenge for care providers that may jeopardize the quality of care provided and have enduring consequences for bereaved family members (Kramer et al., 2006), many who are older spouses left to deal with the aftermath of these experiences. Improving quality of end-of-life care for later life families will require a much better understanding of this phenomenon. Although this study provides preliminary evidence of correlates and predictors of conflict, additional qualitative and quantitative research is needed to further identify the associated familial and environmental characteristics, the causes and contributing factors, and the consequences of conflict. Attention should be given to understanding the distinctive needs of these families and their perspectives on how professionals might assist them to identify strategies to prevent or moderate this phenomenon. This study suggests potential value in developing and testing assessment protocols for early detection of at-risk families, and the need for intervention approaches to address communication barriers and promote shared decision making.
Funding
Funding for the Wisconsin Comprehensive Cancer Control Program is provided by the Centers for Disease Control and Prevention, the Wisconsin Department of Health Services, the Wisconsin Partnership Fund for a Healthy Future and the University of Wisconsin–Paul P. Carbone Comprehensive Cancer Center. This manuscript was prepared with support from the National Institute of Mental Health (T32 MH65185 to J. Greenberg).
Acknowledgments
This study used data from the ACCESS survey, a project of the Wisconsin Comprehensive Cancer Control Program. The authors gratefully acknowledge the bereaved family members for their participation in this study and the contributions of our colleagues who participated in the design of the ACCESS survey.
References
- American Cancer Society. Cancer facts and figures 2008. Atlanta, GA: Author; 2008. [Google Scholar]
- Badr H, Taylor C. Social constraints and spousal communication in lung cancer. Psycho-Oncology. 2006;15:673–683. doi: 10.1002/pon.996. [DOI] [PubMed] [Google Scholar]
- Cameron J, Franche R, Cheung AM, Stewart DE. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94:521–527. doi: 10.1002/cncr.10212. [DOI] [PubMed] [Google Scholar]
- Carr D, Khodyakov D. “Health Care Proxies in Later Life: Whom Do We Choose and Why?”. Journal of Health and Social Behavior. 2007;48:180–194. doi: 10.1177/002214650704800206. [DOI] [PubMed] [Google Scholar]
- Chan CWH, Chang AM. Managing caregiver tasks among family caregivers of cancer patients in Hong Kong. Journal of Advanced Nursing. 1999;29:484–489. doi: 10.1046/j.1365-2648.1999.00911.x. [DOI] [PubMed] [Google Scholar]
- Chekryn J. Cancer recurrence: Personal meaning, communication, and marital adjustment. Cancer Nursing. 1984;7:491–498. [PubMed] [Google Scholar]
- Clark PC, Shields CG, Aycock D, Wolf SL. Preliminary reliability and validity of a family caregiver conflict scale for stroke. Progress in Cardiovascular Nursing. 2003;18:77–82. 92. [PubMed] [Google Scholar]
- Cooper ET. A pilot study on the effects of the diagnosis of lung cancer on family relationships. Cancer Nursing. 1984;7:301–308. [PubMed] [Google Scholar]
- Davis LL. Family conflicts around dementia home-care. Families, Systems & Health. 1997;15:85–98. [Google Scholar]
- Dillman D. Mail and telephone surveys: The total design method. New York: John Wiley & Sons; 1978. [Google Scholar]
- Downey RG, King C. Missing data in Likert ratings: A comparison of replacement methods. Journal of General Psychology. 1998;125:175–191. doi: 10.1080/00221309809595542. [DOI] [PubMed] [Google Scholar]
- Flake DF, Forste R. Fighting families: Family characteristics associated with domestic violence in five Latin American Countries. Journal of Family Violence. 2006;21:19–29. [Google Scholar]
- Hanchate A, Kronman A, Young-Xu Y, Ash A, Emanuel E. Racial and ethnic differences in end-of-life costs. Archives of Internal Medicine. 2009;169:493–501. doi: 10.1001/archinternmed.2008.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawthorne G, Elliott P. Imputing cross-sectional missing data: Comparison of common techniques. Australian and New Zealand Journal of Psychiatry. 2005;39:583–590. doi: 10.1080/j.1440-1614.2005.01630.x. [DOI] [PubMed] [Google Scholar]
- Hilton BA. Family communication patterns in coping with early breast cancer. Western Journal of Nursing Research. 1994;16:366–388. doi: 10.1177/019394599401600403. [DOI] [PubMed] [Google Scholar]
- Hudson P, Quinn K, O’Hanlon B, Aranda S. Family meetings in palliative care: Multidisciplinary clinical practice guidelines. BMC Palliative Care. 2008;7:1–30. doi: 10.1186/1472-684X-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juan O, Albert A, Campos JM, Caranyana JM, Alberola V. Measurement and impact of co-morbidity in elderly patients with advanced non-small cell lung cancer treated with chemotherapy. A phase II study of weekly paclitaxel. Acta Oncologica. 2007;46:367–373. doi: 10.1080/02841860600833178. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Molnar BE, Feurer ID, Appelbaum M. Patterns and mental health predictors of domestic violence in the United States: Results from the National Comorbidity Survey. International Journal of Law and Psychiatry. 2001;24:487–508. doi: 10.1016/s0160-2527(01)00080-2. [DOI] [PubMed] [Google Scholar]
- King DA, Quill T. Working with families in palliative care: One size does not fit all. Journal of Palliative Medicine. 2006;9:704–715. doi: 10.1089/jpm.2006.9.704. [DOI] [PubMed] [Google Scholar]
- Kissane DW, Bloch S, Burns WI, McKenzie DP, Posterino M. Psychological morbidity in the families of patients with cancer. Psycho-Oncology. 1994;3:47–56. [Google Scholar]
- Kissane DW, McKenzie M, Bloch S, Moskowitz C, McKenzie DP, O’Neill I. Family focused grief therapy: A randomized, controlled trial in palliative care and bereavement. American Journal of Psychiatry. 2006;163:1208–1218. doi: 10.1176/ajp.2006.163.7.1208. [DOI] [PubMed] [Google Scholar]
- Kline GH, Wood LF, Moore S. Validation of modified family and interparental conflict scales for use with young adults from divorced and non-divorced families. Journal of Divorce & Remarriage. 2003;39(3/4):125–142. [Google Scholar]
- Kools S, McCarthy M, Durham R, Robrecht L. Dimensional analysis: Broadening the conception of grounded theory. Qualitative Health Research. 1996;6:312–330. [Google Scholar]
- Kramer BJ, Boelk A, Auer C. Family conflict at the end-of-life: Lessons learned in a model program for vulnerable older adults. Journal of Palliative Medicine. 2006;9:791–801. doi: 10.1089/jpm.2006.9.791. [DOI] [PubMed] [Google Scholar]
- Kramer BJ, Christ GH, Bern-Klug M, Francoeur RB. A national agenda for social work research in palliative and end-of-life care. Journal of Palliative Medicine. 2005;8:418–431. doi: 10.1089/jpm.2005.8.418. [DOI] [PubMed] [Google Scholar]
- Lee RM, Choe J, Kim G, Ngo V. Construction of the Asian American Family Conflicts Scale. Journal of Counseling Psychology. 2000;47:211–222. [Google Scholar]
- Moos RH, Moos BH. Family Environment Scale Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1994. [Google Scholar]
- National Consensus Project for Quality Palliative Care. Clinical practice guidelines for quality palliative care. 2nd ed. 2009. Available from http://www.nationalconsensusproject.org. [PubMed] [Google Scholar]
- National Institutes of Health State-of-the-Science Conference Statement: Improving End-of-Life Care. December 6–8, 2004. Accessed December 22, 2004, from http://consensus.nih.gov/2004/2004EndOfLifeCareSOS024html.htm. [Google Scholar]
- Pearman T. Psychosocial factors in lung cancer: Quality of life, economic impact and survivorship implications. Journal of Psychosocial Oncology. 2008;26(1):69–80. doi: 10.1300/j077v26n01_05. [DOI] [PubMed] [Google Scholar]
- Peisah C, Brodaty H, Quadrio C. Family conflict in dementia: Prodigal sons and black sheep. International Journal of Geriatric Psychiatry. 2006;21:485–492. doi: 10.1002/gps.1501. [DOI] [PubMed] [Google Scholar]
- Quirt CF, Mackillop WJ, Ginsburg AD, Sheldon L, Brundage M, Dixon P, et al. Do doctors know when their patients don’t? A survey of doctor-patient communication in lung cancer. Lung Cancer. 1997;18:1–20. doi: 10.1016/s0169-5002(97)00048-2. [DOI] [PubMed] [Google Scholar]
- Scharlach A, Li W, Dalvi T. Family conflict as a mediator of caregiver strain. Family Relations. 2006;55:625–635. [Google Scholar]
- Schrodt P. Family communication schemata and the circumplex model of family functioning. Western Journal of Communication. 2005;69:359–376. [Google Scholar]
- Semple SJ. Conflict in Alzheimer’s caregiving families: Its dimensions and consequences. The Gerontologist. 1992;32:648–655. doi: 10.1093/geront/32.5.648. [DOI] [PubMed] [Google Scholar]
- Sorenson SB, Upchurch DM, Shen H. Violence and injury in marital arguments: Risk patterns and gender differences. American Journal of Public Health. 1996;86:35–40. doi: 10.2105/ajph.86.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stöppler MC, Marks JW. Lung cancer. 2008 Accessed June 1, 2009, from http://www.medicinenet.com/lung_cancer/page4.htm. [Google Scholar]
- Strawbridge WJ, Wallhagen MI. Impact of family conflict on adult child caregivers. The Gerontologist. 1991;31:770–777. doi: 10.1093/geront/31.6.770. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 4th ed. Boston: Allyn & Bacon; 2000. [Google Scholar]
- Tilden VP, Tolle SW, Garland MJ, Nelson CA. Decisions about life-sustaining treatments. Archives of Internal Medicine. 1995;155:633–638. [PubMed] [Google Scholar]
- Updegraff KA, Helms HM, McHale SM, Courter AC, Thayer SM, Sales SM. Who’s the boss? Patterns of perceived control in adolescents’ friendships. Journal of Youth and Adolescence. 2004;33:403–420. [Google Scholar]
- Valdimarsdóttir U, Kreicbergs U, Hauksdóttir A, Hunt H, Onelöv E, Henter J, et al. Parents’ intellectual and emotional awareness of their child's impending death to cancer: A population-based long-term follow-up study. Lancet Oncology. 2007;8:706–714. doi: 10.1016/S1470-2045(07)70209-7. [DOI] [PubMed] [Google Scholar]
- Winter L, Parks SM. Family discord and proxy decision makers’ end-of-life treatment decisions. Journal of Palliative Medicine. 2008;11:1109–14. doi: 10.1089/jpm.2008.0039. [DOI] [PubMed] [Google Scholar]
- Wisconsin Comprehensive Cancer Control Plan. (2005–2010). University of Wisconsin Comprehensive Cancer Center and WI Department of Health and Family Services. [Google Scholar]
- Zhang A, Siminoff L. Silence and cancer: Why to patients and families fail to communicate? Health Communication. 2003a;15:415–429. doi: 10.1207/S15327027HC1504_03. [DOI] [PubMed] [Google Scholar]
- Zhang A, Siminoff L. The role of the family in treatment decision making by patients with cancer. Oncology Nursing Forum. 2003b;30:1022–1028. doi: 10.1188/03.ONF.1022-1028. [DOI] [PubMed] [Google Scholar]