Abstract
Background: Chronic Obstructive Pulmonary Disease (COPD) causes a huge economic burden and >80% of COPD cases are attributable to smoking. Massachusetts introduced a comprehensive Tobacco Control Program (MTCP) in January 1993. A trend analysis of COPD hospitalization rates might indirectly reflect the potential impact of such comprehensive tobacco control programs.
Methods: Age-adjusted COPD hospitalization rates/100 000 was abstracted from the Massachusetts Community Health Information Profile Database between 1989 and 2005. Joinpoint Regression Analyses program was employed to estimate annual percent changes (APC) in COPD rates by age, sex and race.
Results: In 1989, 265/100 000 age-adjusted COPD hospitalization rates were reported that increased to 423/100 000 in 1993, and then declined to 329/100 000 in 2005. A significant annual decline of 5.6 percentage points was observed in overall COPD rates from 1993 onwards. A similar temporal pattern, with an age-gradient and a slower annual decline in female COPD rates relative to male COPD rates, was observed. COPD rates in both Blacks and Whites were similar to the general overall pattern. Such consistent annual declines in COPD hospitalization rates from 1993 onwards in Massachusetts also closely correspond to the introduction of the MTCP in January 1993.
Conclusion: The findings indirectly suggest that smoking cessation should remain the cornerstone strategy for the prevention and control of COPD burden. However, additional studies across different population settings are essential for a definitive conclusion with regard to the immediate impact of a comprehensive tobacco control program on COPD hospitalization rates showing possible gender susceptibility.
Introduction
Chronic obstructive pulmonary disease (COPD) remains a major public health problem. COPD is the fourth leading cause of chronic morbidity and mortality in the USA,1 and is projected to rank fifth in 2020 in burden of disease worldwide.2 A recent study has also shown that COPD death rates doubled across the USA between 1970 and 2002.3 However, temporal patterns in COPD hospitalization rates are limited. COPD hospitalization rates might reflect the immediate impact of underlying comprehensive public-health interventions unlike the COPD death rates, which are more suggestive of a long-term effect.
The state of Massachusetts had introduced a comprehensive Tobacco Control Program (MTCP) in January 1993.4 Significant impacts of the MTCP on the fall in smoking prevalence, as well as on coronary heart disease deaths have been reported.5,6 The MTCP included the following elements: increased tobacco prices, including tax increases, advocacy from health organizations, increasing implementation of smoke-free policies, governmental ordinances and regulations on advertisements and on tobacco products, increased availability of cessation and counseling services, and increased counter-advertising.4 Approximately 80–90% of the COPD is attributable to smoking.7,8 It is therefore plausible that changing temporal patterns in COPD hospitalization rates in Massachusetts might also indirectly suggest the underlying impact of both recent and past tobacco control efforts, including the MTCP, similar to a recent study on lung cancer deaths in Massachusetts.9
Methods
Data sources
The Massachusetts Department of Public Health developed an electronic database called the Massachusetts Community Health Information Profile (MassCHIP) to assist communities and professionals in health planning. Details are available on the website (http://masschip.state.ma.us/about.htm). The MassCHIP is a dynamic, user-friendly information service that provides free, online access to many health and social indicators. With MassCHIP, one can obtain community-level data to assess health needs, monitor health status indicators, and evaluate health programs. MassCHIP provides access to 36 health status, health outcome, program utilization and demographic data sets, from which one can generate two types of reports: (i) instant topics (formerly standard reports) and (ii) custom reports, as well as charts and maps. Instant topics are predefined reports which use MassCHIP’s most current data to supply information on a variety of topic areas for specific geographies. Custom reports are user-defined reports which can be created by downloading the MassCHIP Client and choosing the data set and selectors of interest. Depending on the data source, one can view an entire range of selectors including geography, year, age, race and ethnicity, gender, or income.
For the purpose of this particular study, COPD hospitalizations from 1989 to 2005, using the Ninth International Classification of Diseases (ICD-9: 490–496) were abstracted. Detailed information (aggregate data) on the gender, age and racial distribution by COPD hospitalization rates were also obtained from the MassCHIP online database. The MassCHIP has almost 100% coverage of all hospitals within the state of Massachusetts. MassCHIP has become a model for other states and for the nation. All COPD hospitalizations are age-adjusted per 100 000 persons. As a control, hospitalization rates of injuries for the same periods (1989–2005) were also obtained, using the MassCHIP database.
Statistical analyses
The US National Cancer Institute’s ‘Joinpoint’ Regression Analysis Program (Version 3.0), Windows-based statistical software can delineate exactly when significant changes in the direction of disease rates occur.10 The software analyses can model data where several trend-lines are connected together at ‘joinpoints’. The software takes trend data (in this case age-adjusted COPD hospitalization rates) and fits the simplest inflexion model allowable. The program starts with the minimum number of joinpoints (e.g. 0 joinpoints, which is a straight line) and tests whether more joinpoints are statistically significant and must be added to the model, thus enabling the user to test whether an apparent change in trend is statistically significant. Statistically significant values from ‘zero’ at P = 0.05 were assessed by use of two-sided tests. Each joinpoint estimates the annual-percent-change (APC) in COPD hospitalization rates on a yearly basis. The calculation assumes that rates increase or decrease at a constant rate over time, although the validity of this assumption has not been tested. APC is calculated based on the following regression model:
where log(Ry) is the natural log of the rate in year y.
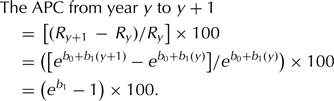 |
Results
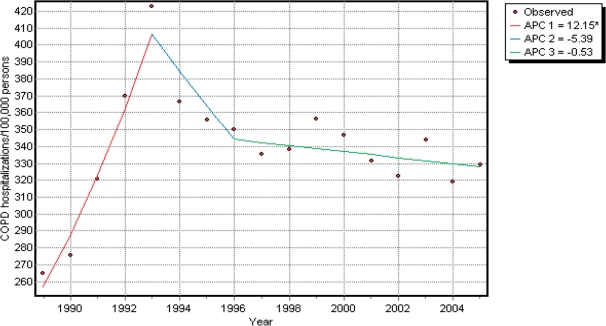
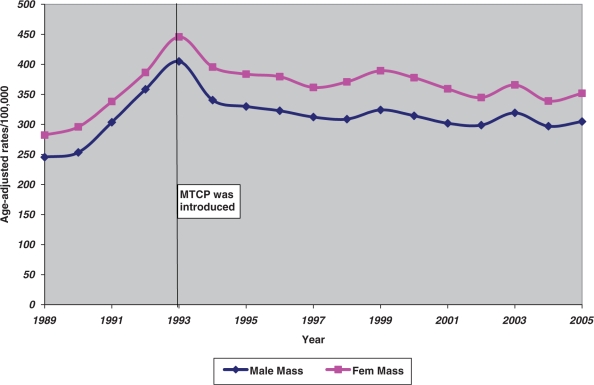
In 1989, 265/100 000 age-adjusted COPD hospitalization rates were reported that increased to 423/100 000 in 1993, and then declined to 329/100 000 in 2005. In other words, COPD hospitalization rates were increasing significantly with a yearly rise of 12.1%, but showed an annual decline of 5.4% from 1993 to 1996 and then a slower decline of 0.5% yearly (Figure 1). Figure 1 also shows the significant inflexion points, namely in 1993 and then again in 1996. A similar temporal pattern persisted (an increasing trend until 1993 followed by a decreasing trend) when the analyses were conducted separately for males and females but COPD rates in females were higher relative to male COPD rates (Figure 2 and Table 1). However, a slower annual decline was observed in females relative to males, with a statistically significant decline in female COPD rates alone (Table 1).
Figure 1.
Total COPD hospitalization rates (age-adusted/100 000 persons) in Massachusetts, 1989–2005.
Figure 2.
Male and female COPD age-adjusted hospitalization rates/100 000 persons in Massachusetts from 1989 to 2005.
Table 1.
Estimated annual percent changes (APC) in COPD hospitalization rates by age, sex and race in Massachusetts, 1989–2005
| Variables | Year | APC (95% confidence interval) |
|---|---|---|
| Age (in years) | ||
| 0–14 | 1989–93 | 2.5 (−6.1; 11.9) |
| 1993–96 | −20.9 (−43.3; 10.3) | |
| 1997–2005 | 0.73 (−2.7; 4.3) | |
| 15–44 | 1989–93 | 2.1 (−2.9; 7.4) |
| 1993–2005 | −4.4 (−5.4; −3.4)a | |
| 45–64 | 1989–93 | 9.3 (5.4; 13.4)a |
| 1993–2005 | −1.3 (−1.9; −0.6)a | |
| 65–84 | 1989–93 | 24.5 (18.1; 31.3)a |
| 1993–2005 | 0.06 (−0.7; 0.8) | |
| Sex | ||
| Males | 1989–93 | 13.4 (9.4; 17.6)a |
| 1993–96 | −7.1 (−16.5; 3.3) | |
| 1996–2005 | −0.4 (−1.4; 0.6) | |
| Females | 1989–93 | 10.3 (6.8; 13.9)a |
| 1993–2005 | −1.6 (−2.1; −1.0)a | |
| Race | ||
| Whites | 1990–92 | 20.3 (0.3; 44.2)a |
| 1992–2005 | −0.7 (−1.6; 0.1) | |
| Blacks | 1990–93 | 9.7 (2.8; 17.0)a |
| 1993–2000 | −6.7 (−8.8; −4.6)a | |
| 2000–05 | −1.2 (−4.5; 2.3) | |
| Hispanics | 1990–2005 | −1.5 (−2.9; −0.05)a |
aStatistically different from ‘zero’ at P = 0.05.
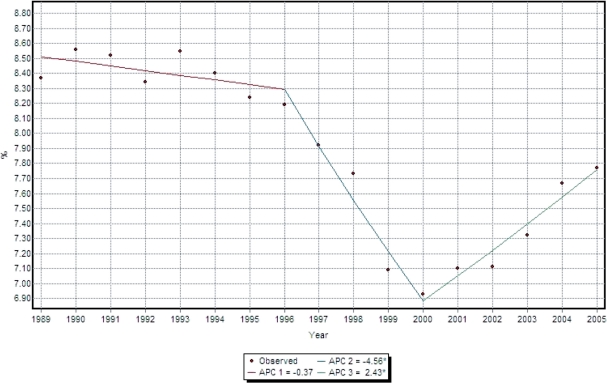
Overall, no distinct patterns emerged when COPD rates were analyzed by age-groups and by race (Table 1). Data for race were only available from 1990 in the Mass CHIP database. In contrast to Blacks and Whites, Hispanics showed a consistent significant annual decline of 1.5% from 1990 to 2005 (Table 1). The oldest age-groups (⩾65 years) did not show a significant annual decline unlike the younger age-groups (Table 1), who showed a significant annual decline from 1993 onwards. When hospitalization rates of injuries (as a control) were analyzed for the same periods, a pattern different from the COPD hospitalization rates was observed (Figure 3).
Figure 3.
Hospitalization rates of injuries (age-adusted/100 000 persons) in Massachusetts, 1989–2005.
Discussion
This trend analysis showed an annual decline in COPD hospitalization rates in Massachusetts from 1993 onwards consistently showing a similar pattern across different age groups, in both the sexes and also in both Blacks and Whites. The fact that a consistent pattern of annual decline in COPD hospitalization rates from 1993 onwards corresponds to the introduction of the comprehensive MTCP in January 1993, such a temporal pattern might suggest a potential link. In addition, the control group (hospitalization rates in injuries) for the same periods showed a different pattern.
ICD-9 codes were modified in 1998 but in 1992 a new ICD-9-CM code, 491.21, was introduced to categorize obstructive chronic bronchitis with acute exacerbation.11 Such changes did not influence the trends, as trends in COPD hospitalizations consistently showed an increase from 1989 to 2000 after an initial fall between 1984 and 1989 for the whole of the USA.11 Also, COPD death rates increased from 1980 to 2000 in the USA.11 The Global Initiative for Obstructive Lung Disease (GOLD) criteria was introduced only in the early 2000,12 thus limiting the influence of changing clinical practice. No influenza epidemics were noted in 1993 in Massachusetts. It was also apparent from an earlier study that smoking rates in Massachusetts were almost stable between 1990 and 1992 but showed a sharp fall in 1993 and then gradually increased peaking in 1996,13 closely corresponding to the deceleration of COPD rates from 1996 in the present study.
Furthermore, a slower annual decline in COPD rates was observed in females relative to males, and the annual declines in female rates were statistically significant. In addition, the female COPD rates were higher relative to male COPD rates. A gender difference was also noted in an Irish study.14 Such observations might indicate the slower and delayed uptake of tobacco use in women vis-à-vis males’ smoking habits in the USA. An earlier study also reported a slower decline in smoking rates among the women in Massachusetts between 1990 and 1999.13 COPD mortality rates are also increasing in females across the whole of USA.12 Studies have demonstrated an increased effect of smoking on lung function in females, after controlling for smoking intensity.15,16 In addition, women might be more susceptible to COPD as a result of sex differences in xenobiotic metabolism, hormones that modify detoxifying enzymes, airway inflammation and responsiveness, and particle deposition.17
COPD causes a huge economic burden.18 Treatment and diagnoses have both improved over the years.1 Although tobacco smoking is the most critical risk factor for the development and progression of COPD, exposure to ambient pollutants both in the home and in workplace are also key factors.19 The indoor air quality has improved dramatically in the USA over the years and smoke-free homes and policies are also significantly increasing in the USA.20 COPD is common among the elderly and severity of COPD is one of the causes of hospitalizations. The present study showed no apparent significant annual decline in COPD rates in the ⩾65 age groups unlike the rates among the relatively young COPD patients. Such observations are consistent with the natural history of COPD among smokers. The reported steady increase in COPD death rates across the whole of the USA, with declining hospitalization rates, suggest that the observed decline is most likely not related to a lower prevalence of severe COPD among the population.12,21 Nevertheless, similar trend analyses in geographic areas with and without a comprehensive tobacco control program are worth considering.
There are limitations using hospitalizations data, for example, the accuracy and completeness of reporting, as well as the chances of in and out-migrations of populations. Also, the referral pattern might be an influencing factor. However, such explanations are less of a probability because of the representative ness of the Mass CHIP database, and also due to the inclusion of all hospitals across Massachusetts. We used hospitalization rates of ‘injuries’ over the same time period in Massachusetts as surrogate measure for changing clinical practices or admission criteria of hospitals in Massachusetts, and found a pattern not consistent with the COPD hospitalization trends.
In conclusion, the significant annual reductions in age-adjusted COPD hospitalization rates in Massachusetts from 1993 to 2005 correspond to the introduction of a comprehensive Tobacco Control Program in 1993. Changing diagnostic criteria are less likely to influence the observed patterns. The findings reflect a gender difference in the temporal pattern for COPD rates, with an age-gradient. The findings also indirectly suggest that smoking cessation is the cornerstone strategy for the prevention and control of COPD burden. However, additional studies across different population settings are essential before concluding the immediate positive impact of a comprehensive tobacco control on COPD hospitalization rates and possible gender susceptibility.
Funding
Dr Zubair Kabir was a research fellow at the Harvard School of Public Health at the time of this study, and was jointly funded through a research grant from the Health Research Board (Ireland) and the National Cancer Institute (USA).
Conflict of interest: None declared.
Acknowledgements
Dr. Howard Koh, former Director of the Division of Public Health Practice, Harvard School of Public Health, is currently the Assistant Secretary for Health in the U.S. Department of Health and Human Services (HHS). The article was written prior to Dr. Koh's appointment as the Assistant Secretary for Health and does not necessarily represent the views of HHS or the United States.
References
- 1.Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–55. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 2.Lopez AD, Shibuya K, Rao C, Mathers CD, Hansell AL, Held LS, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27:397–412. doi: 10.1183/09031936.06.00025805. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Ward E, Hao Y, Thun M. Trends in the leading causes of death in the United States, 1970-2002. JAMA. 2005;294:1255–9. doi: 10.1001/jama.294.10.1255. [DOI] [PubMed] [Google Scholar]
- 4.Koh H, Judge CM, Robbins H, Celebucki CC, Walker DK, Connolly GN. The first decade of the Massachusetts Tobacco Control Program. Public Health Rep. 2005;120:482–95. doi: 10.1177/003335490512000503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biener L, Harris JE, Hamilton W. Impact of the Massachusetts tobacco control programme: population-based trend analysis. BMJ. 2000;321:351–4. doi: 10.1136/bmj.321.7257.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kabir Z, Connolly GN, Clancy L, Koh HK, Capewell S. Coronary heart disease deaths and decreased smoking prevalence in Massachusetts, 1993–2003. Am J Public Health. 2008;98:1468–9. doi: 10.2105/AJPH.2007.129924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US Surgeon General. The Health Consequences of Smoking: Chronic Obstructive Lung Disease. (DHSS publication 84-50205) Washington, DC: US Department of Health and Human Services; 1984. [Google Scholar]
- 8.Bresnitz EA. Epidemiology of advanced lung disease in the United States. Clin Chest Med. 1977;18:421. doi: 10.1016/s0272-5231(05)70392-0. [DOI] [PubMed] [Google Scholar]
- 9.Kabir Z, Connolly GN, Clancy L, Jemal A, Koh HK. Reduced lung cancer deaths attributable to decreased tobacco use in Massachusetts. Cancer Causes Control. 2007;18:833–8. doi: 10.1007/s10552-007-9027-3. [DOI] [PubMed] [Google Scholar]
- 10.Kim H-J, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 11.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance in the US, 1971-2000. MMWR Surveill Summ. 2002;51:1–16. [PubMed] [Google Scholar]
- 12.World Health Organization. Global Initiative for Obstructive Lung Disease. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 13.Weintraub JM, Hamilton WL. Trends in prevalence of current smoking, Massachusetts and states without tobacco control programmes, 1990 to 1999. Tob Control. 2002;11(Suppl. 2):ii8–13. doi: 10.1136/tc.11.suppl_2.ii8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kabir Z, Clarke V, Keogan S, Clancy L. Chronic obstructive pulmonary disease hospitalization trends in Ireland. Ir J Med Sci. 2009;178(Suppl. 11):S439. [Google Scholar]
- 15.Prescott E, Bjerg AM, Andersen PK, Lange P, Vestbo J. Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. Eur Respir J. 1997;10:822–7. [PubMed] [Google Scholar]
- 16.Gold DR, Wang X, Wypij D, Speizer FE, Ware JH, Dockery DW. Effects of cigarette smoking on lung function in adolescent boys and girls. N Engl J Med. 1996;335:931–7. doi: 10.1056/NEJM199609263351304. [DOI] [PubMed] [Google Scholar]
- 17.Sin DD, Cohen SB, Day A, Coxson H, Paré PD. Understanding the biological differences in susceptibility to chronic obstructive pulmonary disease between men and women. Proc Am Thorac Soc. 2007;4:671–4. doi: 10.1513/pats.200706-082SD. [DOI] [PubMed] [Google Scholar]
- 18.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370:765–73. doi: 10.1016/S0140-6736(07)61380-4. [DOI] [PubMed] [Google Scholar]
- 19.Celli BR. Update on the management of COPD. Chest. 2008;133:1451–62. doi: 10.1378/chest.07-2061. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) State-specific secondhand smoke exposure and current cigarette smoking among adults—United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1232–5. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention (CDC) Deaths from chronic obstructive pulmonary disease- United States, 2000-2005. MMWR Morb Mortal Wkly Rep. 2008;57:1229–32. [PubMed] [Google Scholar]