Abstract
Aims
The aims of this research are to begin to understand health care teams in their operational environment, establish metrics of performance for these teams, and validate a series of scenarios in simulation that elicit team and technical skills. The focus is on defining the team model that will function in the operational environment in which health care professionals work.
Methods
Simulations were performed across the United States in 70- to 1000-bed hospitals. Multidisciplinary health care teams analyzed more than 300 hours of videos of health care professionals performing simulations of team-based medical care in several different disciplines. Raters were trained to enhance inter-rater reliability.
Results
The study validated event sets that trigger team dynamics and established metrics for team-based care. Team skills were identified and modified using simulation scenarios that employed the event-set-design process. Specific skills (technical and team) were identified by criticality measurement and task analysis methodology.
Discussion
In situ simulation, which includes a purposeful and Socratic Method of debriefing, is a powerful intervention that can overcome inertia found in clinician behavior and latent environmental systems that present a challenge to quality and patient safety. In situ simulation can increase awareness of risks, personalize the risks, and encourage the reflection, effort, and attention needed to make changes to both behaviors and to systems.
Project Summary
Errors in health care that compromise patient safety are tied to latent failures in the structure and function of systems. Teams of people perform most care delivered today, yet training often remains focused on individual responsibilities. Training programs for all health care workers need to increase the educational experience of working in interdisciplinary teams. The complexities of team training require a multifunctional (systems) approach that crosses organizational divisions to allow communication, accountability, and creation and maintenance of interdisciplinary teams. This paper will discuss research to identify the critical team skills for health care professionals identified in the system and the process that they work in by using in situ simulation.
The Institute of Medicine (IOM) report To Err is Human bluntly states, “[M]ost care delivered today is done by teams of people, yet training often remains focused on individual responsibilities, leaving practitioners inadequately prepared to enter complex settings.…[T]he ‘silos’ created through training and organization of care impede safety improvements.”1
How health professionals learn needs to be redesigned. This must include integration of simulation into every phase of education, establishment of metrics that allow validation of skills (that are performance based), and the integration of team skills into the learning process early in a health care professional's career. Additionally, there must be opportunities for cross-discipline teams to practice these skills to understand the dynamics of team skills in the operational environment.
Our research is the first step toward understanding health care teams in their operational environment, establishing metrics of performance for these teams, and validating a series of scenarios in simulation that elicit team and technical skills. The work focuses on defining the team model that will function in the operational environment that health care professionals work in. In the past 3 years we have designed simulations, validated event sets that trigger team dynamics, established metrics, performed inter-rater reliability training, and had independent multidisciplinary health care teams analyze over 300 hours of videos of health care professionals' clinical performance in different disciplines, based on simulations in hospitals of varying size and at different times of day and night. Specific skills (technical and team) were identified by criticality measurement and task analysis methodology. Team skills were identified and modified using simulation scenarios for modeling employing the event-set-design process.
Background
Clinician behavior change has been shown to be a formidable challenge to quality and patient safety in health care. In situ simulation is a powerful intervention that should increase awareness of risks, personalize the risks, and encourage reflection, effort, and attention to make needed changes. In situ simulation also provides an excellent laboratory for (1) risk assessment and investigation into undetected holes in safety defenses, (2) an environment that engages clinicians in awareness of systemic risks and the risks from communication and teamwork, and (3) the provision of tools to address these risks. Therefore, in situ simulation is a powerful and potentially organizationally transformative intervention.
The importance of effective teamwork in health care is as critical to safety as it is in aviation. Safety scholars2 attribute the failure of a health care team or flight crew to a potential loss of life, noting that “it is the team, not the aircraft or the individual pilot, that is at the root of most accidents and incidents.” Traditionally, pilot training has concentrated mainly on the development of technical skills and on the performance of the individual pilot. Indeed, both researchers and practitioners2–4 suggest that more emphasis should be placed on the performance of the crew as a team and on factors that affect crew coordination and teamwork. They point out that team skills and the principles of crew resource management should be introduced earlier in training, continuously reinforced, and reviewed during flight training. Johnston3 stresses that “if we want pilots to perform as a crew—as team members—we should train them as a crew throughout.” The same situations exist in medicine. In health care, team errors are found in all settings in which care is delivered and engage all categories of health care workers. Errors in health care that compromise patient safety can be tied to latent failures embedded in the structure and function of systems.
Kohn et al1 recommended that the health care industry look to other high-reliability industries for guidance on improving patient safety. One of the specific recommendations called forth in this report was the widespread adoption of Crew Resource Management (CRM) training from commercial aviation. Often referred to as team training or human-factors training, CRM training refers to a family of instructional strategies that are designed to prevent breakdowns in team leadership, communication, and decision making.5–7 Previous research8–9 suggests that CRM training improves attitudes about the importance of teamwork and its effects on safety, the acquisition of factual knowledge concerning effective teamwork strategies, and team performance during simulated flights. Over the past few years, several papers10–14 have been written that purportedly describe “the aviation model” of CRM training and its potential applications in health care. However, what has been missing is a model of teamwork that is focused on the needs of health care professionals, adapted to the work flow of health care professionals, and tailored to health care's unique professional culture.
In the report “Five Years After To Err Is Human,”15 it was noted that “the combination of complexity, professional fragmentation, and a tradition of individualism, enhanced by a well-entrenched hierarchical authority structure and diffuse accountability, forms a daunting barrier to creating the habits and beliefs of common purpose, teamwork, and individual accountability for successful interdependence that a safe culture requires.” Training physicians, nurses, and other professionals to work in teams is a concept that has been promoted by many patient-safety experts. It requires integrating the specific health care team competencies with the technical skills required by the given profession, in a curriculum that allows validation of skills as the health care professionals learn. The training should emphasize team concepts early in a health care professional's career and promote the concept of the team, rather than individuals, caring for patients. This paper will discuss the first step in this process: the identification of health care team skills and roles.
Research Study
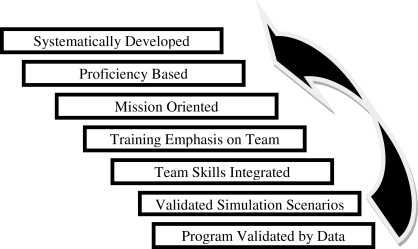
Health care lags behind other high-risk industries in expanding its focus from individual performance to group or team performance, thereby leaving practitioners inadequately prepared to enter complex settings. Several risk assessments have indicated a need for simulation tools integrated into health care professional evaluations in order to understand errors and improve performance by mitigating the effects of errors. This project has applied a series of research concepts originally developed in the airline Advanced Qualification Program (AQP), shown in the figure, and transferred and validated them in a health care setting through a grant funded by the Michigan Economic Development Corporation to use a unique application of the in situ simulation.
Figure.
The Advanced Qualification Program Philosophy
The airline industry was at an interesting point in the development of team training in the late 1980s. Most airlines had been training using a CRM model for more than 10 years. However, the safety data did not indicate improvements in team performance when safety measures in flight were considered. Although everyone understood the importance of team skills, the skills had not been integrated into the actual work environment of the aircraft, and there was no assessment of performance. From the vast research on teams/team functioning, links had to be established between the different roles on the flight team, and the methodology of assessment had to be established. An approach to the use of simulation was needed that was completely different than the traditional model of a repetitive practice of a technical skill in a high-fidelity simulator by aviation professionals. The industry needed a new simulation design in which the focus was on scenario development that would trigger team responses that could be measured quantitatively. It was not until these simulations were created that we truly understood what our team challenges were, so that we could identify and train the appropriate team skills and assess the performance change. The methodology to design, train, and assess team skills in this manner was AQP.
Goals of AQP
The primary goal of AQP is to achieve the highest possible standard of individual and crew performance. In order to achieve this goal, AQP functions to reduce the probability of crew-related errors by aligning training and evaluation requirements more closely with the known causes of human error. For example these crew-related errors:
Crew performance. Most accidents are attributed to crew error. Traditional training programs focus on individual training and evaluation. Under AQP, the focus is on crew and individual performance in both training and evaluation.
Crew Resource Management. Most accidents are caused by errors of judgment, communication, and crew coordination. Traditional training programs focus primarily on flying skills and systems knowledge. Under AQP, competence in flying skills and systems knowledge are integrated with CRM skills in training and evaluation throughout the curriculum.
Scenario-based training and evaluation. Most accidents are caused by a chain of errors that build up over the course of a flight and which, if undetected or unresolved, result in a final, fatal error. Traditional training programs, with their maneuver-based training and evaluation, artificially segment simulation events in such a way as to prevent the realistic buildup of the error chain. Under AQP, both training and evaluation are scenario-based, simulating more closely the actual flight conditions known to cause most fatal carrier accidents.
Additional benefits that are expected for individual applicants will vary but may include the following:
the ability to modify training curricula, media, and intervals
crew evaluation as well as individual assessment
improved standardization across fleets and flight personnel
shift from programmed hours to proficiency-based training
access to innovative training ideas and research
opportunity to achieve more efficient training
The key element of design and focus for our metrics is the event set design.
The complete set of proficiency objectives defines the end result of training: the task activities the team must be able to perform, the set of conditions under which they must be able to perform them, the performance standards that must be met, and the evaluation strategy that will be used to determine proficiency. The objectives do not, however, describe the specific training situations and activities that will be used to achieve this end result, especially in terms of flight training. One means for specifying the flight training situations to be included in a curriculum is by means of events. The suggestion that flight training and testing activities should be developed around a set of events was formalized in 1994 by an industry group tasked to recommend a systematic approach for developing line operational simulation scenarios under AQP. The event set methodology has achieved wide acceptance because of its analytical approach to scenario design and its reinforcement of the use of realistic line conditions that enable crews to practice the full range of flight-management skills. The effectiveness of the event set methodology for integrating technical and CRM training objectives suggests that an event orientation throughout the curriculum, rather than only in line operational flight training or line operational evaluation, could offer important advantages.
Transfer to Health Care Teams
This research has performed the same analysis of health care teams in their operational environment. The next phase of research is the training and maintenance of team skills for health care professionals. This will include simulation-curriculum design that will benefit from science-based behavioral markers and role definition, developed in this study, that are associated with effective team member performance and from which instructional programs can be reverse engineered.
The focus of our research was to define a team model that will function in the operational environment in which health care professionals work. We used the AQP process to link the highest-rated skills in the event set with the highest-rated overall performance to create a functional team model for health care professionals. In the past 3 years we have designed simulations, validated event sets that trigger team dynamics, established metrics, performed inter-rater reliability training, and had independent multidisciplinary health care teams analyze over 300 hours of videos of health care professionals performing in several different disciplines. In addition, we have performed simulations across the United States in 70- to 1000-bed hospitals, and we have performed them during the day and in the middle of the night. What follows is the process of our analysis and results from this work.
Validation of Critical Team Skills, Part 1 (Simulation Participant Input)
As noted at the beginning of this paper, we were deeply skeptical about the extent to which aviation-derived CRM training content could be directly translated to health care without substantial modification. This initial level of skepticism was heightened during a series of discussions with high-level health care practitioners and administrators—several of whom had been involved with CRM-derived medical-team training programs in their own hospitals—who had commented that previous training efforts, although well intentioned, had failed to address their unique operational challenges.
With this in mind, we decided to compile our own profile of health care team skills, using an AQP-inspired approach. We first looked to the published literature16–19 on CRM training to identify aviation- and health care–relevant team skills that had been identified by other researchers. Additional skills were also identified through direct observations of intact health care teams performing in situ simulations,20 along with recommendations that had been submitted from professional colleagues. From this corpus of data, we formed a functional grouping of teamwork skills that, in our opinion, appeared to be associated with safe patient care and could potentially differentiate highly effective health care teams from less effective ones.
After compiling this initial list of teamwork skills, we solicited feedback about their relevance to overall team performance from our simulation participants. For each simulation, the health care team typically consisted of:
2 or 3 doctors (depending on scenario)
3 or 4 nurses (depending on scenario)
Pharmacist
Respiratory therapist
Blood bank and lab technicians
Admissions staff
Imaging (x-ray and computed tomography) staff
Each group for the debriefing consisted of 15 to 20 health care professionals.
Specifically, we asked for their opinion about the extent to which each teamwork skill is relevant to maintaining a high level of team performance, regardless of whether or not their team had actually performed that skill during the simulation. These ratings were made by the entire cadre of simulation participants, which included physicians, anesthesiologists, nurses, technicians, pharmacists, and other direct-care staff (n = 264), during the course of 26 simulations conducted between 2006 and 2007. All ratings were made on a 5-point Likert scale, with anchors ranging from negatively impact patient care (1) to positively impact patient care (5).
Because many of our simulation participants had no prior exposure to human factors or teamwork training of any kind, they immediately realized the importance of teamwork in reducing errors and improving patient safety. The mean importance rating across all of the teamwork skills was high (mean = 4.24, range 3.27 to 4.61). Not unexpectedly, the means for physicians (4.10) and nursing staff (4.33) were very similar. The lesson learned here is that our simulation participants recognized the importance of effective teamwork in health care, even if they did not personally display these behaviors. Moreover, the high level of range restriction from the questionnaire responses suggested that the simulation participants were unable to clearly specify the most critical skills. In their opinion, all teamwork skills were of roughly equal importance.
Validation of Critical Team Skills, Part 2 (Subject Matter Expert Input)
These results presented the research team with a conundrum. Under AQP, training designers use trainee input as part of their needs assessment process to help select and organize the most critical training content. However, the questionnaire data provided little information to help us “down-select” the most critical skills. At the same time, there was some degree of redundancy among several skills and skill categories, at least from a conceptual and definitional perspective. This was inevitable because our initial profile of teamwork skills was drawn from existing training programs. The research team needed some way to cull and reorganize the list of teamwork skills before we could begin developing our team-training curriculum.
Therefore, we undertook a data reduction exercise to down-select the most critical skills per simulation event. Our intention was that once we had selected the most critical skills per event, we could then better train those specific skills given known resource constraints such as time, cost, and access to trainees. For this exercise, we began by indentifying 6 generic or “archetype” training-scenario events that our research team had successfully replicated across a number of simulations, including labor and delivery, emergency medicine, and cardiac care:
Event 1. Patient presents to health care team; more than one qualified health care professional in room.
Event 2. Patient's condition changes, requiring team member changes and external resources.
Event 3. Team expands with the arrival of new team members as a result of change in patient condition.
Event 4. Patient condition changes, requiring critical decisions and implementation of plans; more than one qualified decision maker in room.
Event 5. New team forms in a different setting to perform complicated procedure because of the patient's changed condition.
Event 6. Change in goals for patient because of change in conditions; more than one qualified decision maker in the room.
The down-selection process was completed during a group consensus exercise that involved the project's principal investigator (MD, PhD) along with 4 other research team members (1 MD, 2 PhD, and 1 MPA). Several criteria were used to down-select the critical skills, including the skills' mean importance rating (from the participant questionnaire, described earlier) and consensus ratings about each skill's degree of observability and diagnosticity within each event set. Observability and diagnosticity scores were rated as either “low” or “high.” Once all the data had been compiled, the team selected 6 skills for each scenario event that were the most relevant to team performance during each training-scenario event, readily observable by an independent rater, and diagnostic of overall team success or failure. We specifically limited ourselves to no more than 6 critical behaviors per simulation event. This was done to avoid overloading the raters during the subsequent assessment exercise, because previous research21 demonstrates that observer-based assessments impose tremendous cognitive demands on the rater. Several of these skills were identified as critical in multiple training scenarios.
Validation of Critical Team Skills, Part 3 (Trained Observer Ratings)
After having down-selected the most critical teamwork skills for each of the 6 archetype training-scenario events, we sought to establish an empirical correlation between the critical teamwork skills and relevant outcome variables. For this effort, 2 teams of researchers were organized. The first team was called the “skill measurement rating team.” This team included 5 behavioral scientists (1 PhD, 1 MPA, and 3 MA candidates) along with 2 clinicians (2 RN) who were tasked with watching digital videos of 10 in situ simulations and independently assessing each team's performance using the previously identified skills. To reduce the complexity of the rating task, each video was clearly segmented into the 6 training-scenario events and labeled accordingly. This was done so that the raters would know exactly when one scenario event ended and the next began. Prior to beginning the rating task proper, we conducted a rater calibration exercise to ensure that all team members were using the rating form appropriately and consistently. Raters were given the opportunity to watch each video as many times as they liked; however, most raters watched each video segment only once or twice. After each rater had completed his or her individual ratings, we calculated mean ratings (across all 7 raters) for each teamwork skill within each training-scenario event. This was done to offset any systematic biases among raters that could not otherwise be offset by the rater calibration exercise.
Concurrently, we also organized an “outcome measures rating team.” This team included 4 clinicians (2 MD and 2 RN) who were required to watch the same 10 in situ simulation videos. For each training-scenario event, the raters independently assessed the team's overall performance on all 3 generic criteria: team functioning, leadership effectiveness, and patient safety. For example, patient safety was identified by:
Event set design containing critical patient information that should be transferred from event set to event set. For example, during the door to cardiac catheterization ST-segment Elevated Myocardial Infarction (STEMI) simulation, critical information was presented to the emergency medical services team responding to the 9-1-1 call in the hotel. How much of this critical information made it to the cardiologist after 2 handovers (emergency medical services to emergency department, and emergency department to cardiac catheterization lab)?
Time for critical supplies to reach the patient. For example, in some simulations of obstetrician emergency caesarean sections in which 2 liters of blood was lost in the patient, we observed a range of blood never reaching the patient because of dysfunctional teams to teams that had blood in the operating room (OR) in 10 minutes or less.
Time from critical decisions of care being made to procedure actually being performed.
As with the skills measurement rating team, the outcome measures rating team watched labeled video segments so that they would know exactly when one scenario event ended and the next began. They also received a similar rater calibration training exercise to ensure that all team members were using the rating form appropriately and consistently. Finally, after each rater had completed his or her individual ratings, we again calculated mean ratings (across all 4 raters) for team outcome measures within each training-scenario event to offset any systematic biases among raters that could not be controlled for by the rater calibration exercise. The raters observed event sets (on video) that had established standards and received feedback on their rating against the standard. The training continued over several event sets until the raters achieved agreement with the standard.
At the end of this rating exercise, our research team had 2 sets of independently generated data for each training scenario event: the mean teamwork rating for 6 critical skills and the mean team outcome rating for the 3 outcome measures. Given the relatively large number of data points, we decided to average the 3 outcome measures within each training-scenario event (the average correlation among them was r = 0.70) and use this as a composite outcome variable. With a few minor exceptions, the teamwork behaviors were strongly and positively correlated with the composite outcome measure. Several of the skill-outcome correlations exceeded r = 0.50, and some even exceeded r = 0.70. The data suggest that, at least among this limited sample of health care teams, teamwork skills are in fact positively correlated with relevant outcomes. Of the teamwork skills that were assessed, 12 repeatedly demonstrated high correlations with the team outcomes across the 6 simulation events:
Announce plans and seek confirmation or consultation
Communicate clearly what is needed from outside departments
Follow up until need has been met
Assign and reassign tasks to personnel
Update patient on changing conditions
Announce significant changes in patient status
Verbalize potential threats and risks
Brief team on situation and goals
State directions clearly and using commonly understood language
Ask for patient and family information/input
Request clarification of ambiguous answers
Explain treatment plans and rationale and seek consent
Thus scenarios with specific event set designs were used to link the highest-performing team skills with the highest outcomes for patient care.
Validation of Critical Team Skills, Part 4 (Changes in Organizational Culture)
At one of our partner hospitals, we have also begun to empirically assess the effects of in situ simulation on organizational culture. This study involved assessing changes in teamwork climate, as measured by Sexton's23 Safety Attitudes Questionnaire, over a 6-week period. A total of 83 participants were recruited for this study. Of these, 46 were from the OR department and 57 were from the intensive care unit (20 participants held dual positions in the OR department and intensive care unit and completed both sets of surveys). Of the 83 participants, 45 were in the experimental condition (participated in in situ simulation), and the remaining 38 were in the control condition (did not participate in in situ simulation). Teamwork climate was measured at 3 times: at baseline, 1 week after the in situ simulation, and again 6 weeks after the in situ simulation. At baseline, there were no differences between the participants in the experimental and control groups in either the OR department (z = −0.033; P = .973) or the intensive care unit (z = −0.268; P = .789).22
For the OR department, the percentage of respondents reporting good teamwork climate increased for both groups. The average favorable percentage was 52% at baseline, 60% at 1 week, and 67% at 6 weeks. There were no statistically significant differences between the experimental and control groups. The findings from the descriptive statistics were confirmed by a repeated measures analysis of variance. The results were not statistically significant for group membership (F1,42 = 0.096; P = .758) but were statistically significant for time (F2,84 = 3.704; P = .029). Moreover, the interaction effect of group membership by time (F2,84 = 0.355; P = .702) was also not statistically significant.22
Follow-up interviews suggest that the main effect of time was due to a “spillover effect,” in which several of the control group members surreptitiously were able to watch the experimental group's performance and experience the simulation's effects vicariously. When asked about this, one of the control group nurses responded, “There was so much excitement in the air, and we couldn't stand not being a part of it.” She further stated, “It was killing us not to be able to jump in and help out our colleagues like we would on any other emergency.” Therefore, it is likely that this spillover effect of the simulation contributed to the increased teamwork climate among both the experimental and control groups.22
Training Design and Development
While the teams on videotape were observed, it became immediately clear that the most effective teams seemed to self-organize into 3 different roles. The first role was that of the team leader, who was ultimately responsible for the patient's safety and welfare. This individual—typically the doctor, surgeon, anesthesiologist, or primary nurse in charge—had the primary duty of assigning roles and delegating tasks to the rest of the staff, along with performing his or her own clinical duties. The second role tended to be that of a team resource coordinator. This individual—typically a senior member of the nursing staff—had some clinical responsibilities but spent much of his or her time maintaining situational awareness about the big picture and making sure that critical tasks were performed as directed by the leader. The third role tended to be the team member/direct care provider; these individuals' primary responsibilities were to perform their unique clinical duties and effectively communicate the status of those duties to the resource coordinator and team leader.
The identification of team roles and linking team skills to these roles are critical components of team training. In today's world, health care professionals perceive themselves and their colleagues as working in a chaotic sea of health care. When they join a team, it is as an individual. To change this is critical for any team model to work, dependent on the subculture of the health care organization, and absolutely essential for effective teamwork. The roles must be defined in the subculture, assigned by some methodology to health care professionals, and practiced so that team skills are integrated into their technical skill set. A formal training evaluation is currently underway. When complete, it will use a classic experimental design with a total of 20 intact health care teams, half of whom receive the training intervention. All teams will complete 2 in situ simulations. Performance will be assessed both within teams (gain scores from simulation 1 to simulation 2) and across teams (between the trained and untrained groups). This work is expected to occupy our time well into 2010.
Limitations and Strengths of the Study
Lack of potential generalizability is a limitation because the study took place in only a few disciplines within health care. The small numbers of clinicians involved is an additional limitation to the statistical power of the results, but this could be overcome through expansion of the study. The resource-intensive nature of the methods may be another significant limitation to wide adoption of the in situ simulation approach. However, the strength of the potential benefits from in situ simulation, through improved communication, teamwork, and ongoing assessment of related microsystem risks, provides a compelling counterbalance to this limitation.
Summary
Using the AQP-inspired approach, we have been able to reverse engineer a model for a health care team, using a detailed event set design and performance metrics of health care teams in their operational environment. Using this model, we have demonstrated significant improvement in team performance when health care teams exhibit these teamwork skills. This model can now be integrated into health care education, expanded, and modified as new team challenges are identified. Most importantly, common critical roles were identified that become the focus for team skills performance, which can be modified by the subcultures within the health care organization. It truly becomes a model designed in health care for health care professionals.
Most health care is performed in teams; however, we train as individuals in today's world of health care education. Why not move team training back into medical school, nursing school, and allied health to allow team roles and skills knowledge and practice in cross-disciplinary teams?
Simulation is an effective tool to reinforce technical and team skills in a safe environment. Why are so many basic skills learned on patients rather than in simulation? In the future, health care education should be a continuum of phased validations in which students train to proficiency in simulation before patient contact. A first-year surgery resident will learn knot tying, basic sterile technique, and roles/team skills in simulation prior to that first day in the OR.
The “aviation model,” as it has been frequently described by others, is unlikely to be effective in health care. By its very nature, health care is much less-proceduralized than flying an aircraft; there are many fewer standard operating procedures and checklists to ensure safe performance. Moreover, health care teams are substantially more heterogeneous than pilot crews. Health care teams include representatives from many fields—doctors, nurses, anesthesiologists, technicians, and the like—each with their own sets of skills, areas of expertise, and professional vocabulary. Furthermore, the composition of such teams is highly dynamic. Physicians come and go throughout the day, and nurses rotate during regularly scheduled shift changes. However, by using the AQP-inspired in situ simulation technique, we have been able to better understand the challenges facing health care teams. The results of this study suggest a role-based (team leader, team resource coordinator, team member/direct care provider) approach to training, which not only fits the clinical work flow but which we believe can be applied across a wide range of health care settings, from large university hospitals to small regional hospitals to outpatient surgical centers.
Acknowledgments
The Center of Excellence for Simulation Research grant is a collaborative effort involving Western Michigan University, Michigan State University School of Medicine Kalamazoo Center for Medical Studies, and numerous patient-safety leaders throughout the United States. Our team's research has been generously funded by the Michigan Economic Development Corporation Michigan Technology Tri-Corridor Fund.
Footnotes
William R. Hamman, MD PhD, is Director of Medical Simulation and Research at the Center of Excellence for Simulation Education and Research, William Beaumont Hospitals, and a research scientist at Western Michigan University; Jeffrey M. Beaubien, PhD, is an Industrial and Organizational Psychologist at Aptima, Inc; and Beth M. Beaudin-Seiler, MPA, is a Research Associate at Western Michigan University
Editor's note: The online version of this article contains an initial profile (30.5KB, doc) of health care team skills, an example outcomes rating worksheet (25KB, doc) , an example teamwork skills rating worksheet (111.5KB, doc) , and teamwork skill-outcome measure correlations (52KB, doc) .
References
- 1.Kohn L. T., Corrigan J. M., Donaldson M. S. To Err Is Human. Washington, DC: National Academy Press; 1999. [Google Scholar]
- 2.Hackman R. J. Teams, leaders, and organizations: new directions for creworiented flight training. In: Wiener E., Kanki B., Helmreich R., editors. Cockpit Resource Management. San Diego, CA: Academic Press; 1993. pp. 47–70. [Google Scholar]
- 3.Johnston N. Intergrating human factors training into ab initio airline pilot curricula. ICAO J. 1993;48:14–17. [Google Scholar]
- 4.Diehl A. E. Cockpit decision making. FAA Aviat Safety J. 1991;1:14–16. [Google Scholar]
- 5.Federal Aviation Administration. Crew Resource Management Training. Washington, DC: US Dept of Transportation; 2004. Advisor circular 120-51E. [Google Scholar]
- 6.Helmreich R., Merritt A., Wilhelm J. The evolution of crew resource management training in commercial aviation. Int J Aviat Psychol. 1999;9:19–32. doi: 10.1207/s15327108ijap0901_2. [DOI] [PubMed] [Google Scholar]
- 7.Salas E., Rhodenizer L., Bowers C. The design and delivery of crew resource management training: exploiting available resources. Hum Factors. 2000;42:490–511. doi: 10.1518/001872000779698196. [DOI] [PubMed] [Google Scholar]
- 8.Salas E., Burke C., Bowers C., Wilson K. Team training in the skies: does crew resource management (CRM) training work? Hum Factors. 2001;43:641–674. doi: 10.1518/001872001775870386. [DOI] [PubMed] [Google Scholar]
- 9.Salas E., Wilson K., Burke C., Wightman D. Does crew resource management training work? An update, an extension, and some critical needs. Hum Factors. 2006;48:392–412. doi: 10.1518/001872006777724444. [DOI] [PubMed] [Google Scholar]
- 10.Helmreich R., Merritt A. Culture at Work in Aviation and Medicine: National, Organizational, and Professional Influences. Brookfield, VT: Ashgate; 1998. [Google Scholar]
- 11.Musson D., Helmreich R. Team training and resource management in health care: current issues and future directions. Harvard Health Policy Rev. 2004;5:25–35. [Google Scholar]
- 12.Pizzi L., Goldfarb N., Nash D. Crew resource management and its applications in medicine. In: Shojana K., Duncan B., McDonald K., Wachter R., editors. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Rockville, MD: Agency for Healthcare Research and Quality; 2001. pp. 501–510. [Google Scholar]
- 13.Thomas E., Helmreich R. Will airline safety models work in aviation. In: Rosenthal M., Sutcliffe K., editors. Medical Error: What Do We know? What Do We Do. San Francisco, CA: Jossey-Bass; 2002. pp. 217–234. [Google Scholar]
- 14.Uhlig P., Haan C., Nason A., Niemann P., Camelio A., Brown J. Improving patient care by the application of theory and practice from the aviation safety community. In: Jensen R., editor. Proceedings of the 11th International Symposium on Aviation Psychology. Columbus, OH: Ohio State University Press; 2001. [Google Scholar]
- 15.Leape L., Berwick D. Five years after To Err Is Human: what have we learned? JAMA. 2005;293:2384–2390. doi: 10.1001/jama.293.19.2384. [DOI] [PubMed] [Google Scholar]
- 16.Alonso A., Baker D., Holtzman A. Reducing medical error in the military health system: how can team training help? Hum Resource Manage Rev. 2006;16:396–415. [Google Scholar]
- 17.Cannon-Bowers J., Salas E. Teamwork competencies: the interaction of team member knowledge, skills, and attitudes. In: O'Neil H. Jr, editor. Workforce Readiness: Competencies and Assessment. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 1997. pp. 151–174. [Google Scholar]
- 18.Helmreich R., Butler R., Taggart W., Wilhelm J. The NASA/University of Texas/FAA Line/LOS Checklist: A Behavioral Marker-Based Checklist for CRM Skills Assessment. Houston, TX: University of Texas Aerospace Crew Research Project; 1995. Technical report no. 94-02. [Google Scholar]
- 19.Morey J. C., Simon R., Jay G. D. Error reduction and performance improvement in the emergency department through formal teamwork training: the MedTeams project. Health Serv Res. 2002;37:1553–1581. doi: 10.1111/1475-6773.01104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamman W. R., Rutherford W., Fuqua W. In-situ simulation: moving simulation to new levels of realism within healthcare organizations. In: Patankar M., Ma M., editors. Proceedings of the 3rd Safety Across High Consequence Industries Conference. Vol 1. Vol. 1. St. Louis, MO: St. Louis University Press; 2007. pp. 64–74. In: [Google Scholar]
- 21.Beaubien J., Baker D., Salvaggio A. Improving the construct validity of line operational simulation (LOS) ratings: lessons learned from the assessment center. Int J Aviat Psychol. 2004;14:1–17. [Google Scholar]
- 22.Jones D. Creating a Culture of Safety: The Influence of Medical Simulation on Attitudes of Surgical Team Members [dissertation] Kalamazoo, MI: Western Michigan University; 2007. [Google Scholar]
- 19.Sexton J., Thomas E., Helmreich R. Error, stress, and teamwork in medicine and aviation: cross sectional surveys. British Medical Journal. 2000;320:745–749. doi: 10.1136/bmj.320.7237.745. [DOI] [PMC free article] [PubMed] [Google Scholar]