Subclinical atherosclerosis demonstrated by coronary artery calcium score correlates with future regional wall motion abnormalities, with associated reduced systolic and diastolic function not predicted by specific recorded coronary events.
Abstract
Purpose:
To evaluate subclinical atherosclerosis measured by using coronary artery calcium (CAC) as a predictor of future left ventricular (LV) systolic and diastolic function in asymptomatic elderly participants.
Materials and Methods:
The institutional review boards of the University of Southern California and the Harbor University of California Los Angeles Research and Education Institute (where the South Bay Heart Watch study was initially conducted) approved this HIPAA-compliant study of 386 participants (mean age, 75.2 years) from among the original 1461 participants in the longitudinal South Bay Heart Watch prospective investigation of subclinical atherosclerosis. CAC at computed tomography was correlated with LV ejection fraction (LVEF), regional wall motion abnormalities (RWMAs), and peak filling rate (PFR) assessed a mean of 11.4 years ± 0.6 (standard deviation) later with cardiac magnetic resonance imaging. Analysis of variance and covariance testing was performed with the Wald test, testing for trends across the CAC groups. Covariates included age, level of total cholesterol, level of high-density lipoprotein cholesterol, systolic blood pressure, use of lipid-lowering medication, and smoking status.
Results:
Mean LVEF was 60.3% ± 9.9, with 11 (2.8%) of 386 participants having an LVEF of less than 40%. Forty-six (11.9%) of 386 participants had RWMAs. Higher CAC scores were associated with slightly lower LVEF (P for trend = .04) and a greater percentage of participants with decreased PFR (P for trend = .47) and RWMAs (P for trend = .01). After age- and risk factor–adjustment, only RWMA (P = .05) was associated with higher CAC. RWMAs were associated with significantly (P < .001) lower mean LVEF and PFR. Nineteen (41%) of 46 participants with RWMAs had documented Q-wave myocardial infarction, and three (7%) underwent coronary revascularization. CAC scores of 100 or greater were associated with a 2.2-fold (95% confidence interval: 1.30, 3.75) increase in RWMA (P < .001).
Conclusion:
Subclinical atherosclerosis assessed by using CAC is associated with an increased future likelihood of RWMA, as a marker of previous and possible subclinical coronary artery disease.
© RSNA, 2010
Supplemental material: http://radiology.rsna.org/lookup/suppl/doi:10.1148/radiol.10091868/-/DC1
Introduction
Coronary artery calcium (CAC) scores can modify the predicted risk of coronary artery disease obtained by using the Framingham Risk Score alone, especially among patients in the intermediate-risk category, where clinical decision making is most uncertain (1–6). There are limited published data available on the relationship of CAC to cardiac function. Fernandes et al (7) correlated reduced regional systolic peak left ventricular (LV) midwall circumferential strain and lower diastolic strain rate in participants with increased carotid intima-media thickness. Edvardsen et al (8) demonstrated regional abnormal systolic and diastolic wall strain related to expected supplying vessel CAC scores. In that study, participants with positive one- and two-vessel calcium scores had similar ejection fraction and stroke volumes as those with calcium scores of 0 (8). Neither increased carotid intima-media thickness nor elevated CAC was associated with reduced LV ejection fractions (LVEFs) or visible regional wall motion abnormalities (RWMAs) in these studies.
We hypothesize that subclinical atherosclerosis as measured by using CAC scores will correlate with future LVEF reduction and visible RWMAs as a marker of previous myocardial infarction or subclinical coronary artery disease. We also hypothesize that diastolic function as measured by peak filling rate (PFR) will also be reduced with elevated CAC. We tested this hypothesis over an 11-year follow-up period in the South Bay Heart Watch (SBHW) cohort of asymptomatic elderly participants.
Materials and Methods
Recruitment of Subjects
The SBHW (1,9,10) is a prospective cohort study designed to examine the value of CAC and both traditional and nontraditional risk factors for predicting cardiovascular outcomes and calcium progression in asymptomatic adults. The objective of our investigation was to utilize the SBHW cohort to prospectively evaluate CAC scores as predictors of future cardiac function. The study design of the SBHW has been described previously (1,2). The SBHW cohort comprises respondents to a community-based mailing campaign. The original cohort of 1461 participants greater than 45 years of age with multiple cardiac risk factors (8-year risk of developing coronary heart disease according to the Framingham risk equation, >10%) and without electrocardiographic (ECG) evidence or clinical history of myocardial infarction, revascularization, or typical angina was screened and enrolled between December 1990 and December 1992. Thirty months after enrollment (1993–1994), 1312 surviving participants underwent a second medical evaluation that included completion of a risk factor questionnaire, phlebotomy after fasting, ECG, and determination of CAC at electron-beam computed tomography (CT).
From May of 2005 to November of 2006 (a mean of 11.4 years ± 0.6 [standard deviation] later), 386 SBHW participants (mean age, 75.2 years ± 6.7) underwent functional analysis performed by using cardiac magnetic resonance (MR) imaging. Repeat risk factor questionnaire, ECG, and laboratory data were obtained at this time. Outcomes according to history, medical records, and death reports were evaluated and adjudicated by a panel of three cardiologists (including R.C.D.). The SBHW study timeline is displayed in Figure E1 (online).
All participants gave informed consent at the time of recruitment and again at the time of repeat risk factor assessment and CT and cardiac MR imaging. The Harbor University of California Los Angeles Research and Education Institute Human Participants Committee (at the center where the SBHW study was initially conducted) and the University of Southern California Institutional Review Board approved this Health Insurance Portability and Accountability Act–compliant study.
CAC Scoring
CT examinations were performed within a mean of 2 days ± 2 of the risk factor evaluations by using a previously described (11) and documented (10) technique with an electron-beam CT scanner (Imatron C-100; GE Healthcare, Milwaukee, Wis). CAC was calculated according to the Agatston method (12) with software identical to that used for the Multi-Ethnic Study of Atherosclerosis (13).
Cardiac MR Imaging
Participants completed questionnaires to determine their suitability for cardiac MR imaging. All examinations were performed by using a 1.5-T MR imaging unit (Horizon Echospeed EXCITE; GE Healthcare) with Advanced Cardiac Package acquisition software. A dedicated cardiac phased-array coil (Medical Advances, Milwaukee, Wis) was used. Heart rate and blood pressure were recorded before and after each examination. Coronal and axial breath-hold multisection steady-state free precession (SSFP) localizer images (repetition time msec/echo time msec, 3.6/1.6; flip angle, 45°; field of view, 44 cm) were acquired. A vertical long-axis two-chamber cardiac-triggered breath-hold SSFP cine sequence (3.2/1.4; flip angle, 45°; section thickness, 8 mm) was performed perpendicularly to the long axis of the LV. Contiguous breath-hold ECG-triggered 8-mm-thick short-axis two-dimensional SSFP cine images (3.6/1.6; flip angle, 45°; field of view, 44 cm; matrix, 224 × 224; 20 phase intervals over the cardiac cycle) were acquired from the apex to the base of the LV.
Typical examinations, which included two breath-hold localizer views, a single breath-hold vertical long-axis view, and contiguous short-axis breath-hold views from base to apex, were completed in 15 minutes.
Image Data Processing and Analysis
All coronary CAC CT and cardiac MR imaging Digital Imaging and Communications in Medicine data were stored on individual compact disks. Cardiac MR imaging data were transferred to a dedicated workstation (Advantage Windows Workstation 4.0; GE Healthcare) with cardiac processing software (MR Analysis Software Systems [MASS]; MEDIS, Leiden, the Netherlands). LV endocardial regions of interest (ROIs) were manually outlined for each of the 20 phases of each contiguous 8-mm short-axis section from the LV base to the apex. ROIs were initially manually outlined by physician trainees. All ROIs were reviewed at the workstation and were corrected by an expert (P.M.C., with 20 years of experience with cardiac cine MR imaging). Typically, 160 ROIs were outlined, measured, and recorded for the determination of end-diastolic volume (EDV) (in milliliters), end-systolic volume (in milliliters), stroke volume (in milliliters), and LVEF (as a percentage). Volume-time curves were created to measure PFR as LV EDV per second (14,15).
Vertical long-axis and short-axis cine views were reviewed and evaluated independently for regional wall motion by two investigators (J.E.S., with 3 years of experience with cardiac cine MR imaging, and P.M.C.). A 17-segment wall motion model (16) was applied, with wall motion scores recorded as follows: A score of 2 indicated normal wall motion; a score of 1, hypokinesia; a score of 0, akinesia; and a score of −1, dyskinesia. A completely normal 17-segment wall motion study received a score of 17 segments × two points = 34. Final wall motion determinations were decided by consensus. RWMAs were correlated with the most likely major culprit coronary vessel. Potential supplying coronary vessels were assigned as follows (17):
1. The basal anteroseptal, basal anterior, midanterolateral, midanterior, distal septal, distal anterior, and apical segments were assigned to the left anterior descending coronary artery.
2. The basal anterolateral, basal inferolateral, midanterolateral, midinferolateral, and distal lateral segments were assigned to the left circumflex coronary artery.
3. The basal septal inferior, basal inferior, midseptal inferior, midinferior, and distal inferior segments were assigned to the right coronary artery.
The physicians who performed the analysis and interpretation were blinded to all clinical data.
Statistical Analysis
MR imaging results were transmitted to the University of Southern California Statistical Consultation and Research Center and were merged with the SBHW master database.
Demographic and clinical characteristics collected at baseline for the SBHW cohort (n = 1461) were compared between the participants who underwent follow-up MR imaging at 11 years and the nonparticipants (because they were deceased, too ill to participate, lost to follow-up, declined to participate, or had a contraindication to MR imaging). Baseline characteristics were compared between groups by using the independent sample t test (for continuous variables) or the χ2 test (for discrete variables). In addition, differences between baseline and 11-year follow-up characteristics were evaluated for significance by using a paired t test. Pearson correlation coefficients were calculated to assess the agreement between the two readers in the wall motion assessment. κ Coefficients were calculated to assess interreader agreement for the absence or presence of RWMA.
Baseline CAC scores were categorized into the following four groups: a CAC score of 0, CAC scores of 1–99, CAC scores of 100–399, and CAC scores of 400 or greater. To test the hypotheses that there were differences across the four CAC groups, myocardial function parameters were compared by using an analysis of variance for continuous MR imaging variables (LVEF, diastolic PFR, wall motion score) and χ2 tests for discrete MR imaging variables (percentage of participants with LVEF < 50%, percentage of participants with diastolic PFR < 2.0 EDV per second, and percentage of participants with any RWMA). Tests for trends in myocardial function parameters across the four CAC groups were performed by using the Wald test for continuous variables and the χ2 trend test for discrete variables. Analyses of variance and covariance were performed by using the Wald test to test for trends across the CAC groups. Covariates included age, level of total cholesterol, level of high-density lipoprotein (HDL) cholesterol, systolic blood pressure, use of lipid-lowering medications, and smoking status.
All statistical tests were performed at the .05 significance level. Analyses were performed by using software (SAS, version 9.1; SAS Institute, Cary, NC).
Results
Of 1461 initially screened participants, 386 (26.4%) could be located and were able and willing to undergo cardiac MR imaging at a mean of 11.4 years ± 0.6. The distribution of reasons for nonparticipation were as follows: Five hundred three (46.8%) of the 1075 nonparticipants were deceased, 53 (4.9%) were too ill to participate or had another medical reason for not participating, 253 (23.5%) were lost to follow-up or did not participate for an unknown reason, 197 (18.3%) declined to participate, eight (<1%) had no baseline calcium score, and 61 (5.7%) had contraindications to MR imaging. Participants with MR imaging contraindications included 17 participants with pacemakers, 31 with claustrophobia, four with internal metal, and nine who were too large to image.
Participants were younger at screening (mean age, 63.8 years ± 6.7) than nonparticipants (66.6 years ± 8.1, P < .001) and were more likely to be men (913 [85%] of the 1075 nonparticipants vs 363 [94%] of the 386 participants, P < .001).
Participants with higher CAC scores at baseline had a greater likelihood of being unavailable for follow-up cardiac MR imaging: Among participants who were unavailable, 676 (62.8%) had a CAC score of 0, 748 (69.5%) had a CAC score of 1–99, 798 (74.1%) had a CAC score of 100–399, and 863 (80.2%) had a CAC score of 400 or greater (P < .001). Participants who were unavailable were more likely to have been treated with lipid-lowering medication (P for trend = .04).
Sociodemographic variables, risk factors, CAC scores, and myocardial function factors for the 386 participants are listed in Table 1. Agreement regarding individual wall motion assessment between the two readers was moderate, with a Pearson correlation coefficient of 0.57 (P < .001). Most independent wall motion disagreements related to selections of abnormal adjacent segments. The κ statistic for the absence or presence of RWMA was 0.45 (95% confidence interval: 0.31, 0.59), denoting moderate reviewer agreement. Consensus readings placed RWMAs in 105 (1.6%) of 6562 total segments (the 105 segments included 83 with hypokinesia, 19 with akinesia, and three with dyskinesia). Participants with RWMAs had a mean of two abnormal segments, with a mean wall motion score of 31.6 (of a possible total score of 34) ± 0.7. Of the 105 segments with RWMA, 38 were septal, 13 were anterior, 26 were lateral, 22 were inferior, and six were apical. Nineteen (41%) of 46 participants with RWMAs had previously experienced myocardial infarction according to their history and/or ECG data. Three (7%) of these 46 participants had a history of coronary revascularization without evidence of myocardial infarction. Thus, 22 (48%) of the 46 instances of RWMA correlated with clinical or ECG evidence of coronary artery disease. Twenty-four (52%) of the 46 participants with RWMAs did not have evidence of coronary events. Three of these participants had possible ischemia (ST or T-wave changes), and five had a widened QRS complex (>120 msec) according to ECG data (two participants had left bundle branch block, one had right bundle branch block, and two had nonspecific QRS widening). The two left bundle branch blocks were associated with septal hypokinesia. RWMA correlates are summarized in Table 2. LVEF averaged 62.0% ± 8.73 without RWMA and 48.4% ± 9.79 with RWMA (P < .001). Nine (82%) of 11 participants with an LVEF of less than 40% had RWMAs (P < .001, χ2 test).
Table 1.
Sociodemographic and MR Imaging Factors at Time of Cardiac MR imaging in 386 Participants
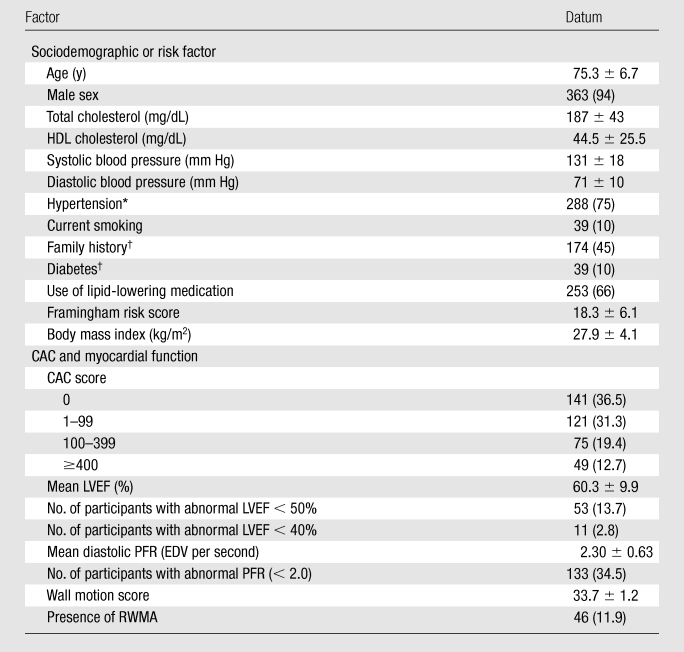
Note.—Continuous variables are presented as means ± standard deviations; discrete variables are presented as numbers of participants, with percentages in parentheses.
Hypertension was indicated by the use of hypertension-related medication, systolic blood pressure ≥ 140 mm Hg, and/or diastolic blood pressure ≥ 90 mm Hg.
Collected at baseline only.
Table 2.
Clinical and ECG Correlates in 46 Participants with RWMAs
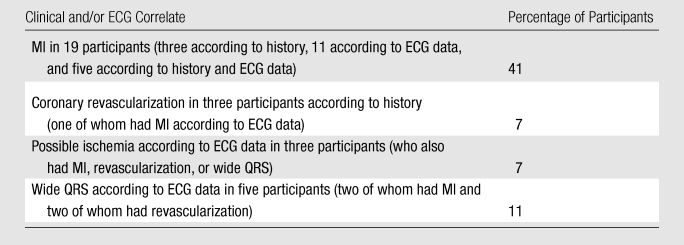
Note.—In total, clinical and/or ECG correlates were present in 30 (65%) of 46 participants with RWMAs. MI = myocardial infarction.
RWMAs in the expected circumflex coronary artery territory correlated with significantly increased CAC scores in the circumflex artery; such scores were 199.4 ± 406.3 in the presence of RWMA versus 28.3 ± 78.6 when no RWMA was present (P = .008). No significant specific vessel CAC–to-RWMA correlations were identified in the left anterior descending or right coronary artery territories. Analysis of specific CAC scores in the 16 participants with RWMAs and Q-wave infarction at ECG demonstrated significantly increased CAC in each of the vessels compared with those of the remaining 270 participants: In the left anterior descending artery, these 16 participants had a mean CAC score of 206.8 ± 322.5 (vs 65.7 ± 175.5 in the other participants, P = .001), while in the left circumflex artery, these 16 participants had a mean CAC score of 129.6 ± 340.7 (vs 29.0 ± 80.2 in the other participants, P = .008), and in the right coronary artery, these 16 participants had a mean CAC score of 232.5 ± 403.8 (vs 48.2 ± 166.5, P < .001). Mean total CAC score for the 16 participants with RWMAs and ECG evidence of Q-wave infarction was 759.5 ± 1282.4 (vs 153.0 ± 350.6 in the other participants, P < .001).
One hundred thirty-three (34.5%) of 386 participants had abnormal diastolic function (PFR < 2 EDV per second [18]). Mean PFR was 2.35 EDV per second ± 0.61 without RWMA and 1.84 EDV per second ± 0.61 with RWMA (P < .001).
Table 3 displays the results of LVEF, PFR, and RWMA with CAC. LVEF and PFR were correlated with each other for CAC scores of 0, 1–99, 100–399, and 400 or greater (Fig E2 [online]). Mean LVEF and PFR were lower in participants with RWMAs (P < .001). After age- and risk factor–adjusted multivariable analysis, only RWMAs (P < .05) were associated with higher CAC scores. Participants with CAC scores of 100 or greater were much more likely to have RWMAs: 19.4% (24 of 124) versus 8.4% (22 of 262) (relative risk = 2.2 [95% confidence interval: 1.30, 3.75], P = .003).
Table 3.
Association of Myocardial Function with CAC in 386 Participants
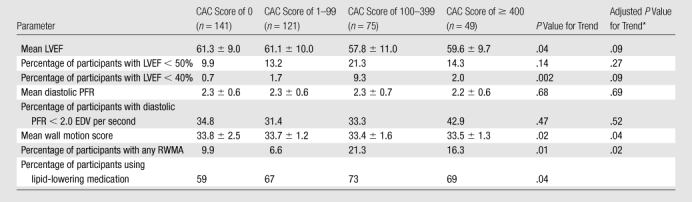
Adjusted for age, level of total cholesterol, level of HDL cholesterol, systolic blood pressure, use of lipid-lowering medication, and smoking status.
Discussion
CAC measured at autopsy (19,20), with fluoroscopy (21), or with CT (22–24) correlates with coronary artery disease and future coronary events (5–7,25–28), but its impact on the long-term development of systolic or diastolic dysfunction has not, to our knowledge, been previously investigated. We evaluated the relationship between CAC and future systolic and diastolic function measured 11 years later.
Minimally reduced mean LVEF and higher prevalence of decreased LVEF and minor reductions in PFR associated with higher baseline CAC scores did not reach statistical significance when corrected for age (29–31), level of total cholesterol, level of HDL cholesterol, systolic blood pressure, use of lipid-lowering medication, and smoking status.
The correlation of circumflex artery CAC with lateral RWMAs suggests the possibility that subclinical calcified plaque may be causally related to specific future events. Absence of similar correlation in the left anterior descending and right coronary artery territories might be explained by the higher percentage of ECG-demonstrated Q-wave infarcts in the circumflex territory (six of 11, 55%) than in the left anterior descending (five of 21, 24%) and right coronary artery (five of 14, 36%) territories. In any event, participants with RWMAs and Q-wave infarcts had significantly higher individual vessel and total CAC scores.
The greater prevalence of RWMAs associated with higher baseline levels of CAC demonstrated in this study may have clinical relevance. Participants with CAC scores of 100 or greater had more than double the chance of having an RWMA compared with participants with lower CAC scores. Participants with RWMAs had significantly lower mean LVEFs (48% vs 62%) and PFRs (1.84 vs 2.35 EDV per second). It is interesting that only 24% (11 of 46) of participants with RWMAs had a known history of myocardial infarction or coronary revascularization without a prior myocardial infarction and that an additional 22% (10 of 46) had unsuspected Q-wave infarcts demonstrated at ECG. These findings are congruent with the Framingham results for elderly participants aged 65–94 years; in that study, 30%–45% of those participants had unrecognized myocardial infarction detected at ECG (32).
While subclinical regional myocardial dysfunction is more likely in participants with elevated CAC, it is not known if this regional myocardial dysfunction is related to silent infarction, microvascular disease, or some other cause.
Our study had several limitations. Loss of participants, particularly in the long-term follow-up of elderly subjects, creates a potential preference for healthier individuals. From among the initially recruited 1461 SBHW participants, 1312 returned at 30 months for baseline risk factor analysis and CAC measurement. Three hundred eighty-six were available and agreeable to cardiac MR imaging 11 years after the initial CAC determination. Participants were younger (63.8 vs 66.6 years old at recruitment) than nonparticipants. Availability for cardiac MR imaging was significantly reduced in participants with higher baseline CAC scores, ranging from 37% of participants with CAC scores of 0 to 20% of participants with CAC scores of 400 or greater. It is likely that many of the 53 (4.9%) participants who were too ill to participate and the 503 (46.8%) participants who were deceased may have experienced coronary events. Thus, our cardiac MR imaging cohort had a lower prevalence of elevated CAC scores than might be expected from our baseline sample, and therefore true associations of CAC with cardiac function are probably stronger than what we observed. Moreover, the effects of lifestyle modification and medication on hypertension, diabetes, lipid levels, and atherosclerosis may have also played a role in attenuating relationships with future cardiac function. The original recruitment of the SBHW cohort by means of community mailer likely biased selection to participants with a greater interest in cardiovascular health. Such a cohort might be expected to be more compliant with recommended lifestyle changes and medications and perhaps to be less prone to adverse cardiac events.
While CAC is strong evidence for subclinical atherosclerosis, it is difficult to predict the amount of associated active lipid plaque burden. Sixty-six percent of the participants in this study were taking lipid-lowering medications. Study participants with higher CAC scores were significantly more likely to be taking lipid-lowering medications. Finally, given that the majority of our included participants were white and male, we were not able to examine relationships separately in women or in other ethnic groups; therefore, our findings have limited generalizability. Delayed contrast material–enhanced MR imaging would likely have added convincing supportive evidence regarding the relationship of RWMAs to prior myocardial events. Furthermore, because we only had a one-time measurement of cardiac function, we were unable to ascertain whether abnormalities detected at the time of the MR imaging examination were also present earlier (eg, at the time of the CAC examination 11 years earlier).
In conclusion, we found that subclinical atherosclerosis demonstrated by CAC score correlates with future RWMAs, with associated reduced systolic and diastolic function not predicted by specific recorded coronary events.
Advances in Knowledge.
Subclinical atherosclerosis demonstrated by coronary artery calcium (CAC) scores greater than 100 predicts a future 2.2-fold increased likelihood of clinically unsuspected left ventricular regional wall motion abnormalities (RWMAs); these RWMAs correlated with significantly (P < .001) lower left ventricular ejection fractions (48.4% vs 62.0%) and peak filling rates (1.84 vs 2.35 end-diastolic volume per second).
Participants with RWMAs and Q-wave infarction at electrocardiography demonstrated significantly increased baseline specific individual CAC scores than did participants without Q-wave infarctions.
Implications for Patient Care.
Patients with CAC scores of 100 or greater are more likely to have future left ventricular RWMAs with lower ejection fractions and decreased left ventricular diastolic filling rates.
Individual-vessel CAC scores may correlate with future RWMAs and Q-wave infarcts.
Supplementary Material
Received October 14, 2009; revision requested December 11; revision received February 10, 2010; accepted March 18; final version accepted April 28.
From the 2009 RSNA Annual Meeting.
Funding: This research was supported by the National Institutes of Health (grant NHLBI R01 HL063963 04A1).
Authors stated no financial relationship to disclose.
Abbreviations:
- CAC
- coronary artery calcium
- ECG
- electrocardiography
- EDV
- end-diastolic volume
- HDL
- high-density lipoprotein
- LV
- left ventricle
- LVEF
- LV ejection fraction
- PFR
- peak filling rate
- RWMA
- regional wall motion abnormality
- SBHW
- South Bay Heart Watch
References
- 1.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA 2004;291(2):210–215 [DOI] [PubMed] [Google Scholar]
- 2.Greenland P, Bonow RO, Brundage BH, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol 2007;49(3):378–402 [DOI] [PubMed] [Google Scholar]
- 3.Taylor AJ, Bindeman J, Feuerstein I, Cao F, Brazaitis M, O’Malley PG. Coronary calcium independently predicts incident premature coronary heart disease over measured cardiovascular risk factors: mean three-year outcomes in the Prospective Army Coronary Calcium (PACC) project. J Am Coll Cardiol 2005;46(5):807–814 [DOI] [PubMed] [Google Scholar]
- 4.Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol 2005;46(1):158–165 [DOI] [PubMed] [Google Scholar]
- 5.Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation 2003;107(20):2571–2576 [DOI] [PubMed] [Google Scholar]
- 6.Vliegenthart R, Oudkerk M, Hofman A, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation 2005;112(4):572–577 [DOI] [PubMed] [Google Scholar]
- 7.Fernandes VR, Polak JF, Edvardsen T, et al. Subclinical atherosclerosis and incipient regional myocardial dysfunction in asymptomatic individuals: the Multi-Ethnic Study of Atherosclerosis (MESA). J Am Coll Cardiol 2006;47(12):2420–2428 [DOI] [PubMed] [Google Scholar]
- 8.Edvardsen T, Detrano R, Rosen BD, et al. Coronary artery atherosclerosis is related to reduced regional left ventricular function in individuals without history of clinical cardiovascular disease: the Multiethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol 2006;26(1):206–211 [DOI] [PubMed] [Google Scholar]
- 9.Secci A, Wong N, Tang W, Wang S, Doherty T, Detrano R. Electron beam computed tomographic coronary calcium as a predictor of coronary events: comparison of two protocols. Circulation 1997;96(4):1122–1129 [DOI] [PubMed] [Google Scholar]
- 10.Wang S, Detrano RC, Secci A, et al. Detection of coronary calcification with electron-beam computed tomography: evaluation of interexamination reproducibility and comparison of three image-acquisition protocols. Am Heart J 1996;132(3):550–558 [DOI] [PubMed] [Google Scholar]
- 11.Detrano RC, Wong ND, Doherty TM, et al. Coronary calcium does not accurately predict near-term future coronary events in high-risk adults. Circulation 1999;99(20):2633–2638 [DOI] [PubMed] [Google Scholar]
- 12.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15(4):827–832 [DOI] [PubMed] [Google Scholar]
- 13.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 2002;156(9):871–881 [DOI] [PubMed] [Google Scholar]
- 14.Hoff FL, Turner DA, Wang JZ, Barron JT, Chutuape MD, Liebson PR. Semiautomatic evaluation of left ventricular diastolic function with cine magnetic resonance imaging. Acad Radiol 1994;1(3):237–242 [DOI] [PubMed] [Google Scholar]
- 15.Kudelka AM, Turner DA, Liebson PR, Macioch JE, Wang JZ, Barron JT. Comparison of cine magnetic resonance imaging and Doppler echocardiography for evaluation of left ventricular diastolic function. Am J Cardiol 1997;80(3):384–386 [DOI] [PubMed] [Google Scholar]
- 16.Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105(4):539–542 [DOI] [PubMed] [Google Scholar]
- 17.Pereztol-Valdés O, Candell-Riera J, Santana-Boado C, et al. Correspondence between left ventricular 17 myocardial segments and coronary arteries. Eur Heart J 2005;26(24):2637–2643 [DOI] [PubMed] [Google Scholar]
- 18.Maceira AM, Prasad SK, Khan M, Pennell DJ. Normalized left ventricular systolic and diastolic function by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2006;8(3):417–426 [DOI] [PubMed] [Google Scholar]
- 19.McCarthy JH, Palmer FJ. Incidence and significance of coronary artery calcification. Br Heart J 1974;36(5):499–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rifkin RD, Parisi AF, Folland E. Coronary calcification in the diagnosis of coronary artery disease. Am J Cardiol 1979;44(1):141–147 [DOI] [PubMed] [Google Scholar]
- 21.Margolis JR, Chen JT, Kong Y, Peter RH, Behar VS, Kisslo JA. The diagnostic and prognostic significance of coronary artery calcification. A report of 800 cases. Radiology 1980;137(3):609–616 [DOI] [PubMed] [Google Scholar]
- 22.Mautner SL, Mautner GC, Froehlich J, et al. Coronary artery disease: prediction with in vitro electron beam CT. Radiology 1994;192(3):625–630 [DOI] [PubMed] [Google Scholar]
- 23.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study. Circulation 1995;92(8):2157–2162 [DOI] [PubMed] [Google Scholar]
- 24.Mintz GS, Pichard AD, Popma JJ, et al. Determinants and correlates of target lesion calcium in coronary artery disease: a clinical, angiographic and intravascular ultrasound study. J Am Coll Cardiol 1997;29(2):268–274 [DOI] [PubMed] [Google Scholar]
- 25.Sangiorgi G, Rumberger JA, Severson A, et al. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol 1998;31(1):126–133 [DOI] [PubMed] [Google Scholar]
- 26.O’Malley PG, Taylor AJ, Jackson JL, Doherty TM, Detrano RC. Prognostic value of coronary electron-beam computed tomography for coronary heart disease events in asymptomatic populations. Am J Cardiol 2000;85(8):945–948 [DOI] [PubMed] [Google Scholar]
- 27.Keelan PC, Bielak LF, Ashai K, et al. Long-term prognostic value of coronary calcification detected by electron-beam computed tomography in patients undergoing coronary angiography. Circulation 2001;104(4):412–417 [DOI] [PubMed] [Google Scholar]
- 28.Poulsen SH, Jensen SE, Egstrup K. Longitudinal changes and prognostic implications of left ventricular diastolic function in first acute myocardial infarction. Am Heart J 1999;137(5):910–918 [DOI] [PubMed] [Google Scholar]
- 29.Bryg RJ, Williams GA, Labovitz AJ. Effect of aging on left ventricular diastolic filling in normal subjects. Am J Cardiol 1987;59(9):971–974 [DOI] [PubMed] [Google Scholar]
- 30.Sinak LJ, Clements IP. Influence of age and sex on left ventricular filling at rest in subjects without clinical cardiac disease. Am J Cardiol 1989;64(10):646–650 [DOI] [PubMed] [Google Scholar]
- 31.Schulman SP, Lakatta EG, Fleg JL, Lakatta L, Becker LC, Gerstenblith G. Age-related decline in left ventricular filling at rest and exercise. Am J Physiol 1992;263(6 Pt 2):H1932–H1938 [DOI] [PubMed] [Google Scholar]
- 32.Kannel WB, Abbott RD. Incidence and prognosis of unrecognized myocardial infarction: an update on the Framingham study. N Engl J Med 1984;311(18):1144–1147 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


