Abstract
Background
Consequences of chronic exposure to cytokines of the innate immune system on sleep in humans and the association of cytokine-induced sleep alterations with behavior, motor performance and cortisol secretion are unknown.
Methods
Thirty-one patients with hepatitis C without pre-existing sleep disorders underwent nighttime polysomnography, daytime multiple sleep latency testing, behavioral assessments, neuropsychological testing and serial blood sampling at baseline and after ~12 weeks of either treatment with the innate immune cytokine, interferon (IFN)-alpha (n=19) or no treatment (n=12). Fatigue and sleepiness were assessed using the Multidimensional Fatigue Inventory and Epworth Sleepiness Scale.
Results
IFN-alpha administration led to significant increases in wake after sleep onset and significant decreases in Stage 3/4 sleep and sleep efficiency. REM latency and Stage 2 sleep were significantly increased during IFN-alpha treatment. Decreases in Stage 3/4 sleep and increases in REM latency were associated with increases in fatigue, whereas decreases in sleep efficiency were associated with reduced motor speed. Increased wake after sleep onset was associated with increased evening plasma cortisol. Despite IFN-alpha-induced increases in fatigue, daytime sleepiness did not increase. In fact, IFN-alpha-treated patients exhibited decreased propensity to fall asleep during daytime nap opportunities.
Conclusions
Chronic exposure to an innate immune cytokine reduced sleep continuity and depth, and induced a sleep pattern consistent with insomnia and hyperarousal. These data suggest that innate immune cytokines may provide a mechanistic link between disorders associated with chronic inflammation including medical and/or psychiatric illnesses and insomnia, which in turn is associated with fatigue, motor slowing and altered cortisol.
Keywords: Sleep, insomnia, hyperarousal, polysomnography, fatigue, depression, interferon-alpha, hepatitis C, neuropsychology, cortisol, cytokines
Introduction
Cytokines of the innate immune system, including interferon (IFN)-alpha, interleukin (IL)-1, IL-6 and tumor necrosis factor (TNF)-alpha, are important mediators of inflammation and have long been known to induce symptoms of depression including alterations in sleep (1–11). For example, studies in rodents have shown that acute administration of innate immune cytokines, or cytokine inducers such as lipopolysaccharide (LPS), suppresses rapid eye movement (REM) sleep, while increasing non-rapid eye movement (non-REM) sleep, especially Stage 3/4 sleep, also referred to as slow wave sleep (SWS)(3,4,6,12) At high doses, however, innate immune cytokines can disrupt non-REM sleep in rodents and reduce SWS (3). In humans, acute effects of innate immune cytokines are more complex and, like in rodents, appear to be dose dependent. For example, low dose IL-6 suppresses non-REM sleep in the first half of the night, while increasing non-REM sleep (and SWS) in the second half of the night (7,8). In addition, low-dose LPS increases non-REM sleep, whereas high-dose LPS suppresses non-REM sleep (13). Consistent with the effects of acute cytokine administration on laboratory animals, acute administration of LPS or innate immune cytokines to humans has been reliably reported to suppress REM sleep (7,9–11).
Although early interest in sleep abnormalities in psychiatric disturbances focused on REM sleep (with the observation that decreased REM latency may be a biological marker of major depression)(14–16), subsequent studies have suggested that patients with major depression, perhaps even more reliably exhibit disruptions in non-REM sleep, especially impairments in sleep initiation/continuity (i.e. latency to sleep onset, wake after sleep onset, and sleep efficiency) as well as reductions in SWS (17–19). This general pattern of sleep disruption is also highly prevalent in a variety of medical illnesses including cancer, cardiovascular disease, and autoimmune and inflammatory disorders. Indeed, these illnesses have all been associated with various measures of sleep disruption and secondary insomnia, including reduced sleep efficiency and increased wake after sleep onset (20–23). Given the association of these medical illnesses as well as major depression with evidence of chronic activation of innate immune responses, these data suggest that innate immune cytokines may serve as a mediator of sleep alterations in these disorders. Nevertheless, there is limited data on the effects of chronic exposure to innate immune cytokines on sleep, and no study to our knowledge has employed polysomnography (PSG) in this regard. Moreover, while much animal literature and a handful of human studies have reported on the effects of short-term cytokine exposure (3–11), these findings may provide limited insight into sleep changes associated with chronic inflammation as might be expected in chronic medical and/or psychiatric disease (24).
Patients undergoing long-term treatment with the innate immune cytokine, IFN-alpha, provide a unique opportunity to address how—and to what degree—chronic inflammation affects sleep in humans (25). While an effective therapy for hepatitis C virus (HCV) infection and cancer, IFN-alpha induces significant behavioral changes including depression, fatigue and sleep disturbances in a high percentage of patients (26–29). Much like other inflammatory stimuli (e.g. LPS) that induce behavioral changes, IFN-alpha also activates other innate immune cytokines, including TNF-alpha, IL-1, IL-6 and their soluble receptors (25,30–33), which have been shown to correlate with development of behavioral disturbances including sleep changes during IFN-alpha treatment (25,31,33). For example, in patients receiving IFN-alpha for HCV, unidirectional relationships among inflammation, sleep and mood disturbance were observed, such that plasma IL-6 predicted poor sleep, and poor sleep, in turn, predicted development of depression (25). In addition, IFN-alpha has been shown to induce neurocognitive changes (motor slowing), a flattened diurnal cortisol slope, and increased evening cortisol (31,34). These neurocognitive and neuroendocrine changes are typical of those observed following experimental sleep disruption (35–38).
To determine the impact of chronic exposure to an innate immune cytokine on human sleep architecture, a longitudinal, case-controlled design using overnight PSG and daytime multiple sleep latency testing (MSLT) in patients receiving IFN-alpha plus ribavirin for HCV was conducted. In addition, the relationship between cytokine-induced changes in sleep parameters and changes in behavioral symptoms, neurocognitive function and circadian neuroendocrine activity known to be affected by sleep disruption was examined. Finally, associations between IFN-alpha and other innate immune cytokines and sleep changes were explored.
Methods and Materials
Subjects
Thirty-one HCV-positive subjects (17 males, 14 females) as determined by serum anti-HCV antibodies or HCV-RNA by reverse transcription-PCR were enrolled. To ensure medically stable HCV patients without an urgent need for IFN-alpha therapy or psychiatric treatment, exclusion criteria included decompensated liver disease; liver disease from any cause other than HCV; unstable cardiovascular, endocrinologic, hematologic, renal or neurologic disease (as determined by physical exam and laboratory testing); <24 on the Mini Mental State Exam (39); and history of schizophrenia or bipolar disorder and/or diagnosis of major depression or substance abuse/dependence within six months of study entry [determined by Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders—Fourth Edition (SCID)](40). Subjects with evidence of a preexisting sleep disorder as determined by an apnea-hypopnea index >15 (i.e. >15 sleep apnea-hypopnea episodes per hour of sleep) or a periodic leg movement index >25 (i.e. >25 leg movements with or without arousal per hour of sleep) during adaptation or baseline sleep nights were also excluded. Subjects were required to be off all antidepressants, antipsychotics, and mood stabilizers for at least 4 weeks (8 weeks for fluoxetine) prior to study entry and throughout the study. Subjects were also required to be off other medications known to affect sleep including narcotics, benzodiazepines and non-benzodiazepine sedative/hypnotics for 2 weeks prior to baseline and 48 hours prior to the 12 week sleep assessment. Of the 31 subjects included in this study, 25 (15 IFN-alpha-treated, 10 controls) participated in a study of IFN-alpha effects on neuroendocrine function and 24 (15 IFN-alpha-treated, 9 controls) participated in a study of IFN-alpha effects on neurocognition (31,34).
Study Design and Polysomnography Assessments
A prospective, longitudinal, case-controlled design was used to examine sleep in HCV patients prior to (Visit 1), and following, ~12 weeks (Visit 2) of either treatment with IFN-alpha plus ribavirin (treatment group) or no treatment (control group). All IFN-alpha-treated subjects received pegylated IFN-alfa-2b (Pegintron®, Schering Plough, Kennilworth, NJ) or pegylated IFN-alfa-2a (PEGASYS®, Roche, Basel, Switzerland) administered subcutaneously once weekly. Participation in treatment versus control groups as well as type of IFN-alpha was determined by patients and their physicians and was not controlled by study protocol. Because of lack of urgency of IFN-alpha therapy in this stable population of HCV patients, decisions regarding initiation of IFN-alpha were largely based on scheduling convenience. In event that a patient met criteria for IFN-alpha-induced major depression during the study, the patient immediately underwent research assessment and was referred for psychiatric care.
All study procedures took place in the Emory General Clinical Research Center (GCRC). To allow for accommodation to the GCRC environment and to screen for sleep disorders, subjects underwent one night of PSG in the GCRC one week prior to study initiation. On study Visits 1 and 2, subjects underwent two nights of PSG (see Supplementary Materials in Supplement 1 for details). For statistical analyses, PSG results were averaged across these two nights during each visit. Each night, lights out occurred at 10pm, and each morning, subjects were awakened at 7:15am. On the second full day of the GCRC stay, MSLT was conducted in a subset of subjects (IFN-alpha: n=17; control: n=10) at 10am, 12noon, 2pm and 4pm (see Supplementary Materials in Supplement 1 for details) (41). MSLT results including latency to sleep onset and cumulative sleep time were averaged across the day for statistical analyses.
During each GCRC admission, blood was withdrawn from an indwelling catheter into EDTA-coated tubes hourly from 9am–9pm for assessment of plasma cortisol as well as TNF-alpha and its soluble receptor, soluble TNF receptor 2 (sTNFR2). Following sampling, blood was immediately centrifuged at 1000Xg for 10 minutes at 4°C. Plasma was removed and frozen at −80°C until assay. For IFN-alpha-treated subjects, Visit 2 was scheduled 4–5 days following the last IFN-alpha injection. Plasma IFN-alpha was assessed at 4pm on both Visits to ensure treatment adherence and to correlate with sleep measures. Urine drug screens were conducted at each visit to rule out substance abuse.
Subjects provided written informed consent, and study procedures received a priori approval by Emory University Institutional Review Board.
Behavioral and Neuropsychological Assessments
Depression was evaluated by trained clinician-raters using the mood disorders module of the SCID and the Montgomery-Asberg Depression Rating Scale (MADRS)(40,42) (see see Supplementary Materials in Supplement 1). Due to the profound nature of IFN-alpha effects on behavior, it was not considered feasible to uniformly blind clinician-raters to treatment assignment. To evaluate severity of fatigue, subjects completed the self-report, 20-item Multidimensional Fatigue Inventory (MFI)(43). Higher MFI scores represent greater symptoms of fatigue (see Supplementary Materials in Supplement 1). The Epworth Sleepiness Scale (ESS) was used to assess subjective sense of daytime sleepiness (44). The ESS is a 24-point scale with 8 different situations rated 0–3 according to likelihood of falling asleep. Higher scores signify greater daytime sleepiness.
Motor speed (choice movement time) was measured at each visit in a subset of subjects (N=25) using a touchscreen computer and reaction time task of the Cambridge Neuropsychological Test Automated Battery (CANTAB) as previously described (34,45)
Assessment of Plasma Cortisol and Immune Variables
Cortisol and the cytokines IFN-alpha, TNF-alpha and sTNFR2 were measured using radioimmunoassay and enzyme-linked immunosorbent assay, respectively. Assays were run in duplicate according to manufacturer’s specifications as previously described (see Supplementary Materials in Supplement 1)(31). Biological samples were analyzed by research staff blinded to clinical status of study participants.
Statistical Analysis
Differences between groups at baseline (Visit 1) were assessed using t-tests for continuous measures and Fischer’s Exact Test for categorical variables. To evaluate effects of IFN-alpha/ribavirin on sleep and the behavioral variables, repeated measures analysis of covariance (ANCOVA) was conducted. In the case of significant main effects of group or visit or a group X visit interaction, post-hoc comparisons between specific means were conducted using Fisher’s Least Significant Difference test. Where indicated, correlation coefficients were computed to evaluate associations among changes in PSG measures. All statistical analyses included the following covariates: age, sex, race, body mass index (BMI), and history of substance abuse and history of depression (both coded individually as present or absent). Each of these factors has been shown to contribute to risk of sleep disorders and/or depression (46–52).
As previously described, cortisol slope was calculated by log-transforming cortisol values and using the beta value of the regression of all cortisol concentrations obtained across the diurnal cycle (31). Larger beta values (i.e. values closer to zero) reflect a flatter slope. Evening (pm) cortisol was calculated as the lowest value among the last three blood draws (i.e. 7–9pm).
To determine the relationship between changes in relevant PSG variables and changes in behavioral, neurocognitive, neuroendocrine and immune outcomes, linear regression models were employed. Automated stepwise and forward elimination strategies were used to identify independent variable(s) of most consistent predictive value. Tests of significance were two-tailed with an alpha level of 0.05.
Results
Sample Characteristics
Age, race, gender, BMI and history of substance abuse were similar in IFN-alpha/ribavirin-treated subjects and controls (Table 1). Of note, there was a trend toward an increase in history of major depression in IFN-alpha/ribavirin-treated subjects. One African American female treated with IFN-alpha met symptom criteria for major depression at 4 weeks and immediately underwent study assessments. All other patients were studied after 12 weeks of IFN-alpha administration. Three patients in the IFN-alpha group were prescribed sleep medications by their treating physicians (2 received low dose non-benzodiazepine sedative/hypnotics as needed 3 times per week and 1 received 1mg lorazepam daily). These sleep aids were discontinued 48 hours prior to week 12 PSG.
Table 1.
Baseline demographic and psychiatric characteristics of study participants
| Characteristic | Interferon-alpha(n=19) | Control(n=12) | p-value |
|---|---|---|---|
| Age (mean, SD) | 48.6 (5.8) | 47.0 (7.3) | 0.53 |
| Gender (n, %) | |||
| Males | 12 (63.2) | 5 (41.7) | |
| Females | 7 (36.8) | 7 (58.3) | |
| Race (n, %) | |||
| Caucasian | 8 (42.1) | 5 (41.7) | |
| African American | 9 (47.4) | 6 (50.0) | |
| Other | 2 (10.5) | 1 (8.3) | |
| BMI | 30.0 (4.1) | 28.3 (5.1) | 0.32 |
| Past MD (n, %) | 6 (31.6) | 0 (0) | 0.06† |
| Past Substance Abuse (n, %) | 12 (63.1) | 7 (58.3) | 1.00† |
SD-standard deviation; BMI- body mass index; MD- Major Depression;
Fisher’s exact test
Sleep measures
As indicated by significant group by visit interactions, a number of sleep parameters including wake after sleep onset (F[1,23]=7.04, p=0.014), sleep efficiency (F[1,23]=6.83, p=0.016), Stage 2 sleep (F[1,23]=4.48, p=0.045), Stage 3/4 sleep (F[1,23]=8.58, p=0.008) and REM latency (F[1,23]=4.69, p=0.041) changed differentially across visits as a function of group (Table 2). Based on post hoc testing, compared to controls, IFN-alpha/ribavirin-treated subjects exhibited significant increases in wake after sleep onset, Stage 2 sleep and REM latency (all p<0.05). In addition, sleep efficiency and Stage 3/4 sleep significantly decreased in IFN-alpha-treated subjects compared to controls (all p<0.05). There was also a significant main effect of group on mean sleep latency in the MSLT (F[1,20]=4.70, p=0.042), with IFN-alpha-treated subjects exhibiting significantly longer mean sleep latency times compared to controls at Visit 2 (p<0.05) (Table 3). Despite significant IFN-alpha-induced increases in wake after sleep onset, no differences were found between groups in spontaneous arousals.
Table 2.
Mean (± SD) Sleep Parameters in IFN-alpha-Treated and Control Subjects
| Interferon-alpha (n=19) |
Control (n=12) |
|||||
|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Delta | Visit 1 | Visit 2 | Delta | |
| Sleep Period Time (min) | 488.9 (73.8) | 505.3 (53.7) | 16.4 (56.3)* | 511.7 (44.6) | 470.7 (58.5) | −41.0 (77.1) |
| Total Sleep Time (min) | 376.3 (61.1) | 345.1 (73.6) | −31.2 (72.7) | 387.5 (40.8) | 382.1 (46.3) | −5.5 (52.8) |
| WASO (min)† | 112.6 (62.6) | 160.2 (62.0)* | 47.6 (76.8)* | 124.2 (66.6) | 88.6 (35.8) | −35.6 (80.1) |
| Spontaneous Arousals | 90.2 (42.6) | 94.9 (53.4) | 4.7 (47.6) | 87.0 (31.0) | 92.7 (39.4) | 5.7 (21.8) |
| Total Sleep Efficiency† | 77.6 (11.4) | 68.0 (12.8)* | −9.6 (14.4)* | 76.3 (11.6) | 81.5 (6.2) | 5.2 (13.6) |
| Sleep Stages | ||||||
| Stage 1 (min) | 23.8 (8.2) | 31.5 (14.1) | 7.7 (13.8) | 29.2 (11.8) | 29.6 (13.3) | 0.4 (12.7) |
| Stage 2 (min)† | 203.9 (40.0) | 283.2 (51.8) | 79.3 (46.1)* | 215.9 (51.7) | 258.8 (41.7) | 42.8 (39.0) |
| Stage 3/4 (min)† | 62.1 (32.3) | 41.6 (26.2)* | −20.5 (24.9)* | 63.8 (32.9) | 61.9 (24.6) | −1.9 (15.2) |
| REM (min) | 86.1 (20.8) | 77.2 (26.1) | −8.9 (28.0) | 78.9 (16.5) | 80.8 (26.8) | 2.0 (29.4) |
| REM Latency (min)† | 81.3 (26.3) | 115.8 (67.8)* | 34.5 (64.4)* | 95.2 (41.1) | 81.5 (28.5) | −13.8 (46.0) |
SD-standard deviation; WASO-wake after sleep onset; REM-rapid eye movement sleep
- significantly different from respective Control value (p<0.05 using Fisher’s Least Significance Difference test);
- significant group X visit interaction (p<0.05); sleep efficiency=1− (wake after sleep onset/sleep period time)
Table 3.
Mean Sleep Latency Test Parameters (± SD) in IFN-alpha-Treated and Control Subjects
| Interferon-alpha (n=17) |
Control (n=10) |
|||||
|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Delta | Visit 1 | Visit 2 | Delta | |
| Mean Sleep Latency† | 8.9 (4.2) | 11.8 (5.2)* | 3.0 (4.3) | 7.9 (4.6) | 7.7 (3.8) | −0.2 (5.5) |
| Cumulative Sleep Time | 13.1 (3.0) | 11.2 (3.6) | −1.9 (4.4) | 14.9 (4.0) | 13.5 (4.5) | −1.4 (3.6) |
SD-standard deviation;
- significantly different from respective Control value (p<0.05 using Fishers Least Significance Difference test):
- significant group effect
Similar differences in delta sleep parameters between groups were revealed when IFN-alpha-treated patients with history of depression (n=6) were removed from the analyses. Moreover, there were no differences in delta nighttime sleep parameters between IFN-alpha-treated patients with and without history of depression. Finally, similar results were obtained when IFN-alpha-treated patients who were receiving sedative/hypnotics prior to Visit 2 (n=3) were removed from the analyses.
Of note, several significant correlations were found among sleep variables that differed as a function of IFN-alpha/ribavirin treatment, including significant correlations between delta (Visit2-Visit1) Stage 3/4 sleep and delta sleep efficiency (r=0.40, df=23, p=0.045); delta Stage 3/4 sleep and delta REM latency (r=−0.44, df=23, p=0.029); and delta sleep efficiency and delta wake after sleep onset (r=−0.64, df=23, p=0.001) (see also Table S1 in Supplement 1).
Behavioral Measures
There were significant group by visit interactions for both depression and fatigue (F[1,23]=10.81, p=0.003 and F[1,23]=18.33, p<0.001, respectively), with IFN-alpha/ribavirin-treated patients exhibiting significant increases in these symptoms during treatment compared to controls (Table 4). Interestingly, there were no main effects or interactions for daytime sleepiness (ESS), which showed no change across visits for either group.
Table 4.
Mean (± SD) Behavioral Parameters in IFN-alpha-Treated and Control Subjects
| Interferon-alpha (n=19) |
Control (n=12) |
|||||
|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Delta | Visit 1 | Visit 2 | Delta | |
| Sleepiness (ESS) | 6.1 (3.2) | 6.6 (3.7) | 0.4 (3.5) | 9.7 (5.7) | 8.0 (5.5) | −1.7 (1.4) |
| Fatigue (MFI)† | 38.3 (10.1) | 61.6 (19.5)* | 23.3 (18.4)* | 37.6 (13.1) | 34.5 (13.2) | −3.1 (6.1) |
| Depression (MADRS)† | 3.7 (5.4) | 12.7 (9.9)* | 9.0 (10.3)* | 2.1 (3.0) | 2.2 (2.8) | 0.2 (2.1) |
SD-standard deviation; ESS-Epworth Sleepiness Scale; MFI-multidimensional fatigue inventory; MADRS-Montgomery Asberg Depression Rating Scale;
- significantly different from respective Control value (p<0.05 using Fishers Least Significance Difference test);
- significant group X visit interaction
Relationship between Sleep Parameters and Behavioral Changes, Motor Slowing and Cortisol
Previous work has demonstrated that IFN-alpha leads to slowing of choice movement time on the reaction time task of the CANTAB, which in turn correlates with fatigue (34); a finding that was replicated in the current sample (see Table S3 in Supplement 1). In addition, IFN-alpha has been shown to be associated with significant increases in pm cortisol and flattening of the cortisol curve (31); both effects which were also replicated in these subjects (data not shown). Sleep parameters that showed significant differences between groups across Visits 1 and 2 were entered into linear regression models to determine their association with IFN-alpha-induced behavioral changes, motor slowing and alterations in cortisol secretion. Changes in nighttime sleep parameters were entered as independent variables, and delta depression and fatigue, delta choice movement time, delta cortisol slope, and delta pm cortisol were entered as dependent variables in separate analyses. Age, race, sex, BMI, history of substance abuse and history of depression were also entered into the models as covariates. Stepwise and forward elimination were used to determine variables that were significant predictors of the indicated dependent measures. In all analyses, these automated elimination strategies yielded similar results.
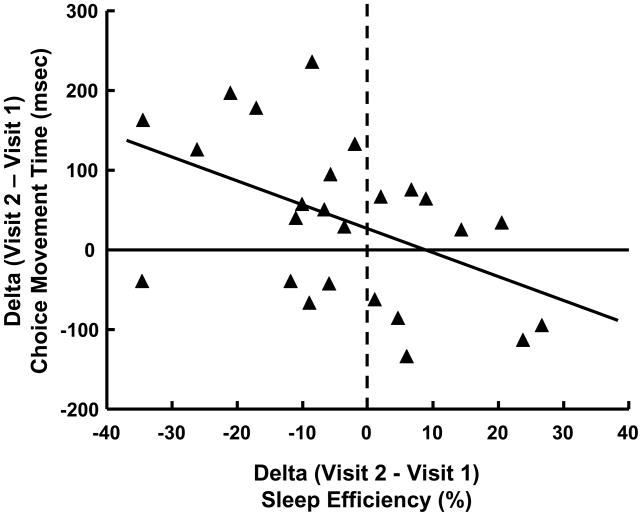
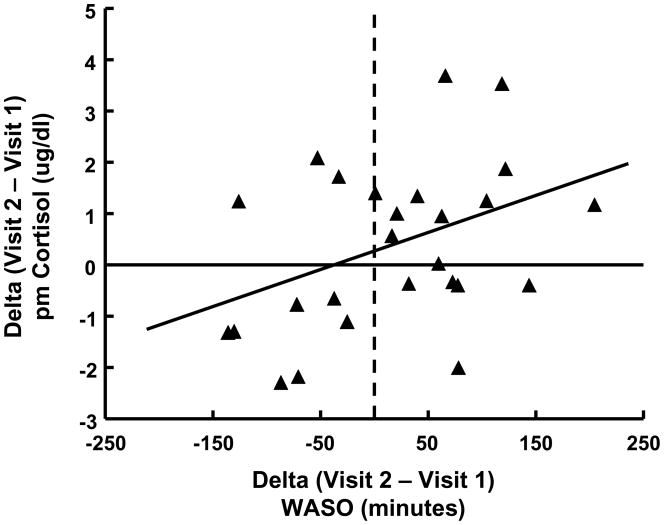
Both delta Stage 3/4 sleep and delta REM latency were significant predictors of changes in fatigue, together accounting for 34.1% of the variance (R2) in delta MFI scores (F[1,30]=7.25, p=0.003). More specifically, decreases in Stage 3/4 sleep and increases in REM latency were associated with increased fatigue (beta=−0.36, t=−2.19, df=2,30, p=0.037 and beta=0.60, t=2.21, df=2,30, p=0.035, respectively). Delta sleep efficiency was a significant predictor of changes in choice movement time (F[1,24]=5.06, p=0.034) with decreases in sleep efficiency being associated with increased choice movement time (beta=−0.42, t=−2.25, df=1,24, p=0.034) (Figure 1). Regarding diurnal cortisol secretion, delta REM latency was a significant predictor of changes in cortisol slope (F[1,29]=6.14, p=0.020) with increases in REM latency being associated with increases in (flattening of) cortisol slope (beta=0.42, t=−2.48, df=1,29, p=0.020). Finally, delta sleep after wake onset was a significant predictor of changes in pm cortisol (F[1,29]=5.6, p=0.025) with increases in wake after sleep onset being associated with increases in evening cortisol (beta=0.41, t=2.37, df=1,29, p=0.025) (Figure 2).
Figure 1. Correlation between change in sleep efficiency and change in motor speed.
Decreased sleep efficiency (%) across Visits 1 and 2 in IFN-alpha-treated and control patients was significantly associated with decreased motor speed as reflected by increased movement time (measured in milliseconds) on the choice movement component of the reaction time task of the Cambridge Neuropsychological Test Automated Battery (r=−0.42, N=25, p=0.034).
Figure 2. Correlation between change in wake after sleep onset and change in evening cortisol concentration.
Increased wake after sleep onset (WASO) (measured in minutes) across Visits 1 and 2 in IFN-alpha-treated and control patients was significantly associated with increased evening (pm) plasma cortisol concentrations (r=0.41, N=30, p=0.025)
Regarding daytime sleep assessments (MSLT), no significant associations were found between delta sleep latency and any behavioral, neurocognitive or neuroendocrine variable. Moreover, no sleep measures were associated with changes in depression scores. Finally, a comprehensive listing of bivariate correlations between delta sleep variables (as well as a composite sleep factor derived from principal components analysis) and the noted behavioral, neurocognitive, and neuroendocrine measures is provided in Table S2 (see Supplement 1).
Relationship between Sleep Parameters and Immune Mediators
IFN-alpha, TNF-alpha and sTNFR2 have been found to correlate with development of IFN-alpha-induced depression and/or fatigue (31). These correlations were also apparent with IFN-alpha and sTNFR2 in the current sample (see Table S3 in Supplement 1). To determine the relationship between changes in these cytokines and sleep variables that were altered by IFN-alpha, linear regression analyses were conducted entering delta IFN-alpha, delta TNF-alpha and delta sTNFR2 as independent variables and the sleep variables as the dependent variables in separate analyses. Analyses were controlled for age, race, sex, BMI, history of substance abuse and history of depression. Delta IFN-alpha was found to significantly predict changes in delta Stage 2 sleep (F[1,24]=10.6, p=0.003), with increases in IFN-alpha being associated with increases in delta Stage 2 sleep (beta=0.56, t=3.26, df=1,24, p=0.003). Similar relationships were observed with sTNFR2 when IFN-alpha was removed from the model (F[1,29]=5.2, p=0.031; beta=0.40, t=2.28, df=1,29, p=0.031), suggesting that sTNFR2-induced effects on Stage 2 sleep may be collinear with those of IFN-alpha. No other relationships between cytokines and sleep parameters were found (see also Table S2 in Supplement 1).
Discussion
Subjects chronically administered IFN-alpha demonstrated increased wake after sleep onset, decreased sleep efficiency and reduced Stage 3/4 sleep. These non-REM sleep disturbances are common in major depression and many medical illnesses and are consistent with the disruption of SWS seen in laboratory animals and humans acutely exposed to high doses of cytokines and cytokine inducers (3,7,8,13,53–55). By providing the first longitudinal evidence that cytokine exposure disrupts non-REM sleep in humans, these data suggest that dysregulation of inflammatory signaling pathways may be an important pathophysiologic mechanism for development of sleep disturbances including insomnia found in medical and psychiatric illnesses. Moreover, the current findings reinforce results from recent studies showing that pharmacological antagonism of innate immune cytokines (i.e. TNF-alpha) can reverse similar sleep disturbances in patients with rheumatoid arthritis and alcoholism (56,57).
IFN-alpha treatment increased REM latency, an effect also observed in humans following acute administration of cytokines (7,9–11), including IFN-alpha (10), but an effect that is opposite to the reduced REM latency that is a hallmark of major depression (58,59). Although little is known regarding REM sleep patterns in depressed individuals with a known source of chronic innate immune system activation (i.e. medically-ill individuals with major depression), these findings raise the intriguing possibility that cytokine-induced behavioral disturbances may have a unique REM phenotype.
In the current study, disturbances in REM and non-REM sleep independently predicted development of behavioral symptoms and physiological changes that are common in both major depression and medical illness, including fatigue, psychomotor slowing and disruptions in the diurnal rhythm of cortisol. Fatigue and loss of the normal descending diurnal cortisol rhythm have been repeatedly associated with increased markers of inflammation (31,37,60–68). Psychomotor slowing is also highly prevalent in depression and medical illness and has been linked to central nervous system effects of innate immune cytokines (34,69). The current study raises the possibility that cytokine-induced sleep disturbances may contribute to the effects of innate immune cytokines on development of these behavioral and physiological abnormalities that are widespread in sickness and depression and have been associated with innate immune cytokines. Numerous studies show that sleep—loss whether naturalistic (i.e. insomnia) or experimentally induced—promotes fatigue and impedes psychomotor performance. Studies show that experimentally-induced sleep loss also increases pm cortisol concentrations (36), all of which provides additional support for the hypothesis that sleep changes may represent a pathway by which cytokines affect behavior and physiological functioning.
Although acute infection and certain types of depression can be associated with hypersomnia, chronic cytokine exposure to IFN-alpha produced sleep alterations more consistent with insomnia. Despite significant increases in fatigue—a cardinal symptom of insomnia (70,71)—IFN-alpha administration did not increase subjective reports of daytime sleepiness, suggesting that, in the context of chronic inflammation, these two constructs (fatigue and sleepiness) are dissociable. Of note, a similar dissociation between fatigue and sleepiness has been observed in primary insomnia (72), a condition which has been repeatedly associated with prolonged sleep latency during the day (as observed in IFN-alpha-treated subjects) as well as increased inflammatory markers (73–78).
Like with primary insomnia (79,80), results from the current study suggest that chronic cytokine exposure may impair sleep quality by inducing a state of physiological hyperarousal that interferes with sleep continuity and depth and impedes attainment of restorative SWS. An adaptive, evolutionary perspective on this phenomenon suggests that hyperarousal may be a potentially beneficial tradeoff, given the increased danger a “sleepy”, infected or wounded animal might face from predation.
Several strengths and weaknesses of the study design warrant consideration. Strengths include use of an objective measure of sleep architecture (PSG) in humans prescreened for sleep disorders and chronically exposed to a standardized dose of an innate immune cytokine in the absence of medications known to affect sleep. The use of a control group not receiving IFN-alpha, but participating in all study procedures is also a strength, especially given that several sleep parameters improved in this group including wake after sleep onset and sleep efficiency, likely secondary to continuing adaptation to the GCRC environment. In terms of weaknesses, only IFN-alpha was administered, and therefore it is possible that administration of other cytokines may have different effects. Nevertheless, it should be noted that IFN-alpha induces multiple other cytokines (including TNF-alpha, IL-1 and IL-6), and both TNF-alpha and IL-6 have been shown to be related to sleep changes during IFN-alpha treatment (25,81). Moreover, as noted above, IFN-alpha-induced sleep changes are consistent with those reported following administration of high doses of innate immune cytokines or cytokine inducers to laboratory animals and humans, as well as being consistent with the clinical literature on sleep disturbances in medically ill patients and depressed patients, who have been shown to exhibit increased peripheral blood concentrations of multiple innate immune cytokines (82). It should also be noted that subjects were not randomized to treatment or control groups, thus potentially contributing to bias in group assignment. Nevertheless, all subjects were required to have been seen by a hepatologist and approved for IFN-alpha treatment, thus ensuring that all subjects had equal access to appropriate medical care for hepatitis C. Similarities in baseline sleep parameters between groups suggest group equivalency. However, by chance, 6 patients in the IFN-alpha-treated group had a history of major depression compared to 0 controls, potentially confounding reported group differences. Nevertheless, when groups were compared excluding patients with history of depression, similar results were obtained, and no significant differences in delta nighttime sleep parameters were found between IFN-alpha-treated patients with and without a depression history. Three patients had prn (n=2) or standing (n=1) sedative/hypnotic medications withheld 48 hours prior to the 12 week sleep study, thereby potentially leading to sleep alterations secondary to medication withdrawal. Nevertheless, when groups were compared excluding patients using sedative/hypnotics, similar results were found. Finally, we chose to study patients at 12 weeks because behavioral changes have been shown to plateau at this time during IFN-alpha treatment (83). Nevertheless, this later time point would not capture sleep difficulties during early stages of IFN-alpha therapy, which have been found to predict later development of depression (25).
In summary, results from this study support the notion that chronic cytokine exposure as a result of chronic medical or psychiatric illness and/or chronic stress may be a relevant causal mechanism in the association of these conditions with insomnia. Moreover, given studies demonstrating that sleep deprivation can activate innate immune cytokines and their signaling pathways (84), these data suggest that a feedforward cascade may exist between sleep and inflammation, whereby chronic inflammation can impair sleep which in turn can lead to increased inflammation. Treatments focused on specific targets in this inflammatory cascade including cytokines themselves (e.g. TNF-antagonists) as well as their signaling pathways (e.g. inhibitors of NF-kB) may be especially relevant in reversing this potentially vicious cycle.
Supplementary Material
Acknowledgments
This study was supported by grants from the National Institutes of Health to CLR (K23 MH064619, R01 MH070553) and AHM (K05 MH069124, R01 HL073921, T32 MH020018) as well as the Centers for Disease Control and Prevention. In addition, the study was supported by PHS Grant UL1 RR025008 from the Clinical and Translational Science Award program and PHS Grant M01 RR0039 from the General Clinical Research Center program, National Institutes of Health, National Center for Research Resources. The authors would like to thank Joseph “Max” Beck (deceased) for his assistance with the polysomnography scoring.
Footnotes
Financial Disclosures
Charles L. Raison has served as a speaker for Lilly and Wyeth and as a consultant or an advisory board member for Lilly and Wyeth and owns equity in ContemplativeHealth; David B. Rye has served as a consultant for Schering-Plough; Andrew H. Miller has served as a consultant for Schering-Plough, AstraZeneca, Janssen, and Centocor, and has received research funding from Centocor, GlaxoSmithKline, and Schering-Plough; Bobbi J Woolwine, Gerald Vogt, Breanne M. Bautista, and James R. Spivey reported no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of major depression. Trend Immun. 2006;27:24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Opp MR, Obal F, Jr, Krueger JM. Interleukin 1 alters rat sleep: temporal and dose-related effects. Am J Physiol. 1991;260:R52–58. doi: 10.1152/ajpregu.1991.260.1.R52. [DOI] [PubMed] [Google Scholar]
- 4.Krueger JM, Obal FJ, Fang J, Kubota T, Taishi P. The role of cytokines in physiological sleep regulation. Ann NY Acad Sci. 2001;933:211–221. doi: 10.1111/j.1749-6632.2001.tb05826.x. [DOI] [PubMed] [Google Scholar]
- 5.Opp MR. Cytokines and sleep. Sleep Med Rev. 2005;9:355–364. doi: 10.1016/j.smrv.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Krueger JM, Majde JA. Microbial products and cytokines in sleep and fever regulation. Crit Rev Immun. 1994;14:355–379. doi: 10.1615/critrevimmunol.v14.i3-4.70. [DOI] [PubMed] [Google Scholar]
- 7.Spath-Schwalbe E, Hansen K, Schmidt F, Schrezenmeier H, Marshall L, Burger K, et al. Acute effects of recombinant human interleukin-6 on endocrine and central nervous sleep functions in healthy men. J Clin Endocrin Metab. 1998;83:1573–1579. doi: 10.1210/jcem.83.5.4795. [DOI] [PubMed] [Google Scholar]
- 8.Benedict C, Scheller J, Rose-John S, Born J, Marshall L. Enhancing influence of intranasal interleukin-6 on slow-wave activity and memory consolidation during sleep. Faseb J. 2009;23:3629–3636. doi: 10.1096/fj.08-122853. [DOI] [PubMed] [Google Scholar]
- 9.Bauer J, Hohagen F, Gimmel E, Bruns F, Lis S, Krieger S, et al. Induction of cytokine synthesis and fever suppresses REM sleep and improves mood in patients with major depression. Biol Psychiatry. 1995;38:611–621. doi: 10.1016/0006-3223(95)00374-x. [DOI] [PubMed] [Google Scholar]
- 10.Spath-Schwalbe E, Lange T, Perras B, Fehm HL, Born J. Interferon-alpha acutely impairs sleep in healthy humans. Cytokine. 2000;12:518–521. doi: 10.1006/cyto.1999.0587. [DOI] [PubMed] [Google Scholar]
- 11.Pollmacher T, Mullington J, Korth C, Hinze-Selch D. Influence of host defense activation on sleep in humans. Adv Neuroimmunol. 1995;5:155–169. doi: 10.1016/0960-5428(95)00006-n. [DOI] [PubMed] [Google Scholar]
- 12.Imeri L, Opp MR. How (and why) the immune system makes us sleep. Nat Rev Neurosci. 2009;10:199–210. doi: 10.1038/nrn2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mullington J, Korth C, Hermann DM, Orth A, Galanos C, Holsboer F, et al. Dose-dependent effects of endotoxin on human sleep. Am J Physiol - Reg Integrat Compar Physiol. 2000;278:R947–955. doi: 10.1152/ajpregu.2000.278.4.R947. [DOI] [PubMed] [Google Scholar]
- 14.Gillin JC, Duncan W, Pettigrew KD, Frankel BL, Snyder F. Successful separation of depressed, normal, and insomniac subjects by EEG sleep data. Arch Gen Psychiatry. 1979;36:85–90. doi: 10.1001/archpsyc.1979.01780010091010. [DOI] [PubMed] [Google Scholar]
- 15.Kupfer DJ, Ulrich RF, Coble PA, Jarrett DB, Grochocinski VJ, Doman J, et al. Electroencephalographic sleep of younger depressives. Comparison with normals. Arch Gen Psychiatry. 1985;42:806–810. doi: 10.1001/archpsyc.1985.01790310068009. [DOI] [PubMed] [Google Scholar]
- 16.Kupfer DJ, Thase ME. The use of the sleep laboratory in the diagnosis of affective disorders. Psychiatr Clin N Am. 1983;6:3–25. [PubMed] [Google Scholar]
- 17.Benca RM, Peterson MJ. Insomnia and depression. Sleep Med. 2008;9(Suppl 1):S3–9. doi: 10.1016/S1389-9457(08)70010-8. [DOI] [PubMed] [Google Scholar]
- 18.Thase ME. Depression and sleep: pathophysiology and treatment. Dialogues Clin Neurosci. 2006;8:217–226. doi: 10.31887/DCNS.2006.8.2/mthase. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brunello N, Armitage R, Feinberg I, Holsboer-Trachsler E, Leger D, Linkowski P, et al. Depression and sleep disorders: clinical relevance, economic burden and pharmacological treatment. Neuropsychobiol. 2000;42:107–119. doi: 10.1159/000026680. [DOI] [PubMed] [Google Scholar]
- 20.Abad VC, Sarinas PS, Guilleminault C. Sleep and rheumatologic disorders. Sleep Med Rev. 2008;12:211–228. doi: 10.1016/j.smrv.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Ranjbaran Z, Keefer L, Stepanski E, Farhadi A, Keshavarzian A. The relevance of sleep abnormalities to chronic inflammatory conditions. Inflamm Res. 2007;56:51–57. doi: 10.1007/s00011-006-6067-1. [DOI] [PubMed] [Google Scholar]
- 22.Davidson JR, MacLean AW, Brundage MD, Schulze K. Sleep disturbance in cancer patients. Soc Sci Med. 2002;54:1309–1321. doi: 10.1016/s0277-9536(01)00043-0. [DOI] [PubMed] [Google Scholar]
- 23.Berry RB, Harding SM. Sleep and medical disorders. Med Clin North Am. 2004;88:679–703. ix. doi: 10.1016/j.mcna.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 24.Graham JE, Christian LM, Kiecolt-Glaser JK. Stress, age, and immune function: toward a lifespan approach. J Behav Med. 2006;29:389–400. doi: 10.1007/s10865-006-9057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prather AA, Rabinovitz M, Pollock BG, Lotrich FE. Cytokine-induced depression during IFN-alpha treatment: The role of IL-6 and sleep quality. Brain Behav Immun. 2009 doi: 10.1016/j.bbi.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Loftis JM, Hauser P. The phenomenology and treatment of interferon-induced depression. J Affect Dis. 2004;82:175–190. doi: 10.1016/j.jad.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 27.Schaefer M, Engelbrecht MA, Gut O, Fiebich BL, Bauer J, Schmidt F, et al. Interferon alpha (IFNa) and psychiatric syndromes: a review. Progr Neuro-Psychopharmacol Biol Psychiatry. 2002;26:731–746. doi: 10.1016/s0278-5846(01)00324-4. [DOI] [PubMed] [Google Scholar]
- 28.Kraus MR, Schafer A, Faller H, Csef H, Scheurlen M. Psychiatric symptoms in patients with chronic hepatitis C receiving interferon alfa-2b therapy. J Clin Psychiatry. 2003;64:708–714. doi: 10.4088/jcp.v64n0614. [DOI] [PubMed] [Google Scholar]
- 29.Raison CL, Demetrashvili M, Capuron L, Miller AH. Neuropsychiatric side effects of interferon-alpha: recognition and management. CNS Drugs. 2005;19:1–19. doi: 10.2165/00023210-200519020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor JL, Grossberg SE. The effects of interferon-alpha on the production and action of other cytokines. Semin Oncol. 1998;25:23–29. [PubMed] [Google Scholar]
- 31.Raison CL, Borisov AS, Woolwine BJ, Massung B, Vogt G, Miller AH. Interferon-alpha effects on diurnal hypothalamic-pituitary-adrenal axis activity: relationship with proinflammatory cytokines and behavior. Mol Psychiatry. 2008 doi: 10.1038/mp.2008.58. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raison CL, Borisov AS, Woolwine BJ, Vogt GJ, Massung B, Miller AH. Activation of CNS inflammatory pathways by interferon-alpha: relationship to monoamines and depression. Biol Psychiatry. 2008;65:296–303. doi: 10.1016/j.biopsych.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wichers MC, Kenis G, Koek GH, Robaeys G, Nicolson NA, Maes M. Interferon-alpha-induced depressive symptoms are related to changes in the cytokine network but not to cortisol. J Psychosom Res. 2007;62:207–214. doi: 10.1016/j.jpsychores.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 34.Majer M, Wellberg LAM, Capuron L, Pagnoni G, Raison CL, Miller AH. IFN-alpha-induced motor slowing is associated with increased depression and fatigue in patients with chronic hepatitis C. Brain Behav Immun. 2008;25:870–880. doi: 10.1016/j.bbi.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferrara M, De Gennaro L, Bertini M. The effects of slow-wave sleep (SWS) deprivation and time of night on behavioral performance upon awakening. Physiol Behav. 1999;68:55–61. doi: 10.1016/s0031-9384(99)00150-x. [DOI] [PubMed] [Google Scholar]
- 36.Leproult R, Copinschi G, Buxton O, Van Cauter E. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 1997;20:865–870. [PubMed] [Google Scholar]
- 37.Palesh O, Zeitzer JM, Conrad A, Giese-Davis J, Mustian KM, Popek V, et al. Vagal regulation, cortisol, and sleep disruption in women with metastatic breast cancer. J Clin Sleep Med. 2008;4:441–449. [PMC free article] [PubMed] [Google Scholar]
- 38.Dahlgren A, Kecklund G, Theorell T, Akerstedt T. Day-to-day variation in saliva cortisol--relation with sleep, stress and self-rated health. Biol Psychol. 2009;82:149–155. doi: 10.1016/j.biopsycho.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 39.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 40.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interveiw for DSM-IV-TR Axis I Disorders, Research Version. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 41.Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep. 1986;9:519–524. doi: 10.1093/sleep/9.4.519. [DOI] [PubMed] [Google Scholar]
- 42.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Brit J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 43.Smets EM, Garssen B, Bonke B, De Haes JC. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315–325. doi: 10.1016/0022-3999(94)00125-o. [DOI] [PubMed] [Google Scholar]
- 44.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 45.Lowe C, Rabbitt P. Test/re-test reliability of the CANTAB and ISPOCD neuropsychological batteries: theoretical and practical issues. Cambridge Neuropsychological Test Automated Battery. International Study of Post-Operative Cognitive Dysfunction. Neuropsychologia. 1998;36:915–923. doi: 10.1016/s0028-3932(98)00036-0. [DOI] [PubMed] [Google Scholar]
- 46.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10(Suppl 1):S3–6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 47.Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA, et al. Age differences in the prevalence and comorbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depress Anxiety. 2009 doi: 10.1002/da.20634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry. 2009;66:785–795. doi: 10.1001/archgenpsychiatry.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 51.Fergusson DM, Boden JM, Horwood LJ. Tests of causal links between alcohol abuse or dependence and major depression. Arch Gen Psychiatry. 2009;66:260–266. doi: 10.1001/archgenpsychiatry.2008.543. [DOI] [PubMed] [Google Scholar]
- 52.Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, et al. A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Arch Gen Psychiatry. 1998;55:694–700. doi: 10.1001/archpsyc.55.8.694. [DOI] [PubMed] [Google Scholar]
- 53.Burns JW, Crofford LJ, Chervin RD. Sleep stage dynamics in fibromyalgia patients and controls. Sleep Med. 2008;9:689–696. doi: 10.1016/j.sleep.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 54.Neu D, Mairesse O, Hoffmann G, Dris A, Lambrecht LJ, Linkowski P, et al. Sleep quality perception in the chronic fatigue syndrome: correlations with sleep efficiency, affective symptoms and intensity of fatigue. Neuropsychobiolol. 2007;56:40–46. doi: 10.1159/000110727. [DOI] [PubMed] [Google Scholar]
- 55.Majer M, Jones JF, Unger ER, Youngblood LS, Decker MJ, Gurbaxani B, et al. Perception versus polysomnographic assessment of sleep in CFS and non-fatigued control subjects: results from a population-based study. BMC Neurol. 2007;7:40. doi: 10.1186/1471-2377-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Irwin MR, Olmstead R, Valladares EM, Breen EC, Ehlers CL. Tumor necrosis factor antagonism normalizes rapid eye movement sleep in alcohol dependence. Biol Psychiatry. 2009;66:191–195. doi: 10.1016/j.biopsych.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zamarron C, Maceiras F, Mera A, Gomez-Reino JJ. Effect of the first infliximab infusion on sleep and alertness in patients with active rheumatoid arthritis. Ann Rheum Dis. 2004;63:88–90. doi: 10.1136/ard.2003.007831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders. A meta-analysis. Arch Gen Psychiatry. 1992;49:651–668. doi: 10.1001/archpsyc.1992.01820080059010. discussion 669–670. [DOI] [PubMed] [Google Scholar]
- 59.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66:1254–1269. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- 60.Bower JE, Ganz PA, Aziz N, Fahey JL. Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med. 2002;64:604–611. doi: 10.1097/00006842-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 61.Bower JE, Ganz PA, Dickerson SS, Petersen L, Aziz N, Fahey JL. Diurnal cortisol rhythm and fatigue in breast cancer survivors. Psychoneuroendocrinol. 2005;30:92–100. doi: 10.1016/j.psyneuen.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 62.Nijm J, Kristenson M, Olsson AG, Jonasson L. Impaired cortisol response to acute stressors in patients with coronary disease. Implications for inflammatory activity. J Int Med. 2007;262:375–384. doi: 10.1111/j.1365-2796.2007.01817.x. [DOI] [PubMed] [Google Scholar]
- 63.Rich T, Innominato PF, Boerner J, Mormont MC, Iacobelli S, Baron B, et al. Elevated serum cytokines correlated with altered behavior, serum cortisol rhythm, and dampened 24-hour rest-activity patterns in patients with metastatic colorectal cancer. Clin Cancer Res. 2005;11:1757–1764. doi: 10.1158/1078-0432.CCR-04-2000. [DOI] [PubMed] [Google Scholar]
- 64.Nater UM, Youngblood LS, Jones JF, Unger ER, Miller AH, Reeves WC, et al. Alterations in diurnal salivary cortisol rhythm in a population-based sample of cases with chronic fatigue syndrome. Psychosom Med. 2008;70:298–305. doi: 10.1097/PSY.0b013e3181651025. [DOI] [PubMed] [Google Scholar]
- 65.Kumari M, Badrick E, Chandola T, Adam EK, Stafford M, Marmot MG, et al. Cortisol secretion and fatigue: associations in a community based cohort. Psychoneuroendocrinol. 2009;34:1476–1485. doi: 10.1016/j.psyneuen.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 66.Torres-Harding S, Sorenson M, Jason L, Maher K, Fletcher MA, Reynolds N, et al. The associations between basal salivary cortisol and illness symptomatology in chronic fatigue syndrome. J Appl Biobehav Res. 2008;13:157–180. doi: 10.1111/j.1751-9861.2008.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lutgendorf SK, Weinrib AZ, Penedo F, Russell D, DeGeest K, Costanzo ES, et al. Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol. 2008;26:4820–4827. doi: 10.1200/JCO.2007.14.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pervanidou P, Kolaitis G, Charitaki S, Margeli A, Ferentinos S, Bakoula C, et al. Elevated morning serum interleukin (IL)-6 or evening salivary cortisol concentrations predict posttraumatic stress disorder in children and adolescents six months after a motor vehicle accident. Psychoneuroendocrinol. 2007;32:991–999. doi: 10.1016/j.psyneuen.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 69.Brydon L, Harrison NA, Walker C, Steptoe A, Critchley HD. Peripheral inflammation is associated with altered substantia nigra activity and psychomotor slowing in humans. Biol Psychiatry. 2008;63:1022–1029. doi: 10.1016/j.biopsych.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Buysse DJ, Thompson W, Scott J, Franzen PL, Germain A, Hall M, et al. Daytime symptoms in primary insomnia: a prospective analysis using ecological momentary assessment. Sleep Med. 2007;8:198–208. doi: 10.1016/j.sleep.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ustinov Y, Lichstein KL, Wal GS, Taylor DJ, Riedel BW, Bush AJ. Association between report of insomnia and daytime functioning. Sleep Med. 2009 doi: 10.1016/j.sleep.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 72.Bailes S, Libman E, Baltzan M, Amsel R, Schondorf R, Fichten CS. Brief and distinct empirical sleepiness and fatigue scales. J Psychosom Res. 2006;60:605–613. doi: 10.1016/j.jpsychores.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 73.Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14:9–15. doi: 10.1016/j.smrv.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 74.Edinger JD, Means MK, Carney CE, Krystal AD. Psychomotor performance deficits and their relation to prior nights’ sleep among individuals with primary insomnia. Sleep. 2008;31:599–607. doi: 10.1093/sleep/31.5.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Drake C, Richardson G, Roehrs T, Scofield H, Roth T. Vulnerability to stress-related sleep disturbance and hyperarousal. Sleep. 2004;27:285–291. doi: 10.1093/sleep/27.2.285. [DOI] [PubMed] [Google Scholar]
- 76.Okun ML, Coussons-Read M, Hall M. Disturbed sleep is associated with increased C-reactive protein in young women. Brain Behav Immun. 2009;23:351–354. doi: 10.1016/j.bbi.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.von Kanel R, Dimsdale JE, Ancoli-Israel S, Mills PJ, Patterson TL, McKibbin CL, et al. Poor sleep is associated with higher plasma proinflammatory cytokine interleukin-6 and procoagulant marker fibrin D-dimer in older caregivers of people with Alzheimer’s disease. J Am Geriatr Soc. 2006;54:431–437. doi: 10.1111/j.1532-5415.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 78.Hong S, Mills PJ, Loredo JS, Adler KA, Dimsdale JE. The association between interleukin-6, sleep, and demographic characteristics. Brain Behav Immun. 2005;19:165–172. doi: 10.1016/j.bbi.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 79.LeBlanc M, Beaulieu-Bonneau S, Merette C, Savard J, Ivers H, Morin CM. Psychological and health-related quality of life factors associated with insomnia in a population-based sample. J Psychosom Res. 2007;63:157–166. doi: 10.1016/j.jpsychores.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 80.Bonnet MH, Arand DL. 24-Hour metabolic rate in insomniacs and matched normal sleepers. Sleep. 1995;18:581–588. doi: 10.1093/sleep/18.7.581. [DOI] [PubMed] [Google Scholar]
- 81.Wichers MC, Kenis G, Koek GH, Robaeys G, Nicolson NA, Maes M. Interferon-alpha-induced depressive symptoms are related to changes in the cytokine network but not to cortisol. J Psychosom Res. 2007;62:207–214. doi: 10.1016/j.jpsychores.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 82.Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65:732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Raison CL, Borisov AS, Broadwell SD, Capuron L, Woolwine BJ, Jacobson IM, et al. Depression during pegylated interferon-alpha plus ribavirin therapy: prevalence and prediction. J Clin Psychiatry. 2005;66:41–48. doi: 10.4088/jcp.v66n0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Irwin MR, Wang M, Campomayor CO, Collado-Hidalgo A, Cole S. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Int Med. 2006;166:1756–1762. doi: 10.1001/archinte.166.16.1756. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.