Educational evidence is hard to find
The BEME (Best Evidence Medical Education) collaboration is aiming to do for medical education what the Cochrane Collaboration has done for medical treatments. But with few information sources dedicated to medical education, searching for evidence to define best practice is daunting. To help the quest, a study in Medical Teacher sets out a vast array of key information resources, although it warns that cast iron answers are hard to obtain. One BEME group found that the percentage of known citations retrieved (sensitivity) ranged between 6.5% and 19.6%, and the percentage of search results that were relevant to the query (specificity) was a disappointing 17.5%.
Medical Teacher 2003;25: 352-63
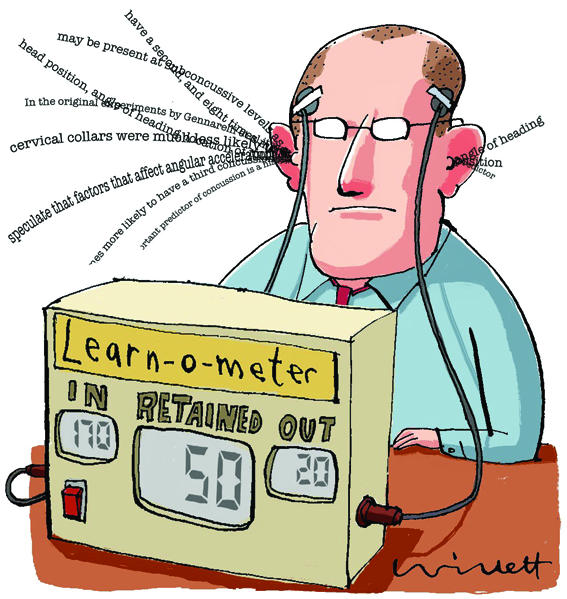
Lifelong learning can be evaluated
Up to now most of us will have assumed that we knew what the term “lifelong learning” means and that we all practise it to some extent. This cosy misapprehension may be about to end with the development of an instrument to measure it. This entails completing a questionnaire based around four domains: self initiation, information seeking skills, ability to identify learning needs, and motivation.
Medical Teacher 2003;25: 433-7
Figure 1.
Jury is still out on PBL
Despite a massive curricular shift towards problem based learning (PBL) there is still uncertainty over the effectiveness of this educational strategy. This is highlighted in a recent meta-analysis undertaken by the Campbell Collaboration, which publishes systematic reviews in social science and education (www.campbellcollaboration.org). Details of the study are on the website of the Learning and Teaching Network (www.ltsn.ac.uk). This site is a useful generic educational site which provides guides on subjects such as portfolio based assessment, planning courses, and e-learning. The subject centre of most direct relevance to medicine is at www.ltsn-01.ac.uk
Medical Teacher 2003;25: 433-7
The SNAPPS approach to improving teaching skills
Do you feel your teaching in your outpatient or GP surgery lacks structure? If so you might like to try out the six-step SNAPPS approach to facilitating student learning: Summarise the case (learner summarises history and findings), Narrow the differential diagnosis (learner offers two or three explanations), Analyse the differential diagnosis (learner compares the relative likelihood of each differential), Probe thinking (learner sounds out trainer's views and identifies learning needs), Plan management (learner draws up management plan with trainer), Select issue (learner identifies an issue for further self directed learning).
Academic Medicine 2003;78: 893-8
Patients and students value bedside case presentations
There is a common belief that when medical students present cases to teachers in front of the patients concerned, the patients get worried or confused. This belief is challenged by a study that was conducted at the University of Washington School of Medicine. In a survey of the views of 108 patients and 142 students, patients expressed a clear preference for their case histories to be presented in their presence rather than “outside the door.” Students valued this approach too; they perceived it improved their diagnostic skills and “bedside manner.”
Academic Medicine 2003;78: 945-9
Educational outcomes are measurable
For years educational researchers have struggled to produce evidence that is acceptable to other academic colleagues. The recent special educational issue of JAMA ( 2003;290(9)) throws light on why this is. Framing research questions to explore abstract concepts like communication and multi-professional learning is not easy (pp 1210-2), nor is finding good outcome measures to assess improvements in performance (pp 1183-9.) But on a more optimistic note, a study on the teaching of communication skills (pp 1157-65) shows that skills can be improved—and can be shown to have improved—when OSCEs (objective structured clinical examinations) are used in the assessment process.
JAMA 2003;290(9)
Professional assessment should relate to patient care
At the recent annual meeting of the Association for the Study of Medical Education, (ASME; www.asme.org.uk) in Edinburgh, Professor Lambert Schuwirth, an educationalist from Maastricht University, warned of the dangers of pursuing “the Holy Grail” of refining the reliability of tests. Reliability should be a tool for analysing test results, not a goal in itself. He also encouraged delegates to go beyond measuring traits such as problem solving skills and move towards assessing outcomes that affect patient care.
GP and hospital training should be complementary
Much of undergraduate medical education now takes place in general practice. A large survey of what students see during their GP attachments says that the area where students get most experience is in the management of chronic illness. The authors recommend that hospital based teaching should therefore concentrate on ensuring that students receive adequate exposure to acute illness to complement their experience in general practice.
Medical Education 2003;37: 790-3
Editorial by Wass et al


