Abstract
BACKGROUND
A randomized controlled trial was conducted to test the effects of hydration and applied muscle tensing on presyncopal reactions to blood donation. Both interventions are designed to prevent the decreases in blood pressure that can contribute to such reactions, but due to the distinct physiological mechanisms underlying their pressor responses it was hypothesized that a combined intervention would yield the greatest benefit.
STUDY DESIGN AND METHODS
Prior to blood donation, first- and second-time blood donors (Mean Age = 20.2 years, SD = 4.9) were randomly assigned to: 1) standard donation, 2) placebo (leg exercise prior to venipuncture), 3) pre-donation water, or 4) pre-donation water and leg exercise during donation.
RESULTS
Main effects of group were observed for phlebotomist classification of vasovagal reactions, X2 (3) = 8.38, p<0.05, and donor reports of presyncopal reactions, X2 (3) = 13.16, p < 0.01. Follow-up analyses of phlebotomist classifications revealed fewer reactions in the pre-donation water and pre-donation water and leg exercise groups relative to placebo but not standard donation. Follow-up analyses of self-reported reactions revealed that women, but not men, had lower scores in both the pre-donation water and pre-donation water and leg exercise groups relative to both placebo and standard donation.
CONCLUSION
Pre-donation hydration and a combination of hydration and leg exercise may help attenuate presyncopal reactions in relatively novice donors, although future studies with larger samples are required to confirm this effect.
Keywords: Blood donation, water, muscle exercise, presyncopal reactions
Introduction
In 2006, 9.6 million donors, or just 3.2% of the US population, provided the nearly 15 million units of blood needed for transfusions.1 Although the blood supply is adequate to meet the need much of the time, shortages are common due to seasonal variation in donation behavior, fluctuations in regional demand, and limited availability of certain blood types. The biggest concern, however, is the future. Because individuals aged 69 and older account for 50% of all transfusions, our progressively aging society is facing a steadily increasing annual demand for blood for use in surgeries and cancer treatments.2,3
A crucial component of the effort to meet the growing demand for blood is the recruitment and retention of young novice donors. Ideally, these new recruits would become lifelong donors, contributing up to six times per year and hundreds of units of blood in a lifetime. In reality, most young donors do not go on to donate on a regular basis.4–7 Syncopal and presyncopal reactions (e.g., fainting, dizziness, and nausea), which are most common in younger and novice donors, are primary deterrents to both recruitment and retention.8–12 In a one-year prospective study of 89,587 donors of all ages, we demonstrated a return rate of 64% for those who did not react versus 40% for those who did.13 Similarly, in a recent large-scale study of 16 year-old high school donors, Eder and colleagues revealed a 21% difference in the rate of return among those who experienced a reaction versus those who did not (52% versus 73%, OR = 0.40, 95% CI = 0.36–0.44).12 Accordingly, an intervention that can allay concerns about reactions and reduce their likelihood has the potential to dramatically enhance recruitment and retention of the next generation of blood donors.
Two interventions that have received empirical support as potential methods to avert or attenuate presyncopal reactions in young donors are acute water loading14,15 and applied muscle tension.16–20 Based on prior evidence of the ability of acute water loading to delay the onset of presyncopal responses to head-up tilt testing,21 the potential benefit of pre-donation water loading was first examined in a small randomized controlled trial of college men and women donating for the first time. Results indicated that donors who consumed 500 ml of water 30 minutes before donating reported significantly fewer presyncopal reactions when compared to donors who did not receive water.14 This finding was later confirmed in a larger study of almost 9000 high school donors,15 which also demonstrated that the salutary effects of hydration increased as the interval between water loading and phlebotomy decreased. The applied muscle tensing technique, which involves repeated contraction of major muscle groups, has been well-studied as a non-pharmacological treatment for syncope.22–26 Because this technique has obvious practical implications for preventing blood donation reactions, in a series of studies we recruited prospective donors at local blood drives and randomly assigned them to either: (1) receive pre-donation instruction in the use of applied muscle tension during donation, (2) placebo, or (3) donation-as-usual control group.16–20 On the whole, these studies demonstrated that donors who used the muscle tensing technique reported lower levels of negative reactions, were less likely to have their donation chair reclined by the phlebotomist, and expressed greater confidence that they would donate blood again in the future.
The present study was conducted as a randomized controlled trial of the combined effect of pre-donation hydration and repeated muscle tension on the experience of presyncopal reactions to blood donation. Although both interventions are designed to prevent presyncopal reactions by attenuating blood pressure reductions, the physiological mechanisms underlying their pressor responses are distinct. Specifically, the pressor effects of acute water loading have been associated with increases in sympathetic nervous system activity and total peripheral resistance.21,27–34 In contrast, physical maneuvers such as tensing of the muscles of the arms and legs are designed to influence blood pressure by promoting increases in venous return and cardiac output.26,35–38 Accordingly, hydration and muscle tensing may reduce the risk of vasovagal reactions during blood donation by helping to maintain blood pressure levels through vascular and cardiac mechanisms, respectively. In the present study it was hypothesized that a combined intervention would yield the greatest benefit.
Materials and Methods
Participants
The final sample included 414 adults (215 women, 199 men) with a mean age of 20.2 years (SD = 4.9); 60.9% were first-time donors and 39.1% were donating blood for the second time. Participants in the sample self-identified as Caucasian (76.3%), African-American (18.1%), Asian-American (2.9%), or chose another category or multiple categories to describe their race (2.7%).
Materials
State Anxiety Inventory
Anxiety was assessed using a version of the State Anxiety Inventory (STAI-Y),39 which is a 20-item scale designed to allow for self-report of state anxiety levels, with total scores ranging from 20 to 80. An example item, rated from 1 (not at all) to 4 (very much), is “I am tense.” In previous studies using this scale, high levels of internal consistency (Cronbach’s α = 0.95) and test-retest reliability (r=0.80 to 0.87) have been demonstrated.40,41
Blood Donation Reactions Inventory
The Blood Donation Reactions Inventory42 asks the donor to rate 11 subjective physiological reactions associated with blood donation on a 0 (not at all) to 5 (to an extreme degree) scale, with total scores ranging from 0 to 55. The eleven items include 1) faintness (as if about to faint or become unconscious), 2) dizziness, 3) weakness, 4) facial flush, 5) visual disturbance (such as blurred vision or tunnel vision), 6) difficulty hearing, 7) lightheadedness, 8) rapid or pounding heartbeat, 9) sweating, 10) rapid or difficult breathing, and 11) nausea or upset stomach. Scores from these 11 items have a high level of internal consistency and have been found to significantly correspond to phlebotomist classification of donor reactions.42,43 High scores on this scale are associated with a decreased likelihood of future donation.9
Blood Donation Satisfaction Survey
A five-item scale to assess satisfaction with the blood donation process includes items relating to satisfaction with staff explanations of procedures, length of time required for donation, staff efforts to make the donor comfortable, treatment by staff, and level of privacy. Level of satisfaction with each area is rated from 0 (not at all) to 5 (extremely), with total scores ranging from 0 to 25. Previous research using this scale has demonstrated good internal consistency for this measure (α = 0.90).44
Muscle Soreness Scale
Potential soreness as a consequence of the muscle tensing technique was assessed by having the subjects rate the level of pain or soreness in their legs on a scale from 0 (no pain) to 10 (worst pain imaginable) for three activities: sitting, standing, and walking. Total scores range from 0 to 30. Muscle soreness was assessed prior to donation and as part of the 24-hour follow-up.
Fatigue Scale
The Fatigue Scale of the Profile of Mood States45 was included to assess the level of fatigue following donation. Donors rated seven descriptors relating to fatigue (e.g., worn-out, exhausted, sluggish) on a scale from 0 (not at all) to 4 (extremely). Total scores range from 0 to 28. A baseline assessment was made prior to donation, and the scale was re-administered as part of the 24-hour follow-up.
Study Design and Treatments
All participants were tested at mobile blood collection sites in central and southeast Ohio, with the majority of the testing sites located on college campuses. Donors who met the study’s inclusion criteria (i.e., first- or second-time blood donors, eligible to donate, at least 18 years of age) were invited to participate in the study as part of the donation process, although this was not a requirement for donating.
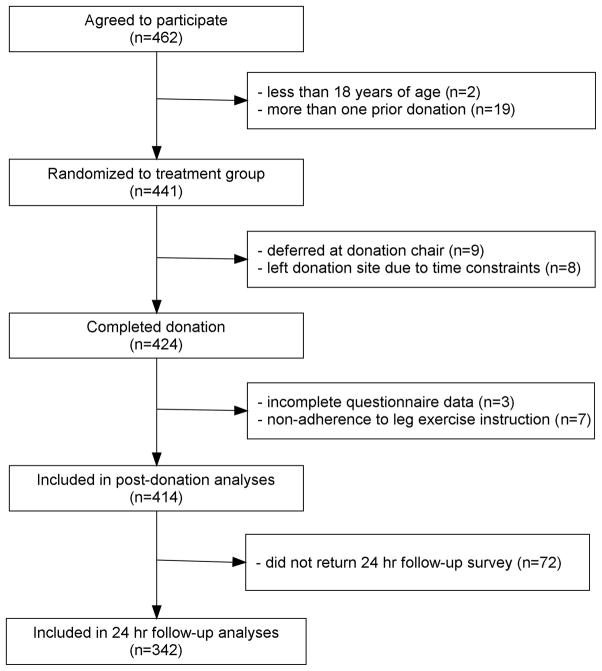
Figure 1 illustrates the flow of participants through each stage of the protocol. Prior to donation, but after the donor health history screening, eligible participants completed informed consent procedures and were randomly assigned to one of four groups: 1) standard donation, 2) placebo control (leg exercise prior to venipuncture), 3) pre-donation water (500 mL of bottled water consumed 30 minutes before donating), and 4) pre-donation water combined with leg exercise during donation. The second group is considered a “placebo” as the donor is taught the same technique and hence should have the same expectancy of benefit from the intervention. However, because only a very small proportion of reactions occur prior to needle insertion, the potential benefits of this intervention are no longer present during the period of greatest risk. Randomized assignment was accomplished by having participants select a slip of paper from an envelope containing an equal number of slips for each treatment group. Male and female donors selected from different envelopes to help ensure a relatively equal gender distribution across the four groups.
Figure 1.
Flow of participants through each stage of the study protocol.
Next, participants were assigned an anonymous identification code to be used on all materials and presented with an envelope containing specific directions for their group and a series of questionnaires. Directions for participants in the water conditions indicated that they would be asked to drink 500 ml of bottled water before they could proceed to the donation chair. Participants in the leg exercise conditions received written and visual descriptions of the simple leg lifting exercise, which instructed that every ten seconds they were to lift one leg approximately 12 inches above the donation bed and then immediately return the leg to the resting position. They were further instructed to alternate between their left and right leg for each trial. Participants in the placebo control condition were instructed to begin the leg lifting exercise when they were first seated in the donation chair and continue until just before the donation needle was inserted. Participants in the water and leg exercise condition were instructed to begin the leg lifting exercise once the donation needle was inserted and continue until the needle was removed.
After participants read and understood the directions and completed the pre-donation questionnaires (demographic information and measures of state anxiety, muscle soreness, and fatigue), the experimenter returned the questionnaires to the envelope and retained the envelope to be reassigned to the participant after donation. Participants in groups one and two were then escorted to an area to wait for the next available donation chair. Donors in groups three and four were provided with 500 ml of bottled water and asked to drink the water as soon as possible. Once they had consumed the water they were asked to wait for 20–25 minutes to allow for significant cardiovascular changes, including increases in vascular constriction and blood pressure, that peak approximately 30 minutes after consuming 500 ml of water and can persist for up to one hour.29,30,33,46–48 They were then escorted to an area to wait for the next available donation chair. Once seated in the donation chair, participants in the leg lifting conditions received a small box with a single red light that blinked at 10 second intervals to help them to time their leg lifting. In addition, a 25 gram accelerometer (Vernier, model ACC-BTA) was attached to their leg with a Velcro strap, and connected to a personal computer and Logger Lite software to monitor their performance. These recordings were used to confirm that participants performed the leg lifting exercise exclusively within their assigned interval (i.e., during pre-donation for the placebo control group and during blood draw for the combined intervention group).
All participants donated according to standard American Red Cross procedures and then proceeded to a post-donation canteen area. At the canteen each participant completed the Blood Donation Reactions Inventory and the Blood Donation Satisfaction Survey and provided a rating of venipuncture pain (from 0 = not at all painful to 5 = extremely painful). Before leaving the testing session, participants were reminded that they would receive an email in 24 hours with a final series of questions concerning their donation experience. This questionnaire included the Muscle Soreness Scale, the Fatigue Scale, and the Blood Donation Reactions Inventory. Donors were asked to complete these questionnaires with respect to how they had felt during the 24 hours after leaving the donation site. Finally, phlebotomist classifications of donor complications, based on the American Red Cross standardized classification system,49 were subsequently collected from donor database records.
The study protocol was approved by the Institutional Review Boards of Ohio University and the American Red Cross, and was pre-registered with www.clinicaltrials.gov (#NCT00302900).
Statistics
Statistical analyses were performed using SPSS software, Version 17.0 (SPSS Inc., IL, USA). Analyses of Variance (ANOVA) were conducted to compare the groups on continuous, normally-distributed variables (i.e., age, body mass index, pre-donation anxiety), non-parametric Kruskal-Wallis tests were conducted for variables that were not normally distributed (i.e., Blood Donation Reactions Inventory, donor satisfaction, venipuncture pain), and chi-square analyses were conducted for categorical variables (i.e., gender, race, proportion of first-time donors, phlebotomist classification of complications). Follow-up analyses were conducted using Mann-Whitney and Fisher’s exact tests with p-values less than 0.05, one-tailed considered significant. Additional analyses were conducted to examine sex and group differences in pre-donation anxiety, venipuncture pain, and donor satisfaction measured immediately after donation. Finally, to assess donor experiences in the 24 hours after they left the donation clinic, analyses were conducted on retrospective measures of presyncopal reactions, leg muscle soreness, and overall fatigue for those who returned completed post-donation surveys.
Results
Table 1 provides descriptive characteristics of participants in the study. Comparisons across the four groups revealed no significant differences with respect to age, body mass index, proportion of first-time donors, or gender and race distributions.
Table 1.
Characteristics of participants in each group.
| Variable | Units | Standard Donation (n = 103) | Placebo Control (n = 102) | Water Only (n = 106) | Water + Leg Exercise (n = 103) |
|---|---|---|---|---|---|
| Age, in years | Mean (SD) | 20.4 (6.1) | 19.8 (3.4) | 20.4 (5.5) | 20.2 (3.8) |
| BMI, in kg/m2 | Mean (SD) | 24.3 (4.4) | 24.6 (4.7) | 24.2 (4.3) | 24.1 (4.2) |
| First-time Donors | n (%) | 70 (68) | 61 (59.8) | 64 (60.4) | 57 (55.3) |
| Female | n (%) | 53 (51.5) | 53 (52.0) | 55 (51.9) | 54 (52.4) |
| Race | |||||
| Caucasian | n (%) | 76 (73.8) | 89 (87.3) | 78 (73.6) | 73 (70.9) |
| African-American | n (%) | 20 (19.4) | 9 (8.8) | 23 (21.7) | 23 (22.3) |
| Asian-American | n (%) | 3 (2.9) | 3 (2.9) | 2 (1.9) | 4 (3.9) |
| Other | n (%) | 4 (3.9) | 1 (1.0) | 3 (2.8) | 3 (2.9) |
Donor Adherence to Interventions
Donors in the water ingestion conditions all consumed 500 ml of water before proceeding to donation. The mean (± SEM) lag time between water consumption and venipuncture was not significantly different between the water loading (31.8 ± 1.3) and water loading combined with leg exercise (32.5 ± 1.2) groups, F = 0.19, p= 0.66. Further, lag time was not significantly correlated with either Blood Donation Reactions Inventory scores (Spearman’s rho = 0.08, p = 0.23) or the proportion of donors identified as having a vasovagal reaction by the phlebotomist (Spearman’s rho = 0.03, p = 0.63).
Adherence to the leg exercise instructions was high for both the placebo group (102/106 or 96.2%) and the combined group (103/106 or 97.2%), and in all cases where the participant failed to comply with instructions it was because they used the tensing procedure both before and during the blood draw. Donors who did not adhere to the instructions were eliminated from the analyses.
Phlebotomist Classification of Donor Complications
As seen in Table 2, most donors in the present study were classified as having had no complications (n = 343/414; 82.9%). Among the 71 donors classified as having a complication, there were 56 vasovagal reactions including 54 presyncopal reactions (13.0%) and 2 episodes of loss of consciousness for less than one minute (0.5%). The remaining complications were phlebotomy-related and included 14 small hematoma (3.4%) and 1 arterial puncture (0.2%).
Table 2.
Number of donors in each group classified as having either no complication, a vasovagal complication (i.e., syncopal or presyncopal), or a phlebotomy-related complication (i.e., small hematoma or arterial puncture). Significantly fewer vasovagal complications were observed in the “water only” and “water + leg exercise” groups versus the “placebo control” group, and marginally fewer vasovagal complications were observed in the “water + leg exercise” group relative to “standard donation”.
| Complication Type | Standard Donation (n = 103) | Placebo Control (n = 102) | Water Only (n = 106) | Water + Leg Exercise (n = 103) |
|---|---|---|---|---|
| None | 82 | 76 | 94 | 91 |
| Vasovagal | 15 | 21 | 12 | 8 |
| Phlebotomy | 6 | 5 | 0 | 4 |
Analyses of vasovagal complications revealed a significant main effect of group, X2 (3) = 8.38, p<.05. Follow-up analyses revealed that, relative to the placebo group, donors had significantly fewer vasovagal reactions in the water loading and water loading combined with leg exercise groups. Similar comparisons to the standard donation group were not significant for the water loading group, but were marginally significant (p=.08, one-tailed) for the water loading combined with leg exercise group.
There was no difference in the frequency of phlebotomist-reported vasovagal reactions between male and female donors, X2 (1) = 1.30, p = 0.25.
Donor Reaction Ratings
Analysis of donor ratings of presyncopal reactions on the Blood Donation Reactions Inventory revealed a significant main effect of study group, X2 (3) = 13.16, p < 0.01. However, because ratings were significantly higher for female versus male donors, X2 (1) = 6.50, p < 0.05, analyses of group differences were conducted separately for male and female donors and revealed a significant main effect of group for women, X2 (3) = 10.74, p < 0.05, but not men, X2 (3) = 3.72, p = 0.29. As can be seen in Table 3, follow-up analyses within female donors revealed significantly lower presyncopal reaction scores in the water loading and water loading combined with leg exercise groups as compared to either standard donation or placebo (all p < 0.05, one-tailed).
Table 3.
Blood Donation Reactions Inventory ratings for female donors in each group. Significantly lower ratings were reported in the “water only” and “water + leg exercise” groups versus both the “standard donation” and the “placebo control” groups.
| Statistic | Standard Donation (n = 53) | Placebo Control (n = 53) | Water Only (n = 55) | Water +Leg Exercise (n = 54) |
|---|---|---|---|---|
| Mean | 10.3 | 10.6 | 6.4 | 5.3 |
| Median | 4 | 5 | 2 | 2 |
| SD | 14.3 | 13.1 | 10.0 | 7.9 |
| Range | 0–55 | 0–51 | 0–38 | 0–37 |
Across all donors, scores on the Blood Donation Reactions Inventory were positively correlated with phlebotomist classification of vasovagal reaction (Spearman’s rho = 0.51, p < 0.001).
Donor Anxiety, Venipuncture Pain, Satisfaction, and Post-donation Experience
Means and standard deviations for donor ratings of pre-donation anxiety, venipuncture pain, and post-donation satisfaction, muscle soreness and fatigue are provided in Table 4. Although there were no significant differences between the groups in pre-donation anxiety, F = 0.67, p= 0.57, or venipuncture pain ratings, X2 (3) = 0.84, p = 0.84, sex differences were observed for both measures. Specifically, relative to male donors, women reported higher pre-donation anxiety, F = 5.67, p < 0.05, and more venipuncture pain, X2 (1) = 19.1, p < 0.001. On the whole donors were highly satisfied with their donation experience, and there were no significant group differences, X2 (3) = 1.52, p = 0.67, or sex differences, X2 (1) = 0.10, p = 0.74, on the post-donation satisfaction scale. However, across all participants there was a significant inverse relationship between Blood Donation Reactions Inventory ratings and donor satisfaction ratings, with more presyncopal reaction symptoms associated with lower satisfaction scores (Spearman’s rho = −0.20, p < 0.001).
Table 4.
Means (SD) of donor ratings of pre-donation anxiety, venipuncture pain, post-donation satisfaction, muscle soreness, and fatigue.
| Rating scale | scale range | Standard Donation (n = 103) | Placebo Control (n = 102) | Water Only (n = 106) | Water +Leg Exercise (n = 103) |
|---|---|---|---|---|---|
| Anxiety | (20–80) | 46.5 (5.2) | 45.7 (5.2) | 46.3 (4.7) | 45.7 (4.6) |
| Pain | (0–5) | 1.7 (1.2) | 1.6 (1.0) | 1.8 (1.2) | 1.7 (1.2) |
| Satisfaction | (0–25) | 22.0 (3.7) | 21.2 (4.0) | 21.6 (4.0) | 21.3 (4.1) |
| Muscle soreness | (0–30) | 0.8 (2.0) | 0.6 (1.3) | 0.7 (2.3) | 1.1 (2.5) |
| Fatigue | (0–28) | 7.1 (6.9) | 6.5 (6.4) | 6.0 (5.9) | 6.9 (6.8) |
The 24-hr follow-up questionnaires were completed by 82.6% (342/414) of participants. Analyses of these 24-hr post-donation measures of presyncopal reactions, leg muscle soreness, and overall fatigue failed to reveal any sex or group differences.
Discussion
The results of the present study provide mixed support for the beneficial effects of water loading and muscle exercise as methods of attenuating presyncopal reactions. Specifically, our findings indicate that the benefit of the interventions varied as a function of both the source of vasovagal ratings (i.e., donor versus phlebotomist) as well as the sex of the donor.
From the donor’s perspective, the pre-donation hydration and the hydration plus muscle exercise groups were associated with significantly lower ratings of vasovagal reactions as compared to either the standard donation or placebo control groups. However, this effect was restricted to female donors. Although this contrasts with prior reports of beneficial effects of water loading 14,15 and muscle tensing 16,17,20 in both male and female donors, it is consistent with one of the largest studies to date in which the beneficial effects of muscle tensing were restricted to female donors.19 Differential effectiveness of these interventions in women versus men may reflect the greater likelihood of such reactions among female donors. This sex difference has been attributed, at least in part, to smaller average body size in women and hence a greater proportional blood volume loss during a standard 500 mL donation. Alternatively, given that there was no significant difference in phlebotomist classifications of vasovagal reactions between men and women in the present study, failure to observe intervention effects on subjective ratings among male donors may reflect their general reluctance to report symptoms.
From the perspective of the phlebotomist, there was a significant overall difference between the groups with regard to the proportion of donors who experienced a vasovagal reaction. Follow-up analyses revealed that the pre-donation water loading group had significantly fewer reactions than the placebo control group, and that the water loading and muscle exercise group had significantly fewer reactions than placebo and marginally fewer reactions than standard donation. Failure to observe significant differences in comparison to standard donation argues against the ability of these interventions to reduce outward signs of donor distress. On the other hand, it is important to note that the combined intervention was associated with marginally fewer reactions and that the failure to show statistical significance should be considered in the context of the sample size and associated statistical power. If similar proportions of reactions were noted in a sample that was 50% larger, then the observed effect would indeed be significant. As a result, rather than relying exclusively on statistical significance, consideration of the absolute proportion of vasovagal reactions to no reactions in each group (e.g., 18.3% in standard donation versus 8.8% in water loading and muscle exercise) is justified when considering the potential of these interventions to alleviate donor distress.
Whereas the present findings do not demonstrate an additive benefit of combining muscle exercise with hydration, it must be noted that the nature of the current design does not provide a test of the independent effect of muscle exercise alone and therefore is not directly comparable to existing evidence of the benefits of applied muscle tensing during donation.16–20 Because hydration and muscle exercise promote blood pressure increases through different physiological mechanisms,26,28 it is possible that either intervention alone can elicit a sufficient pressor response to maintain blood pressure at or above normal resting levels and in so doing help to avert presyncopal reactions. Accordingly, ultimate resolution of the potential benefit of a combined intervention will require a full factorial design wherein donors who receive either intervention alone are directly compared to donors receiving a combined intervention. Further, because there may be individual differences in responsivity to the interventions, a repeated measures design that compares the effects of the interventions across multiple donations within individuals may be particularly valuable. Given recent evidence that ingestion of water closer to the time of actual donation may be more effective at preventing syncopal reactions,15,27 it would also be helpful to manipulate this variable in a systematic fashion to determine the optimum interval for water loading with and without concomitant muscle tensing. Notwithstanding this call for further research, results from the current tightly-controlled study support the idea that it is possible to produce clinically meaningful reductions in reactions with simple, non-pharmacologic techniques.
Strengths of the current study include a relatively homogeneous sample of first- and second-time donors, careful administration and monitoring of interventions, and multiple measures of donor experience. It must be noted, however, that the current sample was restricted to only a few hundred, young adult donors recruited primarily from college campuses. Although these first- and second-time donors are at greater risk of reactions than the general donor pool, it is conceivable that stronger and more consistent effects would be evident if the interventions were tested on larger samples of those at highest risk such as female, first-time, high school donors. Further, while the present report provides some additional support for the potential benefit of donor interventions, an important issue that remains is whether such efforts are associated with increased donor retention. To address this issue we are continuing to follow the current participants to determine their rate of repeat donation during the two years following their index donation.
Acknowledgments
We are most grateful for the cooperation and collaboration of the American Red Cross Blood Services, Central Ohio Region, and particularly for the efforts of Deborah Carvalho, Lori Gaitten, and Mary Schumacher. We are also grateful for the efforts of the research assistants who helped with data entry on this project (Tanya Cornett, Kelsey Fazenbaker, and Rita Murphy). Finally, a special note of appreciation is due to all of the donors who participated in this project.
Funding: Funding for this study was provided by a grant from the National Heart, Lung, and Blood Institute (HL077438).
Footnotes
Conflict of interest statement: The authors certify that they have no conflict of interest or financial involvement with this manuscript.
References
- 1.Whitaker BL, Green J, King MR, et al. The 2007 National Blood Collection and Utilization Survey Report. Washington, D.C: 2007. [Google Scholar]
- 2.United States Census Bureau. US Population Projections. 2009 http://www.census.gov/population/www/projections/projectionsagesex.html.
- 3.American Association of Blood Banks (AABB) About blood and cellular therapies. 2009 http://www.aabb.org/content/about_blood/faq/bloodfaq.htm.
- 4.Ownby HE, Kong F, Watanabe K, et al. Analysis of donor return behavior. Retrovirus Epidemiology Donor Study. Transfusion. 1999;39:1128–35. doi: 10.1046/j.1537-2995.1999.39101128.x. [DOI] [PubMed] [Google Scholar]
- 5.Schlumpf KS, Glynn SA, Schreiber GB, et al. Factors influencing donor return. Transfusion. 2008;48:264–72. doi: 10.1111/j.1537-2995.2007.01519.x. [DOI] [PubMed] [Google Scholar]
- 6.Schreiber GB, Sharma UK, Wright DJ, et al. First year donation patterns predict long-term commitment for first-time donors. Vox Sang. 2005;88:114–21. doi: 10.1111/j.1423-0410.2005.00593.x. [DOI] [PubMed] [Google Scholar]
- 7.Schreiber GB, Sanchez AM, Glynn SA, Wright DJ. Increasing blood availability by changing donation patterns. Transfusion. 2003;43:591–7. doi: 10.1046/j.1537-2995.2003.00388.x. [DOI] [PubMed] [Google Scholar]
- 8.Hupfer ME, Taylor DW, Letwin JA. Understanding Canadian student motivations and beliefs about giving blood. Transfusion. 2005;45:149–61. doi: 10.1111/j.1537-2995.2004.03374.x. [DOI] [PubMed] [Google Scholar]
- 9.France CR, France JL, Roussos M, Ditto B. Mild reactions to blood donation predict a decreased likelihood of donor return. Transfusion and Apheresis Science. 2004;30:17–22. doi: 10.1016/j.transci.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Rader AW, France CR, Carlson B. Donor retention as a function of donor reactions to whole-blood and automated double red cell collections. Transfusion. 2007;47:995–1001. doi: 10.1111/j.1537-2995.2007.01223.x. [DOI] [PubMed] [Google Scholar]
- 11.Newman BH, Newman DT, Ahmad R, Roth AJ. The effect of whole-blood donor adverse events on blood donor return rates. Transfusion. 2006;46:1374–9. doi: 10.1111/j.1537-2995.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- 12.Eder AF, Hillyer CD, Dy BA, et al. Adverse reactions to allogeneic whole blood donation by 16- and 17-year-olds. JAMA. 2008;299:2279–86. doi: 10.1001/jama.299.19.2279. [DOI] [PubMed] [Google Scholar]
- 13.France CR, Rader A, Carlson B. Donors who react may not come back: analysis of repeat donation as a function of phlebotomist ratings of vasovagal reactions. Transfus Apher Sci. 2005;33:99–106. doi: 10.1016/j.transci.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Hanson SA, France CR. Predonation water ingestion attenuates negative reactions to blood donation. Transfusion. 2004;44:924–8. doi: 10.1111/j.1537-2995.2004.03426.x. [DOI] [PubMed] [Google Scholar]
- 15.Newman BH, Tommolino E, Andreozzi C, et al. The effect of a 16-oz. water drink on blood donor reaction rates in high-school students: Two independent studies combined. Transfusion. 2006;46:S80A. doi: 10.1111/j.1537-2995.2007.01293.x. [DOI] [PubMed] [Google Scholar]
- 16.Ditto B, France CR. The effects of applied tension on symptoms in French-speaking blood donors: a randomized trial. Health Psychol. 2006;25:433–7. doi: 10.1037/0278-6133.25.3.433. [DOI] [PubMed] [Google Scholar]
- 17.Ditto B, France CR, Albert M, Byrne N. Dismantling applied tension: mechanisms of a treatment to reduce blood donation-related symptoms. Transfusion. 2007;47:2217–22. doi: 10.1111/j.1537-2995.2007.01449.x. [DOI] [PubMed] [Google Scholar]
- 18.Ditto B, France CR, Albert M, et al. Effects of applied muscle tension on the likelihood of blood donor return. Transfusion. 2009;49:858–62. doi: 10.1111/j.1537-2995.2008.02067.x. [DOI] [PubMed] [Google Scholar]
- 19.Ditto B, France CR, Lavoie P, et al. Reducing reactions to blood donation with applied muscle tension: a randomized controlled trial. Transfusion. 2003;43:1269–75. doi: 10.1046/j.1537-2995.2003.00488.x. [DOI] [PubMed] [Google Scholar]
- 20.Ditto B, Wilkins JA, France CR, et al. On-site training in applied muscle tension to reduce vasovagal reactions to blood donation. J Behav Med. 2003;26:53–65. doi: 10.1023/a:1021795022380. [DOI] [PubMed] [Google Scholar]
- 21.Lu CC, Diedrich A, Tung CS, et al. Water ingestion as prophylaxis against syncope. Circulation. 2003;108:2660–5. doi: 10.1161/01.CIR.0000101966.24899.CB. [DOI] [PubMed] [Google Scholar]
- 22.Krediet CT, de Bruin IG, Ganzeboom KS, et al. Leg crossing, muscle tensing, squatting, and the crash position are effective against vasovagal reactions solely through increases in cardiac output. J Appl Physiol. 2005;99:1697–703. doi: 10.1152/japplphysiol.01250.2004. [DOI] [PubMed] [Google Scholar]
- 23.Krediet CT, van Dijk N, Linzer M, et al. Management of vasovagal syncope: controlling or aborting faints by leg crossing and muscle tensing. Circulation. 2002;106:1684–9. doi: 10.1161/01.cir.0000030939.12646.8f. [DOI] [PubMed] [Google Scholar]
- 24.Krediet CT, van Lieshout JJ, Bogert LW, et al. Leg crossing improves orthostatic tolerance in healthy subjects: a placebo-controlled crossover study. Am J Physiol Heart Circ Physiol. 2006;291:H1768–72. doi: 10.1152/ajpheart.00287.2006. [DOI] [PubMed] [Google Scholar]
- 25.Krediet CT, Van Lieshout JJ, Wieling W. Improved orthostatic tolerance by leg crossing and muscle tensing: indisputable evidence for the arteriovenous pump existence: Response from Krediet et al. J Appl Physiol. 2006 doi: 10.1152/japplphysiol.00434.2006. [DOI] [PubMed] [Google Scholar]
- 26.Wieling W, Colman N, Krediet CT, Freeman R. Nonpharmacological treatment of reflex syncope. Clin Auton Res. 2004;14 (Suppl 1):62–70. doi: 10.1007/s10286-004-1009-x. [DOI] [PubMed] [Google Scholar]
- 27.Ando SI, Kawamura N, Matsumoto M, et al. Simple standing test predicts and water ingestion prevents vasovagal reaction in the high-risk blood donors. Transfusion. 2009;49:1630–6. doi: 10.1111/j.1537-2995.2009.02189.x. [DOI] [PubMed] [Google Scholar]
- 28.Jordan J. Acute effect of water on blood pressure. What do we know? Clin Auton Res. 2002;12:250–5. doi: 10.1007/s10286-002-0055-5. [DOI] [PubMed] [Google Scholar]
- 29.Jordan J, Shannon JR, Black BK, et al. The pressor response to water drinking in humans: a sympathetic reflex? Circulation. 2000;101:504–9. doi: 10.1161/01.cir.101.5.504. [DOI] [PubMed] [Google Scholar]
- 30.Jordan J, Shannon JR, Grogan E, et al. A potent pressor response elicited by drinking water. Lancet. 1999;353:723. doi: 10.1016/S0140-6736(99)99015-3. [DOI] [PubMed] [Google Scholar]
- 31.Brown CM, Barberini L, Dulloo AG, Montani JP. Cardiovascular responses to water drinking: does osmolality play a role? Am J Physiol Regul Integr Comp Physiol. 2005;289:R1687–92. doi: 10.1152/ajpregu.00205.2005. [DOI] [PubMed] [Google Scholar]
- 32.Lipp A, Tank J, Franke G, et al. Osmosensitive mechanisms contribute to the water drinking-induced pressor response in humans. Neurology. 2005;65:905–7. doi: 10.1212/01.wnl.0000176060.90959.36. [DOI] [PubMed] [Google Scholar]
- 33.Scott EM, Greenwood JP, Gilbey SG, et al. Water ingestion increases sympathetic vasoconstrictor discharge in normal human subjects. Clinical Science. 2001;100:335–42. [PubMed] [Google Scholar]
- 34.Rossi P, Andriesse GI, Oey PL, et al. Stomach distension increases efferent muscle sympathetic nerve activity and blood pressure in healthy humans. J Neurol Sci. 1998;161:148–55. doi: 10.1016/s0022-510x(98)00276-7. [DOI] [PubMed] [Google Scholar]
- 35.Foulds J, Wiedmann K, Patterson J, Brooks N. The effects of muscle tension on cerebral circulation in blood-phobic and non-phobic subjects. Behav Res Ther. 1990;28:481–6. doi: 10.1016/0005-7967(90)90134-5. [DOI] [PubMed] [Google Scholar]
- 36.van Lieshout JJ, Pott F, Madsen PL, et al. Muscle tensing during standing: effects on cerebral tissue oxygenation and cerebral artery blood velocity. Stroke. 2001;32:1546–51. doi: 10.1161/01.str.32.7.1546. [DOI] [PubMed] [Google Scholar]
- 37.France CR, France JL, Patterson SM. Blood pressure and cerebral oxygenation responses to skeletal muscle tension: a comparison of two physical maneuvers to prevent vasovagal reactions. Clin Physiol Funct Imaging. 2006;26:21–5. doi: 10.1111/j.1475-097X.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 38.Ditto B, Byrne N, Holly C. Physiological correlates of applied tension may contribute to reduced fainting during medical procedures. Ann Behav Med. 2009;37:306–14. doi: 10.1007/s12160-009-9114-7. [DOI] [PubMed] [Google Scholar]
- 39.Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto, Ca: Consulting Psychologists Press; 1983. [Google Scholar]
- 40.France CR, France JL, Kowalsky JM, Cornett TL. Education in donation coping strategies encourages individuals to give blood: Further evaluation of a new donor recruitment brochure. Transfusion. 2010;50:85–91. doi: 10.1111/j.1537-2995.2009.02381.x. [DOI] [PubMed] [Google Scholar]
- 41.France CR, Montalva R, France JL, Trost Z. Enhancing attitudes and intentions in prospective blood donors: evaluation of a new donor recruitment brochure. Transfusion. 2008;48:526–30. doi: 10.1111/j.1537-2995.2007.01565.x. [DOI] [PubMed] [Google Scholar]
- 42.Meade MA, France CR, Peterson LM. Predicting vasovagal reactions in volunteer blood donors. J Psychosom Res. 1996;40:495–501. doi: 10.1016/0022-3999(95)00639-7. [DOI] [PubMed] [Google Scholar]
- 43.Sauer LA, France CR. Caffeine attenuates vasovagal reactions in female first-time blood donors. Health Psychol. 1999;18:403–9. doi: 10.1037//0278-6133.18.4.403. [DOI] [PubMed] [Google Scholar]
- 44.France JL, France CR, Himawan LK. A path analysis of intention to redonate among experienced blood donors: an extension of the theory of planned behavior. Transfusion. 2007;47:1006–13. doi: 10.1111/j.1537-2995.2007.01236.x. [DOI] [PubMed] [Google Scholar]
- 45.McNair DM, Lorr M, Droppleman LF. Profile of Mood States Manual. San Diego: Educational and Industrial Testing Service; 1992. [Google Scholar]
- 46.Kasprisin DO, Glynn SH, Taylor F, Miller KA. Moderate and severe reactions in blood donors. Transfusion. 1992;32:23–6. doi: 10.1046/j.1537-2995.1992.32192116426.x. [DOI] [PubMed] [Google Scholar]
- 47.Routledge HC, Chowdhary S, Coote JH, Townend JN. Cardiac vagal response to water ingestion in normal human subjects. Clinical Science. 2002;103:157–62. doi: 10.1042/cs1030157. [DOI] [PubMed] [Google Scholar]
- 48.Schroeder C, Bush VE, Norcliffe LJ, et al. Water drinking acutely improves orthostatic tolerance in healthy subjects. Circulation. 2002;106:2806–11. doi: 10.1161/01.cir.0000038921.64575.d0. [DOI] [PubMed] [Google Scholar]
- 49.Eder AF, Dy BA, Kennedy JM, et al. The American Red Cross donor hemovigilance program: complications of blood donation reported in 2006. Transfusion. 2008;48:1809–19. doi: 10.1111/j.1537-2995.2008.01811.x. [DOI] [PubMed] [Google Scholar]