Abstract
Context
Post-traumatic stress disorder (PTSD) is highly prevalent among veterans because of combat and may impair cognition.
Objective
To determine whether PTSD is associated with the risk of developing dementia among older US veterans receiving treatment in Department of Veterans Affairs medical centers.
Design
A stratified, retrospective cohort study conducted using the Department of Veterans Affairs National Patient Care Database.
Setting
Department of Veterans Affairs medical centers in the United States.
Participants
A total of 181,093 veterans 55 years or older without dementia from fiscal years 1997 through 2000 (53,155 veterans with and 127,938 veterans without PTSD).
Main Outcome Measures
During the follow-up period between October 1, 2000, and December 31, 2007, 31,107 (17.2%) veterans were ascertained to have newly diagnosed dementia according to International Classification of Diseases, Ninth Revision, Clinical Modification codes.
Results
The mean baseline age of the veterans was 68.8 years, and174,806 (96.5%) were men. Veterans with PTSD had a 7-year cumulative incident dementia rate of 10.6% whereas those without had a rate of 6.6% (P<.001). With age as the time scale, Cox proportional hazards models indicated that patients with PTSD were more than twice as likely to develop incident dementia compared with those without PTSD (Hazard Ratio [HR] = 2.31, 95% Confidence Interval [CI] 2.24–2.39). After multivariable adjustment for demographics, medical and neuropsychiatric comorbidities, patients with PTSD were still more likely to develop dementia (HR = 1.77, 95% CI 1.70–1.85). Results were similar when we excluded those with a history of head injury, substance abuse, or clinical depression.
Conclusions
We found that in a predominantly male veteran cohort, those diagnosed as having PTSD were at a nearly 2-fold-higher risk of developing dementia compared with those without PTSD. Mechanisms linking these important disorders need to be identified with the hope of finding ways to reduce the increased risk of dementia associated with PTSD.
Background
Post-traumatic stress disorder (PTSD) is a common psychiatric syndrome associated with high rates of morbidity and mortality and is one of the most common sequelae in veterans returning from combat. Among veterans returning from Iraq and Afghanistan, the prevalence of PTSD has been estimated as 17%.1 In addition, PTSD can be a chronic condition. Vietnam veterans have been found to have a 20 to 30% lifetime prevalence of combat-related PTSD and 10 to 15% had the disorder 15 years or longer after returning from Vietnam.2, 3 A study of older World War II and Korean veterans found that the PTSD prevalence remained as high as 12% even 45 years after combat.4
Studies have previously found that PTSD is associated with greater health care utilization and an increased risk of developing a wide range of medical conditions in younger and middle-aged veterans.5–9 Despite evidence that PTSD may impair cognitive performance,10, 11 and that older individuals with PTSD have greater decline in cognitive performance relative to control patients,12 little is known about PTSD as a risk factor for developing dementia. Given that PTSD symptoms often continue until late in life and that alterations in the hypothalamic-pituitary-adrenal axis often accompany PTSD13 and these in turn may be associated with dementia,14 there is reason to believe that PTSD might be associated with accelerated brain aging. Another possible mechanism that may link PTSD to higher rates of dementia is the co-occurrence of depression, head injury, or medical comorbidities, conditions all associated with both PTSD and dementia.15–17 No studies to date have determined if PTSD is independently associated with an increased risk of developing dementia.
The goal of our study was to determine whether PTSD was associated with an increased risk of being diagnosed as having dementia among veterans using Department of Veterans Affairs (VA) health care services in the United States. In addition, we were interested in whether such an association might be explained by medical comorbidities, depression or head injury.
METHODS
Data and Study Participants
Data for this retrospective cohort study were obtained from the VA National Patient Care Database, which captures all inpatient and outpatient services within the VA each fiscal year (October 1 through September 30). Records were extracted for veterans 55 years and older who had been treated at a VA health care facility and did not have a diagnosis of dementia during our baseline period, fiscal years 1997 through 2000, and who also had at least one visit during our follow-up period from fiscal year 2001 (October 1, 2000) to the end of the calendar year 2007.
There were 3,120,213 veterans seen at a VA facility at least once during the 1997 to 2000 fiscal years who were 55 to 100 years of age at the time of their first encounter. We excluded the 170,378 (5.5%) who had received a dementia diagnosis at the VA during this period. Among the remaining 2,949,835 veterans, we identified 59,633 (2.0%) as having received a PTSD diagnosis at least twice during the baseline period, all of whom were included in our potential cohort. The rest of the potential cohort was a group of 178,899 randomly selected veterans (3 per patient with PTSD) without a PTSD diagnosis.
Among the 238,532 patients with and without PTSD selected as potential participants, we excluded the 26,311 (11.0%) who died during the baseline period and the 31,128 (13.1%) who were not seen at a VA health care facility during the follow-up period because we did not have the ability to determine whether they had developed incident dementia. Thus, our final cohort of 181,093 veterans consisted of 53,155 patients with and 127,938 patients without PTSD.
Outcome Measures
Posttraumatic Stress Disorder
Veterans with PTSD were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)18 codes recorded in the VA database. To be conservative, those with a diagnosis code of 309.81 (PTSD) on at least two different visits during the baseline period were classified as having PTSD. Veterans with one diagnosis of PTSD were not included in our primary analyses (combined total=88,568 veterans).
Dementia
Veterans with dementia were identified using ICD-9-CM codes during the baseline period to exclude prevalent cases, and during the follow-up to identify incident cases. Patients with diagnosis codes 290.0, 290.2, 290.3, 331.2 (senile dementias, n=3,450), 290.4 (vascular dementia, n=2,698), 294.8 (dementia not otherwise specified, n=10,291), 331.0 (Alzheimer disease, n=3,882), 331.1 (frontotemporal dementia, n=139), and 331.82 (Lewy Body dementia, n=356) were considered to have dementia diagnoses.
Evaluation of incident dementia diagnosis occurred between October 1, 2000 through December 31, 2007. If dementia was not diagnosed before the patient’s death or the end of the follow-up period, the patient’s data was censored at whichever event occurred first. Dates of death were obtained through the VA Vital Status File, which combines death data from the VA, the Center for Medicare and Medicaid Services, and the Social Security Administration.19
Baseline characteristics
Baseline age in years was calculated on October 1, 2000. Sex and race/ethnicity information was also determined based on VA database records. We classified veterans as living in broad educational and income strata according to zip code tabulation areas (ZCTA) by linking our data to 2000 US census data. For educational level, veterans were categorized according to whether they were living in a ZCTA where ≤25% versus >25% of the adult population had completed a college education (bachelor’s degree or higher). This cutoff was chosen because the average ZCTA in 2000 had a 24.4% college-educated adult population.20 For income, veterans were categorized in tertiles of median ZCTA income for adults <75 or ≥75 years old.
Indicators of prevalent medical comorbidity during the baseline period were obtained using ICD-9-CM diagnosis codes for hypertension, diabetes mellitus, myocardial infarction, cancer, and cerebrovascular disease. Psychiatric comorbidities were also determined using ICD-9-CM codes, including history of tobacco use, alcohol abuse, other substance abuse, major clinical depression, and head injury including concussion, contusion, skull fracture and other head injury (ICD-9-CM codes: 310.2; 800-804.xx; 850.x; 851.x; 854.0; 854.1; 959.01). The Committee on Human Research at the University of California, San Francisco, the Committee for Research and Development at the San Francisco VA, and the Human Research Protection Office of the US Army Medical Research and Material Command approved the study.
Statistical Analyses
Baseline characteristics were summarized with means and standard deviations or percentages for the veterans with and without PTSD. The characteristics of the two groups were compared using t-tests for continuous variables and chi-square tests for categorical variables.
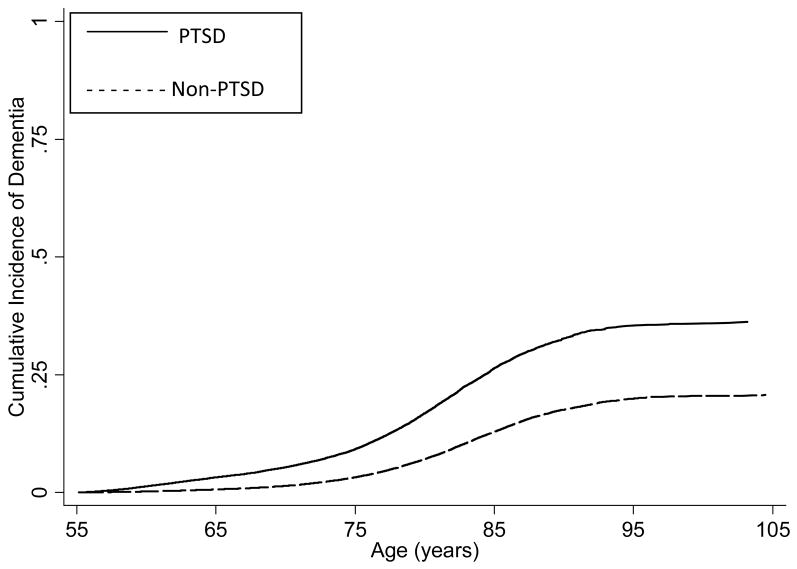
Cumulative incidence of dementia was plotted by patient age in years for each group. These curves show estimates of the cumulative incidence by age in the presence of death as a competing risk; with complete follow-up, this could be estimated by the simple proportion with a dementia diagnosis by any given age. This is in contrast to Kaplan-Meier curves, which estimate the incidence that would be observed if the competing risk could be “removed.” To determine whether the relative rates of incident dementia over time would be different for those without other major neuropsychiatric diagnoses, we also constructed cumulative incidence curves excluding those with diagnoses of major clinical depression, substance abuse, or head injury during the baseline period.
Cox proportional hazards models were used to compare the age in years of incident dementia in patients with and without PTSD. With age as the time-scale, the effects of age on incidence are flexibly modeled by the baseline hazard, which is non-parametric in the Cox model and need not even be estimated to obtain estimates of covariate effects. Several different adjusted Cox models were run to assess the influence of confounding by different types of baseline characteristics. First, models were adjusted for the demographic characteristics of race/ethnicity, sex, and educational and income strata. Second, the models were adjusted for indicators of medical comorbidity at baseline including hypertension, diabetes, myocardial infarction, and cerebrovascular disease followed by adjustments for neuropsychiatric comorbidities such as clinical depression, substance abuse and head injury. To assess the impact of differential opportunity for receiving dementia diagnoses by presence or absence of PTSD, we also ran models adjusting for a time-varying covariate for the number of inpatient or outpatient visits to a VA clinic per month. Proportional hazards assumptions were tested graphically and statistically and were met for all models. All analyses were conducted with Stata version 10.1 (StataCorp LP, College Station, TX) and SAS version 9.1 (SAS Institute Inc, Cary, NC).
RESULTS
Participant Characteristics
The mean (SD) baseline age of the 181,093 veterans in our cohort was 68.8 (8.6) years; 174,806 (96.5%) were men. Baseline characteristics of veterans are presented in Table 1. Compared with the patients without PTSD, those with PTSD were younger, had greater comorbidities and lived in zip codes with more college-educated and higher-income individuals, although the absolute differences were quite small. Substance abuse (P=.004), tobacco use (P=.009), major clinical depression (P=.001), and head injury (P=.009) were also statistically significantly more common among patients with than those without PTSD.
Table 1.
Baseline characteristics of the veterans with and without PTSD
| Characteristic | Study Group, No(%) |
|
|---|---|---|
| Non-PTSD (n=127,938) | PTSD (n=53,155) | |
| Age, mean ± sd (range), y | 69.9 ± 8.2 (55–100) | 66.2 ± 9.0 (55–100) |
| Female sex | 5,118 (4.0) | 1,169 (2.2) |
| > 25% college-educated ZCTA† | 37,358 (29.2) | 16,319 (30.7) |
| Median Income of ZCTA‡ | ||
| Low tertile (<$24.0K) | 41,708 (32.6) | 15,574 (29.3) |
| Middle tertile | 41,836 (32.7) | 17,275 (32.5) |
| High tertile (>$31.8K) | 39,661 (31.0) | 17,807 (33.5) |
| Hypertension | 74,460 (58.2) | 34,710 (65.3) |
| Diabetes | 30,321 (23.7) | 14,511 (27.3) |
| Myocardial infarct | 7,037 (5.5) | 4,146 (7.8) |
| Cerebrovascular disease | 11,898 (9.3) | 6,379 (12.0) |
| Cancer | 20,726 (16.2) | 10,897 (20.5) |
| Alcohol abuse | 4,606 (3.6) | 8,345 (15.7) |
| Other substance abuse | 14,841 (11.6) | 13,927 (26.2) |
| History of Tobacco use | 3,710 (2.9) | 1,860 (3.5) |
| Major depression | 4,222 (3.3) | 20,199 (38.0) |
| Head injury | 384 (0.3) | 478 (0.9) |
Abbreviations: PTSD, posttraumatic stress disorder; ZCTA, zip code tabulation area.
Data are presented as number (percentage) of veterans unless otherwise indicated. P-value by t-test for continuous variables and chi-square test for categorical variables was <.001 for all variables.
Zip Code Tabulation Area from the 2000 US Census. College-educated indicates completion of a bachelor’s degree or higher.
Median income levels are age-specific (<75 years and ≥75 years, calculated separately)
Incident Dementia
The median follow-up time for veterans with and without PTSD was 7.2 (range 0.1 to 7.4) years. Cumulative incidence rates of dementia were significantly higher for veterans with than those without PTSD. Those with PTSD had a 7-year cumulative incidence rate of 10.6% with incident dementia, whereas veterans without PTSD had a 7-year rate of 6.6% (P<.001). Incident dementia rates were higher for patients with PTSD throughout the follow-up period (Figure).
Figure.
Cumulative incidence of dementia by age for all veterans
Cox proportional hazards models using age as the time scale also show that patients with PTSD were more than twice as likely to develop incident dementia compared with those without PTSD (Hazard Ratio [HR] = 2.31, 95% Confidence Interval [CI] 2.24–2.39)(Table 2). After adjusting for the demographic variables of sex, race/ethnicity, educational level and income, results were similar (HR = 2.28, 95% CI 2.21–2.36). Adjustment for medical comorbidities at baseline also was not greatly influential but reduced the risk slightly (HR = 2.21, 95% CI 2.13–2.28).
Table 2.
Association between post-traumatic stress disorder (PTSD) and risk of dementia in multivariable-adjusted models.
| Adjustment Models | Study Group | HR (95% CI)† |
|---|---|---|
| Unadjusted | No PTSD | 1.00 (ref) |
| PTSD | 2.31 (2.24–2.39) | |
| Demographics | No PTSD | 1.00 (ref) |
| PTSD | 2.28 (2.21–2.36) | |
| Medical Comorbidities | No PTSD | 1.00 (ref) |
| PTSD | 2.21 (2.13–2.28) | |
| Neuropsychiatric Comorbidities | No PTSD | 1.00 (ref) |
| PTSD | 1.84 (1.76–1.91) | |
| All | No PTSD | 1.00 (ref) |
| PTSD | 1.77 (1.70–1.85) |
Abbreviations: CI, confidence interval; HR, hazard ratio; PTSD, posttraumatic stress disorder
Hazard ratio (HR) and 95% confidence interval (CI) were determined using age as the time scale.
Adjustment for other neuropsychiatric diagnoses reduced the strength of the association between PTSD and dementia, although those with PTSD were still more likely to develop incident dementia than those without (HR = 1.84, 95% CI 1.76–1.91). In the final multivariable-adjusted model adjusting for demographics, medical and neuropsychiatric comorbidities, patients with PTSD were still nearly twice as likely to develop incident dementia as those without (HR = 1.77, 95% CI 1.70–1.85).
We next determined if the association between PTSD and risk of dementia differed by dementia diagnosis subtype. The unadjusted HR ranged from 1.94 to 3.13, and multivariable adjusted HR ranged from 1.71 to 2.19 (Table 3). There was no consistent pattern other than that PTSD was associated with a higher risk of dementia among all dementia subtypes.
Table 3.
Association between post-traumatic stress disorder (PTSD) and risk of subtypes of dementia‡.
| Result | Study Group | Alzheimer Disease HR (95% CI)† | Frontotemporal Dementia HR (95% CI)† | Senile Dementia HR (95% CI)† | Vascular Dementia HR (95% CI)† | Lewy Body Dementia HR (95% CI)† | Dementia NOS HR (95% CI)† |
|---|---|---|---|---|---|---|---|
| N | All Veterans | 3882 | 139 | 3450 | 2698 | 356 | 10291 |
| Unadjusted model | No PTSD | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| PTSD | 1.94 (1.82–2.08) | 3.13 (2.25–4.37) | 2.57 (2.40–2.75) | 2.40 (2.22–2.59) | 2.41 (1.95–2.98) | 2.36 (2.27–2.46) | |
| Fully adjusted model | No PTSD | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| PTSD | 1.71 (1.58–1.85) | 2.19 (1.43–3.34) | 2.03 (1.87–2.20) | 1.69 (1.54–1.85) | 2.05 (1.59–2.62) | 1.80 (1.72–1.89) |
Abbreviations: CI, confidence interval; HR, hazard ratio; NOS, not otherwise specified; PTSD, posttraumatic stress disorder.
Hazard ratio (HR) and 95% confidence interval (CI) were determined using age as the time scale.
International Classification of Disease, Ninth Revision, Clinical Modification codes: 290.0, 290.2, 290.3, 331.2 (senile dementias); 290.4 (vascular dementia); 294.8 (dementia not otherwise specified); 331.0 (Alzheimer Disease); 331.1 (frontotemporal dementia); and 331.82 (Lewy Body dementia).
We conducted several sensitivity analyses. To determine whether those with PTSD were more likely to receive a diagnosis of dementia because of more frequent care at the VA (inpatient or outpatient), we adjusted for the number of visits to inpatient and outpatient clinics. The addition of adjustment for clinic visits did not appreciably change the model results but those with PTSD did have greater clinic visits (P<.001). To determine whether veterans with PTSD remained at an increased risk for developing dementia even in the absence of psychiatric comorbidities, we excluded veterans with a diagnosis of major clinical depression, substance abuse, or head injury (n=48,241) during the baseline period and found almost identical results. We also repeated our analyses excluding women veterans and including veterans with a diagnosis of PTSD at one or more visits (n=88,568), and our results were similar in both analyses. Finally, we determined whether veterans with PTSD had greater risk of developing dementia compared with veterans without PTSD psychiatric disorders and found an increased risk (adjusted HR =1.47; 95%CI 1.37–1.56).
Discussion
We found that among primarily male veterans, those diagnosed as having PTSD had nearly a two-fold increased risk of dementia compared to those without PTSD. This association remained after adjustment for important differences between those with and without PTSD such as demographics and medical and neuropsychiatric comorbidities.
There are several reasons why patients with PTSD may have an increased risk of developing dementia. One possibility is that PTSD is causally related to the development of dementia. There is some evidence, albeit controversial, that veterans with PTSD perform more poorly on cognitive tests.10–12, 21 This poorer performance on cognitive testing compared to those without PTSD could be a risk factor for development of dementia as those with worse function may have less cognitive reserve and be at higher risk for cognitive impairment.22
Another mechanism possibly linking PTSD to dementia is chronic stress. Stress may damage the hippocampus, a brain structure that is crucial for memory and learning. Indeed, we and others have previously found that PTSD is associated with decreased concentrations of the neuronal marker, N-acetyl aspartate (NAA), in the hippocampus.23 Others have found that veterans with PTSD have smaller hippocampal volumes, which are correlated with deficits in short-term memory performance.24 Smaller hippocampal volumes have been associated with poor cognitive function and increased risk of dementia in healthy elders.25 It is possible then that PTSD leads to hippocampal atrophy which in turn increases risk of cognitive deficits and dementia especially over a short-term follow-up or that a smaller hippocampus is a predisposition for both PTSD and dementia.
PTSD, as a stress-related disorder, also is associated with alterations in the hypothalamic-pituitary-adrenal (HPA) axis and pro-inflammatory cytokines. Acute stress produces increases in cortisol levels, and studies have found that hypercortisolemia is associated with increased risk of dementia.26 Veterans with chronic PTSD typically have reduced cortisol levels, which may reflect an allostatic down-regulation of the glucocorticoid system and may facilitate chronic inflammation.13 Several studies have demonstrated that PTSD is associated with pro-inflammatory immune alterations, including increased levels of cytokines,27 enhanced cellular immune responses28 and increased levels of C-reactive protein.29, 30 We have previously found that inflammation is associated with increased risk of cognitive decline.31 Several other related possible mechanisms include alterations in homocysteine level and other vascular risk factors, possibly due to medications, in the setting of PTSD.32, 33
Another explanation for the association is that dementia and PTSD co-occur more frequently together or that one condition may “unmask” the other. Indeed, there have been several case-series and case-reports that PTSD symptoms may worsen in veterans as they develop dementia or cognitive impairment.34–36 We doubt that this explains our findings as we excluded those veterans with PTSD and a diagnosis of dementia at baseline. In addition, we required a documented PTSD diagnosis on at least 2 visits to ensure a robust clinical diagnosis. Finally, it may be that having PTSD, or other chronic brain disorders, may predispose patients to developing dementia due to an increased nonspecific vulnerability, for example genetic vulnerabilities shared by both disorders or childhood environmental factors.37 It is possible that having PTSD, especially in patients followed by mental health practitioners, may bring more attention to other neuropsychiatric diagnoses such as dementia. We attempted to control for this possible detection bias by adjusting for number of VA visits and our results were not appreciably different.
We believe our study has several important strengths including a large number of veterans with and without PTSD who received care at a VA facility allowing for documentation of dementia diagnosis over several years. In addition, we have attempted to carefully adjust for possible confounding from medical and neuropsychiatric comorbidities. Finally, this study is the first, to our knowledge, to report that PTSD may increase risk of developing dementia. Several limitations of our study are also important to mention. The diagnoses of PTSD, dementia, medical and neuropsychiatric comorbidities were made on the basis of clinician ICD-9-CM codes, an insensitive assessment of symptoms compared with structured research diagnostic interviews and with some differences compared to Diagnostic and Statistical Manual of Mental Disorders-based criteria. Because of this, we were also unable to assess the possibility of any subclinical cases of PTSD or dementia and our data cannot be used to estimate the prevalence of PTSD in the older veteran population. In addition, our population included primarily male veterans followed by the VA system, and therefore, we need to determine whether our findings generalize to women and to those patients not cared for at VA medical centers.
The finding that PTSD is associated with a nearly doubling of risk of dementia has important public health, policy and biological implications. PTSD has emerged as a common sequela of combat and other trauma exposure and its course is often chronic leading to increased mortality and morbidity. As patients with PTSD age, these adverse health conditions usually increase in frequency and some have suggested that PTSD may accelerate the “aging process” in general.38 It is important that those with PTSD are treated, and further investigation is needed to see whether successful treatment of PTSD may reduce risk of adverse health outcomes, including dementia. In addition, it is critical to follow patients with PTSD, especially if they are of an advanced age, in order to screen for cognitive impairment. Finally, mechanisms linking PTSD and dementia need to be identified with the hope of finding ways to improve the care and outcomes of those patients with PTSD.
Acknowledgments
Funding Support: This study was funded by Department of Defense (W81XWH-05-2-0094 PI Yaffe); Dr. Yaffe was supported in part by AG031155 and an anonymous foundation.
Role of the Sponsor: Representatives of the Department of Defense approved the study design and Human Subjects Review.
Footnotes
Author Contributions: Dr. Yaffe had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Yaffe, Vittinghoff, Barnes.
Analysis and interpretation of data: Yaffe, Vittinghoff, Lindquist, Barnes, Covinsky, Neylan, Kluse, Marmar.
Drafting of the manuscript: Yaffe.
Critical revision of the manuscript for important intellectual content: Vittinghoff, Lindquist, Barnes, Covinsky, Neylan, Kluse, Marmar.
Statistical analysis: Yaffe, Vittinghoff, and Lindquist.
Obtained funding: Yaffe.
Administrative, technical, or material support: Yaffe.
Study supervision: Yaffe.
Financial Disclosure: Ms. Lindquist, Ms. Kluse, Dr. Barnes, and Dr. Covinsky report no actual or potential conflicts of interest. Dr. Yaffe reports having served as a consultant to Novartis, Inc. for reasons not related to the current project. Dr. Vittinghoff reports having received grant support from Zelos Therapeutics, Tethys Biosciences, and NPS Pharmaceuticals. Dr. Marmar reports having served as a consultant for Sanofi Aventis and Actelion. Dr. Neylan reports having served as a consultant for Actelion and Takeda, and receiving lecture fees from speaking at the invitation of the Chatham Institute and the Pri-Med Institute.
References
- 1.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 2.Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science. 2006;313(5789):979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kulka R, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam War Generation: Report of Findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel Publishers Inc; 1990. [Google Scholar]
- 4.Spiro A, 3rd, Schnurr PP, Aldwin CM. Combat-related posttraumatic stress disorder symptoms in older men. Psychol Aging. 1994;9(1):17–26. doi: 10.1037//0882-7974.9.1.17. [DOI] [PubMed] [Google Scholar]
- 5.Boscarino JA. Posttraumatic stress disorder and physical illness: results from clinical and epidemiologic studies. Ann N Y Acad Sci. 2004;1032:141–153. doi: 10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- 6.Drescher KD, Rosen CS, Burling TA, Foy DW. Causes of death among male veterans who received residential treatment for PTSD. J Trauma Stress. 2003;16(6):535–543. doi: 10.1023/B:JOTS.0000004076.62793.79. [DOI] [PubMed] [Google Scholar]
- 7.Hearst N, Newman TB, Hulley SB. Delayed effects of the military draft on mortality. A randomized natural experiment. N Engl J Med. 1986;314(10):620–624. doi: 10.1056/NEJM198603063141005. [DOI] [PubMed] [Google Scholar]
- 8.Schnurr PP, Spiro A, 3rd, Paris AH. Physician-diagnosed medical disorders in relation to PTSD symptoms in older male military veterans. Health Psychol. 2000;19(1):91–97. doi: 10.1037//0278-6133.19.1.91. [DOI] [PubMed] [Google Scholar]
- 9.Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, Stewart A, Schlenger WE, Wells KB. Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1997;154(12):1690–1695. doi: 10.1176/ajp.154.12.1690. [DOI] [PubMed] [Google Scholar]
- 10.Samuelson KW, Metzler TJ, Rothlind J, Choucroun G, Neylan TC, Lenoci M, Henn-Haase C, Weiner MW, Marmar CR. Neuropsychological functioning in posttraumatic stress disorder and alcohol abuse. Neuropsychology. 2006;20(6):716–726. doi: 10.1037/0894-4105.20.6.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF. Neuropsychological outcomes of army personnel following deployment of the Iraq war. JAMA. 2006;296(5):519–529. doi: 10.1001/jama.296.5.519. [DOI] [PubMed] [Google Scholar]
- 12.Yehuda R, Tischler L, Golier JA, Grossman R, Brand SR, Kaufman S, Harvey PD. Longitudinal assessment of cognitive performance in Holocaust survivors with and without PTSD. Biological Psychiatry. 2006;60(7):714–721. doi: 10.1016/j.biopsych.2006.03.069. [DOI] [PubMed] [Google Scholar]
- 13.Yehuda R. Post-traumatic stress disorder. N Engl J Med. 2002;346(2):108–114. doi: 10.1056/NEJMra012941. [DOI] [PubMed] [Google Scholar]
- 14.Herbert J, Goodyer IM, Grossman AB, Hastings MH, de Kloet ER, Lightman SL, Lupien SJ, Roozendaal B, Seckl JR. Do corticosteroids damage the brain? Journal of Neuroendocrinology. 2006;18:393–411. doi: 10.1111/j.1365-2826.2006.01429.x. [DOI] [PubMed] [Google Scholar]
- 15.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 16.Keane TM, Kaloupek DG. Comorbid psychiatric disorders in PTSD. Implications for research. Ann N Y Acad Sci. 1997;821:24–34. doi: 10.1111/j.1749-6632.1997.tb48266.x. [DOI] [PubMed] [Google Scholar]
- 17.Yaffe K, Blackwell T, Gore R, Sands L, Reus V, Browner WS. Depressive symptoms and cognitive decline in nondemented elderly women: a prospective study. Arch Gen Psychiatry. 1999;56(5):425–430. doi: 10.1001/archpsyc.56.5.425. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 19.United States Department of Veterans Affairs. [Accessed December 9, 2008];VA vital status files. http://www.virec.research.va.gov/DataSourcesName/VitalStatus/VitalStatus.htm.
- 20.Bauman KJ, Graf NL. Educational attainment: 2000: US Census 2000 brief. Washington DC: U.S. Census Bureau; 2003. pp. 1–11. [Google Scholar]
- 21.Bremner JD, Scott TM, Delaney RC, Southwick SM, Mason JW, Johnson DR, Innis RB, McCarthy G, Charney DS. Deficits in short-term memory in posttraumatic stress disorder. The American Journal of Psychiatry. 1993;150(7):1015–1019. doi: 10.1176/ajp.150.7.1015. [DOI] [PubMed] [Google Scholar]
- 22.Stern Y. Cognitive reserve and Alzheimer disease. Alzheimer Dis Assoc Disord. 2006;20(S2):S69–74. doi: 10.1097/00002093-200607001-00010. [DOI] [PubMed] [Google Scholar]
- 23.Schuff N, Neylan TC, Lenoci MA, Du AT, Weiss DS, Marmar CR, Weiner MW. Decreased hippocampal N-acetylaspartate in the absence of atrophy in posttraumatic stress disorder. Biol Psychiatry. 2001;50(12):952–959. doi: 10.1016/s0006-3223(01)01245-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bremner JD, Randall P, Scott TM, Bronen RA, Seibyl JP, Southwick SM, Delaney RC, McCarthy G, Charney DS, Innis RB. MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995;152(7):973–981. doi: 10.1176/ajp.152.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grundman M, Sencakova D, Jack CR, Jr, Petersen RC, Kim HT, Schultz A, Weiner MF, DeCarli C, DeKosky ST, van Dyck C, Thomas RG, Thal LJ. Brain MRI hippocampal volume and prediction of clinical status in a mild cognitive impairment trial. J Mol Neurosci. 2002 Aug–Oct;19(1–2):23–27. doi: 10.1007/s12031-002-0006-6. [DOI] [PubMed] [Google Scholar]
- 26.Swaab DF, Raadsheer FC, Endert E, Hofman MA, Kamphorst W, Ravid R. Increased cortisol levels in aging and Alzheimer’s disease in postmortem cerebrospinal fluid. J Neuroendocrinol. 1994;6(6):681–687. doi: 10.1111/j.1365-2826.1994.tb00635.x. [DOI] [PubMed] [Google Scholar]
- 27.Sutherland AG, Alexander DA, Hutchison JD. Disturbance of pro-inflammatory cytokines in post-traumatic psychopathology. Cytokine. 2003;24(5):219–225. doi: 10.1016/j.cyto.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 28.Altemus M, Cloitre M, Dhabhar FS. Enhanced cellular immune response in women with PTSD related to childhood abuse. Am J Psychiatry. 2003;160(9):1705–1707. doi: 10.1176/appi.ajp.160.9.1705. [DOI] [PubMed] [Google Scholar]
- 29.Miller RJ, Sutherland AG, Hutchison JD, Alexander DA. C-reactive protein and interleukin 6 receptor in post-traumatic stress disorder: a pilot study. Cytokine. 2001;13(4):253–255. doi: 10.1006/cyto.2000.0825. [DOI] [PubMed] [Google Scholar]
- 30.Spitzer C, Barnow S, Volzke H, Wallaschofski H, John U, Freyberger HJ, Lowe B, Grabe HJ. Association of posttraumatic stress disorder with low-grade elevation of C-reactive protein: Evidence from the general population. Journal of Psychiatric Research. 2010;44(1):15–21. doi: 10.1016/j.jpsychires.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 31.Yaffe K, Lindquist K, Penninx BW, Simonsick EM, Pahor M, Kritchevsky S, Launer L, Kuller L, Rubin S, Harris T. Inflammatory markers and cognition in well-functioning African-American and white elders. Neurology. 2003;61:76–80. doi: 10.1212/01.wnl.0000073620.42047.d7. [DOI] [PubMed] [Google Scholar]
- 32.Jendricko T, Vidovic A, Grubisic-Illic M, Romic Z, Kovacic Z, Kozaric-Kovacic D. Homocysteine and serum lipids concentration in male war veterans with posttraumatic stress disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(1):134–140. doi: 10.1016/j.pnpbp.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 33.Seshadri S, Beiser A, Selhub J, Jacques PF, Rosenberg IH, D’Agostino RB, Wilson PW, Wolf PA. Plasma homocysteine as a risk factor for dementia and Alzheimer’s disease. N Engl J Med. 2002;346(7):476–483. doi: 10.1056/NEJMoa011613. [DOI] [PubMed] [Google Scholar]
- 34.Hamilton JD, Workman RH., Jr Persistence of combat-related posttraumatic stress symptoms for 75 years. J Trauma Stress. 1998;11(4):763–768. doi: 10.1023/A:1024449517730. [DOI] [PubMed] [Google Scholar]
- 35.Johnston D. A series of cases of dementia presenting with PTSD symptoms in World War II combat veterans. J Am Geriatr Soc. 2000;48(1):70–72. doi: 10.1111/j.1532-5415.2000.tb03032.x. [DOI] [PubMed] [Google Scholar]
- 36.Mittal D, Torres R, Abashidze A, Jimerson N. Worsening of post-traumatic stress disorder symptoms with cognitive decline: case series. J Geriatr Psychiatry Neurol. 2001;14(1):17–20. doi: 10.1177/089198870101400105. [DOI] [PubMed] [Google Scholar]
- 37.Gilbertson MW, Paulus LA, Williston SK, Gurvits TV, Lasko NB, Pitman RK, Orr SP. Neurocognitive function in monozygotic twins discordant for combat exposure: Relationship to Posttraumatic Stress Disorder. J Abnorm Psychol. 2006;115(3):484–495. doi: 10.1037/0021-843X.115.3.484. [DOI] [PubMed] [Google Scholar]
- 38.Yehuda R, Golier JA, Harvey PD, Stavitsky K, Kaufman S, Grossman RA, Tischler L. Relationship between cortisol and age-related memory impairments in Holocaust survivors with PTSD. Psychoneuroendocrinology. 2005;30(7):678–687. doi: 10.1016/j.psyneuen.2005.02.007. [DOI] [PubMed] [Google Scholar]